1. Introduction
Aging is a universal, ongoing, and irreversible process that involves loss of function, but it varies among individuals. Although the Chilean population has a life expectancy of over 80 years, total life expectancy includes both healthy and unhealthy years. Chile has a population of 19.6 million people. The portion aged 60 and over accounts for 18% (3.5 million). Of these, 86% are self-sufficient [
1]. Most older adults receive care through the public health system, with 87.6% of those aged 60 to 64 and 91.9% of those aged 65 and older receiving care through this system.
In addition to changes in vision, hearing, smell, taste, and swallowing, there is also a decrease in salivary flow and a higher risk of tooth loss, along with a gradual decline in muscle mass and strength. Geriatric syndromes [
2] emerge as multifactorial health conditions that develop when deficiencies in multiple systems combine, making older individuals vulnerable to various challenges [
3]. These common conditions, if not managed through interdisciplinary care [
4,
5,
6,
7], threaten independence. This includes sarcopenia and frailty. Handgrip strength (HGS) is a strong predictor of sarcopenia, a condition that contributes to frailty. A primary focus of geriatrics is maintaining autonomy and preventing frailty. Research has shown that the masseter muscle thickness in healthy older adults correlates with grip strength. They suggest that decreased grip strength could indicate reduced masseter muscle mass, especially in men. It is possible to increase masseter muscle thickness by restoring occlusion in healthy older adults, regardless of age [
8]. Other researchers have examined the fit and presence of sarcopenia in removable denture users. Individuals with poorly fitting dentures face a significantly higher risk of sarcopenia than those with well-fitting dentures. Their findings indicate that deteriorating dentition is strongly associated with sarcopenia among community-dwelling Japanese adults aged ≥75 years [
9].
In Chile, the public system, which serves patients with health insurance through the National Health Fund (Fonasa), offers preventive medical exams for older adults (EMPAM)[
10], including a Comprehensive Geriatric Assessment for individuals aged 65 and older. This exam is conducted at Family Health Centers (Cesfam) and involves anthropometric measurements, as well as assessments of functional, mental, and social aspects. It is free, performed annually, and supported by ministerial public policies. Its goal is to identify factors that could lead to loss of functionality and to develop a care and follow-up plan for implementation by the health team, as is common in other regions [
11,
12,
13]. In Chile, significant progress has been made in emphasizing the importance of regular check-ups for older adults. Similar to Mexico [
14], today, 65% of older adults enrolled in primary health care (PHC) have current health records.
The Chilean private health system (Isapres) also includes EMPAM, which specifies the providers that beneficiaries must visit. If people choose to get the exam from providers other than those designated by their insurance, they forfeit the free benefit. They receive a thorough evaluation there, but must pay for the tests they request.
Maintaining natural dentition or using removable dental prostheses (RDPs) is crucial for maintaining masticatory function, ensuring adequate nutrition, and preventing geriatric syndromes in the elderly population (EP). The aim of this study was to compare changes in HGS adjusted for masticatory function, risk of malnutrition, and body mass index (BMI) after denture use in two groups of elderly patients aged 70 and older from the public and private sectors.
2. Method
A prospective, pre-post study was conducted. Between March 2020 and 2023, patients aged 70 years and older, who had no molars or premolars and provided informed consent, were included. They were categorized based on masticatory function according to the Eichner index[
15] and assessed for malnutrition risk or absence using calf circumference (CC) and BMI. Handgrip strength was measured in the dominant hand using a hydraulic handheld dynamometer (Jamar MR) for 2 to 3 seconds in a seated patient with proper dental occlusion. According to the European Working Group on Sarcopenia in the Elderly, grip strength levels of ≤30 kg in men and ≤20 kg in older women indicate a risk of sarcopenia. The Eichner Index categories, which include patients with premolar and molar loss, correspond to categories B and C. For calf circumference, a cutoff point of ≤31 cm was used for both sexes to identify malnourished older adults with low muscle mass and nutritional risk[
16]. Regarding BMI, thinness was defined as a BMI <23.0; normal as 23.0–27.9; overweight as >28.0–31.9; and obesity as ≥32.0 [
17].
MPF measurements were taken at two time points: baseline and 15 days after the prosthesis was used. Differences in MPF were assessed using a linear mixed regression model with SAS 9.4 software (p<0.05). The public system cohort includes patients over 70 years old who received prosthetic treatment at a public hospital in Santiago and participated in a project funded by the National Agency for Research and Development (ANID), with approval from the Ethics Committee of the Eastern Metropolitan Health Service, and signed informed consent.
The private system cohort is derived from secondary data obtained from medical records accessible to the authors, provided by private treating clinicians.
3. Results
The purposive sample consisted of 248 older adults, divided into two groups: 124 in the public system group and 124 in the private system group. Each group had 73 women (p > 0.05), with a mean age of 81.2 years in the public system and 75.2 years in the private system (p < 0.0001).
The mean BMI was 27.0 in those in the public system and 24.7 in those in the private system (p < 0.0001).
The risk of malnutrition due to deficiency, as indicated by calf circumference, was found in 5 beneficiaries of the public system and 31 beneficiaries of the private system (p < 0.0001).
Table 1.
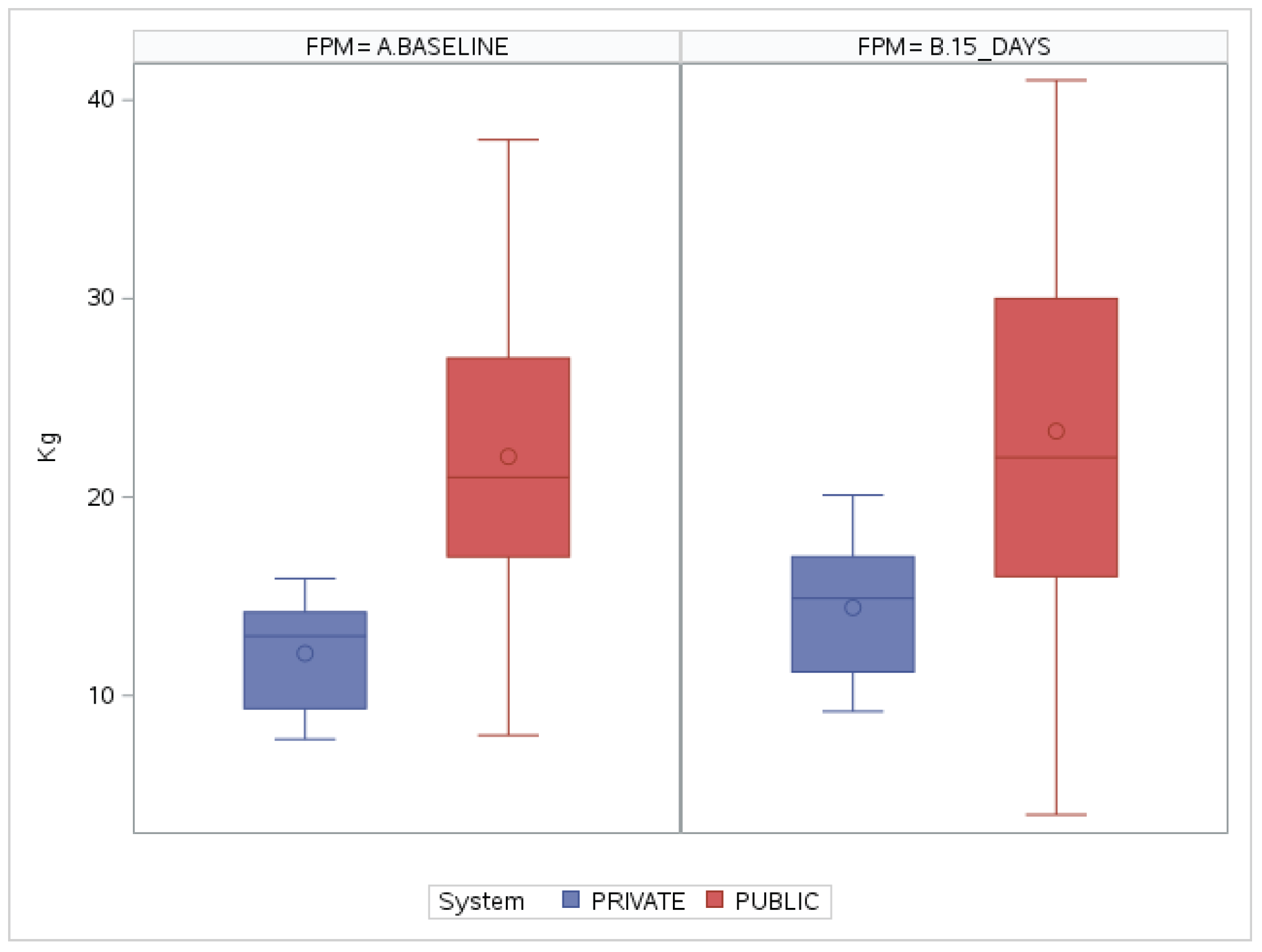
In a multivariate model adjusted for sex, age, BMI, and risk of malnutrition, baseline grip strength before prosthesis use was 22.8 kg in those in the public system and 11.7 kg in those in the private system. The post-prosthesis measurement was 23.0 kg in the public system and 14.2 kg in the private system,
Table 2. The variation in measurements compared to baseline values in the public system was an increase of 1.8 kg, and in the private system, an increase of 2.5 kg.
Comparing the baseline measurements, a positive difference of up to 11.1 kg was observed in the public cohort compared to the private cohort (Δ11.1 kg; p < 0.0001). After treatment, the positive difference decreased slightly to 8.8 kg more handgrip strength in the public system cohort (Δ = 8.8 kg; p<0.0001).
Figure 1.
4. Discussion
The results show a normal nutritional status among older adults in both public and private health systems. This differs from data from the 2016-2017 National Health Survey, which indicated that only 21.5% of people aged 65 and older had a normal nutritional status.
The risk of malnutrition due to deficiency, assessed by calf circumference, was lower than in the Ñuble region of Chile, where 39.6% had deficits, and this was linked to a risk of sarcopenia[
18]. A Spanish study found a higher risk of malnutrition associated with smaller calf circumference measurements, at 74.2%, particularly among individuals over 85 years old [
19].
Regarding handgrip strength values, improvements were seen in both groups, with more notable results at baseline and within the private system. These were analyzed as a continuous numerical variable. In the model used, sex was not a significant explanatory variable because the groups were balanced, so no differences by sex were observed.
The differences between users of the two health systems may stem from the fact that individuals in the public system are regularly monitored at primary care centers, where, through the Preventive Medical Examination for Older Adults (EMPAM), which includes the Comprehensive Geriatric Assessment, they are referred to the appropriate specialist when abnormalities are found. In contrast, monitoring in the private system relies on patients’ spontaneous requests, often leading to additional out-of-pocket costs. This situation could indicate that many older adults in the private system might be experiencing malnutrition or clinically unrecognized muscle loss, which directly affects their handgrip strength and may partly explain the observed findings.
Handgrip strength has been suggested as a new vital sign in older adults, serving as a key health biomarker that assesses muscle function and overall physical capacity. Including HGS in routine health assessments is believed to enhance risk stratification and inform prevention strategies [
20].
5. Conclusions
The use of RDPs immediately improves HGS in older adults in both the Chilean public and private sectors, with significant differences of up to 8.8 kg between the two groups, favoring the cohort served in the public sector.
References
- Felipe Hugo, Luis Rodríguez y Julibeth Rodríguez. Documentos de trabajo ENVEJECIMIENTO EN CHILE: Evolución, características de las personas mayores y desafíos demográficos para la población. Instituto Nacional de Estadísticas, Chile. Septiembre de 2022. https://www.ine.gob.cl/docs/default-source/demografia-y-migracion/documentos-de-trabajo/documentos/envejecimiento-en-chile-evolucion-y-caracteristicas-de-las-personas-mayores.pdf?
- Abellán G, Abizanda P, Alastuey C et al. Tratado de Geriatría para Residentes. Soc Española Geriatría [Internet]. 2020 [cited 2024 Aug 17];143–144. Available from: www.segg.
- Halpern, L.R. The Geriatric Syndrome and Oral Health. Dent. Clin. North Am. 2020, 64, 209–228. [Google Scholar] [CrossRef] [PubMed]
- Zhang, M.; Zhao, M.; Wei, X. Research progress on community health management model for older adults with chronic diseases and multiple morbidities. Br. J. Hosp. Med. 2024, 85, 1–9. [Google Scholar] [CrossRef]
- Zisberg, A.; Rayan-Gharra, N.; Danial-Saad, A.; Rogozinski, A.; Fraiman, P.; Segel-Karpas, D. Age-Friendly Healthcare: An Evolutionary Concept Analysis. J. Clin. Nurs. 2024, 33, 4635–4650. [Google Scholar] [CrossRef] [PubMed]
- Sääskilahti, M.; Kulmala, J.; Nurhonen, M.; Lehtisalo, J.; Peltonen, M.; Mangialasche, F.; Laatikainen, T.; Strandberg, T.; Antikainen, R.; Tuomilehto, J.; et al. The effect of multidomain lifestyle intervention on health care service use and costs - secondary analyses from the Finnish Geriatric Intervention Study to Prevent Cognitive Impairment and Disability (FINGER): a randomised controlled trial. Age and Ageing 2024, 53. [Google Scholar] [CrossRef] [PubMed]
- Gough, C.; Damarell, R.A.; Dizon, J.; Ross, P.D.; Tieman, J. Rehabilitation, reablement, and restorative care approaches in the aged care sector: a scoping review of systematic reviews. BMC Geriatr. 2025, 25, 1–13. [Google Scholar] [CrossRef] [PubMed]
- Yamaguchi, K.; Tohara, H.; Hara, K.; Nakane, A.; Kajisa, E.; Yoshimi, K.; Minakuchi, S. Relationship of aging, skeletal muscle mass, and tooth loss with masseter muscle thickness. BMC Geriatr. 2018, 18, 1–7. [Google Scholar] [CrossRef] [PubMed]
- Iwasaki, M.; Kimura, Y.; Ogawa, H.; Wada, T.; Sakamoto, R.; Ishimoto, Y.; Fujisawa, M.; Okumiya, K.; Ansai, T.; Miyazaki, H.; et al. The association between dentition status and sarcopenia in Japanese adults aged ≥75 years. J. Oral Rehabilitation 2016, 44, 51–58. [Google Scholar] [CrossRef] [PubMed]
- EMPAM, disponible en https://www.minsal.
- Dakey, S.K.; Maxwell, H.; Siette, J. Towards cultural inclusion for older adults from culturally and linguistically diverse communities: A commentary on recent aged care reforms. Australas. J. Ageing 2024, 44. [Google Scholar] [CrossRef]
- Liangruenrom, N.; Thang, L.L.; Satchanawakul, N. Systematic scoping review of ageing in place strategies in Japan, Singapore and Thailand: A comparative analysis. Australas. J. Ageing 2024, 44. [Google Scholar] [CrossRef]
- Mohan, A.; Jothikaran, T.A.J.; Gudi, N.; A K, A.; Ashok, L. Growing old before growing rich: a scoping review on ageing-related policy interventions from the WHO Southeast Asian Region. BMJ Open 2025, 15, e079621. [Google Scholar] [CrossRef]
- Santoyo-Sánchez, G.; Reyes-Morales, H. Health needs of older people: a challenge for primary health care. Gac. medica de Mex. 2024, 160, 249–256. [Google Scholar] [CrossRef]
- Nakatsuka, Y.; Yamashita, S.; Nimura, H.; Mizoue, S.; Tsuchiya, S.; Hashii, K. Location of main occluding areas and masticatory ability in patients with reduced occlusal support. Aust. Dent. J. 2010, 55, 45–50. [Google Scholar] [CrossRef]
- Miranda Ocariz JM, Meza Miranda E. Utilidad de la circunferencia de pantorrilla como marcador de desnutrición en relación con el mini nutritional assessment, nutritional risk screening 2002 y albúmina sérica en adultos mayores. Rev. cient. cienc. 1: salud 2022; 4(2), 2022.
- Mery Cristy Núñez Sánchez y Rossy María Elena Reyes Huarcaya. Importancia de diferenciar puntos de corte del IMC de acuerdo a la edad. Nutr. Hosp. 2017; 34(5):1263 ISSN 0212-1611 - CODEN NUHOEQ S.V.R.
- Barraza-López, R.J.; Muñoz-Navarro, N.A.; Behrens-Pérez, C.C. Relationship between emotional intelligence and depression-anxiety and stress in medical students freshmen. Rev. Chil. Neuro-Psiquiat. 2017, 55, 18–25. [Google Scholar] [CrossRef]
- Emilia María López Lirola, María Concepción Iríbar Ibabe y José María Peinado Herreros. La circunferencia de la pantorrilla como marcador rápido y fiable de desnutrición en el anciano que ingresa en el hospital. Relación con la edad y sexo del paciente. Nutr. Hosp. vol.33 no.3 Madrid may./jun. 2016. https://scielo.isciii.es/pdf/nh/v33n3/10_original9.
- Vaishya, R.; Misra, A.; Vaish, A.; Ursino, N.; D’aMbrosi, R. Hand grip strength as a proposed new vital sign of health: a narrative review of evidences. J. Heal. Popul. Nutr. 2024, 43, 1–14. [Google Scholar] [CrossRef] [PubMed]
|
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2025 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (http://creativecommons.org/licenses/by/4.0/).