1. Introduction
“The central theme of the shoulder is motion” [
1]. The shoulder’s full arc of motion encompasses over-head, across-body, and behind-body reach, and involves eighteen muscles acting across four articulations, chiefly the glenohumeral and scapulothoracic. The scapula dynamically links the body with the arm, coordinating both mobility and stability. Importantly, the scapula must glide along the thoracic wall to perform its two critical functions. First, the scapula maintains optimal length-tension relationships for the extrinsic (deltoid, biceps, triceps) and intrinsic (rotator cuff) muscles of the glenohumeral joint. Second, the scapula prevents impingement of the rotator cuff between the acromion and the humerus. The peri-scapular chain, comprised of the trapezius, rhomboids, levator scapulae, serratus anterior, and the pectoralis minor (PM), coordinates this scapulothoracic glide. Full pain-free shoulder motion truly relies on a
harmony of musculoskeletal and neurologic forces.
Despite noteworthy advances in arthroscopic and open techniques, implant design, and understanding of biomechanics, many patients continue to suffer from chronic pain, neuropathy, and weakness. These patients notoriously fail to improve despite seeing a host of specialists including therapists, pain management physicians, chiropractors, neurologists, and spine, shoulder, and sports surgeons. They are often tagged with challenging and vague diagnoses including thoracic outlet syndrome (TOS), scapular dyskinesia, myofascial tightness, fibromyalgia, complex regional pain syndrome (CRPS), occupational shoulder disorder (ORD), or work-related musculoskeletal disorder (WRMD). Best attempts at conservative therapy and surgical interventions often yield limited results. These historically challenging and intractable scenarios frustrate surgeons, therapists, and patients alike.
In this paper, we report a case series of ten patients who presented with a similar constellation of refractory pain, neuropathy, and weakness. Each patient exhibited coracoid tenderness, neck, shoulder, and upper back pain, and a specific scapular malposition of protraction and internal rotation with anterior tilt. In addition, patients demonstrated varying degrees of neuropathy at the thoracic outlet, suprascapular notch, quadrilateral space, and/or radial and carpal tunnel; rotator cuff impingement; occipital headaches; and limited range of motion (ROM). Patients stemmed from diverse and non-overlapping etiologies, ranging from female athletes to breast cancer survivors to postoperative arthroplasty. Each failed all previous treatments. Crucially, each patient responded dramatically to an isolated tenotomy of the PM off the coracoid process, producing permanent resolution of all symptoms, including clearance of pre-existing neuropathic lesions even at the thoracic outlet, elimination of headaches, and restoration of full ROM. Based on our experience we propose a novel unifying clinical syndrome that (1) explains the similar presentations, (2) accounts for the diverse populations, (3) elucidates the dramatic and durable response to isolated PM tenotomy, and (4) unites these considerations with known understanding of biomechanics and pathology.
2. Materials and Methods
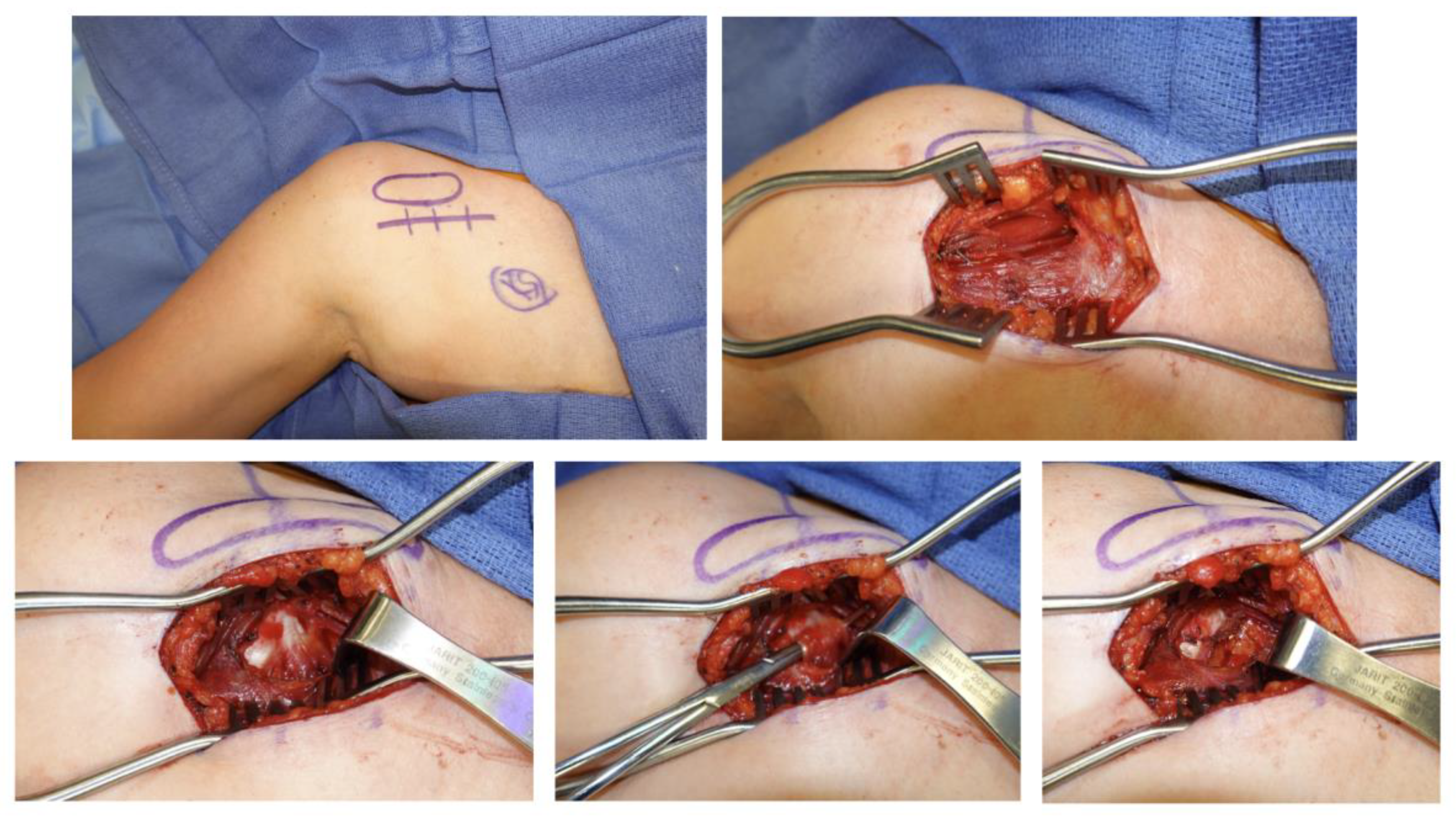
This is a retrospective case series of patients presenting to two clinics. All were treated by a fellowship-trained board-certified hand or sports surgeon. Inclusion criteria included: age > 18 years; physical exam with coracoid tenderness and scapula malposition of protraction with anterior tilt and internal rotation. Exclusion criteria included: follow-up < 6 months. Patients were evaluated pre-operatively and then at 2, 6, 12, and 24 weeks. Patients completed self-reported pain diagrams and symptoms questionnaires. A certified hand and physical therapist (PT) independently performed a full brachial plexus and musculoskeletal evaluation. Provocative testing identified neuropathic lesions at the thoracic outlet, PM, suprascapular notch, quadrilateral space, radial and carpal tunnels. Musculoskeletal exams included Medical Research Council (MRC) grade muscle testing and shoulder range of motion (ROM) values in forward flexion, abduction, and external rotation planes. Each patient underwent isolated PM tenotomy through an open direct approach. (
Figure 1) Outcomes included pain scores and distribution, presence of headaches, presence of neuropathic lesions, shoulder ROM, and muscle strengths. Institutional Review Board (IRB) approval was obtained and need for consent was waived by the ethics committee as all data was anonymous, the study was observational only and involved standard of care treatments, and the study posed minimal risk to the included patients.
3. Results
Ten patients originated from diverse etiologies (
Table 1) but presented with similar signs and symptoms. (
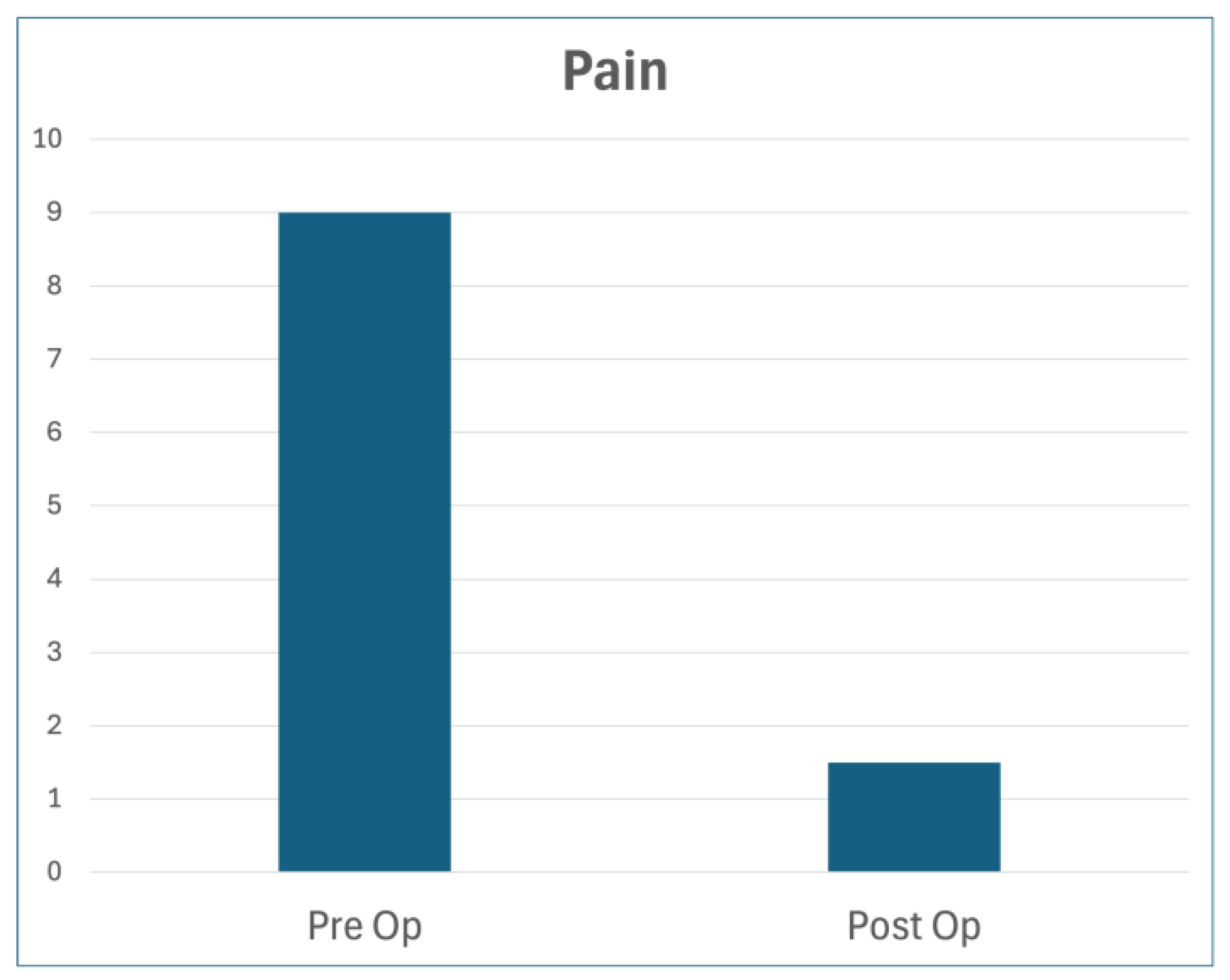
Table 2) Median age was 42. Each had failed all previous treatments by multiple subspecialists. In addition to the variable symptoms listed below, each patient exhibited significant coracoid tenderness with specific scapular dyskinesia of protraction, internal rotation, and anterior tilt, and endorsed shoulder pain extending to the neck and upper back. Median pre-op pain was 9.0/10; median post-op pain was 1.5/10. (
Figure 2) Appropriate diagnostic imaging and testing was carried out at the discretion of the examiner based on presentation to rule out concomitant pathologies.
Table 1.
Patient Characteristics.
Table 1.
Patient Characteristics.
| Variable |
Frequency |
| Age |
37 [26 – 58]1
|
| Hand Dominance |
Right 9
Left 1 |
| Etiology |
Breast cancer s/p- radiation 1
Macromastia 1
s/p- reverse TSA 1
Bodybuilder 1
Female athlete 1
Iatrogenic block injury 1
Persistent impingement despite cuff repair 1
Cervical stenosis 1
Direct traction (Burner’s/Stinger’s) 1
OSD/WRMD 1 |
| Pre-Operative Pain |
9.0 [7.8 – 10] |
| Post-Operative Pain |
1.5 [0.8 – 2] |
| Pre-Operative ROM2
|
85 degrees |
| Post-Operative ROM |
180 degrees |
Table 2.
Clinical Presentation of Human Disharmony Loop.
Table 2.
Clinical Presentation of Human Disharmony Loop.
| Loop Element |
PM Tightness |
Scapula Malposition |
C4-6 Root Stretch |
| Symptom/Sign |
|
Peri-scapular pain and tightness Thoracic outlet -
Mechanical impingement
- o
Hawkin’s sign - o
Neer’s sign
Shoulder weakness and limited ROM Upper trapezius tightness and occipital headaches |
Neck, shoulder, lateral forearm and hand pain, numbness/tingling, burning, weakness -
Secondary neuropathy
- o
Quadrilateral space - o
Suprascapular notch - o
Radial tunnel - o
Carpal tunnel
|
Figure 2.
Self-Reported Pain Scores. Median pain score (out of 10), before and after surgery, with minimum of 6 months follow-up.
Figure 2.
Self-Reported Pain Scores. Median pain score (out of 10), before and after surgery, with minimum of 6 months follow-up.
Case Examples
Patient 1. 56 y/o RHD female presented with a history of Left breast cancer s/p- mastectomy with adjuvant radiation. Since then, she suffered 8/10 Left arm pain that emanated from the shoulder to the dorsal forearm along with global hand numbness and weakness. She had full ROM of the shoulder. She trialed physical therapy and pain management for >6 years with no relief. She had no findings of rotator cuff weakness, focal neurologic deficit, or cervical spine pathology to justify further diagnostic workup. She underwent a Left PM tenotomy. At 2 weeks postoperatively, all symptoms had resolved except for mild surgical incision pain, which was permanent at most recent 1-year follow-up.
Patient 2. 31 y/o RHD female presented with macromastia and multiple years of Right shoulder and neck pain, forearm burning, hand numbness/tingling, and severe ipsilateral occipital migraines. She had been treated with physical therapy, chiropractors, pain management, and neurology, with minimal relief. On exam, she was additionally provocative at the carpal tunnel and quadrilateral space. She had full ROM of the shoulder. She had no findings of rotator cuff weakness, focal neurologic deficit, or cervical spine pathology to justify further diagnostic workup. She underwent isolated Right PM tenotomy, resulting in resolution of all symptoms including migraines, shoulder pain and other neuropathic lesions.
Patient 3. 63 y/o RHD male with a history of Left reverse TSA 16 months prior presented with continued shoulder pain, constant hand numbness/tingling, and principal complaint of shoulder weakness. He exhibited active abduction and external rotation ROM to 60-degrees only; he had a positive scratch-collapse test at the quadrilateral space. suprascapular notch, and distal radial and carpal tunnels. After Left PM tenotomy, he immediately noted full shoulder strength with 180 degrees of abduction. Additionally, all other neuropathic lesions resolved. (
Figure 3).
Patient 4. 59 y/o RHD male bodybuilder with no history of trauma presented with progressive multi-year history of severe 10/10 Left shoulder, neck, and upper back pain. He had full shoulder ROM. He had undergone four prior surgeries (arthroscopy with biceps tenodesis, revision tenodesis and labral repair, arthroscopic debridement x2) and numerous rounds of injections and physical therapy, with no relief. He had no findings of rotator cuff weakness, focal neurologic deficit, or cervical spine pathology to justify further diagnostic workup. After isolated PM tenotomy he exhibited complete resolution of all symptoms by 3 months, which remained durable.
Patient 5. 21 y/o RHD female college athlete (swimming, volleyball) without a history of trauma presented with progressive Right shoulder and neck pain and hand numbness and weakness. On exam, she was also provocative at the thoracic outlet. She had full shoulder ROM. Her symptoms were severe enough to prevent playing sports. She had been unsuccessfully treated at a tertiary academic center for presumed thoracic outlet syndrome including scalene botulinum toxin injections. She had no findings of rotator cuff weakness, focal neurologic deficit, or cervical spine pathology to justify further diagnostic workup. Right PM tenotomy produced rapid and complete resolution of all symptoms, allowing full return to sport.
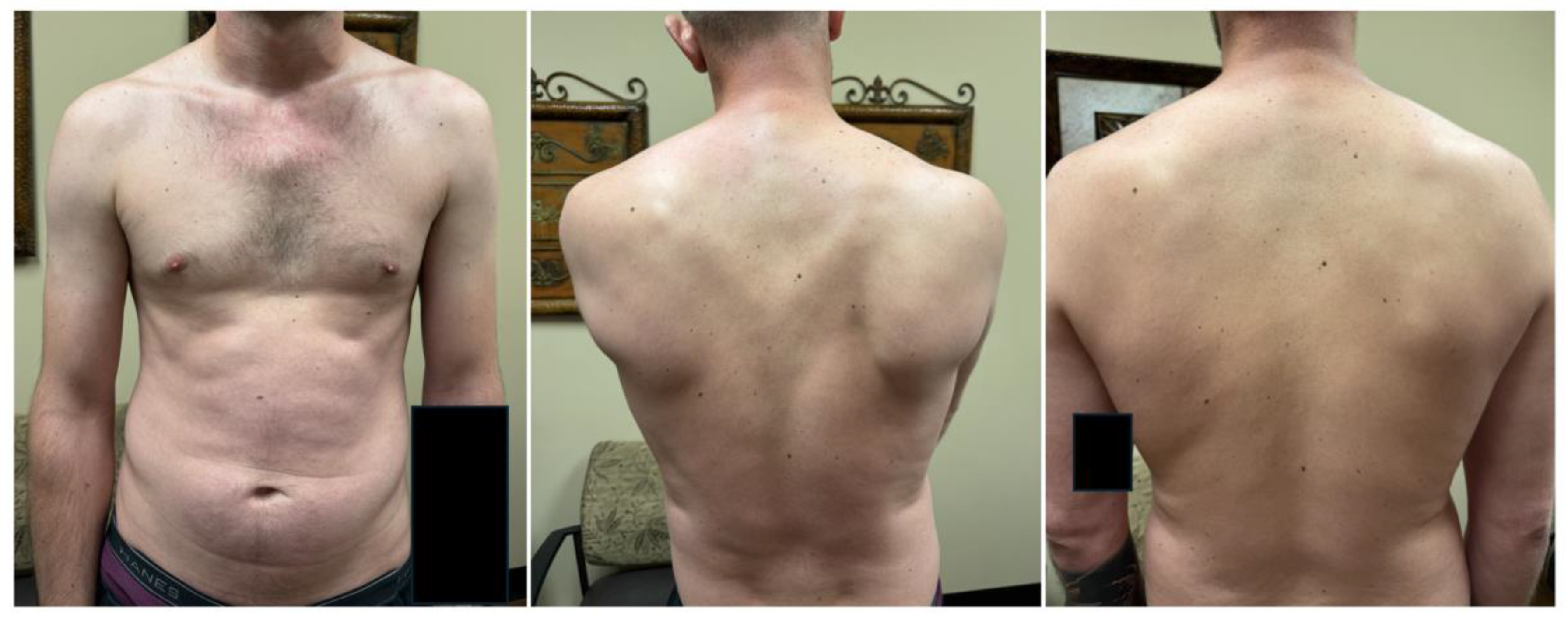
Patient 6. 28 y/o RHD male presented 3 years after SLAP tear repair with pre-operative interscalene regional block. Although symptoms related to the SLAP tear resolved, he presented with unrelenting 10/10 Right neck and shoulder pain with occipital migraines severe enough to prevent work. On exam, he was provocative at the quadrilateral space. He had full ROM of the shoulder. EMG confirmed denervation of biceps and infraspinatus consistent with iatrogenic regional block injury to the upper trunk. He had been previously treated by pain management, neurology, physical therapy, and shoulder and sports specialists, with no relief. He admitted to being “suicidal” due to pain. He responded very well but temporarily to a coracoid injection in clinic and subsequently underwent isolated PM tenotomy. This produced rapid and permanent resolution of all symptoms, restored normal scapular positioning (
Figure 4) and cleared his quadrilateral space lesion as well. He thereby returned to work and felt “normal” and “happy” for the first time in years.
Patient 7. 59 y/o RHD male worker’s compensation injury with a history of biceps tenodesis and revision rotator cuff repair 5 months prior, presented with severe chronic and worsening Left shoulder pain and ulnar hand numbness preventing work. He had no history of trauma. On exam he exhibited positive impingement signs and active shoulder forward flexion to 150 degrees and abduction to 100 degrees. Physical therapy failed to help. He ad complete relief of symptoms with a diagnostic coracoid injection. He had no findings of rotator cuff weakness, focal neurologic deficit, or cervical spine pathology to justify further diagnostic workup. He thereafter underwent isolated PM tenotomy. Two weeks postoperatively his pain and impingement symptoms had resolved, he exhibited full pain-free ROM of the shoulder, he had improvement of distal neurologic symptoms, and he returned to work.
Patient 8. 42 y/o RHD female with a history of cervical stenosis treated with anterior C4-5 and posterior C4-6 cervical fusion years ago, presented with bilateral chronic Left greater than Right shoulder, neck, and upper back pain. She also endorsed occipital headaches and global hand weakness. She received mild relief after the cervical surgeries. On exam she was additionally provocative at the quadrilateral space, radial tunnel, and carpal tunnel. She had full ROM of the shoulder. Her symptoms did not respond to physical therapy, subacromial? injections, pain management, and acupuncture. She had no findings of rotator cuff weakness, focal neurologic deficit, or cervical spine pathology to justify further diagnostic workup. She underwent Left isolated PM tenotomy. Her pain and other neuropathic lesions on that side resolved completely and has elected to have the contralateral PM released.
Patient 9. 22 y/o LHD female who sustained a sudden traction injury while overhead lifting 2 years prior at work and felt a severe “pop, then burn”. Thereafter, she suffered Right arm global dysfunction with constant 10/10 pain and allodynia of the forearm, guarding, debilitating hand weakness and coldness, and shoulder active range of motion forward flexion and abduction of 30 degrees. She did not respond to treatments including physical therapy, pain management, chiropractors, and assessment by shoulder surgeons. She had been diagnosed with thoracic outlet, complex regional pain syndrome, fibromyalgia, and pain seeking behavior, but no treatment helped. EMG/NCS was normal. MRI showed type II SLAP tear and mild insertional supraspinatus tendinopathy, both deemed non-contributory. Her pain was so severe she was considering arm amputation. She underwent isolated PM tenotomy. Her pain rapidly resolved, her ROM improved, and her hand function normalized, which remained permanent at most recent 1-year follow-up.
Patient 10. 25 y/o RHD F who worked as an administrative assistant presented with severe Left chronic shoulder pain, trapezius myalgia, and hand weakness and numbness. Her severe symptoms interfered with work, and she was diagnosed with WRMD. She had been evaluated by occupational health and treated by physical therapy with ergonomics and postural conditioning for >3 years with mild relief. Shoulder MRI was normal. On exam, she was additionally provocative at the suprascapular notch, quadrilateral space, and radial and carpal tunnels. After isolated PM tenotomy, her pain, myalgia, weakness, and numbness resolved, and she returned to work without issue.
4. Discussion
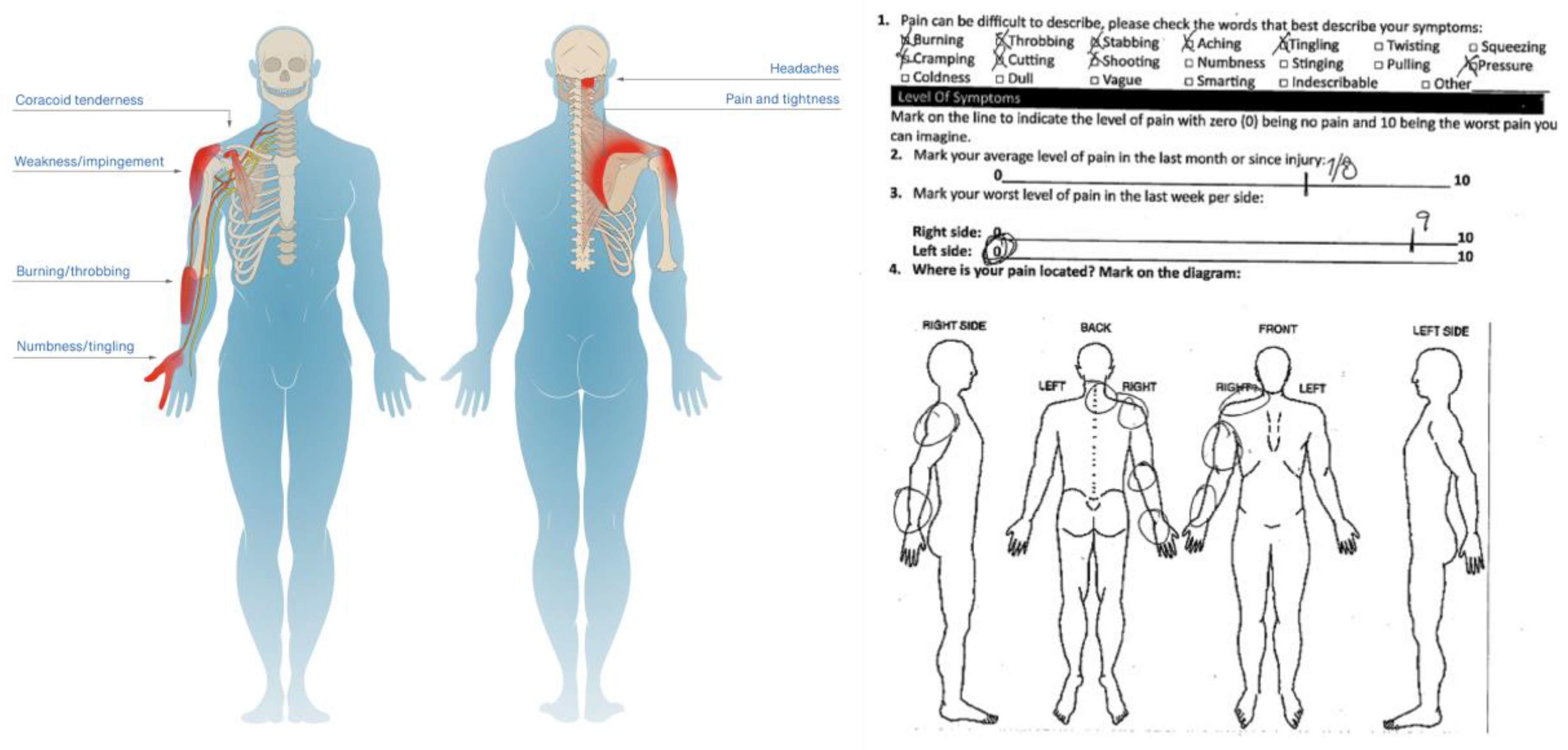
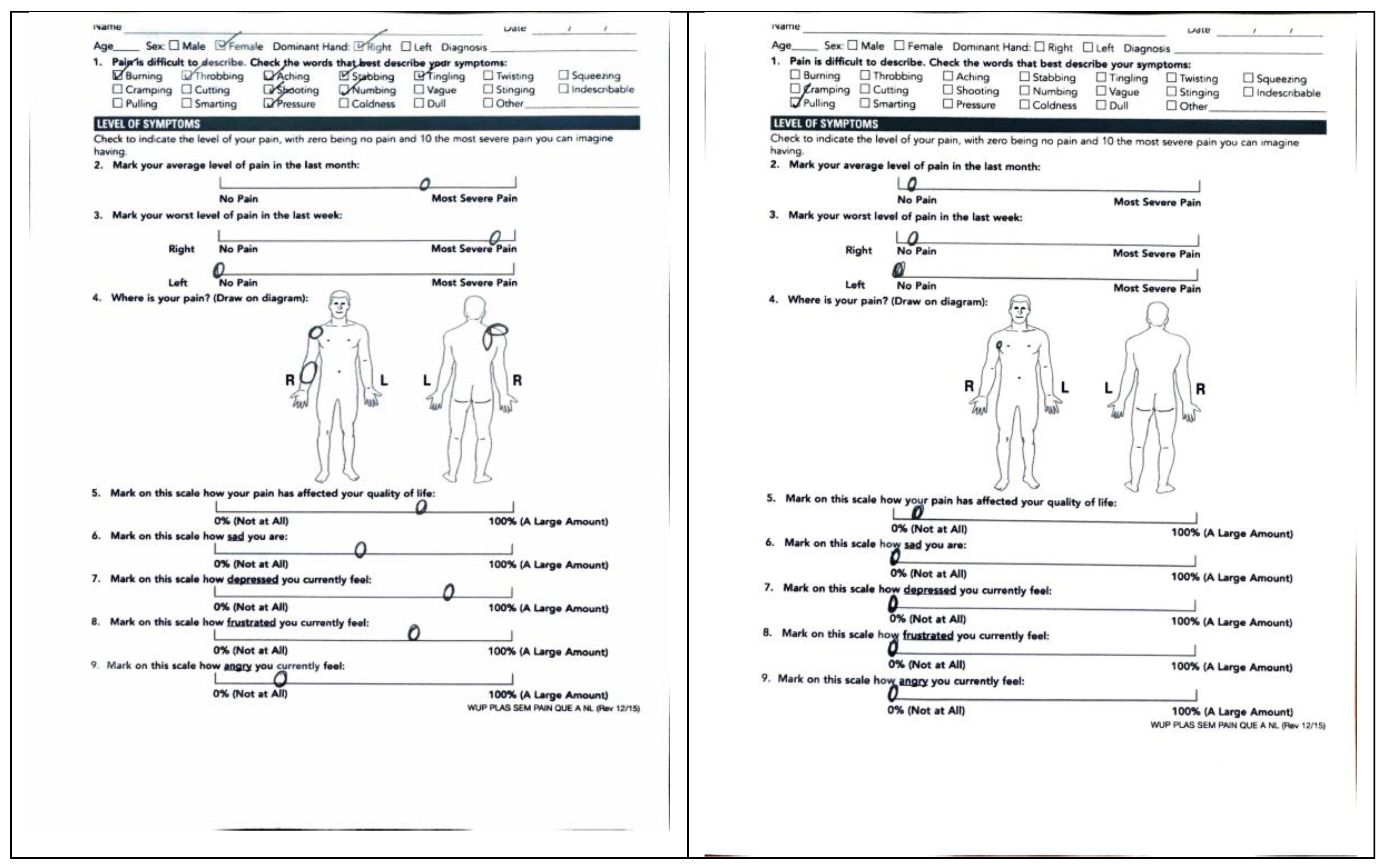
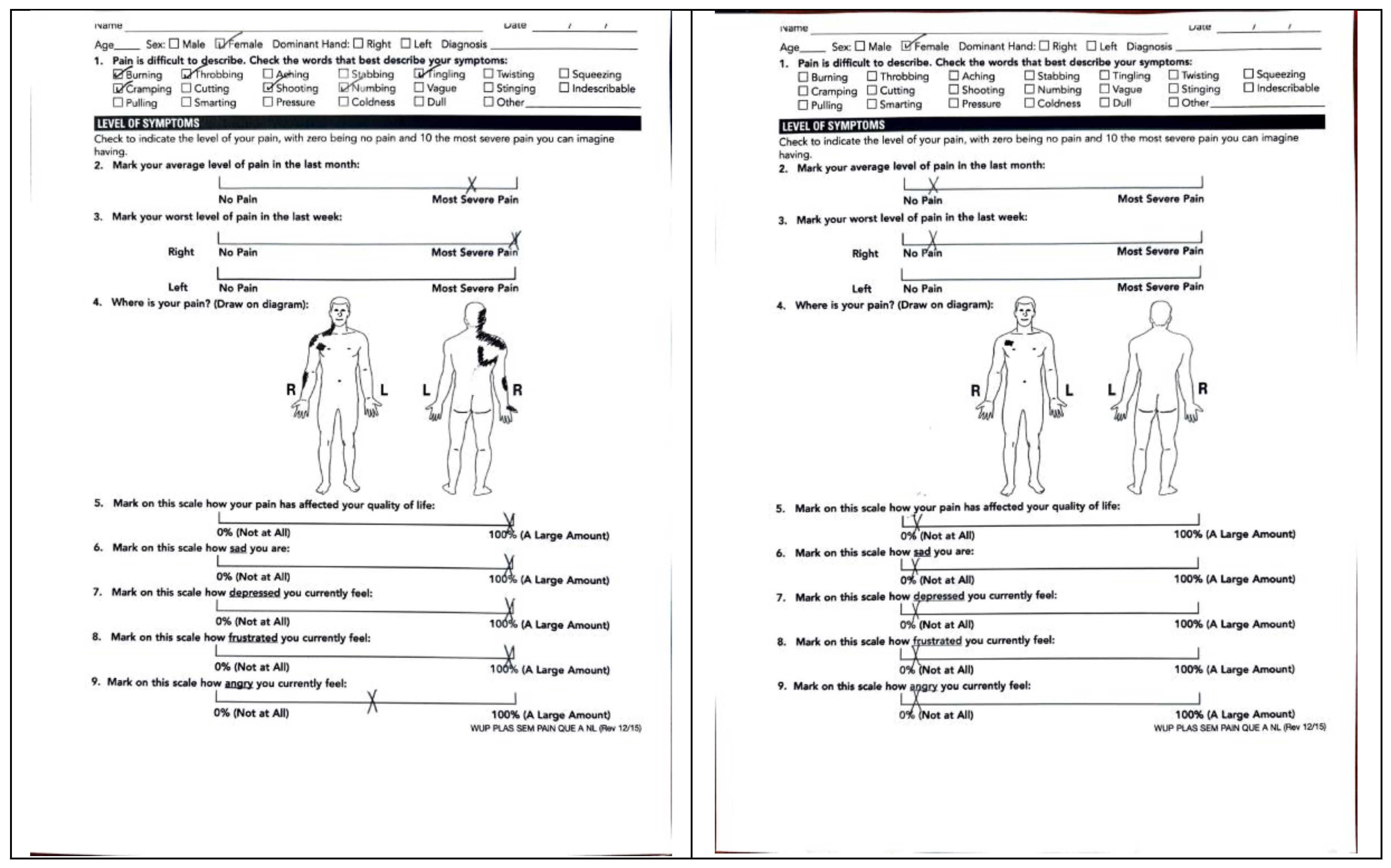
In this paper, we present a series of ten challenging and complex patients who originated from diverse etiologies but displayed remarkably similar presentations. All endorsed shoulder pain extending to the neck and upper back, and on physical exam exhibited coracoid tenderness with specific scapula malposition of protraction with anterior tilt and internal rotation. (
Figure 5) Additional variable symptoms included pain and weakness with motion; numbness/tingling and burning of the shoulder, forearm and hand; and occipital headaches. (
Table 2) Moreover, both nonoperative and operative treatments by a variety of multidisciplinary specialists failed to help. However, isolated PM tenotomy dramatically cured these patients (
Figure 6), which suggests that tightness of this muscle inserting anteriorly onto the coracoid process of the scapula plays a central and unique role in their intractable pathophysiology.
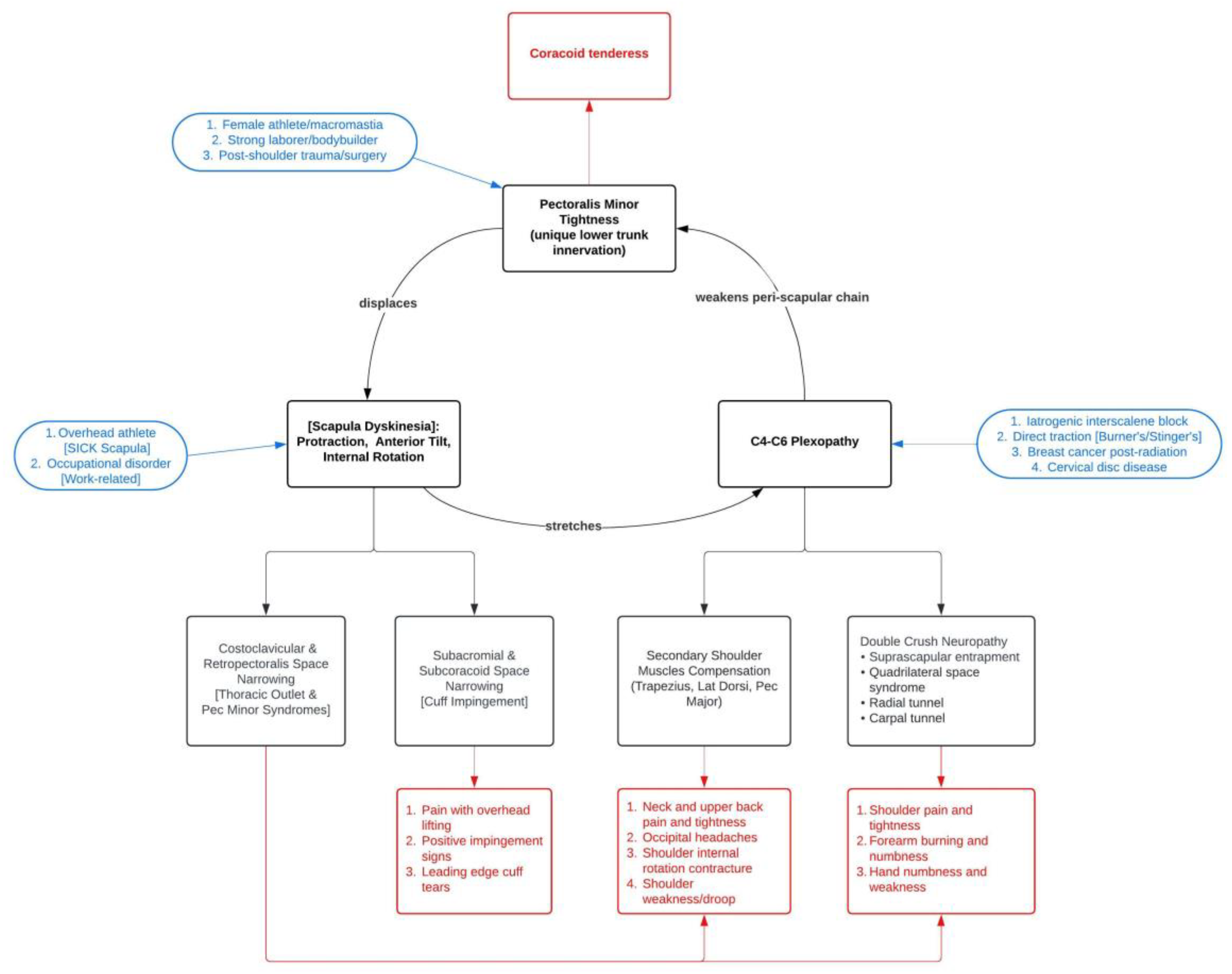
From these considerations, we propose a novel clinical syndrome: The Human Disharmony Loop. (
Figure 7) Our syndrome centers on a positive feedback cycle: PM tightness displaces the scapula which stretches the upper C4-6 roots which weakens the remaining peri-scapular chain. Hence, PM tightness reinforces itself. The peri-scapular muscles responsible for coordinating scapulothoracic motion are all innervated by the upper C4-6 roots, except for the PM, which additionally receives lower C8-T1 input via the medial pectoral nerve [
2]. Anatomically, the upper roots remain far more susceptible to stretch or traction and are more frequently injured than the lower roots [
2,
3,
4]. Hence, any stretch or traction to the brachial plexus will preferentially strengthen the PM and weaken the other peri-scapular stabilizers.
As the PM overpowers these other muscles, the scapula displaces to a disequilibrium of protraction, anterior tilt, and internal rotation. Since the scapula dynamically links the thorax to the arm, this deranges the entire anatomy of the upper limb girdle, pathologizing the bones, joints, muscles, and nerves, and causing numerous anatomic effects. (
Figure 5) Consequently, the symptoms span the neck to the fingertips. The shoulder assumes a dropped and internally rotated (“hunched”) posture. (
Figure 4) The costoclavicular space narrows, producing thoracic outlet syndrome. The subacromial and subcoracoid spaces narrow, impinging or even tearing the rotator cuff [
13,
14]. (
Figure 2) Traction on the C4-6 roots weakens the peri-scapular chain, yields neuropathic pain in their respective dermatomes, and generates secondary neuropathy at the suprascapular notch, quadrilateral space, and radial and carpal tunnels. The peri-scapular stabilizers further weaken as they fall out of optimal length-tension relationships. Upper trapezius stretch from scapula displacement irritates the occipital nerves to the scalp, producing headaches/migraines. In summary, patients endorse neck, shoulder, and upper back pain and tightness; weakness with overhead reach; limited ROM; occipital headaches; and numbness/tingling and burning of the shoulder, forearm, or hand. (
Figure 4) Broadly, the constellation of symptoms categorically aligns with the three components of the loop: coracoid tenderness (from PM tightness), peri-scapular pain with rotator cuff impingement (from scapula malposition), and C4-6 neuropathy (from root stretch). (
Table 2)
Human disharmony loop is a clinical diagnosis based on the patient’s presenting complaints and physical exam; it is not a diagnosis of exclusion. Crucially, patients must exhibit both key mechanistic determinants: coracoid tenderness and scapula malposition of protraction, anterior tilt, and internal rotation. Notably, the scapula dyskinesia can be static (at rest) or dynamic (with motion). (
Table 2) Diagnostic testing is important but frequently nonsensitive, nonspecific, and does not affect treatment. MRIs may be normal except for incidental findings of loop sequelae (i.e., rotator cuff tendinopathy). EMG/NCS may be negative, except for revealing concomitant distal neuropathy, or if the initial inciting entry into the loop is neurologic (i.e., upper trunk block injury). The peri-scapular chain weakness is primarily due to muscle malposition. Furthermore, disharmony presents as a spectrum: magnitude of PM tightness governs degree of scapular dyskinesia which determines the severity of clinical presentation. While all patients must exhibit the two key determinants, they variably display differing degrees of secondary neuropathy, occipital headaches, and mechanical impingement or weakness. Diagnostic testing and imaging may be helpful but is frequently normal or incidental.
Notably, patients may enter the central loop through three different avenues corresponding to the three elements. For female athletes, women with macromastia, strong laborers/bodybuilders, or following shoulder trauma or surgery, the PM tightens primarily. Overhead athletes and OSD/WRMD patients protract the scapula primarily. Interscalene block injuries, direct plexus traction, radiation after breast cancer, and cervical stenosis injure the C4-6 roots primarily. However, once inside the loop, patients cycle through the same pathophysiological sequence, explaining the starkly similar presentations. (
Figure 6) These patients are often historically challenging and notoriously intractable to standard treatments. Patients will often see a host of subspecialists to individually treat the separate downstream sequelae of the disharmony loop, such as cuff impingement, distal neuropathy, proximal thoracic outlet, upper back tightness, trapezius myalgia, shoulder pain, occipital headaches, etc... However, they respond poorly because the central source – PM tightness – reinforces itself via a positive feedback cycle. Critically, tenotomizing the PM off the scapula breaks this cycle by restoring normal scapulothoracic kinesthetic glide, reharmonizing the anatomy of the upper limb girdle, and obliterating the pathological sequelae. Hence, the pectoralis minor – often overlooked and arguably misnamed – may constitute the source of much musculoskeletal and neurologic upper limb pathology.
The unique lower trunk innervation to the PM deserves mention. We believe this asymmetry underlies much challenging shoulder and arm pathology. (
Table 3) We hypothesize this innervation results from an evolutionary idiosyncrasy. For our quadrupedal ancestors, coordination between the forepaw and ventral chain is essential for running, leaping, and pouncing. As Homo sapiens are the only obligate bipedal mammal, the human shoulder, which beautifully relies on neurologic and musculoskeletal balance, remains nonetheless highly prone to imbalance because it evolved from a limb optimized for quadrupedal gait. In fact, we suspect all humans are prone to disharmony; notably, chronic neck and shoulder pain plague over 60% of the population [
5].
Our syndrome unifies and elucidates several well-known yet incomplete models of upper limb pathology. Pectoralis minor syndrome is conventionally described as compression of the infraclavicular plexus producing distal pain and paresthesia [
6,
7]. However, this alone cannot explain the resolution of proximal thoracic outlet, cuff impingement, scapula malposition, and occipital headaches that we observed following isolated PM tenotomy. Instead, rather than compressing neurovascular structures akin to other infra-clavicular lesions, PM tightness displaces the scapula. TOS remains highly controversial due to wide variability in presentation, lack of reliable diagnostic testing, and unpredictable response to treatment [
2,
8]. Both abnormal scapular kinematics and postural derangement are well documented [
8]. In our series, we observed dramatic obliteration of TOS after PM tenotomy in patients who failed prior targeted anti-TOS therapy. Hence, we suspect TOS results from PM tightness, as the scapula malposition narrows the costoclavicular space via the acromioclavicular joint and compresses the brachial plexus. OSD/WRMD is defined as work and activity related pain and tightness of the neck, shoulder, and upper back, and patients frequently exhibit trapezius and parascapular myalgia, rotator cuff tendinitis, and impingement [
1]. Frustratingly, the symptom presentation is vague, the diagnosis is challenging, and the etiology is unknown [
1]. But interpreted within the context of our syndrome, these are simply patients entering the loop via scapular protraction. SICK Scapula occurs in throwing athletes and includes asymmetric scapula malposition with coracoid tenderness [
9]. However, in this description, the scapula is dyskinetic due to the “ellipsoid shape of the thorax… it tends to ride ‘up and over’ the top … the [PM] and short head of the biceps becomes adaptively tight” [
9]. Here, we disagree and reverse the causality: PM tightness pulls the scapula into dyskinesia, which results from an imbalance of muscular forces and not bony shapes. Scapular dyskinesia itself has been observed in TOS, SICK scapula, OSD/WRMD, and throwing and athletic disorders [
4,
10,
11]. Many alleged bony, articular, and neurologic causes have been proposed [
11], but whether these are instead effects remains unclear [
10]. Interestingly, scapula protraction is always observed [
11]. We believe our model finally answers the true cause behind the dyskinesia: specifically, the asymmetric neurologic innervation between the ventral PM and the dorsal peri-scapular stabilizers predisposes the scapula to protraction along the thorax.
Our study has important limitations. As a small case series, our results and interpretations must be taken cautiously and replicated before adoption. Our volume of PM tenotomy has grown considerably and we intend to refute or validate our hypotheses in future, much larger studies; this pilot study is meant to demonstrate proof of concept. Nonetheless, conceptually, our model accounts for the similarity in presentation and diversity of etiology observed in these patients, and most importantly explains the dramatic degree of clinical improvement witnessed in these notoriously challenging patients who failed all prior treatments. Our model integrates these considerations with a pathophysiological framework founded on well-established anatomy and biomechanical principles. Furthermore, our model elucidates currently known yet poorly understood syndromes and hypothesizes an underlying evolutionary mechanism for the causative neurologic asymmetry.
In conclusion, the remarkable motion of the human shoulder mandates a harmony between musculoskeletal and neurologic forces. However, this harmony is prone to imbalance due to the unique lower trunk innervation of the only ventral chain stabilizer of the scapula, the PM. When the balance is lost and the scapula displaces, disharmony of the system occurs, deranging the anatomy of the upper limb girdle, and producing a clinical dysfunction that spans the neck to the fingertips. We propose a novel unifying syndrome which centralizes the PM to causing chronic pain, neuropathy, and weakness in these patients and elucidates many well-known yet poorly-understood conditions. Patients presenting with the Human Disharmony Loop may benefit dramatically from isolated PM tenotomy. Future research is required to confirm or refute the numerous corollaries of our proposed syndrome.
5. Conclusions
The unique asymmetric neurologic innervation to the sole ventral stabilizer of the scapula, the pectoralis minor, renders the human shoulder prone to neurologic and musculoskeletal imbalance. This produces the Human Disharmony Loop: a clinical syndrome spanning the neck to the fingertips of chronic pain, neuropathy, and weakness. These challenging and historically intractable patients may benefit dramatically from isolated PM tenotomy.
Author Contributions
Dr. Ketan Sharma and Dr. James Friedman contributed equally to the conceptualization, methodology, validation, analysis, investigation, data curation, writing of this project. All authors have read and agreed to the published version of the manuscript.
Funding
This research received no external funding.
Institutional Review Board Statement
The study was conducted in accordance with the Declaration of Helsinki, and approved by the Institutional Review Board (or Ethics Committee) of St. Luke’s Clinic (protocol 2024-0107 on 10/14/24) and St. Joseph’s Medical Center (7/11/24).
Informed Consent Statement
Patient consent was waived by the ethics committee as all data was anonymous, the study was observational only and involved standard of care treatments, and the study posed minimal risk to the included patients.
Data Availability Statement
The original contributions presented in this study are included in the article/supplementary material. Further inquiries can be directed to the corresponding author(s).
Acknowledgments
In this section, you can acknowledge any support given which is not covered by the author contribution or funding sections. This may include administrative and technical support, or donations in kind (e.g., materials used for experiments).
Conflicts of Interest
The authors declare no conflicts of interest.
Abbreviations
The following abbreviations are used in this manuscript:
| PM |
Pectoralis minor |
| TOS |
Thoracic outlet syndrome |
| CRPS |
Complex regional pain syndrome |
| OSD |
Occupational shoulder disorder |
| WRMD |
Work-related musculoskeletal disorder |
| ROM |
Range of motion |
| MRC |
Medical Research Council |
| IRB |
Institutional Review Board |
| RHD |
Right hand dominant |
| TSA |
Total shoulder arthroplasty |
| SLAP |
Superior Labrum Anterior Posterior |
| EMG |
Electromyography |
| LHD |
Left hand dominant |
| MRI |
Magnetic Resonance Imaging |
References
- Rockwood CA. Rockwood and Matsen’s the shoulder. Fifth edition. ed. Philadelphia, PA: Elsevier; 2017. xix, 1284 pages p.11-37. ISBN 978-0-323-69836-8.
- Kuhn JE, Lebus VG, Bible JE. Thoracic outlet syndrome. J Am Acad Orthop Surg. 2015;23(4):222-32. [CrossRef]
- Mackinnon SE. Nerve surgery. New York: Thieme; 2015. xv, 627 pages p.391-467. ISBN 978-1-60406-282-3.
- Noland SS, Bishop AT, Spinner RJ, Shin AY. Adult Traumatic Brachial Plexus Injuries. J Am Acad Orthop Surg. 2019;27(19):705-16. [CrossRef]
- Cools AM, Struyf F, De Mey K, Maenhout A, Castelein B, Cagnie B. Rehabilitation of scapular dyskinesis: from the office worker to the elite overhead athlete. Br J Sports Med. 2014;48(8):692-7. [CrossRef]
- Sanders RJ, Annest SJ. Pectoralis Minor Syndrome: Subclavicular Brachial Plexus Compression. Diagnostics (Basel). 2017;7(3). [CrossRef]
- Sanders RJ, Rao NM. The forgotten pectoralis minor syndrome: 100 operations for pectoralis minor syndrome alone or accompanied by neurogenic thoracic outlet syndrome. Ann Vasc Surg. 2010;24(6):701-8. [CrossRef]
- Mackinnon SE, Novak CB. Thoracic outlet syndrome. Curr Probl Surg. 2002;39(11):1070-145. [CrossRef]
- Burkhart SS, Morgan CD, Kibler WB. The disabled throwing shoulder: spectrum of pathology Part III: The SICK scapula, scapular dyskinesis, the kinetic chain, and rehabilitation. Arthroscopy. 2003;19(6):641-61. [CrossRef]
- Jayasinghe GS. Scapula Dyskinesis: A Review of Current Concepts and Evaluation of Assessment Tools. Curr Sports Med Rep. 2018;17(10):338-46. [CrossRef]
- Roche SJ, Funk L, Sciascia A, Kibler WB. Scapular dyskinesis: the surgeon’s perspective. Shoulder Elbow. 2015;7(4):289-97. [CrossRef]
- Moran SL, Steinmann SP, Shin AY. Adult brachial plexus injuries: mechanism, patterns of injury, and physical diagnosis. Hand Clin. 2005;21(1):13-24. [CrossRef]
- Provencher CM, Makani A, McNeil JW, Pomerantz ML, Golijanin P, Gross D. The role of the scapula in throwing disorders. Sports Med Arthrosc Rev. 2014;22(2):80-7. [CrossRef]
- Provencher MT, Kirby H, McDonald LS, Golijanin P, Gross D, Campbell KJ, et al. Surgical Release of the Pectoralis Minor Tendon for Scapular Dyskinesia and Shoulder Pain. Am J Sports Med. 2017;45(1):173-8. [CrossRef]
Figure 1.
Technique for Pectoralis Minor Tenotomy. Open technique. (a) ~4-cm transverse incision inferior to palpable coracoid process. (b) Dissection down to deltoid (up), pectoralis major (down), and exposed cephalic vein (center). (c) Further dissection down to coracoid with conjoined tendon (left) and pectoralis minor tendon (right). (d) Isolating the pec minor tendon for release. (e) Complete pectoralis minor release off coracoid. .
Figure 1.
Technique for Pectoralis Minor Tenotomy. Open technique. (a) ~4-cm transverse incision inferior to palpable coracoid process. (b) Dissection down to deltoid (up), pectoralis major (down), and exposed cephalic vein (center). (c) Further dissection down to coracoid with conjoined tendon (left) and pectoralis minor tendon (right). (d) Isolating the pec minor tendon for release. (e) Complete pectoralis minor release off coracoid. .
Figure 3.
Complete Restoration of Range of Motion. Persistent weakness and limited ROM following reverse total shoulder arthroplasty (top left) and despite arthroscopic repair of leading-edge supraspinatus tear (bottom left). Both responded dramatically to surgery restoring full motion (right).
Figure 3.
Complete Restoration of Range of Motion. Persistent weakness and limited ROM following reverse total shoulder arthroplasty (top left) and despite arthroscopic repair of leading-edge supraspinatus tear (bottom left). Both responded dramatically to surgery restoring full motion (right).
Figure 4.
Shoulder Posture and Scapula Malposition in the Human Disharmony Loop. Preoperatively, disharmonic Right shoulder exhibits drooping and internal rotation (“hunched”) posture (left). Preoperatively, disharmonic Right scapula exhibits protraction, anterior tilt, and internal rotation (middle). Two weeks postoperatively, the shoulder and scapula are symmetric to the normal side with scapulothoracic kinesthesia restored, correlating with symptom resolution.
Figure 4.
Shoulder Posture and Scapula Malposition in the Human Disharmony Loop. Preoperatively, disharmonic Right shoulder exhibits drooping and internal rotation (“hunched”) posture (left). Preoperatively, disharmonic Right scapula exhibits protraction, anterior tilt, and internal rotation (middle). Two weeks postoperatively, the shoulder and scapula are symmetric to the normal side with scapulothoracic kinesthesia restored, correlating with symptom resolution.
Figure 5.
Illustrative Pain Diagram of Human Disharmony Loop. Illustrative diagram (left) with sample patient example (right). Constellation of symptoms includes shoulder/neck/upper back pain and tightness; coracoid tenderness; forearm burning, hand numbness and tingling; pain with overhead reach. Pain is exhibited in C4-6 dermatomes, indicating stretch on these roots from the scapula malposition.
Figure 5.
Illustrative Pain Diagram of Human Disharmony Loop. Illustrative diagram (left) with sample patient example (right). Constellation of symptoms includes shoulder/neck/upper back pain and tightness; coracoid tenderness; forearm burning, hand numbness and tingling; pain with overhead reach. Pain is exhibited in C4-6 dermatomes, indicating stretch on these roots from the scapula malposition.
Figure 6.
Global Symptom Resolution Following Pectoralis Minor Tenotomy. Illustrative pain diagrams showing resolution of global symptoms after surgery. Top row: Pre op to post op for first patient. Bottom row: Pre op to post op for second patient. Symptoms are broad but nonetheless tend to categorize as: coracoid tenderness, peri-scapular pain, C4-6 neuropathy.
Figure 6.
Global Symptom Resolution Following Pectoralis Minor Tenotomy. Illustrative pain diagrams showing resolution of global symptoms after surgery. Top row: Pre op to post op for first patient. Bottom row: Pre op to post op for second patient. Symptoms are broad but nonetheless tend to categorize as: coracoid tenderness, peri-scapular pain, C4-6 neuropathy.
Figure 7.
The Human Disharmony Loop. The positive feedback loop in the center is visualized: pectoralis minor tightness displaces the scapula which stretches the C4-6 roots which reinforces pectoralis minor tightness due to its unique lower trunk C8-T1 innervation. Diverse groups of patients can enter the loop through different points seen in blue. Clinical signs and symptoms are seen in red. Other challenging and vague syndromes – including scapular dyskinesia, SICK scapula, occupational / work-related musculoskeletal disorder, thoracic outlet, conventional pectoralis minor syndrome, cuff impingement, and Burner’s and Stinger’s – are incorporated into the loop and seen in [brackets]. Pectoralis minor tenotomy breaks the cycle, reharmonizing the upper limb and obliterating the pathologic sequelae.
Figure 7.
The Human Disharmony Loop. The positive feedback loop in the center is visualized: pectoralis minor tightness displaces the scapula which stretches the C4-6 roots which reinforces pectoralis minor tightness due to its unique lower trunk C8-T1 innervation. Diverse groups of patients can enter the loop through different points seen in blue. Clinical signs and symptoms are seen in red. Other challenging and vague syndromes – including scapular dyskinesia, SICK scapula, occupational / work-related musculoskeletal disorder, thoracic outlet, conventional pectoralis minor syndrome, cuff impingement, and Burner’s and Stinger’s – are incorporated into the loop and seen in [brackets]. Pectoralis minor tenotomy breaks the cycle, reharmonizing the upper limb and obliterating the pathologic sequelae.
Table 3.
Historically Challenging Patient Populations Who May be in the Human Disharmony Loop.
Table 3.
Historically Challenging Patient Populations Who May be in the Human Disharmony Loop.
Chronic shoulder pain Chronic neck and upper back pain and tightness Occipital / cervicogenic headaches Thoracic outlet syndrome (TOS) Occupational shoulder disorder (ORD) / work-related musculoskeletal disorder (WRMD) Subacromial impingement Persistent pain and weakness after shoulder arthroplasty, other shoulder surgeries, or shoulder trauma Persistent distal neuropathy SICK scapula CRPS Fibromyalgia |
|
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2025 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (http://creativecommons.org/licenses/by/4.0/).