1. Introduction
The success of implant-supported single-tooth restorations is often assessed based on the survival rate of the implants, as this allows conclusions to be drawn about the risk of implant loss. However, a consideration of osseointegration alone is insufficient, as the long-term success of a restoration is also defined by functional stability, freedom from complications, and the long-term integrity of the prosthetic components. Against this background, the present study is dedicated to analyzing the clinical success of implants and their prosthetic restoration in the posterior region over a period of three years. For implant-supported single crowns, the literature reports a survival rate of 95.2% after ten years [
1].
The Pisa Consensus Conference (2007) definition is often used to assess implant success. In addition to clinical parameters such as freedom from pain, stability, and freedom from exudate, this definition specifies radiographically detectable bone loss of less than 2 mm as a decisive criterion [
2]. Marginal bone loss (MBL) is subject to a variety of individual influencing factors. In addition to non-modifiable risk factors such as genetic disposition or anatomical conditions, behavioral factors, in particulary tobacco consumption, are among the most significant influencing factors. A meta-analysis has shown that MBL is lowest in non-smokers and increases significantly with increasing cigarette consumption [
3]. Another relevant risk factor is existing or previous periodontitis. Significantly higher bone loss rates are observed, particularly when rough implant surfaces are used [
4].
On the other hand, there are protective factors that can reduce the risk of marginal bone loss. These include regular professional teeth cleaning, which significantly reduces the risk of peri-implant diseases [
5]. Avoiding repeated abutment changes has also proven to be beneficial. Single-stage placement of the final abutment is associated with a lower MBL rate [
6]. Bruxism, on the other hand, is a significant risk factor for the long-term stability of dental implants and for technical complications in prosthetic restorations [
7].
The type of prosthetic restoration also has a significant influence on the long-term outcome. In particular, the type of fixation (cemented vs. screw-retained) and the design of the crown play a central role in terms of biological and technical stability. While both types of restorations carry potential risks, peri-implantitis is considered the most serious biological complication that can occur with both cemented and screw-retained reconstructions [
8,
9]. However, screw-retained restorations tend to show more favorable biological parameters, such as lower bleeding tendency (BOP) and reduced plaque accumulation, which are associated with a lower risk of inflammation [
10,
11]. A decisive disadvantage of cemented constructions is the risk of cement retention in subgingival areas. Remaining cement residues can trigger inflammatory reactions, biofilm formation, and subsequent bone loss [
12].
Hybrid abutment crowns offer a promising alternative in this context. These constructions consist of a titanium base onto which the ceramic superstructure is cemented extraorally so that excess cement can be removed under visual control. The finished crown is then screwed into place. A one-year survival rate of 98.15% is reported for this restoration concept [
13]. The crown material used also has a significant influence on the long-term prognosis. Zirconium dioxide impresses with its high fracture resistance and, in combination with titanium bases, shows improved mechanical performance compared to single-piece zirconium abutments [
14]. Lithium disilicate is also considered a suitable material due to its aesthetic properties, translucency, and good machinability in CAD/CAM processes [
15]. Hybrid ceramics (PICN) combine the hardness of ceramics with the elasticity of polymer components and are characterized by advantageous mechanical properties, particularly with regard to fracture behavior and marginal fit [
16].
The increasing digitalization of prosthetic workflows has contributed to the establishment of efficient treatment strategies. Intraoral scans (IOS) in combination with CAD/CAM-fabricated restorations enable a significant reduction in treatment time for single-tooth restorations [
17]. Despite overall high success rates, the incidence of technical complications remains a clinical challenge. Late implant losses are often due to prosthetic or functional overload [
18]. A distinction must be made between biological and technical complications. The latter affect the mechanical components of the system, including the implant, abutment, screw connection, and superstructure. The most serious technical complication is implant fracture, which occurs in about 0.14% of single implants [
19], mostly due to chronic overload. Screw loosening occurs more frequently, with an incidence of 8.8% after five years [
1], and is influenced by factors such as the type of fixation, implant-abutment design, and axial deviations [
20,
21].
Loss of crown retention is the second most common technical complication, at 4.1% [
1]. Metal-ceramic crowns that have been conventionally cemented have a higher failure rate (5.5%) than adhesively bonded ceramic crowns, where the rate is only 1.1% [
22]. Here, too, the influence of the choice of material on the stability of the restoration is evident. Another frequently observed problem is chipping, especially in the posterior region. With an incidence of 3.5% after five years [
1], it impairs both the function and aesthetics of the restoration. Due to the lack of proprioceptive feedback, implants have up to 8.7 times less tactile sensitivity than natural teeth, which can lead to increased stress on the prosthetic components [
23].
Overall, the correlations presented clearly show that the long-term success of implant-supported single tooth restorations is significantly influenced by the targeted selection of suitable materials and precise prosthetic planning. Both biological and technical complications are closely linked to the restoration design, material properties, and patient-specific risk factors and should therefore be considered in an integrated manner.
This clinical study investigates whether the crown material used, particularly in terms of its modulus of elasticity (E-modulus), has an influence on the biological and technical success of implant-supported single tooth restorations. The analysis focuses on a comparison between lithium disilicate ceramics (LS2) and hybrid ceramic materials (HC) with a polymer component, which differ significantly in terms of their mechanical properties. The hypothesis is tested that crowns made of HC lead to reduced stress transfer to the implant and the peri-implant tissue due to their lower E-modulus and the associated damping material properties. This reduced stress concentration could manifest clinically in lower marginal bone loss and a lower incidence of technical complications compared to LS2 crowns. The aim of the study is to systematically record potential differences in the medium-term performance of both materials over a period of three years and to evaluate their clinical relevance.
2. Materials and Methods
2.1. Trial Design
The present study is a single-center, randomized, controlled clinical trial with blinded data analysis. The aim was to evaluate the biological and technical success of two different crown materials in implant-supported single-tooth restorations in the posterior region over a period of three years. A total of 60 patients who required implant-supported prosthetic restoration of a single tooth in the upper or lower jaw were included in the study.
2.2. Ethical Considerations
The study was approved by the Ethics Committee of the University of Ulm under file number 327/15 (approval date: October 29, 2015). The prospective study is registered in the German Clinical Trials Registry (DRKS) under DRKS ID: DRKS00009628.
All participating subjects were fully informed about the objectives, procedure, and possible risks of the study before the start of treatment. A written consent form was obtained from each patient at the start of the study.
2.3. Sample Size, Randomization and Blinding
As there was insufficient prior clinical data available for the primary endpoint, no formal case number estimate could be made. The case number of 60 patients (30 per study group) is based on experience from comparable studies in which this group size is considered methodologically appropriate.
The study participants were randomized using a concealed randomization procedure with neutral, opaque envelopes. A total of 60 envelopes were prepared in advance by an independent person not involved in the study and numbered consecutively in a 1:1 ratio (lithium disilicate ceramic vs. hybrid ceramic). The envelopes were kept secure until use. Assignment to the respective study group was performed on an individual patient basis immediately after implant placement. A member of the study staff randomly selected an envelope, opened it, and documented the group assignment. This procedure ensures concealed randomization, prevents systematic bias (selection bias), and ensures an even distribution of participants between the two intervention groups.
The evaluation was conducted blinded. After complete data collection and statistical evaluation, the blinding was lifted.
2.3.1. Inclusion Criteria
Only patients who met all of the following inclusion criteria were considered for participation in the study:
Presence of a single tooth gap in the upper or lower posterior region with indication for implant-supported prosthetic restoration
The tooth loss occurred at least three months ago (late or early implantation)
The gap to be filled was bordered by adjacent natural teeth or implants
There was a natural tooth on the contralateral side for functional reference
Antagonistic dentition was completely present
Written informed consent to participate in the study was obtained
2.3.2. Exclusion Criteria
Patients with one or more of the following characteristics were excluded from participation in the study:
Age under 18 or lack of legal capacity
Presence of untreated periodontal disease with staging > stage II and/or grading B or C
Heavy nicotine use (more than 10 cigarettes per day)
Taking bisphosphonates
Pregnancy
Alcohol or drug addiction
Diagnosed infectious diseases such as hepatitis B/C or HIV/AIDS
Uncontrolled or severe diabetes mellitus
Patients who wear mouth guards due to severe bruxism
Need for immediate implantation
Primarily recognizable extensive augmentation requirements, such as a sinus lift
2.4. Clinical Procedure and Intervention Groups
After preliminary examination and consultation, suitable patients were included in the study. All surgical and prosthetic procedures were performed in a standardized manner by an experienced practitioner (SiS). For preoperative planning of the implant position and to assess any need for augmentation, a digital volume tomography (CBCT) with a resolution of 0.2 mm voxel was performed on all patients at the start of the study (Gendex CB500, Gendex Dental Systems, Des Plaines, USA).
The implant position was determined virtually using the CBCT data and the SMOP planning software (Swissmeda, Zurich, Switzerland) in accordance with prosthetic specifications. The planning was documented in at least sagittal and lateral views and archived using screenshots. In cases where the facial cortical bone thickness was <2 mm, simultaneous bone augmentation was performed. For this purpose, autologous bone was combined with a xenogeneic bone substitute material and covered with a resorbable collagen membrane.
The iSy screw implant (ALTATEC GmbH, Wimsheim, Deutschland) was used as the implant system. The implants were inserted according to the manufacturer's protocol and left to heal openly. The wound was closed without tension using a single-button suture and monofilament polyamide suture material (Resolon 5/0, Resorba, Nuremberg, Germany). The sutures were routinely removed seven days after surgery.
The impression for the prosthetic restoration was taken depending on the bone consistency after a healing period of eight weeks for compact bone and twelve weeks for spongy bone structure or in cases of augmentation accompanying implantation. A fast-setting vinyl polysiloxane impression material (Imprint 4 Super Quick, 3M Espe, Seefeld, Germany) was used. The impression was taken using the closed tray technique with the iSy multifunctional cap. Individual trays were fabricated from Erkoplast PLA-W material (Erkodent Erich Kopp GmbH, Pfalzgrafenweiler, Germany).
After removal, the impression tray was prepared for digitization with an implant duplicate (identical diameter to the original implant). The impression was then scanned and archived as an STL data set. The corresponding master model was fabricated using a super-hard plaster (HS-CAD/CAM plaster, Henry Schein Inc., Melville, NY, USA) specially designed for CAD/CAM processing.
2.5. Hybrid Abutment Crowns
Two different materials were used in the study to fabricate the one-piece, screw-retained hybrid abutment crowns:
Lithium disilicate ceramic (IPS e.max CAD, Ivoclar Vivadent AG, Schaan, Liechtenstein)
Hybrid ceramic with polymer content (VITA Enamic, VITA Zahnfabrik GmbH, Bad Säckingen, Germany)
The materials were allocated randomly. Both crown types were cemented extraorally onto a standardized titanium base and any cement residue was removed. The finished hybrid abutment crowns were then screwed in place using the torque recommended by the manufacturer (20 Ncm). The screw channel was closed with Teflon tape and sealed with composite (Ceram-X mono, Dentsply DeTrey, Konstanz, Germany).
All dental work was carried out centrally by dental technicians from the same dental laboratory to ensure consistent quality and standardized production. Production was carried out in accordance with the manufacturer's protocol. Particular attention was paid to a consistent surface treatment process for the crowns. The manufacturer's specifications for the firing process and polishing protocol were strictly adhered to.
2.6. Radiological Analysis of Marginal Bone Loss
To assess marginal bone loss, standardized digital intraoral single-tooth X-rays were taken at two defined time points:
For reproducible repositioning of the X-ray film holders, individual positioning templates made of transparent plastic material were fabricated on plaster models in the dental laboratory.
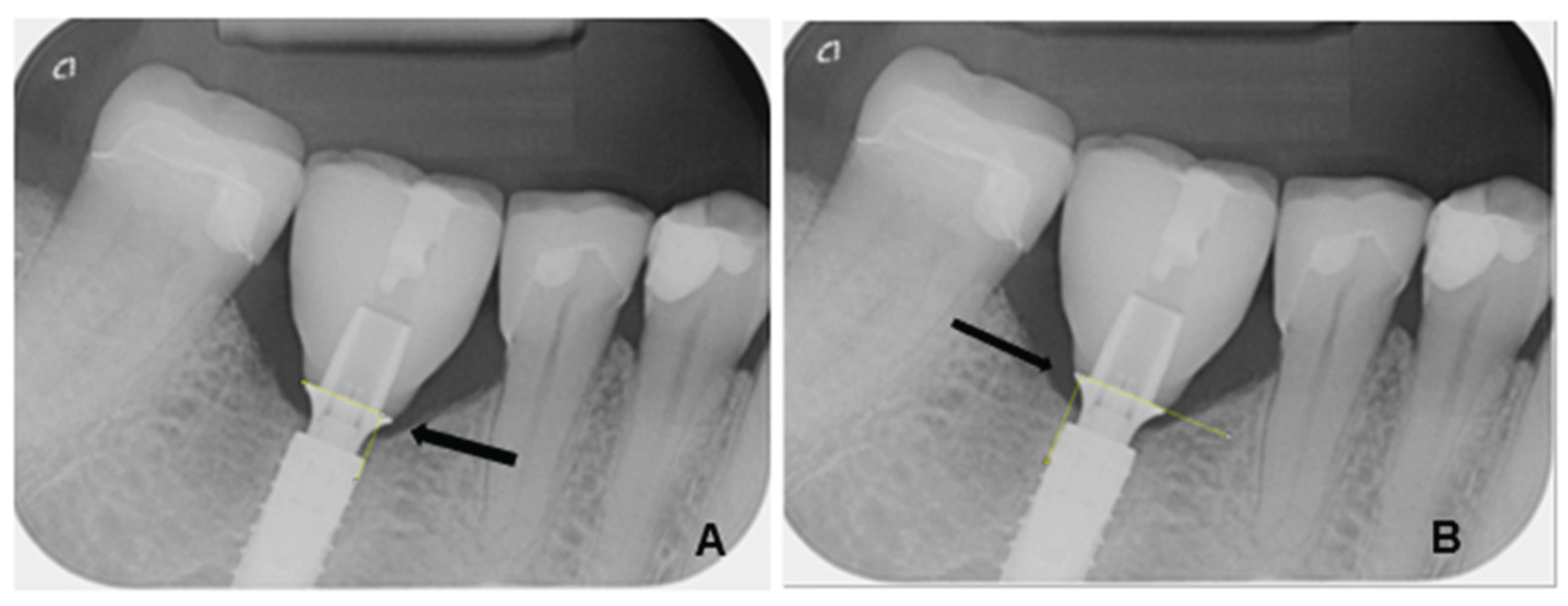
The radiological images were evaluated using the image analysis software ImageJ (Image Processing and Analysis in Java, version 1.53, macOS Monterey 12.7.4), a scientifically established open-source software for quantitative image processing. The measurements were calibrated based on the known diameter of each implant used. The measurement of marginal bone loss was performed both mesially and distally, orthogonally to the implant shoulder. The measurement was taken from the outer edge of the implant shoulder to the crestal bone edge (
Figure 1). The examiners were calibrated prior to the measurement. In addition, several series of repeat measurements were performed at different times to reduce intraobserver variations.
All X-ray images were zoomed in for measurement to ensure maximum precision. Two bone measurements and one control measurement of the implant diameter were performed per patient at each measurement time point. The results were numbered consecutively, systematically documented, and archived in an Excel spreadsheet. Marginal bone loss was determined by calculating the difference between the baseline value (T0) and the follow-up measurements (T1).
2.7. Recording Technical Complications
In addition, all technical complications were systematically recorded and documented during the observation period. These included in particular:
Documentation was carried out continuously during the check-ups and was evaluated in terms of quality and quantity.
2.8. Statistical Evaluation
The statistical analysis was performed using SPSS (version 29.0.2.0, IBM, Armonk, USA) and Microsoft Excel (Microsoft, Redmond, USA). The study is exploratory and descriptive in nature, as there are no reliable preliminary studies available in the literature on comparable types of restorations, especially for the crown materials selected in combination with hybrid abutment crowns.
The aim of the analysis was to identify and describe differences between the two study groups in terms of implant survival, marginal bone loss, and technical complications. Due to the exploratory nature of the study, formal hypothesis testing was not performed; this is a hypothesis-generating study to prepare for further multicenter studies.
All statistical analyses were performed with a two-sided significance level of α = 0.05. No adjustment was made for multiple comparisons. The primary endpoint of the study was implant loss within a three-year observation period, which was defined as a dichotomous target variable (yes/no). The groups were compared using the chi-square test for independent samples. To quantify the statistical uncertainty, the 95% confidence interval of the difference in the proportion values was calculated.
For the analysis of marginal bone loss, group differences were examined using a two-sided t-test for independent samples in the presence of a normal distribution. In the event of deviations from the normal distribution, equivalent non-parametric methods, in particular the Wilcoxon sign rank test, were used.
3. Results
3.1. Patient Population and Implant Distribution
Data from a total of 58 patients could be included in the evaluation. Two patients were excluded from the study due to early implant loss. No subsequent recruitment took place. Due to the subsequent reimplantation, these patients were excluded from further investigation.
The average age was 50.3 years (range, 22-79 years). Of the 58 cases evaluated, 28 patients were in the hybrid ceramic crown group and 30 patients were in the lithium disilicate ceramic group. The total collective consisted of 35 female and 23 male subjects.
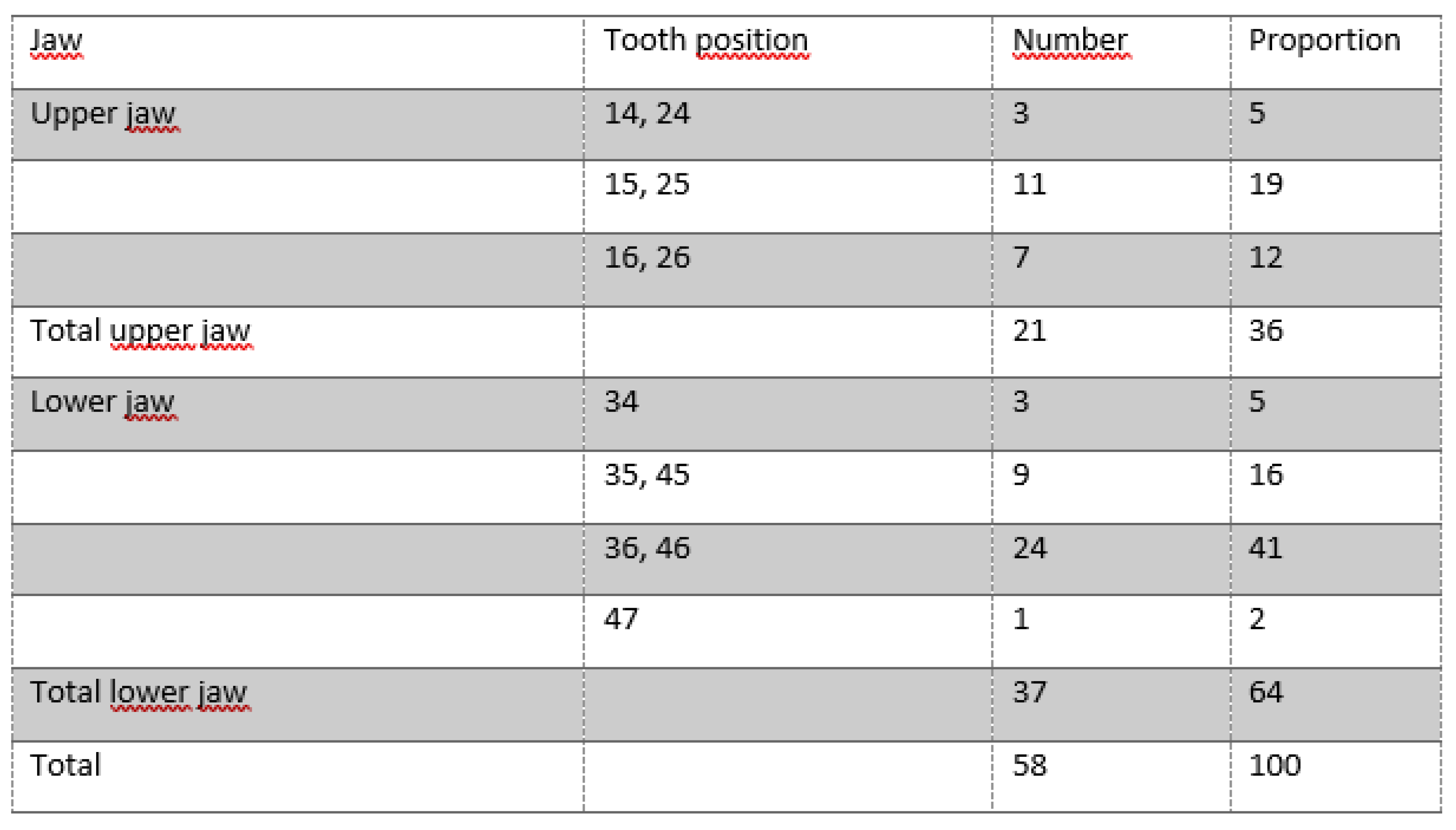
A total of 37 implants were inserted in the mandible (63.8%) and 21 implants in the maxilla (36.2%). The distribution of implant positions is shown in
Table 1.
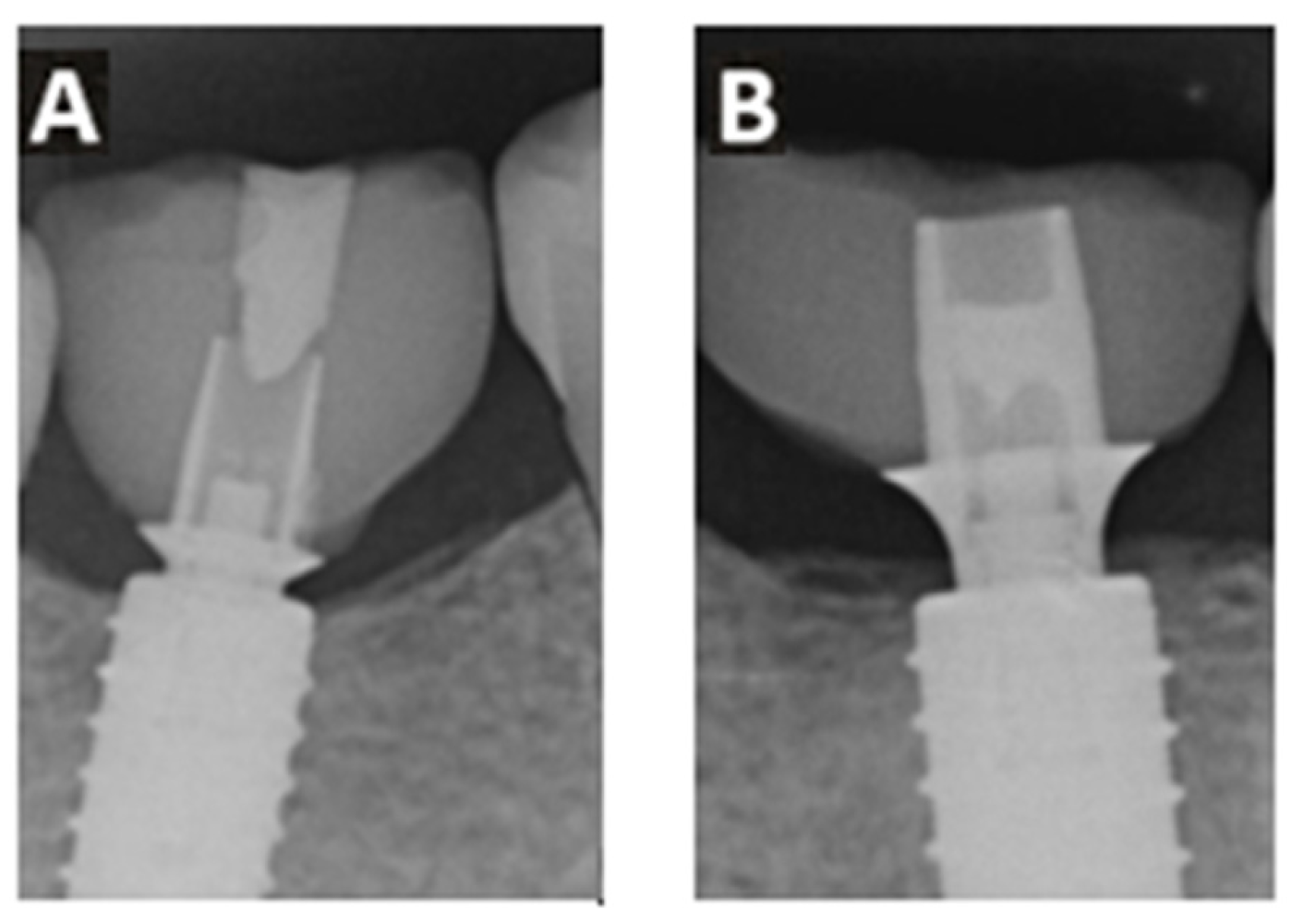
The implant system used offered two different heights of titanium adhesive bases (
Figure 3). In 27 cases, an adhesive base height of 0.8 mm was used, while in the remaining 31 cases, a height of 2.0 mm was selected.
Table 1.
Position and proportion of implant losses evaluated in the study.
Table 1.
Position and proportion of implant losses evaluated in the study.
3.2. Implant Survival
During the observation period of 36 months after the denture was fitted, no implant loss was recorded, corresponding to a survival rate of 100%.
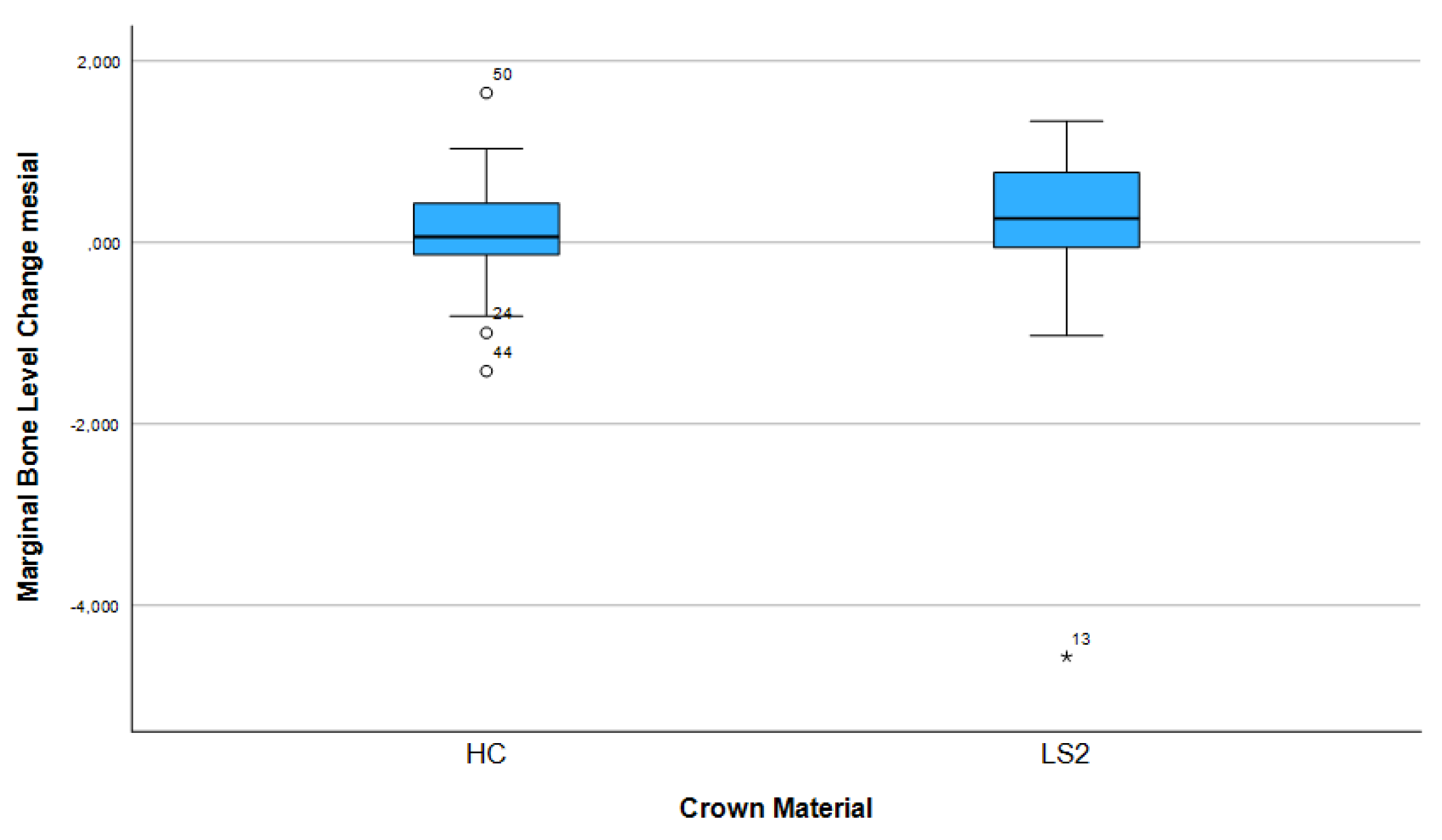
3.3. Changes in Marginal Bone Profile
After three years, 74.1% (n = 43) of the implants showed bone apposition mesially and 63.8% (n = 37) distally. Marginal bone loss was observed in 25.9% of the implants mesially and 36.2% distally. The mean bone remodeling was 0.13 mm mesially (range: −4.56 to 1.65 mm; SD: 0.88) (
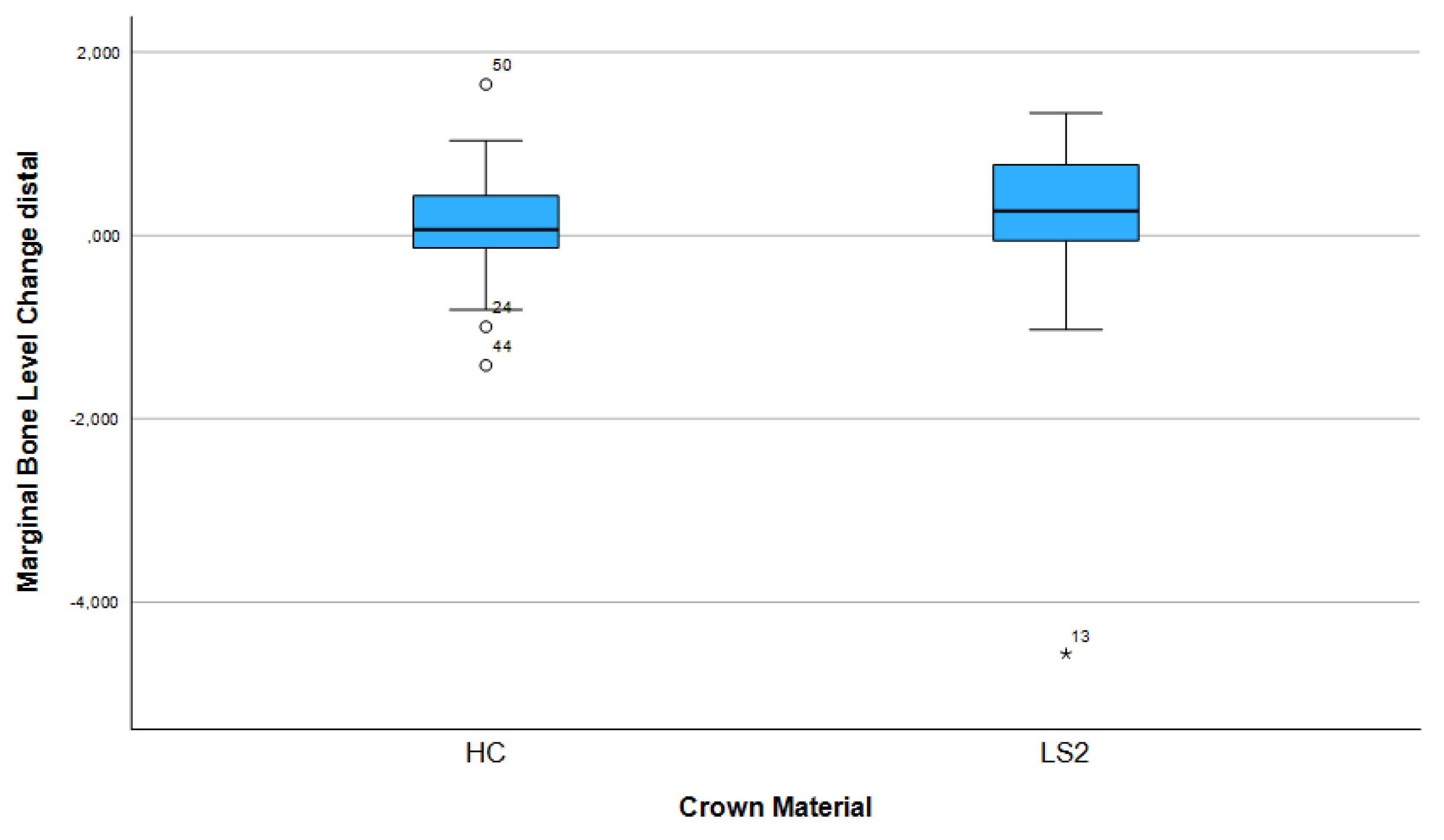
Figure 5) and 0.12 mm distally (range: −3.95 to 1.73 mm; SD: 0.78) (
Figure 6).
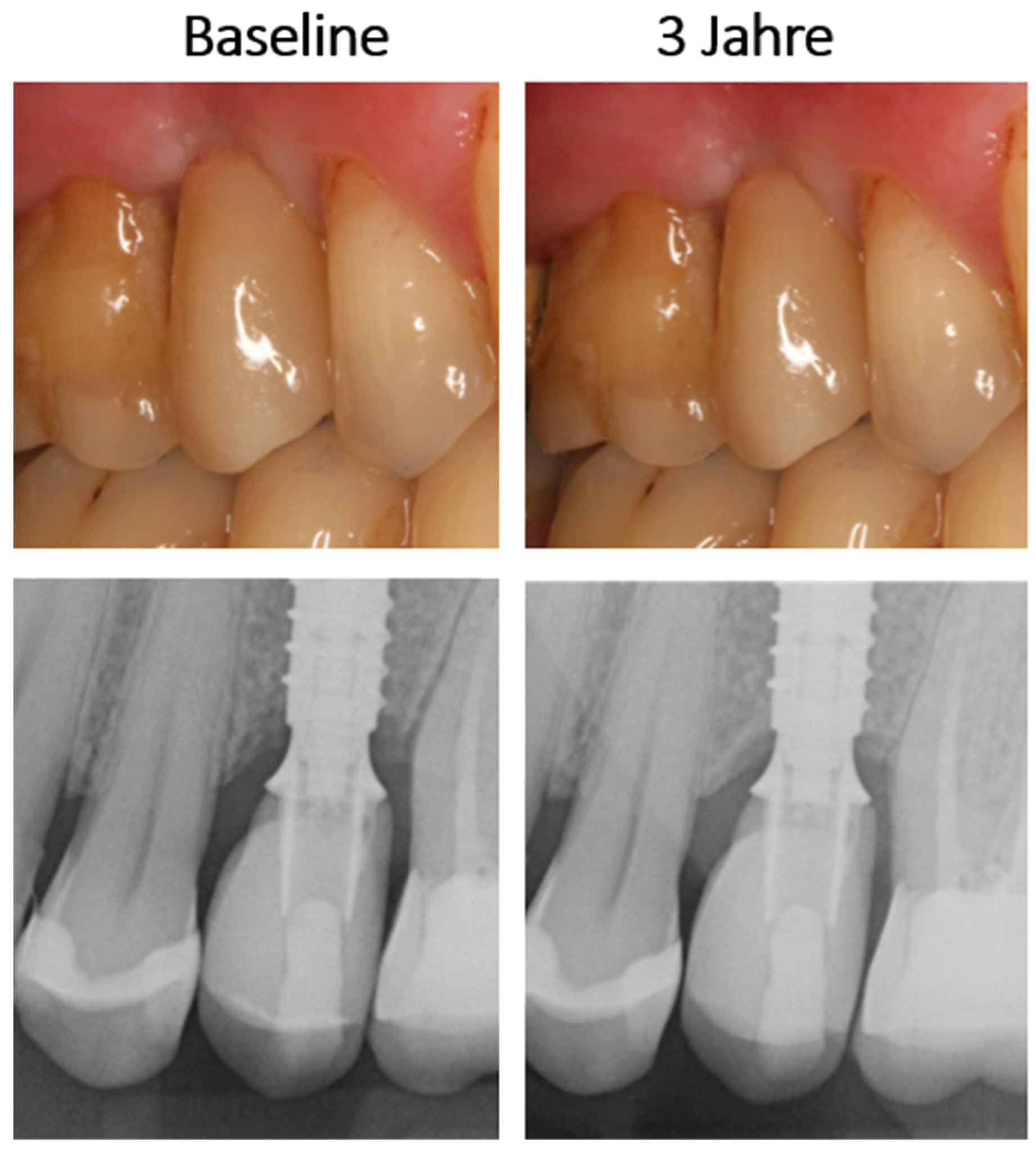
Figure 4.
Exemplary documentation of an LS2-Hybrid-abutment crown baseline and after 3 years in clinical and radiological examination.
Figure 4.
Exemplary documentation of an LS2-Hybrid-abutment crown baseline and after 3 years in clinical and radiological examination.
Figure 5.
Marginal bone loss depending on the crown material (mesial).
Figure 5.
Marginal bone loss depending on the crown material (mesial).
Figure 6.
Marginal bone loss depending on the crown material (distal).
Figure 6.
Marginal bone loss depending on the crown material (distal).
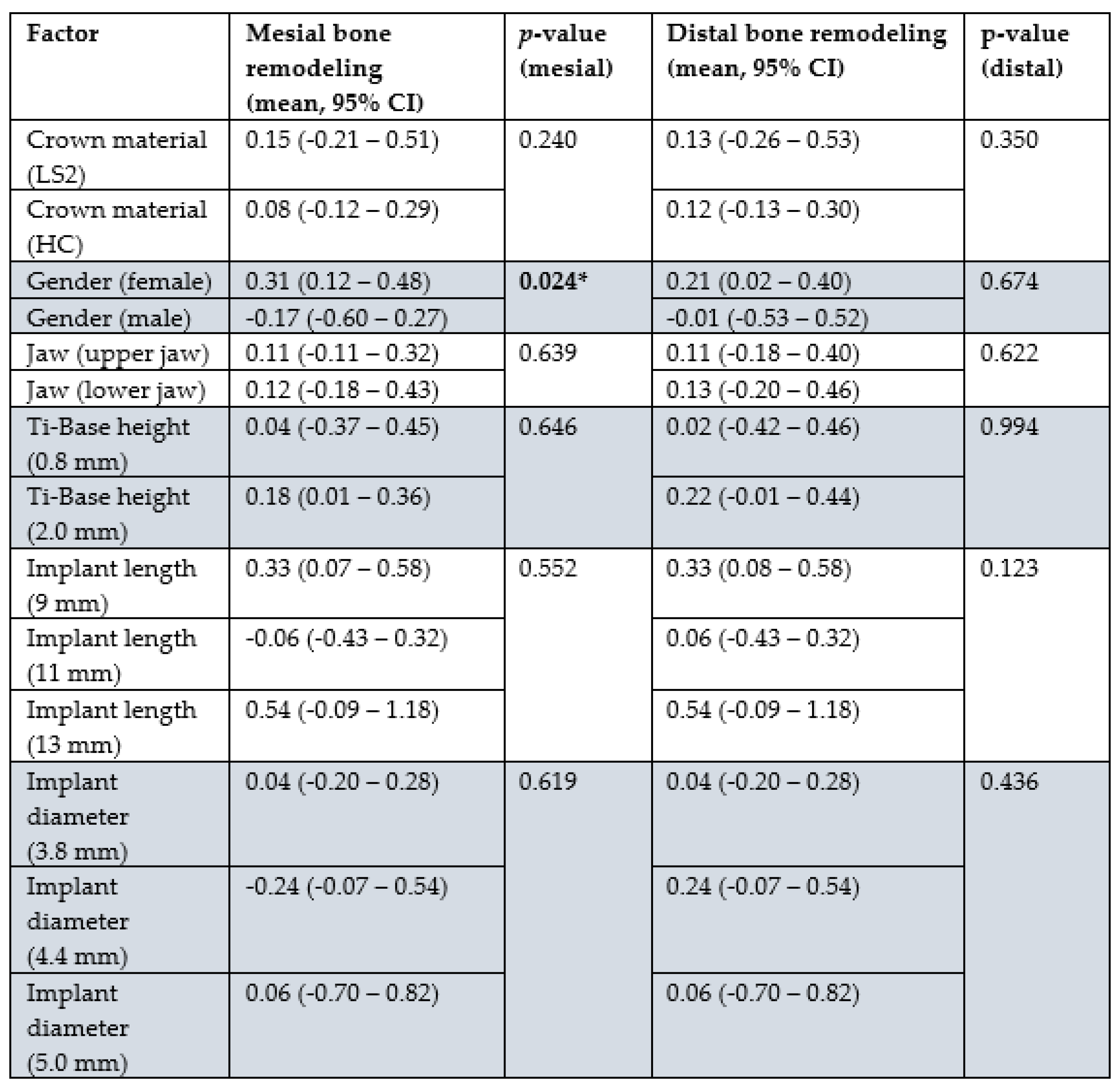
Statistical analysis showed that gender had a significant influence on bone remodeling: In female patients, a mean bone gain of 0.31 mm (95% CI: 0.12–0.48) was observed mesially and bone loss of −0.17 mm (95% CI: −0.60–0.27) was observed in male patients (p = 0.024). A similar trend was observed distally, but without statistical significance (p = 0.674).
Other influencing factors such as crown material (LS2 vs. HC), jaw position (upper vs. lower jaw), height of the Ti base (0.8 mm vs. 2.0 mm), implant length, and implant diameter showed no statistically significant influence on bone remodeling, neither mesially nor distally (all p > 0.05). The results of the corresponding group comparisons are shown in
Table 2.
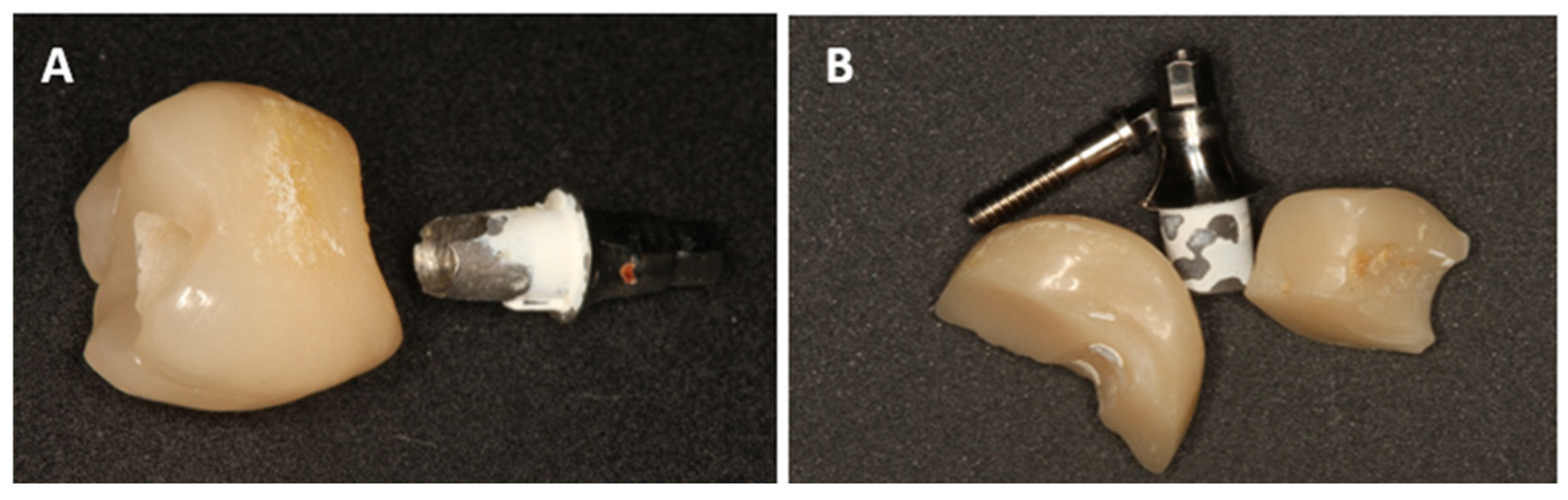
3.4. Technical Complications
Overall, technical complications occurred with both materials, with severe damage observed exclusively in the HC group.
Crown fractures were observed exclusively in HC crowns (n = 7; 25.0%) with an average occurrence after 12.86 months. In all cases, the crown had to be remade.
Screw loosening occurred in both groups: in HC in 14.3% (n = 4; mean time: 17.25 months) and in LS2 in 12.5% (n = 4; mean time: 3.75 months).
Loss of bonding (decementation) between the crown and Ti base was observed exclusively in HC in 17.9% (n = 5; mean time: 27.0 months). Rebonding was performed in the dental laboratory.
While minor technical complications such as screw loosening occurred with comparable frequency across groups, major (decementation) and critical (fracture) complications were observed exclusively in the HC group.
4. Discussion
The objective of this clinical study was to evaluate the biological and technical outcomes of hybrid abutment crowns fabricated from either lithium disilicate (LS2) or a high-performance polymer composite (HC), with particular attention to their influence on peri-implant bone remodeling and prosthetic complications. Across the evaluated cohort of 58 patients, no implant loss occurred during the 36-month follow-up period [
24], thereby allowing for a valid assessment of the primary endpoint: the influence of the superstructure material on implant survival. The results revealed no significant difference between the two materials in terms of implant survival at both one and three years, aligning with existing literature that reports similar survival rates regardless of crown material.
The study further demonstrated subtle changes in marginal bone levels around the implants. Average bone remodeling was 0.15 mm mesially and 0.13 mm distally in the LS2 group, and 0.08 mm mesially and 0.12 mm distally in the HC group. These differences were not statistically significant, indicating that both materials are clinically comparable regarding their impact on peri-implant bone stability. These findings are consistent with those of Mangano et al. (2018), who also observed favorable medium-term outcomes with CAD/CAM-fabricated ceramic hybrid abutment crowns [
25].
A notable strength of this investigation is its single-center design, which ensured standardized treatment protocols and consistent procedural execution. The influence of operator variability, a well-documented factor in implantology as shown by Jemt et al. (1989) and Chrcanovic et al. (2014), was thus effectively minimized [
26,
27].
Interestingly, mesial bone remodeling appeared to be gender-dependent: female patients exhibited significantly greater bone apposition than their male counterparts. A similar trend was reported by Cheng et al. (2025) [
28], although such gender-specific effects have not been consistently reported across the literature [
29].
A limitation of the study is the relatively short observation period of three years and the limited sample size. Although two early implant losses occurred prior to loading, the literature indicates average survival rates ranging from 95% to 98% in the early postoperative years [
30]. Within the monitored follow-up period, no further implant failures were recorded.
Bone apposition was documented in 74.1% of implants, potentially attributable to the combination of subcrestal implant placement, platform switching, and regenerative surgical protocols, as previously described by Linkevicius et al. (2009) [
31]. Only a few cases exhibited marginal bone resorption, with the overall remodeling rates being lower than those commonly reported in similar studies [
32].
The employed surgical approach—minimally invasive flap formation with transgingival healing—is considered especially conservative. Reduced tissue trauma and improved healing associated with flapless procedures have been confirmed by Pisoni et al. (2016) [
33], although long-term success appears unaffected by the flap technique itself [
34]. The minimal bone loss observed here supports the hypothesis that careful, low-trauma site preparation, possibly aided by single-use drills, contributes to bone preservation.
Postoperative care represents another important factor. According to Atieh et al. (2021), regular peri-implant maintenance significantly reduces marginal bone loss [
5]. While this study did not quantify follow-up care frequency, all patients were instructed in proper oral hygiene and selected based on good compliance, suggesting that both home and professional care were adequately provided.
Regarding prosthetic protocol, a single-stage transgingival healing concept was implemented, minimizing abutment manipulation. This approach is supported by Vatenas and Linkevičius (2021), Nunes et al. (2025), and Atieh et al. (2017), who reported superior bone maintenance with reduced abutment disconnections [
35,
36,
37].
In summary, no significant material-dependent differences were found regarding marginal bone remodeling, and all implants exhibited successful osseointegration.
The adoption of CAD/CAM workflows and the development of novel all-ceramic materials have broadened the indications for aesthetic, metal-free implant restorations. All-ceramic solutions offer excellent biocompatibility and high aesthetic standards [
38]. This study focused on comparing the clinical and technical performance of LS2 and HC crowns in single-implant restorations over 36 months.
The hybrid abutment crowns in this study consisted of monolithic CAD/CAM-milled all-ceramic restorations adhesively bonded to prefabricated titanium bases. The occlusal screw channel was sealed with Teflon tape and composite in accordance with clinical standards (Sailer et al., 2018). This type of restoration is well-established in contemporary prosthodontics [
39].
A systematic review by Pjetursson et al. (2021) provides survival data for implant-supported all-ceramic single crowns (iSCs): three-year survival rates of 97.6% for veneered and reinforced glass-ceramic iSCs, 97.0% for monolithic glass-ceramics, and 96.3% for veneered zirconia; monolithic zirconia showed similar performance at 96.1%. Resin nano-ceramics showed markedly lower survival at 36.3%. The annual complication rate was 3.9% for veneered iSCs and 1.8% for monolithic designs [
40].
The findings from the present study are in line with these data. No complications occurred in the LS2 group during the 36-month observation. In contrast, 25% of the HC crowns failed and required replacement. Additionally, decementation events were observed solely in the HC group. This supports the results reported by Zhang et al. (2023), who compared monolithic lithium disilicate and veneered zirconia crowns in an RCT. After three years, the survival rate was 94% in the LS2 group (one fracture) and 100% in the zirconia group [
41]. Spitznagel et al. (2021) similarly reported a 100% survival rate over five years for LS2 monolithic restorations on ceramic implants [
42].
Pjetursson et al.’s meta-analysis also highlighted inferior performance of resin-based materials, citing an RCT with 70% survival at five years (n = 25) and a prospective cohort study with 14% survival at one year (n = 50) [
40,
41,
43].
Monolithic ceramics are generally considered more durable than veneered designs. Lower fracture rates and reduced complication risk favor monolithic crowns, particularly in posterior regions [
44,
45]. Spitznagel et al. (2017) emphasized the clinical reliability and esthetic benefits of lithium disilicate as a fully anatomical restorative material [
46].
5. Conclusions
In conclusion, this study affirms the clinical efficacy and predictability of lithium disilicate (LS2) hybrid abutment crowns for posterior single-tooth implant restorations. The three-year outcomes—marked by a 100% survival rate, absence of complications, and no required reinterventions—support the use of LS2 as a dependable material. Conversely, HC restorations demonstrated a higher incidence of technical complications, consistent with previously reported limitations of polymer-based materials.
These findings support the clinical recommendation that hybrid abutment crowns -particularly those made from lithium disilicate - offer a reliable treatment modality with stable peri-implant tissue outcomes over at least three years. Nevertheless, further randomized controlled trials with larger cohorts and extended follow-up are needed to validate and expand upon these conclusions.
Author Contributions
Conceptualization, S.S and M.W.; methodology, S.S.; software, S.S.; validation, M.W., M.R. and R.L.; formal analysis, S.S.; investigation, S.S., M.W. and M.R.; resources, S.S.; data curation, M.W; writing—original draft preparation, S.S. and M.W.; writing—review and editing, R.L.; visualization, S.S. and M.R.; supervision, R.L.; project administration, S.S.; funding acquisition, S.S. All authors have read and agreed to the published version of the manuscript
Funding
The work was supported by the Oral Reconstruction Foundation (formerly the Camlog Foundation), Grant No. CF 41.506. The major part of the research was self-funded by the authors and their institutions. The study design, data collection and data analysis, as well as the writing of the manuscript, were carried out completely independently by the authors. All authors read and approved the final draft of this manuscript.
Institutional Review Board Statement
The study was conducted in accordance with the Declaration of Helsinki. All patient data were collected after approval of the Ethics Committee of Ulm University (Application No. 327/15).
Informed Consent Statement
Informed consent was obtained from all subjects involved in the study.
Data Availability Statement
The complete documentation of all patients enrolled in this study belongs to the authors and is available only upon reasonable request.
Conflicts of Interest
The authors declare no conflicts of interest. The funders had no role in the design of the study; in the collection, analyses, or interpretation of data; in the writing of the manuscript; or in the decision to publish the results.
References
- Jung, R. E.; Zembic, A.; Pjetursson, B. E.; Zwahlen, M.; Thoma, D. S. , Systematic review of the survival rate and the incidence of biological, technical, and aesthetic complications of single crowns on implants reported in longitudinal studies with a mean follow-up of 5 years. Clin Oral Implants Res 2012, 23 Suppl 6, 2–21. [Google Scholar] [CrossRef]
- Misch, C. E.; Perel, M. L.; Wang, H. L.; Sammartino, G.; Galindo-Moreno, P.; Trisi, P.; Steigmann, M.; Rebaudi, A.; Palti, A.; Pikos, M. A.; Schwartz-Arad, D.; Choukroun, J.; Gutierrez-Perez, J. L.; Marenzi, G.; Valavanis, D. K. , Implant success, survival, and failure: the International Congress of Oral Implantologists (ICOI) Pisa Consensus Conference. Implant Dent 2008, 17(1), 5–15. [Google Scholar] [CrossRef]
- Afshari, Z.; Yaghini, J.; Naseri, R. , Levels of Smoking and Peri-Implant Marginal Bone Loss: A Systematic Review and Meta-Analysis. J Evid Based Dent Pract 2022, 22(3), 101721. [Google Scholar] [CrossRef]
- Lin, C. Y.; Chen, Z.; Pan, W. L.; Wang, H. L. , Is History of Periodontal Disease Still a Negative Risk Indicator for Peri-implant Health Under Supportive Post-implant Treatment Coverage? Int J Oral Maxillofac Implants 2020, 35(1), 52–62. [Google Scholar] [CrossRef]
- Atieh, M. A.; AlAli, F.; Alsabeeha, N. H. M. , Outcome of supportive peri-implant therapy on the rates of peri-implant diseases and marginal bone loss: a systematic review and meta-analysis. Quintessence Int 2021, 52(2), 122–131. [Google Scholar] [CrossRef]
- de Carvalho Barbara, J. G.; Luz, D.; Vianna, K.; Porto Barboza, E. , The influence of abutment disconnections on peri-implant marginal bone: A systematic review. Int J Oral Implantol (Berl) 2019, 12(3), 283–296. [Google Scholar]
- Häggman-Henrikson, B.; Ali, D.; Aljamal, M.; Chrcanovic, B. , Bruxism and dental implants: A systematic review and meta-analysis. Journal of Oral Rehabilitation 2023, 51, 202–217. [Google Scholar] [CrossRef]
- Hamed, M. T.; Abdullah Mously, H.; Khalid Alamoudi, S.; Hossam Hashem, A. B.; Hussein Naguib, G. , A Systematic Review of Screw versus Cement-Retained Fixed Implant Supported Reconstructions. Clin Cosmet Investig Dent 2020, 12, 9–16. [Google Scholar] [CrossRef]
- de Brandao, M. L.; Vettore, M. V.; Vidigal Junior, G. M. , Peri-implant bone loss in cement- and screw-retained prostheses: systematic review and meta-analysis. J Clin Periodontol 2013, 40(3), 287–95. [Google Scholar] [CrossRef]
- Raval, N. C.; Wadhwani, C. P.; Jain, S.; Darveau, R. P. , The Interaction of Implant Luting Cements and Oral Bacteria Linked to Peri-Implant Disease: An In Vitro Analysis of Planktonic and Biofilm Growth--A Preliminary Study. Clin Implant Dent Relat Res 2015, 17(6), 1029–35. [Google Scholar] [CrossRef]
- Weber, H. P.; Kim, D. M.; Ng, M. W.; Hwang, J. W.; Fiorellini, J. P. , Peri-implant soft-tissue health surrounding cement- and screw-retained implant restorations: a multi-center, 3-year prospective study. Clin Oral Implants Res 2006, 17(4), 375–9. [Google Scholar] [CrossRef]
- Freitas, A. C., Jr.; Bonfante, E. A.; Rocha, E. P.; Silva, N. R.; Marotta, L.; Coelho, P. G. , Effect of implant connection and restoration design (screwed vs. cemented) in reliability and failure modes of anterior crowns. Eur J Oral Sci 2011, 119 (4), 323-30. [CrossRef]
- Sailer, I.; Karasan, D.; Todorovic, A.; Ligoutsikou, M.; Pjetursson, B. E. , Prosthetic failures in dental implant therapy. Periodontol 2000 2022, 88(1), 130–144. [Google Scholar] [CrossRef]
- Pitta, J.; Hjerppe, J.; Burkhardt, F.; Fehmer, V.; Mojon, P.; Sailer, I. , Mechanical stability and technical outcomes of monolithic CAD/CAM fabricated abutment-crowns supported by titanium bases: An in vitro study. Clin Oral Implants Res 2021, 32(2), 222–232. [Google Scholar] [CrossRef] [PubMed]
- Stimmelmayr, M.; Edelhoff, D.; Guth, J. F.; Erdelt, K.; Happe, A.; Beuer, F. , Wear at the titanium-titanium and the titanium-zirconia implant-abutment interface: a comparative in vitro study. Dent Mater 2012, 28(12), 1215–20. [Google Scholar] [CrossRef]
- Alseddiek, A.; Al-Zordk, W.; Attia, A. , Retention of hybrid-abutment-crowns with offset implant placement: influence of Crown materials and Ti-base height. BMC Oral Health 2023, 23(1), 784. [Google Scholar] [CrossRef]
- Muhlemann, S.; Kraus, R. D.; Hammerle, C. H. F.; Thoma, D. S. , Is the use of digital technologies for the fabrication of implant-supported reconstructions more efficient and/or more effective than conventional techniques: A systematic review. Clin Oral Implants Res 2018, 29 Suppl 18, 184–195. [Google Scholar] [CrossRef] [PubMed]
- Derks, J.; Hakansson, J.; Wennstrom, J. L.; Tomasi, C.; Larsson, M.; Berglundh, T. , Effectiveness of implant therapy analyzed in a Swedish population: early and late implant loss. J Dent Res 2015, 94 (3 Suppl), 44S–51S. [Google Scholar] [CrossRef]
- Tomasi, C.; Derks, J. , Etiology, occurrence, and consequences of implant loss. Periodontol 2000 2022, 88(1), 13–35. [Google Scholar] [CrossRef]
- Pjetursson, B. E.; Asgeirsson, A. G.; Zwahlen, M.; Sailer, I. , Improvements in implant dentistry over the last decade: comparison of survival and complication rates in older and newer publications. Int J Oral Maxillofac Implants 2014, 29 Suppl, 308–24. [Google Scholar] [CrossRef]
- Hotinski, E.; Dudley, J. , Abutment screw loosening in angulation-correcting implants: An in vitro study. J Prosthet Dent 2019, 121(1), 151–155. [Google Scholar] [CrossRef] [PubMed]
- Pjetursson, B. E.; Bragger, U.; Lang, N. P.; Zwahlen, M. , Comparison of survival and complication rates of tooth-supported fixed dental prostheses (FDPs) and implant-supported FDPs and single crowns (SCs). Clin Oral Implants Res 2007, 18 Suppl 3, 97–113. [Google Scholar] [CrossRef]
- Hammerle, C. H.; Wagner, D.; Bragger, U.; Lussi, A.; Karayiannis, A.; Joss, A.; Lang, N. P. , Threshold of tactile sensitivity perceived with dental endosseous implants and natural teeth. Clin Oral Implants Res 1995, 6(2), 83–90. [Google Scholar] [CrossRef] [PubMed]
- Mikeli, A.; Walter, M. H.; Rau, S. A.; Raedel, M.; Raedel, M. , Three-year clinical performance of posterior monolithic zirconia single crowns. J Prosthet Dent 2022, 128(6), 1252–1257. [Google Scholar] [CrossRef]
- Mangano, F.; Veronesi, G. , Digital versus Analog Procedures for the Prosthetic Restoration of Single Implants: A Randomized Controlled Trial with 1 Year of Follow-Up. Biomed Res Int 2018, 2018, 5325032. [Google Scholar] [CrossRef]
- Jemt, T.; Lekholm, U.; Adell, R. , Osseointegrated implants in the treatment of partially edentulous patients: a preliminary study on 876 consecutively placed fixtures. Int J Oral Maxillofac Implants 1989, 4(3), 211–7. [Google Scholar] [PubMed]
- Chrcanovic, B. R.; Albrektsson, T.; Wennerberg, A. , Reasons for failures of oral implants. J Oral Rehabil 2014, 41(6), 443–76. [Google Scholar] [CrossRef]
- Cheng, Y.; Lai, Z.; Yu, W. , Influencing factors and survival rates in immediate vs. delayed dental implant placement: a six-year retrospective analysis. Front Dent Med 2025, 6, 1563641. [Google Scholar] [CrossRef] [PubMed]
- Khehra, A.; Zanner, O.; Samet, N.; Levin, L. , The Influence of Patient-, Site-, and Implant-Related Factors on Marginal Bone Levels of Dental Implants in a Rural Population in China: A Retrospective Study. Clin Exp Dent Res 2024, 10(6), e70045. [Google Scholar] [CrossRef] [PubMed]
- Garcia-Sanchez, R.; Dopico, J.; Kalemaj, Z.; Buti, J.; Pardo Zamora, G.; Mardas, N. , Comparison of clinical outcomes of immediate versus delayed placement of dental implants: A systematic review and meta-analysis. Clin Oral Implants Res 2022, 33(3), 231–277. [Google Scholar] [CrossRef]
- Linkevicius, T.; Apse, P.; Grybauskas, S.; Puisys, A. , The influence of soft tissue thickness on crestal bone changes around implants: a 1-year prospective controlled clinical trial. Int J Oral Maxillofac Implants 2009, 24(4), 712–9. [Google Scholar]
- Tomar, S.; Saxena, D.; Kaur, N. , Marginal bone loss around implants with platform switching and platform matched connection: A systematic review. J Prosthet Dent 2023. [CrossRef]
- Pisoni, L.; Ordesi, P.; Siervo, P.; Bianchi, A. E.; Persia, M.; Siervo, S. , Flapless Versus Traditional Dental Implant Surgery: Long-Term Evaluation of Crestal Bone Resorption. J Oral Maxillofac Surg 2016, 74(7), 1354–9. [Google Scholar] [CrossRef] [PubMed]
- Cai, H.; Liang, X.; Sun, D. Y.; Chen, J. Y. , Long-term clinical performance of flapless implant surgery compared to the conventional approach with flap elevation: A systematic review and meta-analysis. World J Clin Cases 2020, 8(6), 1087–1103. [Google Scholar] [CrossRef] [PubMed]
- Vatenas, I.; Linkevicius, T. , One abutment one time vs. repeatable abutment disconnections in implants, restored with cemented / screw retained fixed partial dentures: Marginal bone level changes. A systematic review and meta-analysis. Stomatologija 2021, 23 (2), 35-40.
- Nunes, M.; Leitao, B.; Pereira, M.; Fernandes, J. C. H.; Fernandes, G. V. O. , Final Prosthetic Abutment Insertion Time (One-Time Abutment Insertion Protocol Versus Conventional Protocol) and Related Outcomes: A Systematic Review of Randomized Controlled Trials with Meta-analysis. Int J Oral Maxillofac Implants 2025, 40(2), 162–170. [Google Scholar]
- Atieh, M. A.; Tawse-Smith, A.; Alsabeeha, N. H. M.; Ma, S.; Duncan, W. J. , The One Abutment-One Time Protocol: A Systematic Review and Meta-Analysis. J Periodontol 2017, 88(11), 1173–1185. [Google Scholar] [CrossRef]
- Denry, I.; Kelly, J. R. , Emerging ceramic-based materials for dentistry. J Dent Res 2014, 93(12), 1235–42. [Google Scholar] [CrossRef]
- Sailer, I.; Muhlemann, S.; Kohal, R. J.; Spies, B. C.; Pjetursson, B. E.; Lang, N. P.; Gotfredsen, K. L.; Ellingsen, J. E.; Francisco, H.; Ozcan, M.; Hassan, B.; Esteve-Pardo, G.; Bardaji, J. A.; Kraus, R. D.; Wennerberg, A. , Reconstructive aspects: Summary and consensus statements of group 3. The 5(th) EAO Consensus Conference 2018. Clin Oral Implants Res 2018, 29 Suppl 18, 237-242. [CrossRef]
- Pjetursson, B. E.; Sailer, I.; Latyshev, A.; Rabel, K.; Kohal, R. J.; Karasan, D. , A systematic review and meta-analysis evaluating the survival, the failure, and the complication rates of veneered and monolithic all-ceramic implant-supported single crowns. Clin Oral Implants Res 2021, 21 (Suppl 21), 254–288. [Google Scholar] [CrossRef]
- Zhang, Y.; Wei, D.; Tian, J.; Zhao, Y.; Lin, Y.; Di, P. , Clinical evaluation and quantitative occlusal change analysis of posterior implant-supported all-ceramic crowns: A 3-year randomized controlled clinical trial. Clin Oral Implants Res 2023, 34(11), 1188–1197. [Google Scholar] [CrossRef] [PubMed]
- Spitznagel, F.; Balmer, M.; Wiedemeier, D.; Jung, R.; Gierthmuehlen, P. , Clinical outcomes of all-ceramic single crowns and fixed dental prostheses supported by ceramic implants: A systematic review and meta-analyses. Clin Oral Implants Res 2021, 33, 1–20. [Google Scholar] [CrossRef]
- Schepke, U.; Meijer, H. J.; Vermeulen, K. M.; Raghoebar, G. M.; Cune, M. S. , Clinical Bonding of Resin Nano Ceramic Restorations to Zirconia Abutments: A Case Series within a Randomized Clinical Trial. Clin Implant Dent Relat Res 2016, 18(5), 984–992. [Google Scholar] [CrossRef]
- Sailer, I.; Feher, A.; Filser, F.; Gauckler, L. J.; Luthy, H.; Hammerle, C. H. , Five-year clinical results of zirconia frameworks for posterior fixed partial dentures. Int J Prosthodont 2007, 20(4), 383–8. [Google Scholar] [PubMed]
- Sailer, I.; Makarov, N. A.; Thoma, D. S.; Zwahlen, M.; Pjetursson, B. E. , All-ceramic or metal-ceramic tooth-supported fixed dental prostheses (FDPs)? A systematic review of the survival and complication rates. Part I: Single crowns (SCs). Dent Mater 2015, 31 (6), 603-23.
- Spitznagel, F. A.; Horvath, S. D.; Gierthmuehlen, P. C. , Prosthetic protocols in implant-based oral rehabilitations: A systematic review on the clinical outcome of monolithic all-ceramic single- and multi-unit prostheses. Eur J Oral Implantol 2017, 10 Suppl 1, 89–99. [Google Scholar] [PubMed]
|
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2025 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (http://creativecommons.org/licenses/by/4.0/).