Submitted:
03 September 2025
Posted:
04 September 2025
You are already at the latest version
Abstract
Keywords:
1. Introduction
2. Materials and Methods
2.1. Patients
2.2. Biochemical Parameters and Cytokines
2.3. MicroRNA RT qPCR Assays
2.4. Statistical Analysis
2.5. Ethical Declaration
3. Results
4. Discussion
5. Conclusions
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Acknowledgments
Conflicts of Interest
Appendix A
Appendix B
References
- Magliano, D. J.; Boyko, E. J. IDF Diabetes Atlas, 10th edition. scientific committee. Brussels: International Diabetes Federation. 2021.
- O’Hearn, M.; Lara-Castor, L.; Cudhea, F.; Miller, V.; Reedy, J.; Shi, P.; Zhang, J.; Wong, J.B.; Economos, C.D.; Micha, R.; Mozaffarian, D. Incident type 2 diabetes attributable to suboptimal diet in 184 countries. Nat Med. 2023;29(4):982-995. [CrossRef]
- Instituto Nacional de Estadística y Censos (INEC). Boletín Técnico Registro Estadístico de Defunciones Generales. 2020.
- World Health Organization (WHO). Definition, diagnosis, and classification of Diabetes Mellitus and its Complications. World Health Organization (WHO), Department of Noncommunicable Disease Survelliance. 1999. pp. 1–66.
- Alicic RZ, Rooney MT, Tuttle KR. Diabetic Kidney Disease: Challenges, Progress, and Possibilities. Clin J Am Soc Nephrol CJASN. 2017 Dec 7;12(12):2032–45.
- Reidy K, Kang HM, Hostetter T, Susztak K. Molecular mechanisms of diabetic kidney disease. J Clin Invest. 2014 Jun;124(6):2333–40.
- Donate-Correa, J.; Ferri, C.M.; Sanchez-Quintana, F.; Perez-Castro, A.; Gonzalez-Luis, A.; Martín-Núñez, E. ; Mora-Fernandez,C.; Navarro-Gonzalez, J.F. Inflammatory Cytokines in Diabetic Kidney Disease : Pathophysiologic and Therapeutic Implications. Front Med (Lausanne). 2021;7. [CrossRef]
- Pérez-Pevida B, Llavero M, Gargallo J, Escalada J. Complicaciones microvasculares de la diabetes. Med - Programa Form Médica Contin Acreditado. 2016 Sep 1;12(17):958–70.
- Ritz E, Rychlík I, Locatelli F, Halimi S. End-stage renal failure in type 2 diabetes: A medical catastrophe of worldwide dimensions. Am J Kidney Dis Off J Natl Kidney Found. 1999 Nov;34(5):795–808.
- Wada J, Makino H. Inflammation and the pathogenesis of diabetic nephropathy. Clin Sci Lond Engl 1979. 2013 Feb;124(3):139–52.
- Tang SCW, Yiu WH. Innate immunity in diabetic kidney disease. Nat Rev Nephrol. 2020 Apr;16(4):206–22.
- Zhao L, Zou Y, Liu F. Transforming Growth Factor-Beta1 in Diabetic Kidney Disease. Front Cell Dev Biol. 2020 Mar 24;8:187.
- Hildebrandt X, Ibrahim M, Peltzer N. Cell death and inflammation during obesity: “Know my methods, WAT(son).” Cell Death Differ. 2023 Feb;30(2):279–92.
- Liu SY, Chen J, Li YF. Clinical significance of serum interleukin-8 and soluble tumor necrosis factor-like weak inducer of apoptosis levels in patients with diabetic nephropathy. J Diabetes Investig. 2018 Sep;9(5):1182–8.
- Hung PH, Hsu YC, Chen TH, Lin CL. Recent Advances in Diabetic Kidney Diseases: From Kidney Injury to Kidney Fibrosis. Int J Mol Sci. 2021 Nov 1;22(21):11857.
- Boldin MP, Taganov KD, Rao DS, Yang L, Zhao JL, Kalwani M, et al. miR-146a is a significant brake on autoimmunity, myeloproliferation, and cancer in mice. J Exp Med. 2011 Jun 6;208(6):1189–201.
- Chen S, Feng B, Thomas AA, Chakrabarti S. miR-146a regulates glucose induced upregulation of inflammatory cytokines extracellular matrix proteins in the retina and kidney in diabetes. PloS One. 2017;12(3):e0173918.
- O’Connell RM, Kahn D, Gibson WSJ, Round JL, Scholz RL, Chaudhuri AA, et al. MicroRNA-155 promotes autoimmune inflammation by enhancing inflammatory T cell development. Immunity. 2010 Oct 29;33(4):607–19.
- Prieto I, Kavanagh M, Jimenez-Castilla L, Pardines M, Lazaro I, Herrero del Real I, et al. A mutual regulatory loop between miR-155 and SOCS1 influences renal inflammation and diabetic kidney disease. Mol Ther Nucleic Acids. 2023 Sep 27;34:102041.
- D’Marco L, Puchades MJ, Gorriz JL, Romero-Parra M, Lima-Martínez M, Soto C, et al. Epicardial Adipose Tissue, Adiponectin and Leptin: A Potential Source of Cardiovascular Risk in Chronic Kidney Disease. Int J Mol Sci. 2020 Feb 1;21(3):978.
- Korczynska J, Czumaj A, Chmielewski M, Swierczynski J, Sledzinski T. The Causes and Potential Injurious Effects of Elevated Serum Leptin Levels in Chronic Kidney Disease Patients. Int J Mol Sci. 2021 Apr 28;22(9):4685.
- Zorena K, Jachimowicz-Duda O, Ślęzak D, Robakowska M, Mrugacz M. Adipokines and Obesity. Potential Link to Metabolic Disorders and Chronic Complications. Int J Mol Sci. 2020 May 18;21(10):3570.
- American Diabetes Association. Diagnosis and Classification of Diabetes Mellitus. Diabetes Care. 2011 Jan;34(Suppl 1):S62.
- Knijff EM, Breunis MN, van Geest MC, Kupka RW, Ruwhof C, de Wit HJ, et al. A relative resistance of T cells to dexamethasone in bipolar disorder. Bipolar Disord. 2006 Dec;8(6):740–50.
- Pérez-Galarza J, Baldeón L, Franco OH, Muka T, Drexhage HA, Voortman T, et al. Prevalence of overweight and metabolic syndrome, and associated sociodemographic factors among adult Ecuadorian populations: the ENSANUT-ECU study. J Endocrinol Invest. 2021 Jan;44(1):63–74.
- Hotamisligil GS, Shargill NS, Spiegelman BM. Adipose expression of tumor necrosis factor-alpha: direct role in obesity-linked insulin resistance. Science. 1993 Jan 1;259(5091):87–91.
- Boden, G. Obesity, insulin resistance and free fatty acids. Curr Opin Endocrinol Diabetes Obes. 2011 Apr;18(2):139–43.
- ResearchGate [Internet]. [cited 2025 Sep 1]. (PDF) Interleukin 8 and diabetic nephropathy. Available from: https://www.researchgate.net/publication/284186255_Interleukin_8_and_diabetic_nephropathy.
- Assessment of Interleukin (8) in Type 2 Diabetes Mellitus. ResearchGate [Internet]. 2025 Aug 6 [cited 2025 Sep 1]; Available from: https://www.researchgate.net/publication/367929534_Assessment_of_Interleukin_8_in_Type_2_Diabetes_Mellitus.
- Loretelli C, Rocchio F, D’Addio F, Ben Nasr M, Castillo-Leon E, Dellepiane S, et al. The IL-8-CXCR1/2 axis contributes to diabetic kidney disease. Metabolism. 2021 Aug;121:154804.
- Mirza S, Hossain M, Mathews C, Martinez P, Pino P, Gay JL, et al. Type 2-diabetes is associated with elevated levels of TNF-alpha, IL-6 and adiponectin and low levels of leptin in a population of Mexican Americans: a cross-sectional study. Cytokine. 2012 Jan;57(1):136–42.
- Feigerlová E, Battaglia-Hsu SF. IL-6 signaling in diabetic nephropathy: From pathophysiology to therapeutic perspectives. Cytokine Growth Factor Rev. 2017 Oct;37:57–65.
- Jo HA, Kim JY, Yang SH, Han SS, Joo KW, Kim YS, et al. The role of local IL6/JAK2/STAT3 signaling in high glucose-induced podocyte hypertrophy. Kidney Res Clin Pract. 2016 Dec;35(4):212–8.
- Kim DI, Park SH. Sequential signaling cascade of IL-6 and PGC-1α is involved in high glucose-induced podocyte loss and growth arrest. Biochem Biophys Res Commun. 2013 Jun 14;435(4):702–7.
- Hanai K, Babazono T, Mugishima M, Yoshida N, Nyumura I, Toya K, et al. Association of serum leptin levels with progression of diabetic kidney disease in patients with type 2 diabetes. Diabetes Care. 2011 Dec;34(12):2557–9.
- Wilson C, Nelson R, Nicolson M, Pratley R. Plasma leptin concentrations: no difference between diabetic Pima Indians with and without nephropathy. Diabetologia. 1998 Jul;41(7):861–2.
- Lee JY, Yang JW, Han BG, Choi SO, Kim JS. Adiponectin for the treatment of diabetic nephropathy. Korean J Intern Med. 2019 May;34(3):480–91.
- Jia T, Carrero JJ, Lindholm B, Stenvinkel P. The complex role of adiponectin in chronic kidney disease. Biochimie. 2012 Oct;94(10):2150–6.
- Szostak J, Gorący A, Durys D, Dec P, Modrzejewski A, Pawlik A. The Role of MicroRNA in the Pathogenesis of Diabetic Nephropathy. Int J Mol Sci. 2023 Mar 25;24(7):6214.
- Baldeón R L, Weigelt K, de Wit H, Ozcan B, van Oudenaren A, Sempértegui F, et al. Decreased serum level of miR-146a as sign of chronic inflammation in type 2 diabetic patients. PloS One. 2014;9(12):e115209.
- Xie Y, Chu A, Feng Y, Chen L, Shao Y, Luo Q, et al. MicroRNA-146a: A Comprehensive Indicator of Inflammation and Oxidative Stress Status Induced in the Brain of Chronic T2DM Rats. Front Pharmacol. 2018;9:478.
- Ghaffari M, Razi S, Zalpoor H, Nabi-Afjadi M, Mohebichamkhorami F, Zali H. Association of MicroRNA-146a with Type 1 and 2 Diabetes and their Related Complications. J Diabetes Res. 2023;2023:2587104.
- Bhatt K, Lanting LL, Jia Y, Yadav S, Reddy MA, Magilnick N, et al. Anti-Inflammatory Role of MicroRNA-146a in the Pathogenesis of Diabetic Nephropathy. J Am Soc Nephrol JASN. 2016 Aug;27(8):2277–88.
- Gilyazova I, Asadullina D, Kagirova E, Sikka R, Mustafin A, Ivanova E, et al. MiRNA-146a—A Key Player in Immunity and Diseases. Int J Mol Sci. 2023 Aug 14;24(16):12767.
- Maratni NPT, Saraswati MR, Ayu Dewi NN, Suastika K. MIRNA146a And Diabetes-Related Complications: A Review. Curr Diabetes Rev. 2023;19(9):e141022209958.
- Rottiers V, Näär AM. MicroRNAs in Metabolism and Metabolic Disorders. Nat Rev Mol Cell Biol. 2012 Mar 22;13(4):239–50.
- Baldeón R L, Weigelt K, de Wit H, Ozcan B, van Oudenaren A, Sempértegui F, et al. Type 2 Diabetes Monocyte MicroRNA and mRNA Expression: Dyslipidemia Associates with Increased Differentiation-Related Genes but Not Inflammatory Activation. PloS One. 2015;10(6):e0129421.
- Ghuwalewala S, Ghatak D, Das S, Roy S, Das P, Butti R, et al. MiRNA-146a/AKT/β-Catenin Activation Regulates Cancer Stem Cell Phenotype in Oral Squamous Cell Carcinoma by Targeting CD24. Front Oncol. 2021;11:651692.
- Wu D, Xi QY, Cheng X, Dong T, Zhu XT, Shu G, et al. miR-146a-5p inhibits TNF-α-induced adipogenesis via targeting insulin receptor in primary porcine adipocytes. J Lipid Res. 2016 Aug;57(8):1360–72.
- Ren Y, Zhao H, Yin C, Lan X, Wu L, Du X, et al. Adipokines, Hepatokines and Myokines: Focus on Their Role and Molecular Mechanisms in Adipose Tissue Inflammation. Front Endocrinol. 2022;13:873699.
| NDC (n=49) | C-T2D (n=50) | NC-T2D (n=50) | DKD (n=49) | p-value | ||
|---|---|---|---|---|---|---|
| Female (%) | 39(79.52) | 40 (80.0) | 45 (90.0) | 45(91.84) | 0.175 | |
| Male (%) | 10(20.41) | 10(20.0) | 5(10.0) | 4(8.16) | ||
|
Age (years) |
59 ± 8 |
60 ± 8 |
59 ± 10 |
72 ± 11 |
0.000 NDC vs. DKD p=0.000 C-T2D vs. DKD p=0.000 NC-T2D vs. DKD p=0.000 |
|
| Exercise | Yes | 6 (12.24) | 41 (83.67) | 38 (79.17) | 39 (79.59) | 0.649 |
| Not | 43 (87.76) | 8 (16.33) | 10 (20.83) | 10 (20.41) | ||
| Smoker | Yes | 7 (14.29) | 4 (8.16) | 6 (12.24) | 5 (10.20) | 0.795 |
| Not | 42 (85.71) | 45 (91.84) | 43 (87.76) | 44 (89.80) | ||
| Length of illness (years) | 8 ± 5 | 9 ± 7 | 16 ± 11 |
0.000 C-T2D vs. NC-T2D p=0.042 C-T2D vs. DKD p=0.000 NC-T2D vs. DKD p=0.000 |
||
| Age at diagnosis (years) | 53 ± 10 | 54 ± 12 | 52 ± 14 |
0.005 NC-T2D vs C-T2D p=0.018 NC-T2D vs. DKD p=0.012 C-T2D vs. DKD p=1.00 |
||
| Medication | Metformin | 39 (79.59) | 17 (36.17) | 3 (6.12) |
0.000 C-T2D vs. Metf p=0.000 DKD vs. Metf p=0.000 |
|
| Metformin/Gilbenclamide | 3 (6.12) | 12 (25.53) | 15 (30.61) | |||
| Insuline | 0 (0) | 1 (2.13) | 6 (12.24) | |||
| Insuline/Metformine | 7 (14.29) | 16 (34.04) | 23 (46.95) | |||
| Gilbenclamide/Insuline/Metformine | 0 (0) | 1 (2.13) | 2 (4.08) | |||
| Family history | Yes | 39 (79.59) | 32 (65.31) | 29 (58) | 26 (54.17) | 0.006 |
| Not | 10 (20.41) | 17 (34.69) | 21 (42) | 22 (45.83) | ||
| BMI (kg/m2) | 31.1 ± 4.2 | 30.8 ± 5.6 | 30.4 ± 4.4 | 27.2 ± 4.2 |
0.001 NDC vs. DKD p=0.007 C-T2D vs. DKD p=0.002 NC-T2D vs. DKD p=0.029 |
|
| SBP (mmHg) | 121 ± 12 | 121 ± 10 | 121 ± 12 | 124 ± 16 | 0.427 | |
| DBP (mmHg) | 74 ± 6 | 74 ± 7 | 73 ± 74.74 | 70 ± 8 |
0.03 NDC vs. DKD p=0.036 |
|
| Glucose (mg/dL) | 82 ± 9 | 100 ± 15 | 141 ± 84.84 | 161 ± 46 |
0.000 NDC vs. DKD p=0.000 C-T2D vs. DKD p=0.000 NC-T2D vs. DKD p=0.000 |
|
|
HbA1C (%) |
5.6 ± 0.5 |
5.8 ± 0.4 |
7.5 ± 0.3 |
8.8 ± 0.9 |
0.000 NDC vs. DKD p=0.000 C-T2D vs. DKD p=0.000 NC-T2D vs. DKD p=0.000 |
|
| Cholesterol (mg/dL) | 193 ± 37 | 185 ± 38 | 174 ± 37.37 | 200 ± 37 | 0.136 | |
| Triglycerides (mg/dL) | 174 ± 68 | 161 ± 85 | 168 ± 68.68 | 171 ± 76 | 0.801 | |
| HDL (mg/dL) | 47 ± 13 | 48 ± 10 | 45 ± 8 | 48 ± 13 | 0.653 | |
| LDL (mg/dL) | 106 ± 33 | 104 ± 35 | 92 ± 33 | 105 ± 31 | 0.369 | |
| SGOT (U/L) | 21.90 ± 12.96 | 22.35 ± 13.93 | 23.25 ± 10.23 | 21.00 ± 24.08 | 0.583 | |
| SGPT (U/L) | 12.85 ± 10.73 | 13.40 ± 7.61 | 15.20 ± 6.24 | 11.00 ± 7.21 | 0.657 | |
| Urea (mg/dL) | 33.00 ± 8.90 | 32.00 ± 10.16 | 27.50 ± 9.27 | 40.00 ± 45.01 |
0.000 NDC vs. NC-T2D p= 0.020 NC-T2D vs. DKD p=0.000 C-T2D vs. DKD p=0.002 |
|
| Creatine (mg/dL) | 0.90 ± 0.15 | 0.90 ± 0.15 | 0.85 ± 0.0 | 1.10 ± 1.02 |
0.000 NDC vs. DKD p=0.000 NC-T2D vs. DKD p=0.000 C-T2D vs. DKD p=0.002 |
|
| MDRD (mL/min) |
70.10 ± 11.04 | 73.35 ± 11.48 | 76.45 ± 10.75 | 52.80 ± 17.56 |
0.000 NDC vs. DKD p=0.000 C-T2D vs. DKD p=0.000 NC-T2D vs. DKD p=0.000 |
|
| Variable | NDC | C-T2D | NC-T2D | DKD | p-value |
|---|---|---|---|---|---|
| IL-8 (pg/mL) | 14.91 ± 12.05 | 30.66 ± 27.45 | 30.38 ± 27.94 | 30.66 ± 24.78 |
0.000 NDC vs. C-T2D p=0.000 NDC vs. NC-T2D p=0.000 NDC vs. DKD p=0.000 |
| IL-6 (pg/mL) | 3.09 ± 10.63 | 11.62 ± 9.10 | 10.48± 14.13 | 12.16 ± 13.29 |
0.000 NDC vs. C-T2D p=0.001 NDC vs. NC-T2D p=0.001 NDC vs. DKD p=0.000 |
| TNF-α (pg/mL) | 9.28 ± 3.17 |
6.73 ± 3.43 | 6.90 ± 2.70 | 5.58 ± 3.94 |
0.001 NDC vs. C-T2D p=0.011 NDC vs. NC-T2D p=0.011 NDC vs. DKD p=0.002 |
| Leptin (ng/mL) | 1.32 ± 4.46 | 11.14 ± 6.96 | 9.84 ± 7.85 | 8.65 ± 8.12 |
0.000 NDC vs. C-T2D p=0.000 NDC vs. NC-T2D p=0.000 NDC vs. DKD p=0.000 |
| Adiponectin (ug/mL) | 6.17 ± 5.54 | 9.30 ± 5.43 | 6.65 ± 4.12 | 11.30 ± 6.55 |
0.000 NDC vs. C-T2D p=0.006 NDC vs. NC-T2D p=0.000 NDC vs. DKD p=0.001 |
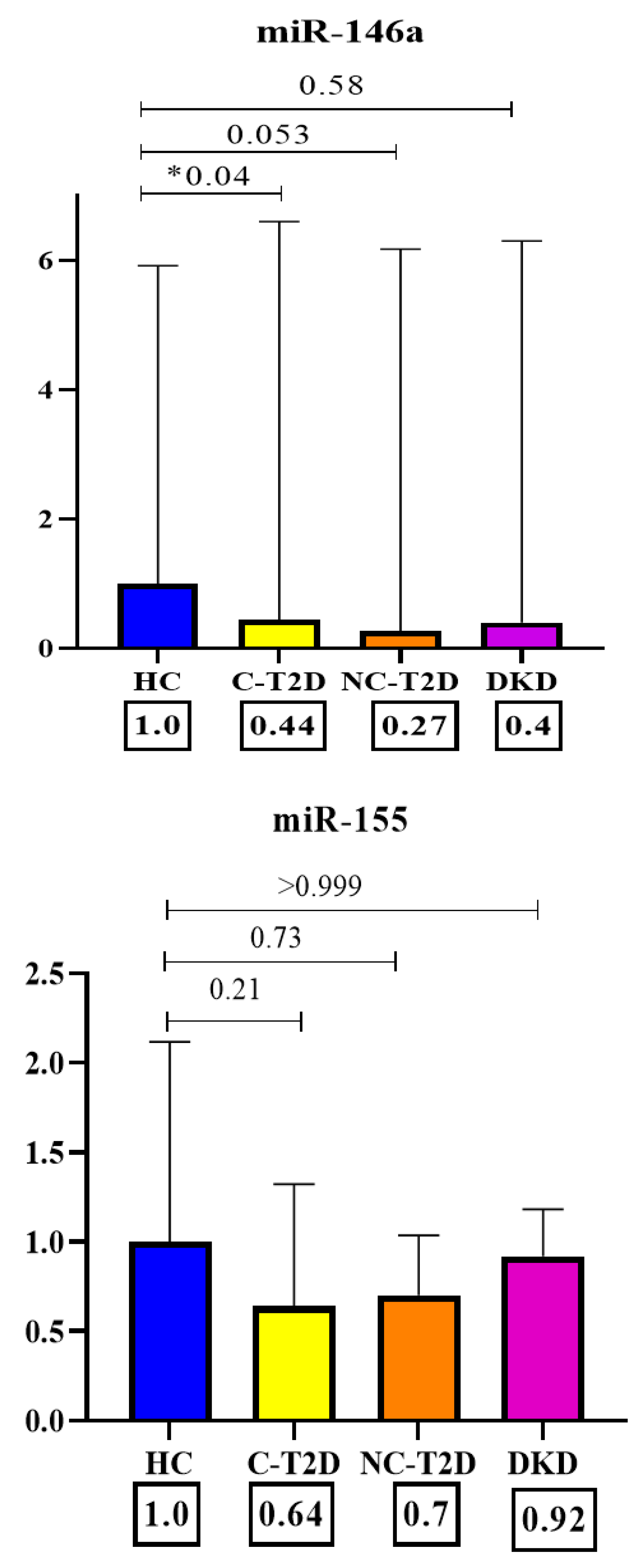
| miR-146a (CT) | 6.09 ± 21.44 | 23.67 ± 34.30 | 15.57 ± 32.87 | 12.70 ± 25.50 |
0.0299 NDC vs. C-T2D p=0.041 NDC vs. NC-T2D p=0.053 NDC vs. DKD p=0.583 |
| miR-155 (CT) | 0.82 ± 5 | 2.05 ± 3.67 | 1.68 ± 1.87 | 1.06 ± 1.44 | 0.1529 NDC vs. C-T2D p=0.213 NDC vs. NC-T2D p=0.734 NDC vs. DKD p=0.999 |
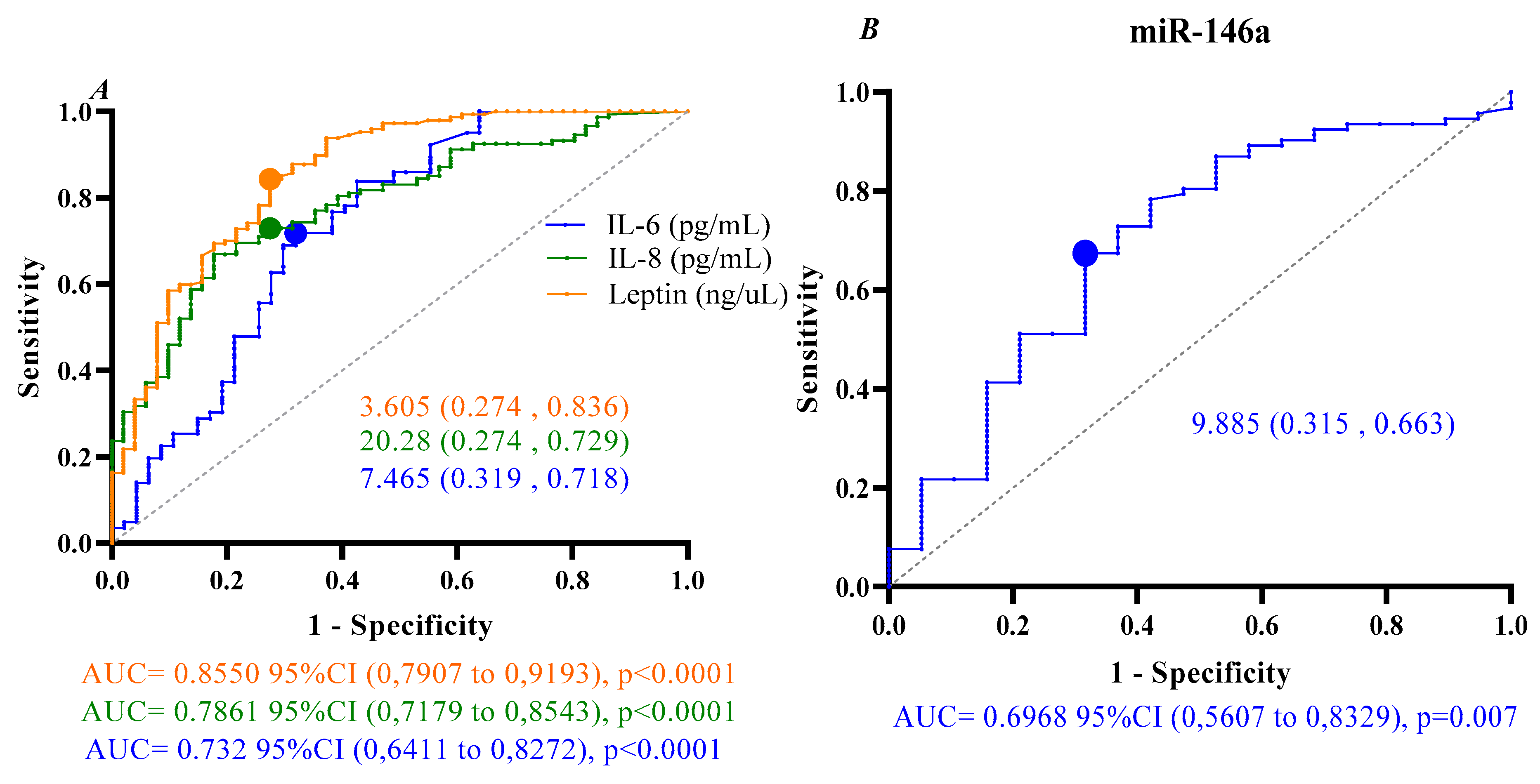
| Variable | p-value | B | OR | OR 95% CI | |
|---|---|---|---|---|---|
| LI | HI | ||||
| IL-8 ≥ 20.28 (pg/mL) | 0.000 | 1.907 | 6.733 | 3.307 | 13.709 |
| IL-6 ≥ 7.465 (pg/mL) | 0.001 | 1.490 | 4.436 | 2.266 | 8.987 |
| Leptin ≥ 3.605 (ng/mL) | 0.001 | 2.622 | 13.765 | 6.474 | 29.267 |
| miR-146a ≥ 9.885 (real expression) | 0.009 | 1.402 | 4.062 | 1.410 | 11.705 |
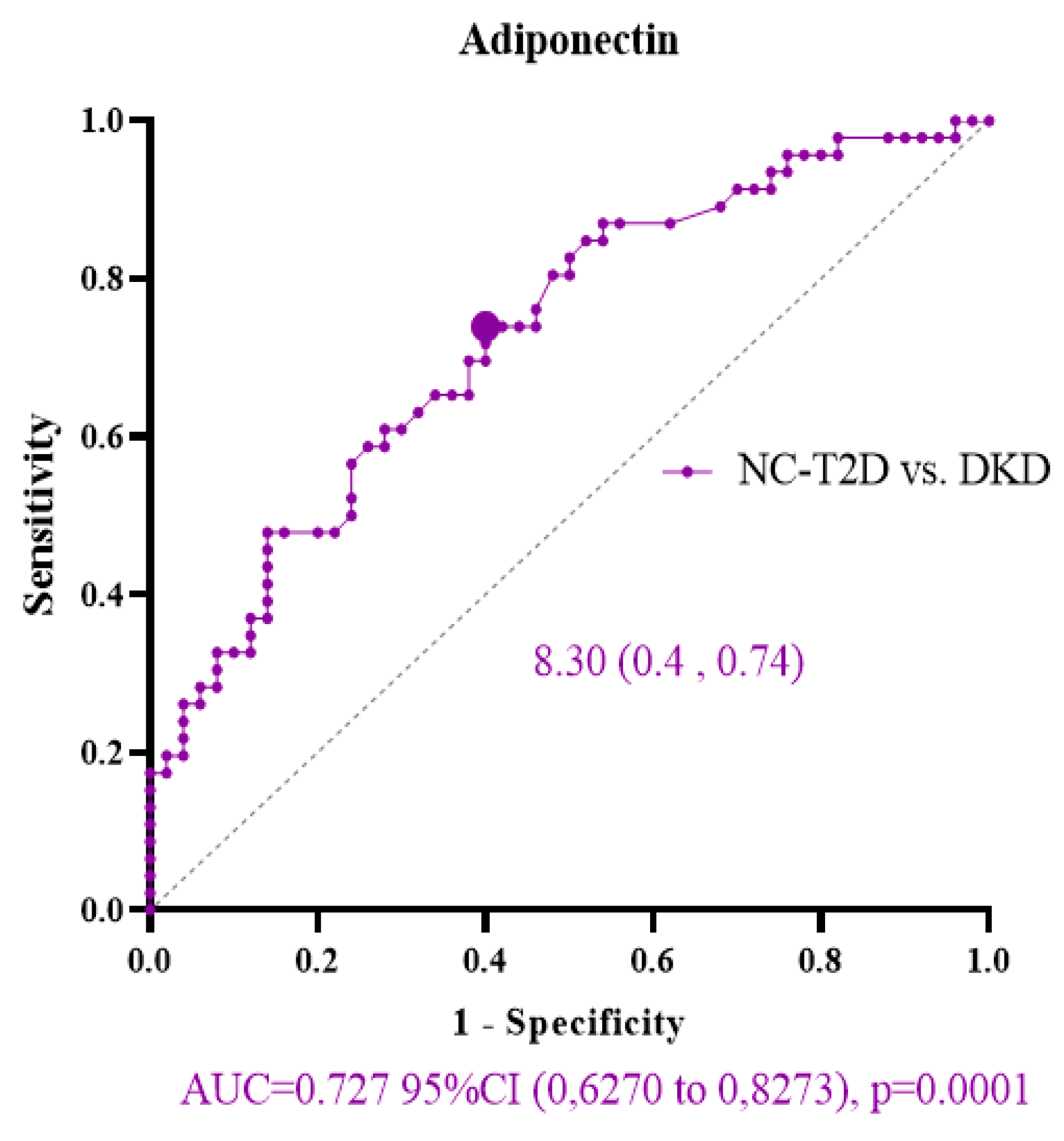
| Variable | p-value | B | OR | OR 95% CI | |
|---|---|---|---|---|---|
| LI | HI | ||||
| Adiponectin ≥ 8.30 (ug/mL) NC-T2D vs. DKD | 0.001 | 1.424 | 4.154 | 1.776 | 9.718 |
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2025 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (http://creativecommons.org/licenses/by/4.0/).





