Submitted:
13 September 2025
Posted:
17 September 2025
You are already at the latest version
Abstract
Background: Scapular dyskinesis is a common dysfunction among athletes, particularly in overhead sports, leading to pain, reduced range of motion (ROM), and impaired performance. Movement-based exercises are increasingly used to address these issues, but their overall impact on sports performance remains unclear. Objective: This systematic review aims to evaluate the effects of movement-based exercises on sports performance in athletes with scapular dyskinesis. Methods: A comprehensive search was conducted in Web of Science, Scopus, and PubMed up to July 30, 2025, following PRISMA guidelines. Data were extracted and assessed for risk of bias using RoB-2 and ROBINS-I tools. A narrative synthesis was performed due to study heterogeneity. Results: Fourteen studies (8 RCTs, 6 non-RCTs) comprising 412 athletes (mean age 23.8 ± 3.1 years) were included. Interventions ranged from 6 to 24 weeks and primarily targeted scapular stabilization, neuromuscular control, and proprioception. Across studies, exercise interventions led to consistent reductions in pain and disability, with sustained improvements observed in long-term protocols. Significant gains were reported in ROM (particularly internal rotation), rotator cuff and scapular stabilizer strength, and scapulohumeral rhythm. Several trials also documented enhanced functional performance, including throwing velocity, proprioceptive accuracy, and sport-specific outcomes. Overall, 6–8-weeks programs with two to three sessions per week were effective, while longer or more intensive protocols yielded more durable benefits. Conclusion: Movement-based exercises are effective in enhancing sports performance and reducing disability in athletes with scapular dyskinesis. Tailored rehabilitation programs focusing on scapular stability and neuromuscular control are recommended for optimal outcomes.
Keywords:
1. Introduction
2. Materials and Methods
2.1. Protocol Registration
2.2. Search Strategy
2.3. Eligibility Criteria and Study Selection
2.4. Data Extraction
2.5. Quality Assessment
2.6. Data Synthesis
3. Results
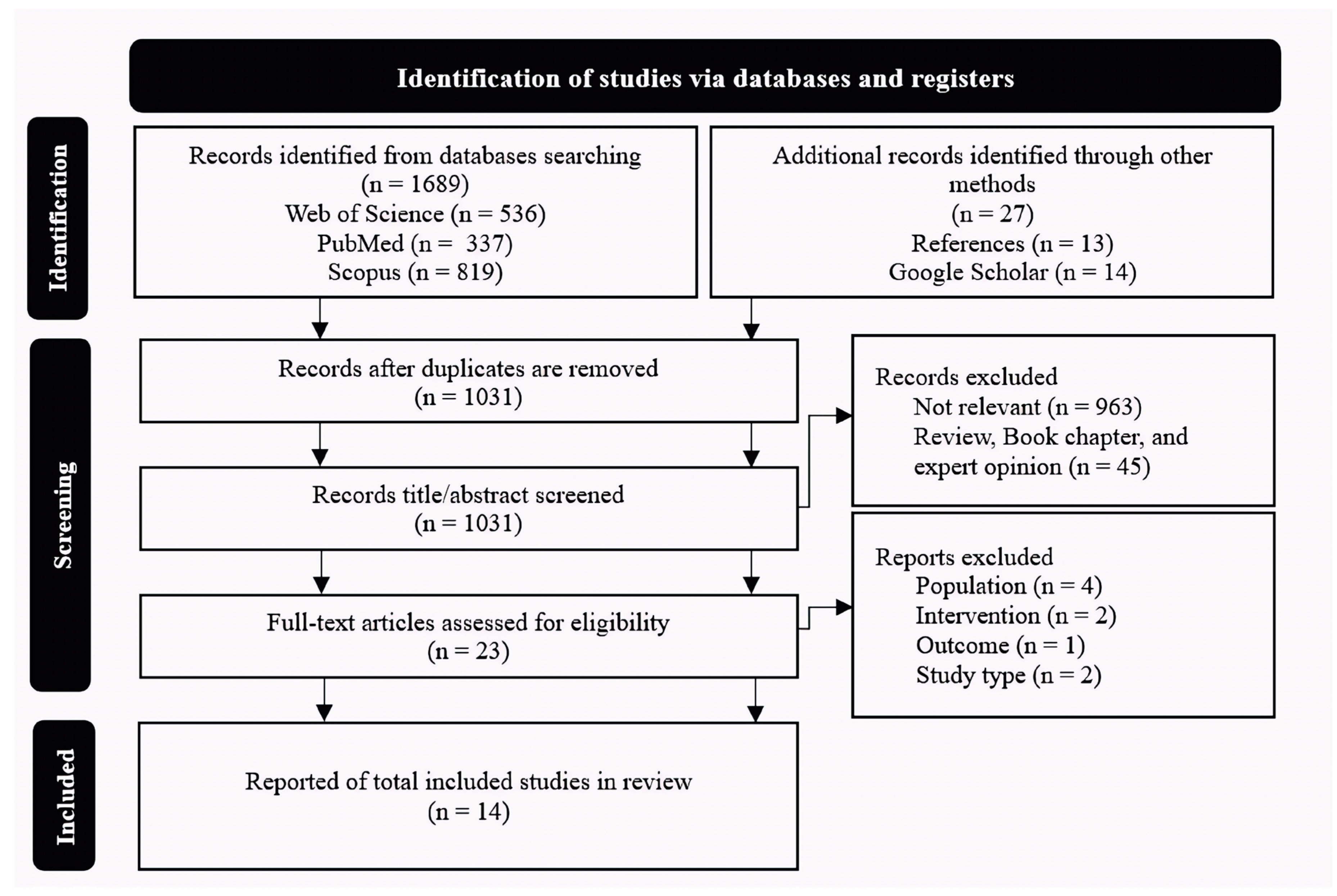
3.1. Study Identification
3.2. Effects of Exercises on Sports Performance
3.2.1. Upper Limb Function and Performance
3.2.2. Range of Motion
3.2.3. Muscle Activity and Strength
3.2.4. Scapular Kinematics
3.2.5. Pain and Disability
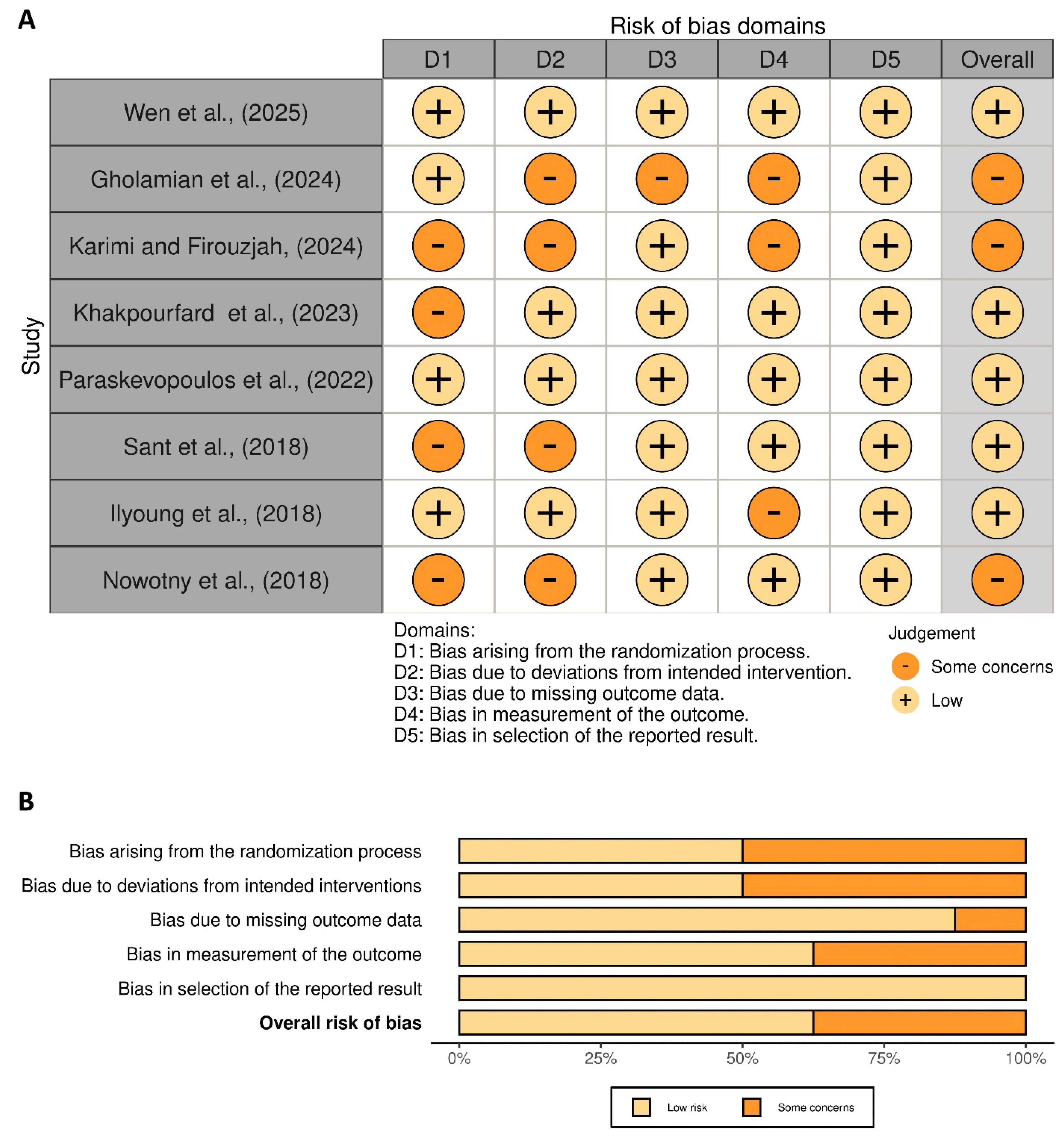
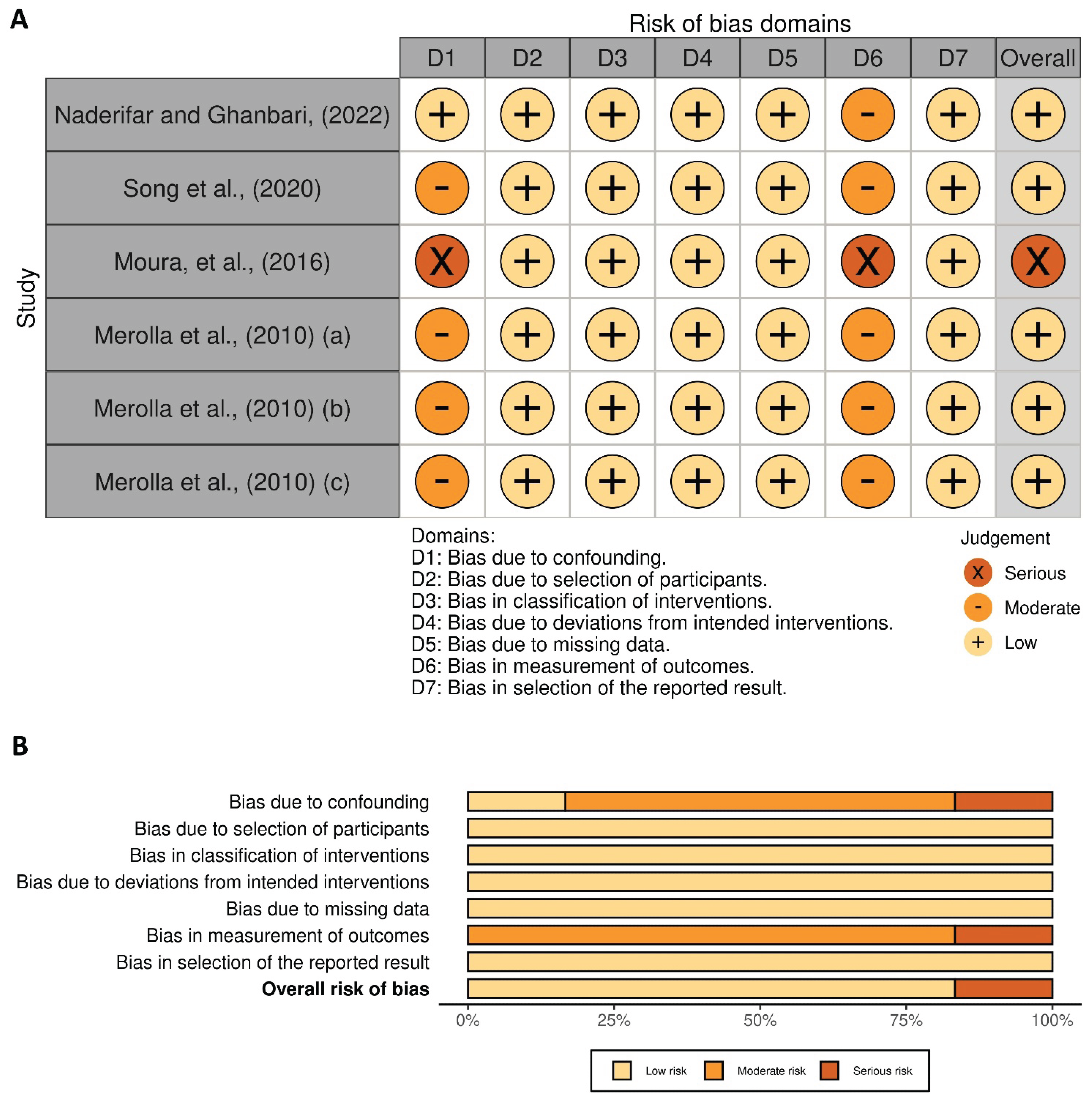
3.3. Quality Assessment
4. Discussion
4.1. Impact on Pain and Disability
4.2. Improvements in ROM and Muscle Strength
4.3. Scapular Kinematics and Functionality
4.4. Limitations and Future Directions
4.5. Clinical Implications
5. Conclusions
Supplementary Materials
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Conflicts of Interest
Abbreviations
| ROM | Range of Motion |
| PRISMA | Preferred Reporting Items for Systematic Reviews and Meta-Analyses |
| PROSPERO | International Prospective Register of Systematic Reviews |
| PICOS | Population, Intervention, Comparison, Outcome, and Study design |
| ROBINS-I | Risk Of Bias In Non-randomized Studies - of Interventions |
| RCT | Randomized Controlled Trial |
| RoB-2 | Risk of Bias 2 (tool) |
| SWiM | Synthesis Without Meta-Analysis |
References
- Kouchi, D.; Sahebozamani, M.; Daneshjoo, A.; Amatachaya, S.; Alimoradi, M.; Iranmanesh, M. Effects of an 8-week corrective dance exercises intervention on thoracic hyperkyphosis, scapular position, respiratory function, and happiness in girls aged 10–12 years. Pediatr. Exerc. Sci. 2024, 1, 1–8. [Google Scholar] [CrossRef] [PubMed]
- Kibler, W.B.; McMullen, J. Scapular dyskinesis and its relation to shoulder pain. J. Am. Acad. Orthop. Surg. 2003, 11, 142–151. [Google Scholar] [CrossRef]
- Burn, M.B.; McCulloch, P.C.; Lintner, D.M.; Liberman, S.R.; Harris, J.D. Prevalence of scapular dyskinesis in overhead and nonoverhead athletes: a systematic review. Orthop. J. Sports Med. [CrossRef]
- Jildeh, T.R.; Ference, D.A.; Abbas, M.J.; Jiang, E.X.; Okoroha, K.R. Scapulothoracic dyskinesis: a concept review. Curr. Rev. Musculoskelet. Med. 2021, 14, 246–254. [Google Scholar] [CrossRef]
- Wen, M.; Hu, X.; Bao, G. Scapular dyskinesis-based exercise therapy versus multimodal physical therapy for subacromial impingement syndrome in young overhead athletes with scapular dyskinesis: a randomized controlled trial. BMC Sports Sci. Med. Rehabil. 2025, 17, 204. [Google Scholar] [CrossRef]
- Wilk, K.E.; Obma, P.; Simpson, C.D.; Cain, E.L.; Dugas, J.; Andrews, J.R. Shoulder injuries in the overhead athlete. J. Orthop. Sports Phys. Ther. 2009, 39, 38–54. [Google Scholar] [CrossRef]
- Kibler, W.B.; Sciascia, A. The shoulder at risk: scapular dyskinesis and altered glenohumeral rotation. Oper. Tech. Sports Med. 2016, 24, 162–169. [Google Scholar] [CrossRef]
- Kibler, W.B.; Sciascia, A.; Wilkes, T. Scapular dyskinesis and its relation to shoulder injury. J. Am. Acad. Orthop. Surg. 2012, 2, 364–372. [Google Scholar] [CrossRef] [PubMed]
- Hickey, D.; Solvig, V.; Cavalheri, V.; Harrold, M.; McKenna, L. Scapular dyskinesis increases the risk of future shoulder pain by 43% in asymptomatic athletes: a systematic review and meta-analysis. Br. J. Sports Med. 2018, 52, 102–110. [Google Scholar] [CrossRef]
- Moghadam, A.N.; Rahnama, L.; Dehkordi, S.N.; Abdollahi, S. Exercise therapy may affect scapular position and motion in individuals with scapular dyskinesis: a systematic review of clinical trials. J. Shoulder Elbow Surg. 2020, 29, e29–e36. [Google Scholar] [CrossRef]
- Kamonseki, D.H.; Haik, M.N.; Ribeiro, L.P.; Almeida, R.F.; Camargo, P.R. Scapular movement training is not superior to standardized exercises in the treatment of individuals with chronic shoulder pain and scapular dyskinesis: randomized controlled trial. Disabil. Rehabil. 2023, 45, 2925–2935. [Google Scholar] [CrossRef] [PubMed]
- Khakpourfard, M.; Minoonejad, H.; Barati, A.; Kalantariyan, M. The effect of suspension training on some factors related to the shoulder injuries in athletes with scapular dyskinesis. Stud. Sport. 2023, 17, 30–41. [Google Scholar] [CrossRef]
- Gholamian, P.; Akoochakian, M.; Daneshmandi, H. The effect of a functional training program on improving scapular-brachial rhythm and performance of elite tennis players with scapular dyskinesia. Sadra Med. J. 2024, 12, 53–63. [Google Scholar] [CrossRef]
- Karimi, R.; Mohammad Ali Nasab Firouzjah, E. Impact of scapular stabilization exercises on pain, shoulder position, and volleyball performance in players with scapular dyskinesia. J. Rehabil. Sci. Res. 2024, 11, 132–138. [Google Scholar]
- Merolla, G.; De Santis, E.; Campi, F.; Paladini, P.; Porcellini, G. Supraspinatus and infraspinatus weakness in overhead athletes with scapular dyskinesis: strength assessment before and after restoration of scapular musculature balance. Musculoskelet. Surg. 2010, 94, 119–125. [Google Scholar] [CrossRef]
- Merolla, G.; De Santis, E.; Campi, F.; Paladini, P.; Porcellini, G. Infraspinatus scapular retraction test: a reliable and practical method to assess infraspinatus strength in overhead athletes with scapular dyskinesis. J. Orthop. Traumatol. 2010, 11, 105–110. [Google Scholar] [CrossRef] [PubMed]
- Merolla, G.; De Santis, E.; Sperling, J.W.; Campi, F.; Paladini, P.; Porcellini, G. Infraspinatus strength assessment before and after scapular muscles rehabilitation in professional volleyball players with scapular dyskinesis. J. Shoulder Elbow Surg. 2010, 19, 1256–1264. [Google Scholar] [CrossRef]
- Geronimo, S.M.; Baracho, W.F.; da Silva Triani, F. Effects of strength training on scapular dyskinesia: a systematic review. J. Health Sci. 2019, 21, 409–413. [Google Scholar] [CrossRef]
- Hwang, M.; Lee, S.; Lim, C. Effects of the proprioceptive neuromuscular facilitation technique on scapula function in office workers with scapula dyskinesis. Medicina 2021, 57, 332. [Google Scholar] [CrossRef]
- Moradi, M.; Hadadnezhad, M.; Letafatkar, A.; Thomas, A.C.; Hosseinzadeh, M. Effect of motor control retraining program on symptoms, strength, and function in individuals with shoulder impingement syndrome and scapular dyskinesis: a randomized controlled trial. J. Bodyw. Mov. Ther. 2025, 43, 201–209. [Google Scholar] [CrossRef]
- Page, M.J.; McKenzie, J.E.; Bossuyt, P.M.; Boutron, I.; Hoffmann, T.C.; Mulrow, C.D.; Moher, D. The PRISMA 2020 statement: an updated guideline for reporting systematic reviews. Int. J. Surg. 2021, 88, 105906. [Google Scholar] [CrossRef]
- Ouzzani, M.; Hammady, H.; Fedorowicz, Z.; Elmagarmid, A. Rayyan—a web and mobile app for systematic reviews. Syst. Rev. 2016, 5, 210. [Google Scholar] [CrossRef]
- Methley, A.M.; Campbell, S.; Chew-Graham, C.; McNally, R.; Cheraghi-Sohi, S. PICO, PICOS and SPIDER: a comparison study of specificity and sensitivity in three search tools for qualitative systematic reviews. BMC Health Serv. Res. 2014, 14, 579. [Google Scholar] [CrossRef]
- McGuinness, L.A.; Higgins, J.P. Risk-of-bias VISualization (robvis): an R package and Shiny web app for visualizing risk-of-bias assessments. Res. Synth. Methods 2021, 12, 55–61. [Google Scholar] [CrossRef]
- Campbell, M.; McKenzie, J.E.; Sowden, A.; Katikireddi, S.V.; Brennan, S.E.; Ellis, S.; Hartmann-Boyce, J.; Ryan, R.; Shepperd, S.; Thomas, J.; Welch, V.; Thomson, H. Synthesis without meta-analysis (SWiM) in systematic reviews: reporting guideline. BMJ 2020, 368, l6890. [Google Scholar] [CrossRef] [PubMed]
- De Vries, N.; Lavreysen, O.; Boone, A.; Bouman, J.; Szemik, S.; Baranski, K.; de Winter, P. Retaining healthcare workers: a systematic review of strategies for sustaining power in the workplace. Healthcare 2023, 11, 1541. [Google Scholar] [CrossRef] [PubMed]
- Sedaghati, P.; Alghosi, M.; Hosseini, F. The effect of fatigue on postural control in individuals with multiple sclerosis: a systematic review. BMC Neurol. 2023, 23, 409. [Google Scholar] [CrossRef] [PubMed]
- Cohen, J. Weighted kappa: Nominal scale agreement provision for scaled disagreement or partial credit. Psychol. Bull. 1968, 70, 213–220. [Google Scholar] [CrossRef]
- Sant, K.N.; Busuttil, L.; Salo, A. Scapular dyskinesis in asymptomatic water polo players: does prehabilitation prevent negative outcomes? Int. J. Physiother. 2018, 5, 132–140. [Google Scholar] [CrossRef]
- Nowotny, J.; Kasten, P.; Kopkow, C.; Biewener, A.; Mauch, F. Evaluation of a new exercise program in the treatment of scapular dyskinesis. Int. J. Sports Med. 2018, 39, 782–790. [Google Scholar] [CrossRef]
- Paraskevopoulos, E.; Simeonidis, T.; Tsolakis, C.; Koulouvaris, P.; Papandreou, M. Mirror cross-exercise on a kinetic chain approach improves throwing performance in professional volleyball athletes with scapular dyskinesis. J. Sport Rehabil. 2021, 31, 131–139. [Google Scholar] [CrossRef]
- Ilyoung, Y.; Minhyeok, K.; Jaeseop, O. The effects of posterior shoulder stretch on rotator cuff strength ratio in adolescent baseball players with scapular dyskinesis: A randomized controlled trial. Isokinet. Exerc. Sci. 2018, 26, 63–71. [Google Scholar] [CrossRef]
- Moura, K.F.; Monteiro, R.L.; Lucareli, P.R.; Fukuda, T.Y. Rehabilitation of subacromial pain syndrome emphasizing scapular dyskinesis in amateur athletes: a case series. Int. J. Sports Phys. Ther. 2016, 11, 552–562. [Google Scholar]
- Ki-Jae, S.; Jin-Ho, Y.; Jae-Keun, O. Effects of scapular kinetic-chain exercise on muscle activity in overhead-pitching baseball players. Iran. J. Public Health 2020, 49, 875–883. [Google Scholar]
- Naderifar, H.; Ghanbari, L. Effect of selected corrective exercises on glenohumeral rotation range of motion in overhead athletes with scapular dyskinesis. Stud. Sport. 2022, 16, 54–62. [Google Scholar] [CrossRef]
- Cools, A.M.; Struyf, F.; De Mey, K.; Maenhout, A.; Castelein, B.; Cagnie, B. Rehabilitation of scapular dyskinesis: from the office worker to the elite overhead athlete. Br. J. Sports Med. 2014, 48, 692–697. [Google Scholar] [CrossRef] [PubMed]
- Iranmanesh, M.; Shafiei Nikou, S.; Saadatian, A.; Alimoradi, M.; Khalaji, H.; Monfaredian, O.; Kouchi, D. The training and detraining effects of 8-week dynamic stretching of hip flexors on hip range of motion, pain, and physical performance in male professional football players with low back pain. A randomized controlled trial. J. Sports Sci. 2025, 43, 1572–1576. [Google Scholar] [CrossRef] [PubMed]
- Sluka, K.A.; Frey-Law, L.; Bement, M.H. Exercise-induced pain and analgesia? Underlying mechanisms and clinical translation. Pain 2018, 159, S91–S97. [Google Scholar] [CrossRef] [PubMed]
- Karimi, K.; Seidi, F.; Mousavi, S.H.; Alghosi, M.; Morad, N.H. Comparison of postural sway in individuals with and without dynamic knee valgus. BMC Sports Sci. Med. Rehabil. 2023, 15, 75. [Google Scholar] [CrossRef]
- Eller-Smith, O.C.; Nicol, A.L.; Christianson, J.A. Potential mechanisms underlying centralized pain and emerging therapeutic interventions. Front. Cell. Neurosci. 2018, 12, 35. [Google Scholar] [CrossRef]
- Meier, M.L.; Vrana, A.; Schweinhardt, P. Low back pain: the potential contribution of supraspinal motor control and proprioception. Neuroscientist 2019, 25, 583–596. [Google Scholar] [CrossRef]
- Melo, A.S.; Soares, A.L.; Castro, C.; Matias, R.; Cruz, E.B.; Vilas-Boas, J.P.; Oliveira, R. Shoulder and scapular function before and after a scapular therapeutic exercise program for chronic shoulder pain and scapular dyskinesis: a pre–post single-group study. J. Pers. Med. 2025, 15, 285. [Google Scholar] [CrossRef] [PubMed]
- Paige, C.A. Mechanistic sex differences underlying the development of chronic pain. Ph.D. Thesis, The University of Texas at Dallas, Dallas, TX, USA, 2021. https://hdl.handle.net/10735. [Google Scholar]
- Marzetti, E.; Rabini, A.; Piccinini, G.; Piazzini, D.B.; Vulpiani, M.C.; Vetrano, M.; Specchia, A. Neurocognitive therapeutic exercise improves pain and function in patients with shoulder impingement syndrome: a single-blind randomized controlled clinical trial. Eur. J. Phys. Rehabil. Med. 2014, 50, 255–264. [Google Scholar] [PubMed]
- Özlü, A.; Üstündağ, S.; Bulut Özkaya, D.; Menekşeoğlu, A.K. Effect of exergame on pain, function, and quality of life in shoulder impingement syndrome: a prospective randomized controlled study. Games Health J. 2024, 13, 109–119. [Google Scholar] [CrossRef] [PubMed]
- Borsa, P.A.; Laudner, K.G.; Sauers, E.L. Mobility and stability adaptations in the shoulder of the overhead athlete: a theoretical and evidence-based perspective. Sports Med. 2008, 38, 17–36. [Google Scholar] [CrossRef]
- Pozzi, F.; Plummer, H.A.; Shanley, E.; Thigpen, C.A.; Bauer, C.; Wilson, M.L.; Michener, L.A. Preseason shoulder range of motion screening and in-season risk of shoulder and elbow injuries in overhead athletes: systematic review and meta-analysis. Br. J. Sports Med. 2020, 54, 1019–1027. [Google Scholar] [CrossRef]
- Behera, D.; Vishwanath, S. Comparative study on the effectiveness of muscle energy technique and active release technique on the glenohumeral internal rotation deficit (GIRD) in young throwing athletes. Eur. J. Phys. Educ. Sport Sci. 2023, 9. [Google Scholar] [CrossRef]
- Reeser, J.C.; Joy, E.A.; Porucznik, C.A.; Berg, R.L.; Colliver, E.B.; Willick, S.E. Risk factors for volleyball-related shoulder pain and dysfunction. PM&R 2010, 2, 27–36. [Google Scholar] [CrossRef]
- Dwelly, P.M.; Tripp, B.L.; Tripp, P.A.; Eberman, L.E.; Gorin, S. Glenohumeral rotational range of motion in collegiate overhead-throwing athletes during an athletic season. J. Athl. Train. 2009, 44, 611–616. [Google Scholar] [CrossRef]
- Shim, J.; Park, M.; Lee, S.; Lee, M.; Kim, H. The effects of shoulder stabilization exercise and shoulder isometric resistance exercise on shoulder stability and hand function. J. Phys. Ther. Sci. 2010, 22, 227–232. [Google Scholar] [CrossRef]
- Park, S.I.; Choi, Y.K.; Lee, J.H.; Kim, Y.M. Effects of shoulder stabilization exercise on pain and functional recovery of shoulder impingement syndrome patients. J. Phys. Ther. Sci. 2013, 25, 1359–1362. [Google Scholar] [CrossRef]
- Huegel, J.; Williams, A.A.; Soslowsky, L.J. Rotator cuff biology and biomechanics: a review of normal and pathological conditions. Curr. Rheumatol. Rep. 2015, 17, 476. [Google Scholar] [CrossRef]
- Sangwan, S.; Green, R.A.; Taylor, N.F. Stabilizing characteristics of rotator cuff muscles: a systematic review. Disabil. Rehabil. 2015, 37, 1033–1043. [Google Scholar] [CrossRef]
- Niederbracht, Y.; Shim, A.L.; Sloniger, M.A.; Paternostro-Bayles, M.; Short, T.H. Effects of a shoulder injury prevention strength training program on eccentric external rotator muscle strength and glenohumeral joint imbalance in female overhead activity athletes. J. Strength Cond. Res. 2008, 22, 140–145. [Google Scholar] [CrossRef]
- Brumitt, J.; Meira, E.P.; Gilpin, H.E.; Brunette, M. Comprehensive strength training program for a recreational senior golfer 11-months after a rotator cuff repair. Int. J. Sports Phys. Ther. 2011, 6, 343–355. [Google Scholar]
- Batalha, N.; Paixão, C.; Silva, A.J.; Costa, M.J.; Mullen, J.; Barbosa, T.M. The effectiveness of a dry-land shoulder rotators strength training program in injury prevention in competitive swimmers. J. Hum. Kinet. 2020, 71, 11–21. [Google Scholar] [CrossRef]
- Micoogullari, M.; Uygur, S.F.; Yosmaoglu, H.B. Effect of scapular stabilizer muscles strength on scapular position. Sports Health 2023, 15, 349–356. [Google Scholar] [CrossRef] [PubMed]
- Kim, D.H.; Kwon, O.Y.; Yi, C.H.; Jeon, H.S. The effects of 4-week serratus anterior strengthening exercise program on the scapular position and pain of the neck and interscapular region. J. Korean Phys. Ther. 2007, 14, 58–65. [Google Scholar]
- Struyf, F.; Nijs, J.; Meeus, M.; Roussel, N.A.; Mottram, S.; Truijen, S.; Janssens, L. Does scapular positioning predict shoulder pain in recreational overhead athletes? Int. J. Sports Med. 2014, 35, 75–82. [Google Scholar] [CrossRef] [PubMed]
- Ramasamy, Y.; Usman, J.; Razman, R.; Wei, Y.M.; Towler, H.; King, M. A systematic review of the biomechanical studies on shoulder kinematics in overhead sporting motions: Types of analysis and approaches. Appl. Sci. 2023, 13, 9463. [Google Scholar] [CrossRef]
- Roller, C.L. Function and movement of the shoulder and scapula. In *Kinesiology for the Occupational Therapy Assistant*; Routledge: New York, NY, USA, 2024. [Google Scholar] [CrossRef]
- Pascoal, A.G.; Ribeiro, A.; Infante, J. Scapular resting posture and scapulohumeral rhythm adaptations in volleyball players: Implications for clinical shoulder assessment in athletes. Sports 2023, 1. [Google Scholar] [CrossRef]
- Kibler, W.B. The role of the scapula in athletic shoulder function. Am. J. Sports Med. 1998, 26, 325–337. [Google Scholar] [CrossRef] [PubMed]
- De Mey, K.; Danneels, L.; Cagnie, B.; Cools, A.M. Scapular muscle rehabilitation exercises in overhead athletes with impingement symptoms: effect of a 6-week training program on muscle recruitment and functional outcome. Am. J. Sports Med. 2022, 40, 1906–1915. [Google Scholar] [CrossRef] [PubMed]
- Kibler, W.B.; Stone, A.V.; Zacharias, A.; Grantham, W.J.; Sciascia, A.D. Management of scapular dyskinesis in overhead athletes. Oper. Tech. Sports Med. 2021, 29, 150797. [Google Scholar] [CrossRef]
- Voight, M.L.; Thomson, B.C. The role of the scapula in the rehabilitation of shoulder injuries. J. Athl. Train. 2000, 35, 364–372. [Google Scholar]
- Green, R.A.; Taylor, N.F.; Watson, L.; Ardern, C. Altered scapula position in elite young cricketers with shoulder problems. J. Sci. Med. Sport. 2013, 16, 22–27. [Google Scholar] [CrossRef]
| Database | Complete search strategy |
|---|---|
| Web of Science | athlet* OR sport* OR sportsman* OR sportswoman* OR sportsperson* (Topic) AND exercis* OR train* OR rehabilitat* OR physiotherap* OR "therapeutic exercise" (Topic) AND perform* OR strength* OR mobil* OR "range of motion" OR endurance OR function* OR skill* OR agility OR speed OR power OR injur* OR fatigue OR strength (Topic) AND "scapular dyskinesis" OR "scapular dyskinesia" OR scapul* (Topic) |
| Scopus | ( TITLE-ABS-KEY ( athlet* OR sport* OR sportsman* OR sportswoman* OR sportsperson* ) AND TITLE-ABS-KEY ( exercis* OR train* OR rehabilitat* OR physiotherap* OR "therapeutic exercise" ) AND TITLE-ABS-KEY ( perform* OR strength* OR mobil* OR "range of motion" OR endurance OR function* OR skill* OR agility OR speed OR power OR injur* OR fatigue OR strength ) AND TITLE-ABS-KEY ( "scapular dyskinesis" OR "scapular dyskinesia" OR scapul* ) ) |
| PubMed | (((athlet*[Title/Abstract] OR sport*[Title/Abstract] OR sportsman*[Title/Abstract] OR sportswoman*[Title/Abstract] OR sportsperson*[Title/Abstract]) AND (exercis*[Title/Abstract] OR train*[Title/Abstract] OR rehabilitat*[Title/Abstract] OR physiotherap*[Title/Abstract] OR "therapeutic exercise"[Title/Abstract])) AND (perform*[Title/Abstract] OR strength*[Title/Abstract] OR mobil*[Title/Abstract] OR "range of motion"[Title/Abstract] OR endurance[Title/Abstract] OR function*[Title/Abstract] OR skill*[Title/Abstract] OR agility[Title/Abstract] OR speed[Title/Abstract] OR power[Title/Abstract] OR injur*[Title/Abstract] OR fatigue[Title/Abstract] OR strength[Title/Abstract])) AND ("scapular dyskinesis"[Title/Abstract] OR "scapular dyskinesia"[Title/Abstract] OR scapul*[Title/Abstract]) |
| Inclusion criteria | Exclusion criteria | |
|---|---|---|
| Population | Athletes with diagnosis of scapular dyskinesis | Athletes with scapular dyskinesis and concurrent injuries (e.g., rotator cuff tendinopathy, superior labrum anterior to posterior lesions, labral tears). Scapular dyskinesis in non-athletic populations. |
| Intervention | Movement-based interventions, such as physical activity and other methods that involve active movement. | Other interventions occurring simultaneously. |
| Comparison | Studies investigating the effects of a exercise protocol compared to a control condition (e.g., no exercise or a placebo intervention) as the primary comparison. | Studies without a control condition. |
| Outcome | Pain intensity during activity or at rest should be assessed using the Visual Analog Scale or Numeric Rating Scale, while objective sport-performance metrics relevant to athletic activity, such as jump height, muscle activity measured by electromyography, velocity, and other sport-specific performance measures, should also be collected. | Absence of measurements for pain intensity or performance-related outcomes. |
| Study design | RCTs and non-RCTs. | Single-group intervention; Case studies; Reviews. |
| Study details | Study design | Sample description | Exercise characteristics of EG |
CG intervention | Sports performance measures | Main outcomes |
|---|---|---|---|---|---|---|
| Wen et al., (2025) [5] China |
RCT | N=32 Sex=32 males Age=20.8 ± 2.4 years SD type=NA |
D=8 weeks F=3 per week I=NA T=NA minutes T=EG1: Scapular dyskinesisbased exercise therapy; EG2: Multimodal physical therapy |
NA | Pain, ROM, strength, disability index, scapular kinematics | Disability improved in both groups by week 8 (p < 0.001) and remained only in SDBET at week 12 (p < 0.001). Pain reduced more in MPT at week 8 (p = 0.018) but not at week 12 (p = 0.268). Active ROM improved in both groups by week 8 and remained only in SDBET at week 12 (p < 0.001). Strength improved only in SDBET at weeks 8 and 12 (p < 0.001). Scapular kinematics improved in 43.8% of SDBET participants, with no change in MPT (p = 0.001–0.004). |
| Gholamian et al., (2024) [13] Iran |
RCT | N=30 Sex=30 males Age=26.3 ± 1.4 years SD type=NA |
D=8 weeks F=3 per week I=NA T=NA minutes T=Functional exercises |
Regular tennis training and daily activities | Scapular brachial rhythm, upper limb function | The results indicated that functional exercises significantly improved scapulohumeral rhythm at 0° (p = 0.004), 45° (p < 0.001), 90° (p < 0.001), and 135° (p < 0.001), as well as upper limb function (p = 0.002) in the experimental group. |
| Karimi and Firouzjah, (2024) [14] Iran |
RCT | N=30 Sex=30 females Age=22.7 ± 2.6 years SD type=NA |
D=8 weeks F=3 per week I=NA T=40 minutes T=Scapular stabilization exercises |
Usual daily activities | Specific performance, Shoulder position, Pain | Training led to significant improvements in shoulder position and performance (p = 0.001 for both). The control group also showed performance gains at eight weeks. After adjusting for pre-test scores, post-test differences favored the exercise group in shoulder position (p = 0.001) and performance (p = 0.02). Training also reduced dominant shoulder pain, reinforcing between-group differences at post-test. |
| Khakpourfard et al., (2023) [12] Iran |
RCT | N=30 Sex=30 males Age=26.8 ± 5.5 years SD type=NA |
D=8 weeks F=3 per week I=NA T=25-30 minutes T=suspension training |
NA | Internal and external rotator muscle strength, functional stability, proprioception | There were significant time-by-group interactions for internal rotator strength, external rotator strength, functional stability, and shoulder proprioception accuracy (p = 0.001), indicating that changes over time differed between groups. In addition, there were significant main effects of time and of training across all variables. Specifically, internal rotator strength showed significant effects of time (p = 0.005) and training (p = 0.021); external rotator strength showed time (p = 0.003) and training (p = 0.009); functional stability improved with both time (p = 0.001) and training (p = 0.001); and proprioception accuracy improved with time (p = 0.001) and training (p = 0.001). |
| Paraskevopoulos et al., (2022) [31] Greece |
RCT | N=39 Sex=NA Age=21.8 ± (NA) years SD type=NA |
D=6 weeks F=3 per week I=NA T=60 minutes T=EG1: kinetic chain approach; EG2: mirror cross exercise |
NA | Functional throwing performance index Throwing performance (velocity, strength) |
The Functional throwing performance Index and throwing velocity significantly improved in both the kinetic chain approach (p < 0.011 and p = 0.001) and mirror cross exercise (p = 0.004 and p < 0.001) groups, with no changes in controls. Throwing force increased significantly only in the mirror cross exercise group (P = 0.011). |
| Study details | Study design | Sample description |
Exercise characteristics of EG |
CG intervention | Sports performance measures | Main outcomes |
| Naderifar and Ghanbari, (2022) [35] Iran |
Non-RCT | N=54 Sex=54 females Age=22.2 ± 2.4 years SD type=NA |
D=8 weeks F=3 per week I=moderate T=NA minutes T=Selected Corrective Exercises |
Typical training regimen | Internal and external rotation ROM | Results revealed that, in the experimental group, glenohumeral internal rotation significantly increased (p = 0.001) following the exercise program. No significant changes were observed in the control group. |
| Song et al., (2020) [34] Republic of Korea |
Non-RCT | N=27 Sex=27 males Age=19.6 ± 1.9 years SD type=Sick |
D=8 weeks F=3 per week I=NA T=40 minutes T=Scapular KineticChain Exercise |
NA | Muscle activation | Maximal and mean muscular activation significantly increased after exercise in Normal-Dominant and SICK-Dominant upper and lower trapezius muscles (p < 0.05). The SICK-Dominant serratus anterior showed lower activation than Normal-Dominant at pre-test (p = 0.034), with differences persisting post-test compared to Normal-Non-Dominant (p = 0.031) |
| Sant et al., (2018) [29] United Kingdom |
RCT | N=25 Sex=25 males Age=23.2 ± 3.6 years SD type= Unilateral |
D=NA weeks F=NA per week I=NA T=NA minutes T=Prehabilitation |
Usual routine | Functional throwing performance index, power, upper extremity stability | Pain was reported in 3 athletes in the control group versus 1 in the study group (p = 0.59). Athletes receiving prehabilitation showed significantly greater improvements in external rotation (p = 0.01) and internal rotation (p = 0.03) compared to controls. No significant differences were found between groups in functional tests, scores, or abduction strength. |
| Ilyoung et al., (2018) [32] Republic of Korea |
RCT | N=24 Sex=24 males Age=25.7 ± 1.4 years SD type= Inferomedial winging and medial border winging |
D=6 weeks F=3 per week I=70%-90% stretch T=NA minutes T=EG1: PSSE group; EG2: SSE |
NA | Isokinetic peak moment/body weight, ROM, Pain | Significant time × group interactions were found for concentric and eccentric external rotation peak moment/body weight (p = 0.039, p = 0.008), ERe to IRc ratio (p = 0.025), and rotation ROM (IRROM p < 0.001, ERROM p = 0.001). The PSSE group showed improvements at 6 weeks in ERc, ERe, ERe/IRc ratio, IRROM (↑15°), ER ROM (↓12°), and GIRD (↓17°); the SSE group did not show significant changes in strength or ROM. Pain decreased over time in both groups (p < 0.001) with no group interaction (p = 0.56). |
| Nowotny et al., (2018) [30] Germany |
RCT | N=28 Sex=16 males and 12 females Age=33 ± (NA) years SD type=type I |
D=6 weeks F= 2per week I=NA T=60 minutes T= specific exercise |
Massage Therapy | ROM, Pain, disability, Scapular kinematics, shoulder function |
Both exercise and massage reduced pain (VAS: exercise p = 0.007; control p = 0.004), but only the exercise group showed significant improvement in shoulder function (QuickDASH p = 0.001; SICK Scapula p = 0.003; Hand Press-up p = 0.026). |
| Moura et al., (2016) [33] Brazil |
Non-RCT | N=4 Sex=2 males and 2 females Age=24.7 ± (NA) years type=NA |
D=1 session F=NA I=NA T=120 minutes T=Specific training |
NA | ROM, pain, sports performance, muscle activation, strength, function | Participants showed reduced pain, improved function and performance, increased shoulder strength, greater ROM, and enhanced serratus anterior activation. |
| Merolla et al., (2010) [15] Italy |
Non-RCT | N=29 Sex=18 males and 11 females Age=23 ± 4.2 years SD type=NA |
D=24 weeks F=NA I=NA T=NA T=Rehabilitation program for restoring scapular muscular control and balance |
NA | Strength, pain, ROM | Muscle strength of the supraspinatus and infraspinatus, measured by EC and IST tests, significantly increased at 3- and 6-months post-rehabilitation (p < 0.01). Additionally, glenohumeral internal rotation ROM improved at both time points. Patient pain intensity decreased significantly from 7.5 ± 2.3 at baseline to 3.4 ± 1.8 at 3 months and 2.9 ± 2.1 at 6 months (p < 0.01). |
| Study details | Study design | Sample description |
Exercise characteristics of EG |
CG intervention | Sports performance measures | Main outcomes |
| Merolla et al., (2010) [16] Italy |
Non-RCT | N=29 Sex=16 males and 13 females Age=23 ± 4.5 years SD type=NA |
D=24 weeks F=NA I=NA T=NA T=Rehabilitation program for restoring scapular muscular control and balance |
NA | ROM, strength | Isometric strength of the infraspinatus muscle, assessed using the infraspinatus strength test, significantly increased after 6 months—3.3 ± 1.54 kg for examiner 1 (p = 0.0069) and 3.9 ± 1.6 kg for examiner 2 (p = 0.0058). The mean difference between infraspinatus strength test and the infraspinatus scapular retraction test results at 6 months was not statistically significant (p = 0.061). Glenohumeral internal rotation also showed significant improvement, increasing from 54.5 ± 9.8 to 67.3 ± 10.1 degrees for examiner 1 (p = 0.0096) and from 53.9 ± 10.2 to 68.1 ± 11.4 degrees for examiner 2 (p = 0.0089) |
| Merolla et al., (2010) [17] Italy |
Non-RCT | N=31 Sex=22 males and 9 females Age=22 ± 2.5 years SD type=NA |
D=24 weeks F=NA I=NA T=NA T=Rehabilitation program for restoring scapular muscular control and balance |
NA | Pain, strength | The mean force values of the infraspinatus strength test increased significantly after 3 months (p < 0.01) and 6 months (p < 0.001) of rehabilitation. The mean difference between infraspinatus strength test and the infraspinatus scapular retraction test decreased from 4.72 ± 0.007 at baseline to 1.2 ± 0.26 at 3 months and 0.4 ± 0.006 at 6 months. Mean pain scores were 2.4 ± 1.8 at 3 months and 2.6 ± 1.4 at 6 months. |
| Parameters | Number of studies | Significant negative effect | Significant positive effect | No significant effect |
|---|---|---|---|---|
| Upper limb function and performance | 4/14 studies | NA | [12,14,29–31] | NA |
| Range of motion | 6/14 studies | NA | [5,15,16,32,33,35] | NA |
| Muscle activity and strength | 8/14 studies | NA | [12,15–17,32–34] | NA |
| Scapular kinematics | 4/14 studies | NA | [5,13,30,35] | NA |
| Pain and disability | 8/14 studies | [5,12,14,30,32,33] | [29] |
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2025 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (http://creativecommons.org/licenses/by/4.0/).





