Submitted:
05 September 2025
Posted:
08 September 2025
You are already at the latest version
Abstract
Keywords:
1. Introduction
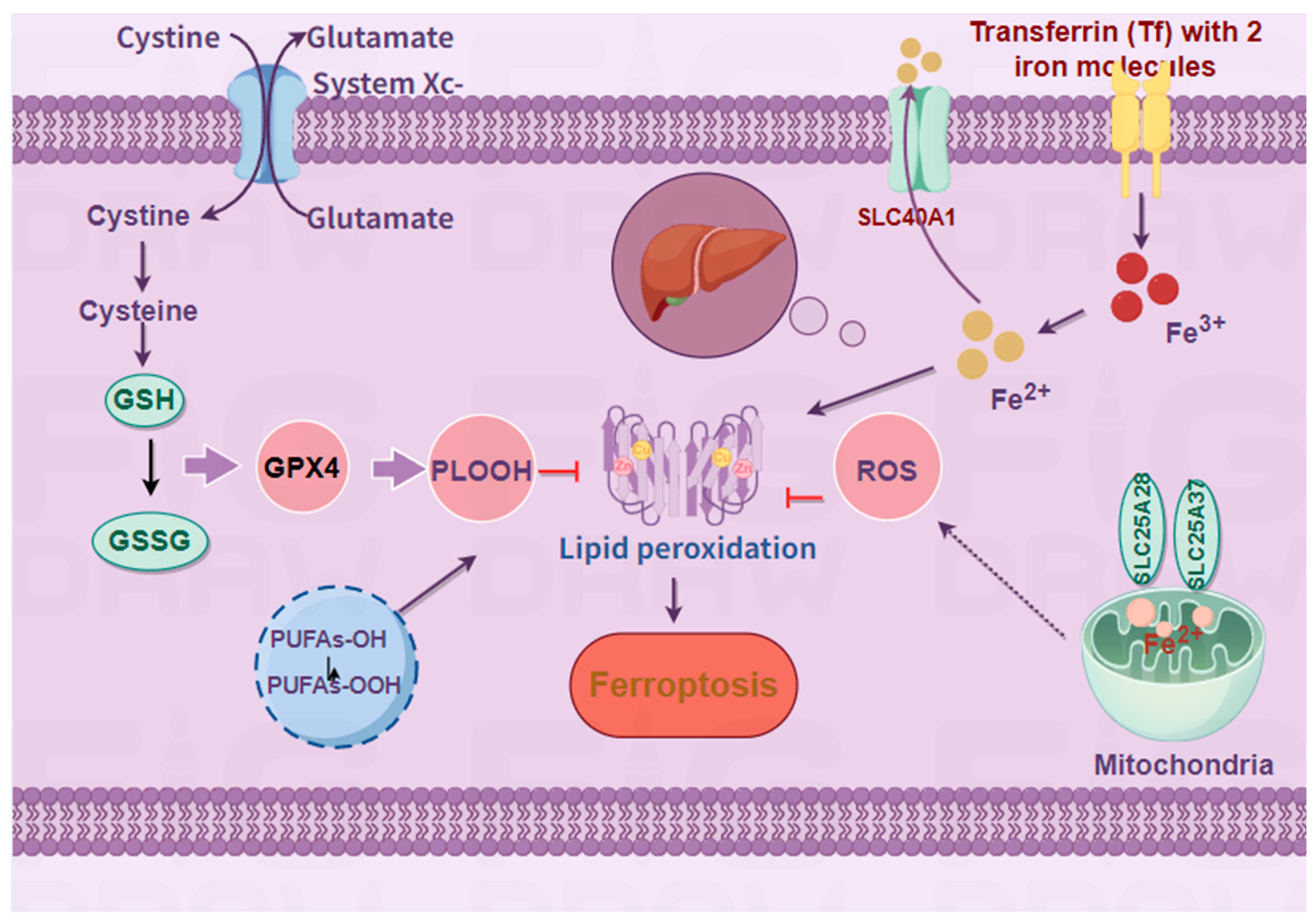
2. Overview and Important Components of Ferroptosis
2.1. Overview
2.2. Important Components and Pathways of Ferroptosis
3. Metabolism of Ferroptosis
3.1. Role of Amino Acid Metabolism in Ferroptosis
3.2. Role of Iron Metabolism in Ferroptosis
3.3. Lipid Metabolism - An Important Link in Ferroptosis
4. Ferroptosis and Signaling Pathways of the Immune System
4.1. The JAK/STAT Signaling Pathway
4.1.1. JAK/STAT Signaling Pathway and Immune Response
4.1.2. JAK/STAT Signaling Pathway and Ferroptosis
4.2. NF-κB Signaling Pathway
4.2.1. NF-κB Signaling Pathway and Immune Response
4.2.2. NF-κB Signaling Pathway and Ferroptosis
5. Ferroptosis in Immune Diseases
5.1. Rheumatoid Arthritis (RA)
5.2. Systemic Lupus Erythematosus (SLE)
5.3. Psoriasis (PsO)
5.4. Inflammatory Bowel Disease (IBD)
5.5. Multiple Sclerosis (MS)
5.6. Type I Diabetes
6. Conclusion
Author Contributions
Funding
Data Availability
Conflicts of Interest
References
- Y. Song, J. Li, and Y. Wu, “Evolving understanding of autoimmune mechanisms and new therapeutic strategies of autoimmune disorders,” (in eng), Signal Transduct Target Ther, vol. 9, no. 1, p. 263, Oct 4 2024. [CrossRef]
- C. Chen et al., “Mendelian randomization as a tool to gain insights into the mosaic causes of autoimmune diseases,” (in eng), Autoimmun Rev, vol. 21, no. 12, p. 103210, Dec 2022. [CrossRef]
- L. Wang, F. S. Wang, and M. E. Gershwin, “Human autoimmune diseases: a comprehensive update,” (in eng), J Intern Med, vol. 278, no. 4, pp. 369-95, Oct 2015. [CrossRef]
- S. T. Ngo, F. J. Steyn, and P. A. McCombe, “Gender differences in autoimmune disease,” (in eng), Front Neuroendocrinol, vol. 35, no. 3, pp. 347-69, Aug 2014. [CrossRef]
- F. W. Miller, “The increasing prevalence of autoimmunity and autoimmune diseases: an urgent call to action for improved understanding, diagnosis, treatment, and prevention,” (in eng), Curr Opin Immunol, vol. 80, p. 102266, Feb 2023. [CrossRef]
- D. M. Maahs, N. A. West, J. M. Lawrence, and E. J. Mayer-Davis, “Epidemiology of type 1 diabetes,” (in eng), Endocrinol Metab Clin North Am, vol. 39, no. 3, pp. 481-97, Sep 2010. [CrossRef]
- S. J. Dixon et al., “Ferroptosis: an iron-dependent form of nonapoptotic cell death,” (in eng), Cell, vol. 149, no. 5, pp. 1060-72, May 25 2012. [CrossRef]
- X. Jiang, B. R. Stockwell, and M. Conrad, “Ferroptosis: mechanisms, biology and role in disease,” (in eng), Nat Rev Mol Cell Biol, vol. 22, no. 4, pp. 266-282, Apr 2021. [CrossRef]
- Y. Xie, R. Kang, D. J. Klionsky, and D. Tang, “GPX4 in cell death, autophagy, and disease,” (in eng), Autophagy, vol. 19, no. 10, pp. 2621-2638, Oct 2023. [CrossRef]
- C. Xu et al., “The glutathione peroxidase Gpx4 prevents lipid peroxidation and ferroptosis to sustain Treg cell activation and suppression of antitumor immunity,” (in eng), Cell Rep, vol. 35, no. 11, p. 109235, Jun 15 2021. [CrossRef]
- P. Li et al., “Glutathione peroxidase 4-regulated neutrophil ferroptosis induces systemic autoimmunity,” (in eng), Nat Immunol, vol. 22, no. 9, pp. 1107-1117, Sep 2021. [CrossRef]
- H. Eagle, “Nutrition needs of mammalian cells in tissue culture,” (in eng), Science, vol. 122, no. 3168, pp. 501-14, Sep 16 1955. [CrossRef]
- H. Eagle, K. A. Piez, and V. I. Oyama, “The biosynthesis of cystine in human cell cultures,” (in eng), J Biol Chem, vol. 236, pp. 1425-8, May 1961.
- A. Meister, “Glutathione metabolism,” (in eng), Methods Enzymol, vol. 251, pp. 3-7, 1995. [CrossRef]
- L. A. Timmerman et al., “Glutamine sensitivity analysis identifies the xCT antiporter as a common triple-negative breast tumor therapeutic target,” (in eng), Cancer Cell, vol. 24, no. 4, pp. 450-65, Oct 14 2013. [CrossRef]
- G. Xing et al., “PPARα alleviates iron overload-induced ferroptosis in mouse liver,” (in eng), EMBO Rep, vol. 23, no. 8, p. e52280, Aug 3 2022. [CrossRef]
- N. Geng et al., “Knockdown of ferroportin accelerates erastin-induced ferroptosis in neuroblastoma cells,” (in eng), Eur Rev Med Pharmacol Sci, vol. 22, no. 12, pp. 3826-3836, Jun 2018. [CrossRef]
- J. N. Moloney and T. G. Cotter, “ROS signalling in the biology of cancer,” (in eng), Semin Cell Dev Biol, vol. 80, pp. 50-64, Aug 2018. [CrossRef]
- F. Ursini, M. Maiorino, M. Valente, L. Ferri, and C. Gregolin, “Purification from pig liver of a protein which protects liposomes and biomembranes from peroxidative degradation and exhibits glutathione peroxidase activity on phosphatidylcholine hydroperoxides,” (in eng), Biochim Biophys Acta, vol. 710, no. 2, pp. 197-211, Feb 15 1982. [CrossRef]
- R. Brigelius-Flohé and M. Maiorino, “Glutathione peroxidases,” (in eng), Biochim Biophys Acta, vol. 1830, no. 5, pp. 3289-303, May 2013. [CrossRef]
- X. Hu, J. Li, M. Fu, X. Zhao, and W. Wang, “The JAK/STAT signaling pathway: from bench to clinic,” (in eng), Signal Transduct Target Ther, vol. 6, no. 1, p. 402, Nov 26 2021. [CrossRef]
- Q. Hu et al., “JAK/STAT pathway: Extracellular signals, diseases, immunity, and therapeutic regimens,” (in eng), Front Bioeng Biotechnol, vol. 11, p. 1110765, 2023. [CrossRef]
- H. J. Ko and Y. J. Kim, “Signal transducer and activator of transcription proteins: regulators of myeloid-derived suppressor cell-mediated immunosuppression in cancer,” (in eng), Arch Pharm Res, vol. 39, no. 11, pp. 1597-1608, Nov 2016. [CrossRef]
- P. Jayaraman et al., “Tumor-expressed inducible nitric oxide synthase controls induction of functional myeloid-derived suppressor cells through modulation of vascular endothelial growth factor release,” (in eng), J Immunol, vol. 188, no. 11, pp. 5365-76, Jun 1 2012. [CrossRef]
- K. Movahedi et al., “Identification of discrete tumor-induced myeloid-derived suppressor cell subpopulations with distinct T cell-suppressive activity,” (in eng), Blood, vol. 111, no. 8, pp. 4233-44, Apr 15 2008. [CrossRef]
- B. Becknell and M. A. Caligiuri, “Interleukin-2, interleukin-15, and their roles in human natural killer cells,” (in eng), Adv Immunol, vol. 86, pp. 209-39, 2005. [CrossRef]
- A. Bernasconi et al., “Characterization of immunodeficiency in a patient with growth hormone insensitivity secondary to a novel STAT5b gene mutation,” (in eng), Pediatrics, vol. 118, no. 5, pp. e1584-92, Nov 2006. [CrossRef]
- L. Zhou, M. M. Chong, and D. R. Littman, “Plasticity of CD4+ T cell lineage differentiation,” (in eng), Immunity, vol. 30, no. 5, pp. 646-55, May 2009. [CrossRef]
- M. A. Burchill, J. Yang, C. Vogtenhuber, B. R. Blazar, and M. A. Farrar, “IL-2 receptor beta-dependent STAT5 activation is required for the development of Foxp3+ regulatory T cells,” (in eng), J Immunol, vol. 178, no. 1, pp. 280-90, Jan 1 2007. [CrossRef]
- D. M. Woods et al., “Decreased Suppression and Increased Phosphorylated STAT3 in Regulatory T Cells are Associated with Benefit from Adjuvant PD-1 Blockade in Resected Metastatic Melanoma,” (in eng), Clin Cancer Res, vol. 24, no. 24, pp. 6236-6247, Dec 15 2018. [CrossRef]
- D. Reddy, R. Kumavath, P. Ghosh, and D. Barh, “Lanatoside C Induces G2/M Cell Cycle Arrest and Suppresses Cancer Cell Growth by Attenuating MAPK, Wnt, JAK-STAT, and PI3K/AKT/mTOR Signaling Pathways,” (in eng), Biomolecules, vol. 9, no. 12, Nov 27 2019. [CrossRef]
- P. Xin et al., “The role of JAK/STAT signaling pathway and its inhibitors in diseases,” (in eng), Int Immunopharmacol, vol. 80, p. 106210, Mar 2020. [CrossRef]
- C. Nunes, L. Almeida, R. M. Barbosa, and J. Laranjinha, “Luteolin suppresses the JAK/STAT pathway in a cellular model of intestinal inflammation,” (in eng), Food Funct, vol. 8, no. 1, pp. 387-396, Jan 25 2017. [CrossRef]
- A. Mukherjee et al., “Exposure-Response Characterization of Tofacitinib Efficacy in Moderate to Severe Ulcerative Colitis: Results From Phase II and Phase III Induction and Maintenance Studies,” (in eng), Clin Pharmacol Ther, vol. 112, no. 1, pp. 90-100, Jul 2022. [CrossRef]
- Deodhar et al., “Tofacitinib for the treatment of ankylosing spondylitis: a phase III, randomised, double-blind, placebo-controlled study,” (in eng), Ann Rheum Dis, vol. 80, no. 8, pp. 1004-1013, Aug 2021. [CrossRef]
- S. A. Hasni et al., “Phase 1 double-blind randomized safety trial of the Janus kinase inhibitor tofacitinib in systemic lupus erythematosus,” (in eng), Nat Commun, vol. 12, no. 1, p. 3391, Jun 7 2021. [CrossRef]
- P. R. Little, V. L. King, K. R. Davis, S. B. Cosgrove, and M. R. Stegemann, “A blinded, randomized clinical trial comparing the efficacy and safety of oclacitinib and ciclosporin for the control of atopic dermatitis in client-owned dogs,” (in eng), Vet Dermatol, vol. 26, no. 1, pp. 23-30, e7-8, Feb 2015. [CrossRef]
- M. Abe et al., “Tofacitinib for the treatment of moderate to severe chronic plaque psoriasis in Japanese patients: Subgroup analyses from a randomized, placebo-controlled phase 3 trial,” (in eng), J Dermatol, vol. 44, no. 11, pp. 1228-1237, Nov 2017. [CrossRef]
- R. Kong, N. Wang, W. Han, W. Bao, and J. Lu, “IFNγ-mediated repression of system xc(-) drives vulnerability to induced ferroptosis in hepatocellular carcinoma cells,” (in eng), J Leukoc Biol, vol. 110, no. 2, pp. 301-314, Aug 2021. [CrossRef]
- W. Wang et al., “CD8(+) T cells regulate tumour ferroptosis during cancer immunotherapy,” (in eng), Nature, vol. 569, no. 7755, pp. 270-274, May 2019. [CrossRef]
- X. Yu, D. Zhu, B. Luo, W. Kou, Y. Cheng, and Y. Zhu, “IFNγ enhances ferroptosis by increasing JAK-STAT pathway activation to suppress SLCA711 expression in adrenocortical carcinoma,” (in eng), Oncol Rep, vol. 47, no. 5, May 2022. [CrossRef]
- K. V. Kowdley, E. M. Gochanour, V. Sundaram, R. A. Shah, and P. Handa, “Hepcidin Signaling in Health and Disease: Ironing Out the Details,” (in eng), Hepatol Commun, vol. 5, no. 5, pp. 723-735, May 2021. [CrossRef]
- F. Ren et al., “The Effects of Dandelion Polysaccharides on Iron Metabolism by Regulating Hepcidin via JAK/STAT Signaling Pathway,” (in eng), Oxid Med Cell Longev, vol. 2021, p. 7184760, 2021. [CrossRef]
- L. Yang et al., “Auranofin mitigates systemic iron overload and induces ferroptosis via distinct mechanisms,” (in eng), Signal Transduct Target Ther, vol. 5, no. 1, p. 138, Jul 31 2020. [CrossRef]
- S. C. Sun, “The non-canonical NF-κB pathway in immunity and inflammation,” (in eng), Nat Rev Immunol, vol. 17, no. 9, pp. 545-558, Sep 2017. [CrossRef]
- N. Jounai, K. Kobiyama, F. Takeshita, and K. J. Ishii, “Recognition of damage-associated molecular patterns related to nucleic acids during inflammation and vaccination,” (in eng), Front Cell Infect Microbiol, vol. 2, p. 168, 2012. [CrossRef]
- L. E. Muñoz, K. Lauber, M. Schiller, A. A. Manfredi, and M. Herrmann, “The role of defective clearance of apoptotic cells in systemic autoimmunity,” (in eng), Nat Rev Rheumatol, vol. 6, no. 5, pp. 280-9, May 2010. [CrossRef]
- A. N. Suthers and S. Sarantopoulos, “TLR7/TLR9- and B Cell Receptor-Signaling Crosstalk: Promotion of Potentially Dangerous B Cells,” (in eng), Front Immunol, vol. 8, p. 775, 2017. [CrossRef]
- M. Irla et al., “Autoantigen-specific interactions with CD4+ thymocytes control mature medullary thymic epithelial cell cellularity,” (in eng), Immunity, vol. 29, no. 3, pp. 451-63, Sep 19 2008. [CrossRef]
- M. S. Hayden and S. Ghosh, “NF-κB in immunobiology,” (in eng), Cell Res, vol. 21, no. 2, pp. 223-44, Feb 2011. [CrossRef]
- G. Xiao, E. W. Harhaj, and S. C. Sun, “NF-kappaB-inducing kinase regulates the processing of NF-kappaB2 p100,” (in eng), Mol Cell, vol. 7, no. 2, pp. 401-9, Feb 2001. [CrossRef]
- S. C. Sun, “The noncanonical NF-κB pathway,” (in eng), Immunol Rev, vol. 246, no. 1, pp. 125-40, Mar 2012. [CrossRef]
- R. M. Steinman and H. Hemmi, “Dendritic cells: translating innate to adaptive immunity,” (in eng), Curr Top Microbiol Immunol, vol. 311, pp. 17-58, 2006. [CrossRef]
- K. L. Willmann et al., “Biallelic loss-of-function mutation in NIK causes a primary immunodeficiency with multifaceted aberrant lymphoid immunity,” (in eng), Nat Commun, vol. 5, p. 5360, Nov 19 2014. [CrossRef]
- H. D. Brightbill et al., “NF-κB inducing kinase is a therapeutic target for systemic lupus erythematosus,” (in eng), Nat Commun, vol. 9, no. 1, p. 179, Jan 12 2018. [CrossRef]
- A. R. Noort, P. P. Tak, and S. W. Tas, “Non-canonical NF-κB signaling in rheumatoid arthritis: Dr Jekyll and Mr Hyde?,” (in eng), Arthritis Res Ther, vol. 17, no. 1, p. 15, Jan 28 2015. [CrossRef]
- P. Kucharzewska et al., “NIK-IKK complex interaction controls NF-κB-dependent inflammatory activation of endothelium in response to LTβR ligation,” (in eng), J Cell Sci, vol. 132, no. 7, Apr 3 2019. [CrossRef]
- W. Tan et al., “MiR-93-5p promotes granulosa cell apoptosis and ferroptosis by the NF-kB signaling pathway in polycystic ovary syndrome,” (in eng), Front Immunol, vol. 13, p. 967151, 2022. [CrossRef]
- N. Yan, Z. Xu, C. Qu, and J. Zhang, “Dimethyl fumarate improves cognitive deficits in chronic cerebral hypoperfusion rats by alleviating inflammation, oxidative stress, and ferroptosis via NRF2/ARE/NF-κB signal pathway,” (in eng), Int Immunopharmacol, vol. 98, p. 107844, Sep 2021. [CrossRef]
- Y. Liang et al., “HSPB1 facilitates chemoresistance through inhibiting ferroptotic cancer cell death and regulating NF-κB signaling pathway in breast cancer,” (in eng), Cell Death Dis, vol. 14, no. 7, p. 434, Jul 15 2023. [CrossRef]
- X. Zhong et al., “Hepatic NF-κB-Inducing Kinase and Inhibitor of NF-κB Kinase Subunit α Promote Liver Oxidative Stress, Ferroptosis, and Liver Injury,” (in eng), Hepatol Commun, vol. 5, no. 10, pp. 1704-1720, Oct 2021. [CrossRef]
- J. J. Cush, “Rheumatoid Arthritis: Early Diagnosis and Treatment,” (in eng), Rheum Dis Clin North Am, vol. 48, no. 2, pp. 537-547, May 2022. [CrossRef]
- J. S. Smolen, D. Aletaha, and I. B. McInnes, “Rheumatoid arthritis,” (in eng), Lancet, vol. 388, no. 10055, pp. 2023-2038, Oct 22 2016. [CrossRef]
- W. Grassi, R. De Angelis, G. Lamanna, and C. Cervini, “The clinical features of rheumatoid arthritis,” (in eng), Eur J Radiol, vol. 27 Suppl 1, pp. S18-24, May 1998. [CrossRef]
- H. L. Wright, R. J. Moots, and S. W. Edwards, “The multifactorial role of neutrophils in rheumatoid arthritis,” (in eng), Nat Rev Rheumatol, vol. 10, no. 10, pp. 593-601, Oct 2014. [CrossRef]
- G. S. Firestein, “Evolving concepts of rheumatoid arthritis,” (in eng), Nature, vol. 423, no. 6937, pp. 356-61, May 15 2003. [CrossRef]
- X. Li, A. He, Y. Liu, Y. Huang, and X. Zhang, “Bioinformatics identification of ferroptosis-related genes and therapeutic drugs in rheumatoid arthritis,” (in eng), Front Med (Lausanne), vol. 10, p. 1192153, 2023. [CrossRef]
- P. Fritz, J. G. Saal, C. Wicherek, A. König, W. Laschner, and H. Rautenstrauch, “Quantitative photometrical assessment of iron deposits in synovial membranes in different joint diseases,” (in eng), Rheumatol Int, vol. 15, no. 5, pp. 211-6, 1996. [CrossRef]
- W. Xiao et al., “Iron overload increases osteoclastogenesis and aggravates the effects of ovariectomy on bone mass,” (in eng), J Endocrinol, vol. 226, no. 3, pp. 121-34, Sep 2015. [CrossRef]
- N. Hakobyan, T. Kazarian, A. A. Jabbar, K. J. Jabbar, and L. A. Valentino, “Pathobiology of hemophilic synovitis I: overexpression of mdm2 oncogene,” (in eng), Blood, vol. 104, no. 7, pp. 2060-4, Oct 1 2004. [CrossRef]
- Y. Liu et al., “Heterogeneous ferroptosis susceptibility of macrophages caused by focal iron overload exacerbates rheumatoid arthritis,” (in eng), Redox Biol, vol. 69, p. 103008, Feb 2024. [CrossRef]
- S. Datta, S. Kundu, P. Ghosh, S. De, A. Ghosh, and M. Chatterjee, “Correlation of oxidant status with oxidative tissue damage in patients with rheumatoid arthritis,” (in eng), Clin Rheumatol, vol. 33, no. 11, pp. 1557-64, Nov 2014. [CrossRef]
- S. Z. Hassan, T. A. Gheita, S. A. Kenawy, A. T. Fahim, I. M. El-Sorougy, and M. S. Abdou, “Oxidative stress in systemic lupus erythematosus and rheumatoid arthritis patients: relationship to disease manifestations and activity,” (in eng), Int J Rheum Dis, vol. 14, no. 4, pp. 325-31, Oct 2011. [CrossRef]
- Y. Sun and H. S. Cheung, “p53, proto-oncogene and rheumatoid arthritis,” (in eng), Semin Arthritis Rheum, vol. 31, no. 5, pp. 299-310, Apr 2002. [CrossRef]
- S. Mateen, S. Moin, A. Q. Khan, A. Zafar, and N. Fatima, “Increased Reactive Oxygen Species Formation and Oxidative Stress in Rheumatoid Arthritis,” (in eng), PLoS One, vol. 11, no. 4, p. e0152925, 2016. [CrossRef]
- Z. Xie, H. Hou, D. Luo, R. An, Y. Zhao, and C. Qiu, “ROS-Dependent Lipid Peroxidation and Reliant Antioxidant Ferroptosis-Suppressor-Protein 1 in Rheumatoid Arthritis: a Covert Clue for Potential Therapy,” (in eng), Inflammation, vol. 44, no. 1, pp. 35-47, Feb 2021. [CrossRef]
- L. L. Ni et al., “The therapeutic effect of wasp venom (Vespa magnifica, Smith) and its effective part on rheumatoid arthritis fibroblast-like synoviocytes through modulating inflammation, redox homeostasis and ferroptosis,” (in eng), J Ethnopharmacol, vol. 317, p. 116700, Dec 5 2023. [CrossRef]
- J. Wu et al., “TNF antagonist sensitizes synovial fibroblasts to ferroptotic cell death in collagen-induced arthritis mouse models,” (in eng), Nat Commun, vol. 13, no. 1, p. 676, Feb 3 2022. [CrossRef]
- H. Ling et al., “Glycine increased ferroptosis via SAM-mediated GPX4 promoter methylation in rheumatoid arthritis,” (in eng), Rheumatology (Oxford), vol. 61, no. 11, pp. 4521-4534, Nov 2 2022. [CrossRef]
- Y. Zhang, G. Wang, T. Wang, W. Cao, L. Zhang, and X. Chen, “Nrf2-Keap1 pathway-mediated effects of resveratrol on oxidative stress and apoptosis in hydrogen peroxide-treated rheumatoid arthritis fibroblast-like synoviocytes,” (in eng), Ann N Y Acad Sci, vol. 1457, no. 1, pp. 166-178, Dec 2019. [CrossRef]
- Y. Wang et al., “Alleviated NCOA4-mediated ferritinophagy protected RA FLSs from ferroptosis in lipopolysaccharide-induced inflammation under hypoxia,” (in eng), Inflamm Res, vol. 73, no. 3, pp. 363-379, Mar 2024. [CrossRef]
- A. A. Justiz Vaillant, A. Goyal, and M. A. Varacallo, “Systemic Lupus Erythematosus,” in StatPearls. Treasure Island (FL) with ineligible companies. Disclosure: Amandeep Goyal declares no relevant financial relationships with ineligible companies. Disclosure: Matthew Varacallo declares no relevant financial relationships with ineligible companies.: StatPearls Publishing.
- Copyright © 2025, StatPearls Publishing LLC., 2025.
- L. Bowlus, “The role of iron in T cell development and autoimmunity,” (in eng), Autoimmun Rev, vol. 2, no. 2, pp. 73-8, Mar 2003. [CrossRef]
- Nathan, “Neutrophils and immunity: challenges and opportunities,” (in eng), Nat Rev Immunol, vol. 6, no. 3, pp. 173-82, Mar 2006. [CrossRef]
- G. S. Garcia-Romo et al., “Netting neutrophils are major inducers of type I IFN production in pediatric systemic lupus erythematosus,” (in eng), Sci Transl Med, vol. 3, no. 73, p. 73ra20, Mar 9 2011. [CrossRef]
- H. Zhang, L. Wang, and Y. Chu, “Reactive oxygen species: The signal regulator of B cell,” (in eng), Free Radic Biol Med, vol. 142, pp. 16-22, Oct 2019. [CrossRef]
- J. Muri, H. Thut, G. W. Bornkamm, and M. Kopf, “B1 and Marginal Zone B Cells but Not Follicular B2 Cells Require Gpx4 to Prevent Lipid Peroxidation and Ferroptosis,” (in eng), Cell Rep, vol. 29, no. 9, pp. 2731-2744.e4, Nov 26 2019. [CrossRef]
- M. Zhao et al., “Downregulation of BDH2 modulates iron homeostasis and promotes DNA demethylation in CD4(+) T cells of systemic lupus erythematosus,” (in eng), Clin Immunol, vol. 187, pp. 113-121, Feb 2018. [CrossRef]
- A. Perl, P. Gergely, Jr., and K. Banki, “Mitochondrial dysfunction in T cells of patients with systemic lupus erythematosus,” (in eng), Int Rev Immunol, vol. 23, no. 3-4, pp. 293-313, May-Aug 2004. [CrossRef]
- Y. Chang et al., “Erucic acid improves the progress of pregnancy complicated with systemic lupus erythematosus by inhibiting the effector function of CD8(+) T cells,” (in eng), MedComm (2020), vol. 4, no. 5, p. e382, Oct 2023. [CrossRef]
- Q. Feng et al., “Broadening horizons: the multifaceted functions of ferroptosis in kidney diseases,” (in eng), Int J Biol Sci, vol. 19, no. 12, pp. 3726-3743, 2023. [CrossRef]
- S. Marks et al., “Renal iron accumulation occurs in lupus nephritis and iron chelation delays the onset of albuminuria,” (in eng), Sci Rep, vol. 7, no. 1, p. 12821, Oct 9 2017. [CrossRef]
- A. A. Alli et al., “Kidney tubular epithelial cell ferroptosis links glomerular injury to tubulointerstitial pathology in lupus nephritis,” (in eng), Clin Immunol, vol. 248, p. 109213, Mar 2023. [CrossRef]
- K. Vats et al., “Keratinocyte death by ferroptosis initiates skin inflammation after UVB exposure,” (in eng), Redox Biol, vol. 47, p. 102143, Nov 2021. [CrossRef]
- A. W. Armstrong and C. Read, “Pathophysiology, Clinical Presentation, and Treatment of Psoriasis: A Review,” (in eng), Jama, vol. 323, no. 19, pp. 1945-1960, May 19 2020. [CrossRef]
- X. Liang et al., “Interplay Between Skin Microbiota Dysbiosis and the Host Immune System in Psoriasis: Potential Pathogenesis,” (in eng), Front Immunol, vol. 12, p. 764384, 2021. [CrossRef]
- G. Schett, P. Rahman, C. Ritchlin, I. B. McInnes, D. Elewaut, and J. U. Scher, “Psoriatic arthritis from a mechanistic perspective,” (in eng), Nat Rev Rheumatol, vol. 18, no. 6, pp. 311-325, Jun 2022. [CrossRef]
- P. E. Stuart et al., “Genome-wide Association Analysis of Psoriatic Arthritis and Cutaneous Psoriasis Reveals Differences in Their Genetic Architecture,” (in eng), Am J Hum Genet, vol. 97, no. 6, pp. 816-36, Dec 3 2015. [CrossRef]
- V. M. Bhole et al., “Differences in body mass index among individuals with PsA, psoriasis, RA and the general population,” (in eng), Rheumatology (Oxford), vol. 51, no. 3, pp. 552-6, Mar 2012. [CrossRef]
- U. Gazel, G. Ayan, D. Solmaz, S. Akar, and S. Z. Aydin, “The impact of smoking on prevalence of psoriasis and psoriatic arthritis,” (in eng), Rheumatology (Oxford), vol. 59, no. 10, pp. 2695-2710, Oct 1 2020. [CrossRef]
- N. R. Telfer, R. J. Chalmers, K. Whale, and G. Colman, “The role of streptococcal infection in the initiation of guttate psoriasis,” (in eng), Arch Dermatol, vol. 128, no. 1, pp. 39-42, Jan 1992.
- O. Kızılyel, N. Akdeniz, M. S. Metin, and F. Elmas Ö, “Investigation of oxidant and antioxidant levels in patients with psoriasis,” (in eng), Turk J Med Sci, vol. 49, no. 4, pp. 1085-1088, Aug 8 2019. [CrossRef]
- Benhadou, D. Mintoff, and V. Del Marmol, “Psoriasis: Keratinocytes or Immune Cells - Which Is the Trigger?,” (in eng), Dermatology, vol. 235, no. 2, pp. 91-100, 2019. [CrossRef]
- Y. Shou, L. Yang, Y. Yang, and J. Xu, “Inhibition of keratinocyte ferroptosis suppresses psoriatic inflammation,” (in eng), Cell Death Dis, vol. 12, no. 11, p. 1009, Oct 27 2021. [CrossRef]
- M. N. Wu et al., “Genetic analysis of potential biomarkers and therapeutic targets in ferroptosis from psoriasis,” (in eng), Front Immunol, vol. 13, p. 1104462, 2022. [CrossRef]
- Miotto et al., “Insight into the mechanism of ferroptosis inhibition by ferrostatin-1,” (in eng), Redox Biol, vol. 28, p. 101328, Jan 2020. [CrossRef]
- M. Fumery, S. Singh, P. S. Dulai, C. Gower-Rousseau, L. Peyrin-Biroulet, and W. J. Sandborn, “Natural History of Adult Ulcerative Colitis in Population-based Cohorts: A Systematic Review,” (in eng), Clin Gastroenterol Hepatol, vol. 16, no. 3, pp. 343-356.e3, Mar 2018. [CrossRef]
- A. Dignass et al., “Second European evidence-based consensus on the diagnosis and management of ulcerative colitis part 1: definitions and diagnosis,” (in eng), J Crohns Colitis, vol. 6, no. 10, pp. 965-90, Dec 2012. [CrossRef]
- M. C. Dubinsky et al., “Impact of Bowel Urgency on Quality of Life and Clinical Outcomes in Patients With Ulcerative Colitis,” (in eng), Crohns Colitis 360, vol. 4, no. 3, p. otac016, Jul 2022. [CrossRef]
- E. V. Loftus, Jr., “Clinical epidemiology of inflammatory bowel disease: Incidence, prevalence, and environmental influences,” (in eng), Gastroenterology, vol. 126, no. 6, pp. 1504-17, May 2004. [CrossRef]
- J. T. Chang, “Pathophysiology of Inflammatory Bowel Diseases,” (in eng), N Engl J Med, vol. 383, no. 27, pp. 2652-2664, Dec 31 2020. [CrossRef]
- C. A. Dinarello, “Interleukin-1beta and the autoinflammatory diseases,” (in eng), N Engl J Med, vol. 360, no. 23, pp. 2467-70, Jun 4 2009. [CrossRef]
- M. Gu et al., “IL-17 induces AKT-dependent IL-6/JAK2/STAT3 activation and tumor progression in hepatocellular carcinoma,” (in eng), Mol Cancer, vol. 10, p. 150, Dec 15 2011. [CrossRef]
- M. M. Fort et al., “IL-25 induces IL-4, IL-5, and IL-13 and Th2-associated pathologies in vivo,” (in eng), Immunity, vol. 15, no. 6, pp. 985-95, Dec 2001. [CrossRef]
- C. Günther, H. Neumann, M. F. Neurath, and C. Becker, “Apoptosis, necrosis and necroptosis: cell death regulation in the intestinal epithelium,” (in eng), Gut, vol. 62, no. 7, pp. 1062-71, Jul 2013. [CrossRef]
- T. Clavel and D. Haller, “Bacteria- and host-derived mechanisms to control intestinal epithelial cell homeostasis: implications for chronic inflammation,” (in eng), Inflamm Bowel Dis, vol. 13, no. 9, pp. 1153-64, Sep 2007. [CrossRef]
- T. Werner et al., “Depletion of luminal iron alters the gut microbiota and prevents Crohn’s disease-like ileitis,” (in eng), Gut, vol. 60, no. 3, pp. 325-33, Mar 2011. [CrossRef]
- Y. Kobayashi et al., “Association between dietary iron and zinc intake and development of ulcerative colitis: A case-control study in Japan,” (in eng), J Gastroenterol Hepatol, vol. 34, no. 10, pp. 1703-1710, Oct 2019. [CrossRef]
- J. C. Carrier, E. Aghdassi, K. Jeejeebhoy, and J. P. Allard, “Exacerbation of dextran sulfate sodium-induced colitis by dietary iron supplementation: role of NF-kappaB,” (in eng), Int J Colorectal Dis, vol. 21, no. 4, pp. 381-7, May 2006. [CrossRef]
- A. D. Millar, D. S. Rampton, and D. R. Blake, “Effects of iron and iron chelation in vitro on mucosal oxidant activity in ulcerative colitis,” (in eng), Aliment Pharmacol Ther, vol. 14, no. 9, pp. 1163-8, Sep 2000. [CrossRef]
- S. Wang, W. Liu, J. Wang, and X. Bai, “Curculigoside inhibits ferroptosis in ulcerative colitis through the induction of GPX4,” (in eng), Life Sci, vol. 259, p. 118356, Oct 15 2020. [CrossRef]
- S. Dong et al., “Furin inhibits epithelial cell injury and alleviates experimental colitis by activating the Nrf2-Gpx4 signaling pathway,” (in eng), Dig Liver Dis, vol. 53, no. 10, pp. 1276-1285, Oct 2021. [CrossRef]
- M. Minaiyan, E. Mostaghel, and P. Mahzouni, “Preventive Therapy of Experimental Colitis with Selected iron Chelators and Anti-oxidants,” (in eng), Int J Prev Med, vol. 3, no. Suppl 1, pp. S162-9, Mar 2012.
- R. Dobson and G. Giovannoni, “Multiple sclerosis - a review,” (in eng), Eur J Neurol, vol. 26, no. 1, pp. 27-40, Jan 2019. [CrossRef]
- P. Browne et al., “Atlas of Multiple Sclerosis 2013: A growing global problem with widespread inequity,” (in eng), Neurology, vol. 83, no. 11, pp. 1022-4, Sep 9 2014. [CrossRef]
- N. Koch-Henriksen and P. S. Sørensen, “The changing demographic pattern of multiple sclerosis epidemiology,” (in eng), Lancet Neurol, vol. 9, no. 5, pp. 520-32, May 2010. [CrossRef]
- A. Ascherio, “Environmental factors in multiple sclerosis,” (in eng), Expert Rev Neurother, vol. 13, no. 12 Suppl, pp. 3-9, Dec 2013. [CrossRef]
- B. R. Cardoso, D. J. Hare, A. I. Bush, and B. R. Roberts, “Glutathione peroxidase 4: a new player in neurodegeneration?,” (in eng), Mol Psychiatry, vol. 22, no. 3, pp. 328-335, Mar 2017. [CrossRef]
- M. Neema et al., “Deep gray matter involvement on brain MRI scans is associated with clinical progression in multiple sclerosis,” (in eng), J Neuroimaging, vol. 19, no. 1, pp. 3-8, Jan 2009. [CrossRef]
- X. Zhang, N. Surguladze, B. Slagle-Webb, A. Cozzi, and J. R. Connor, “Cellular iron status influences the functional relationship between microglia and oligodendrocytes,” (in eng), Glia, vol. 54, no. 8, pp. 795-804, Dec 2006. [CrossRef]
- A. V. Singh and P. Zamboni, “Anomalous venous blood flow and iron deposition in multiple sclerosis,” (in eng), J Cereb Blood Flow Metab, vol. 29, no. 12, pp. 1867-78, Dec 2009. [CrossRef]
- P. Jhelum et al., “Ferroptosis Mediates Cuprizone-Induced Loss of Oligodendrocytes and Demyelination,” (in eng), J Neurosci, vol. 40, no. 48, pp. 9327-9341, Nov 25 2020. [CrossRef]
- Cattani-Cavalieri et al., “Dimethyl Fumarate Attenuates Lung Inflammation and Oxidative Stress Induced by Chronic Exposure to Diesel Exhaust Particles in Mice,” (in eng), Int J Mol Sci, vol. 21, no. 24, Dec 18 2020. [CrossRef]
- L. Kwiatkowski et al., “Deferiprone vs deferoxamine for transfusional iron overload in SCD and other anemias: a randomized, open-label noninferiority study,” (in eng), Blood Adv, vol. 6, no. 4, pp. 1243-1254, Feb 22 2022. [CrossRef]
- A. Rayatpour, F. Foolad, M. Heibatollahi, K. Khajeh, and M. Javan, “Ferroptosis inhibition by deferiprone, attenuates myelin damage and promotes neuroprotection in demyelinated optic nerve,” (in eng), Sci Rep, vol. 12, no. 1, p. 19630, Nov 16 2022. [CrossRef]
- R. D. Leslie et al., “Adult-Onset Type 1 Diabetes: Current Understanding and Challenges,” (in eng), Diabetes Care, vol. 44, no. 11, pp. 2449-2456, Nov 2021. [CrossRef]
- Ogrotis, T. Koufakis, and K. Kotsa, “Changes in the Global Epidemiology of Type 1 Diabetes in an Evolving Landscape of Environmental Factors: Causes, Challenges, and Opportunities,” (in eng), Medicina (Kaunas), vol. 59, no. 4, Mar 28 2023. [CrossRef]
- S. Muntoni et al., “High meat consumption is associated with type 1 diabetes mellitus in a Sardinian case-control study,” (in eng), Acta Diabetol, vol. 50, no. 5, pp. 713-9, Oct 2013. [CrossRef]
- E. Syrjälä et al., “A Joint Modeling Approach for Childhood Meat, Fish and Egg Consumption and the Risk of Advanced Islet Autoimmunity,” (in eng), Sci Rep, vol. 9, no. 1, p. 7760, May 23 2019. [CrossRef]
- M. Cnop, J. C. Hannaert, A. Y. Grupping, and D. G. Pipeleers, “Low density lipoprotein can cause death of islet beta-cells by its cellular uptake and oxidative modification,” (in eng), Endocrinology, vol. 143, no. 9, pp. 3449-53, Sep 2002. [CrossRef]
- R. Buzzetti, S. Zampetti, and P. Pozzilli, “Impact of obesity on the increasing incidence of type 1 diabetes,” (in eng), Diabetes Obes Metab, vol. 22, no. 7, pp. 1009-1013, Jul 2020. [CrossRef]
- L. Campbell, T. W. Kay, L. Oxbrow, and L. C. Harrison, “Essential role for interferon-gamma and interleukin-6 in autoimmune insulin-dependent diabetes in NOD/Wehi mice,” (in eng), J Clin Invest, vol. 87, no. 2, pp. 739-42, Feb 1991. [CrossRef]
- E. Padgett, K. A. Broniowska, P. A. Hansen, J. A. Corbett, and H. M. Tse, “The role of reactive oxygen species and proinflammatory cytokines in type 1 diabetes pathogenesis,” (in eng), Ann N Y Acad Sci, vol. 1281, no. 1, pp. 16-35, Apr 2013. [CrossRef]
- A. I. S. Sobczak, S. J. Pitt, T. K. Smith, R. A. Ajjan, and A. J. Stewart, “Lipidomic profiling of plasma free fatty acids in type-1 diabetes highlights specific changes in lipid metabolism,” (in eng), Biochim Biophys Acta Mol Cell Biol Lipids, vol. 1866, no. 1, p. 158823, Jan 2021. [CrossRef]
- Y. Lee, H. Hirose, M. Ohneda, J. H. Johnson, J. D. McGarry, and R. H. Unger, “Beta-cell lipotoxicity in the pathogenesis of non-insulin-dependent diabetes mellitus of obese rats: impairment in adipocyte-beta-cell relationships,” (in eng), Proc Natl Acad Sci U S A, vol. 91, no. 23, pp. 10878-82, Nov 8 1994. [CrossRef]
- M. Norris et al., “Omega-3 polyunsaturated fatty acid intake and islet autoimmunity in children at increased risk for type 1 diabetes,” (in eng), Jama, vol. 298, no. 12, pp. 1420-8, Sep 26 2007. [CrossRef]
- Zhang, Y. Xiao, J. Hu, S. Liu, Z. Zhou, and L. Xie, “Lipid metabolism in type 1 diabetes mellitus: Pathogenetic and therapeutic implications,” (in eng), Front Immunol, vol. 13, p. 999108, 2022. [CrossRef]
- Y. Wang et al., “Hydrogen sulfide alleviates the anxiety-like and depressive-like behaviors of type 1 diabetic mice via inhibiting inflammation and ferroptosis,” (in eng), Life Sci, vol. 278, p. 119551, Aug 1 2021. [CrossRef]
- Bao, Y. Jin, J. Han, W. Wang, L. Qian, and W. Wu, “Berberine Regulates GPX4 to Inhibit Ferroptosis of Islet β Cells,” (in eng), Planta Med, vol. 89, no. 3, pp. 254-261, Mar 2023. [CrossRef]
- H. Feng et al., “Human umbilical cord mesenchymal stem cells ameliorate erectile dysfunction in rats with diabetes mellitus through the attenuation of ferroptosis,” (in eng), Stem Cell Res Ther, vol. 13, no. 1, p. 450, Sep 5 2022. [CrossRef]
| Pathway | Inhibitor | Experimental Methods |
Experimenta l Subject |
Experimental results |
|
| JAK/STAT | Tofacitinib | A nonlinear mixed-effects model |
Patients with ulcerative colitis (UC) |
Tofacitinib 5 mg b.i.d. has good clinical efficacy in UC patients, while 10 mg b.i.d has additional clinical benefits |
[34] |
| JAK/STAT | Tofacitinib | Randomized, double-blind, placebo-controlle d clinical trial |
Patients with ankylosing spondylitis (AS) |
Tofacitinib at a dose of 5mg and10mg twice daily will show superior efficacy over placebo at week 12, with a safety profile consistent with other indications |
[35] |
| JAK/STAT | Tofacitinib | Randomized, double-blind, placebo-controlle d clinical trial |
Patients with systemic lupus erythematos us (SLE) |
Improve SLE early-onset atherosclerosis related cardiac metabolism and immunological parameters |
[36] |
| JAK/STAT | Tofacitinib | Randomized, double-blind, placebo-controlle d clinical trial |
Patients with canine atopic dermatitis |
Good curative effects |
[37] |
| JAK/STAT | Tofacitinib | Randomized, double-blind, placebo-controlle d clinical trial |
Patients with psoriasis |
Both cow skin and shingles have good curative effect |
[38] |
| NF-κB | A small-m olecule NI K inhibitor |
Basic experiment | NZB/WF1 mice |
Good curative effects |
[55] |
| NF-κB | A small-m olecule NI K inhibitor |
Basic experiment | Pathological extracts from RA patients |
Good curative effects |
[56] |
| NF-κB | A small-m olecule NI K inhibitor |
Basic experiment | Pathological extracts from patients with endodermati tis |
Good curative effects |
[57] |
| Disease | Approach | Mechanism | Effect | Reference |
| RA | By inhibiting the occurrence of ferroptosis | Mice with induced arthritis were treated with ferroptosis inhibitor (LPX-1)) |
Effectively relieve joint swelling and synovial hyperplasia in mice, inhibit inflammation |
[74] |
| RA | By inhibiting the occurrence of ferroptosis |
Targeted activation of Nrf2 reduces ROS |
Effectively inhibit the proliferation and migration of FSL |
[80] |
| RA | By inhibiting the occurrence of ferroptosis |
FLS isolated from RA patients were treated with LPS and ferroptosis inducers and ferroptosis inhibitors, respectively |
Ferroptosis inhibitors can inhibit NCOA4-mediated iron phagocytosis to protect FLS |
[81] |
| RA | By inhibiting the occurrence of ferroptosis | Wasp venom (WV) accumulates ROS to induce GPX4-mediated ferroptosis |
Ferroptosis inducers are effective in RA treatment |
[77] |
| RA | By inducing the occurrence of ferroptosis |
For collagen-induced arthritis mice exhibiting a significant increase in fibroblast-like synoviocytes (FLS), the ferroptosis inducer IKE was administered. |
Ferroptosis inducer IKE can reduce inflammation and tissue damage by reducing the number of fibroblasts in mouse synovium |
[77] |
| RA | By inducing the occurrence of ferroptosis | Glycine was used in the CIA mouse model and the effect was evaluated |
Glycine promotes ferroptosis by increasing theconcentration of S-adenosylmethionine (SAM) to treat RA |
[79] |
| SLE | By inhibiting the occurrence of ferroptosis |
Erucic acid was used to suppress T cells in patients with SLE | Erucic acid regulates the immune response of pathogenic T cells and improves pregnancy response in SLE |
[90] |
| SLE | By inhibiting the occurrence of ferroptosis |
Erucic acid was used to suppress T cells in patients with SLE |
The ferroptosis inhibitor Liproxstatin-2 can reverse the serum induced ferroptosis in proximal renal tubular epithelial cells of LN patients and improve LN symptoms |
[81,93] |
| PsO | By inhibiting the occurrence of ferroptosis |
The ferroptosis inhibitor Fer-1 was administered |
Fer-1 inhibits lipid peroxidation to block the inflammatory response |
[106] |
| PsO | By inhibiting the occurrence of ferroptosis |
Fer-1 was applied to mice with IMQ-induced psoriasis-like dermatitis |
Fer-1 improved the increase of skin thickness and dyskeratosis in mice |
[104] |
| IBD | By inhibiting the occurrence of ferroptosis |
Use of CUR in a mouse model of colitis |
Significantly upregulated GPX4 expression and decreased UC ferroptosis |
[121] |
| IBD | By inhibiting the occurrence of ferroptosis |
The expression of Furin protease was measured in UC |
Significantly upregulated GPX4 expression and decreased UC ferroptosis |
[122] |
| IBD | By inhibiting the occurrence of ferroptosis |
Use of iron chelators (including maltol and kojic acid) in a male |
Effectively reduce inflammation index |
[123] |
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2025 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (http://creativecommons.org/licenses/by/4.0/).




