1. Introduction
Metabolic dysfunction-associated steatotic liver disease (MASLD), formerly known as metabolic dysfunction-associated fatty liver disease (MAFLD) and non-alcoholic fatty liver disease (NAFLD), encompasses a broad spectrum of hepatic and extra-hepatic pathophysiological and clinical manifestations resulting from the liver steatosis [
1]. According to the current definition, MASLD is diagnosed after excluding causes of steatosis other than metabolic ones [
2,
3].
Prevalence of MASLD is continuously rising, making it is the most common liver disease worldwide, affecting approximately 20–30% of adults [
4,
5]. The risk factors for MASLD are well established with strong association observed with obesity, poor nutrition, dyslipidaemia, and sedentary lifestyle. These factors contribute to lipotoxicity, reactive oxygen species production, dysbiosis of intestinal microbiome, genetic predisposition, and the induction of proinflammatory immune mediators [
6].
Consequently, patients with MASLD not only present with a worsened cardiometabolic profile [
7,
8] but are also at a significantly higher risk of death from cardiovascular disease than from liver diseases complications [
9].
The heterogeneity between females and males in the prevalence, risk factors, and mechanisms of MASLD has long been recognized but remains incompletely understood. Regarding sex differences, the prevalence and severity of MASLD are higher in men than in women during the reproductive age. However, after menopause, the condition becomes more frequent in women, suggesting a protective effect of oestrogens [
10]. Additionally, oestradiol influences fatty acid synthase expression in hepatic and adipose cells, while saturated fatty acids induce endoplasmic reticulum stress and increase mitochondrial free radical generation, leading to cellular injury and liver steatosis [
11].
Moreover, sex and age differences are also observed in the prevalence of diabetes mellitus type 2 (T2DM), visceral adipose tissue accumulation, and components of metabolic syndrome- all major risk factors for MASLD [
12,
13].
There is a lack of evidence exploring sex-related differences in the epidemiological risk factors for MASLD. Therefore, we aimed to investigate the prevalence of MASLD and its characteristics in men and women.
2. Materials and Methods
2.1. Study Design
The prospective, multicentre, and observational study involved patients from the Polish Gallstone Surgery Registry. Patients who underwent cholecystectomy due to gallstone disease were consecutively enrolled across six surgical hospitals, including four academic centres and two regional hospitals, providing a comprehensive overview of surgical approaches in Poland. The data included patients admitted to one of the participating centres between 2019 and 2022, either for elective or emergency procedures. To ensure an unbiased selection process and create a cohort reflective of real-world conditions, no specific exclusion criteria were applied.
2.2. Patient Involvement
Consecutively hospitalised patients who underwent cholecystectomy were included in the study. MASLD was diagnosed based on the current criteria recommended in June 2023 by experts from the following hepatology societies: European Association for the Study of the Liver (EASL), La Asociación Latinoamericana para el Estudio del Hígado (ALEH) and the American Association for the Study of Liver Diseases (AASLD) [
10].
The diagnostic criteria of MASLD included the presence of liver steatosis with at least one cardiometabolic factors:
- BMI ≥ 25 kg/m2,
- fasting serum glucose ≥ 5.6 mmol/L (100 mg/dL) or 2-hour post-load glucose level ≥ 7.8 mmol/L (≥ 140 mg/dL) or HbA1c ≥ 5.7% (39 mmol/L) or diabetes mellitus type 2 (T2DM) or treatment for T2DM,
- blood pressure ≥ 130/85 mmHg or specific antihypertensive drug treatment,
- plasma triglycerides ≥ 1.7 mmol/L (150 mg/dL) or lipid lowering treatment,
- plasma high-density lipoprotein cholesterol (HDL-C) ≤ 1.0 mmol/L (40 mg/dL) - men and ≤ 1.3 mmol/L (50 mg/dL) - women or lipid lowering treatment.
In the presented study two last factors were collectively referred to as atherogenic dyslipidaemia.
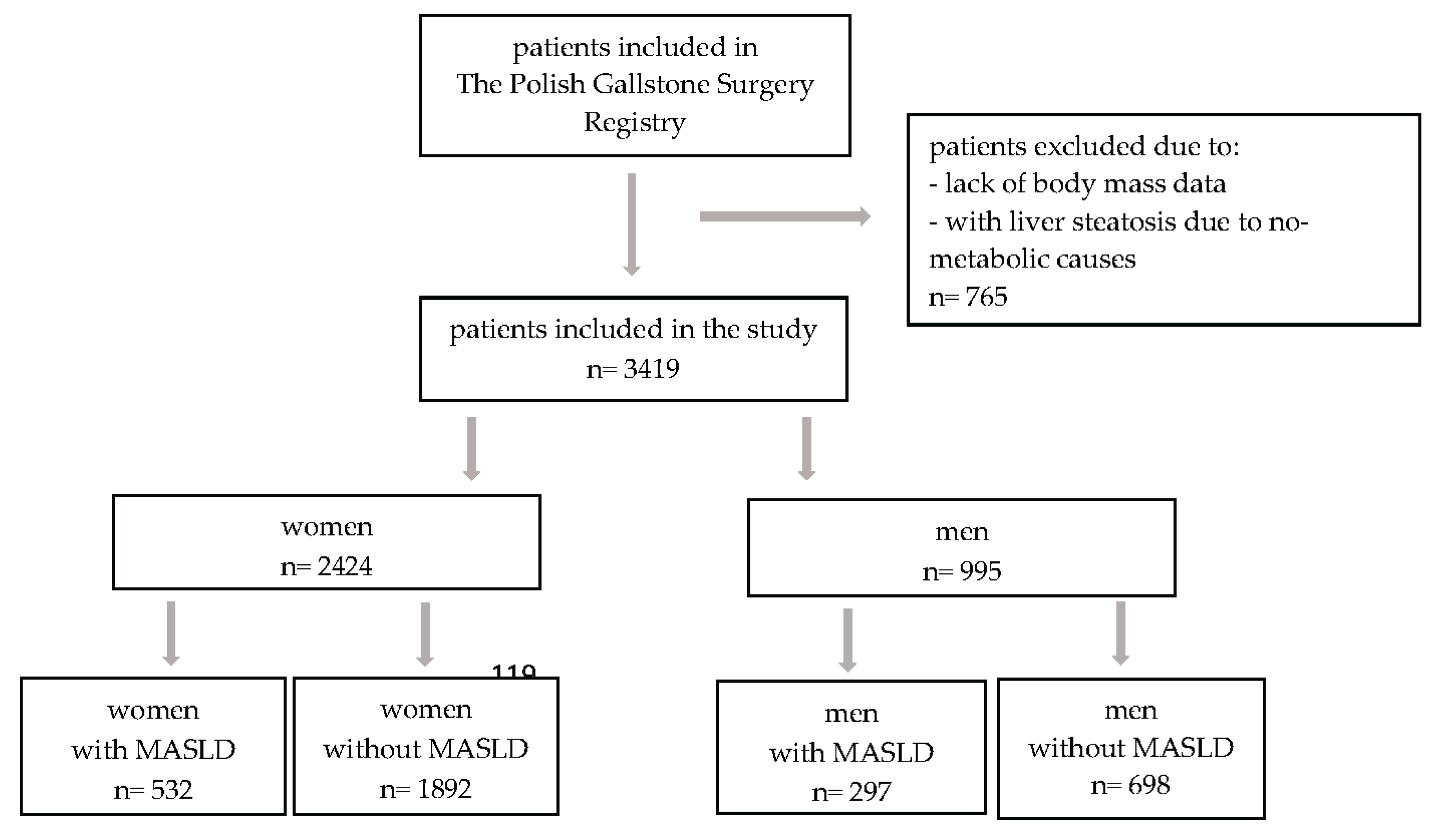
Patients with incomplete diagnostic data for MASLD, particularly those without BMI information, as well as individuals with liver steatosis due to non-metabolic causes, were excluded from the analysis (
Figure 1).
The study was approved by the Ethics Committee of the Collegium Medicum of The Jan Kochanowski University (104/2022). This work adhered to the ethical guidelines outlined in the Declaration of Helsinki and its subsequent amendments. The requirement for patient informed consent was waived, as this was a retrospective study conducted exclusively using de-identified data.
2.3. Statistical Analyses
Continuous data were described using means and standard deviations, while categorical data were summarized as frequencies and percentages. Groups comparisons were conducted using the chi-square or Fisher exact test for categorical variables and t-test or Mann-Whitney test for continuous variables. Univariable and multivariable analyses were performed using logistic regression models. For these analyses, odds ratios (OR) with 95% confidence intervals (95% CI) were calculated. A two-tailed p-value <0.05 was considered statistically significant. All statistical analyses were conducted using the R software package version 4.0.3.
3. Results
3.1. Patient Characteristics
A total of 3,419 participants were analyzed, including 995 men (29.1%) and 2,424 women (70.9%). Th
e mean age of the study
population was 54.8 years (SD: 15.3). Among the participants, 27 (0.8%) were underweight, 849 (24.8%) had a normal body mass, 1,310 (38.3%) were overweight, and 1,233 (36.1%) had obesity. Hypertension was diagnosed in 1,433 patients (41.9%), T2DM or prediabetes in 519 patients (15.2 %), and atherogenic dyslipidemia in 432 patients (12.6%). The baseline characteristics of the study participants according to sex are presented in
Table 1.
3.2. Prevalence of MASLD in Men and Women
Among the patients included in the study, MASLD was diagnosed in 829 patients (24.2%). Its prevalence was significantly higher in men (n=297, 29.8%) than in women (n=532, 21.9%) p<0.0001). Lean MASLD was diagnosed in 94 patients (11.3% of those with MASLD), including 63 women (8.9% of women without overweight/obesity) and 31 men (17.2% of men without overweight/obesity), p=0.0012. MASLD in patients with overweight/obesity was diagnosed in 469 women (27.3% of them with overweight/obesity) and in 266 men (32.6% of them with overweight/obesity), p=0.0057.
3.3. Prevalence of Cardiometabolic MASLD Diagnostic Criteria in Men and Women According to BMI
Most patients met two diagnostic criteria for MASLD diagnosis. No significant differences were observed in the number of diagnostic criteria between men and women.
Table 2 presents the number of diagnostic criteria by sex.
In the normal body mass group, hypertension, T2DM or prediabetes, and atherogenic dyslipidemia were diagnosed more frequently in men than in women (37.7% vs 23.4%; 11.2% vs 5.7%; 14.0% vs 6.7%). In contrast, no significant differences in the incidence of these conditions were observed between male and female patients in the overweight group (
Table 3).
3.4. Comparison of Men and Women with MASLD
In the present study, women and men with MASLD did not differ significantly in age (59.6 vs 58.5, p=0.2383). The proportion of patients with MASLD and obesity was not statistically higher in women than in men (57.3% vs 50.5%, p=0.0516). However, gender-related differences were observed across obesity classes. Among patients with MASLD and obesity, class I obesity was diagnosed in 180 women (58.8%) and 107 men (71.3%), p=0.0094, class II obesity was diagnosed in 82 women (26.8%) and 27 men (18%), p=0.0385 and class III obesity was observed in 44 women (14.4%) and 16 men (10.7%), p=0.2705.
The clinical characteristics of men and women with MASLD were similar, with no significant differences in the incidence of hypertension, T2DM or prediabetes, atherogenic dyslipidemia, heart failure or atrial fibrillation (
Table 1).
3.5. Prevalence of MASLD and Stratification by Age, BMI, and Metabolic Disorder
The prevalence of MASLD was not linearly associated with age (
Figure 2). In the overall population, the prevalence gradually increased with age, peaking at 32.1% in the 70-79 age group. Interestingly, in men, the prevalence of MASLD rose sharply between the ages of 40-49 and remained stable until age 79, reaching a peak of 33% in the 70-79 age group. In contrast, MASLD prevalence in women gradually increased in the 50-59 age range, peaking at 33.3% between ages 70-79. As expected, the lowest incidence of MASLD in both women and men was observed in the < 30 and ≥ 80 age groups.
The prevalence rates of MASLD in different cardiometabolic groups by sex differed only in patients with overweight and obesity, with a higher incidence in men than in women (32.6% vs 27.2%, p=0.0057). In patients with hypertension, with T2DM or prediabetes, and with atherogenic dyslipidemia, the prevalence of MASLD did not differ between women and men. (
Table 4).
3.6. Risk Factors for MASLD
The relationship between MASLD, age and BMI is presented in
Table 5, which shows the incidence of MASLD across BMI groups and various age categories.
Independent of sex, each age group was associated with MASLD incidence, with a higher risk observed in older individuals. However, this observation does not apply to patients over 80 years of age. In both men and women, the highest risk of MASLD was observed in the 70-79 age group. As expected, the risk increased with an increase in BMI. In patients with BMI ≥25 kg/m2, the risk is significantly higher in women than in men. Notably, it increased significantly for both men and women when the BMI was ≥30 kg/m2 and reached ORs of 5.51 (95% CI 4.10-7.40) for women and 3.44 (95% CI 2.21-5.34) for men.
4. Discussion
The prevalence of MASLD appears to differ between men and women depending on age and the presence of comorbidities. The major findings of this study are as follows. First, our country-specific registry data revealed that the incidence of MASLD is higher in men than in women. Second, the incidence of MASLD increases with age and in both sexes, reaching a peak between 70 and 79 years. Third, the higher the body weight, the greater the risk of developing MASLD, with this relationship being particularly pronounced in women.
Our findings indicate that MASLD poses a significant burden on the population undergoing cholecystectomy, with an overall prevalence of 24.2%. Although the study population consists of patients with gallstone disease, the incidence of MASLD is similar to that in the general population. Notably, we observed a sex-specific difference in MASLD prevalence, with men having a higher prevalence (29.8%) than women (21.9%), suggesting that men are more susceptible to MASLD than women. The higher prevalence of MASLD in men may increase their vulnerability to chronic diseases such as hypertension, cardiovascular disease, T2DM, and stroke.
Crudele et al. [
14] reported that MASLD was diagnosed in 59% of patients with metabolic syndrome, with a higher incidence in men. A Spanish study found the overall prevalence of NAFLD to be 19.1%, with rates of 27.9% in men and 6.8% in women, increasing across age groups [
15]. Data from the National Health and Nutrition Examination Survey III (NHANES III) also indicated that MASLD is more common in men than in women. Similarly, Chang et al. [
17] demonstrated a clear male predominance in MAFLD prevalence, with a higher rate in men (45.7%) than in women (23.9%). It is important to note that MAFLD is more frequently observed in Asian populations [
18,
19]. However, another study reported a higher prevalence in women (31.7%) compared to men (25.5%), which may be attributed to a smaller sample size and, more significantly, differences in the age distribution of the study population [
20]. That study included patients with a mean age of 67 years, whereas the mean age in our study was 55.
The inclusion of a higher proportion of postmenopausal women may have influenced the results, as estrogen has been shown to have a protective effect against MASLD [
21,
22,
23]. Studies on sex differences in MASLD show that it is more prevalent in men than in women of reproductive age. However, after menopause, this difference diminishes, exposing older women to higher rates of MASLD. The results of the Polish Gallstone Surgery Registry showed that the incidence of MASLD increased with age, with the highest percentage of patients observed in the 70–79 age group for both women and men. Chang et al. [
17] reported the highest prevalence of MAFLD in the 50–59 age group, suggesting that MAFLD is more common in middle-aged individuals. A high proportion of MASLD diagnoses in men was observed between 40 and 49 years, whereas in women it was most common between 50 and 59 years. This difference may be influenced by hormonal changes in women, making them more susceptible to MASLD at an older age. Conversely, younger men have a higher incidence of metabolic and cardiovascular diseases, which may predispose them to develop MASLD at an earlier age than women.
Interestingly, in the present study, the incidence of MASLD did not differ between men and women in the subgroups of patients with hypertension, T2DM/prediabetes, or atherogenic dyslipidemia. Numerous epidemiological studies have shown that overweight and obesity are significant, independent, and modifiable risk factors for MASLD, as evidenced by the parallel rise in obesity rates and MASLD prevalence [
7,
24]. Chen et al. [
18] also identified a strong, nearly linear relationship between MASLD incidence and increased BMI. Regardless of other metabolic abnormalities, patients with obesity face a higher risk of developing MASLD.
However, our subgroup analysis of age and BMI revealed distinct sex differences, showing that women are more prone to MASLD than men at any given BMI. Chen et al. [
18] reported similar findings. Furthermore, our data demonstrated a significant link between MASLD, BMI, and age, with higher BMI and older age strongly associated with greater prevalence. These findings suggest that both elevated BMI and advancing age may be key factors in the onset and progression of MASLD.
5. Limitations
This study has inherent limitations. The primary limitation is the specific population analyzed - patients who underwent cholecystectomy for gallstone disease. Consequently, these findings may not be generalizable to a broader group, even though the incidence of MASLD observed in this study aligns with that of the general population. Additionally, it is important to note that the study cohort consists predominantly of women, which could have influenced the results.
6. Conclusions
Our results suggest a high prevalence of MASLD and other metabolic conditions, particularly obesity, in patients undergoing cholecystectomies. In both men and women, the prevalence of MASLD increased with age and BMI. Prioritizing the prevention and management of metabolic disorders, especially obesity, is crucial for the effective treatment of MASLD. These findings underscore the importance of developing personalized interventions to prevent and manage MASLD in both women and men.
Author Contributions
Conceptualization, I.G.-G., L.N., K.R.-S., P.M.; methodology, I.G.-G., L.N., R.M., K.R.-S., M.C., K.M., M.P., K.R.; formal analysis, I.G.-G., L.N., M.K., R.M., K.R.-S., M.C., P.R., K.R., M.S., M.Sz.; investigation, I.G.-G., L.N., M.K., R.M., M.N., M.C., S.L.., L.K., P.R.; resources, I.G.-G., R.M., M.N., K.R.-S., S.L., K.M., L.K., M.P., P.R., K.R., M.S., M.Sz.; data curation, I.G.-G., L.N., M.K., R.M., M.N., S.L., K.M., L.K., M.S., M.Sz.; writing-original draft preparation, I.G.-G., L.N., M.K., P.M., M.P.; writing-review and editing, R.M., K.R.-S.; project administration, I.G.-G., L.N., P.M. All authors have read and agreed to the published version of the manuscript.
Funding
The science project of Jan Kochanowski University in Kielce, Poland (project number, SUPS.RN.25.029; to IG-G).
Institutional Review Board Statement
The study was conducted in accordance with the Declaration of Helsinki, and approved by the Ethics Committee of the Collegium Medicum The Jan Kochanowski University (104/2022) – November 4, 2022.
Informed Consent Statement
The requirement for patient informed consent was waived.
Conflicts of Interest
The authors declare no conflict of interest.
References
- Rinella, M.E.; Lazarus, J.V.; Ratziu, V.; Francque, S.M.; Sanyal, A.J.; Kanwal, F.; Romero, D.; Abdelmalek, M.F.; Anstee, Q.M.; Arab, J.P., et al. NAFLD Nomenclature consensus group. A multi-society Delphi consensus statement on new fatty liver disease nomenclature. J. Hepatol. 2023, 6, 1542-1556. [CrossRef]
- Janczura, J.; Brzdęk, M.; Dobrowolska, K.; Flisiak, R.; Martonik, D.; Brzdęk, K., Pleśniak, R.; Kukla-Woźnica, D.; Wajdowicz, M.; Zarębska-Michaluk, D. Steatotic liver disease in patients treated for chronic hepatitis B. Pol. Arch. Intern. Med. 2025, 31, 16942. [CrossRef]
- Dixon, W.; Corey, K.E.; Luther, J.; Goodman, R.P.; Schaefer, E.A. Prevalence and Clinical Correlation of Cardiometabolic Risk Factors in Alcohol-Related Liver Disease and Metabolic Dysfunction and Alcohol Associated Liver Disease (MetALD). J. Clin. Exp. Hepatol. 2025, 15, 102492. [CrossRef]
- Pimpin, L.; Cortez-Pinto, H.; Negro, F.; Corbould, E.; Lazarus, J.V.; Webber, L.; Sheron, N. Burden of liver disease in Europe: Epidemiology and analysis of risk factors to identify prevention policies. J. Hepatol. 2018, 69, 718-735. [CrossRef]
- Yang, A. H.; Tincopa, M. A.; Tavaglione, F.; Ajmera, V. H.; Richards, L. M.; Amangurbanova, M.; Butcher, C.; Hernandez, C.; Madamba, E.; Singh, S. Prevalence of steatotic liver disease, advanced fibrosis and cirrhosis among community-dwelling overweight and obese individuals in the USA. Gut. 2024, 73, 2045-2053. [CrossRef]
- Hong, S.; Sun, L.; Hao, Y.; Li, P.; Zhou, Y.; Liang, X.; Hu, J.; Wei, H. From NAFLD to MASLD: when metabolic comorbidity matters. Ann. Hepatol. 2024, 29, 101281. [CrossRef]
- Zhao, D.; Zheng, X.; Wang, L.; Xie, Y.; Chen, Y.; Zhang Y. Overlap prevalence and interaction effect of cardiometabolic risk factors for metabolic dysfunction-associated steatotic liver disease. Nutr. Metab (Lond). 2025, 22, 10. [CrossRef]
- Stefan, N.; Yki-Järvinen, H.; Neuschwander-Tetri, B.A. Metabolic dysfunction-associated steatotic liver disease: heterogeneous pathomechanisms and effectiveness of metabolism-based treatment. Lancet Diabetes Endocrinol. 2025, 13, 134-148. [CrossRef]
- Mayén, A. L.; Sabra, M.; Aglago, E. K.; Perlemuter, G.; Voican, C.; Ramos, I.; Debras, C.; Blanco, J.; Viallon, V.; Ferrari, P.; et al. Hepatic steatosis, metabolic dysfunction and risk of mortality: findings from a multinational prospective cohort study. BMC Med. 2024, 22, 2212. [CrossRef]
- Lonardo, A.; Nascimbeni, F.; Ballestri, S.; Fairweather, D.; Win, S.; Than, T.A.; Abdelmalek, M.F.; Suzuki, A. Sex differences in nonalcoholic fatty liver disease: state of the art and identification of research gaps. Hepatology. 2019, 70, 1457-1469. [CrossRef]
- Chen, K.L.; Madak-Erdogan, Z. Estrogens and female liver health. Steroids. 2018, 133, 38-43. [CrossRef]
- Colosimo, S.; Mitra, S.K.; Chaudhury, T.; Marchesini, G. Insulin resistance and metabolic flexibility as drivers of liver and cardiac disease in T2DM. Diabetes Res. Clin. Pract. 2023, 206, 111016. [CrossRef]
- Qureshi, K.; Abrams, G.A. Metabolic liver disease of obesity and role of adipose tissue in the pathogenesis of nonalcoholic fatty liver disease. World. J. Gastroenterol. 2007, 13, 3540-3553. [CrossRef]
- Najafi, F.; Pasdar, Y.; Nazar, M.M.; Darbandi, M. Association between obesity phenotypes and non-alcoholic fatty liver: a large population-based study. BMC Endocr. Disord. 2024, 24, 96. [CrossRef]
- Fresneda, S.; Abbate, M.; Busquets-Cortés, C.; López-González, A.; Fuster-Parra, P.; Bennasar-Veny, M.; Yáñez, A.M. Sex and age differences in the association of fatty liver index-defined non-alcoholic fatty liver disease with cardiometabolic risk factors: a cross-sectional study. Biol. Sex. Differ. 2022, 13, 64. [CrossRef]
- Ji, H.; Cheng, S. Heart-Liver Axis Research Collaboration. Sex differences in prevalence and prognosis of steatotic liver disease phenotypes: Biological sex matters. J. Hepatol. 2024, 80, e68-e69. [CrossRef]
- Chang, M.; Shao, Z.; Wei, W.; Shen, P.; Shen, G. Sex-specific prevalence and risk factors of metabolic-associated fatty liver disease among 75,570 individuals in eastern China. Front. Endocrinol (Lausanne). 2023, 14, 1241169. [CrossRef]
- Chen, Y. L.; Li, H.; Li, S.; Xu, Z.; Tian, S.; Wu, J.; Liang, X. Y.; Li, X.; Liu, Z. L.; Xiao, J.; et al. Prevalence of and risk factors for metabolic associated fatty liver disease in an urban population in China: a cross-sectional comparative study. BMC Gastroenterol. 2021, 21, 212. [CrossRef]
- Lei, F.; Qin, J.J.; Song, X.; Liu, Y.M.; Chen, M.M.; Sun, T.; Huang, X.; Deng, K.Q.; Zuo, X.; Yao, D.; et al. The prevalence of MAFLD and its association with atrial fibrillation in a nationwide health check-up population in China. Front Endocrinol (Lausanne). 2022, 13, 1007171. [CrossRef]
- Duan, H.; Gong, M.; Yuan, G.; Wang Z. Sex Hormone: A Potential Target at Treating Female Metabolic Dysfunction-Associated Steatotic Liver Disease? J. Clin. Exp. Hepatol. 2025, 15, 102459. [CrossRef]
- Alves, E.S.; Santos, J.D.M.; Cruz, A.G.; Camargo, F.N.; Talarico, C.H.Z.; Santos, A.R.M.; Silva, C.A.A.; Morgan, H.J.N.; Matos, S.L.; Araujo, L.C.C..; Camporez, J.P. Hepatic Estrogen Receptor Alpha Overexpression Protects Against Hepatic Insulin Resistance and MASLD. Pathophysiology. 2025, 32, 1. [CrossRef]
- Cherubini, A.; Della Torre, S.; Pelusi, S.; Valenti, L. Sexual dimorphism of metabolic dysfunction-associated steatotic liver disease. Trends. Mol. Med. 2024, 30, 1126-1136. [CrossRef]
- Ma, X.M.; Guo, Y.M.; Jiang, S.Y.; Li, K.X.; Zheng, Y.F.; Guo, X.G.; Ren, Z.Y. Potential predictive role of Non-HDL to HDL Cholesterol Ratio (NHHR) in MASLD: focus on obese and type 2 diabetic populations. BMC Gastroenterol. 2025, 25, 79. [CrossRef]
- Shi, S.; Zhou, F.; Shen, J. Trends in the prevalence of cardiometabolic diseases in US adults with newly diagnosed and undiagnosed diabetes, 1988-2020. Public Health. 2025, 239, 94-102. [CrossRef]
|
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2025 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (http://creativecommons.org/licenses/by/4.0/).