1. Introduction
Nurse managers are pivotal in translating organizational policies into frontline healthcare operations. Their competencies—including supervision, staff development, communication, fiscal management, and strategic planning—directly affect workforce stability, patient safety, and quality of care. [
1,
2]. Globally, nursing shortages have intensified due to increased demand, staff burnout, and heightened turnover, a trend accelerated by the COVID-19 pandemic [
3,
4]. These workforce challenges have profound implications, including diminished patient outcomes, increased costs, and reduced organizational efficiency.
In Saudi Arabia, the healthcare system is undergoing significant transformation under Vision 2030, emphasizing leadership development, workforce sustainability, and quality improvement [
5,
6]. Nurse managers are central to achieving these goals; however, gaps often exist between managers’ self-perceived competencies and staff nurses’ perceptions, which may contribute to turnover intentions, reduced job satisfaction, and compromised care quality [
1,
3,
7].
While leadership competency is widely studied, few investigations have systematically explored perception gaps between managers and staff nurses in relation to retention, particularly in Middle Eastern healthcare settings. Studies addressing this misalignment are limited, highlighting a critical knowledge gap in understanding how leadership deficiencies directly influence turnover [
1,
3,
7].
This study addresses this gap by investigating perceived competency gaps in nurse leadership, their relationship to staff nurse turnover intentions, and the role of demographic characteristics, providing insights applicable globally.
1.1. Aim
To explore nurse manager competency gaps, their association with staff nurse turnover intentions, and the influence of demographic characteristics.
1.2. Research Questions:
What competency gaps do staff nurses perceive in their nurse managers?
How do nurse managers’ self-perceptions compare with staff nurses’ perceptions?
How are competency gaps associated with staff nurse turnover intentions?
Do demographic characteristics (age, experience, education) influence perceptions of competency gaps and turnover intention?
1.3. Theoretical and Conceptual Framework
The present study is grounded in a combination of leadership and behavioral theories that provide a comprehensive understanding of how nurse manager competencies affect staff nurse turnover intentions. The Three-Skills Approach to Management, originally proposed by Katz [
8], emphasizes that effective leadership requires a combination of technical, human, and conceptual skills [
8]. Technical skills reflect clinical knowledge and operational proficiency, human skills involve communication and interpersonal effectiveness, and conceptual skills encompass strategic thinking and problem-solving. In the context of nursing, these competencies are critical for ensuring safe, efficient, and high-quality care delivery. This framework supports the study by identifying the core competencies required for nurse managers to lead their teams effectively and highlights potential gaps that could influence staff retention.
Complementing this, the Transformational Leadership Theory [
9] underscores the importance of leaders who inspire, intellectually stimulate, and individually support their staff. Transformational leadership has been shown to foster engagement, commitment, and resilience among nursing personnel, which can directly influence staff satisfaction and intention to remain in their positions. The inclusion of this theory allows the study to examine not only the skills and tasks of nurse managers but also the relational and motivational aspects of leadership that shape nurses’ perceptions and behaviors.
Finally, the Theory of Planned Behavior (TPB) [
10] provides a behavioral lens for understanding how perceived leadership gaps translate into turnover intentions among staff nurses. TPB posits that behavioral intentions are influenced by attitudes, subjective norms, and perceived behavioral control. This study helps explain how staff nurses’ perceptions of their managers’ competencies influence their intention to leave and why demographic characteristics, such as experience, age, and education, might alter these perceptions. The integration of TPB ensures that the study addresses both the managerial competencies themselves and the cognitive processes that mediate how these competencies affect turnover behaviors.
By combining these three theoretical perspectives, the study establishes a robust framework to examine the mechanisms by which leadership competencies—or the lack thereof—influence workforce retention in nursing.
1.4. Conceptual Framework:
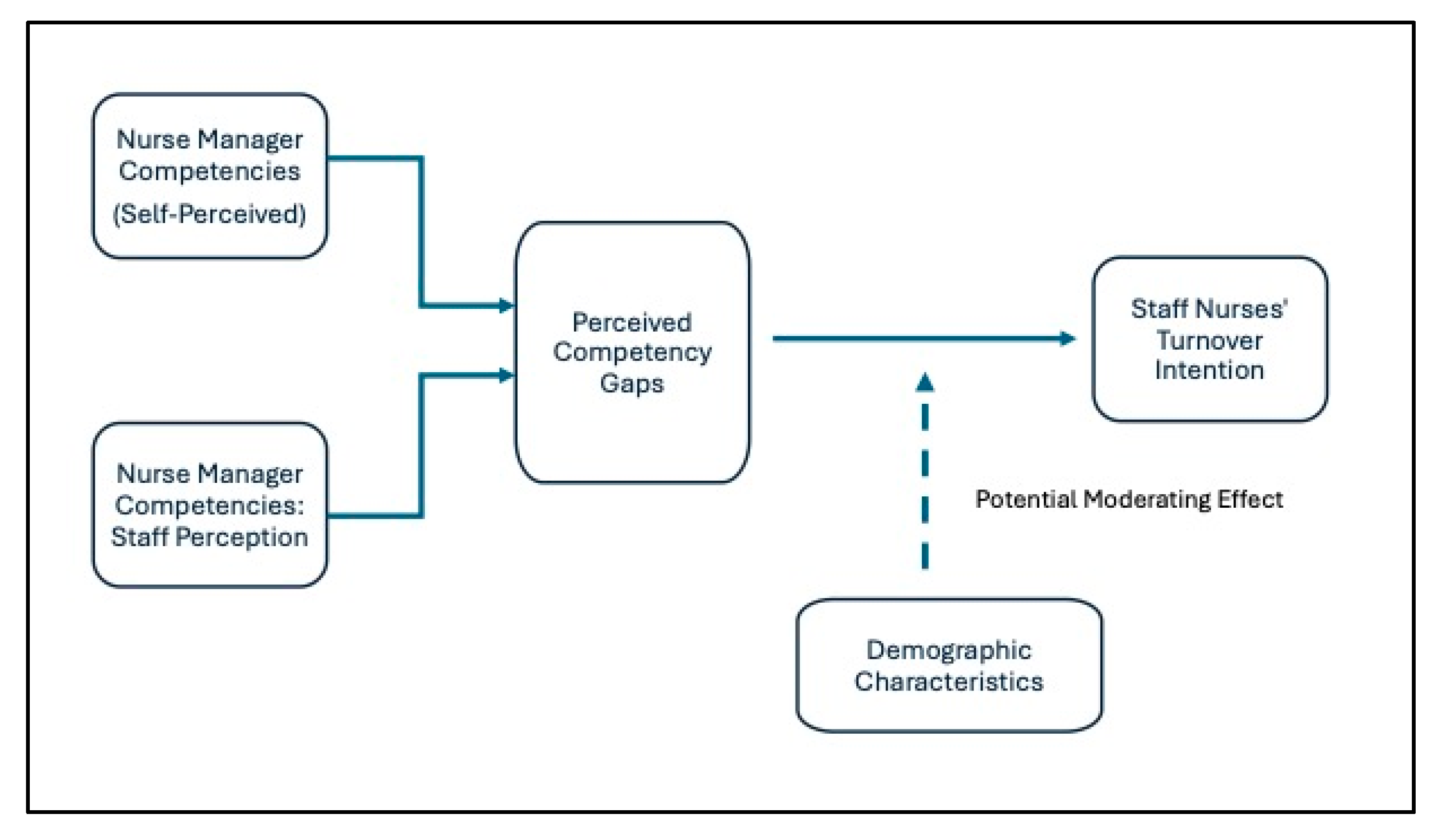
The conceptual framework of this study depicts the relationships among nurse manager competencies, perceived competency gaps, staff nurse turnover intention, and demographic characteristics as potential moderators. Nurse manager competencies—measured across domains such as recruitment, retention strategies, and supervisory responsibilities—form the independent variable. Perceived competency gaps, operationalized as differences between managers’ self-assessments and staff nurses’ perceptions, act as the primary explanatory variable influencing staff nurses’ turnover intentions, the dependent outcome.
Demographic characteristics—including age, experience, and education—are conceptualized as potential moderating factors that could influence the strength of the relationship between perceived gaps and turnover intention. For instance, less experienced nurses may be more sensitive to leadership deficiencies, which could intensify the impact of competency gaps on their intention to leave, whereas more experienced nurses may tolerate certain gaps. Although formal moderation analysis was not conducted in this study, incorporating demographics in the conceptual framework highlights avenues for future research to explore tailored interventions.
Figure 1 visually represents this framework: nurse manager competencies influence perceived gaps, which in turn affect turnover intention, with demographics positioned as potential moderators influencing the perceived gap–turnover link. This framework not only reflects the empirical focus of the study but also aligns with global and regional evidence suggesting that leadership gaps and individual nurse characteristics jointly shape retention outcomes.
2. Materials and Methods
2.1. Study Design and Setting
A cross-sectional, descriptive-correlational design was employed. Data were collected from two tertiary governmental hospitals located in Riyadh and Dammam, Saudi Arabia.
2.2. Participants
The study included 225 staff nurses and 171 nurse managers (n=396). Inclusion criteria required at least one year of experience, with staff nurses providing direct patient care and managers holding supervisory and administrative responsibilities. Participant characteristics, including age, gender, education, experience, and marital status, were collected (
Table 1).
2.3. Instruments
2.3.1. Nurse Manager Competency Inventory (NMCI): developed by DeOnna [11] and measures competencies across 11 domains (staff retention, recruitment, supervisory responsibilities, patient safety, quality improvement, professional practice models, fiscal planning, communication, community/organizational outreach, and self-development). It contains 93 items scored on a five-point Likert scale (1 = never, 5 = always). The NMCI has demonstrated high reliability (α = 0.93) and has been validated in previous studies [11,12,13].2.3.2. Expanded Multidimensional Turnover Intention Scale (EMTIS): developed by Ike et al. [14], and measures turnover intention across five dimensions: subjective social status, organizational culture, personal orientation, expectations, and career growth. It contains 25 items, rated on a five-point Likert scale, with higher scores indicating higher turnover intention. Reliability (α = 0.93) and validity have been confirmed [14].
2.4. Data Collection
Data were gathered using an electronic survey (e-survey) distributed to eligible participants through a secure online platform. Prior to survey administration, several steps were taken to ensure compliance with ethical, legal, and institutional requirements:
2.4.1. Instrument Permission: Approval was obtained from the original authors of the Nurse Manager Competency Inventory (NMCI) and the Expanded Multidimensional Turnover Intention Scale (EMTIS) to use and adapt these tools for the study. Written consent was secured, ensuring adherence to copyright regulations and proper acknowledgment of the instruments’ developers.2.4.2. Ethical Clearance: Formal approval was granted by the Institutional Review Board (IRB) of Health Sciences Colleges Research on Human Subjects, King Saud University, in compliance with national ethical standards for research involving human participants.2.4.3. Administrative Permissions: Official authorization was obtained from the administration of each participating hospital. The study objectives, methodology, and anticipated benefits were presented to nursing staff and hospital management to secure their cooperation and support during the data collection phase.
Following these approvals, the e-survey was sent to participants meeting the inclusion criteria via email. The invitation included a concise description of the study, assurance of anonymity, and a link to access the survey. Participants were required to provide electronic informed consent before proceeding. To maximize participation, a reminder was sent one week after the initial invitation, encouraging staff nurses to complete the survey and highlighting the importance of their input for improving nursing leadership practices and workforce policies.
2.5. Ethical Considerations
Ethical approval for this study was obtained from the Institutional Review Board (IRB) of Health Sciences Colleges Research on Human Subjects, King Saud University (IRB No. E-24-8856 on 26/6/2024). Before participation, informed consent was collected electronically, ensuring that participants were fully informed about the study’s objectives, procedures, and their rights, including the right to withdraw at any time without consequence.
The anonymity and confidentiality of participants were strictly maintained throughout data collection and analysis. All data were stored securely and encrypted, with access limited exclusively to the research team. To address the specific ethical considerations of electronic surveys, each participant was assigned a unique identifier, and responses were stored in a secure cloud-based platform compliant with regional and institutional data protection regulations.
The study adhered to ethical standards consistent with the Declaration of Helsinki, ensuring the protection of participants and the integrity of the research process.
2.6. Data Analysis
Data were analyzed using SPSS version 26. Descriptive statistics summarized participant demographics, competencies, and turnover intentions. Independent-sample t-tests compared managers’ self-perceptions with staff nurses’ perceptions. Pearson correlation coefficients examined relationships between competencies and turnover intentions. Multiple regression analyses evaluated the influence of demographic characteristics. Statistical significance was set at p < 0.05.
3. Results
Staff nurses reported lower scores for staff recruitment (M = 3.01, SD = 0.67), retention strategies (M = 2.98, SD = 0.65), and supervisory responsibilities (M = 3.10, SD = 0.69) compared to managers’ self-assessments (
Table 2). These differences indicate that managers may overestimate their performance in critical leadership domains. In practice, this misalignment can lead to inefficient staffing, higher turnover, and reduced morale, explaining why some units experience persistent shortages despite confident leadership.
Lower perceived competencies were significantly associated with higher turnover intentions: recruitment (r = -0.47, p < 0.001), retention strategies (r = -0.42, p < 0.001), and supervision (r = -0.39, p < 0.001) (
Table 3). In real-world terms, units where leadership competencies are perceived as weak are at higher risk of staff attrition, decreased team cohesion, and compromised patient outcomes.
Demographic factors influenced perceptions and turnover intention. Less experienced nurses (<5 years) and bachelor-prepared nurses reported larger competency gaps and higher turnover intentions. Age was inversely correlated with perceived gaps (r = -0.21, p = 0.03), indicating that younger nurses are more sensitive to leadership deficiencies.
4. Discussion
This study demonstrates that competency gaps in nurse leadership have direct and measurable effects on staff nurse turnover intentions. Among the competency domains, deficiencies in staff recruitment, retention strategies, and supervisory responsibilities were the most prominent. These results are congruent with international literature highlighting leadership quality as a key determinant of workforce stability [
1,
7], which found that inadequate managerial competencies were strongly associated with higher turnover intentions, reduced staff morale, and compromised unit performance. Alsadaan et al. and Goens & Giannotti similarly emphasized that transformational and competency-based leadership significantly influences nurses’ job satisfaction, retention, and patient safety outcomes [
1,
15].
The comparison between nurse managers’ self-perceptions and staff nurses’ evaluations highlights a critical misalignment, a phenomenon observed globally where managers often overestimate their effectiveness. In practical terms, this misalignment can result in staff nurses feeling unsupported, undervalued, or insufficiently guided, thereby increasing turnover intentions and contributing to chronic staffing challenges. These findings are aligned with Jooste & Cairns, Long & Sochalski, Moradi et al., Abd-Elmoghith & Abd-Elhady, and Perez-Gonzalez et al., who underscored the importance of feedback-informed leadership programs that integrate staff perceptions into competency assessments to identify and address hidden gaps [
12,
13,
16,
17,
18].
Demographic characteristics appear to influence both the perception of competency gaps and turnover intention, suggesting their potential moderating role. Less experienced nurses and those with higher educational attainment were more likely to detect leadership deficiencies and report higher turnover intentions. This aligns with findings from Falatah and Goens & Giannotti [
1,
3], indicating that novice nurses and highly educated staff may have elevated expectations for leadership support and organizational guidance. Age, experience, and education are therefore important considerations when developing tailored interventions, as these factors can alter the sensitivity to perceived competency gaps and the subsequent decision to remain in a position [
1,
3].
These findings have critical implications in the context of current healthcare challenges, particularly in post-pandemic environments characterized by staff shortages, high turnover, and increased workload pressures. Ineffective leadership in recruitment and retention contributes to persistent staffing gaps, higher stress among remaining staff, and potential compromises in patient care quality. Globally, healthcare systems are grappling with similar issues, with leadership gaps often undermining workforce resilience, engagement, and retention [
19,
20,
21,
22]. In the Gulf region, including Saudi Arabia, where Vision 2030 emphasizes healthcare transformation and workforce development, these findings highlight the urgent need for structured, competency-based leadership development programs that integrate continuous staff feedback and performance evaluation to enhance retention [
23,
24,
25].
The study further illuminates current phenomena in healthcare workforce dynamics, such as the high turnover of highly qualified nurses in critical care and high-acuity units. Perceived gaps in supervisory support, recruitment effectiveness, and retention measures contribute to rapid staff turnover, destabilizing teams and threatening patient safety. Addressing these gaps is therefore essential to foster organizational resilience, improve team cohesion, and sustain the quality of care in increasingly demanding healthcare environments.
Regionally, studies have shown that Saudi nurses often face challenges related to limited managerial support, inequitable workload distribution, and insufficient recognition, all of which can heighten turnover intentions. [
26,
27,
28]. Internationally, research in Europe and North America corroborates that perceived leadership deficiencies are associated with burnout, emotional exhaustion, and attrition, emphasizing the global relevance of these findings. [
7,
29,
30]. By identifying specific competency gaps and their differential effects across demographic groups, this study provides evidence-based guidance for leadership development initiatives that are sensitive to workforce composition and expectations.
Overall, this study underscores the need for targeted leadership interventions that address both skill-based competencies and staff perceptions. Feedback-informed, competency-driven leadership programs, combined with strategic recruitment, retention, and supervision initiatives, can reduce turnover intentions, enhance staff satisfaction, and support workforce sustainability. Tailoring these interventions to the needs of novice, highly educated, or younger nurses may maximize their effectiveness, ultimately contributing to higher organizational performance and better patient outcomes.
4.1. Limitations
Despite the valuable insights gained from this study, several limitations must be acknowledged. First, the cross-sectional design constrains the ability to infer causality between nurse manager competencies, perceived competency gaps, and staff nurse turnover intentions. This design prevents the identification of changes over time, such as how perceptions of leadership or turnover intentions might evolve as nurses gain experience, encounter new organizational policies, or face prolonged crises. Future longitudinal studies could provide a more nuanced understanding of these dynamics, offering insight into how leadership perceptions and retention intentions fluctuate across different stages of professional development and organizational change.
Second, the study relied on self-reported data, which may be subject to various biases, including social desirability or response bias. Staff nurses and nurse managers might have unintentionally over- or under-reported competencies or perceptions, potentially affecting the accuracy of the findings. Future research could address this limitation by incorporating mixed methods approaches, such as structured interviews, focus groups, or observational assessments, to validate and enrich self-reported data.
Third, the study was conducted in two tertiary governmental hospitals located in Saudi Arabia, which may limit the generalizability of the findings. While these hospitals represent significant clinical settings and provide insight applicable to similar healthcare environments in the region, the results may not fully reflect dynamics in smaller facilities, private hospitals, or healthcare systems in other countries. Expanding the geographic and institutional scope in future research would enhance generalizability and provide broader insights into how organizational structure, resource availability, and regional healthcare policies influence competency gaps and turnover intentions.
Finally, while the study focused on nurse manager competencies and selected demographic characteristics, other potentially influential factors were not examined in depth. Variables such as organizational culture, staffing ratios, workload, support systems, and external stressors may interact with perceived competency gaps, shaping turnover intentions and staff satisfaction. Future research should explore these additional factors to provide a more holistic understanding of the determinants of nurse retention and workforce stability, particularly in high-pressure or crisis-prone healthcare settings.
4.2. Implications and Recommendations:
The findings of this study have important implications for nursing practice, healthcare management, education, and future research. They highlight the critical role of nurse leadership competencies in shaping workforce stability and the necessity of addressing gaps to enhance staff retention and patient care quality.
4.2.1. Implications for Nursing Practice
Healthcare organizations should implement structured, competency-based leadership development programs that target the domains identified as gaps in this study, particularly staff recruitment, retention strategies, and supervisory responsibilities. These programs should be tailored to different staff groups, recognizing that novice and highly educated nurses may be more sensitive to leadership deficiencies.
Feedback-informed leadership evaluation systems can be instituted, whereby staff nurses’ perceptions are systematically collected and used to guide managerial development. This approach ensures that leadership improvements are aligned with the actual needs and expectations of the nursing workforce.
Nurse managers should engage in continuous professional development focused on both technical skills (operational and clinical competencies) and relational skills (communication, mentoring, and motivational leadership), which are essential for fostering a supportive work environment and enhancing nurse satisfaction.
4.2.2. Implications for Healthcare Policy
Policymakers can leverage these findings to establish national competency frameworks for nurse managers, integrating standardized assessment, evaluation, and certification processes. Such frameworks will help ensure leadership quality across healthcare institutions and support workforce sustainability in the long term.
Retention strategies should be context-specific, recognizing differences in workforce demographics. For instance, targeted mentorship and recognition programs for less experienced nurses or newly qualified staff may mitigate turnover risks in critical care and high-acuity units.
4.2.3. Implications for Nursing Education
Nursing curricula should incorporate leadership development modules that prepare future nurse managers for the challenges of contemporary healthcare environments, emphasizing practical skills in supervision, retention strategies, and staff recruitment.
Simulation-based and scenario-driven training can provide prospective nurse managers with opportunities to practice decision-making, conflict resolution, and team leadership in safe, controlled environments, bridging the gap between theory and real-world practice.
4.2.4. Implications for Future Research
Future studies should explore the moderating effects of demographic characteristics (age, experience, education) through formal moderated regression analyses to understand how these factors influence the relationship between perceived leadership competency gaps and turnover intention.
Longitudinal studies are recommended to examine changes in competency perceptions and turnover intention over time, particularly in the context of healthcare transformations or crises such as pandemics.
Comparative studies across multiple countries or regions could investigate cultural and organizational influences on leadership perception, competency gaps, and retention outcomes, providing insights for global nursing workforce planning.
4.2.4. Actionable Recommendations
Develop customized leadership development initiatives focusing on weak competency domains identified in this study.
Implement regular staff feedback mechanisms to monitor leadership effectiveness and identify emerging competency gaps.
Tailor retention strategies considering staff demographics to maximize engagement and reduce turnover risk.
Promote a culture of continuous improvement in nurse leadership, integrating evidence-based strategies and benchmarking against best practices both regionally and internationally.
5. Conclusions
This study demonstrates that perceived gaps in nurse leadership competencies are a significant determinant of staff nurse turnover intentions. Deficiencies in recruitment, retention strategies, and supervisory responsibilities emerged as critical areas influencing workforce stability. Furthermore, demographic characteristics such as age, experience, and education may shape staff sensitivity to these gaps, suggesting the need for tailored leadership interventions.
Addressing these competency gaps through targeted, evidence-based leadership development programs can enhance staff retention, improve team cohesion, and strengthen workforce sustainability. These interventions are especially important in high-pressure healthcare settings and during periods of systemic transformation, such as those observed in the post-pandemic era.
The findings have both regional and global relevance, informing strategies to optimize nurse leadership effectiveness, reduce turnover, and maintain high-quality patient care. Future research should explore longitudinal changes in perceptions of managerial competencies, examine additional organizational and environmental factors, and evaluate the effectiveness of tailored interventions to ensure the long-term stability and resilience of the nursing workforce.
Author Contributions
Conceptualization, H.A. and D.A.; methodology, H.A.; software, D.A.; validation, H.A. and D.A.; formal analysis, D.A.; investigation, D.A.; resources, D.A.; data curation, H.A..; writing—original draft preparation, H.A.; writing—review and editing, H.A.; visualization, D.A.; supervision, H.A.; project administration, H.A.; funding acquisition, H.A. All authors have read and agreed to the published version of the manuscript.
Funding
This research was funded by the Ongoing Research Funding Program for Project number (ORF-FT2025-xxx), King Saud University, Riyadh, Saudi Arabia.
Institutional Review Board Statement
The study was conducted in accordance with the Declaration of Helsinki and approved by the Institutional Review Board of King Saud University, Riyadh, Saudi Arabia (protocol code XXX and date of approval).
Informed Consent Statement
Informed consent was obtained from all participants involved in the study.
Data Availability Statement
The data that support the findings of this study are available from the corresponding author upon reasonable request.
Acknowledgments
The authors extend their appreciation to the Ongoing Research Funding Program – Fast Track for Project number (ORF-FT2025-xxx), at King Saud University, for supporting this research project.
Conflicts of Interest
The authors declare no conflicts of interest.
Abbreviations
The following abbreviations are used in this manuscript:
| NMCI |
Nurse Manager Competency Inventory |
| EMTIS |
Expanded Multidimensional Turnover Intention Scale |
| TPB |
Theory of Planned Behavior |
References
- Goens, B.; Giannotti, N. Transformational Leadership and Nursing Retention: An Integrative Review. Nursing Research and Practice 2024, 3179141. [Google Scholar] [CrossRef]
- Wang, S.; Tong, J.; Wang, Y.; Zhang, D. A Study on Nurse Manager Competency Model of Tertiary General Hospitals in China. International Journal of Environmental Research and Public Health. 2022, 19, 8513. [Google Scholar] [CrossRef] [PubMed]
- Falatah, R. The Impact of the Coronavirus Disease (COVID-19) Pandemic on Nurses’ Turnover Intention: An Integrative Review. Nursing Reports (Pavia, Italy). 2021, 11, 787–810. [Google Scholar] [CrossRef]
- Spetz, J.; Chu, L.; Blash, L. Forecasts of the Registered Nurse Workforce in California. San Francisco, CA: Philip R. Lee Institute for Health Policy Studies, August 2022. Available at: https://www.rn.ca.gov/pdfs/forms/forecast2022.pdf. Accessed August 2025.
- Alasiri, A.A.; Mohammed, V. Healthcare Transformation in Saudi Arabia: An Overview Since the Launch of Vision 2030. Health Services Insights. 2022, 15, 11786329221121214. [Google Scholar] [CrossRef] [PubMed]
- Mani, Z.A.; Goniewicz, K. Transforming Healthcare in Saudi Arabia: A Comprehensive Evaluation of Vision 2030’s Impact. Sustainability. 2024, 16, Article 8. [Google Scholar] [CrossRef]
- AbdELhay, E.S.; Taha, S.M.; El-Sayed, M.M.; Helaly, S.H.; AbdELhay, I.S. Nurses’ retention: The impact of transformational leadership, career growth, work well-being, and work-life balance. BMC Nursing. 2025, 24, 148. [Google Scholar] [CrossRef]
- Katz, R.L. Skills of an Effective Administrator. Harvard Business Review. 1974, 52, 90–102, https://hbr.org/1974/09/skills-of-an-effective-administrator . [Google Scholar]
- Bass, B.M. Leadership: Good, better, best. Organizational Dynamics. 1985, 13, 26–40. [Google Scholar] [CrossRef]
- Ajzen, I. The theory of planned behavior. Organizational Behavior and Human Decision Processes. 1991, 50, 179–211. [Google Scholar] [CrossRef]
- DeOnna, J. Developing and Validating an Instrument to Measure the Perceived Job Competencies Linked to Performance and Staff Retention of First-Line Nurse Managers Employed in a Hospital Setting—Blacklight [Dissertation] 2006. https://etda.libraries.psu.edu/catalog/7168.
- Abd-Elmoghith, N.; Abd-Elhady, T. Nurse Managers’ Competencies and its relation to their Leadership Styles. Assiut Scientific Nursing Journal, 2021, 9, 79–86. [Google Scholar] [CrossRef]
- Perez-Gonzalez, S.; Marques-Sanchez, P.; Pinto-Carral, A.; Gonzalez-Garcia, A.; Liebana-Presa, C.; Benavides, C. Characteristics of leadership competency in nurse managers: A scoping review. Journal of Nursing Management 2024, 5594154. [Google Scholar] [CrossRef]
- Ike, O.; Ugwu, L.; Enwereuzor, I.; Eze, I.; Omeje, O.; Okonkwo, A. Expanded-multidimensional turnover intentions: Scale development and validation. BMC Psychology. 2023, 11. [Google Scholar] [CrossRef]
- Alsadaan, N.; Salameh, B.; Reshia, F.A.A.E.; Alruwaili, R.F.; Alruwaili, M.; Awad Ali, S.A.; Alruwaili, A.N.; Hefnawy, G.R.; Alshammari, M.S.S.; Alrumayh, A.G.R.; Alruwaili, A.O.; Jones, L.K. Impact of Nurse Leaders Behaviors on Nursing Staff Performance: A Systematic Review of Literature. Inquiry: A Journal of Medical Care Organization, Provision and Financing 2023, 60, 00469580231178528. [Google Scholar] [CrossRef]
- Jooste, K.; Cairns, L. Comparing nurse managers and nurses’ perceptions of nurses’ self-leadership during capacity building. Journal of Nursing Management. 2014, 22. [Google Scholar] [CrossRef] [PubMed]
- Long, N.H.; Sochalski, J. Discrepancies between supervisor self-evaluations and staff perceptions of leadership: A cross-sectional study in healthcare. BMC Nursing. 2025, 24, 1049. [Google Scholar] [CrossRef] [PubMed]
- Moradi, T.; Mehraban, M.A.; Moeini, M. Comparison of the perceptions of managers and nursing staff toward performance appraisal. Iranian Journal of Nursing and Midwifery Research. 2017, 22, 128–134. [Google Scholar] [CrossRef] [PubMed]
- Albalawi, A.M.; Pascua, G.P.; Alsaleh, S.A.; Sabry, W.; Ahajan, S.N.; Abdulla, J.; Abdulalim, A.; Salih, S.S. Factors Influencing Nurses Turnover in Saudi Arabia: A Systematic Review. Nursing Forum 2024, 4987339. [Google Scholar] [CrossRef]
- Chang, S.-Y. , Sunaryo, E. Y. A. B., Kristamuliana, K., Lee, H.-F., & Chen, C.-M. Factors influencing nurses’ turnover: An umbrella review. Nursing Outlook. 2025, 73, 102464. [Google Scholar] [CrossRef]
- Kelly, L.A.; Gee, P.M.; Butler, R.J. Impact of nurse burnout on organizational and position turnover. Nursing Outlook. 2021, 69, 96–102. [Google Scholar] [CrossRef]
- Pattali, S. , Sankar, J. P., Al Qahtani, H., Menon, N., & Faizal, S. Effect of leadership styles on turnover intention among staff nurses in private hospitals: The moderating effect of perceived organizational support. BMC Health Services Research. 2024, 24, 199. [Google Scholar] [CrossRef]
- Al Mutair, A.; Al Bazroun, M.I.; Almusalami, E.M.; Aljarameez, F.; Alhasawi, A.I.; Alahmed, F.; Saha, C.; Alharbi, H.F.; Ahmed, G.Y. Quality of Nursing Work Life among Nurses in Saudi Arabia: A Descriptive Cross-Sectional Study. Nursing Reports (Pavia, Italy). 2022, 12, 1014–1022. [Google Scholar] [CrossRef] [PubMed]
- Alharbi, A.; Rasmussen, P.; Magarey, J. Clinical nurse managers’ leadership practices in Saudi Arabian hospitals: A descriptive cross-sectional study. Journal of Nursing Management. 2021, 29, 1454–1464. [Google Scholar] [CrossRef] [PubMed]
- Sawafi, A.A.; Yahyaei, A.A.; Azri, N.H.A.; Sabei, S.D.A.; Maamari, A.-M.A.; Battashi, H.A.; Ismaili, S.R.A.; Maskari, J.K. A. Bridging the Leadership Gap: Developing a Culturally Adapted Leadership Program for Healthcare Professionals in Oman. Journal of Healthcare Leadership. 2025, 17, 365–381. [Google Scholar] [CrossRef] [PubMed]
- Alilyyani, B.; Althobaiti, E.; Al-Talhi, M.; Almalki, T.; Alharthy, T.; Alnefaie, M.; Talbi, H.; Abuzaid, A. Nursing experience and leadership skills among staff nurses and intern nursing students in Saudi Arabia: A mixed methods study. BMC Nursing. 2024, 23, 87. [Google Scholar] [CrossRef]
- Jaber, M.J.; Bindahmsh, A.A.; Baker, O.G.; Alaqlan, A.; Almotairi, S.M.; Elmohandis, Z.E.; Qasem, M.N.; AlTmaizy, H.M.; du Preez, S.E.; Alrafidi, R.A.; Alshodukhi, A.M.; Al Nami, F.N.; Abuzir, B. M. Burnout combating strategies, triggers, implications, and self-coping mechanisms among nurses working in Saudi Arabia: A multicenter, mixed methods study. BMC Nursing. 2025, 24, 590. [Google Scholar] [CrossRef]
- Saleh, Z.T.; Aslanoğlu, A.; Elshatarat, R.A.; Al-Za’areer, M.S.; Almagharbeh, W.T.; Alhejaili, A.A.; Alhumaidi, B.N.; Al-Akash, H.Y.; Al-Momani, M.M.; Alfanash, H.A.; Alasmari, A.A. Exploring the reasons and significant influencing factors of serious turnover intentions among nurses in Saudi Arabia. Journal of Education and Health Promotion. 2025, 14, 206. [Google Scholar] [CrossRef]
- Adhikari, R.; Smith, P. Global nursing workforce challenges: Time for a paradigm shift. Nurse Education in Practice. 2023, 69, 103627. [Google Scholar] [CrossRef]
- Ofei, A.M.A.; Poku, C.A.; Paarima, Y.; Barnes, T.; Kwashie, A.A. Toxic leadership behaviour of nurse managers and turnover intentions: The mediating role of job satisfaction. BMC Nursing. 2023, 22, 374. [Google Scholar] [CrossRef]
|
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2025 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (http://creativecommons.org/licenses/by/4.0/).