Submitted:
08 September 2025
Posted:
10 September 2025
You are already at the latest version
Abstract
Keywords:
1. Introduction
2. Materials and Methods
2.1. Model Objective and Design
2.2. Age Stratification and Data Transformation
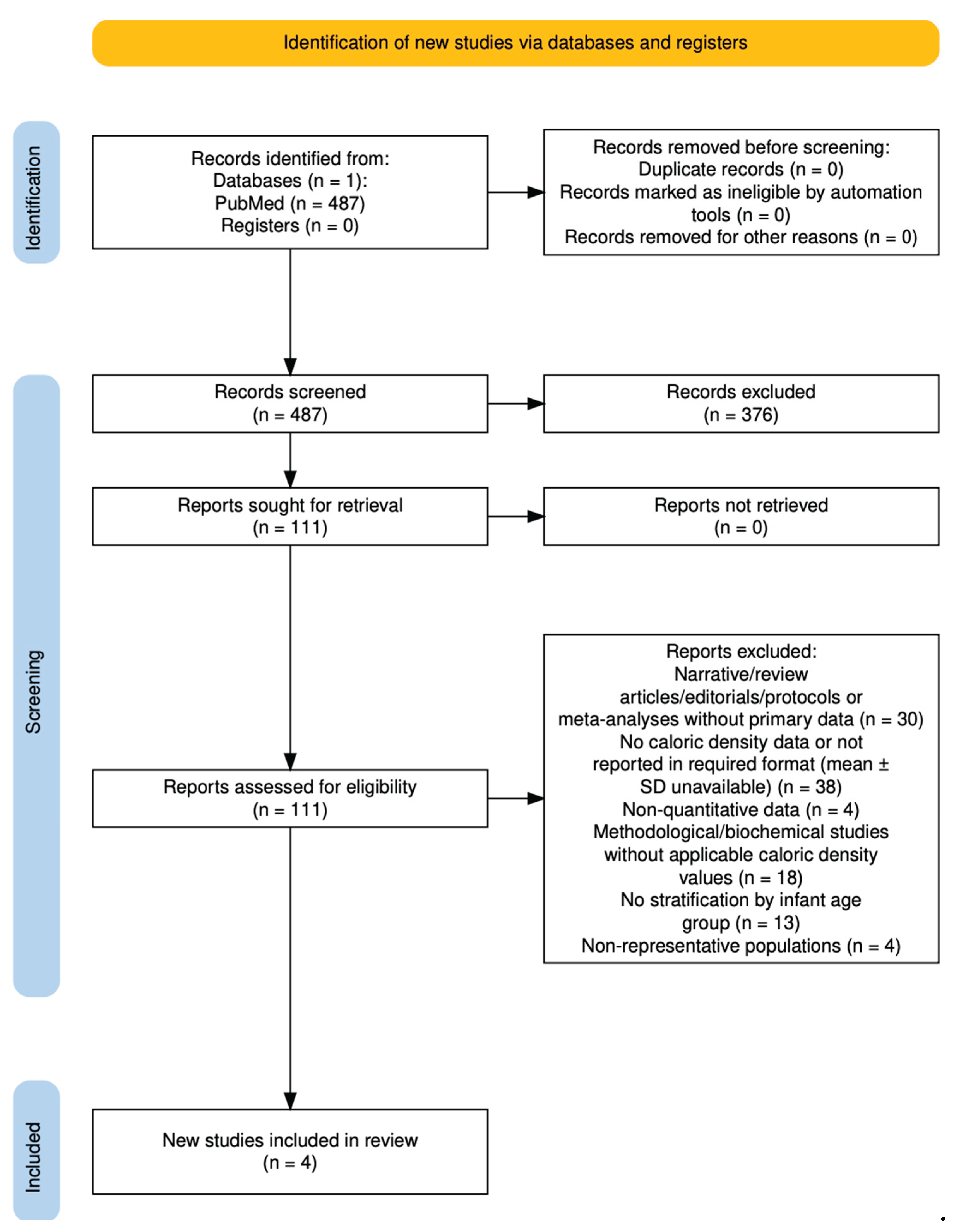
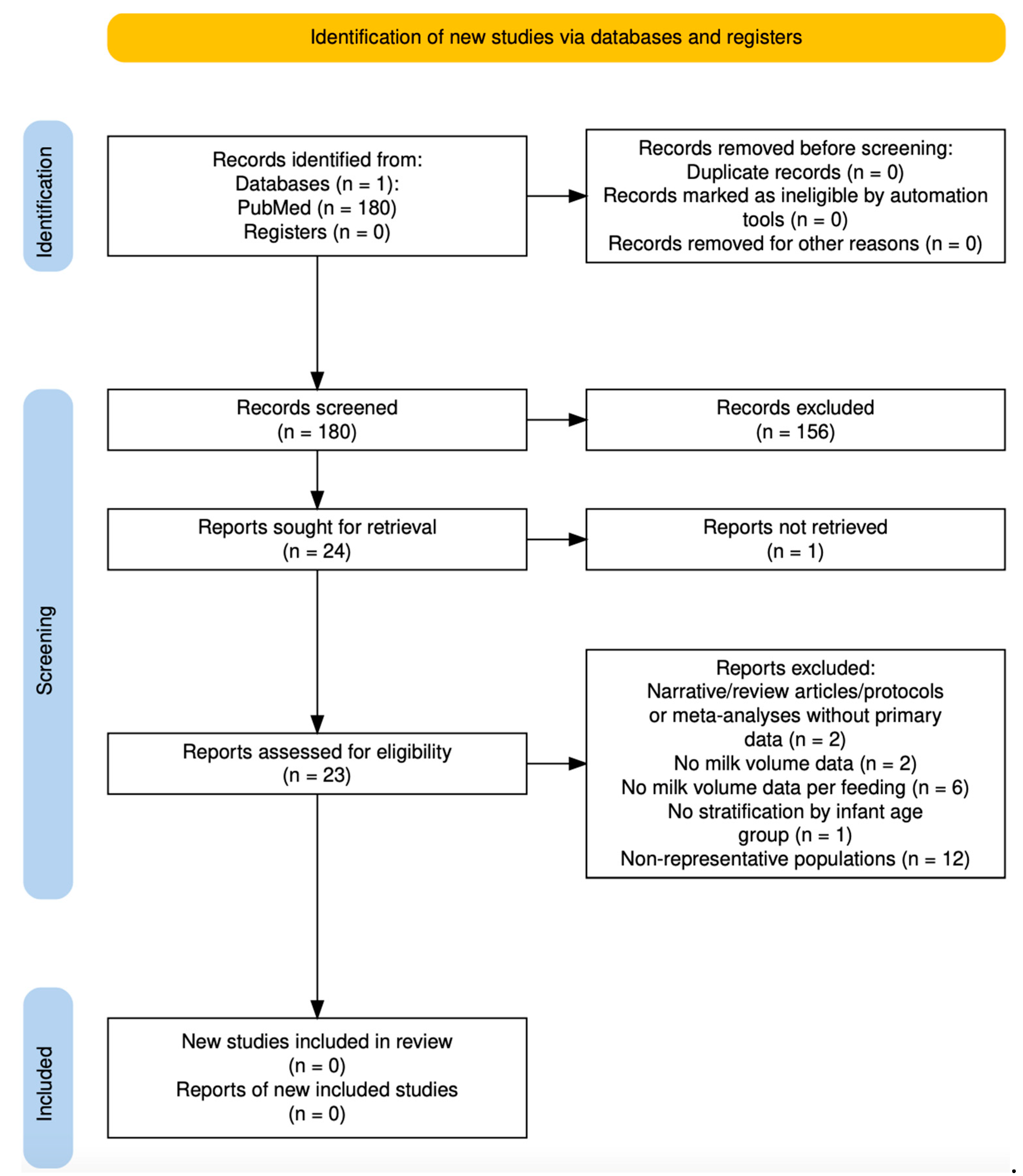
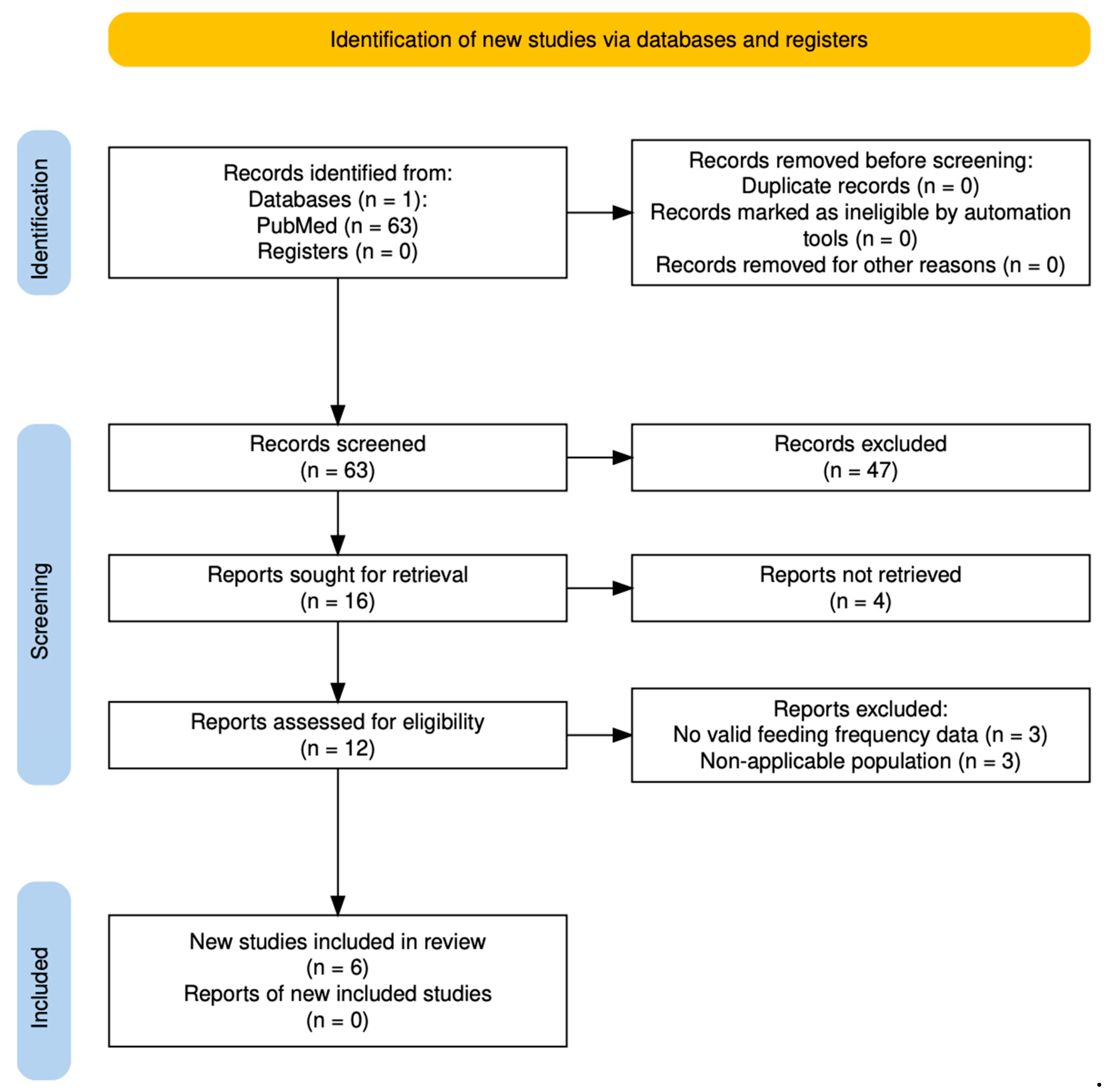
2.3. Systematic Review and Meta-Analysis
- Inclusion: original observational or interventional studies reporting quantitative data on the target variables; healthy, full-term infants aged 0–24 months; and results stratified by infant age or time since birth.
- Exclusion (general):
- Narrative/review articles, editorials, protocols, or meta-analyses without primary data.
- Preterm infants only (unless data for term infants were reported separately).
- Out of time range (<2005).
- Non-human or animal studies.
- Non-applicable populations (e.g., cohorts with severe maternal malnutrition, rare diseases, or humanitarian crisis contexts).
- Studies analyzing donor human milk, due to compositional changes introduced by pasteurization that may alter caloric density and nutrient content [13].
- Other: abstracts without usable data, duplicates, or incomplete reports.
- Caloric density: studies not reporting caloric density or macronutrient content of BM, data not in quantitative format (mean and standard deviation), or those focused solely on biochemical/methodological analyses without cohort-level values.
- BM volume per feeding: studies not reporting BM volume, not providing data per feeding, lacking quantitative format (no means/medians), or using only indirect methods (e.g., maternal recall without test weighing or D2O).
- Feeding frequency: studies not reporting the number of feeds per day in an applicable format (e.g., only weekly frequency, feeding duration without daily count, or broad categorical groups without averages).
2.4. Infant Weight as Input Parameter
2.5. Probability Distributions and Simulation
- Feeding frequency (feeds/day) was modeled using a triangular distribution, suitable for variables with limited data and defined minimum, maximum, and most likely values.
- Volume per feeding (mL/feed) were modeled using Project Evaluation and Review Technique (PERT) distributions, which account for asymmetry and wide individual variability while limiting the influence of outliers. These are appropriate for continuous variables when expert-informed minimum, most likely, and maximum values are available, and normality cannot be assumed.
- Caloric density (kcal/dL) was modeled using either a normal or a PERT distribution, depending on the heterogeneity observed in the meta-analysis. For age groups with low to moderate heterogeneity, a normal distribution was applied using the pooled mean and standard deviation (from the 95% confidence interval). For groups with high heterogeneity, a PERT distribution was used, with CI limits defining the range and the pooled mean as the most likely value. This approach enabled accurate representation of both consistent and variable results while minimizing outlier effects.
- Infant weight was further bounded using a uniform distribution, with the lower and upper limits defined by the 50th percentile values for girls and boys, respectively, according to the WHO Child Growth Standards. This choice constrained values to a biologically plausible range, assuming equal probability across the interval in the absence of more detailed distributional data.
3. Results
3.1. Results of the Systematic Review and Meta-Analysis
3.1.1. Breast Milk Caloric Density
3.1.1. Volume per Feeding
3.1.3. Breastfeeding Frequency
- 1–3 months: 7–10 feeds/day
- 3–6 months: 6–9 feeds/day
- 6–9 months: 5–8 feeds/day
- 9–12 months: 4–7 feeds/day
- 12–18 months: 2–6 feeds/day
- 18–24 months: 2–4 feeds/day
3.1.4. Final Input Parameters for the Probabilistic Analysis
| Age | Feedings per day | Caloric density (kcal/dL) | Volume per feeding (mL) | Median weight stratified by age (WHO growth charts) (kg) |
|---|---|---|---|---|
| (months) | ||||
| 0-1 | 14-8月 | 63.70 [62.10; 65.31] | 30-110 | 3.2-3.3 |
| 1-3 | 10-7月 | 64.95 [62.52; 67.38] | 100-150 | 4.7-5 |
| 3-6 | 9-6月 | 61.66 [60.18; 63.15] | 110-180 | 6.3-7 |
| 6-9 | 8-5月 | 61.74 [60.19; 63.29] | 120-200 | 7.6-8.3 |
| 9-12 | 7-4月 | 76.73 [55.16; 98.30] | 140-200 | 8.5-9.2 |
| 12-18 | 6-2月 | 83.65 [74.32; 92.97] | 160-240 | 9.5-10.2 |
| 18-24 | 4-2月 | 90.43 [81.76; 99.10] | 180-240 | 10.8-11.4 |
| Reference | Thomas et al., 2005; Study Group, 2006, Kent et al. 2006; Saki et al., 2013; Kent et al., 2013; Chen et al., 2015; Gridneva et al., 2018; Huang et al., 2020; Ongpraset et al., 2025 | Saarela et al., 2005; Chang et al., 2015; Grote et al., 2016; Czosnykowska-Łukacka et al., 2018; Fischer Fumeaux et al. 2019; Ongprasert et al., 2020 | Olga et al., 2023; Kent et al. 2006; Kent et al. 2013; Mohr et al., 2023; WHO, 2009. | Child growth standards (WHO) |
| Age | Feedings per day | Caloric density (kcal/dL) | Volume per feeding (mL) | Median weight stratified by age (WHO growth charts) (kg) |
|---|---|---|---|---|
| (months) | ||||
| Distribution | Triangular | PERT*/Normal** | PERT | Uniform |
| 0-1 | a: 8; m: 11; b: 14 | *a: 62.10; m: 63.70; b: 65.3 | a: 30; m: 70; b: 110 | a: 3.2; b: 3.3 |
| 1-3 | a: 7; m: 8.5; b: 10 | *a:62.52; m:64.95; b:67.38 | a: 100; m: 125; b: 150 | a: 4.7; b: 5.0 |
| 3-6 | a: 6; m: 7.5; b: 9 | ** μ: 61.66; σ: 0.76 | a: 110; m: 145; b: 180 | a: 6.3; b: 7.0 |
| 6-9 | a: 5; m: 6.5; b: 8 | ** μ: 61.74; σ: 0.79 | a: 120; m: 160; b: 200 | a: 7.6; b: 8.3 |
| 9-12 | a: 4; m: 5.5; b: 7 | *a: 55.16; m: 76.73; b: 98.30 | a: 140; m: 180; b: 200 | a: 8.5; b: 9.2 |
| 12-18 | a: 2; m: 4; b: 6 | *a: 74.32; m: 83.65; b: 92.97 | a: 160; m: 200; b: 240 | a: 9.5; b: 10.2 |
| 18-24 | a: 2; m: 3; b: 4 | *a: 81.76; m: 90.43; b: 99.10 | a: 180; m: 210; b: 240 | a: 10.8; b: 11.4 |
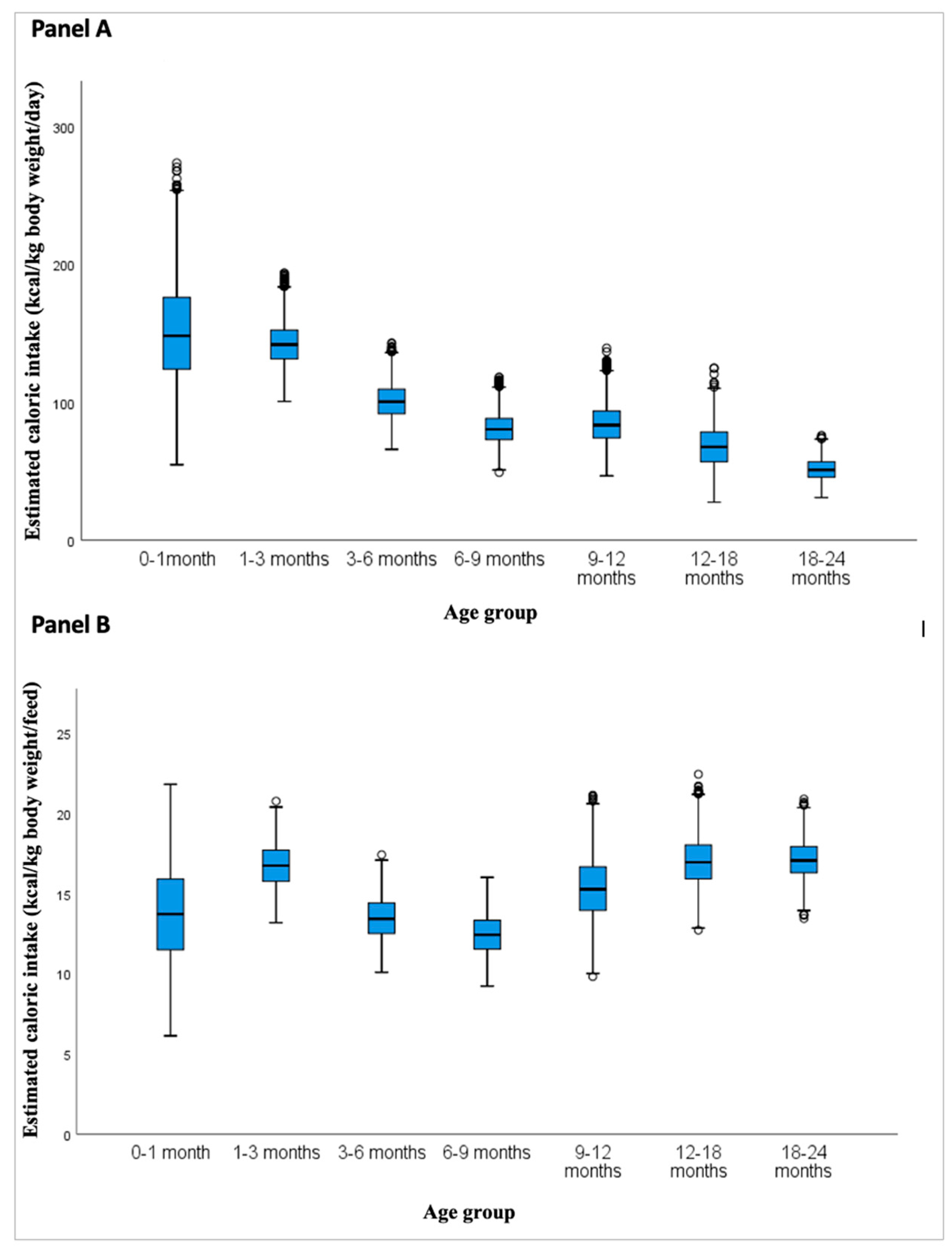
3.2. Probabilistic Model Results
5. Conclusions
Supplementary Materials
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Acknowledgments
Conflicts of Interest
Abbreviations
| BM | Breast Milk |
| CI | Confidence Interval |
| DTM | Deuterium Dilution Technique |
| FT-IR | Fourier-Transform Infrared Spectroscopy |
| GC | Gas Chromatography |
| HIC | High Caloric Intake |
| HPLC | High-Performance Liquid Chromatography |
| IQR | Interquartile Ranges |
| KCAL | Kilocalories |
| LCI | Low Caloric Intake |
| MCI | Medium Caloric Intake |
| MIRIS | Mid-Infrared Human Milk Analyzer |
| PERT | Project Evaluation and Review Technique |
| SD | Standard Deviation |
| USA | United States of America |
| WHO | World Health Organization |
References
- World Health Organization. Global Strategy for Infant and Young Child Feeding; World Health Organization: Geneva, Switzerland, 2003. [Google Scholar]
- Ren, M.; Qiu, Y. The Volume of Breast Milk Intake in Infants and Young Children: A Systematic Review and Meta-Analysis. Breastfeed. Med. 2023, 18, 1–12. [Google Scholar] [CrossRef] [PubMed]
- Hartmann, P.E.; Saint, L. Measurement of Milk Yield in Women. J. Pediatr. Gastroenterol. Nutr. 1984, 3, 270–274. [Google Scholar] [CrossRef] [PubMed]
- George, A.D.; Gay, M.C.L.; Murray, K.; Muhlhausler, B.S.; Geddes, D.T.; et al. Human Milk Sampling Protocols Affect Estimation of Infant Lipid Intake. J. Nutr. 2020, 150, 2924–2932. [Google Scholar] [CrossRef]
- Napoli, C.D.; Pallaro, A.; Fustiñana, C.A.; Mazza, C.S.; Zorzoli, A. Breast Milk Intake and Nutritional Assessment of Exclusively Breastfed Infants. Nutr. Clin. Diet. Hosp. 2019, 39, 120–127. [Google Scholar] [CrossRef]
- Weisgerber, M. C.; Lye, P. S.; Nugent, M.; Li, S.-H.; De Fouw, K.; Gedeit, R.; Simpson, P.; Gorelick, M. H. Relationship between Caloric Intake and Length of Hospital Stay for Infants with Bronchiolitis. Hosp. Pediatr. 2013, 3, 24–30. [Google Scholar] [CrossRef]
- Rocha-Pinto, I.; Pereira-da-Silva, L.; Silva, D. E.; Cardoso, M. Factors That May Affect Breast Milk Macronutrient and Energy Content: A Critical Review. Nutrients 2025, 17, 2503. [Google Scholar] [CrossRef]
- Suwaydi, M.A.; Lai, C.T.; Rea, A.; Gridneva, Z.; Perrella, S.L.; Wlodek, M.E.; Geddes, D.T. Circadian Variation in Human Milk Hormones and Macronutrients. Nutrients 2023, 15, 3729. [Google Scholar] [CrossRef]
- World Health Organization. Child Growth Standards. Available online: https://www.who.int/toolkits/child-growth-standards (accessed on 22 August 2025).
- Fischer Fumeaux, C.J.; Garcia-Rodenas, C.L.; De Castro, C.A.; Courtet-Compondu, M.-C.; Thakkar, S.K.; Beauport, L.; Tolsa, J.-F.; Affolter, M. Longitudinal Analysis of Macronutrient Composition in Preterm and Term Human Milk: A Prospective Cohort Study. Nutrients 2019, 11, 1525. [Google Scholar] [CrossRef]
- Chang, N.; Jung, J.A.; Kim, H.; Jo, A.; Kang, S.; Lee, S.-W. Macronutrient Composition of Human Milk from Korean Mothers of Full Term Infants Born at 37–42 Gestational Weeks. Nutr. Res. Pract. 2015, 9, 433–438. [Google Scholar] [CrossRef]
- Kung, J. Elicit (Product Review). J. Can. Health Libr. Assoc. 2023, 44, 1–3. [Google Scholar] [CrossRef]
- Piemontese, P.; Mallardi, D.; Liotto, N.; Tabasso, C.; Menis, C.; Perrone, M.; Roggero, P.; Mosca, F. Macronutrient Content of Pooled Donor Human Milk before and after Holder Pasteurization. BMC Pediatr. 2019, 19, 58. [Google Scholar] [CrossRef]
- MetaAnalysisOnline. Available online: https://metaanalysisonline.com/ (accessed on 25 August 2025).
- GitHub. pyscripter/XLRisk: Excel Add-in for Performing Monte Carlo Simulation. Available online: https://github.com/pyscripter/XLRisk (accessed on 25 August 2025).
- Czosnykowska-Łukacka, M.; Królak-Olejnik, B.; Orczyk-Pawiłowicz, M. Breast Milk Macronutrient Components in Prolonged Lactation. Nutrients 2018, 10, 1893. [Google Scholar] [CrossRef]
- Ongprasert, K.; Ruangsuriya, J.; Malasao, R.; Sapbamrer, R.; Suppansan, P.; Ayood, P.; Kittisakmontri, K.; Siviroj, P. Macronutrient, Immunoglobulin A and Total Antioxidant Capacity Profiles of Human Milk from 1 to 24 Months: A Cross-Sectional Study in Thailand. Int. Breastfeed. J. 2020, 15, 90. [Google Scholar] [CrossRef]
- Grote, V.; Verduci, E.; Scaglioni, S.; Vecchi, F.; Contarini, G.; Giovannini, M.; Koletzko, B.; Agostoni, C.; for the European Childhood Obesity Project. Breast Milk Composition and Infant Nutrient Intakes during the First 12 Months of Life. Eur. J. Clin. Nutr. 2016, 70, 250–256. [Google Scholar] [CrossRef]
- Saarela, T.; Kokkonen, J.; Koivisto, M. Macronutrient and Energy Contents of Human Milk Fractions during the First Six Months of Lactation. Acta Paediatr. 2005, 94, 1176–1181. [Google Scholar] [CrossRef]
- Kent, J.C.; Mitoulas, L.R.; Cregan, M.D.; Ramsay, D.T.; Doherty, D.A.; Hartmann, P.E. Volume and Frequency of Breastfeedings and Fat Content of Breast Milk throughout the Day. Pediatrics 2006, 117, e387–e395. [Google Scholar] [CrossRef] [PubMed]
- Kent, J.C.; Hepworth, A.R.; Sherriff, J.L.; Cox, D.B.; Mitoulas, L.R.; Hartmann, P.E. Longitudinal Changes in Breastfeeding Patterns from 1 to 6 Months of Lactation. Breastfeed. Med. 2013, 8, 401–407. [Google Scholar] [CrossRef]
- Casey, C. E.; Hambidge, K. M.; Neville, M. C. Studies in Human Lactation: Zinc, Copper, Manganese and Chromium in Human Milk in the First Month of Lactation. Am. J. Clin. Nutr. 1985, 41, 1193–1200. [Google Scholar] [CrossRef] [PubMed]
- Olga, L.; Vervoort, J.; van Diepen, J.A.; Gross, G.; Petry, C.J.; Prentice, P.M.; Chichlowski, M. Associations between Breast Milk Intake Volume, Macronutrient Intake and Infant Growth in a Longitudinal Birth Cohort: The Cambridge Baby Growth and Breastfeeding Study (CBGS-BF). Br. J. Nutr. 2023, 130, 56–64. [Google Scholar] [CrossRef] [PubMed]
- Mohr, A.E.; Senkus, K.E.; McDermid, J.M.; Berger, P.K.; Perrin, M.T.; Handu, D. Human Milk Nutrient Composition Data Is Critically Lacking in the United States and Canada: Results from a Systematic Scoping Review of 2017–2022. Adv. Nutr. 2023, 14, 1617–1632. [Google Scholar] [CrossRef]
- World Health Organization. Infant and Young Child Feeding: Model Chapter for Textbooks for Medical Students and Allied Health Professionals; World Health Organization: Geneva, Switzerland, 2009. [Google Scholar]
- Huang, S.-K.; Chih, M.-H. Increased Breastfeeding Frequency Enhances Milk Production and Infant Weight Gain: Correlation with the Basal Maternal Prolactin Level. Breastfeed. Med. 2020, 15, 639–645. [Google Scholar] [CrossRef] [PubMed]
- Chen, Y.-J.; Yeh, T.-F.; Chen, C.-M. Effect of Breast-Feeding Frequency on Hyperbilirubinemia in Breast-Fed Term Neonates. Pediatr. Int. 2015, 57, 1121–1125. [Google Scholar] [CrossRef] [PubMed]
- Saki, A.; Eshraghian, M. R.; Tabesh, H. Patterns of Daily Duration and Frequency of Breastfeeding among Exclusively Breastfed Infants in Shiraz, Iran: A 6-Month Follow-Up Study Using Bayesian Generalized Linear Mixed Models. Glob. J. Health Sci. 2013, 5, 123–133. [Google Scholar] [CrossRef]
- WHO Multicentre Growth Reference Study Group. Breastfeeding in the WHO Multicentre Growth Reference Study. Acta Paediatr. Suppl. 2006, 450, 16–26. [Google Scholar] [CrossRef]
- Ongprasert, K.; Chawachat, J.; Kiratipaisarl, W.; Siviroj, P. Breast Milk Feeding Practices and Frequencies among Complementary-Fed Children: A Cross-Sectional Study in Northern Thailand. Int. Breastfeed. J. 2025, 20, 28. [Google Scholar] [CrossRef]
- Gridneva, Z.; Rea, A.; Hepworth, A.R.; Ward, L.C.; Lai, C.T.; Hartmann, P.E.; Geddes, D. T. Relationships between Breastfeeding Patterns and Maternal and Infant Body Composition over the First 12 Months of Lactation. Nutrients 2018, 10, 45. [Google Scholar] [CrossRef]
- Thomas, K.A.; Foreman, S.W. Infant Sleep and Feeding Pattern: Effects on Maternal Sleep. J. Midwifery Womens Health 2005, 50, 399–404. [Google Scholar] [CrossRef]
- Martínez Costa, C. Requerimientos energéticos y nutritivos del niño. Recomendaciones dietéticas. In Manual Básico de Nutrición Clínica y Dietética; Mesejo Arizmendi, A., Martínez Valls, J. F., Martínez Costa, C., Eds.; Editorial Médica Panamericana: Madrid, Spain, 2012. [Google Scholar]
| Source | Study (Author, Year) | Country | Design | Sample Size | Age Range Covered | Method Used | Included in Meta-analysis |
|---|---|---|---|---|---|---|---|
| PubMed and Elicit | Saarela et al., 2005 | Finland | Longitudinal cohort | 483 | 1 week–6 months | Chemical/enzymatic methods | Yes |
| Elicit | Chang et al., 2015 | South Korea | Observational cohort | 2000+ | 0–9 months | FT-IR | Yes |
| PubMed and Elicit | Grote et al., 2016 | Multicountry | Cohort | 174 | 1–6 months | GC, HPLC, etc. | Yes |
| PubMed and Elicit | Czosnykowska-Łukacka et al., 2018 | Poland | Mixed methods | 137 | 0–24 months | MIRIS | Partially (9–24 months) |
| PubMed and Elicit | Fischer Fumeaux et al., 2019 | Switzerland | Longitudinal cohort | 61 | 0–3 months | MIRIS | Yes |
| Elicit | Ongprasert et al., 2020 | Thailand | Cross-sectional | 184 | 6–24 months | Colorimetric | Partially (9–24 months) |
| Source | Study (Author, Year) | Country | Design | Sample Size | Age Range Covered | Method Used | Included in Analysis |
|---|---|---|---|---|---|---|---|
| PubMed | Thomas et al., 2005 | USA | Longitudinal cohort | 37 | 4-10 weeks | Structured maternal interviews | Yes |
| Elicit | Study Group, 2006 | Multicountry | Longitudinal cohort | 1743 | 0–24 months | 24-hour recall, structured interview | Yes |
| PubMed and Elicit | Kent et al., 2006 | Australia | Cross-sectional observational | 71 | 1–6 months | Direct observation (not explicitly stated) | Yes |
| Elicit | Saki et al., 2013 | Iran | Longitudinal cohort | 287 | 0–6 months | Structured maternal interviews | Yes |
| Elicit | Kent et al., 2013 | Australia | Longitudinal cohort | 52 | 0–6 months | Direct observation (not explicitly stated) | Yes |
| PubMed | Chen et al. 2015 | Taiwan | Longitudinal cohort | 98 | 0-2 weeks | Direct observation | Yes |
| PubMed | Gridneva et al., 2018 | Australia | Longitudinal cohort | 20 | 0-12 months | Direct observation and structured maternal interviews | Yes |
| PubMed | Huang et al., 2020 | Taiwan | Longitudinal cohort | 65 | 1-28 days | Structured maternal interviews | Yes |
| PubMed | Ongpraset et al., 2025 | Northern Thailand | Cross-sectional observational | 1122 | 6-24 months | Structured maternal interviews | Yes |
| Age | 0-1 | 1-3 | 3-6 | 6-9 | 9-12 | 12-18 | 18-24 | |
|---|---|---|---|---|---|---|---|---|
| (months) | ||||||||
| Mean (p50) | Kcal/kg/feed | 13.71 | 16.75 | 13.46 | 12.43 | 15.32 | 16.99 | 17.11 |
| Kcal/kg/day | 150.8 | 142.34 | 100.92 | 80.83 | 84.28 | 67.94 | 51.33 | |
| SD | Kcal/kg/feed | 2.96 | 1.33 | 1.31 | 1.23 | 1.92 | 1.49 | 1.16 |
| Kcal/kg/day | 36.88 | 16.27 | 12.77 | 11.13 | 14.17 | 15.03 | 7.77 | |
| LCI (Q1) | Kcal/kg/feed | 11.49 | 15.76 | 12.51 | 11.54 | 13.95 | 15.92 | 16.03 |
| Kcal/kg/day | 124.11 | 131.53 | 91.68 | 72.89 | 74.14 | 56.91 | 45.73 | |
| MCI (Q2) | Kcal/kg/feed | 13.71 | 16.74 | 13.42 | 12.43 | 15.27 | 12.72 | 17.06 |
| Kcal/kg/day | 148.33 | 141.98 | 100.41 | 80.46 | 83.42 | 67.64 | 51.01 | |
| HCI (Q3) | Kcal/kg/feed | 15.91 | 17.71 | 14.42 | 13.33 | 16.67 | 18.02 | 17.93 |
| Kcal/kg/day | 176.09 | 152.49 | 109.56 | 88.27 | 93.68 | 78.45 | 56.9 |
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2025 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (http://creativecommons.org/licenses/by/4.0/).





