1. Introduction
At the International Dental Congress in Berlin in 1909, Emil Herbst presented a fixed bite jump device for the treatment of class II, device which held the mandible in a forced anterior position [
1]. The maxilla, mandible and muscle function are changed and the appliance was therefore considered as a fixed functional appliance [
2]. Until 1979 there were few publications; in that year Pancherz drew attention to the possibilities of stimulating the condylar growth of the mandible by means of this device [
3,
4,
5]. The growing diffusion of this device in recent times depends on the advantage of not requiring the patient's collaboration and the reduction in treatment times compared to equipment such as the twin block. The objective is to correct the sagittal discrepancy, stimulate mandibular growth and reshape the condyle-glenoid fossa relationship [
6,
7], causing anterior rotation of the mandible [
8]. Therapy with the Herbst device alone typically lasts 6 to 9 months [
8]. The therapy is integrated by treatment with multi-brackets equipment, which in some studies represents a second phase of treatment [
9,
10], in others the modality and timing of this therapeutic phase is not specified [
11]; in others it is not even foreseen, so the treatment ends only with treatment with Herbst [
12].
This extremely heterogeneous condition, both in terms of the therapeutic devices used, the sequence of their use, and the length of time they are used, makes it difficult to evaluate the problems and outcomes related to anterior mandibular repositioning.
In fact, the presence of anterior mandibular repositioning devices that are either fixed or mobile should be considered a major factor. In fact, they hold the mandible in therapeutic position either continuously or intermittently: the adaptation of musculo-skeletal structures might be affected differently. With Herbst device, the condyles are initially repositioned inferiorly and anteriorly compared to their original position [
13]. The application of the device induces an immediate movement of the condyles along the path of the articular eminence, in a different position from the initial one: this leads to the hypothesis of morphological changes [
14]. However, subsequent studies indicate that at the end of treatment there are no significant differences in the condylar posi-tion compared to the initial [
14,
15,
16,
17]. In these studies, however, patients were treated with unspecified functional devices [
17] or different from traditional Herbst, i.e. with the use of acrylic splints [
15] or FMA [
16].
Treatment with Herbst has been shown not to increase the prevalence of temporo-mandibular disorders. Some studies demonstrate significant joint improvements with initial disc displacement anteriorly, whit MR [
18,
19]. Furthermore, treatment with Herbst does not appear to produce clinically significant changes in the middle cranial fossa and central skull base [
20,
21]. Nevertheless, an assessment of the exact position of the condylar disc in relation to the fossa with detailed three-dimensional images would be appropriate whenever mandibular displacement devices are used. In fact, the device is applied in patients in the evolutionary growth phase that ensure an adaptation of the structures from an anatomical-functional point of view, but not in patients at the end of growth. In any case, with this device it is advisable to treat patients who have completed the dental permutation phase up to the first premolars to ensure better strategic anchorage. Respiratory function has a huge impact not only on physiology but also affects the quality of life of patients [
22]. It is known that the pharyngeal airway space is influenced by the craniofacial sagittal shape. Therefore, subjects have different airway dimensions [
23] in relation to a normal, retrognathic or prognathic mandible. The sagittal position of the mandible influences the position of the hyoid bone and tongue by the genioglossus and mylohyoid muscles, which have a close relationship with the size of the pharyngeal airway. Mandibular retrognathism is associated with narrower airway passage. The posterior and inferior directions of mandibular growth can influence obstructive sleep apnoea syndrome [
24]. In some studies it has been observed that the Herbst appliance provides an improvement in oropharyngeal and hypopharyngeal airway dimensions [
25].
It is therefore clear that the therapeutic results of the studies present in the literature can be influenced by the lack of standardization of the therapeutic phases in combination with brackets, from the difference in the design of the DJ Herbst device (as will be described later), from the confluence in the results of studies of therapies performed with devices that are very different from each other in terms of materials used, modes of operation, neuro-muscular adaptation, possibility of removing the device, hours of application of the equipment in the oral cavity and related prescription.
In our opinion, the standardization of therapy according to precise protocols can positively influence the therapeutic result, through obtaining rapid occlusal stabilization, neuro-muscular balance, less stress on the anchoring units and shorter treatment time. To evaluate the effects and effectiveness of the device, at a diagnostic level, it is necessary to identify the real II skeletal classes due to mandibular retrusion without micrognathia since the effect of the Herbst device in any case can only express a growth potential inherent in the individual, without substantially modifying it. Therefore, a genetically small jaw cannot be substantially modified with advance therapy. It is therefore essential at a diagnostic level, a detailed understanding of the measurements that refer to mandibular morphology. Furthermore, the presence of border-line cases in which the patient presents a class II canine of over 7 mm with further protrusion of the incisors and therefore a clinical picture of a mixed defect where a partial distalization of the anterior dentition of the upper arch is also necessary, can modify the outcome is an anterior repositioning of the mandible using the Hesbst device beyond the effective limit achievable and compatible with the new condylar position. This can easily lead to a recurrence of the advancement treatment with Herbst. For this reason, preventive preparation of the arches with multi-brackets equipment is essential to correct all the problems of excessive protrusion of the anterior teeth, diastemas, alteration of the shape of the dental arches (especially even slight contraction of the maxillary dental arch given that it affects the mandibular position in terms of retrusion), asymmetries of the dental class due to particular clinical conditions, for example rotations, dysmorphism of dental elements, etc. Secondly, a fundamental aspect for therapeutic success and for the containment of unwanted effects is represented by obtaining occlusal stabilization in the shortest possible time following the application of the Herbst de-vice.
2. Materials and Methods
The main features of the two devices are described, and then a clinical case treated with the simplified device is reported.
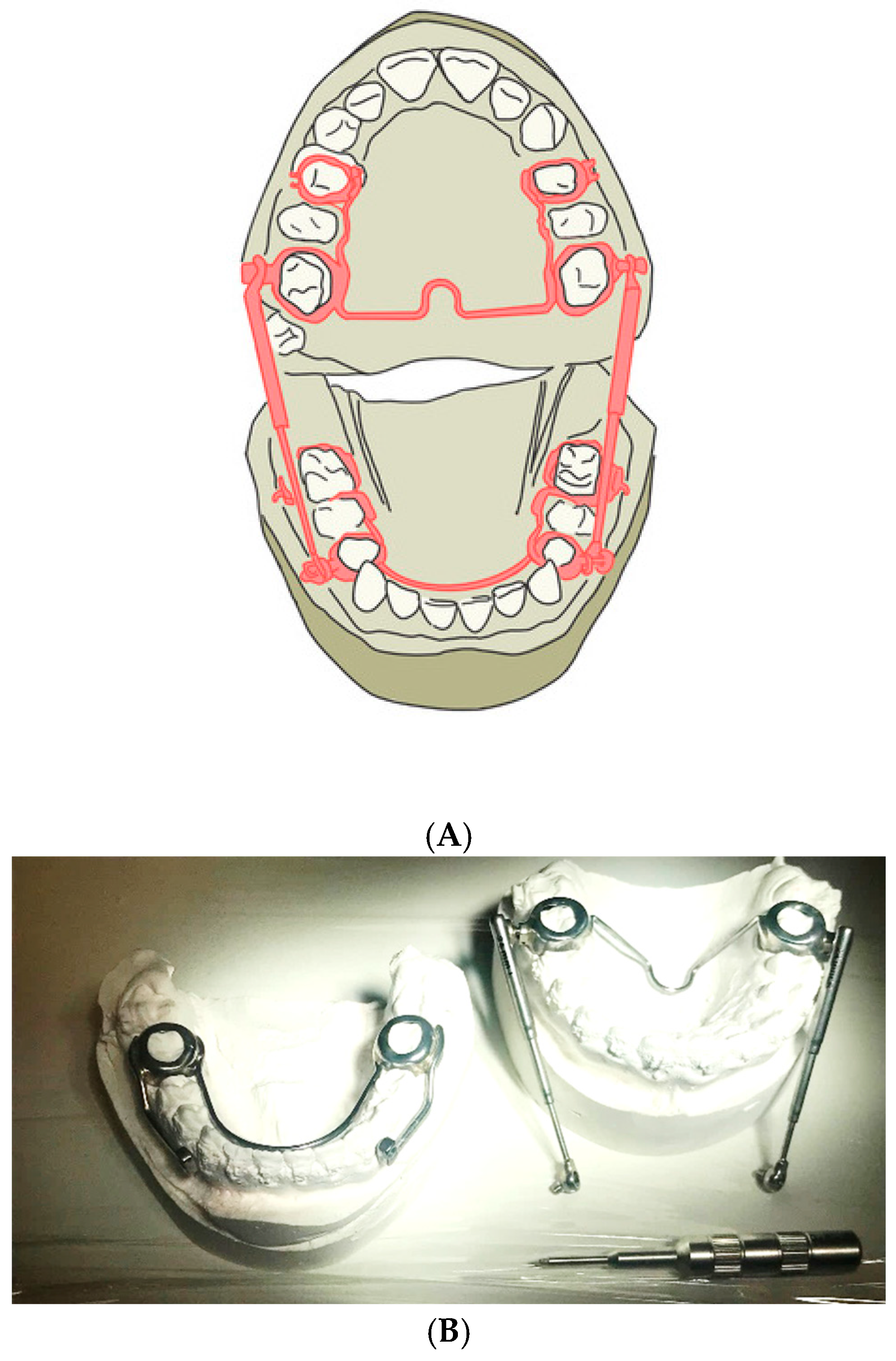
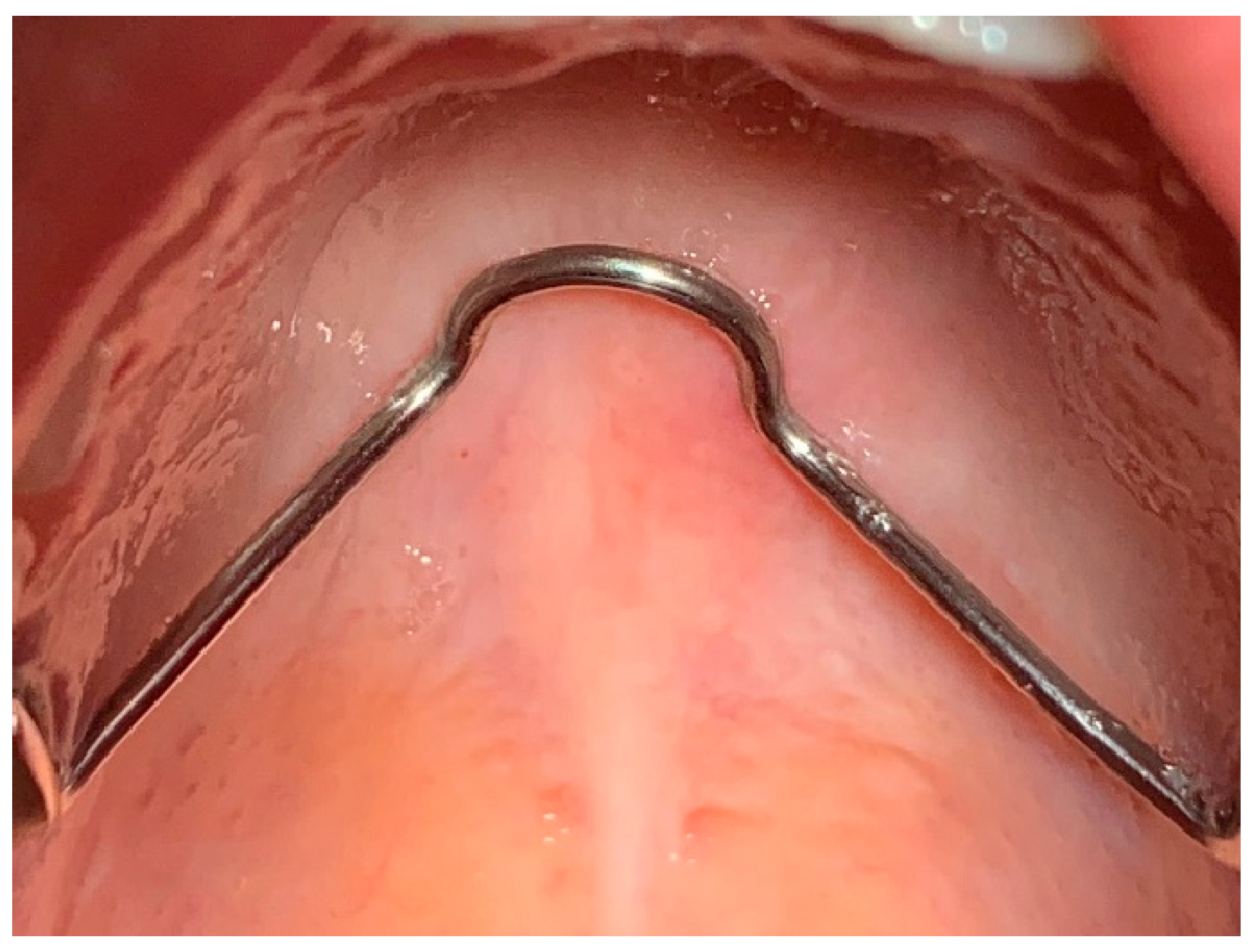
2.1. Traditional Design
Traditionally, the Herbst device involves taking impressions of patients with permanent dentition with 4 bands for each arch, respectively first molars and first permanent premolars. The technical laboratory proceeds to solidify the bands by including the second premolar with shaped buccal and palatal bars in the archorage unit. Therefore the premolars and the molar of the same hemi- arch work as a single anchorage unit. The right unit and the left unit of the same arch are connected and mutually stabilized by wire elements of appropriate diameter: for the upper arch there is a trans-palatal bar welded onto the bands of the sixths and distanced from the soft tissues to avoid mucous decubitus on the palate; for the lower arch there is a lingual arch welded onto the first premolar which touches the tracks of the lower incisors. These wire elements serve to increase the stability of the anchoring units and reduce the effects of unwanted muscle forces (
Figure 1A). In our opinion, this structure is the most solid, least subject to breakage, most effective in managing anchorage and best performing since it leaves the dental cusps of the teeth with bands exposed. Indeed this allows the dental gear when you bring your teeth to contact.
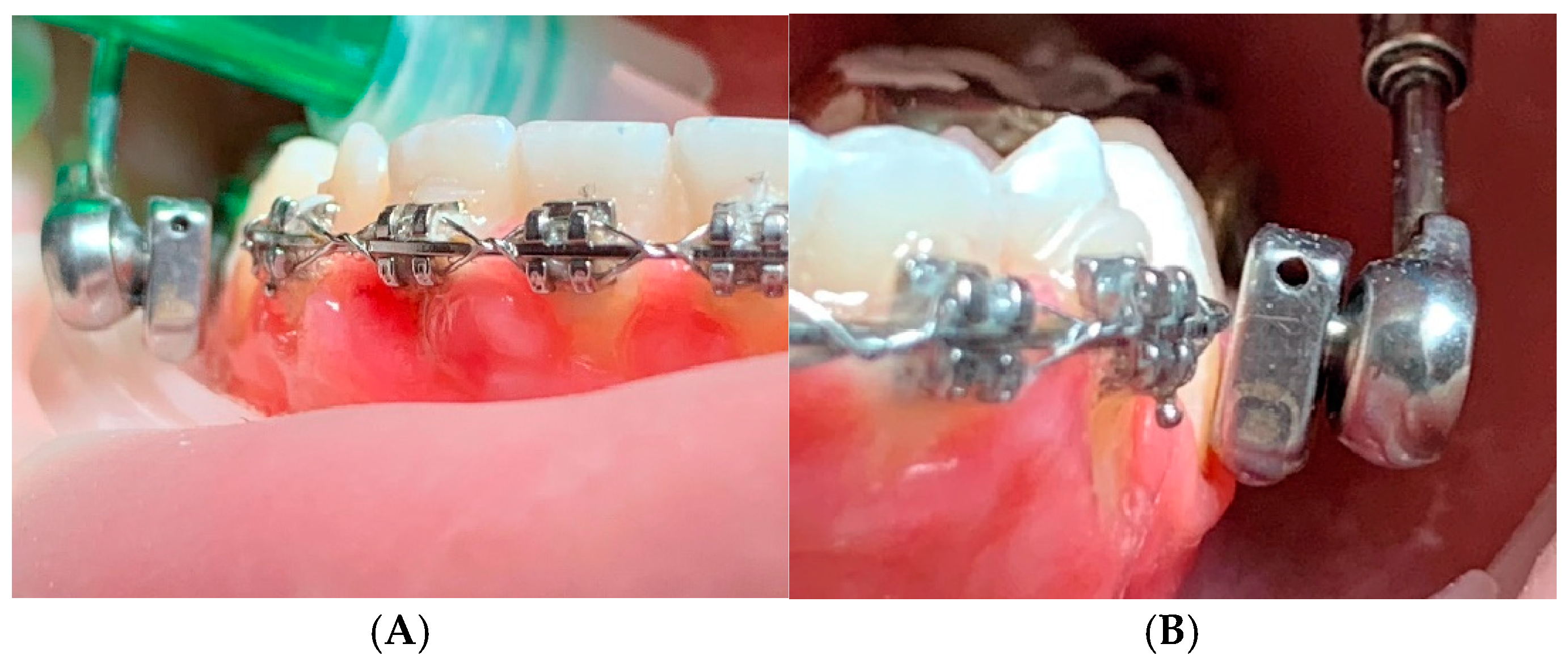
2.2. Simplified Design
The Herbst device can be modified by not providing the bands on the premolars: instead it has an arm welded onto the band of the lower molar which extends horizontally up to the first lower premolar: it is spaced from the mucosa by approximately 1 mm to reduce the bulk in the oral fornix and is positioned approximately at the height of the gingival margin of the first premolar. The joint of the telescopic tube is inserted in this point of the arm, which in this version of the device allows greater freedom in lateral movements thanks to its characteristics. The telescopic tube at the top fits onto another joint welded onto the band of the upper sixth. This allows the presence of the equipment on the upper arch limited to the sixths, while the rest of the arch is not obstructed. The design of the band provides almost total occlusal coverage to increase band retention and control over the dental effects of the applied forces (
Figure 1B).
The main differences can be summarised in
Table 1 to make the explanation more intuitive.
| |
Traditional design |
Simplified design |
| Total number of bands per arch |
4 |
2 |
| First molar bands |
Normal |
Partial occlusal coverage |
| Goshgarin trans-palatal bar |
Present |
Present |
| Welded lingual arch |
Present |
Present |
| Welded arm extension from molar to first premolar |
Present |
Absent |
| Left and right telescopic tube |
Present |
Present |
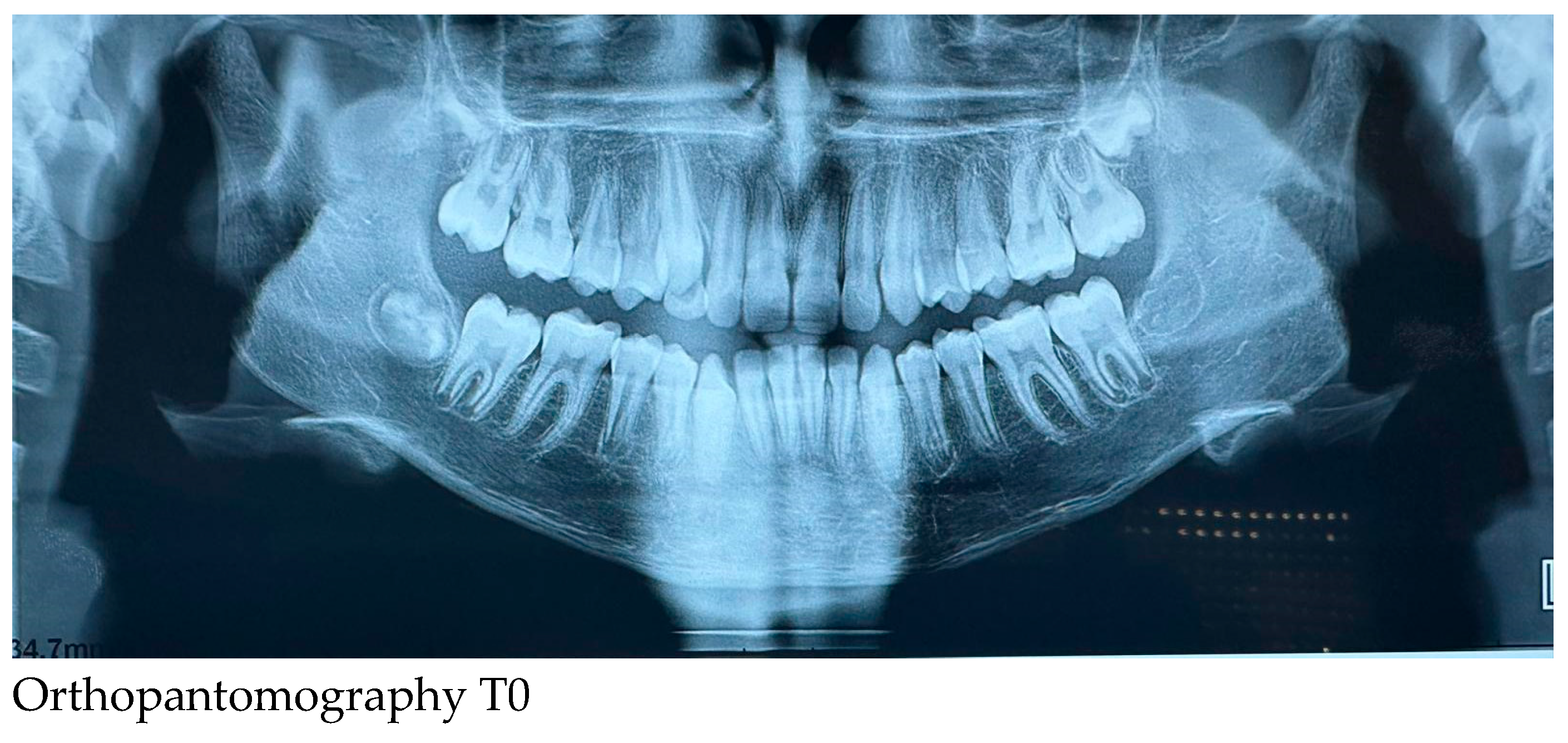
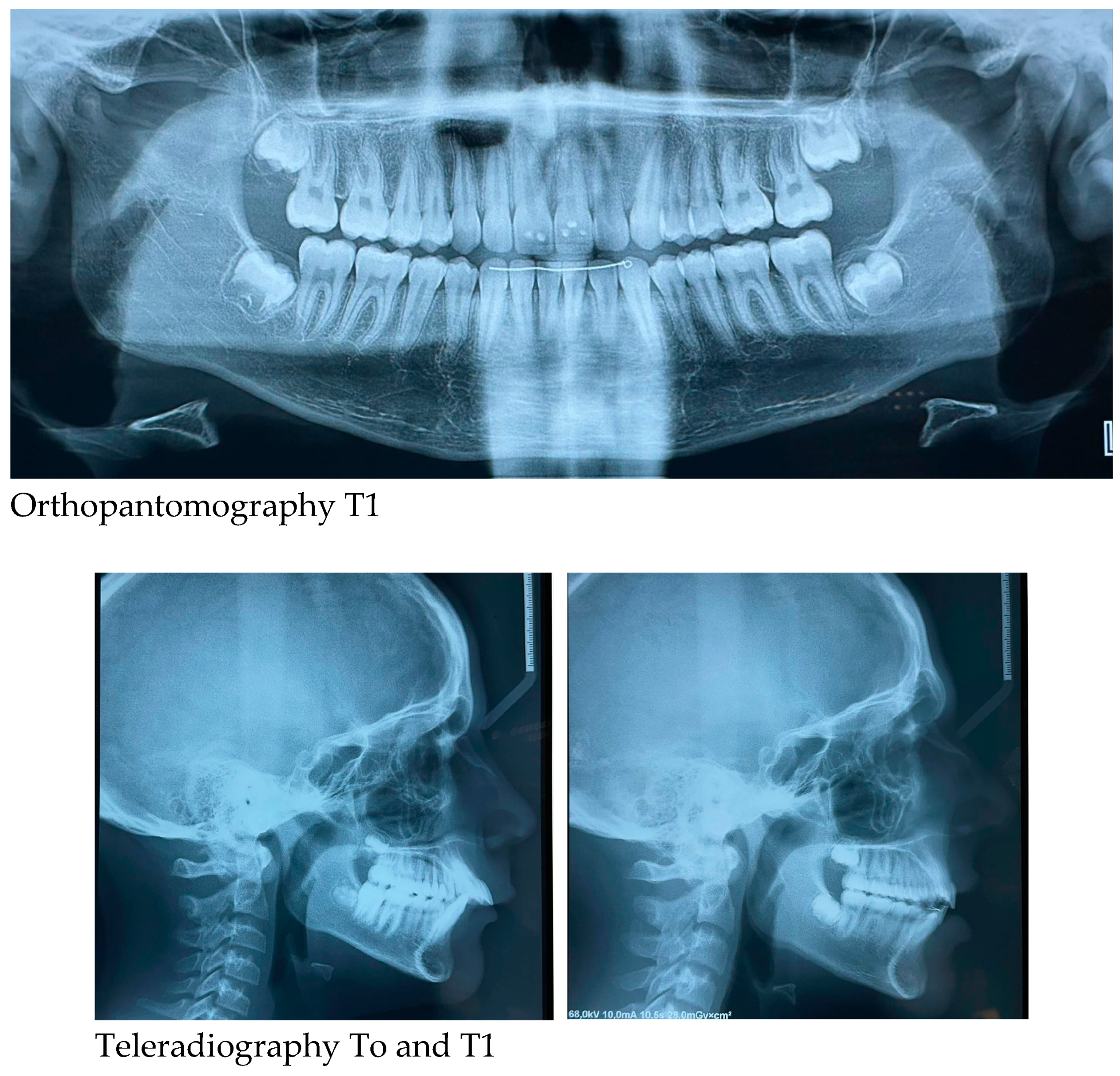
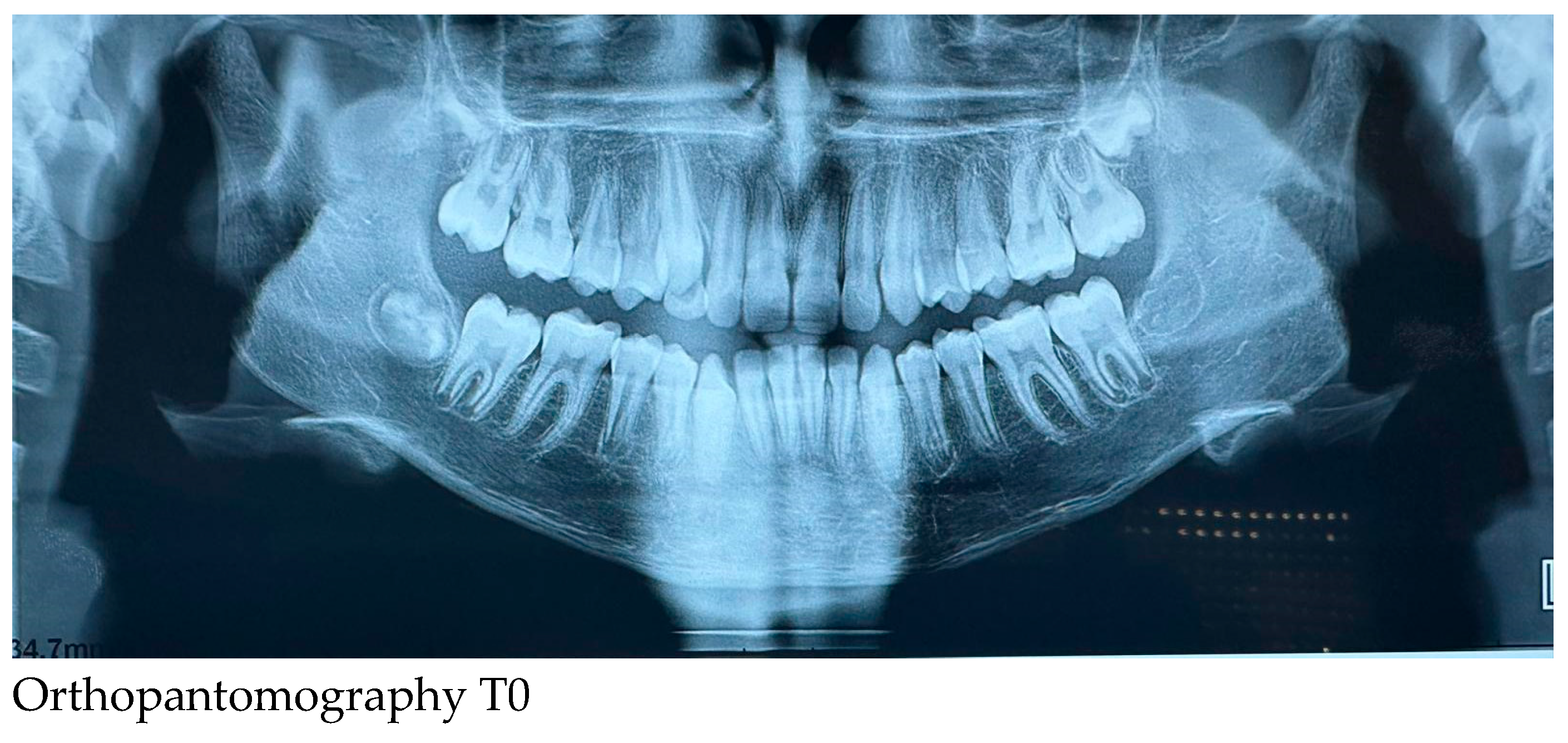
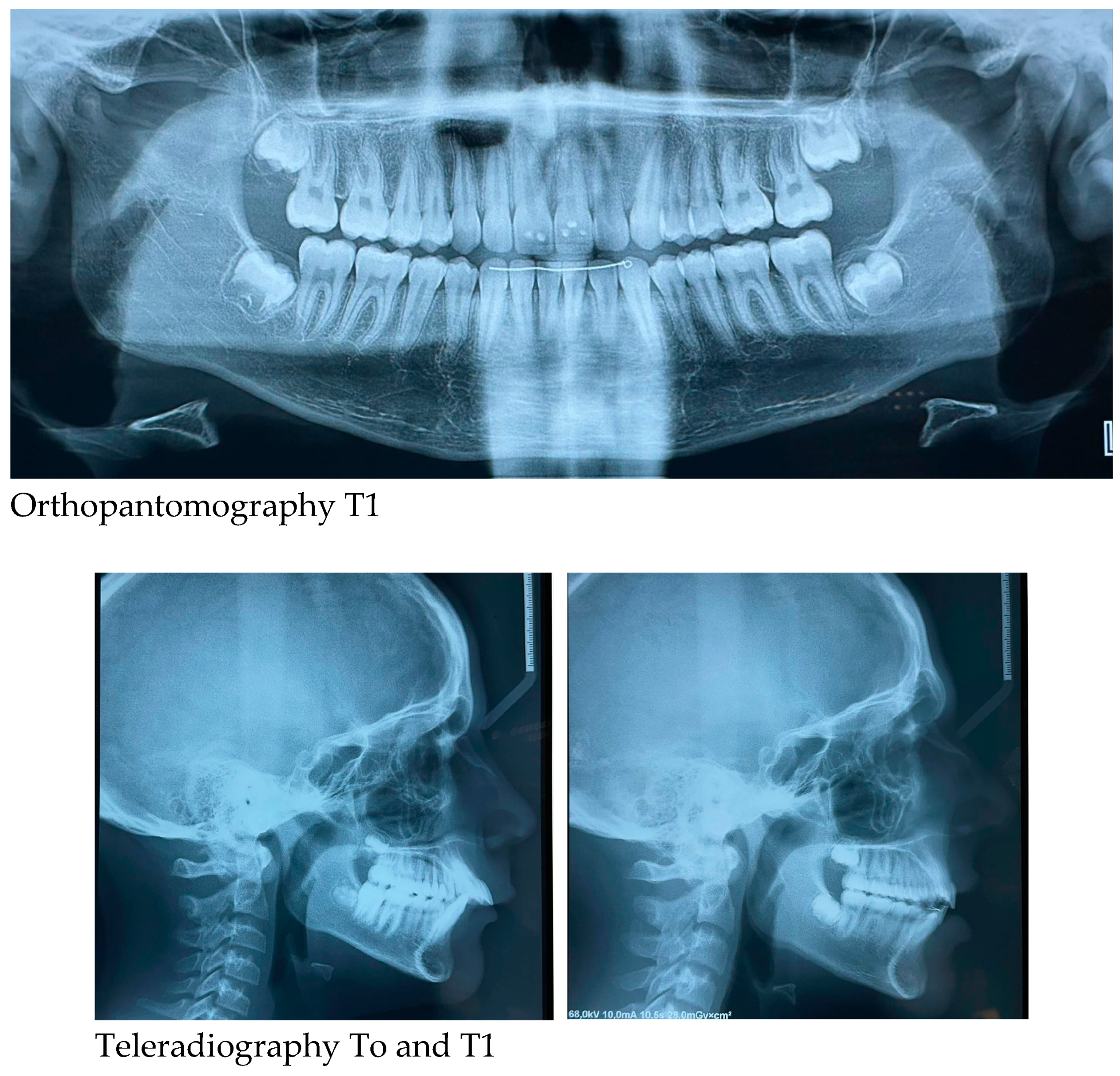
2.3. Initial and Post-Treatment Records
Orthopantomography of the dental arches and lateral skull teleradiography taken before (T0-at the start of treatment) and at the end of Herbst-RPE therapy (T1-after removal of braces) were evaluated. The subject was positioned in the natural head position, with the teeth in centric occlusion and with the lips slightly closed for lateral cephalometric radiographs.
2.4. Results (Primary and Secondary)
Radiographs such as orthopantomography and lateral skull teleradiography are provided. The cephamolecular analysis shows some changes: improvement of the Wits index, growth of the mandibular ramus while keeping the position of the lower incisors almost unchanged (
Table 1).
| |
Reference values |
Measurements T0 |
Measurements T1 |
| SN^A |
82° |
80° |
82,5° |
| SN^B |
80° |
75° |
76° |
| AN^B |
2° |
5° |
6,5° |
| WITS |
0 mm |
4 mm |
3 mm |
| SN^GoMe |
32° |
35° |
36° |
| SN^SnaSnp |
8° |
7° |
6° |
| SnaSnp^GoMe |
26° |
28° |
30° |
| P.O.^GoMe |
16° |
19,5° |
17° |
| GoMe^GoPc |
126° |
128° |
122° |
| GoMe^GoN |
73° |
71° |
73° |
| GoN^GoPc |
53° |
57° |
49° |
| SGn^SN |
67° |
68° |
69° |
| SGo /NMe |
62% |
62% |
63% |
| |
|
|
|
| I+^I- |
131° |
106° |
130° |
| SnaSnp^I+ |
109° |
126° |
105° |
| GoMe^I- |
90° |
102° |
104° |
| Overjet |
2 mm |
9 mm |
2,5 mm |
| NB^LsPgC |
8° |
17° |
11,5° |
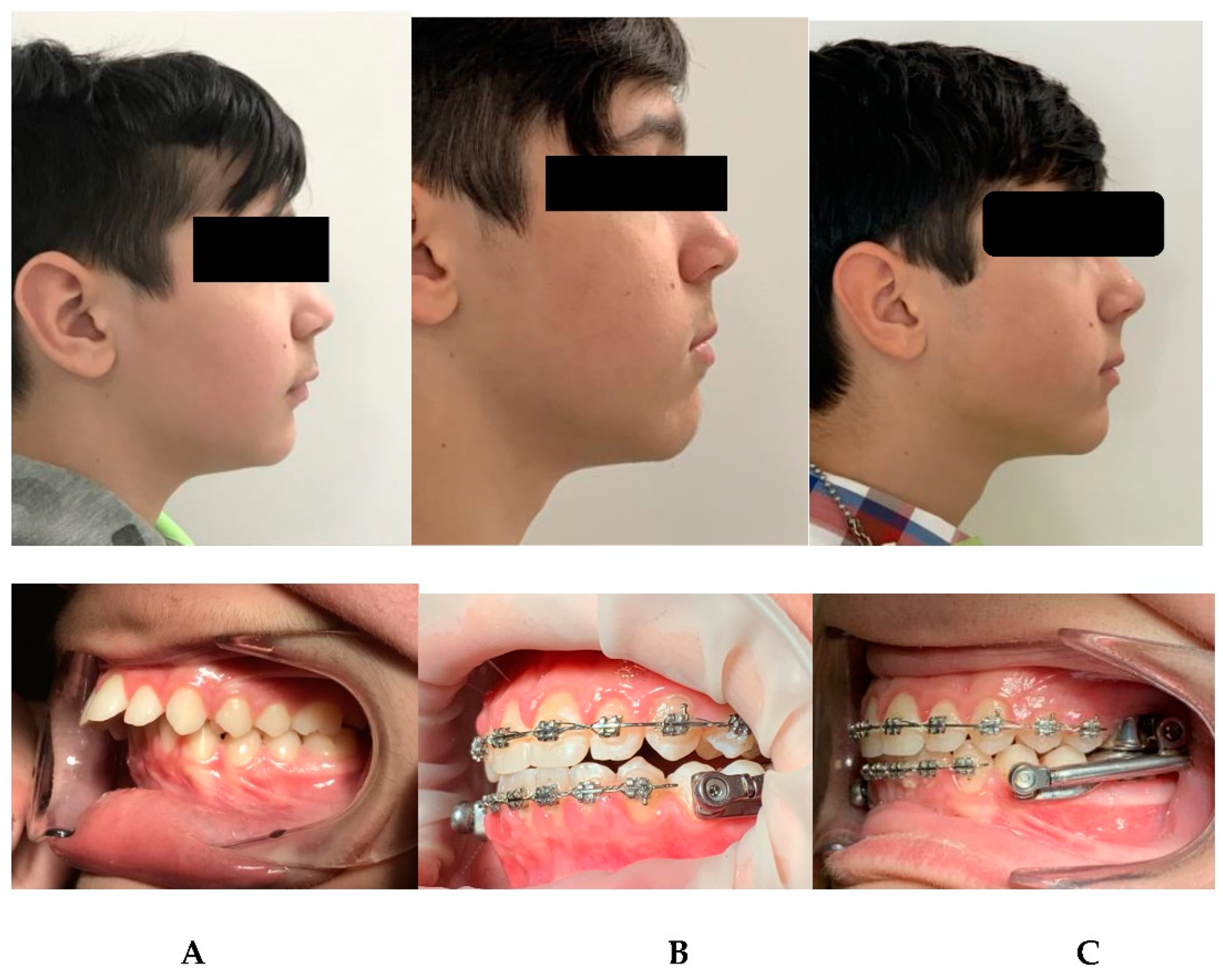
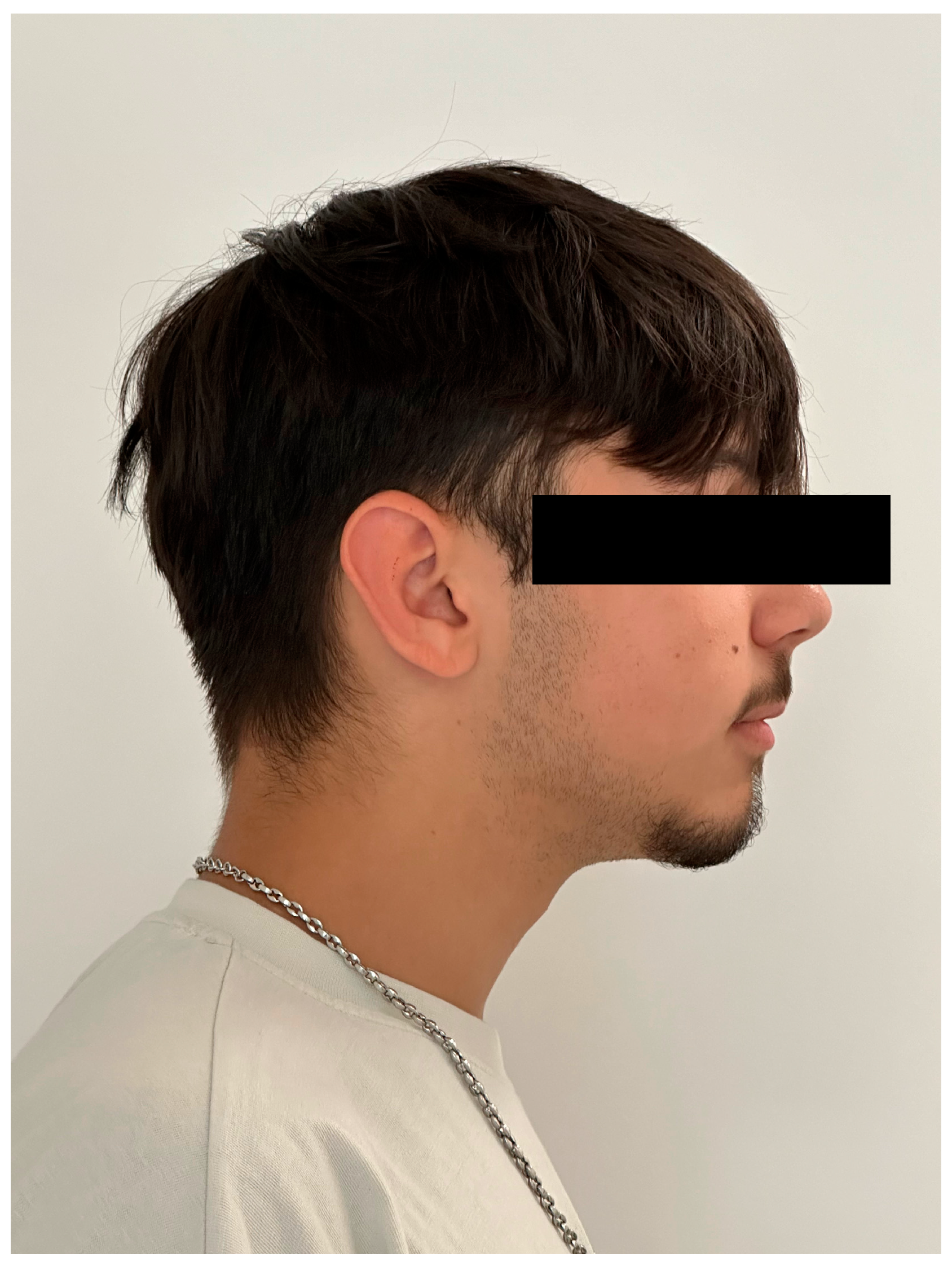
2.5. Case Report Throughout Clinical Phases
The following is a case in which the simplified model and the sequence of clinical phases were used. In our clinical practice, the treatment begins with a phase of alignment and leveling of the arches, elimination of the excessive pro-inclination of the incisors (for example in the case of diastemas as visible in photo (
Figure 2a,b), coordination of the arches through coordinated final steel arches; coordination is checked clinically by manually guiding the patient and asking for the positioning of the protruding mandible with contact of the incisal edges with approximately 2 mm of overjet.
At this point of the treatment, the simplified Herbst device is applied: the dental arches remain spaced apart for a period of 7 days from the application of the device in the mouth. In this adaptation period, initially only the incisors of the upper arch make contact with those of the lower arch, in a ratio of 1mm of overjet (
Figure 3). The re-maining dental elements of the frontal group are supported by a rectangular sectional wire. Through the procedure of preparing the arches with MBA, phase with the Herbst device, and finalizing the therapy again with MBA, the treatment times in this clinical case were reduced in the phase with Herbst to 5 months compared to the 6-9 expected. This can be an interesting aspect both for less permanence of the device in the mouth which has a specific size, and for greater cleanability of the oral cavity and patient comfort.
3. Results and Discussion
3.1. Clinical Observations When Using the Herbst Device
The increased overjet (compared to what is usually brought to 0 mm) allows for faster achievement of intercuspation. After a week the overjet will have increased and will allow the intercuspation of the posterior teeth. In this period of time the dentoskeletal system and the neuromuscular system undergo adaptive phenomena that allow the dental arches to return to contact. Even with this modification to the classic protocol, there is the possibility of reactivating the device weeks later, when normally there is a mild recurrence (1-2 mm) of class II. So since it does not affect this aspect, our goal is to obtain molar intercuspation as quickly as possible which would be much slower with overjet brought to 0 mm. Therefore, after approximately 1 week the patient presents an occlusion of numerous teeth in contact with maximum intercuspation. This phase of muscular and joint adaptation is clinically visible in the photos of the patients as soon as the device is cemented in the mouth and subsequently at the check-up after 7 days: initially the muscles appear "forced" to maintain the protruded position (an aspect common to many functional devices including the Frankel), while the muscular posture improves significantly already after a week when intercuspation has been obtained (
Figure 4 A,B,C).
This may lead one to think that obtaining dental intercuspation in a very short time is beneficial to neuro-muscular balance. We know that the possibility of correct contact of the posterior teeth during the swallowing phase which occurs after approximately 7 days is an important aspect for receptor stimulation. When this does not happen immediately, the jaw blocked in a protruded position continues to continuously activate the mandibular retrusor muscles during the swallowing act, placing greater stress on the anchoring unit. In the "adaptive" period just mentioned, the retrusive muscular forces are very strong and are limited by the presence of a mechanical block represented by the telescopic tubes of the Herbst device: the length of these tubes influences the action on the muscles and therefore modifies their state of contractile activation. In this phase, therefore, the dental anchoring unit is highly stressed, considering the average load expressed in kilograms and perpetrated during 24 hours. If the dental occlusion obtainable after the adaptive phase is deficient, due to various problems, the side effects and the therapeutic result will inevitably be penalized. Therefore, to reduce stress on the anchoring unit, a first aspect to be carefully evaluated is the coordination of the arches obtained through MBA in the preparatory phase. If the arches are not well coordinated with each other, during the mandibular advancement phase using the Herbst apparatus, it will not be possible to obtain stabilization in the desired position since the dental interference in the occlusion will cause a distalizing recurrence on the mandible. It has already been underlined that in many articles that deal with this device, it is possible to see photos of cases in which the equipment is mounted with the arches not coordinated with each other, or the multi-brackets phase represents a second moment of the therapy when the device Hesbst has already been removed, or no such therapy is performed at the end of the treatment.
3.2. Clinical Observations After Using the Simplified Design
In relation to what has been said about the need for rapid occlusal stabilization in order not to stress the dental anchoring elements both to avoid excessive loads and to avoid unwanted movements (for example lower dental protrusion), the use of occlusal covering bands. This typology occupies the occlusal table: since the occlusion expected after application of the device is dental class I, the bands of the upper and lower molars are at mutual contact. This determines a significant occlusal rise which is at least 2 mm considering the metal thickness. Therefore in the stabilization phase the first permanent molars are the only teeth to occlude each other: the rest of the teeth in the arch are not in mutual contact. It will be necessary to wait for spontaneous eruption of the teeth not supported by arches for the occlusal load to be distributed. This can take months and may not necessarily be completed. The elements that come into contact most easily are the seventh ones which in no way can remain united with strings during this phase. In fact, if the space of the arm welded to the band of the sixth from the vestibular surfaces of the premolars allows it, it is possible to solidify the teeth with a rectangular wire arch to avoid unwanted movements. However, at the level of the sevenths the arch cannot be used due to the presence of welding on the bands of the sixths. However, upon removal of the Herbst after 6-9 months according to traditional times recommended in the literature, it must be considered that the sixths will not be in occlusion since other dental elements will be extruded. This effect can be dangerous both due to uncontrolled extrusions, not only on the vertical plane but other movements on other spatial planes must be considered. The elements that are free to move because they are not stabilized will be able to vestibularize or lingualize as well as extrude to a different extent. In fact, upon removal of the device, we usually witness the spontaneous and unwanted eruption of the sevenths which cannot be retained during the 6-8 months through the use of rectangular wire sectionals as happens for the anterior sector. The precontact of these teeth favors occlusal interference and posterior sliding of the mandible, as the stomatognathic neuromuscular system seeks stabilization. A further aspect to consider is the occlusal flat design of this type of band. This design prevents intercuspation between the molars when they are in contact, a factor which is indispensable for occlusal stabilization. In fact, the narrow occlusal indentation represents the effective stabilization of the result of mandibular anterior repositioning using the Herbst device. Therefore it is reasonable to think that in the initial stages the anchoring teeth are still predominantly affected by the forces of mandibular retrusion. In fact, it is clinically known that, during the temporary removal of the telescopic tubes (for example due to leakage from excessive opening of the mouth as in the historical models of this device, or due to unscrewing of the lateral fixing screw) there is a spontaneous retrusion of the mandible: this confirms how in the first months of therapy the expression of retrusive muscle forces is still very strong. To overcome this drawback, the device with occlusal coverage bands was used with occlusal elimination of the interfering metal parts until dental contact was achieved while maintaining an extended metal coverage. This type of Herbst device does not include bands on the premolars. Instead, it has an arm welded onto the band of the lower molar which extends horizontally up to the first lower premolar: it is spaced from the mucosa by approximately 1 mm to reduce the bulk in the oral fornix and is positioned approximately at the height of the gingival margin of the first premolar. This allows the presence of the equipment on the upper arch limited to the sixths, while the rest of the arch is not obstructed. The intention is certainly to promote home hygiene and reduce the incidence of tooth decay on the anchoring teeth. These variations reduce the bulk at the level of the premolars since the metal structure that cages these teeth is eliminated. We have found that in the upper arch the retrusive and occlusal muscular forces determine a stress only on the sixths which are forced to bear the load. This can cause a selective intrusion of these dental elements in the upper arch with consequent occlusal variation and decubitus of the trans-palatal Goshgarian bar (
Figure 5).
This inconvenience may require demolition of the equipment to be resolved, since the units are only welded, with consequent loss of chair time and disturbance of the therapeutic position reached at that moment. We have overcome this inconvenience by applying a greater distance of the bar from the palatal mucosa during the manufacturing phase but always maintaining monitoring of the situation during clinical checks.
In the lower arch the molars alone suffer the mesializing forces, while in the original equipment there are as many as 6 dental elements per arch instead of two that bear the muscular forces. Furthermore, the muscular forces acting on the only two anchoring teeth can cause negative effects including tooth displacement with more accentuated intrusion and mesialization/distalization compared to the previous model and possible rhizalysis due to inappropriate control of the acting forces.
The spatial instability of the metal elements can also occur on the lower arm welded to the band of the lower molar: in fact the application of the muscular force which has the anterior joint as its fulcrum determines the creation of a lever arm which discharges its force on the lower molars: slight displacements of the terminal part of the arm can be observed which can create a direct mucosal decubitus or due to secondary vestibularization of the first premolar which cannot be controlled by wire sectionals on the MBA (
Figure 6 A,B).
The reduced space between the arm and the dental surfaces of the premolars prevents the rectangular wire sectional used in the anterior sector from being extended from canine to canine to reduce the displacement of the dental elements. Therefore the lower premolars remain without any movement control. The premolars may vestibularize and come into contact with the appliance. We therefore recommend increasing the space between the welded arm and the teeth in order to control this aspect. The patient will be able to monitor the status of the device on a daily basis during daily home oral hygiene procedures. In fact, the area can be cleaned with threads specific interdentals and the correct passage of it on the area of interest is a guarantee of stability of the spaces (
Figure 7).
The treatment was concluded with good results in terms of intercuspation, muscular and joint wellbeing status assessed by a clinical chart including muscle palpation, evaluation of mouth opening and closing dynamics (
Figure 8,
Figure 9 and
Figure 10).
4. Conclusions
As regards the purpose of this article, we try to underline how occlusal stabilization is of fundamental importance for the acquisition of a new neuromuscular engram which limits the deleterious effects due precisely to the action of the muscles on the anchoring units.
We believe that the Herbst device remains an excellent aid for the correction of class II mandibular retrusion and that studies should be conducted with the optimization of standardized protocols to obtain faster and more effective results, but above all to be able to compare scientific data in a more selective way. We are conducting not only clinical but diagnostic investigations to clarify these aspects. These small technical measures could also have an advantage in reducing stress on the anchoring units.
Author Contributions
All authors made a significant contribution to the work reported, whether that is in the conception, study design, execution, acquisition of data, analysis and interpretation, or in all these areas; took part in drafting, revising or critically reviewing the article; gave final approval of the version to be published; have agreed on the journal to which the article has been submitted.
Funding
This research received no external funding.
Institutional Review Board Statement
Ethical approval (number 23, 8 November 2018) was obtained by Independent Ethics Committee of Chieti hospital. The study protocol was drawn following the European Union Good Practice Rules and the Helsinki Declaration.
Informed Consent Statement
Written informed consent has been obtained from the patients or the legally authorised representative to publish this paper.
References
- Herbst, E. Dreissigjahrige Erfahrungen mit dem retentionsscharnier. Zahnarztl. Rundsch. 1934, 43, 1515–1524. [Google Scholar]
- Panchers, H. The effects, limitations, and long-term dentofacial adaptations to treatment with the Herbst appliance. Semin. Orthod. 1997, 3, 232–43. [Google Scholar] [CrossRef] [PubMed]
- Panchers, H. Treatment of class II malocclusion by jumping the bite with the Herbst appliance. A cephalometric investigation. Am. J. Orthod. 1979, 76, 423–442. [Google Scholar] [CrossRef]
- Panchers, H. Activity of the temporal and masseter muscles in class II, division 1 malocclusions. Am. J. Orthod. 1980, 77, 679–688. [Google Scholar] [CrossRef] [PubMed]
- Panchers, H. Vertical dentofacial changes during Herbst appliance treatment. Swed. Dent. J. Suppl. 1982, 15, 189–196. [Google Scholar]
- Güner, D.; Öztürk, Y.; Sayman, H.B. Evaluation of the effects of functional orthopaedic treatment on temporomandibular joint with single- proton emission computerized tomography. Eur. J. Orthod. 2003, 25, 9–12. [Google Scholar] [CrossRef] [PubMed]
- Le Cornu, M.; Cevidanes, L.H.S.; Zhu, H.; Wu, C.; Larson, B.; Nguyenf, T. Three-dimensional treatment outcomes in Class II patients treated with the Herbst appliance: A pilot study. Am. J. Orthod. Dentofac. Orthop. 2013, 144, 818–30. [Google Scholar] [CrossRef] [PubMed]
- Serbesis-Tsarudis, C.; Pancherz, H. ‘’Effective’’ TMJ and chin position changes in Class II treatment. Angle Orthod. 2008, 78, 813–8. [Google Scholar] [CrossRef] [PubMed]
- Vigorito, F.d.A.; Dominguez, G.C.; Aidar, L.A.d.A. Dental and skeletal changes in patients with mandibular retrognathism following treatment with Herbst and pre-adjusted fixed appliance. Dent. Press. J. Orthod. 2014, 19, 46–54. [Google Scholar] [CrossRef] [PubMed]
- Wadhawan, N.; Kumar, S.; Kharbanda, O.P.; Duggal, R.; Sharma, R. Temporomandibular joint adaptations following two-phase therapy: an MRI study. Orthod. Craniofac Res. 2008, 11, 235–50. [Google Scholar] [CrossRef] [PubMed]
- Schwartz, J.P.; Raveli, T.B.; Almeida, K.C.; Schwartz-Filho, H.O.; Raveli, D.B. Cone beam computed tomography study of apical root resorption induced by Herbst appliance. J. Appl. Oral. Sci. 2015, 23, 479–85. [Google Scholar] [CrossRef]
- Jakobsone, G.; Latkauskiene, D.; McNamara, J.A., Jr. Mechanisms of Class II correction induced by the crown Herbst appliance as a single-phase Class II therapy: 1 year follow-up. Prog. Orthod. 2013, 14, 27. [Google Scholar] [CrossRef] [PubMed]
- Kinzinger, G.S.M.; Hourfar, J.; Kober, C.; Lisson, J.A. Mandibular fossa morphology during therapy with a fixed functional orthodontic appliance. J. Orofac. Orthop. 2018, 79, 116–32. [Google Scholar] [CrossRef] [PubMed]
- Katsavrias, E.G. The effect of mandibular protrusive (activa- tor) appliances on articular eminence morphology. Angle Orthod. 2003, 73, 647–53. [Google Scholar] [PubMed]
- Franco, A.; Yamashita, H.; Lederman, H.; Cevidanes, L.H.S.; Proffit, W.; Vigorito, J.W. Fränkel appliance therapy and the temporomandibular disc: A prospective magnetic resonance imaging study. Am. J. Orthod. Dentofac. Orthop. 2002, 121, 447–57. [Google Scholar] [CrossRef] [PubMed]
- Nindra, J.; Sidhu, M.S.; Kochhar, A.S.; Dabas, A.; Valletta, R.; Rongo, R.; Spagnuolo, G. Three-Dimensional Evaluation of Condyle-Glenoid Fossa Complex Following Treatment with Herbst Appliance. J. Clin. Med. 2021, 10, 4730. [Google Scholar] [CrossRef] [PubMed]
- Kinzinger, G.; Hourfar, J.; Kober, C.; Lissan, J.A. Mandibular fossa morphology during therapy with a fixed functional orthodontic appliance: A magnetic resonance imaging study. J. Orofac. Orthop. 2018, 79, 116–132. [Google Scholar] [CrossRef] [PubMed]
- Wadhawan, N.; Kumar, S.; Kharbanda, O.P.; Duggal, R.; Sharma, R. Temporomandibular joint adaptations following two-phase therapy: an MRI study. Orthod. Craniofac Res. 2008, 11, 235–50. [Google Scholar] [CrossRef]
- Kinzinger, G.; Kober, C.; Diedrich, P. Topography and Morphology of the Mandibular Condyle during Fixed Functional Orthopedic Treatment -a Magnetic Resonance Imaging Study. J. Orofac. Orthop. 2007, 68, 124–47. [Google Scholar] [CrossRef]
- Pancherz, H.; Fischer, S. Amount and Direction of Temporomandibular Joint Growth Changes in Herbst Treatment: A Cephalometric Long-Term Investigation. Angle Orthod. 2003, 73, 493–501. [Google Scholar] [PubMed]
- Okano, K.S.; Cevidanes, L.H.S.; Cheib, P.L.; Ruellas, A.C.d.O.; Yatabe, M.; Nguyen, T.; Franchi, L.; McNamara, J.A.; Souki, B.Q. Three-dimensional assessment of the middle cranial fossa and central skull base following Herbst appliance treatment. Angle Orthod. 2018, 88, 757–764. [Google Scholar] [CrossRef] [PubMed]
- Lawton, H.M.; Battagel, J.M.; Kotecha, B. A comparison of the Twin Block and Herbst mandibular advancement splints in the treatment of patients with obstructive sleep apnoea: a prospective study. Eur. J. Orthod. 2005, 27, 82–90. [Google Scholar] [CrossRef] [PubMed]
- Shaikh, S.Y.; Malik, A.M.; Khalid, O.; Mahnoor, M. Comparison of upper pharyngeal airway space in Class II and Class III malocclu- sion cases. Pak. Orthod. J. 2014, 6, 2–6. [Google Scholar]
- Iwasaki, T.; Sato, H.; Suga, H.; Takemoto, Y.; Inada, E.; Saitoh, I.; Kakuno, K.; Kanomi, R.; Yamasaki, Y. Influence of pharyngeal airway respiration pressure on Class II mandibular retrusion in children: a computational fluid dynamics study of inspiration and expiration. Ortho- Dontics Craniofacial Res. 2017, 20, 95–101. [Google Scholar] [CrossRef] [PubMed]
- Gul Amuk, N.; Kurt, G.; Baysal, A.; Turker, G. Changes in pharyngeal airway dimensions following incremental and maximum bite advancement during Herbst-rapid palatal expander appliance therapy in late adolescent and young adult patients: a randomized non-controlled prospective clinical study. Eur. J. Orthod. 2019, 41, 322–330. [Google Scholar] [CrossRef] [PubMed]
|
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2025 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (http://creativecommons.org/licenses/by/4.0/).