1. Introduction
Breast cancer is one of the most common cancers worldwide. As the leading cause of cancer-related death in women under 50 years of age, substantial efforts have focused on increasing the understanding of breast cancer pathophysiology and developing novel treatments [
1]. Despite reductions in breast cancer mortality, incidence rates continue to rise, in part due to more advanced and proactive screening practices and possibly increased prevalence of risk factors [
2]. These increased risk factors can include obesity, physical inactivity, red meat consumption, alcohol use, smoking, and oral contraceptives [
3].
Breast cancer subtypes are classified based on the presence or absence of hormone receptors (HR) and the human epidermal growth factor receptor 2 (HER2) protein, a tyrosine kinase oncogene. HR-positive breast cancers express either estrogen or progesterone receptors, enabling cancer cells to receive hormone signals that promote tumor growth [
4]. Overexpression of HER2 results in excessive cancer cell proliferation and suppression of normal apoptotic signals; thus, HER2-positive cancers are generally more aggressive malignancies [
4,
5,
6].
Typically, breast cancer is classified into four major subtypes: HR+/HER2+, HR+/HER2−, HR−/HER2+, and HR−/HER2−. Of these, HR+/HER2− is the most common, accounting for approximately 70% of diagnosed cases [
4]. This subtype is generally associated with a favorable prognosis due to slower growth and responsiveness to hormone therapies [
7]. In patients with advanced (Stage III) HR+/HER2− breast cancer, mutations frequently occur in the phosphoinositide-3-kinase (PI3K)/protein kinase B (AKT)/mammalian target of rapamycin (mTOR) pathway, accounting for up to 40% of mutations in this population [
8]. Given the prevalence of such mutations, the PI3K/AKT/mTOR pathway has become a meaningful therapeutic target [
9].
The standard of care for HR+/HER2− breast cancer is a drug regimen consisting of endocrine therapy combined with a cyclin-dependent kinase 4/6 inhibitor (CDK4/6i) [
6]. However, endocrine resistance often develops, resulting in a substantial loss of efficacy of endocrine-based therapies [
4]. In October 2024, the FDA approved the PI3Kα inhibitor inavolisib (ITOVEBI™) in combination with the standard-of-care agents palbociclib and fulvestrant for adults with endocrine-resistant, PIK3CA-mutated, HR+/HER2−, locally advanced or metastatic breast cancer [
10]. In the phase III INAVO120 trial (NCT04191499), stomatitis was reported as an adverse event in 51% of patients who received this treatment regimen [
11]. Given its recent approval, real-world data for patients receiving inavolisib (ITOVEBI™) remain limited, and incidence rates of stomatitis should be carefully monitored as inavolisib (ITOVEBI™) progresses through two additional phase III trials, INAVO121 (NCT05646862) and INAVO122 (NCT05894239), and into the postmarketing phase [
12,
13].
Stomatitis is an umbrella term describing inflammation of the oral mucosal membranes, which may include the lining of the oral cavity, lips, gingiva, tongue, palate, and pharynx [
14]. The condition is typically characterized by ulcers, blisters, erythema (redness), or desquamation (peeling) of these membranes [
15,
16]. Diagnosis usually relies on oral tissue appearance, occasionally supplemented with laboratory culture to exclude oral infection, and review of the medical history [
15,
16]. The etiology of stomatitis includes medications, radiation, viral or fungal infections, smoking, physical trauma, nutritional deficiencies, and autoimmune disorders [
17]. To refine diagnosis, stomatitis is often subcategorized according to etiology, such as
Candida-related stomatitis, herpetic gingivostomatitis, or autoimmune stomatitis [
18].
The term “stomatitis” is usually used to describe the adverse effect induced by targeted agents, such as inavolisib. In contrast, oral mucosal inflammation caused by other chemotherapy agents is sometimes referred to as “oral mucositis” [
19]. Notably, the term “stomatitis” does not appear in the most recent version (v5.0) of the Common Terminology Criteria for Adverse Events (CTCAE) from the U.S. Department of Health and Human Services; instead, the preferred term is “mucositis oral” [
20]. At the same time, the
Encyclopedia of Otolaryngology, Head and Neck Surgery lists stomatitis as synonymous with aphthous stomatitis and mucositis [
21]. Specifically, mucositis is defined as involving tissue thinning in addition to inflammation and is typically caused by chemotherapy and radiation; interestingly, no such comment on etiology is provided in the definition for stomatitis [
17,
22]. The lack of clear differentiation between stomatitis and oral mucositis, and the absence of consensus on which oral structures, such as the pharynx, are affected in stomatitis, contribute to the challenges of monitoring stomatitis incidence in clinical trials and during postmarketing pharmacovigilance.
While stomatitis is not generally a life-threatening condition, it can significantly diminish quality of life of patients [
15]. Risk for stomatitis-associated adverse events is included as label warnings for other chemotherapies targeting the PI3K/AKT/mTOR pathway, with mTOR-inhibitor–associated stomatitis (mIAS) being well documented in the literature [
23].
The purpose of this review is to provide a comprehensive analysis of the reporting rates of stomatitis associated with four HR+/HER2− breast cancer medications, alpelisib/PIQRAY®, capivasertib/TRUQAP™, everolimus/AFINITOR®, and palbociclib/IBRANCE®, using data from the Food and Drug Administration Adverse Event Reporting System (FAERS) database. In addition to a comparative analysis of stomatitis reporting rates between these drugs, this study evaluates the potential impact of different criteria and definitions of stomatitis as a safety signal.
Everolimus is an mTOR kinase inhibitor that received initial FDA approval in 2009 for the treatment of advanced renal cell carcinoma after failure of treatment with sunitinib or sorafenib, and for subependymal giant cell astrocytoma associated with tuberous sclerosis in patients requiring therapeutic intervention but not eligible for curative surgical resection. In 2012, it was approved for the treatment of advanced HR+/HER2− breast cancer in postmenopausal women, in combination with exemestane, after failure of treatment with either letrozole or anastrozole [
24].
Palbociclib is a cyclin-dependent kinase (CDK) 4/6 inhibitor used alongside other medications in first-line therapy for HR+/HER2− advanced or metastatic breast cancers. The FDA initially granted accelerated approval for palbociclib in February 2015, in combination with letrozole, for the treatment of postmenopausal women with estrogen receptor (ER)-positive, HER2− advanced breast cancer as initial endocrine-based therapy for metastatic disease [
25].
Alpelisib is a Phosphoinositide 3-kinase alpha (PI3Kα) inhibitor approved in May 2019 by the FDA, in combination with fulvestrant, for postmenopausal women and men with HR+/HER2−, PIK3CA-mutated, advanced or metastatic breast cancer, as detected by an FDA-approved test, following progression on or after an endocrine-based regimen [
26].
Capivasertib is an AKT inhibitor, also known as protein kinase B inhibitor, approved by the FDA in November 2023, in combination with fulvestrant, for adult patients with HR+/HER2− locally advanced or metastatic breast cancer with one or more PIK3CA/AKT1/PTEN alterations, as detected by an FDA-approved test, following progression on at least one endocrine-based regimen in the metastatic setting or recurrence on or within 12 months of completing adjuvant therapy [
27].
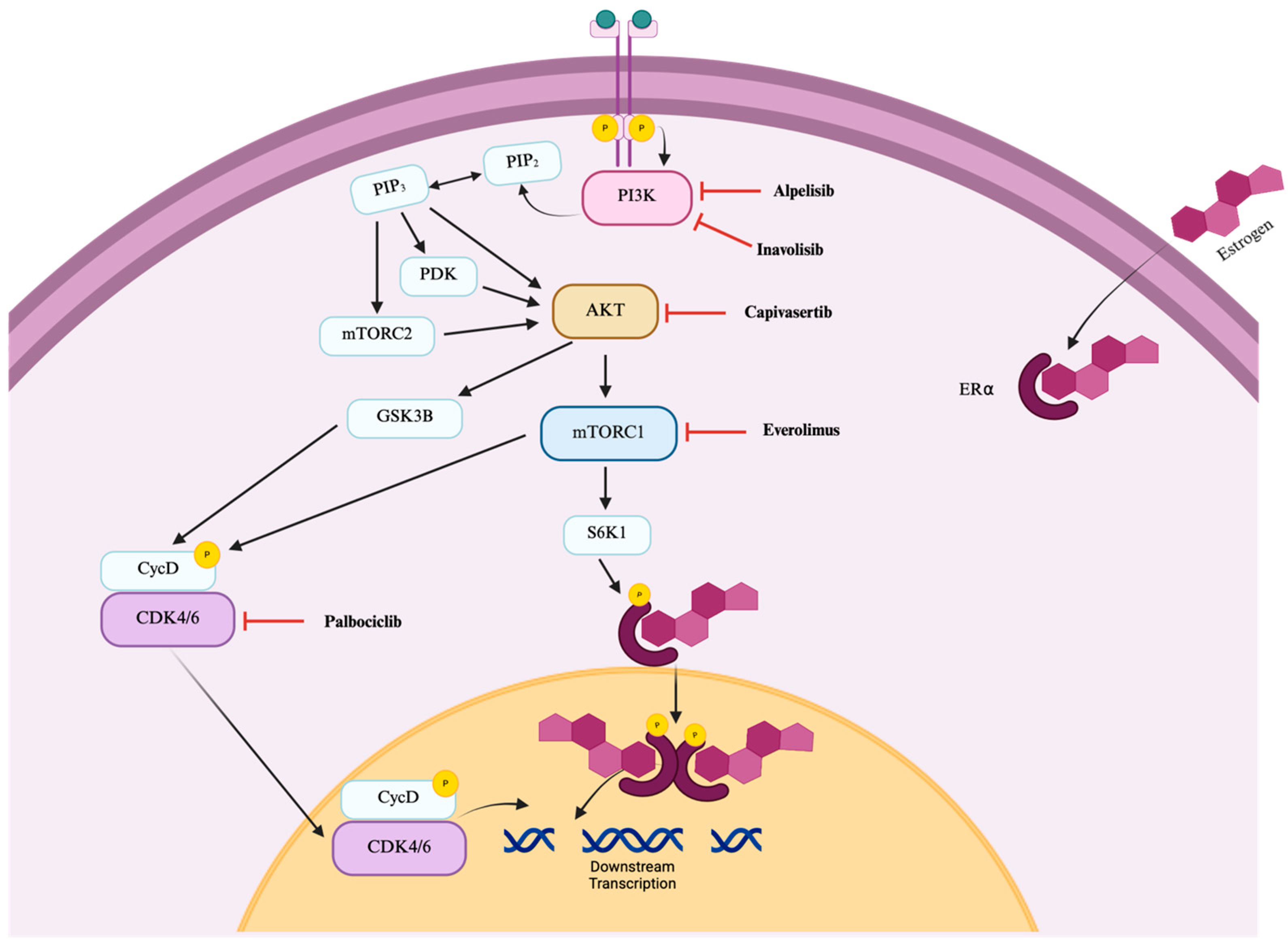
Alpelisib, capivasertib, and everolimus disrupt the PI3K/AKT/mTOR pathway in a manner similar to inavolisib (
Figure 1) and are associated with the incidence of stomatitis. Palbociclib, in contrast, acts further downstream (
Figure 1) and was included in this analysis given its role in the inavolisib regimen as well as prior reports linking CDK4/6 inhibitors to an increased risk of stomatitis in breast cancer patients [
28].
PI3K/AKT/mTOR inhibitors used in breast cancer differ in their toxicity profiles, particularly regarding stomatitis rates. This study developed synonym-based screening filters to improve identification of stomatitis and compared its incidence across four targeted drugs. Everolimus, an mTOR inhibitor, showed the highest rates. Alpelisib and palbociclib showed a moderate risk for stomatitis, although alpelisib had greater risk than palbociclib, suggesting a key role for PI3K inhibition. Capivasertib showed the lowest occurrence, but continued monitoring is needed given the limited data on AKT inhibitors.
2. Materials and Methods
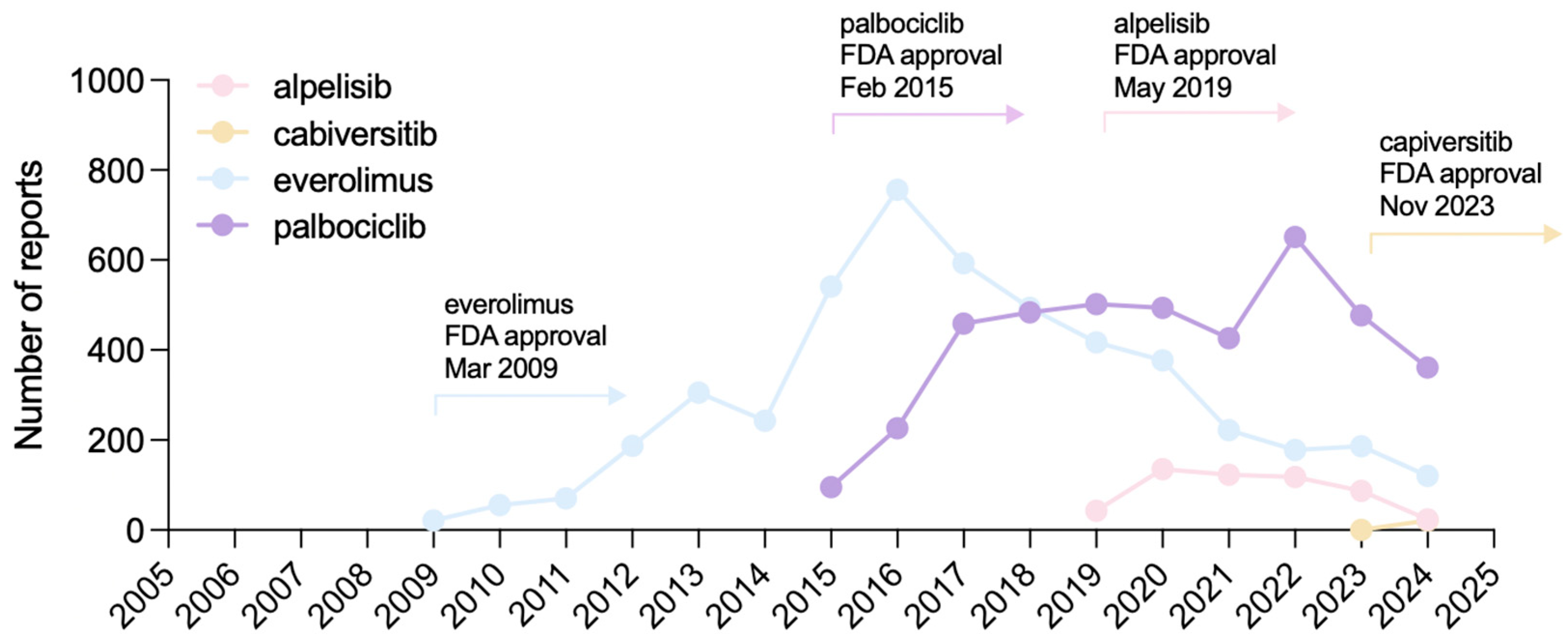
This retrospective pharmacovigilance study analyzed data from the FAERS database, which contained 30,179,725 reports as of 31 March 2025 (end of Q1 2025). Reports for alpelisib/PIQRAY
® (10,510,579), capivasertib/TRUQAP™ (2,494,572), everolimus/AFINITOR
® (18,559,838), and palbociclib/IBRANCE
® (16,603,480) were retrieved (
Figure 2).
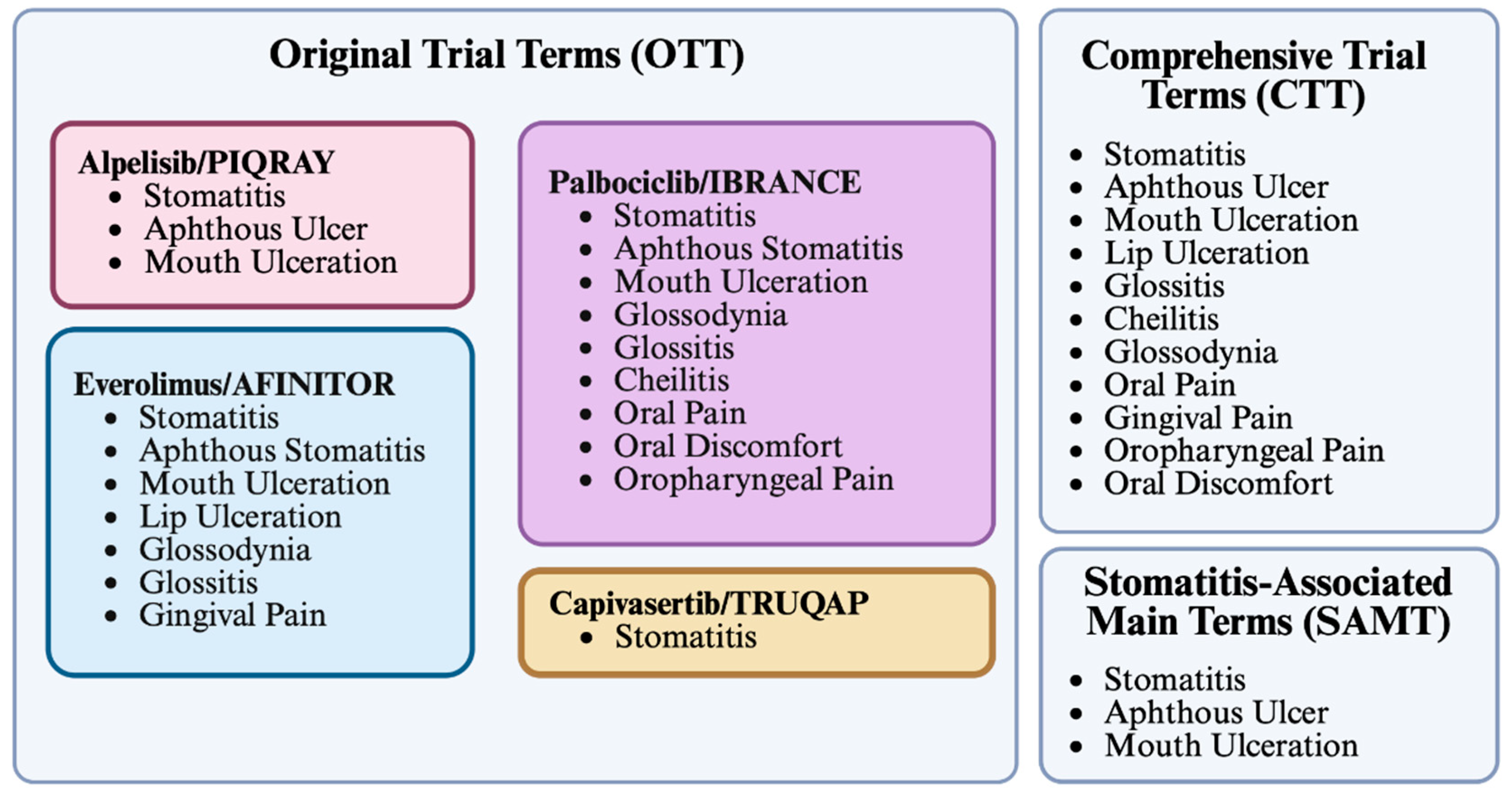
To capture stomatitis incidence comprehensively, three filter strategies were applied. The Original Trial Terms (OTT) filter used adverse event terms reported in the phase III clinical trials of each drug, as listed in the FDA label (
Figure 3). The Comprehensive Trial Terms (CTT) filter combined the definitions applied across all four drugs’ phase III clinical trials (
Figure 3). The Stomatitis-Associated Main Terms (SAMT) filter focused on the three most frequent stomatitis-related terms: “stomatitis,” “aphthous ulcer,” and “mouth ulceration” (
Figure 3).
Some terms were considered but excluded. For example, “aphthous stomatitis” was not included in SAMT because it is not indexed within FAERS. Similarly, “mucosal inflammation,” which appeared in the PALOMA-2 trial for palbociclib, was omitted from OTT due to its poor specificity for oral localization. Of note, the PALOMA-3 trial employed the term “oropharyngeal discomfort” rather than the “oral discomfort” used in PALOMA-2.
Data were extracted from the FAERS database and analyzed using a custom Python script generated with the help of ChatGPT-4 (
https://github.com/DSimoens/FAERS_PHARMACOVIGILANCE_ANALYSIS). Both generic and brand names were included in the search. The alpelisib dataset also included some reports for VIJOICE
®, alpelisib marketed and indicated for PIK3CA-related overgrowth spectrum. Individual report counts for each drug and search term are provided in
Table 1.
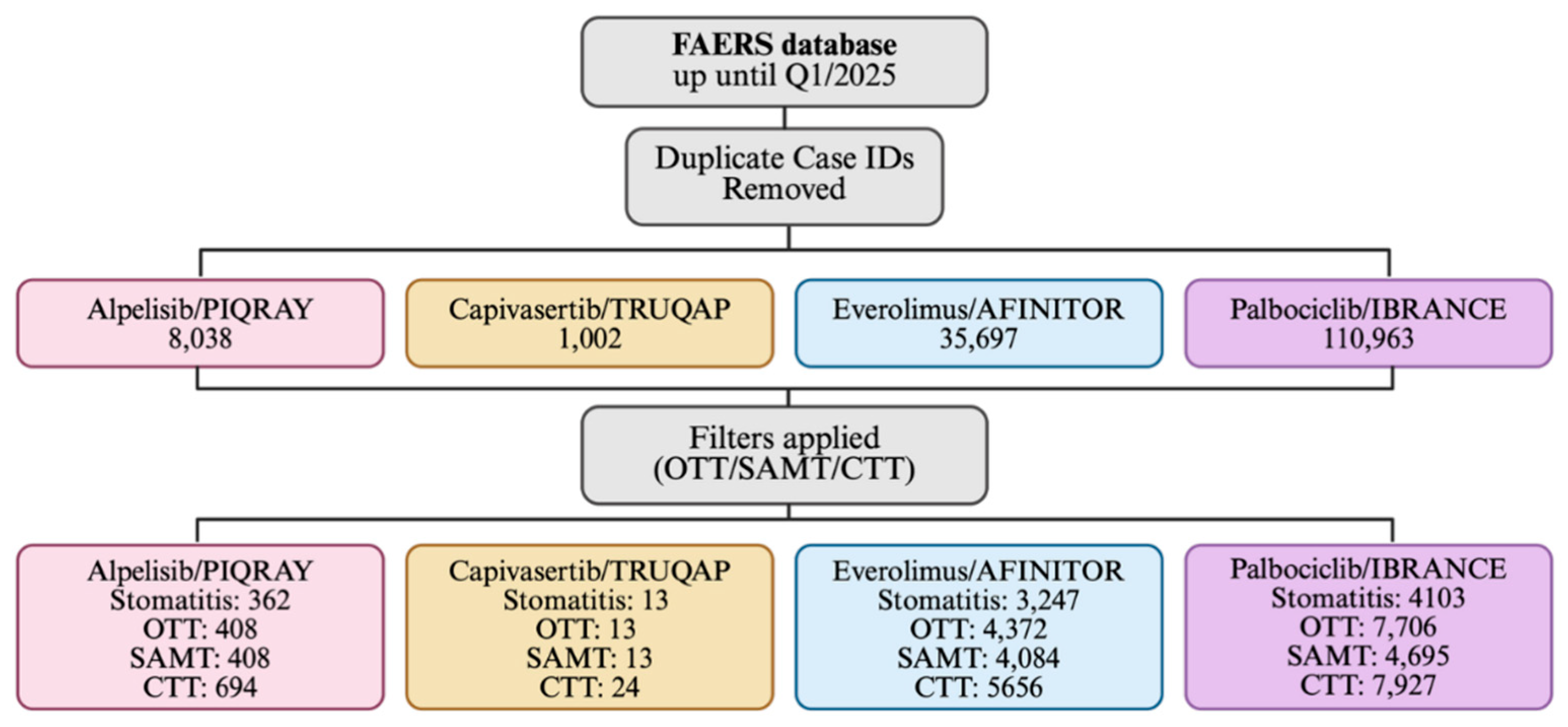
Disproportionality analyses were performed following the removal of duplicate reports. For each adverse event group, a two-by-two contingency table was constructed to compare the frequency of reports involving the drug of interest with those involving all other drugs in FAERS. From these data, disproportionality metrics, including the reporting odds ratio (ROR) and proportional reporting ratio (PRR), were calculated with 95% confidence intervals. A flowchart showing the data analysis strategy is shown in
Figure 4. Statistical significance for the ROR was assessed using Fisher’s exact test as well as chi-square testing, with and without Yates’ continuity correction.
3. Results
Adverse event reports for alpelisib/PIQRAY
®, capivasertib/TRUQAP™, everolimus/AFINITOR
®, and palbociclib/IBRANCE
® were extracted from the FAERS database, including data up to the end of Q1 2025 (March 31, 2025). Initial extraction prior to duplicate removal yielded 8,038 reports for alpelisib, 1,002 for capivasertib, 35,697 for everolimus, and 110,963 for palbociclib (
Figure 3). These absolute differences in the number of reports reflect the earlier FDA approvals of palbociclib (2015) and everolimus (2009) compared with the more recent approvals of alpelisib (2019) and capivasertib (2023).
To identify stomatitis-related cases, three filter strategies were applied: Original Trial Terms (OTT), Comprehensive Trial Terms (CTT), and Stomatitis-Associated Main Terms (SAMT). The OTT filter was based on the event terms reported in the phase III trials of each drug and therefore differed across drugs. The CTT filter combined all terms used in the phase III trials of the four drugs. The SAMT filter focused on the three most common stomatitis terms reported in phase III trials: “stomatitis,” “aphthous ulcer,” and “mouth ulceration” (
Figure 3). Some terms were excluded due to poor specificity or lack of compatibility with FAERS (e.g., “mucosal inflammation,” “aphthous stomatitis”).
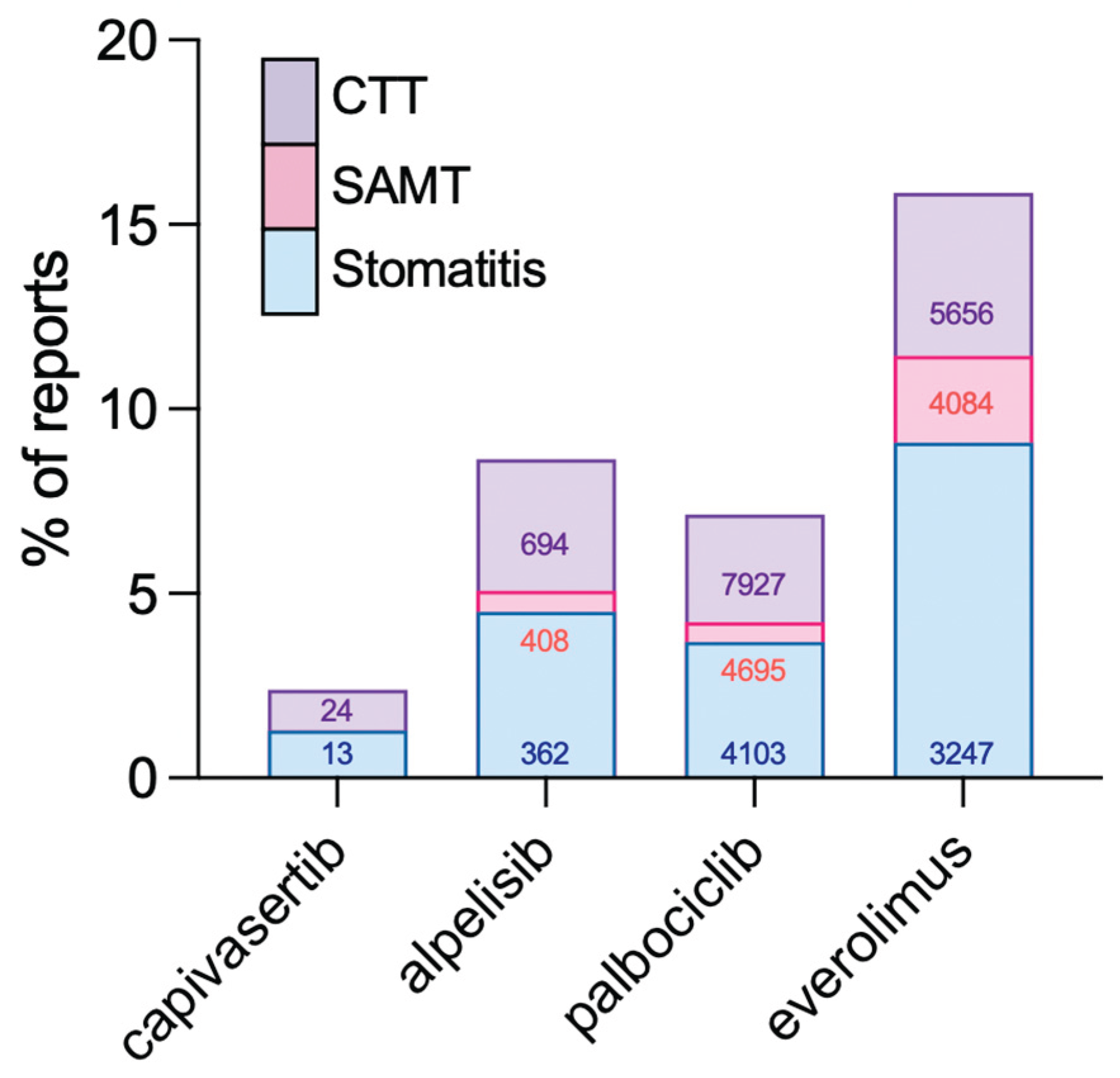
Stomatitis-associated adverse events were detected for all four drugs. Using the CTT filter, 694 reports were identified for alpelisib, 24 for capivasertib, 5,656 for everolimus, and 7,927 for palbociclib. Corresponding counts for the SAMT filter were 408, 13, 4,084, and 4,695, respectively. For “stomatitis” alone, the numbers were 362, 13, 3,247, and 4,103, respectively (
Table 1).
Reporting odds ratios (ROR) and proportional reporting ratios (PRR) were calculated for stomatitis events using “stomatitis” alone, or the three filters, SAMT, OTT, and CTT (
Figure 5). All four drugs demonstrated ROR values greater than 1, indicating increased odds of stomatitis relative to other drugs in FAERS. PRR values were overall highly similar to ROR. Among the evaluated drugs, everolimus showed the highest disproportionality signal, while capivasertib showed the lowest. Alpelisib had a higher ROR than palbociclib, and the ROR for palbociclib was moderate in comparison.
To evaluate the performance of the different filters, stomatitis cases captured by SAMT, CTT, and “stomatitis” alone were compared (
Figure 6). The number of identified reports increased with broader term sets, as expected. The difference between SAMT and CTT was modest (~2% for most drugs), while differences between SAMT and “stomatitis” alone were minimal (0–1.5%). Differences between CTT and “stomatitis” ranged from 1% to 3.5%.
Across all filter strategies, everolimus consistently showed the highest proportion of stomatitis-related reports relative to its total FAERS cases. Alpelisib also showed a higher percentage of stomatitis-related reports compared with palbociclib.
4. Discussion
4.1. Mechanistic Considerations
We identified significant disproportionality signals for stomatitis across all four drugs, with everolimus showing the highest reporting odds ratio, alpelisib demonstrating an intermediate risk, palbociclib showing a moderate risk, and capivasertib displaying the lowest. These differences suggest that the risk of stomatitis may vary depending on the molecular target within the PI3K/AKT/mTOR signaling pathway.
Everolimus, an mTOR inhibitor, produced the strongest signal, consistent with the well-documented phenomenon of mTOR-inhibitor-associated stomatitis (mIAS). mTOR plays a critical role in epithelial cell growth, mucosal turnover, and repair. Generally, its inhibition is thought to impair mucosal regeneration, thus leading to aphthous-like ulcerations [
23].
Alpelisib, a PI3Kα inhibitor, also showed an elevated risk compared with palbociclib. PI3K signaling influences both epithelial cell survival and immune regulation, and its inhibition may directly contribute to stomatitis pathophysiology. Palbociclib, in contrast, acts further downstream at CDK4/6 and demonstrated only a moderate signal, suggesting that inhibition of cell-cycle progression alone may not be sufficient to trigger the same degree of oral mucosal injury [
9].
Capivasertib, an AKT inhibitor, showed the lowest apparent risk. While this may suggest that AKT inhibition is less directly involved in the pathways leading to oral inflammation, limited real-world data due to the recent approval of the drug may skew results. Furthermore, as stomatitis was addressed during clinical development and on the drug label at the time of approval, this may reduce postmarketing reporting. Therefore, both limited real-world exposure and expectedness of the event could underestimate the true signal.
Taken together, these findings are consistent with a potential mechanistic gradient, where inhibition of PI3K or mTOR more strongly predisposes to stomatitis than inhibition at CDK4/6 or AKT. However, additional post-marketing data, especially for capivasertib, is necessary to confirm whether lower apparent risk reflects true biology or limitations of the current pharmacovigilance dataset.
4.2. Current State of Oral Toxicities and Cancer Treatments
Targeted and combination therapies, including the protein kinase inhibitors described here, have provided new and promising avenues for effective cancer treatment. However, toxicities affecting the oral cavity, such as stomatitis, continue to occur with these agents, albeit with different clinical presentations compared with toxicities caused by conventional chemotherapy or radiotherapy [
29,
30]. Although typically mild, these oral toxicities can substantially impair quality of life, causing pain and interfering with eating, drinking, and speaking [
15]. Secondary complications, including dehydration and malnutrition, may arise and can further exacerbate stomatitis, sometimes leading to non-adherence or discontinuation of therapy. Medical attention and proactive evaluation of management strategies are, therefore, essential for patients receiving these drugs.
Baseline oral health examinations can help detect stomatitis early and identify patients with pre-existing conditions that may increase susceptibility to oral toxicities. Incorporating comprehensive oral health assessments into the clinical evaluation of drug candidates during phase trials may also facilitate the development of monitoring protocols that can be carried forward into the postmarketing setting.
Given the clinical significance of these toxicities, our analysis of stomatitis signals in FAERS provides important insight into how oral adverse events are reported with PI3K, AKT, mTOR, and CDK4/6 inhibitors, and highlights the need for systematic monitoring of oral health in patients treated with targeted therapies.
4.3. Recommendations for Identification of Stomatitis Safety Signals
Quantitative differences were observed between stomatitis-associated reports depending on the filter used (
Figure 6,
Table 1). The percentage of stomatitis cases captured by the SAMT filter differed slightly from the CTT filter, with an average difference of approximately 2%. While this difference may be relevant, it does not appear substantial enough to justify using all 11 terms included in the CTT filter over the three terms in SAMT. Differences between SAMT and “stomatitis” alone were even smaller (0–1.5%). However, a notable discrepancy was observed between “stomatitis” alone and the broader SAMT or CTT filters, suggesting that relying only on the term “stomatitis” would miss relevant cases that align with stomatitis events. To minimize the risk of underreporting, we recommend the use of the SAMT filter when screening for stomatitis safety signals in both clinical trials and postmarketing settings.
The SAMT filter captures pertinent stomatitis reports without being overly expansive, unlike the CTT filter. Although some cases may still be missed, the SAMT filter offers a practical balance that maximizes signal detection by relying on the most clinically relevant medical terms associated with stomatitis. Importantly, the use of SAMT can help prevent unintentional disregard of stomatitis, which is often underestimated as an adverse event in oncology where patients often tolerate a high burden of side effects [
31].
Our data also suggest that drugs targeting the PI3K/AKT/mTOR pathway, particularly PI3K and mTOR inhibitors, are associated with a higher risk of stomatitis than downstream targets such as CDK4/6. This finding is relevant in the context of combination regimens, where multiple protein kinase inhibitors may be administered simultaneously. Awareness of this increased risk may help clinicians anticipate, monitor, and manage stomatitis more effectively. For example, providers may preemptively counsel patients about oral toxicities if their regimen includes both a PI3K and a CDK4/6 inhibitor, such as the FDA-approved combination of inavolisib and palbociclib. Increased awareness may also lead to more frequent reporting of stomatitis events, even if the true incidence remains unchanged.
It should also be recognized that the number of reports varies significantly across drugs. Palbociclib, a first-in-class and first-line treatment for postmenopausal, metastatic HR+/HER2− breast cancer, regardless of mutational status, had the highest number of reports. In contrast, capivasertib had very few reports, most likely due to its recent market entry in 2023. As capivasertib use expands, its safety profile, including stomatitis risk, may become clearer with additional data.
Finally, infectious causes of stomatitis, including herpes simplex virus type 1 (HSV-1), herpes zoster, and
Candida albicans, are common in oncology patients, particularly in the setting of chemotherapy or prolonged corticosteroid exposure [
15,
16]. As it is not possible to reliably distinguish infection-associated stomatitis from drug-related stomatitis in FAERS, reports of herpes or
Candida infections were not excluded from the analysis. Screening indicated that herpes and
Candida infections accounted for ~3% of stomatitis-related reports included in the CTT filter for drugs with substantial report numbers, while no such reports were identified for capivasertib (data not shown). Given this low prevalence, herpes and
Candida infections were not considered a significant confounder in this study.
4.4. Stomatitis and Oral Mucositis Treatment
There is no standardized treatment for stomatitis or oral mucositis. Common recommendations for patients with stomatitis include maintaining proper oral hygiene and avoiding products that could irritate the oral mucosa, such as spicy, acidic, or crunchy foods, alcohol, peroxide-based mouthwashes, and mint-flavored toothpaste [
14]. Pain management strategies for stomatitis caused by targeted therapies or oral mucositis caused by chemotherapy/radiotherapy have included the use of ice chips, topical lidocaine, steroid ointments, low-level laser therapy, and, in severe cases, systemic analgesics [
29,
32,
33].
Although not yet evaluated for stomatitis caused by targeted therapies, palifermin remains a potential option for future management of oral mucosal tissue damage. Palifermin, a recombinant human keratinocyte growth factor, was FDA approved in 2004 to reduce the incidence and duration of oral mucositis in patients receiving intensive chemotherapy and radiotherapy for hematologic cancers [
34]. Binding of keratinocyte growth factor to its receptor, some of which are expressed in the oral cavity, promotes epithelial proliferation, differentiation, and migration. Future investigations may evaluate palifermin for targeted therapy–associated stomatitis; however, caution is warranted, as chemotherapy/radiotherapy-induced oral mucositis is better understood than the pathobiology of stomatitis associated with PI3K/mTor/AKT pathway inhibitors [
35,
36]. In addition, some targeted therapies may produce distinct stomatitis phenotypes, such as mIAS, which more closely resembles recurrent aphthous stomatitis [
23]. Even if palifermin is effective, its benefit may depend on the specific targeted agent involved.
In recent years, corticosteroid-containing mouthwashes have been studied for the prevention or mitigation of stomatitis and oral mucositis. These trials demonstrated particular efficacy of dexamethasone-based mouthwashes in breast cancer patients treated with chemotherapy, in breast cancer patients receiving everolimus (SWISH trial), and in head and neck cancer patients undergoing chemoradiation [
37,
38,
39]. Some targeted therapies, such as inavolisib and everolimus, already mention corticosteroid-containing mouthwashes in their FDA labeling as an option for treatment or prevention of stomatitis. Expanding such labeling to other protein kinase inhibitors with known stomatitis risk may improve both provider and patient awareness and facilitate more consistent care [
40]. This is particularly important given that pharmacies often dispense individualized “magic mouthwash” formulations that vary considerably in content [
41]. Directly specifying dexamethasone-based mouthwashes on labels, with standardized dosing and swishing instructions, could help optimize symptom management. This is especially relevant since some “magic mouthwash” formulations contain antifungal agents such as nystatin, whereas the FDA label for everolimus specifically advises against antifungal use unless fungal infection is confirmed [
42].
Although this study focused on stomatitis reports for four PI3K/mTOR/AKT pathway inhibitors individually, many targeted therapies are used in combination with chemotherapy or radiotherapy [
9]. For patients receiving targeted therapies with even moderate stomatitis risk, preventive care may be valuable in minimizing incidence and severity. This is especially relevant in regimens combining multiple stomatitis-associated agents, such as the FDA-approved combination of inavolisib with fulvestrant and palbociclib. Since both inavolisib and palbociclib have been linked to increased risk of stomatitis, proactive measures could substantially improve tolerability. Notably, while the FDA label for inavolisib recommends corticosteroid-containing mouthwash only after stomatitis develops, the everolimus label advises initiating dexamethasone alcohol-free mouthwash at the start of treatment. Amending labels to emphasize preventive strategies and specify effective treatments such as dexamethasone-based mouthwashes may ultimately improve patient outcomes.
4.5. Limitations of the Study
4.5.1. Filters and Terms
The CTT filter used in this study comprises the terms applied in registration trials to detect stomatitis. However, it does not represent a comprehensive list of all possible terms that may signal a stomatitis event. Additional terms present in the FAERS database include lip blister, mouth swelling, oedema mouth, oral blood blister, oral mucosal blistering, tongue ulceration, and tongue blistering. Furthermore, the CTT filter in this analysis was restricted to the terms reported in registration trials, and did not incorporate terms such as mouth sores or mouth ulcers—descriptors that often appear in FDA approval labels, prescribing information, or patient-facing literature. As stomatitis functions as an umbrella term encompassing oral mucosal inflammation, swelling, and ulceration, identifying discrete terms suitable for signal detection remains challenging. Further complexity arises in determining the anatomical boundaries of stomatitis, particularly when considering involvement of the pharynx. For example, it is not always clear whether pharyngeal ulcerations should be classified under stomatitis.
4.5.2. Polypharmacy and Underlying Patient Conditions
Many of the drugs examined in this study are prescribed as part of complex regimens or treatment plans, which complicates attribution of adverse events to a single agent. Polypharmacy, as well as drug–drug and drug–food interactions, may further exacerbate certain adverse events or obscure their true cause [
43].
Patient-specific factors may also play an important role. Underlying conditions or lifestyle choices can predispose individuals to adverse events or even be the primary cause. For example, a patient who smokes and frequently consumes sour or spicy foods may develop a mouth sore independent of drug exposure. However, if that patient is taking a medication with mouth sores listed as a potential adverse effect, the event may still be reported as drug-related.
These background influences can also alter the severity of a stomatitis event, potentially amplifying its presentation compared to what might occur if the medication were taken in isolation, without external risk factors.
4.5.3. Health Literacy and Medical Terminology
An important consideration in evaluating stomatitis signals is the health literacy of both patients and healthcare providers [
44]. In the literature, there is no standardized distinction between oral mucositis and stomatitis. In some contexts, the terms are used interchangeably, while in others oral mucositis is defined more narrowly as oral mucosal inflammation secondary to chemotherapy or radiotherapy. This inconsistency is reflected in the Common Terminology Criteria for Adverse Events (CTCAE), which does not include “stomatitis” as a term but instead lists “mucositis oral,” defined as “a disorder characterized by ulceration or inflammation of the oral mucosa.” The lack of clarity regarding terminology may contribute to incomplete capture or misclassification of stomatitis incidents in safety reviews.
While such distinctions may be relevant to clinical investigators and healthcare professionals, they are unlikely to resonate with patients. When reporting adverse events, patients often use colloquial terms such as “canker sores,” “mouth sores,” or describe symptoms like “burning in the mouth.” This creates challenges for systematic signal detection, since databases rely on standardized medical terminology. For example, the SAMT filter—comprising stomatitis, aphthous ulcer, and mouth ulceration—may be more biased toward terminology familiar to clinicians and underrepresent patient-reported language. In practice, “mouth ulceration” is likely closer to the phrasing patients would use, whereas “stomatitis” or “aphthous ulcer” are more specialized terms. This discrepancy raises concerns that signals based on patient or consumer reports may be underdetected compared with those generated by healthcare professionals or pharmaceutical companies.
4.5.4. Constraints of the FAERS Database
Inherently, the FAERS database cannot be used to determine the true incidence of adverse events. Instead, FAERS data are most appropriately applied to generate disproportionality measures, such as the reporting odds ratio (ROR), which reflect relative reporting patterns rather than absolute risk. Therefore, it is important to note that FAERS signals indicate whether an event is reported more often with one drug than with others, but they do not establish how frequently the event occurs in the treated population. Here were report ROR and PRR analyses. ROR is generally the most statistically robust metric for FAERS data. Unlike incidence rates reported in clinical trials, ROR represents the relative likelihood of an adverse event being reported for one drug compared to others, rather than the absolute probability of the event occurring. The PRR reports the proportion of the specific adverse events, and as expected, was overall similar to the ROR for the four drugs and the different filters.
Reporting frequencies in FAERS are influenced by external factors such as label warnings, provider or patient awareness, media coverage, regulatory emphasis, and differences in manufacturer pharmacovigilance systems. Reports may also reflect comorbidities, lifestyle factors, or the underlying disease rather than the medication itself. Thus, while FAERS is valuable for detecting safety signals and generating hypotheses, it must be interpreted as complementary to clinical trial data and cannot substitute for incidence data derived from rigorously monitored studies.
Author Contributions
Conceptualization, Monica Marni, Walter Jones and Simon Kaja; Data curation, Monica Marni, Djamilla Simoens and Simon Kaja; Formal analysis, Monica Marni, Djamilla Simoens, Nicholas Romero and Simon Kaja; Funding acquisition, Walter Jones and Simon Kaja; Investigation, Monica Marni, Djamilla Simoens, Nicholas Romero and Simon Kaja; Methodology, Monica Marni, Djamilla Simoens, Nicholas Romero and Simon Kaja; Project administration, Walter Jones and Simon Kaja; Resources, Djamilla Simoens and Simon Kaja; Software, Monica Marni, Djamilla Simoens and Nicholas Romero; Supervision, Walter Jones and Simon Kaja; Validation, Monica Marni, Djamilla Simoens and Simon Kaja; Visualization, Monica Marni and Simon Kaja; Writing – original draft, Monica Marni and Djamilla Simoens; Writing – review & editing, Monica Marni, Djamilla Simoens, Nicholas Romero, Walter Jones and Simon Kaja.
Figure 1.
Molecular targets of protein kinase inhibitors for the treatment of HR+/HER2- breast cancer. Schematic representation of the the PI3K/AKT/mTOR pathway. Alpelisib, capiversitib and everolimus target PI3K, AKT, and mTORC1, respectively. In contrast, palbociclib inhibits CDK4/6 signaling downstream of mTORC1 activation. Abbreviations: PI3K: phosphatidylinositol-3 kinase, AKT: protein kinase B, mTORC1: mammalian target of rapamycin complex 1, mTORC2: mammalian target of rapamycin complex 2, PIP2: phosphatidylinositol 4,5-bisphosphate, PIP3: phosphatidylinositol 3,4,5-trisphosphate, PDK: phosphoinositide-dependent protein kinase, CycD: cyclin D, CDK4/6: cyclin-dependent kinase types 4 and 6, S6K1: ribosomal S6 kinase 1, Erα: estrogen receptor alpha, P: phosphorylated indication. Created in BioRender. Kaja, S. (2025) https://BioRender.com/q7my3m5.
Figure 1.
Molecular targets of protein kinase inhibitors for the treatment of HR+/HER2- breast cancer. Schematic representation of the the PI3K/AKT/mTOR pathway. Alpelisib, capiversitib and everolimus target PI3K, AKT, and mTORC1, respectively. In contrast, palbociclib inhibits CDK4/6 signaling downstream of mTORC1 activation. Abbreviations: PI3K: phosphatidylinositol-3 kinase, AKT: protein kinase B, mTORC1: mammalian target of rapamycin complex 1, mTORC2: mammalian target of rapamycin complex 2, PIP2: phosphatidylinositol 4,5-bisphosphate, PIP3: phosphatidylinositol 3,4,5-trisphosphate, PDK: phosphoinositide-dependent protein kinase, CycD: cyclin D, CDK4/6: cyclin-dependent kinase types 4 and 6, S6K1: ribosomal S6 kinase 1, Erα: estrogen receptor alpha, P: phosphorylated indication. Created in BioRender. Kaja, S. (2025) https://BioRender.com/q7my3m5.
Figure 2.
Graphical representation of the total number of reports submitted to the FAERS database for each drug since its FDA approval.
Figure 2.
Graphical representation of the total number of reports submitted to the FAERS database for each drug since its FDA approval.
Figure 3.
Description of term filters used to detect stomatitis-associated adverse events. The OTT, CTT, and SAMT filters were defined to screen for stomatitis-associated AEs for each drug. The OTT filter differed for each drug, as it was based on the specific terms used during the respective registration trial. Created in BioRender. Kaja, S. (2025)
https://BioRender.com/alglb8u.
Figure 3.
Description of term filters used to detect stomatitis-associated adverse events. The OTT, CTT, and SAMT filters were defined to screen for stomatitis-associated AEs for each drug. The OTT filter differed for each drug, as it was based on the specific terms used during the respective registration trial. Created in BioRender. Kaja, S. (2025)
https://BioRender.com/alglb8u.
Figure 4.
Flowchart of FAERS data extraction and filtering for stomatitis analysis. The FAERS database up to Q1 2025 was screened, with duplicate case IDs removed. Adverse event reports were retrieved for alpelisib/PIQRAY
®, capivasertib/TRUQAP™, everolimus/AFINITOR
®, and palbociclib/IBRANCE
®. Stomatitis-associated cases were then identified using three predefined filters—Original Trial Terms (OTT), Stomatitis-Associated Main Terms (SAMT), and Comprehensive Trial Terms (CTT). The number of reports identified for each drug and filter is shown. Created in BioRender. Kaja, S. (2025)
https://BioRender.com/pmx1mls.
Figure 4.
Flowchart of FAERS data extraction and filtering for stomatitis analysis. The FAERS database up to Q1 2025 was screened, with duplicate case IDs removed. Adverse event reports were retrieved for alpelisib/PIQRAY
®, capivasertib/TRUQAP™, everolimus/AFINITOR
®, and palbociclib/IBRANCE
®. Stomatitis-associated cases were then identified using three predefined filters—Original Trial Terms (OTT), Stomatitis-Associated Main Terms (SAMT), and Comprehensive Trial Terms (CTT). The number of reports identified for each drug and filter is shown. Created in BioRender. Kaja, S. (2025)
https://BioRender.com/pmx1mls.
Figure 5.
Disproportionality analysis of stomatitis-associated terms in FAERS. (A) Heatmap showing reporting odds ratios (ROR) for individual stomatitis-related terms across capivasertib, alpelisib, palbociclib, and everolimus. (B) Heatmap showing aggregated ROR values for stomatitis detected using the Original Trial Terms (OTT), Stomatitis-Associated Main Terms (SAMT), and Comprehensive Trial Terms (CTT) filters. (C) Heatmap showing proportional reporting ratios (PRR) for individual stomatitis-related terms across capivasertib, alpelisib, palbociclib, and everolimus. (D) Heatmap showing aggregated PRR values for the different filters. Color intensity reflects ROR magnitude.
Figure 5.
Disproportionality analysis of stomatitis-associated terms in FAERS. (A) Heatmap showing reporting odds ratios (ROR) for individual stomatitis-related terms across capivasertib, alpelisib, palbociclib, and everolimus. (B) Heatmap showing aggregated ROR values for stomatitis detected using the Original Trial Terms (OTT), Stomatitis-Associated Main Terms (SAMT), and Comprehensive Trial Terms (CTT) filters. (C) Heatmap showing proportional reporting ratios (PRR) for individual stomatitis-related terms across capivasertib, alpelisib, palbociclib, and everolimus. (D) Heatmap showing aggregated PRR values for the different filters. Color intensity reflects ROR magnitude.
Figure 6.
Percentage of stomatitis-associated reports identified for each drug in FAERS. The percentage of reports for capivasertib, alpelisib, palbociclib, and everolimus associated with stomatitis is shown. Cases were categorized according to predefined filters: Stomatitis-Associated Main Terms (SAMT), Comprehensive Trial Terms (CTT), or the single term “stomatitis.” Absolute case counts for each filter are indicated within the bars.
Figure 6.
Percentage of stomatitis-associated reports identified for each drug in FAERS. The percentage of reports for capivasertib, alpelisib, palbociclib, and everolimus associated with stomatitis is shown. Cases were categorized according to predefined filters: Stomatitis-Associated Main Terms (SAMT), Comprehensive Trial Terms (CTT), or the single term “stomatitis.” Absolute case counts for each filter are indicated within the bars.
Table 1.
Stomatitis-associated adverse event reports in FAERS by drug and search term.
Table 1.
Stomatitis-associated adverse event reports in FAERS by drug and search term.
| |
|
|
Term |
Capivasertib/
TRUQAP®
|
Alpelisib/
PIQRAY®
|
Palbociclib/
IBRANCE®
|
Everolimus/
AFINITOR®
|
| |
|
|
Total number of reports |
1002 |
8038 |
110,963 |
35,697 |
| |
|
|
Stomatitis |
13 |
362 |
4103 |
3247 |
| |
Aphthous
Ulcer |
0 |
22 |
218 |
279 |
| |
Mouth
Ulceration |
0 |
24 |
374 |
558 |
| |
|
Lip Ulceration |
0 |
1 |
6 |
14 |
| |
|
Glossodynia |
1 |
31 |
353 |
167 |
| |
|
Glossitis |
0 |
4 |
53 |
28 |
| |
|
Cheilitis |
0 |
16 |
103 |
74 |
| |
|
Oral Pain |
6 |
150 |
1242 |
775 |
| |
|
Gingival Pain |
1 |
17 |
215 |
79 |
| |
|
Oral
Discomfort |
1 |
23 |
141 |
91 |
| |
|
Oropharyngeal Pain |
2 |
44 |
1119 |
344 |
| |
|
|
Total Reports: Stomatitis |
13 |
362 |
4103 |
3247 |
| |
|
|
Total Reports: SAMT |
13 |
408 |
4695 |
4084 |
| |
|
|
Total Reports: CTT |
24 |
694 |
7927 |
5656 |