Submitted:
28 August 2025
Posted:
28 August 2025
You are already at the latest version
Abstract
Keywords:
1. Introduction
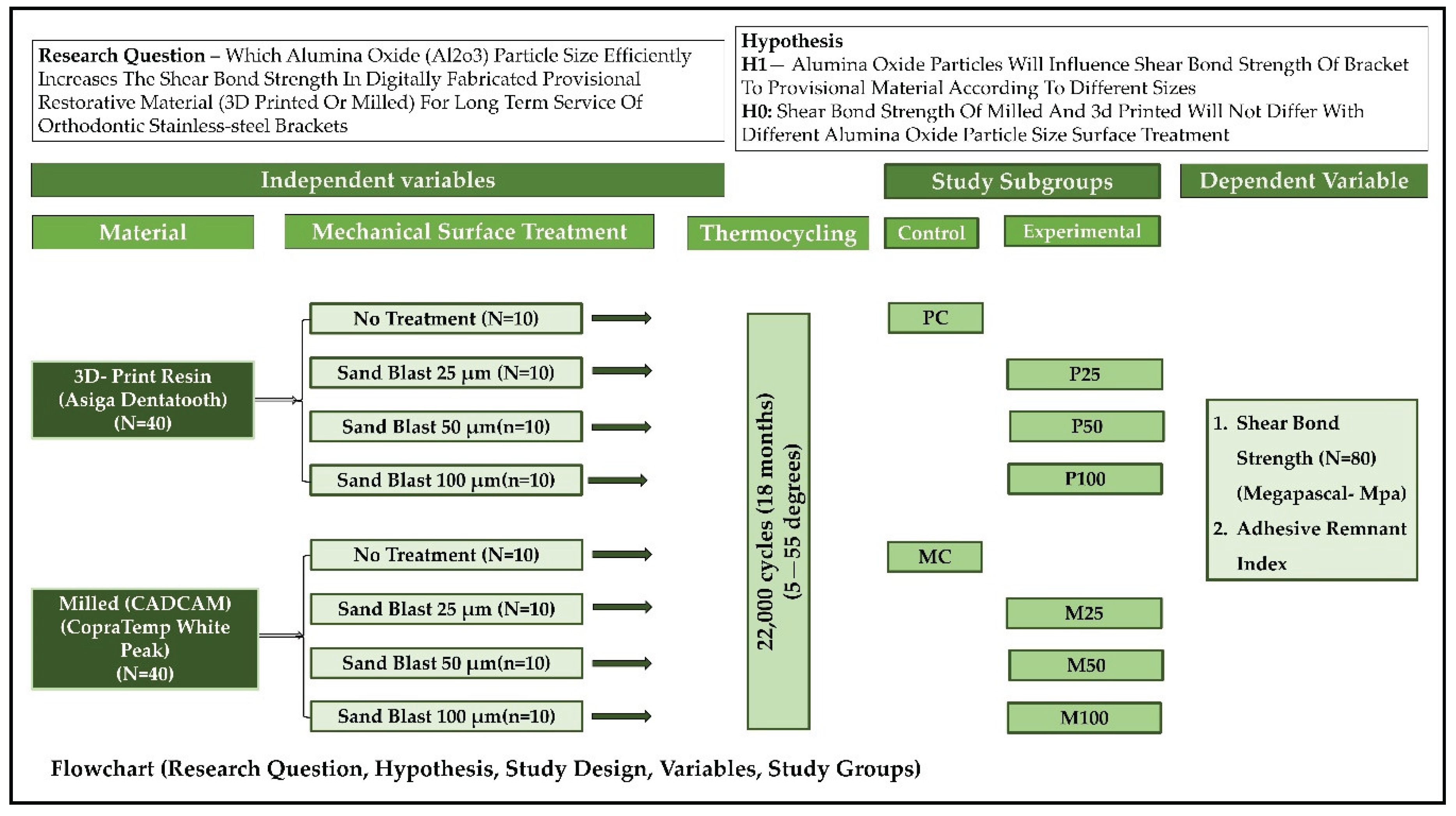
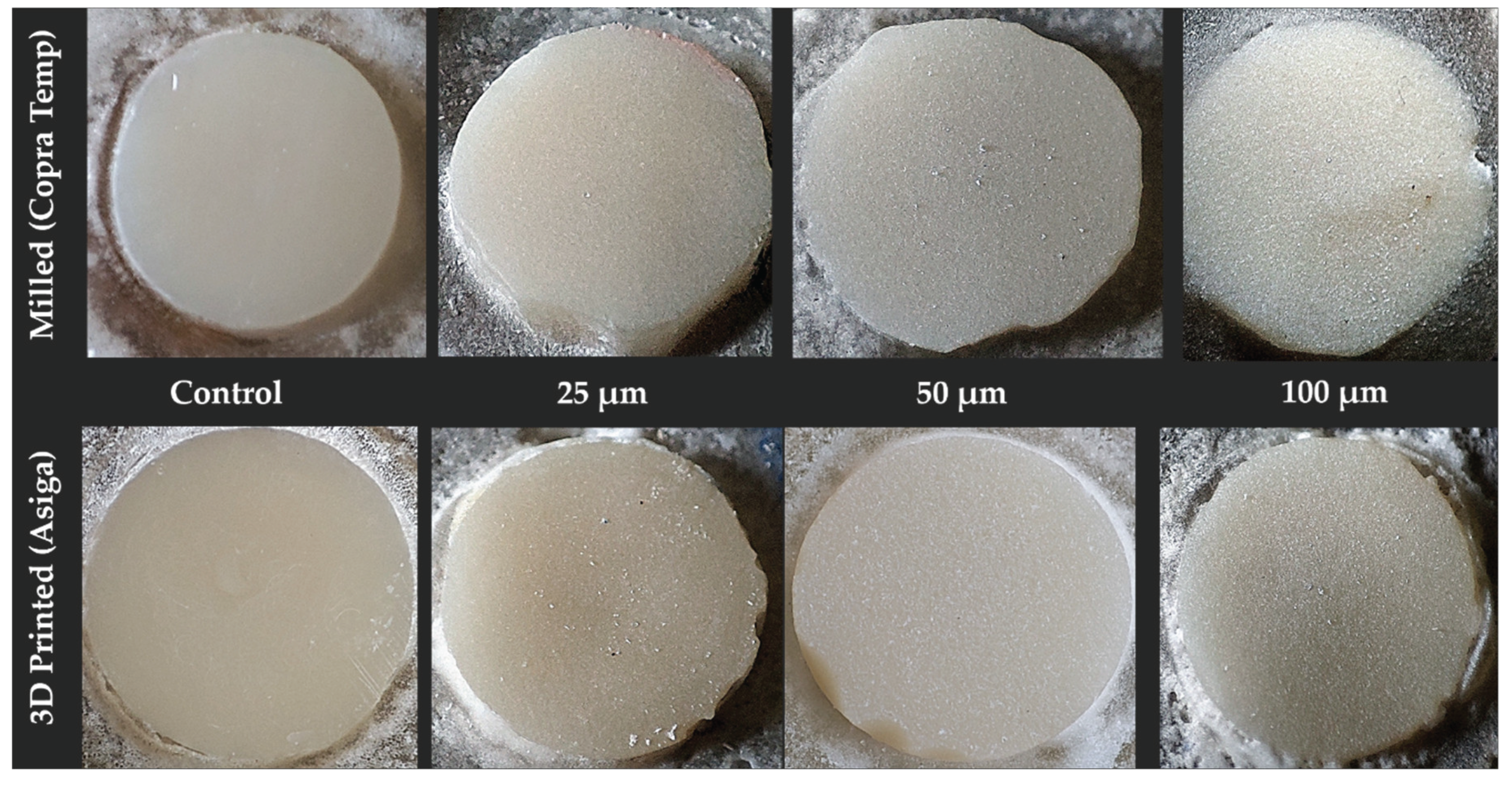
2. Materials and Methods
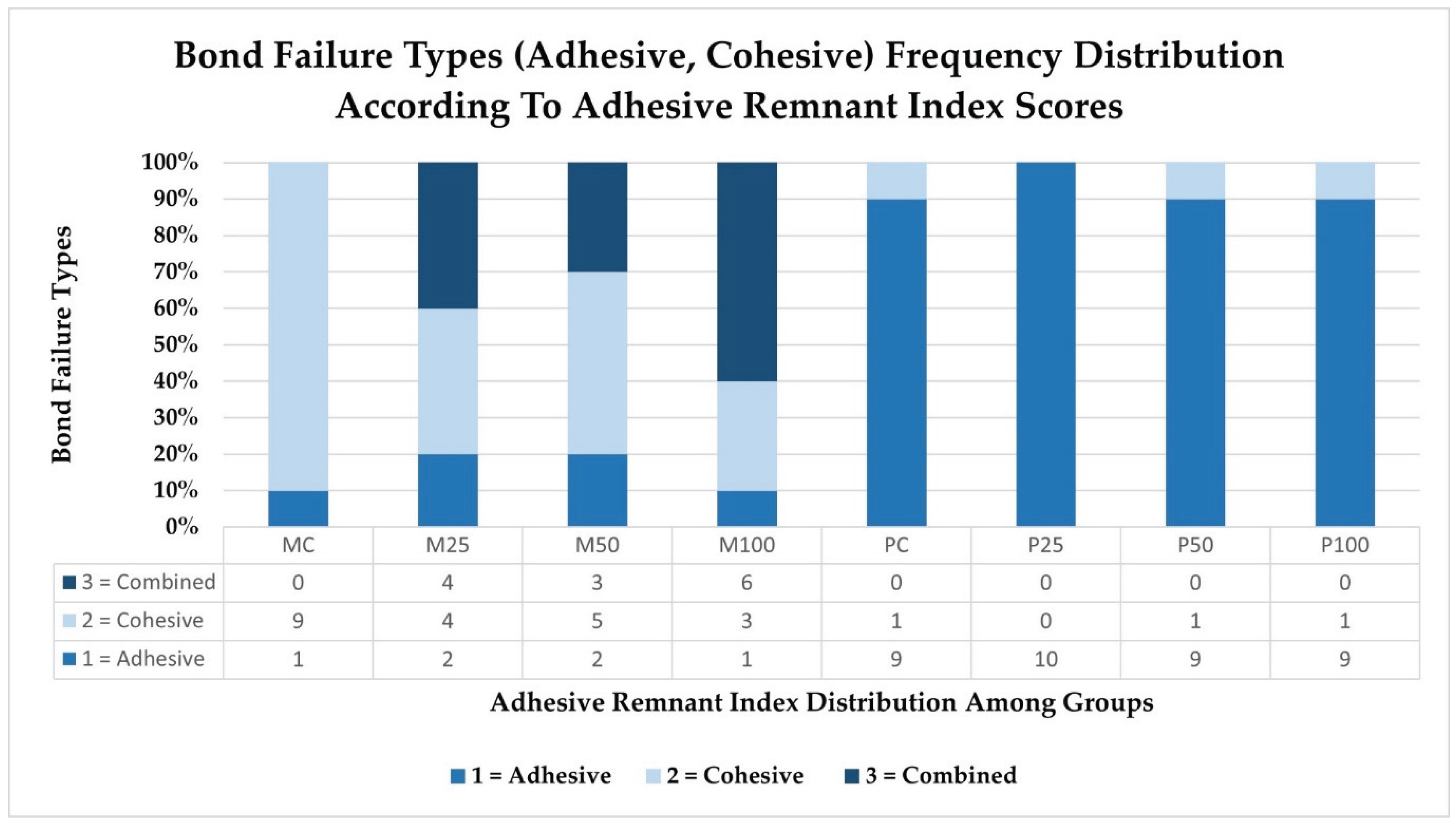
3. Results
4. Discussion
5. Conclusions
Author Contributions
Funding
Institutional Review Board Statement
Data Availability Statement
Conflicts of Interest
References
- Hassan, N.N.; Mattoo, K.; Khawaji, A.; Najmi, H.; Sadeli, A.; Alshahrani, A.A.; Qahtani, A.A.; Alshehri, A.H.; Almarzouki, M.; Sayed, M.E. Influence of Surface Treatment and Protracted Ageing on the Shear Bond Strength of Orthodontic Brackets to Two Digitally Fabricated (Milled and 3D-Printed) Polymethacrylate-Based Provisional Crowns. Polymers 2025, 17, 699. [Google Scholar] [CrossRef]
- Rathi, N.; Jain, K.; Mattoo, K.A. Placing an implant fixture during ongoing orthodontic treatment. SSRG Int. J. Med. Sci. 2019, 6, 19–21. [Google Scholar] [CrossRef]
- Vlasa, A.; Bud, E.S.; Păcurar, M.; Lazăr, L.; Streiche, L.; Bucur, S.M.; Cocoș, D.I.; Bud, A. Effects of Composite Resin on the Enamel After Debonding: An In Vitro Study—Metal Brackets vs. Ceramic Brackets. Appl. Sci. 2021, 11, 7353. [Google Scholar] [CrossRef]
- Oskoee, P.A.; Kachoei, M.; Rikhtegaran, S.; Fathalizadeh, F.; Navimipour, E.J. Effect of surface treatment with sandblasting and Er,Cr:YSGG laser on bonding of stainless-steel orthodontic brackets to silver amalgam. Med. Oral. Patol. Oral. Cir. Bucal 2012, 17, e292–e296. [Google Scholar] [CrossRef] [PubMed]
- Reynolds, I.R. A review of direct orthodontic bonding. Br. J. Orthod. 1975, 2, 171–178. [Google Scholar] [CrossRef]
- Finnema, K.J.; Ozcan, M.; Post, W.J.; Ren, Y.; Dijkstra, P.U. In-vitro orthodontic bond strength testing: A systematic review and meta-analysis. Am. J. Orthod. Dentofac. Orthop. 2010, 137, 615–622.e3. [Google Scholar] [CrossRef]
- Eliades, T.; Brantley, W.A. The inappropriateness of conventional orthodontic bond strength assessment protocols. Eur. J. Orthod. 2000, 22, 13–23. [Google Scholar] [CrossRef] [PubMed]
- Hajrassie, M.K.; Khier, S.E. In-vivo and in-vitro comparison of bond strengths of orthodontic brackets bonded to enamel and debonded at various times. Am. J. Orthod. Dentofac. Orthop. 2007, 131, 384–390. [Google Scholar] [CrossRef]
- Linklater, R.A.; Gordon, P.H. An ex vivo study to investigate bond strengths of different tooth types. J. Orthod. 2001, 28, 59–65. [Google Scholar] [CrossRef]
- Ash, S.; Hay, N. Adhesive pre-coated brackets: A comparative clinical study. Br. J. Orthod. 1996, 23, 325–329. [Google Scholar] [CrossRef]
- Gonçalves, C.M.; da Silva, V.R.; Pecorari, V.G.; Martins, L.R.; Santos, E.C. Shear bond strength of different orthodontic bracket bonding systems on saliva-contaminated enamel: In vitro. J. Media Crit. 2024, 10, e142. [Google Scholar] [CrossRef]
- Fonseca-Silva, T.; Otoni, R.P.; Magalhães, A.A.; Ramos, G.M.; Gomes, T.R.; Rego, T.M.; Araújo, C.T.; Santos, C.C. Comparative analysis of shear bond strength of steel and ceramic orthodontic brackets bonded with six different orthodontic adhesives. Int. J. Odontostom. 2020, 14, 658–663. [Google Scholar] [CrossRef]
- Bayram, M.; Yeşilyurt, C.; Kuşgöz, A.; Ülker, M.; Nur, M. Shear bond strength of orthodontic brackets to aged resin composite surfaces: Effect of surface conditioning. Eur. J. Orthod. 2011, 33, 174–179. [Google Scholar] [CrossRef]
- Danha, L.S.; Rafeeq, R.A. Assessment of Effect of Flowable Composite on the Shear Bond Strength of Sapphire Bracket Bonded to Composite Restoration: An in Vitro Study. Dent. Hypotheses 2024, 15, 41–44. [Google Scholar] [CrossRef]
- Valizadeh, S.; Alimohammadi, G.; Nik, T.H.; Etemadi, A.; Tanbakuchi, B. In vitro evaluation of shear bond strength of orthodontic metal brackets to aged composite using a self-adhesive composite: Effect of surface conditioning and different bonding agents. Int. Orthod. 2020, 18, 528–537. [Google Scholar] [CrossRef]
- Babaahmadi, F.; Aghaali, M.; Saleh, A.; Mehdipour, A. Comparing the Effect of Zirconia Surface Conditioning Using Nd: YAG Laser and Conventional Method on Shear Bond Strength of Ceramic Brackets to Zirconia Surface: An In vitro Study. J. Maz. Univ. Med. Sci. 2023, 33, 139–145. [Google Scholar]
- Pinho, M.; Manso, M.C.; Almeida, R.F.; Martin, C.; Carvalho, Ó.; Henriques, B.; Silva, F.; Pinhão Ferreira, A.; Souza, J.C. Bond strength of metallic or ceramic orthodontic brackets to enamel, acrylic, or porcelain surfaces. Materials 2020, 13, 5197. [Google Scholar] [CrossRef]
- Buyukyilmaz, T.; Zachrisson, B.U. Improved orthodontic bonding to silver amalgam. Part 2. Lathe-cut, admixed, and spherical amalgams with different intermediate resins. Angle Orthod. 1998, 68, 337–344. [Google Scholar] [PubMed]
- Haber, D.; Khoury, E.; Ghoubril, J.; Cirulli, N. Effect of different surface treatments on the shear bond strength of metal orthodontic brackets bonded to CAD/CAM provisional crowns. Dent. J. 2023, 11, 38. [Google Scholar] [CrossRef] [PubMed]
- Goracci, C.; Özcan, M.; Franchi, L.; Di Bello, G.; Louca, C.; Vichi, A. Bracket bonding to polymethylmethacrylate-based materials for computer-aided design/ manufacture of temporary restorations: Influence of mechanical treatment and chemical treatment with universal adhesives. Korean J. Orthod. 2019, 49, 404–412. [Google Scholar] [CrossRef]
- Goymen, M.; Topcuoglu, T.; Topcuoglu, S.; Akin, H. Effect of different temporary crown materials and surface roughening methods on the shear bond strengths of orthodontic brackets. Photomed. Laser Surg. 2015, 33, 55–60. [Google Scholar] [CrossRef]
- Najafi, H.Z.; Moradi, M.; Torkan, S. Effect of different surface treatment methods on the shear bond strength of orthodontic brackets to temporary crowns. Int. Orthod. 2019, 17, 89–95. [Google Scholar] [CrossRef] [PubMed]
- Mattoo, K.; Boreak, N.; Alsuhaymi, M.O.; Ganawi, A.A.; Houmady, R.A.; Alibrahim, H.M.; Otayf, T.S.; Al Moaleem, M.M. Different Methods of Measuring Mid-Palatine Suture Maturation in Determining the Timing for Rapid Palatine Expansion. Int. J. Morphol. 2025, 43, 209–217. [Google Scholar] [CrossRef]
- Ayman, A.D. The residual monomer content and mechanical properties of CAD\CAM resins used in the fabrication of complete dentures as compared to heat cured resins. Electron. Physician 2017, 9, 4766. [Google Scholar] [CrossRef]
- Sayed, M.E.; Lunkad, H.; Mattoo, K.; Jokhadar, H.F.; Al Resayes, S.S.; Alqahtani, N.M.; Alshehri, A.H.; Alamri, M.; Altowairqi, S.; Muaddi, M.; et al. Evaluation of the effects of digital manufacturing, preparation taper, cement type, and aging on the color stability of anterior provisional crowns using colorimetry. Med. Sci. Monit. Basic. Res. 2023, 29, e941919-1. [Google Scholar] [CrossRef]
- Eslamian, L.; Borzabadi-Farahani, A.; Mousavi, N.; Ghasemi, A. A comparative study of shear bond strength between metal and ceramic brackets and artificially aged composite restorations using different surface treatments. Eur. J. Orthod. 2012, 34, 610–617. [Google Scholar] [CrossRef]
- Oh, S.H.; Chae, J.M.; Chang, N.Y. Color stability of various plastic and ceramic brackets: An in vitro study. Clin. J. Korean Assoc. Orthod. 2022, 12, 189–199. [Google Scholar] [CrossRef]
- Premkumar, S.; Amit, K. Assessment of Enamel Loss After Debonding of Ceramic, Composite Plastic and Metal Brackets-An In Vitro Study. J. Contemp. Orthod. 2019, 3, 1–10. [Google Scholar]
- Della Bona, A.; Kochenborger, R.; Di Guida, L.A. Bond strength of ceramic and metal orthodontic brackets to aged resin-based composite restorations. Curr. Dent. 2019, 1, 40–45. [Google Scholar] [CrossRef]
- Al Jabbari, Y.S.; Al Taweel, S.M.; Al Rifaiy, M.; Alqahtani, M.Q.; Koutsoukis, T.; Zinelis, S. Effects of surface treatment and artificial aging on the shear bond strength of orthodontic brackets bonded to four different provisional restorations. Angle Orthod. 2014, 84, 649–655. [Google Scholar] [CrossRef] [PubMed]
- Ellakany, P.; Fouda, S.M.; Mahrous, A.A.; Al Ghamdi, M.A.; Aly, N.M. Influence of CAD/CAM milling and 3d-printing fabrication methods on the mechanical properties of 3-unit interim fixed dental prosthesis after thermo-mechanical aging process. Polymers 2022, 14, 4103. [Google Scholar] [CrossRef] [PubMed]
- Kumar, L.; Verma, A.; Pal, U.S.; Mattoo, K.; Algarni, Y.A.; Bin Hassan, S.A.; Baba, S.M.; Jeri, S.Y.; Khateeb, S.U. Influence of prosthodontic rehabilitation using zygomatic implants in COVID-19 related mucormycosis (rhino–orbital–cerebral) maxillectomy patients upon post-operative stress, anxiety and functional impairment: A prospective cohort study. Clin. Interv. Aging 2023, 18, 1201–1219. [Google Scholar] [CrossRef]
- Sindi, A.S.; Kumar, L.; Verma, A.; Pal, U.S.; Sayed, M.E.; Mattoo, K.; Morsy, M.S.; Baba, S.M.; Khalid, I.; Baig, F.A.; et al. Prosthodontic rehabilitation’s role in alleviating anxiety and depression in mucormycosis-induced maxillectomy patients post-COVID-19. Med. Sci. Monit. Int. Med. J. Exp. Clin. Res. 2023, 29, e941488-1. [Google Scholar]
- Coelho, C.; Calamote, C.; Pinto, A.C.; Esteves, J.L.; Ramos, A.; Escuin, T.; Souza, J.C. Comparison of CAD-CAM and traditional chairside processing of 4-unit interim prostheses with and without cantilevers: Mechanics, fracture behavior, and finite element analysis. J. Prosthet. Dent. 2021, 125, 543.e1–543.e10. [Google Scholar] [CrossRef]
- Shin, J.-W.; Kim, J.-E.; Choi, Y.-J.; Shin, S.-H.; Nam, N.-E.; Shim, J.-S.; Lee, K.-W. Evaluation of the color stability of 3D-printed crown and bridge materials against various sources of discoloration: An in vitro study. Materials 2020, 13, 5359. [Google Scholar] [CrossRef]
- Yau, H.T.; Yang, T.J.; Lin, Y.K. Comparison of 3-D Printing and 5-Axis Milling for the Production of Dental e-Models from Intra-oral Scanning. Comput. Aided Des. Appl. 2016, 13, 32–38. [Google Scholar] [CrossRef]
- Lee, W.S.; Lee, D.H.; Lee, K.B. Evaluation of internal fit of interim crown fabricated with CAD/CAM milling and 3D printing system. J. Adv. Prosthodont. 2017, 9, 265. [Google Scholar] [CrossRef]
- Peng, C.C.; Chung, K.H.; Ramos, V., Jr. Assessment of the adaptation of interim crowns using different measurement techniques. J. Prosthodont. 2020, 29, 87–93. [Google Scholar] [CrossRef] [PubMed]
- Park, J.M.; Ahn, J.S.; Cha, H.S.; Lee, J.H. Wear resistance of 3D printing resin material opposing zirconia and metal antagonists. Materials 2018, 11, 1043. [Google Scholar] [CrossRef] [PubMed]
- Tahayeri, A.; Morgan, M.; Fugolin, A.P.; Bompolaki, D.; Athirasala, A.; Pfeifer, C.S.; Ferracane, J.L.; Bertassoni, L.E. 3D printed versus conventionally cured provisional crown and bridge dental materials. Dent. Mater. 2018, 34, 192–200. [Google Scholar] [CrossRef]
- Al-Dwairi, Z.N.; Al Haj Ebrahim, A.A.; Baba, N.Z. A Comparison of the Surface and Mechanical Properties of 3D Printable Denture-Base Resin Material and Conventional Polymethylmethacrylate (PMMA). J. Prosthod. 2023, 32, 40–48. [Google Scholar] [CrossRef]
- Sayed, M.E. Comparative Evaluation of Shear Bond Strength of Aesthetic Orthodontic Brackets Bonded to Aged Composite Restorative Resin Materials. Polymers 2025, 17, 621. [Google Scholar] [CrossRef]
- Layton, D.M.; Morgano, S.M.; Muller, F.; Kelly, J.A.; Nguyen, C.T.; Scherrer, S.S.; Salinas, T.J.; Shah, K.C.; Att, W.; Frelich, M.A.; et al. Glossary of Prosthodontic Terms 2023, 10th edition. J. Prosthet. Dent. 2023, 130, e1–e126. [Google Scholar] [CrossRef]
- Faggion, C.M., Jr. Guidelines for reporting pre-clinical in vitro studies on dental materials. J. Evid. Based Dent. Pract. 2012, 12, 182–189. [Google Scholar] [CrossRef]
- Whitepeaks Dental Solutions GmbH. Available online: https://www.white-peaks-dental.com/en/produkt-details/copra-temp/ (accessed on 20 January 2025).
- Alp, G.; Johnston, W.M.; Yilmaz, B. Optical properties and surface roughness of prepolymerized poly (methyl methacrylate) denture base materials. J. Prosthet. Dent. 2019, 121, 347–352. [Google Scholar] [CrossRef] [PubMed]
- Reicheneder, C.; Baumert, U.; Gedrange, T.; Proff, P.; Faltermeier, A.; Muessig, D. Frictional properties of aesthetic brackets. Eur. J. Orthod. 2007, 29, 359–365. [Google Scholar] [CrossRef]
- Yamakawa, J. Inventor. Resin Block for Dental Cad/Cam. Available online: https://patents.google.com/patent/JP2014161440A/en (accessed on 12 February 2025).
- Iwaki, M.; Kanazawa, M.; Arakida, T.; Minakuchi, S. Mechanical properties of a polymethyl methacrylate block for CAD/CAM dentures. J. Oral Sci. 2020, 62, 420–422. [Google Scholar] [CrossRef] [PubMed]
- Stawarczyk, B.; Trottmann, A.; Hämmerle, C.H.; Özcan, M. Adhesion of veneering resins to polymethylmethacrylate-based CAD/CAM polymers after various surface conditioning methods. Acta Odontol. Scand. 2013, 71, 1142–1148. [Google Scholar] [CrossRef] [PubMed]
- Hosokawa, M.; Fujimura, H. Dental Photopolymerizable Composition for 3D Printer. U.S. Patent 11,744,781, 5 September 2023. [Google Scholar]
- Urethane Dimethacrylate Compound Summary. PubChem. Available online: https://pubchem.ncbi.nlm.nih.gov/compound/170472#section=Chemical-and-Physical-Properties (accessed on 12 February 2025).
- Floyd, C.J.; Dickens, S.H. Network structure of Bis-GMA-and UDMA-based resin systems. Dent. Mater. 2006, 22, 1143–1149. [Google Scholar] [CrossRef]
- Grauzeliene, S.; Schuller, A.S.; Delaite, C.; Ostrauskaite, J. Biobased vitrimer synthesized from 2-hydroxy-3-phenoxypropyl acrylate, tetrahydrofurfuryl methacrylate and acrylated epoxidized soybean oil for digital light processing 3D printing. Eur. Poly. J. 2023, 198, 112424. [Google Scholar] [CrossRef]
- Bilgic, F.; Alkis, H.; Gungor, A.Y.; Tuncdemir, A.R.; Malkoc, M.A. Shear Bond Strength of Ceramic Brackets Bonded to Three Different Porcelain Surfaces. Eur. J. Prosthodont. 2013, 1, 17–20. [Google Scholar] [CrossRef]
- Choi, Y.; Moon, W.; Manso, A.P.; Park, Y.-S.; Lim, B.-S.; Chung, S.H. Shear bond strength of orthodontic brackets bonded with primer-incorporated orthodontic adhesives and unpolymerized 3-dimensional printing materials on 3-dimensional-printed crowns. Am. J. Orthod. Dentofac. Orthop. 2024, 165, 663–670. [Google Scholar] [CrossRef]
- Kim, J.-E.; Choi, W.-H.; Lee, D.; Shin, Y.; Park, S.-H.; Roh, B.-D.; Kim, D. Color and translucency stability of three-dimensional printable dental materials for crown and bridge restorations. Materials 2021, 14, 650. [Google Scholar] [CrossRef] [PubMed]
- Haselton, D.R.; Diaz-Arnold, A.M.; Vargas, M.A. Flexural strength of provisional crown and fixed partial denture resins. J. Prosthet. Dent. 2002, 87, 225–228. [Google Scholar] [CrossRef] [PubMed]
- De Almeida, J.X.; Deprá, M.B.; Marquezan, M.; Retamoso, L.B.; Tanaka, O. Effects of surface treatment of provisional crowns on the shear bond strength of brackets. Dent. Press J. Orthod. 2013, 18, 29–34. [Google Scholar] [CrossRef] [PubMed]
- Soon, H.I.; Gill, D.S.; Jones, S.P. A study to investigate the bond strengths of orthodontic brackets bonded to prosthetic acrylic teeth. J. Orthod. 2015, 42, 192–499. [Google Scholar] [CrossRef]
- Shahin, S.Y.; Abu Showmi, T.H.; Alzaghran, S.H.; Albaqawi, H.; Alrashoudi, L.; Gad, M.M. Bond strength of orthodontic brackets to temporary crowns: In vitro effects of surface treatment. Int. J. Dent. 2021, 2021, 9999933. [Google Scholar] [CrossRef]
| 3D- print resin ink (PC) | Asiga Dentatooth Alexandria, Australia |
|
| 3D Printing Machine | Asiga Pty Ltd. Alexandria, Australia |
|
| CopraTemp | CopraTemp WhitePeaks Dental Solutions GmbH, Wesel, Germany |
|
| DGShape Five Axis milling machine | Roland DGA, Irvine, CA, USA |
|
| Thermocycling machine | Model 1100, SD Mechatronik, Bayern, Germany |
|
| Benchtop 3D Scanner | MEDIT Model MD-ID0300, Medit Corp, South-Korea |
|
| Imaging powder | VITA CEREC, VITA, Bad Sackingen, Germany |
|
| Assure Plus | Reliance Orthodontic Products, Itasca, IL, USA |
|
| Transbond XT | 3M Unitek, Monrovia, CA, USA |
|
| Variable 1 | Variable 2 | Subgroup | N | Median | IQR | Minimum | Maximum | MRS | H Statistic | pValue |
| Material | Surface Treatment | Codes | Mpa | |||||||
|
Milled (Gp M) (N = 40) |
No Treatment | MC | 10 | 14.98 | 2.72 | 12.15 | 16.91 | 20.65 | 65.0397 | 0.0000 * |
| Alumina oxide (25 µm) | M25 | 10 | 16.13 | 2.71 | 14.29 | 19.54 | 35.70 | |||
| Alumina oxide (50 µm) | M50 | 10 | 23.10 | 2.30 | 20.50 | 26.46 | 72.90 | |||
| Alumina oxide (100 µm) | M100 | 10 | 20.00 | 2.36 | 17.10 | 22.39 | 57.60 | |||
|
3d Printed (Gp P) (N = 40) |
No Treatment | PC | 10 | 12.8 | 2.74 | 10.41 | 14.41 | 8.95 | ||
| Alumina oxide (25 µm) | P25 | 10 | 15.08 | 1.55 | 12.50 | 16.71 | 22.6 | |||
| Alumina oxide (50 µm) | P50 | 10 | 20.72 | 2.31 | 17.71 | 23.88 | 61.0 | |||
| Alumina oxide (100 µm) | P100 | 10 | 17.99 | 3.45 | 15.43 | 20.02 | 44.6 | |||
|
Milled (Gp M) (N = 40) |
No Treatment | MC | 10 | 14.98 | 2.72 | 12.15 | 16.91 | 7.4 | 31.8648 | 0.0000 * |
| Alumina oxide (25 µm) | M25 | 10 | 16.13 | 2.71 | 14.29 | 19.54 | 14.4 | |||
| Alumina oxide (50 µm) | M50 | 10 | 23.10 | 2.30 | 20.50 | 26.46 | 34.7 | |||
| Alumina oxide (100 µm) | M100 | 10 | 20.00 | 2.36 | 17.10 | 22.39 | 25.5 | |||
|
3d Printed (Gp P) (N = 40) |
No Treatment | PC | 10 | 12.8 | 2.74 | 10.41 | 14.41 | 6.9 | 31.4283 | 0.0000 * |
| Alumina oxide (25 µm) | P25 | 10 | 15.08 | 1.55 | 12.50 | 16.71 | 14.9 | |||
| Alumina oxide (50 µm) | P50 | 10 | 20.72 | 2.31 | 17.71 | 23.88 | 33.9 | |||
| Alumina oxide (100 µm) | P100 | 10 | 17.99 | 3.45 | 15.43 | 20.02 | 26.3 |
| Subgroups | Parameters | MC | M25 | M50 | M100 | PC | P25 | P50 | P100 |
| MC | MRD | −15.05 | −52.25 | −36.95 | 11.7 | −1.95 | −40.35 | −23.95 | |
| ‘p’ value | 0.1476 | 0.0000 * | 0.0003 * | 0.2602 | 0.8512 | 0.0001 * | 0.0211 | ||
| M25 | MRD | −15.05 | −37.2 | −21.9 | 26.75 | 13.1 | −25.3 | −8.9 | |
| ‘p’ value | 0.1476 | 0.0003 * | 0.0350 | 0.0100 | 0.2075 | 0.0149 | 0.3918 | ||
| M50 | MRD | −52.25 | −37.2 | 15.3 | 63.95 | 50.3 | 11.9 | 28.3 | |
| ‘p’ value | 0.0000 * | 0.0003 * | 0.141 | 0.0000 * | 0.0000 * | 0.2522 | 0.0064 | ||
| M100 | MRD | −36.95 | −21.9 | 15.3 | 48.65 | 35 | −3.4 | 13 | |
| ‘p’ value | 0.0003 * | 0.0350 | 0.141 | 0.0000 * | 0.0007 * | 0.7435 | 0.211 | ||
| PC | MRD | 11.7 | 26.75 | 63.95 | 48.65 | −13.65 | −52.05 | −35.65 | |
| ‘p’ value | 0.2602 | 0.0100 | 0.0000 * | 0.0000 * | 0.189 | 0.0000 * | 0.0006 * | ||
| P25 | MRD | −1.95 | 13.1 | 50.3 | 35 | −13.65 | −38.4 | −22 | |
| ‘p’ value | 0.8512 | 0.2075 | 0.0000 * | 0.0007 * | 0.189 | 0.0002 * | 0.0342 | ||
| P50 | MRD | −40.35 | −25.3 | 11.9 | −3.4 | −52.05 | −38.4 | 16.4 | |
| ‘p’ value | 0.0001 * | 0.0149 | 0.2522 | 0.7435 | 0.0000 * | 0.0002 * | 0.1145 | ||
| P100 | MRD | −23.95 | −8.9 | 28.3 | 13 | −35.65 | −22 | 16.4 | |
| ‘p’ value | 0.0211 | 0.3918 | 0.0064 | 0.211 | 0.0006 * | 0.0342 | 0.1145 |
| Subgroups | Parameters | MC | M25 | M50 | M100 | Subgroups | PC | P25 | P50 | P100 |
| MC | MRD | −7 | −27.3 | −18.1 | PC | −8 | −27 | −19.4 | ||
| ‘p’ value | 0.1806 | 0.0000 * | 0.0005 | 0.1264 | 0.0000 * | 0.0002 * | ||||
| M25 | MRD | −7 | −20.3 | −11.1 | P25 | −8 | −19 | −11.4 | ||
| ‘p’ value | 0.1806 | 0.0001 | 0.0337 | 0.1264 | 0.0002 * | 0.0292 | ||||
| M50 | MRD | −27.3 | −20.3 | 9.2 | P50 | −27 | −19 | 7.6 | ||
| ‘p’ value | 0.0000 * | 0.0001 | 0.0784 | 0.0000 * | 0.0002 * | 0.146 | ||||
| M100 | MRD | −18.1 | −11.1 | 9.2 | P100 | −19.4 | −11.4 | 7.6 | ||
| ‘p’ value | 0.0005 | 0.0337 | 0.0784 | 0.0002 * | 0.0292 | 0.146 |
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2025 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (http://creativecommons.org/licenses/by/4.0/).





