1. Introduction
Dental implant placement in cases of severe alveolar bone loss, especially after traumatic injuries, requires precise planning and advanced regenerative techniques to restore both function and esthetics. Post-traumatic ridge deficiencies often involve complex vertical and horizontal bone resorption that can compromise implant stability and esthetic results [
1,
3,
5]. Contemporary approaches utilize guided bone regeneration (GBR) with particulate allografts and barrier membranes to promote new bone formation [
2,
6]. The use of fixation devices such as allograft bone plates and tenting screws has been shown to maintain space and prevent graft collapse, which is critical in vertical ridge augmentation [
7,
8].
Soft tissue management is equally important for long-term implant success. Insufficient keratinized mucosa and scarred vestibules can hinder healing and affect prosthetic outcomes. Acellular dermal matrix (ADM) has emerged as an effective alternative to autogenous soft tissue grafts, providing predictable soft tissue volume and quality [
9,
10]. The application of a full-thickness flap with palatal release allows tension-free primary closure, minimizing wound complications [
11].
In the posterior maxilla, sinus pneumatization commonly necessitates sinus augmentation procedures. Open sinus lift techniques combined with allograft placement under the elevated Schneiderian membrane have demonstrated favorable implant survival rates [
12,
14]. Collagen membranes and fixation tacks further stabilize the graft and reduce micromotion [
13].
Furthermore, low-level laser therapy (LLLT) has shown promise in enhancing soft tissue healing, reducing postoperative pain and edema, and accelerating recovery after oral surgical procedures [
15,
17]. Several studies support its use adjunctively in bone augmentation and implantology [
16,
18].
This case report describes the combined use of vertical and horizontal ridge augmentation with cortical cancellous allograft, bone plates, tenting screws, sinus lift, and ADM in a 46-year-old female patient with severe post-traumatic alveolar ridge loss. The clinical procedures, radiographic assessments, and postoperative outcomes over a 12-month follow-up are detailed.
2. Case Presentation
A 46-year-old female patient was referred to our clinic with a history of maxillary trauma resulting from a motor vehicle accident. She reported aesthetic concerns and difficulty in mastication due to missing teeth and ridge defects. The patient had no relevant medical history and was a non-smoker.
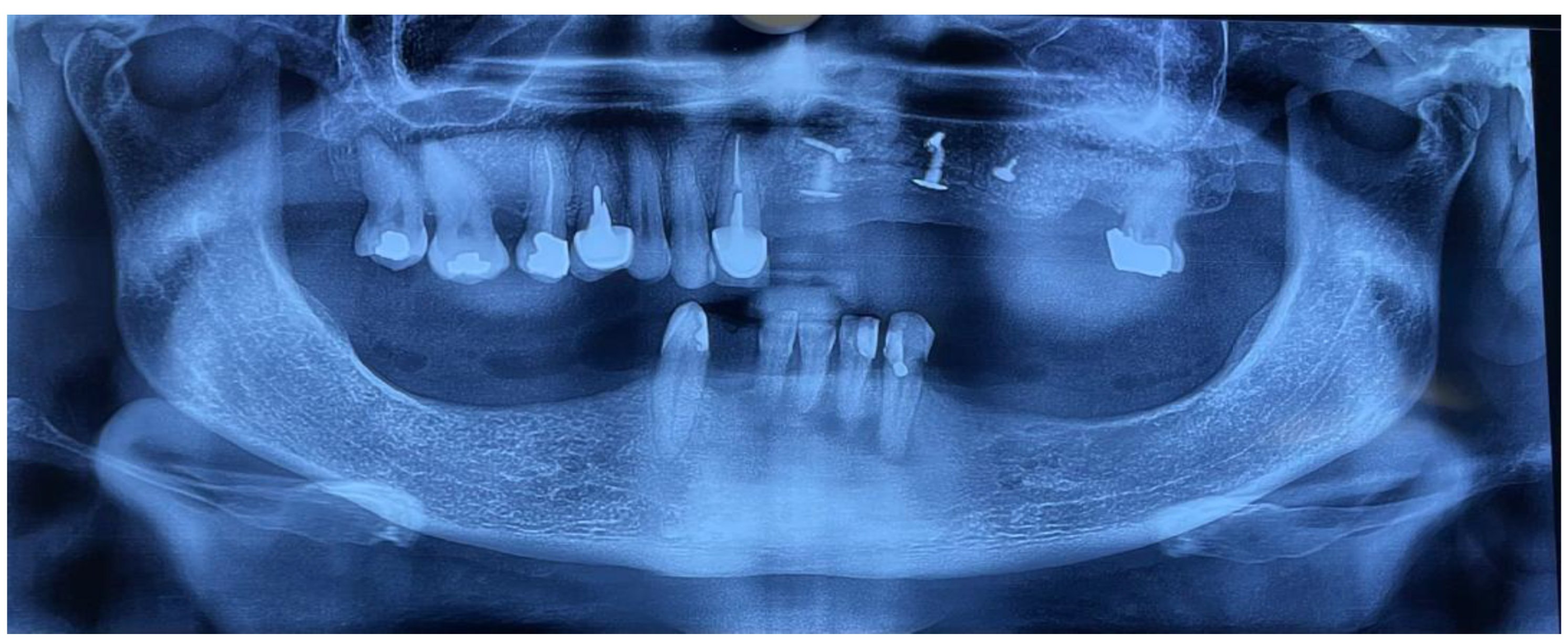
Clinical examination revealed severe horizontal and vertical ridge deficiencies in the maxilla, with notable lack of keratinized soft tissue and vestibular scarring from previous injuries. The alveolar ridge width measured approximately 1.8 mm in the anterior region, with vertical height ranging from 2 to 5 mm to the nasal floor. right maxillary central incisor (FDI 11) and left maxillary central incisor, lateral incisor, first premolar, second premolar and first molar (FDI 21, 22,23, 24, 25, 26) were missing.
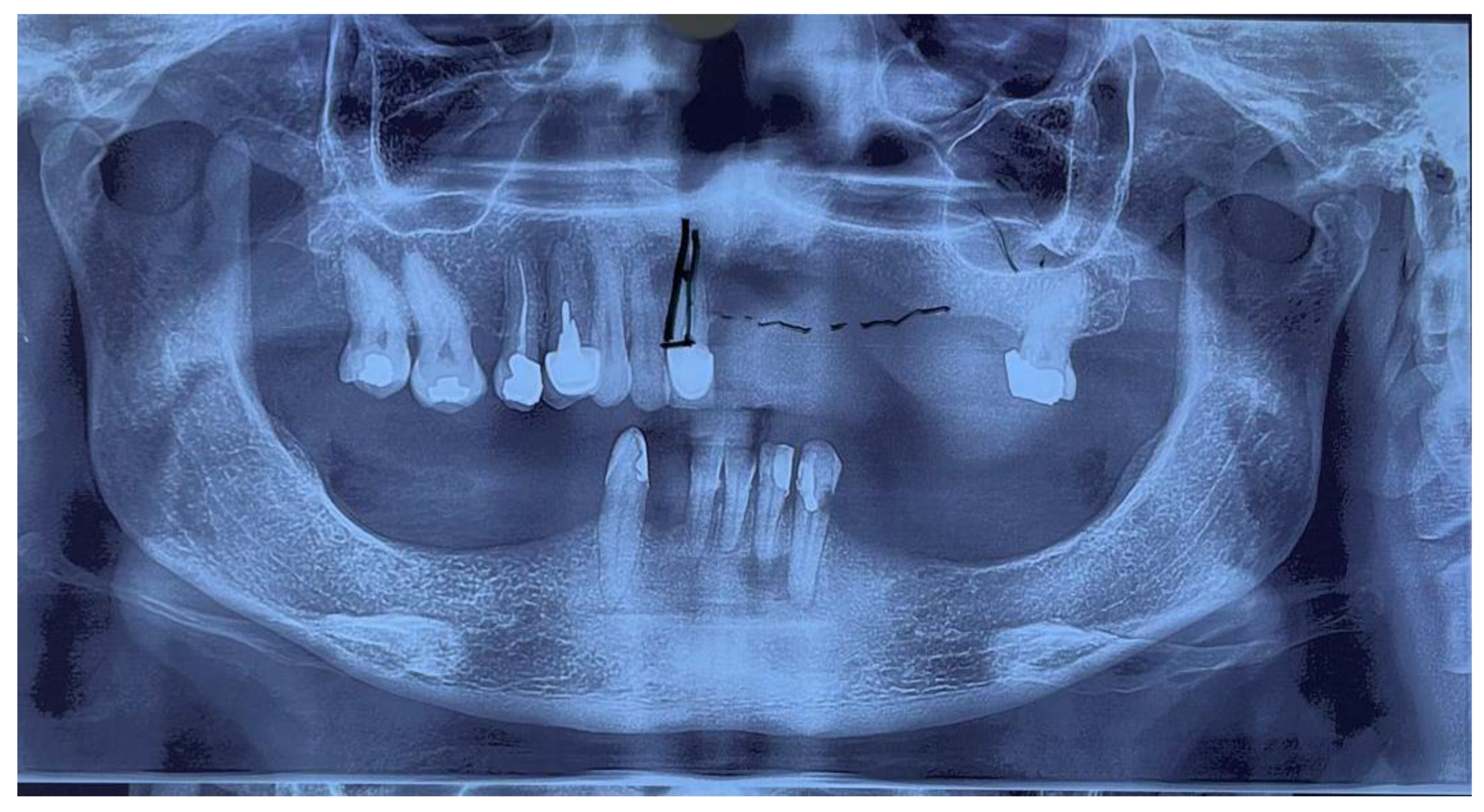
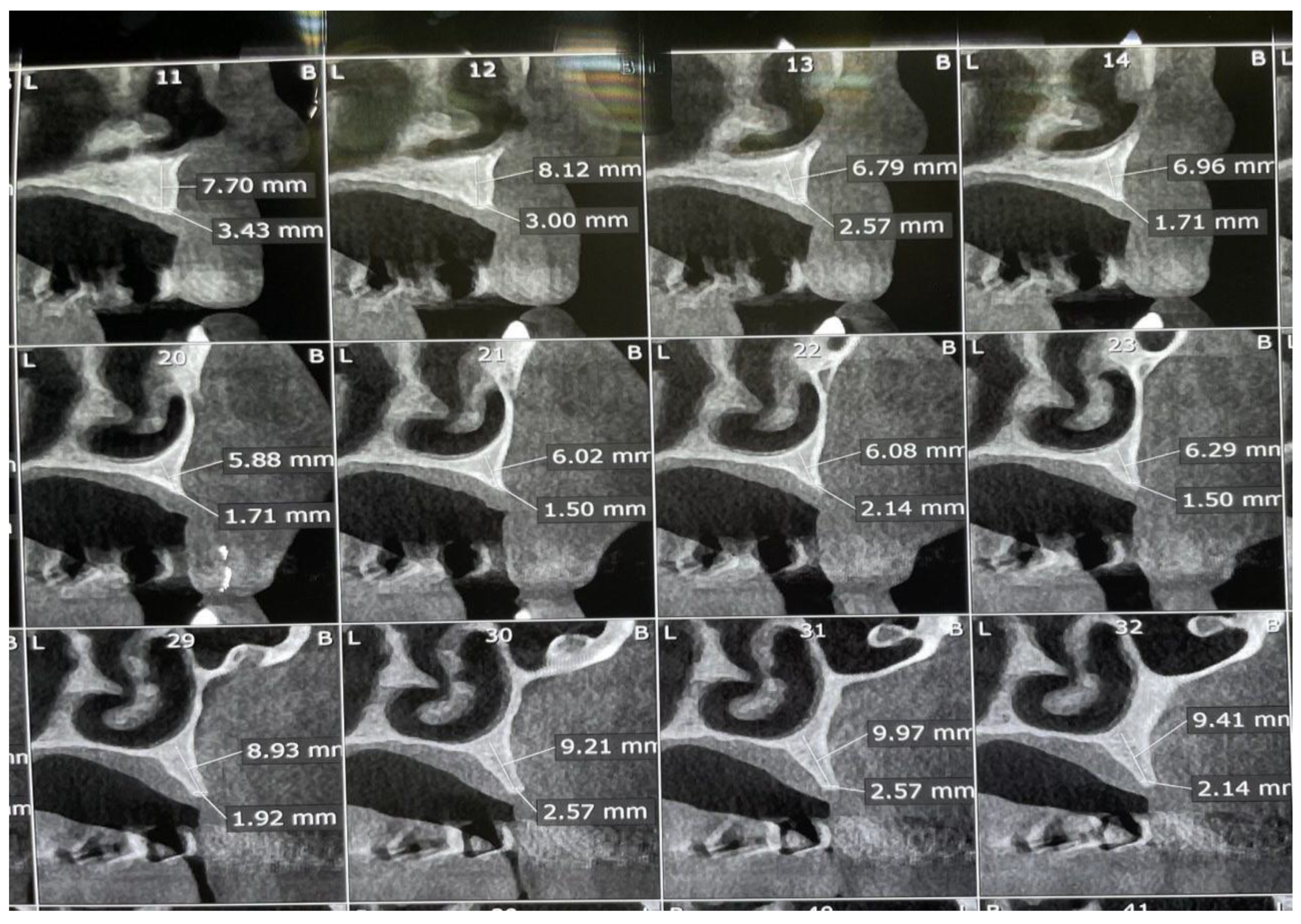
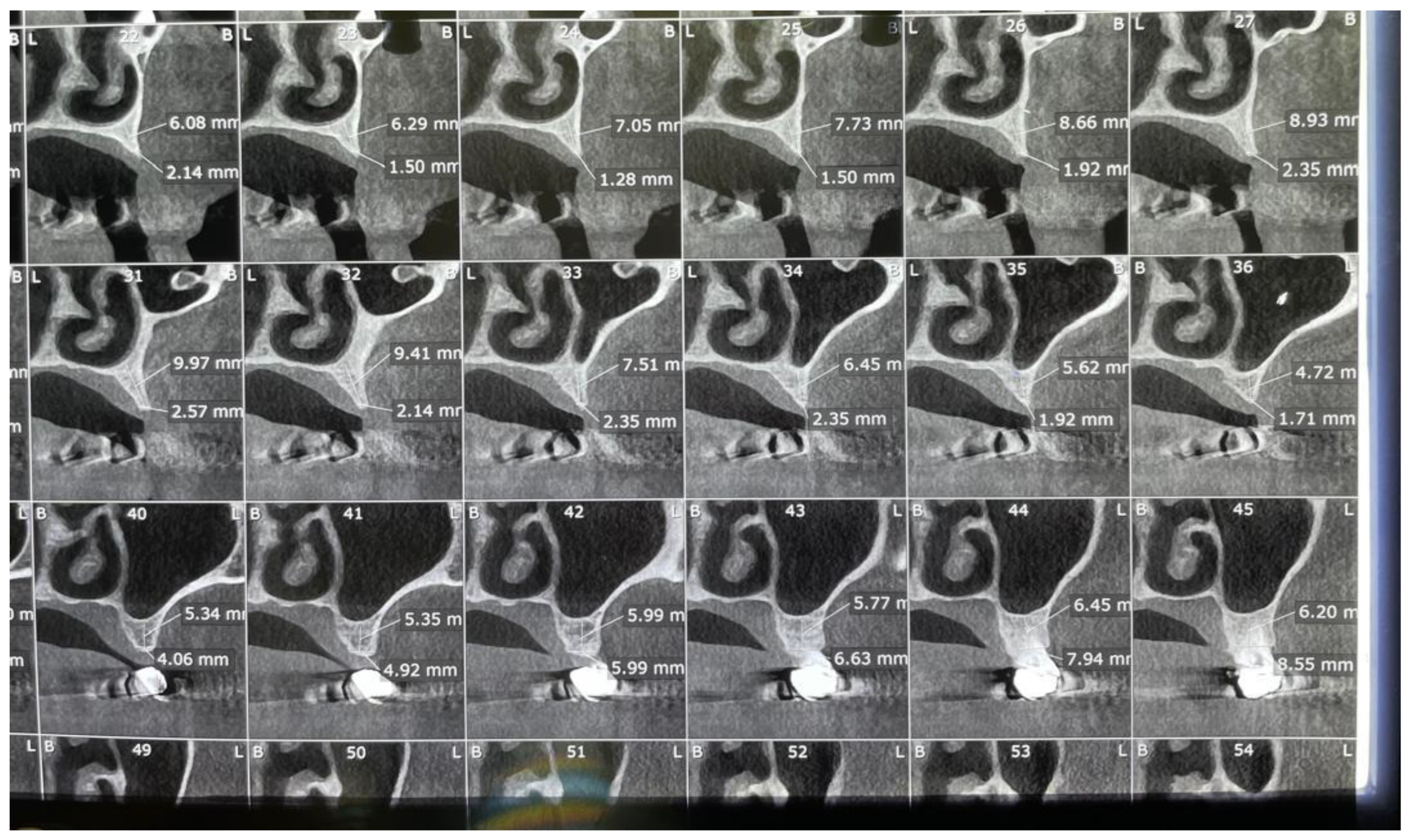
The diagnostic records, including preoperative intraoral photographs, study casts, panoramic radiographs, and CBCT scans, clearly illustrated the pronounced ridge deficiencies and the absence of keratinized mucosa in the anterior maxilla (
Figure 1,
Figure 2, Figure 3,
Figure 4 and
Figure 5).
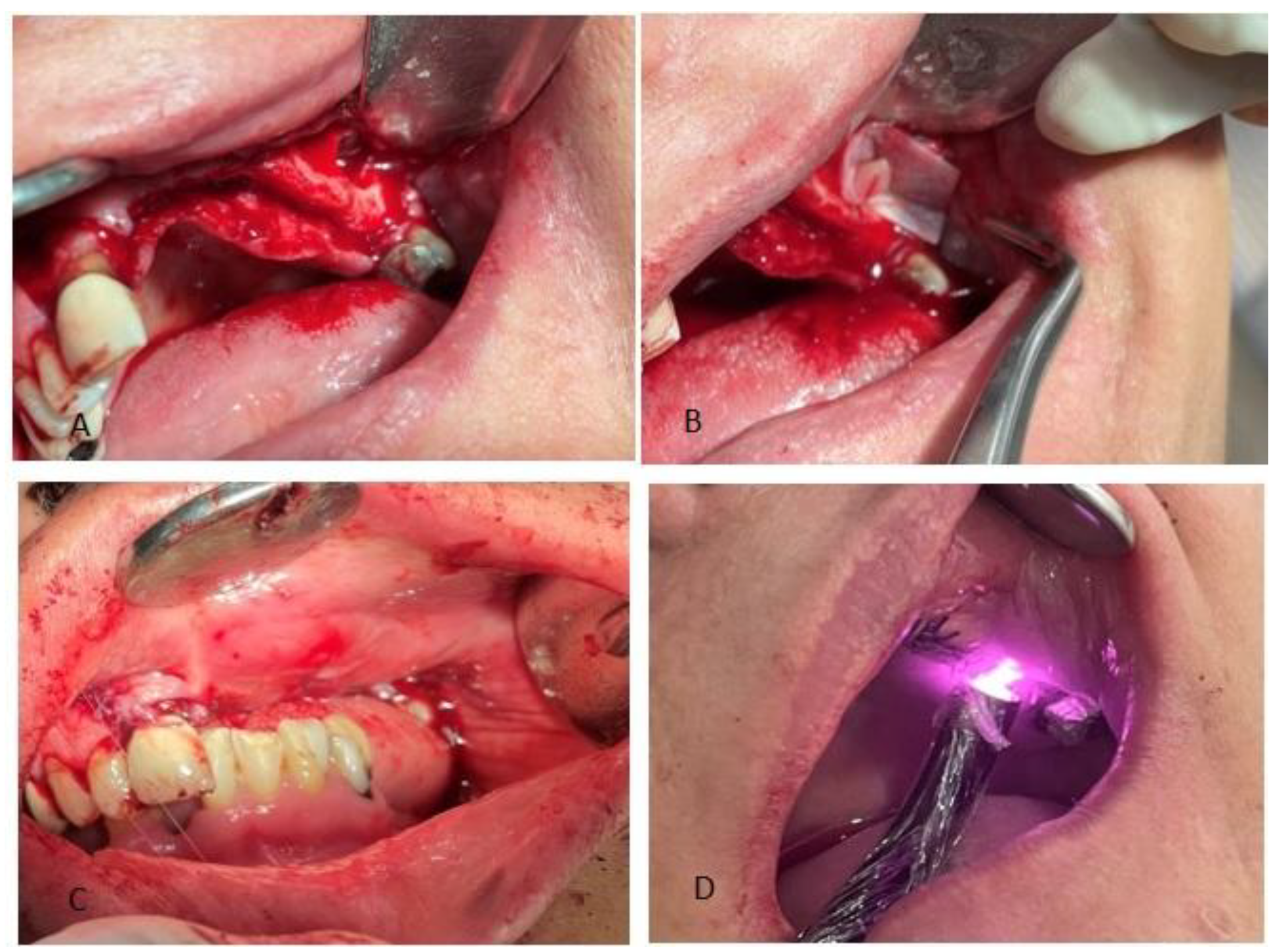
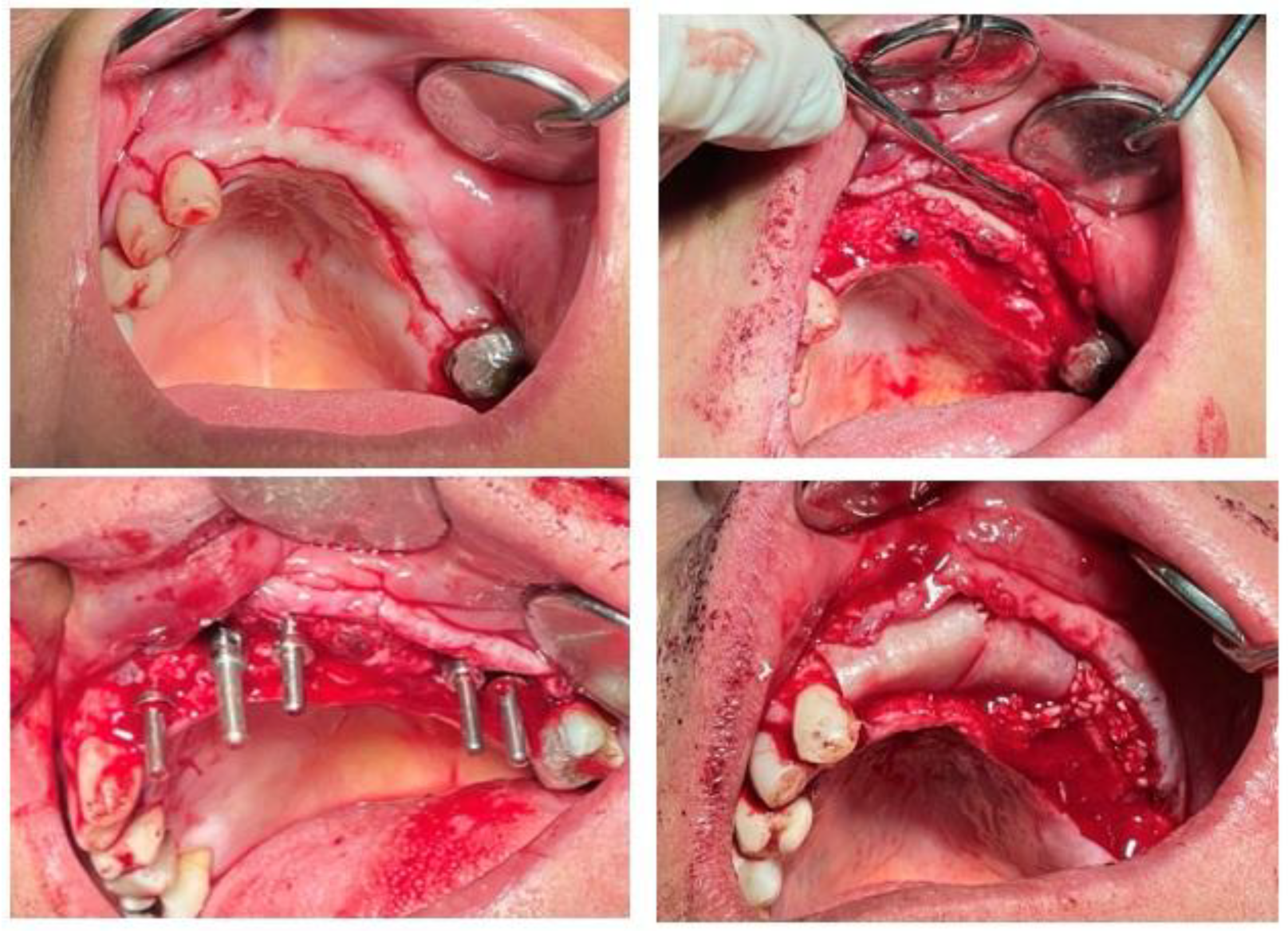
Soft tissue management included a full-thickness flap with palatal incision to mobilize keratinized mucosa from the palate to the buccal aspect. Acellular dermal matrix (ADM) was placed under the flap to enhance soft tissue volume. A laser frenectomy was performed to reduce tension and improve vestibular depth.
The treatment plan involved staged surgical procedures starting with simultaneous horizontal and vertical ridge augmentation using cortical cancellous allograft powder. Two titanium tenting screws were placed to maintain vertical dimension, and two bone screws fixed a customized allograft bone plate to stabilize the graft horizontally. A resorbable collagen membrane was placed over the graft and secured with a single fixation tack. An open sinus lift was performed in the posterior maxilla with allograft placement beneath the elevated Schneiderian membrane and collagen membrane coverage. Following completion of the surgical procedures, low-level laser therapy (LLLT) was applied to promote and accelerate soft tissue healing through photobiomodulation. An 808 nm diode laser was used at a power output of 0.3 W (300 mW), delivering an energy density of 6 J/cm² to the surgical site. The application of LLLT immediately postoperatively is illustrated in
Figure 6.
Postoperative panoramic radiograph confirmed the presence of two tenting screws for vertical augmentation, two bone screws securing the allograft bone plates, and a single tack screw stabilizing the resorbable collagen membrane. The open sinus lift site in the posterior maxilla is also evident (
Figure 7).
Postoperative medication included amoxicillin, metronidazole, ibuprofen, and acetaminophen. Low-level laser therapy was applied during the healing phase to promote tissue regeneration and minimize postoperative discomfort.
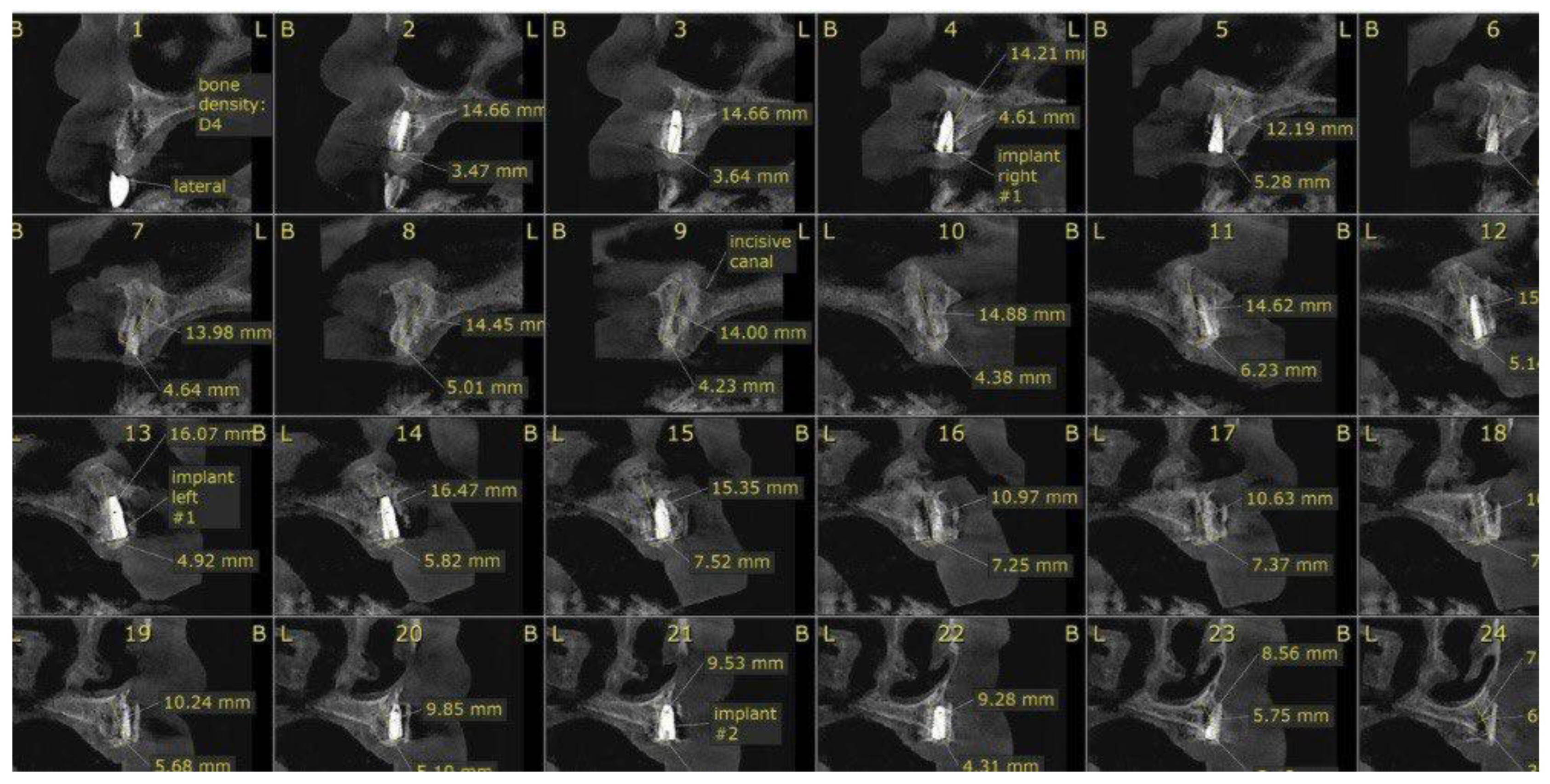
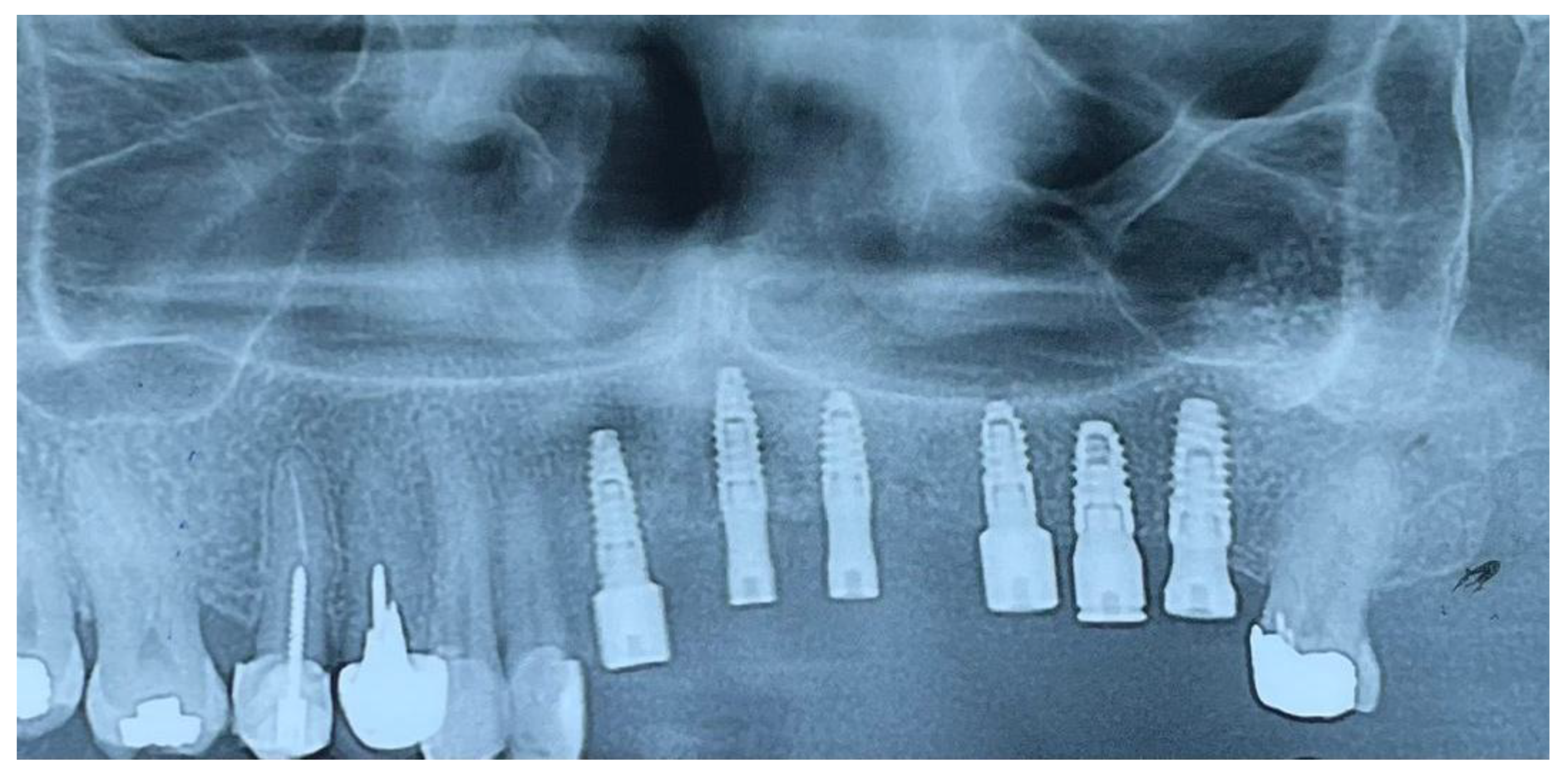
At six months post-augmentation, CBCT evaluation confirmed sufficient bone volume and density to proceed with implant placement. Six IRES Swiss implants were inserted according to the prosthetic plan: two 3.3 × 10 mm fixtures in the maxillary central incisor positions (teeth #1), one 3.3 × 8 mm fixture in the lateral incisor site (tooth #2), one 3.3 × 8 mm fixture in the first premolar site (tooth #4), one 3.7 × 8 mm fixture in the second premolar site (tooth #5), and one 3.7 × 10 mm fixture in the first molar site (tooth #6). Primary stability was achieved in all sites. The postoperative panoramic radiograph confirmed accurate three-dimensional implant positioning, parallelism, and intimate bone contact along the implant surfaces. The surgical procedure began with a crestal alveolar incision to expose the augmented ridge. Sequential osteotomy preparation and placement of IRES Swiss dental implants were performed according to the planned positions. Following implant placement, cortical cancellous allograft was applied around the implants to increase alveolar ridge width, which not only enhanced bone thickness but also improved labial support (
Figure 8) .
CBCT scans at follow-up confirmed stable bone levels and healthy peri-implant soft tissue with no measurable bone loss(
Figure 9).
Healing abutments were connected six months following implant placement
Figure 10. The patient reported no pain, swelling, or complications during the 12-month follow-up period
A final panoramic radiograph was obtained following healing abutment placement to verify implant positioning and peri-implant bone stability (
Figure 11). Two weeks later, a follow-up clinical photograph demonstrated healthy soft tissue contours before referring the patient for the prosthetic phase (
Figure 12).
3. Discussion
The rehabilitation of severe alveolar ridge defects, especially those resulting from traumatic injuries, remains a major challenge in implant dentistry. Both vertical and horizontal deficiencies require meticulous surgical planning and execution to achieve optimal functional and esthetic outcomes [
1,
3]. In this case, the use of a combined approach involving cortical cancellous allograft, allograft bone plates, tenting screws, and open sinus lift allowed for successful simultaneous vertical and horizontal ridge augmentation.
The choice of cortical cancellous allograft provided a suitable osteoconductive scaffold, reducing donor site morbidity associated with autogenous graft harvesting [
4,
5]. Previous studies have demonstrated favorable outcomes using allograft materials in GBR procedures with comparable success rates to autografts when combined with proper fixation techniques [
6,
7].
Space maintenance is critical in vertical ridge augmentation, and the application of tenting screws and allograft bone plates effectively prevented graft collapse and maintained volume during healing [
8,
9]. Fixation of resorbable collagen membranes using tacks further stabilized the graft, minimizing micromovements that could impair bone regeneration [
13,
14].
Soft tissue management is often underestimated but plays a pivotal role in the success of bone augmentation. The lack of keratinized tissue in this patient was addressed by palatal incision and the application of acellular dermal matrix (ADM), which has been shown to improve soft tissue volume and quality without the need for additional donor sites [
9,
10]. Primary closure with a tension-free full-thickness flap reduced the risk of wound dehiscence and graft exposure [
11].
The open sinus lift procedure facilitated implant placement in the posterior maxilla by increasing vertical bone height beneath the sinus membrane. Using allograft beneath the elevated Schneiderian membrane combined with a collagen membrane barrier has been supported by several studies as a predictable technique with high implant survival rates [
12,
15].
Additionally, the adjunctive use of low-level laser therapy (LLLT) contributed to rapid soft tissue healing, decreased postoperative pain and inflammation, and possibly enhanced bone regeneration [
16,
17]. This aligns with clinical reports demonstrating the beneficial effects of LLLT in oral surgical procedures [
18,
19].
At the 12-month follow-up, CBCT imaging confirmed stable bone volume around the implants with no signs of peri-implant bone loss or soft tissue complications. The successful clinical outcome of this case highlights the effectiveness of combining multiple regenerative techniques for complex alveolar defects.
4. Review of the Current Evidence
A focused literature review was conducted using recent clinical trials, systematic reviews, and meta-analyses on horizontal and vertical ridge augmentation, sinus lift procedures, soft tissue regeneration, and adjunctive therapies. Twenty peer-reviewed studies published between 2012 and 2025 were included based on their clinical relevance to the present case.
Bone Augmentation Techniques:
Vorovenci et al. [
1] in a meta-analysis reported mean horizontal bone gains of 4.04 mm for guided bone regeneration (GBR) and 3.66 mm for ridge-split (RS) techniques, with GBR showing greater long-term stability. Chavda and Levin [
16] compared autografts and allografts, concluding that vertical gains with allografts (mean 4.1 mm) approached those of autografts (mean 4.3 mm) without donor site morbidity. A systematic review by Clementini et al. [
17] found implant survival rates of 95–100% in sites augmented via GBR, regardless of graft type.
Allograft Outcomes:
Horizontal augmentation with freeze-dried bone allograft (FDBA) achieved mean width gains of ~2.2 mm in randomized controlled trials [
6,
18]. Customized allograft bone blocks demonstrated minimal resorption at 5-month follow-up [
9]. A case series by BMC Oral Health [
5] showed that the tooth-shell technique (TST) had less graft resorption compared to bone-shell technique in horizontal maxillary augmentation.
Fixation Devices:
Periodontol 2000 [
7] reported mean vertical gains of 4.75 mm with tenting screws and plates, emphasizing their role in space maintenance. Titanium mesh and rigid plate fixation have been identified as predictable methods for atrophic site reconstruction [
8]. Fixation of collagen membranes with tacks reduced micromovement and improved graft stability [
13].
Soft Tissue Regeneration:
Use of acellular dermal matrix (ADM) for increasing keratinized tissue showed consistent improvements in tissue thickness and quality without donor site harvesting [
9,
10]. Palatal tissue mobilization combined with ADM provided stable results in scarred or deficient vestibules [
11].
Sinus Augmentation:
Open sinus lift combined with allograft placement beneath the Schneiderian membrane achieved mean vertical bone height gains of 4–6 mm, with implant survival rates above 92% at 5 years [
12,
14]. Long-term follow-up studies (Chappuis et al. [
15]) demonstrated stable lateral ridge augmentation results when autogenous grafts were combined with GBR.
Adjunctive Low-Level Laser Therapy (LLLT):
LLLT application post-augmentation improved soft tissue healing scores, reduced pain, and enhanced early bone density in randomized trials [
16,
17,
18]. Clinical reports suggest faster epithelialization and reduced postoperative swelling when used after GBR and implant placement [
19].
Summary of Evidence:
The literature supports a combined approach integrating cortical cancellous allograft, rigid fixation devices, sinus lift, ADM for soft tissue, and adjunctive LLLT. This protocol addresses both hard and soft tissue deficiencies, optimizes implant site preparation, and contributes to predictable functional and esthetic outcomes
5. Conclusion
This case report demonstrates that simultaneous vertical and horizontal alveolar ridge augmentation using cortical-cancellous allograft, an allograft bone plate with titanium tenting screws, open sinus lift, and soft tissue management with acellular dermal matrix (ADM) can achieve predictable and stable outcomes in complex post-traumatic maxillary defects. The adjunctive use of low-level laser therapy further enhanced postoperative healing.
Funding
This research received no external funding.
Institutional Review Board Statement
Ethical review and approval were waived for this study due to its nature as a single case report. Written informed consent was obtained from the patient for publication of this case report and accompanying images.
Informed Consent Statement
Written informed consent has been obtained from the patient to publish this paper.
Data Availability Statement
No new data were created or analyzed in this study. Data sharing is not applicable to this article.
Conflicts of Interest
“The authors declare no conflicts of interest.”
Abbreviations
The following abbreviations are used in this manuscript:
| MDPI |
Multidisciplinary Digital Publishing Institute |
| DOAJ |
Directory of open access journals |
| TLA |
Three letter acronym |
| LD |
Linear dichroism |
References
- Vorovenci A, D. Meta-analysis of ridge augmentation procedures: osseodensification, GBR, ridge-split. Biomed Res Int. 2024; avg horizontal gain GBR 4.04 mm, RS 3.66 mm MDPI+4Spandidos Publications+4Wiley Online Library+4.
- Ridge augmentation in implant dentistry. Int J Oral Maxillofac Implants. 2020; review horizontal more stable than vertical PMC.
- Horizontal alveolar ridge augmentation with allogeneic bone block. J Oral Maxillofac Res. 2019; systematic review implant outcomes vs autograft PMC+1.
- Wiley J, Collagen membrane in vertical ridge augmentation: randomized trial. J Clin Periodontol. 2025; non-inferiority trial outcomes arxiv.org+15Wiley Online Library+15link.springer.com+15.
- BMC Oral Health. Tooth shell vs bone shell technique for horizontal maxillary ridge augmentation. 2025; TST lower graft resorption bmcoralhealth.biomedcentral.com.
- Cell Tissue Bank. FDBA + amnion chorion membrane for horizontal ridge defects. 2025; mean gain ~2.2 mm link.springer.com.
- Techniques on vertical ridge augmentation: indications and outcomes. Periodontol 2000. 2023; mean vertical gain 4.75 mm Wiley Online Library.
- Sciedirect review. Titanium mesh for guided bone regeneration in atrophic sites. 2024; predictable method sciencedirect.com+2Spandidos Publications+2.
- Allograft customized bone blocks for ridge reconstruction. Appl Sci. 2021; case report vertical gain, no resorption after 5 mo MDPI+1.
- Regenerative approaches in alveolar bone augmentation. Clin Oral Investig. 2025; materials and outcomes sciencedirect.com.
- 3D printed biodegradable membrane for vertical/horizontal augmentation. Chosun Ob/Gyn Res. 2024; case report with 3D membrane chosunobr.org.
- Innovative 3D ridge augmentation in posterior mandible. Clin Case Reports. 2024; to enable stable implants sciencedirect.com.
- Multidisciplinary vertical ridge defect management. Eur J Med Case Rep. 2023; multidisciplinary approach scienceopen.com.
- Horizontal augmentation techniques in the mandible: systematic review. Int J Implant Dent. 2022; efficacy of graft materials SpringerOpen.
- Chappuis V, Cavusoglu Y, Buser D, von Arx T. Lateral ridge augmentation using autogenous block grafts + GBR: 10-year case series. Clin Implant Dent Relat Res. 2017; high success, long follow-up link.springer.com+1.
- Chavda S, Levin L. Human studies of vertical and horizontal augmentation comparing graft types: systematic review. J Oral Implantol. 2018; compare allograft vs autograft link.springer.com.
- Clementini M et al. Success rate implants in GBR areas: systematic review. Int J Oral Maxillofac Surg. 2012; implant outcomes after augmentation link.springer.com.
- Hashemipoor M et al. Horizontal ridge augmentation using FDBA ± autogenous bone: RCT clinical trial. Clin Implant Dent Relat Res. 2020; histological and radiologic evaluation link.springer.com.
- Holtzclaw D, Tofe R. Primer on amnion-chorion allografts in dental procedures. J Implant Adv Clin Dent. 2017; overview Allograft membranes link.springer.com.
|
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2025 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (http://creativecommons.org/licenses/by/4.0/).