1. Introduction
Inflammatory Bowel Disease (IBD) are heterogenic inflammatory conditions, characterized by chronic inflammation of the bowel. The relapsing intestinal inflammation frequently results in abdominal pain, fatigue, weight loss, and diarrhea[
1]. The most common IBD subtypes are ulcerative colitis (UC) and Crohn's disease (CD). IBD typically presents during adolescence or early adulthood[
2]. Accordingly, the disease onset coincide with the time many people establish relationships[
3]. Intimacy, sexuality and reproductive issues are for this reason of great importance to patients with IBD[
4], and they seek information and support often without receiving it[
5,
6].
Sexual dysfunction (SD) is defined as “a sexual problem that is persistent or recurring and causes marked personal distress or interpersonal difficulty”[
7]. SD and reduced fertility are seen in both female and male IBD patients[
3,
8,
9,
10,
11,
12,
13]. By nature, these concerns
differ between women and men but are also depending on the subtype of IBD[
13,
14]
. Disease-specific factors such as duration and activity of the disease, drug use and surgical procedures may contribute to the clinical picture, and control of IBD activity does not appear to be sufficient to improve patients’ quality of life[
15]. Overall, there is a lack of knowledge in how to best support patients with IBD within the areas of intimacy and sexuality[
3,
12]. Clinical guidelines for the treatment of SD in patients with IBD are lacking[
15], albeit patients inquire information from an IBD specialist. Improved clinical awareness and understanding of the etiology, risk factors, and impact of SD for patients with IBD are suggested to result in improved diagnosis, care, and ultimately better health and wellbeing for this patient population[
3,
12,
16].
The aim of the study was to investigate the experiences of intimacy and sexuality related problems among Swedish patients with IBD and to explore patients’ and healthcare professionals’ experiences of discussing these topics.
2. Materials and Methods
2.1. Study design
This study was a cross-sectional cohort investigation that utilized two distinct, internet-based and study-specific questionnaires (Supplementary material 1 and 2). The first questionnaire was designed to examine the experiences of patients with IBD regarding how the disease and its treatment impacts relationships and sexuality, as well as how these issues are addressed by the healthcare system. It included seven questions, four of which were general (age, gender, type of disease, previous surgeries). The remaining three questions had a qualitative approach with free text answers.
The second questionnaire aimed to explore healthcare professionals' perspectives on discussing relationship and sexuality-related matters with IBD patients. It contained 19 questions, six of which were general (profession, gender, age, and work experience).
Both surveys were presented to representatives of the Swedish Patient Association for diseases and functional disorders of the gastrointestinal tract (Magtarmförbundet) and healthcare providers, respectively, and underwent several revisions before reaching their final forms. The on-line patient survey was closed after eight weeks due to the large number of responses. The healthcare professionals' survey remained open for five months. The study was approved by the national ethical review board, Etikprövningsnämnden (registration number: 2025-00089-01).
2.2. Study population
From the Swedish Patient Association, a cohort of patients with IBD was identified. Healthcare professionals were identified through members registries of professionals working with IBD-patients; the Swedish Society of Gastroenterology, the Swedish Society for Colon and Rectal Surgeons, the Swedish Association for Gastroenterological Nursing, the Swedish Society for Pediatric Gastroenterology, Hepatology and Nutrition, the Swedish Society of Young Gastroenterologists, the Association for Stoma Therapists and Nurses in Colorectal Care, as well as users of the Swedish Inflammatory Bowel Disease Registry.
2.3. Survey distribution
For the patient survey, an invitation letter was sent to all members of Swedish Patient Association for diseases and functional disorders of the gastrointestinal tract with a registered IBD diagnosis, and for the healthcare professionals survey, an invitation letter was sent to the professional associations described above. The letters contained information about the study and a link to the electronic questionnaire hosted on the secure Webropol research environment (Helsinki, Finland). All answers were anonymous and could not be traced back to individual responders. One reminder was sent halfway through the survey´s opening time. Participants were not offered any kind of economical or other compensation.
2.3. Statistical analysis
For the patient survey, characteristics, including age, gender, diagnosis and previous surgical procedures were collected for all respondents. Descriptive statistics were reported as mean or proportions. Free text responses regarding relationships and sexuality were analysed qualitatively with content analysis. A frequency analysis was performed where the occurrence of specific words, phrases, or themes were examined. The number of times that particular words, phrases, or topics appeared in the data were quantified providing an understanding in primary concerns, perceptions, and priorities for an individual topic.
For the healthcare professional survey, characteristics, including profession, age, gender, number of working years in the IBD-field were gathered for all respondents. Characteristics and responses concerning relationships and sexuality were reported as mean or proportions. The analyses were conducted in SPSS version 29.0.2.0.
3. Results
From the Swedish Patient Association, 2,274 patients with IBD diagnosis were identified. The survey was completed by 556 individuals giving a response rate of 24%. The number of healthcare professionals who received the request to complete the second survey through the professional associations working with IBD-patients was not recorded, but 118 responded to the questionnaire.
3.1. The IBD cohort
The patients were on average 55 years at the conduct of the study (
Table 1) and the majority (69%) were women. The distribution between UC (46%) and CD (45%) were even, while microscopic colitis (6%) and IBD-unclassified (3%) were uncommon. About a third (36) had previously undergone surgery due to IBD.
Most responders (78%) reported problems related to relationships and sexuality (
Table 2). Common physical issues included pain (n=76), fecal incontinence or urgency (n=61), and bloating or gas (n=48). Frequent psychological problems were fear of fecal leaking (n=76), decreased sexual desire (n=62), and fatigue (n=42). Several patients (n=12) reported the need to carefully plan sexual activity, whereas others (n=13) indicated they avoided intimate relationships altogether.
A majority (64%) of respondents considered healthcare professionals to be essential in addressing sexuality as a natural part of care. Despite this, 84% of participants had never initiated discussions on these topics, attributing this to factors such as embarrassment, time constraints at outpatient visits, or overall limited interaction with healthcare providers. In addition, many sought accesses to a psychologist or social worker, ideally with involvement from their partner.
3.2. The healthcare professional cohort
Among the healthcare respondents, 54% were IBD nurses, 29% gastroenterologists, 10% surgeons, and 7% had other professions; no dieticians participated (
Table 3). Most were female (76%), 22% male, and 2% did not specify their gender. The majority worked at university hospitals (51%), followed by county hospitals (15%), private hospitals (14%), regional hospitals (13%), private healthcare receptions (6%), and primary care (1%). Median IBD experience was 13 years (IQR 15), and median age was 47 years (IQR 13).
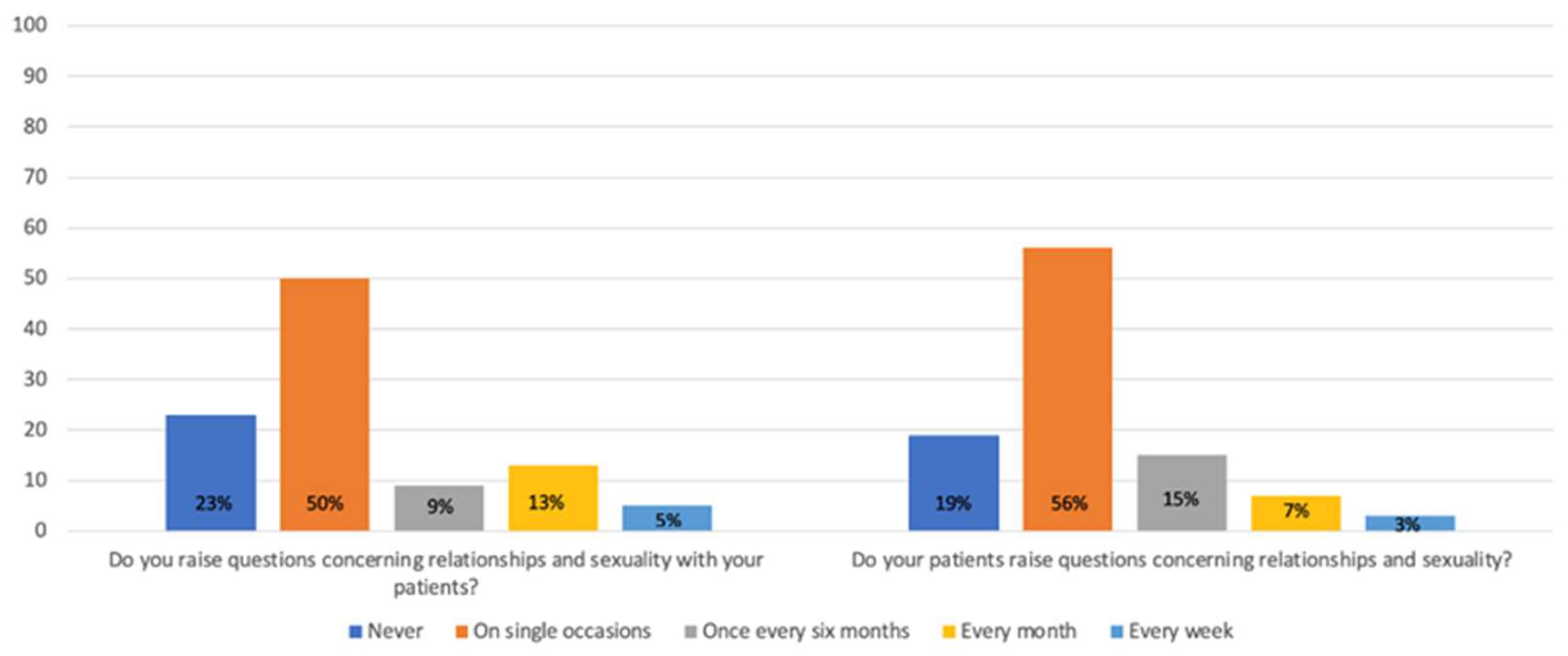
Overall, responses were consistent across professional groups; therefore, results are presented for the entire cohort. Half of the respondents indicated that they occasionally address issues related to relationships and sexuality with their patients, while 23% reported that they never discuss these topics (
Figure 1). Similarly, 56% stated that patients occasionally initiate such conversations, whereas 19% said this never happens (
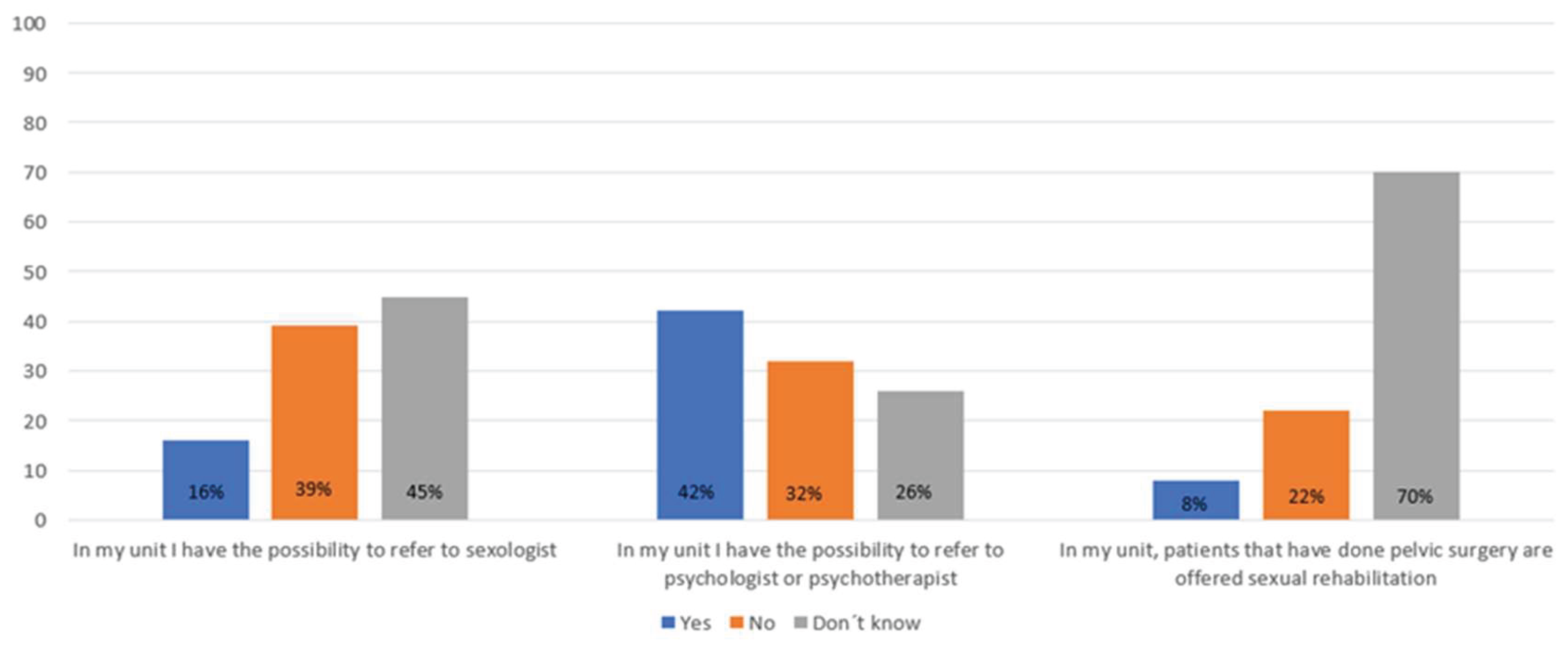
Figure 1). Only 15% of respondents reported having access to a sexologist, while 45% had the possibility to refer patients to a psychologist or psychotherapist (
Figure 2). Only 8% of the healthcare providers reported that they offered sexual rehabilitation to patients following pelvic surgery.
When patients with IBD raise concerns related to relationships and sexuality, the most frequently reported issues, according to healthcare professionals, include fertility concerns among women and erectile dysfunction among men. Healthcare professionals also observed that both male and female patients experience reduced sexual desire, feelings of unattractiveness, and anxiety about possible fecal leakage. Issues and concerns related to the presence of a stoma were also frequently mentioned. Among women, pain during intercourse—often associated with perianal fistulas or abdominal discomfort—was commonly reported.
4. Discussion
This study highlights the often underrecognized impact of IBD on interpersonal relationships and sexual health, revealing substantial gaps in how these issues are addressed within clinical settings. The majority of patients with IBD responding to the survey reported significant challenges related to relationships and sexuality, with physical symptoms like pain, fecal urgency, and bloating, as well as psychological factors such as fear of leakage and reduced sexual desire, all playing key roles for the development of SD. Despite the clear need, healthcare professionals do not routinely address these concerns, with only 50% occasionally raising the topic with patients. As a result, individual patients are likely seldom, if ever, asked about SD, in line with previous studies[
6,
17,
18].
Our findings align with the existing literature that demonstrates how IBD-related symptoms, such as perianal disease or abdominal discomfort, contribute to decreased sexual function and quality of life for both male and female patients[
12,
14,
16,
19]. Notably, our results indicate that issues such as erectile dysfunction in men and pain during intercourse in women, often linked to perianal fistulas or pelvic discomfort, are common. Furthermore, psychological factors like feelings of unattractiveness and concerns about fecal incontinence, frequently reported by both genders, have a profound impact on intimacy and self-esteem. The presence of a stoma[
20] was additionally reported to be associated with SD. These results emphasize the need for a more personalized and comprehensive care that addresses both the physical and psycho-social aspects of IBD[
5,
14,
16,
17].
Despite a clear wish (64%) from patients for healthcare providers to initiate discussions about sexuality as a routine part of care, 84% of patients had never themselves brought up the topic. This gap indicates a potential discomfort or reluctance from both patients and healthcare providers in addressing sensitive subjects. Time constraints, perceived embarrassment, and a lack of structured guidelines for discussing sexual health within the IBD context may contribute to this neglect[
5,
17]. This aligns with our previous studies indicating that healthcare professionals also tend to overlook the closely related topic of fertility[
1,
21]. Taken together, the findings suggest a broader pattern of unmet needs in which sensitive, yet crucial, aspects of patients’ sexual and reproductive health are insufficiently integrated into routine care[
5,
17].
In terms of clinical practice, the availability of resources for managing relational and sexual health concerns remains limited. Although 45% of healthcare professionals reported access to psychological support services, only 15% had the ability to refer patients to a sexologist. This limited access to multidisciplinary care highlights the need for a greater integration of sexual health and psychosocial services within IBD care, given the profound impact of SD on overall patient well-being[
6,
14,
17].Authors should discuss the results and how they can be interpreted from the perspective of previous studies and of the working hypotheses. The findings and their implications should be discussed in the broadest context possible. Future research directions may also be highlighted.
The strengths of this study lie in the inclusion of both patient and healthcare professional perspectives, providing a dual lens through which to assess the management of sexual health in IBD. An additional strength is the qualitive approach in the patient survey, enabling patients to freely describe their concerns with their own words. The relatively low patient response rate (24%) introduces a potential selection bias, and we cannot exclude that individuals with more pronounced issues may have been over- or underrepresented. Given the qualitative design, further data collection was deemed methodologically unfeasible, and the survey was closed after exceeding 500 responses. Moreover, the lack of the total number of invited healthcare professionals limits the ability to assess the representativeness of the responses.
5. Conclusions
In conclusion, our findings highlight the significant, yet often neglected, impact of sexual health issues among patients with IBD, underscoring the need for routine screening and proactive discussions in clinical practice. Given the complexity of SD in IBD, a multidisciplinary approach, involving gastroenterologists, nurses, psychologists, and sexologists, is critical to addressing the full spectrum of patient needs. Future research should focus on developing standardized protocols for integrating relational and sexual health discussions into routine IBD care and exploring the benefits of specialized interventions aimed at improving sexual function and quality of life for the patients.
Informed Consent Statement
Invitation on participation in the study was sent from the Swedish Patient Association and by answering the questionnaire informed consent was obtained. The same procedure was used to health care professionals but with help from different work associations. The study reports anonymized responses to two internet based questioners where none of the responding patients or healthcare personnel could be linked to any of the responses obtained.
Supplementary Materials
The following supporting information can be downloaded at the website of this paper posted on Preprints.org. Supplementary material 1: questionnaire to patients; Supplemenatary material 2: questionnaire to health care professionals.
Author Contributions
Conceptualization, S.A and S.J.; methodology, E.D, S.A, and S.J; software, SJ.; formal analysis, E.D and S.J; investigation, E.D, S.A and S.J.; data curation, S.J; writing—original draft preparation, E.D.; writing—review and editing, P.M, E.F, A.F, F.B, S.A and S.J; visualization, E.D and S.J: project administration, S.J, and S.A.; funding acquisition, E.D. All authors have read and agreed to the published version of the manuscript.
Funding
This work was supported by grants from Futurum – Academy for Health and Care, Region Jönköping County, Sweden (FUTURUM-1004805) to ED.
Institutional Review Board Statement
The study was approved by the national ethical review board, Etikprövningsnämnden (registration number: 2025-00089-01).
Data Availability Statement
Compiled de-identified survey responses will be shown upon request.
Conflicts of Interest
The authors declare no conflicts of interest. The funders had no role in the design of the study; in the collection, analyses, or interpretation of data; in the writing of the manuscript; or in the decision to publish the results.
Abbreviations
The following abbreviations are used in this manuscript:
| CD |
Crohn´s disease |
| IBD |
Inflammatory bowel disease |
| SD |
Sexual dysfunction |
| UC |
Ulcerative colitis |
References
- Singh, S.; Blanchard, A.; Walker, J.R.; Graff, L.A.; Miller, N.; Bernstein, C.N. Common Symptoms and Stressors Among Individuals With Inflammatory Bowel Diseases. Clin. Gastroenterol. Hepatol. 2011, 9, 769–775. [Google Scholar] [CrossRef] [PubMed]
- Nørgård, B.M.; Nielsen, J.; Fonager, K.; Kjeldsen, J.; Jacobsen, B.A.; Qvist, N. The incidence of ulcerative colitis (1995–2011) and Crohn's disease (1995–2012) — Based on nationwide Danish registry data. J. Crohn’s Colitis 2014, 8, 1274–1280. [Google Scholar] [CrossRef] [PubMed]
- Boyd, T.; de Silva, P.S.; Friedman, S. Sexual Dysfunction in Female Patients with Inflammatory Bowel Disease: An Overview. Clin. Exp. Gastroenterol. 2022, ume 15, 213–224. [Google Scholar] [CrossRef] [PubMed]
- Maunder, R.; Toner, B.; de Rooy, E.; Moskovitz, D. Influence of Sex and Disease on Illness-Related Concerns in Inflammatory Bowel Disease. Can. J. Gastroenterol. Hepatol. 1999, 13, 728–732. [Google Scholar] [CrossRef] [PubMed]
- Fourie, S.; Norton, C.; Jackson, D.; Czuber-Dochan, W. ‘These Discussions Aren’t Happening’: Experiences of People Living with Inflammatory Bowel Disease and Talking About Sexual Well-being with Health Care Professionals. J. Crohn’s Colitis 2021, 15, 1641–1648. [Google Scholar] [CrossRef] [PubMed]
- Fretz, K.M.; E Hunker, K.; A Tripp, D. The Impact of Inflammatory Bowel Disease on Intimacy: A Multimethod Examination of Patients’ Sexual Lives and Associated Healthcare Experiences. Inflamm. Bowel Dis. 2024, 30, 382–394. [Google Scholar] [CrossRef] [PubMed]
- McCabe, M.P. , et al., Definitions of Sexual Dysfunctions in Women and Men: A Consensus Statement From the Fourth International Consultation on Sexual Medicine 2015. J Sex Med, 2016. 13(2): p. 135-43.
- Bel, L.G.; Vollebregt, A.M.; Jong, A.E.V.d.M.-D.; Fidder, H.H.; Hove, W.R.T.; Vliet-Vlieland, C.W.; ter Kuile, M.M.; de Groot, H.E.; Both, S. Sexual Dysfunctions in Men and Women with Inflammatory Bowel Disease: The Influence of IBD-Related Clinical Factors and Depression on Sexual Function. J. Sex. Med. 2015, 12, 1557–1567. [Google Scholar] [CrossRef] [PubMed]
- Hammami, M.B.; Mahadevan, U. Men With Inflammatory Bowel Disease: Sexual Function, Fertility, Medication Safety, and Prostate Cancer. Am. J. Gastroenterol. 2020, 115, 526–534. [Google Scholar] [CrossRef] [PubMed]
- Druvefors, E.; Landerholm, K.; Hammar, U.; Myrelid, P.; E Andersson, R. Impaired Fertility in Women With Inflammatory Bowel Disease: A National Cohort Study From Sweden. J. Crohn’s Colitis 2020, 15, 383–390. [Google Scholar] [CrossRef] [PubMed]
- Druvefors, E.; Andersson, R.E.; Hammar, U.; Landerholm, K.; Myrelid, P. Minor impact on fertility in men with inflammatory bowel disease: A National Cohort Study from Sweden. Aliment. Pharmacol. Ther. 2022, 56, 292–300. [Google Scholar] [CrossRef] [PubMed]
- Nardone, O.M.; Calabrese, G.; Bertin, L.; Ford, A.C.; Castiglione, F.; Zingone, F.; Savarino, E.; Barberio, B. Prevalence of Sexual Dysfunction in Inflammatory Bowel Disease: Systematic Review and Meta-analysis. J. Crohn’s Colitis 2024, 19. [Google Scholar] [CrossRef] [PubMed]
- Zhang, J.; Wei, S.; Zeng, Q.; Wu, X.; Gan, H. Prevalence and risk factors of sexual dysfunction in patients with inflammatory bowel disease: systematic review and meta-analysis. Int. J. Color. Dis. 2021, 36, 2027–2038. [Google Scholar] [CrossRef] [PubMed]
- Perez de Arce, E. , et al., Sexual Dysfunction in Inflammatory Bowel Disease: What the Specialist Should Know and Ask. Int J Gen Med, 2021. 14: p. 2003-2015.
- Marín, L.; Mañosa, M.; Garcia-Planella, E.; Gordillo, J.; Zabana, Y.; Cabré, E.; Domènech, E. Sexual function and patients' perceptions in inflammatory bowel disease: a case–control survey. J. Gastroenterol. 2012, 48, 713–720. [Google Scholar] [CrossRef] [PubMed]
- Elias, S.; Nandi, N.; Fourie, S.; Grover, L.; Newman, K.L. Addressing Factors that Impact Sexual Well-Being and Intimacy in IBD Patients. Curr. Gastroenterol. Rep. 2025, 27, 1–10. [Google Scholar] [CrossRef] [PubMed]
- Christensen, B.; E Prentice, R.; Al-Ani, A.H.; Zhang, E.; Bedell, A.; Rubin, D.T. Self-Reported Failure to Address Sexual Function in Patients With Inflammatory Bowel Disease by Gastroenterologists: Barriers and Areas for Improvement. Inflamm. Bowel Dis. 2022, 28, 1465–1468. [Google Scholar] [CrossRef] [PubMed]
- Romano, L.; Zagari, R.M.; Arcaniolo, D.; Crocetto, F.; Spirito, L.; Sciorio, C.; Gravina, A.G.; Dajti, E.; Barone, B.; La Rocca, R.; et al. Sexual dysfunction in gastroenterological patients: Do gastroenterologists care enough? A nationwide survey from the Italian Society of Gastroenterology (SIGE). Dig. Liver Dis. 2022, 54, 1494–1501. [Google Scholar] [CrossRef] [PubMed]
- Roseira, J.; Magro, F.; Fernandes, S.; Simões, C.; Portela, F.; Vieira, A.I.; Patita, M.; Leal, C.; Lago, P.; Caldeira, P.; et al. Sexual Quality of Life in Inflammatory Bowel Disease: A Multicenter, National-Level Study. Inflamm. Bowel Dis. 2019, 26, 746–755. [Google Scholar] [CrossRef] [PubMed]
- E. , C.; I., B.; S., N. What Concerns Subjects with Inflammatory Bowel Disease and an Ileostomy? Scand. J. Gastroenterol. 2003, 38, 978–984. [Google Scholar] [CrossRef] [PubMed]
- Druvefors, E. , et al., Reasons for Reduced Fertility after Colectomy in Ulcerative Colitis. Scand J Gastroenterol, 2024. 59(12): p. 1289-1296.
|
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2025 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).