Introduction
Congenital adrenal hyperplasia (CAH), one of the most prevalent inherited disorders, encompasses to a group of autosomal recessive conditions caused by inactivating mutations in single enzymes essential for cortisol biosynthesis. The most common form is due to 21-hydroxylase deficiency, which is associated with genital virilization in 46XX individuals, often necessitating complex surgical interventions for the purpose of restoring normal and functional anatomy [
1]. Genital reconstructive surgeries are technically complex and can lead to intraoperative and postoperative complications, with variable long-term outcomes [
2]. According to a recent systematic review, complications such as clitoral sensitivity loss, vaginal stenosis, and difficulties with penetration remain prevalent after surgery, affecting up to 27% of cases [
3], and significantly impacting long-term outcomes and quality of life [
2,
4]. Sexual dysfunction also remains a key concern despite some surgical advancements[
2,
5].
One common complication of such surgeries that often require re-intervention is vaginal stenosis [
6]. Traditional vaginal dilators are often uncomfortable and poorly adapted to individual anatomy, leading to inconsistent usage and suboptimal results. This study aims to introduce a novel, custom-designed vaginal dilator as a possible solution to these challenges, while also presenting the surgical approach used in this case, highlighting the importance of tailored interventions for optimal outcomes.
Methodology
A 29-year-old virilized female individual (46, XX karyotype), diagnosed with CAH due to 21-hydroxylase deficiency[
1] came to our institution to consider surgery. On initial evaluation, she showed clitoromegaly, fusion of the labia minora and a stenotic vaginal orifice (Prader II), consistent with cases of moderate to severe virilization as previously described[
6,
7]. The first surgical intervention involved a clitoral reduction and the opening of the vaginal introitus. Following this initial surgery, the patient experienced re-stenosis due to inconsistent use of standard dilators as she experienced severe discomfort with the available marketed models. Commercially available vaginal dilators often present significant disadvantages, including inadequate dimensions that fail to fit the patient’s anatomy, frequently being excessively long or rigid. Moreover, their shape is not always appropriate for patients with previous genital reconstructive surgery, as they do not accommodate to potential anatomical variations resulting from genitoplasty. These limitations can contribute to patient discomfort, poor adherence, and ultimately, suboptimal surgical outcomes. Given these concerns, we developed a custom-engineered vaginal dilator was developed in collaboration with the Unit of Biomedical Engineering at the University of Barcelona (Spain).
Written informed consent was obtained from the patient for the publication of this case. The study was conducted in accordance with institutional ethical guidelines.
Design of the Custom-Engineered Vaginal Dilator
The customized dilator was designed as a cylinder with rounded bases, with diameter and length tailored to the patient’s anatomy using MRI imaging. The dilator was crafted from a silicone elastomer (Elastosil
® Vario 15 crosslinked with Elastosil
® Cat Vario in a 10:1 ratio, Wacker Chemie AG, Munich, Germany), a biocompatible material commonly used in biomedical applications [
8]. This material was chosen for its ease of preparation, as it does not require degassing, cures at room temperature in 3 hours, and retains low hardness (15 Shore A), making it ideal for vaginal use. Additionally, the external side of the dilator is equipped with a thread loop to facilitate easy removal by the patient.
The fabrication process involved mixing 100 g of silicone elastomer with 10 g of crosslinker. These components are translucent, as will be the resulting dilator. This mixture was manually stirred for 3 minutes (e.g., with a disposable pipette tip), and poured directly (since the crosslink had already started), into a custom 3D-printed mold, designed using polylactic acid (PLA) as printing ink, in a conventional 3D printer. The dilator dimensions can be easily modified using free 3D-printer software (e.g., UltiMaker Cura®).
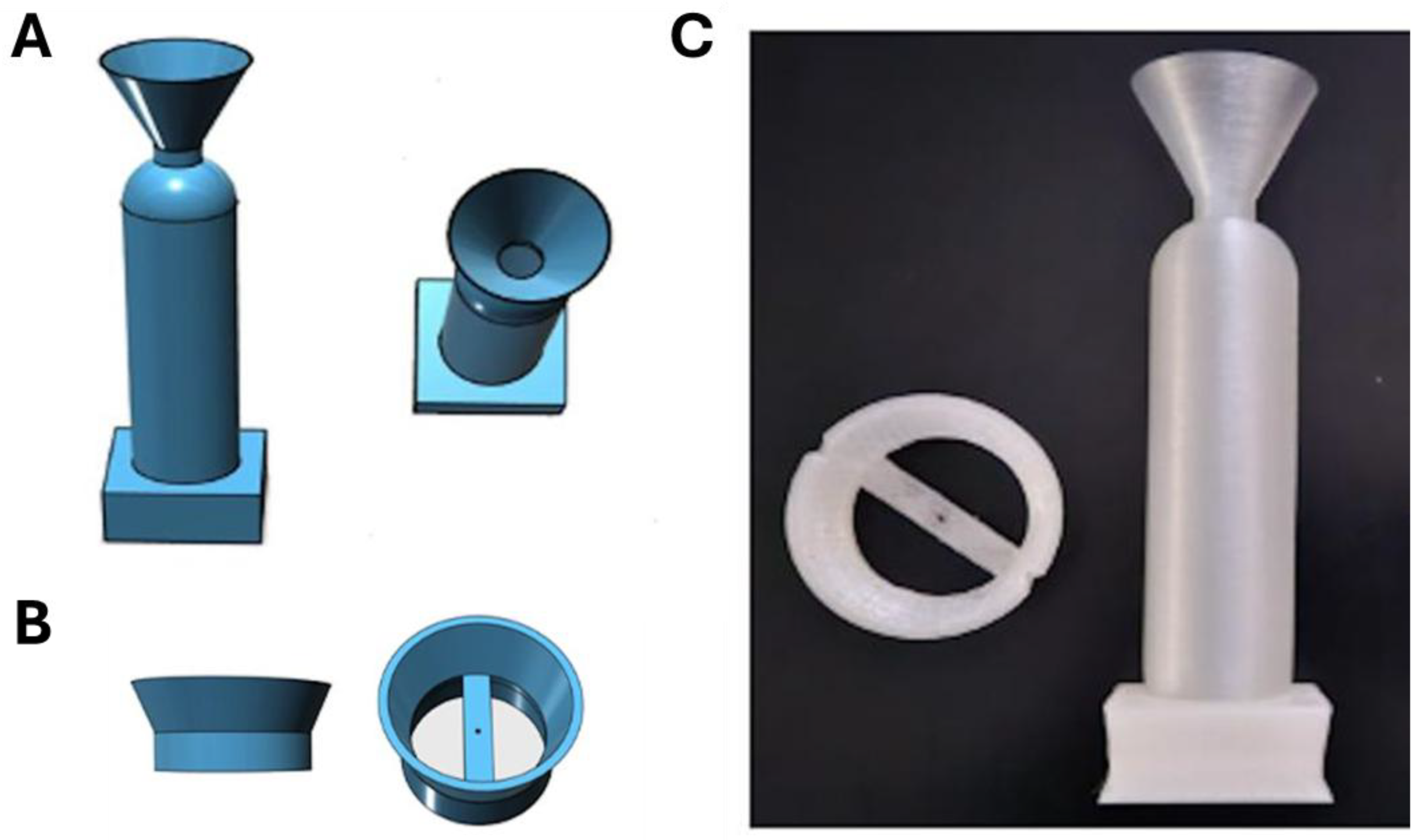
The molding set consists of two pieces as seen in
Figure 1. A disposable mold with a funnel for introducing the silicone mixture (
Figure 1A), and a reusable piece that aligns the external thread loop along the cylinder axis (
Figure 1B). The open-source standard (.STL format.) files allowing the preparation of the three required pieces by any conventional 3D printer can be found as Supplementary Material.
For the retrieval loop we used a polypropylene monofilament (Metric 4, Surgipro®, Medtronic, Madrid, Spain). We selected this surgical thread among others because we verified that it presents less reduction in traction force failure after conventional sterilization with ethylene oxide. A detailed graphical description of how the mold is prepared can be shown in Supplementary Material.
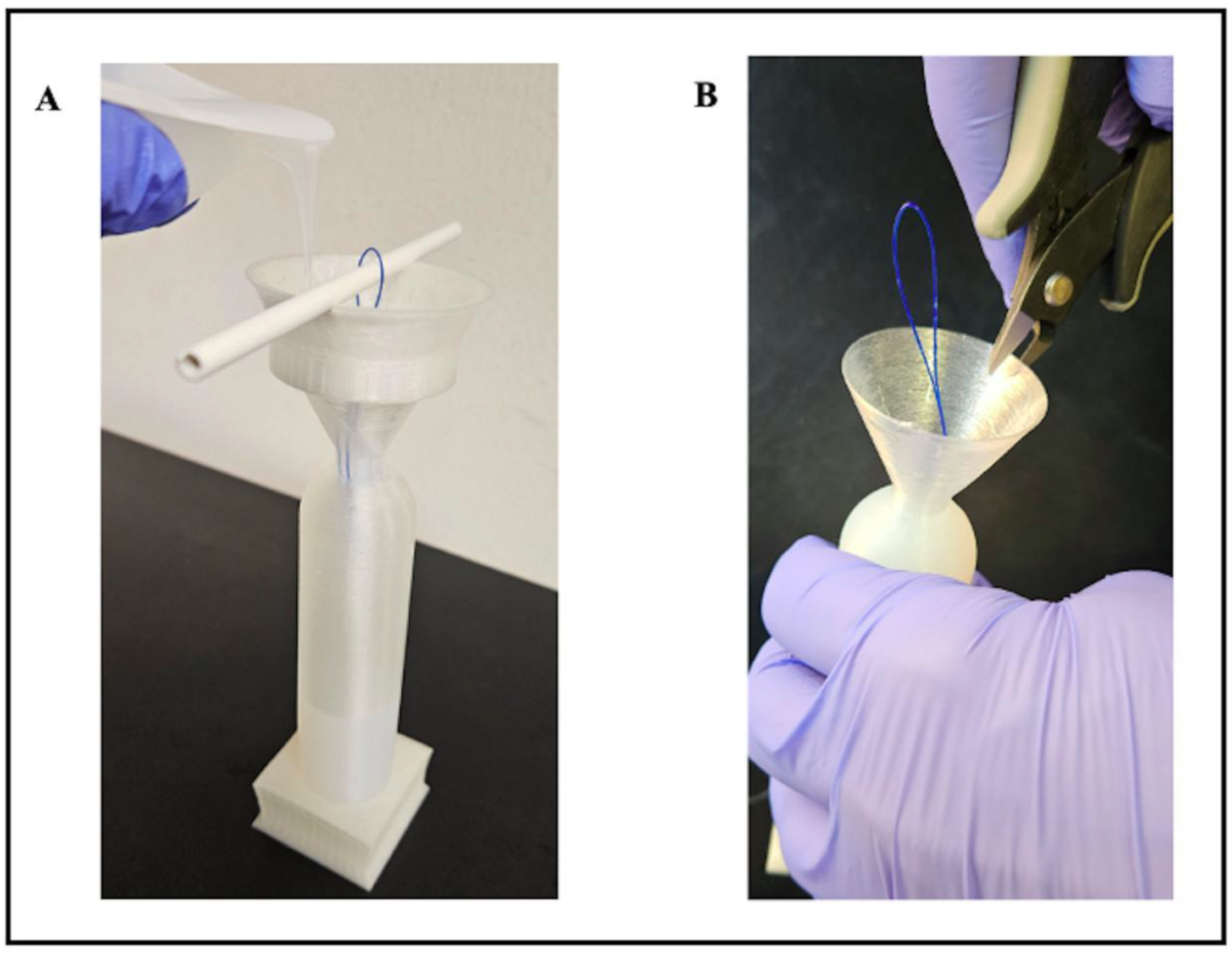
Figure 2A shows how the recently mixed components are placed into the mold. To avoid contact between the mixture and the external part of the filament, the mixture is carefully poured close to the lateral side of the funnel. Pouring should be slow enough to avoid accumulation of components in the narrow section of the funnel. The translucent walls of the mold allow observation of the rising mixture surface. If poured smoothly, no air bubbles will form within the mold (thus, eliminating the need for degassing). The mold should be filled until the surface of the mixture reaches the rounded top of the dilator. A conventional syringe and needle (e.g., for intramuscular injection) can be used to remove or add any small amount of mixture to adjust its level to the rounded tip of the dilator. After curing at room temperature for 4 h, the very thin wall (0.75 mm) of the mold is easily cut to extract the dilator (
Figure 2B). Subsequently, as graphically shown in
Supplementary material, the thread at the bottom of the dilator is cut flush, and the dilator is then dipped once in recently prepared mix of components (silicone plus crosslinker) and allowed to cure (for 2 h) while hold by the retrieval loop. This procedure ensures that the area of the thread cut at the dilator’s bottom is uniformly covered by silicone and the whole dilator has a very smooth surface (regardless of the resolution at which the mold was 3D-printed Finally, the dilator is washed with surgical soap, sterilized with conventional ethylene oxide and made ready for use.
Results
The patient’s sexual function and satisfaction were restored, highlighting the efficacy of a tailored surgical approach and the successful integration of the surgical and engineering innovations.
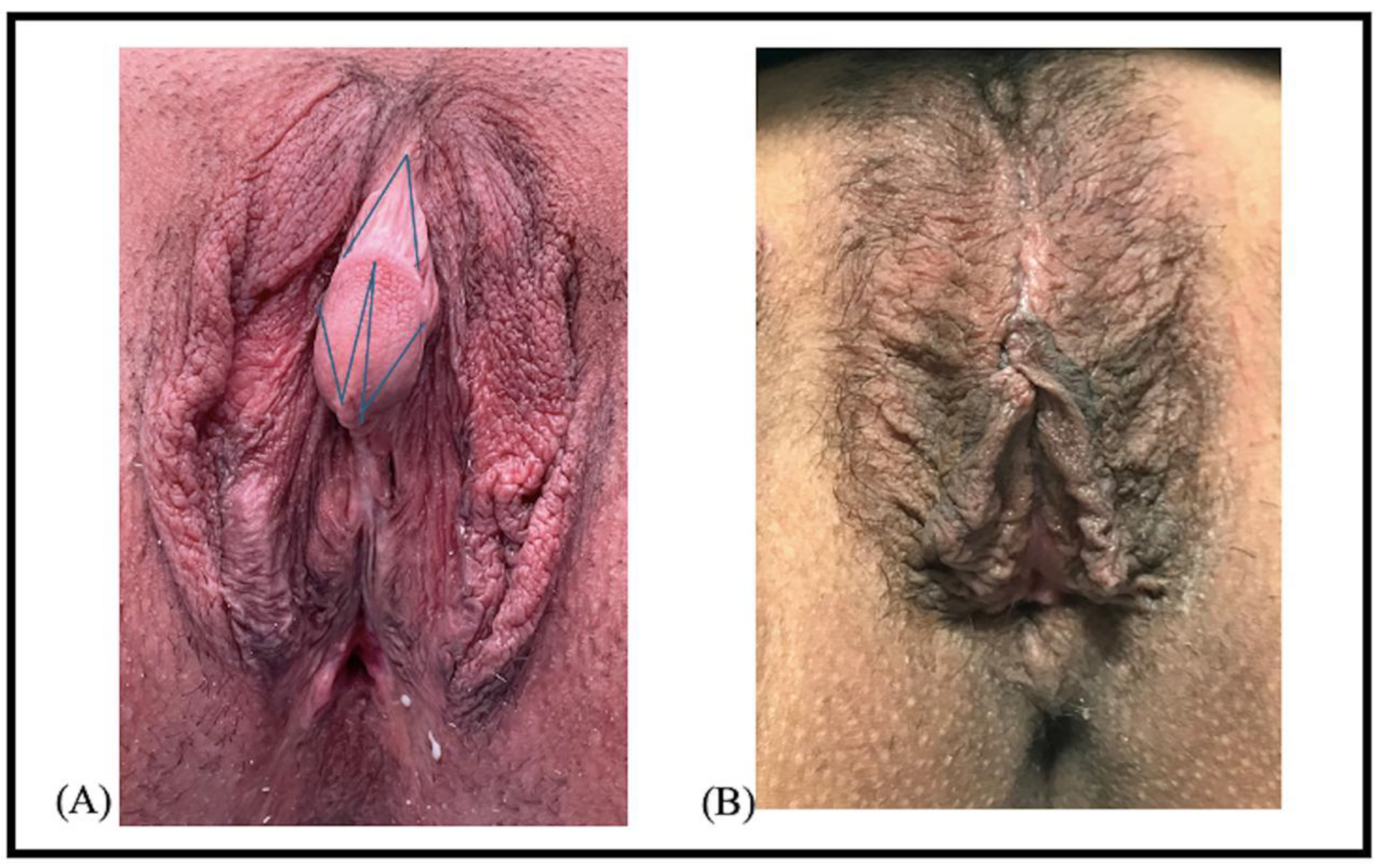
The first surgical approach for clitoral reduction through two V-W shaped (one inverted) and the creation of a clitoral hood is shown in
Figure 3. We carefully preserved the neurovascular bundle, which prevented complications such as pain or loss of sensitivity often reported in similar cases [
4].
More importantly, the custom-designed dilator significantly improved the surgical outcome in this patient. The patient reported high levels of comfort and adherence to the prescribed regimen, with no re-stenosis observed at 12- and 24-month follow-ups. As seen in
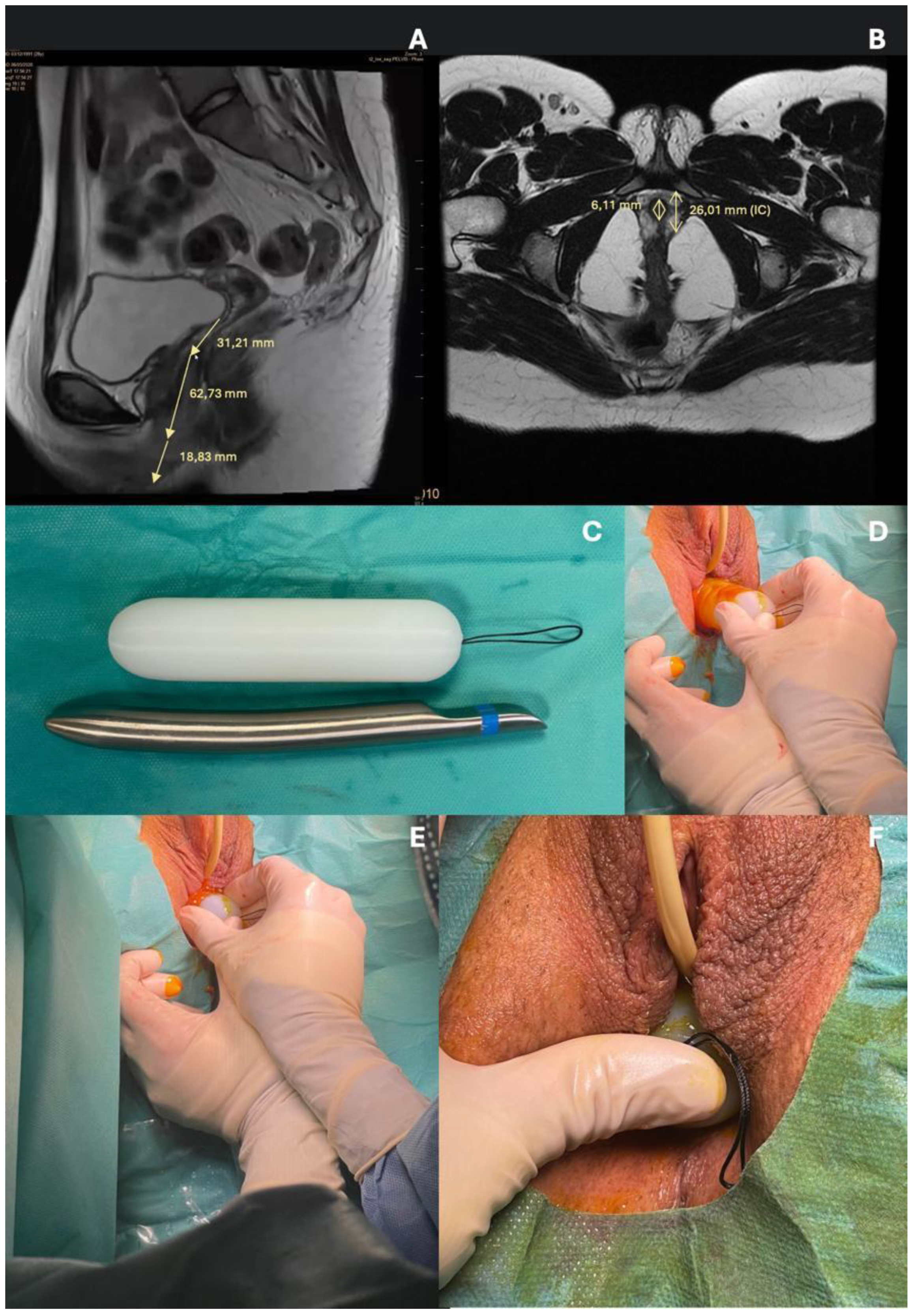
Figure 4, the customed vaginal dilator in this patient measured 26 mm in diameter and 12 cm in length according to her vaginal distance end to end measured by magnetic resonance imaging (
Figure 4A and 4B), and was equipped with the polypropylene monofilament previously described (
Figure 4C). The dilator was inserted immediately post-surgery and used daily to prevent the vaginal introitus from closing (
Figure 4D, 4E and 4F).
Compared to conventional dilators, this methodology provided superior anatomical fit and patient compliance, leading to improved overall outcomes.
Discussion
Congenital adrenal hyperplasia (CAH) is one of the most common autosomal recessive disorders. Despite significant advancements in medical and surgical management over the past two decades [
9], including earlier adoption of single-stage surgeries for genital anomalies, long-term outcomes often remain unsatisfactory [
10]. Complications such as vaginal stenosis, impaired sexual function, and dissatisfaction with cosmetic results continue to be prevalent challenges, as highlighted in retrospective studies [
3]. This underscores the importance of fostering global collaboration among experts to share clinical experiences and improve management strategies for CAH patients.
Our case highlights the value of a tailored approach that integrates surgical techniques with innovative biomedical solutions. The use of custom-designed vaginal dilator tailored to our patient’s anatomy represents a significant advancement over standard models, reducing complications and potentially enhancing patient satisfaction. In our case, the patient effectively reported that the custom-designed dilator was significantly more comfortable and preferable compared to the standard model prescribed initially. The described methodology for preparing the dilator is straightforward, requiring minimal training and preparation time, with the entire process - from mixing to extraction - taking less than 20 minutes. The open-source mold design, (Supplementary material), allows for easy replication and adaptation, making it highly versatile for patient-specific needs.
Moreover, this interdisciplinary approach could have potential applications beyond CAH, including conditions requiring vaginal dilators such as post-radiation therapy or gender-affirming surgeries. Future research should explore the applicability of this methodology, while also evaluating long-term outcomes to further optimize care for these complex cases. By combining clinical expertise with innovative technologies, significant advancements can be made in improving both functional and psychosocial outcomes for CAH patients.
Conclusions
Genital surgery in patients with CAH is technically complex and remains controversial; it is difficult to assess optimal time of surgery, type of surgery considering issues such as potential poor long-term somatic and psychological effects and complications such as pain, incontinence and appearance of fistulas [
7]. The custom biomedical engineered vaginal dilator designed specifically for this patient was essential in obtaining good surgical outcomes, preventing re-stenosis, and improving the patient’s overall quality of life. The collaboration between surgical teams and biomedical engineering departments, as seen in this case, highlights the importance of interdisciplinary innovation in improving patient care [
11].
Supplementary Materials
The following supporting information can be downloaded at the website of this paper posted on Preprints.org.
Institutional Review Board Statement
Ethical approval was not required for this study.
Informed Consent Statement
Informed consent was obtained from the patient.
Data Availability Statement
All relevant data generated or analyzed during this study are included in the published article. No additional datasets were generated.
Artificial Intelligence
No artificial intelligence tools have been used for this research and manuscript writing.
Acknowledgments
The authors wish to thank Mr. Miguel A. Martínez.Lázaro (Unit of Biophysics and Bioengineering, University of Barcelona) for his technical contribution.
Conflicts of Interest
Authors declare no competing interests.
Code Availability
The open-source standard (.STL format.) files allowing the preparation of the three required pieces by any conventional 3D printer can be found as Supplementary material.
References
- L. C. Wang and D. P. Poppas. Surgical outcomes and complications of reconstructive surgery in the female congenital adrenal hyperplasia patient: What every endocrinologist should know. J Steroid Biochem Mol Biol. 2017; 165: 137–144. [CrossRef]
- R. Krysiak, A. Drosdzol-Cop, V. Skrzypulec-Plinta, and B. Okopien, Sexual Function and Depressive Symptoms in Young Women With Nonclassic Congenital Adrenal Hyperplasia J Sex Med. 2016;13(1): 34–39. [CrossRef]
- J. Almasri et al. Genital reconstructive surgery in females with congenital adrenal hyperplasia: A systematic review and meta-analysis. J Clin Endocrinol Metab. 2018;103(11): 4089–4096. [CrossRef]
- A. Zainuddin et al. Malaysian females with congenital adrenal hyperplasia: Surgical outcomes and attitudes. Front Pediatr. 2019;7. [CrossRef]
- M. Dwiggins, B. Brookner, K. Fowler, P. Veeraraghavan, V. Gomez-Lobo, and D. P. Merke. Multidimensional aspects of female sexual function in congenital adrenal hyperplasia: A case-control study. J Endocr Soc. 2020; 4(11):144. [CrossRef]
- S. Hennayake et al. 45 years’ experience with early childhood anatomical technique of feminising genitoplasty for 46 XX Congenital Adrenal Hyperplasia –observations of vaginal introital anatomy and its relationship to the perineal body. J Pediatr Urol. 2022;18(5): 611-8. [CrossRef]
- M. Ogilvie, N. S. Crouch, G. Rumsby, S. M. Creighton, L. M. Liao, and G. S. Conway. Congenital adrenal hyperplasia in adults: A review of medical, surgical and psychological issues. Clin Endocrinol. 2006;64(1):2-11. [CrossRef]
- M. Zare, E. R. Ghomi, P. D. Venkatraman, and S. Ramakrishna. Silicone-based biomaterials for biomedical applications: Antimicrobial strategies and 3D printing technologies. J Appl Polym Sci. 2021;138(38):1-18. [CrossRef]
- P. W. Speiser and P. C. White. Congenital adrenal hyperplasia. N Engl J Med. 2003;349:776-88. [CrossRef]
- Simeoli et al. Severe impact of late diagnosis of congenital adrenal hyperplasia on gender identity, sexual orientation and function: case report and review of the literature. Front Genet. 2022:13;1-12. [CrossRef]
- J. Otero, J. M. Pearce, D. Gozal, and R. Farré. Open-source design of medical devices. Nat Rev Bioeng. 2024:2(4);280–281. [CrossRef]
|
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2025 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (http://creativecommons.org/licenses/by/4.0/).