1. Introduction
Neurofibromatosis Type 1 (NF-1) is the most common autosomal dominant multiorgan genetic disorder, caused by mutation in the NF-1 gene located on chromosome 1711.2. It is primarily characterized by a wide range of clinical features, including cutaneous neurofibromas, Café-au-lait macules, axillary or inguinal freckling, Lisch nodules, and skeletal abnormalities. NF-1 is also associated with tumor formation along peripheral nerves.
Gastrointestinal (GI) manifestations occur in approximately 10-25% of NF-1 cases but are often nonspecific and underdiagnosed. Among these, Mesenteric neurofibromatosis is a rare entity for both adults and children and has been described only in a limited number of case reports. These lesions are typically benign, some may undergo malignant transformation, making early detection crucial for optimal management. Clinical presentations range from asymptomatic to varied GI symptoms such as abdominal pain, diarrhea, weight loss, ulceration, bowel obstruction, intussusception, or volvulus.
In this report, we present a rare case of mesenteric neurofibromatosis in a 15-year-old boy who presented with abdominal pain and features of bowel obstruction.
Imaging raised suspicion for an infiltrative mesenteric process, and histopathological analysis confirmed the diagnosis. This case underscores the importance of considering mesenteric neurofibromatosis in NF-1 patients with gastrointestinal symptoms and adds to the growing literature on this rare manifestation.
2. Case Presentation
A 15-year-old male was admitted to the department of general surgery Prathima institute of Medical Sciences with complaints of abdominal pain, vomiting and abdominal distinction. He reported a history of similar symptoms one year prior, including intermittent abdominal pain, vomiting and alternating episodes of Constipation and diarrhea, which were managed conservatively.
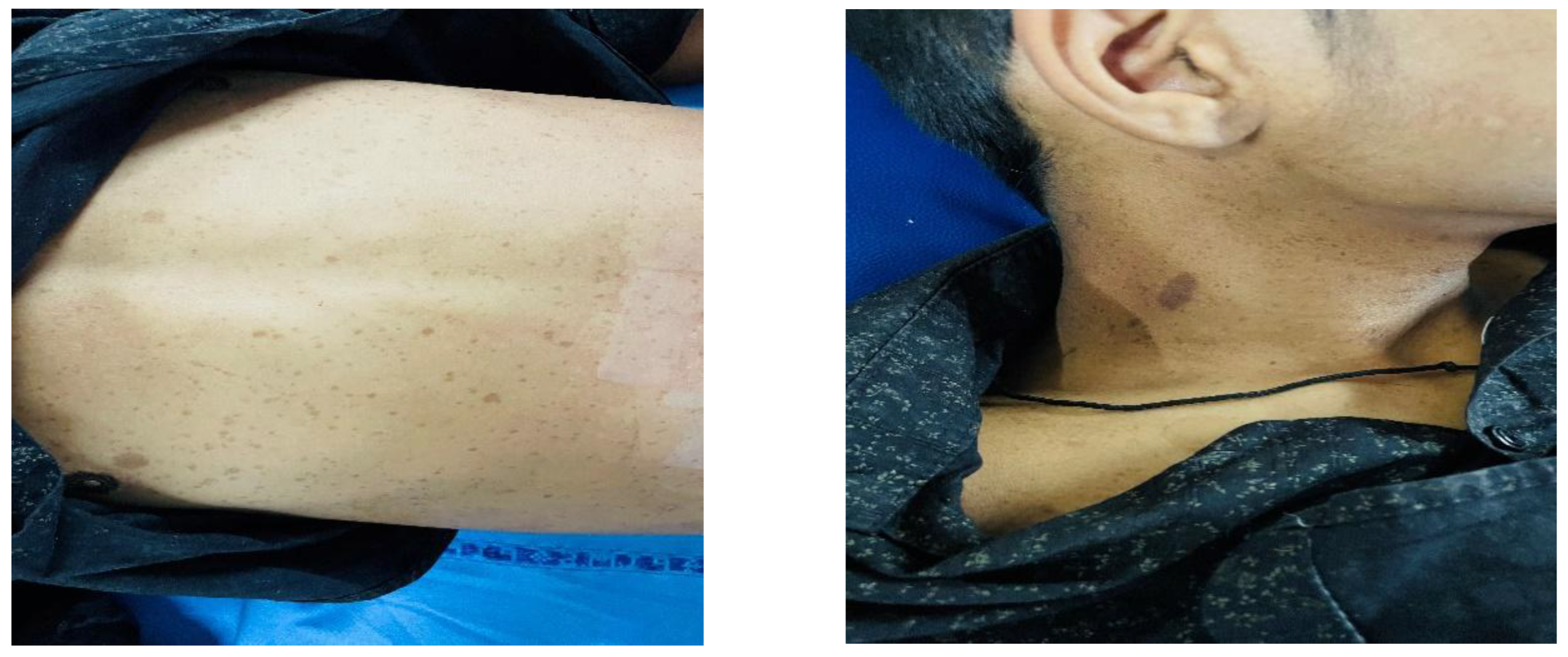
On this occasion the abdominal pain was more severe and persistent. Clinical examination revealed multiple Café-au-lait spots, the largest measuring approximately
2x1cm on the neck along with several smaller spots distributed over the abdomen [
Figure 2]. Abdominal examination demonstrated localized tenderness in the right iliac fossa, left lumber and left iliac region. A firm, diffuse, irregular mass was palpable in the right iliac fossa crossing the midline. No signs of peritoneal irritation were noted. Digital rectal examination revealed an empty rectal balloon.
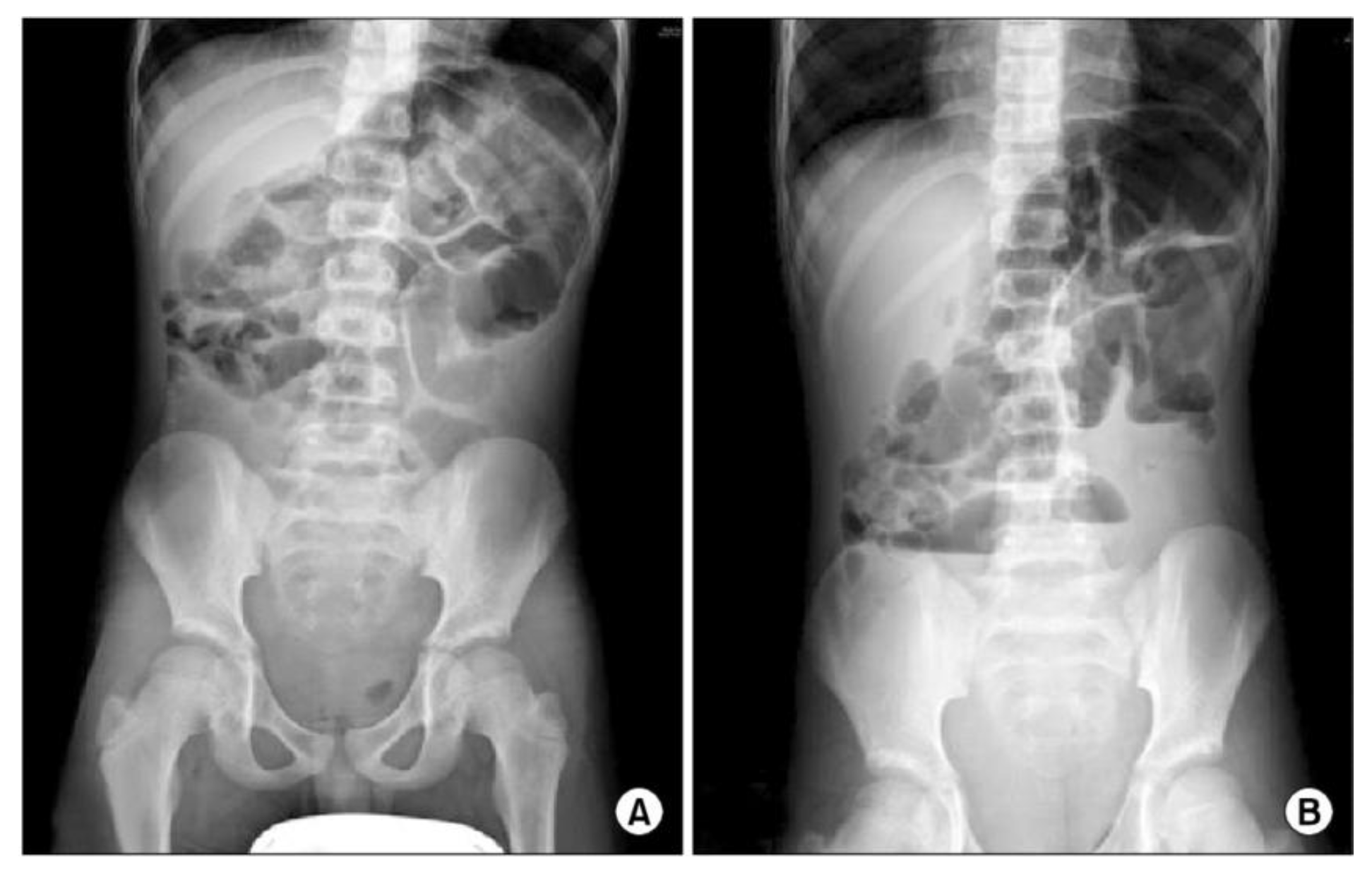
His abdomen x ray image showed a lot of air fluid levels [
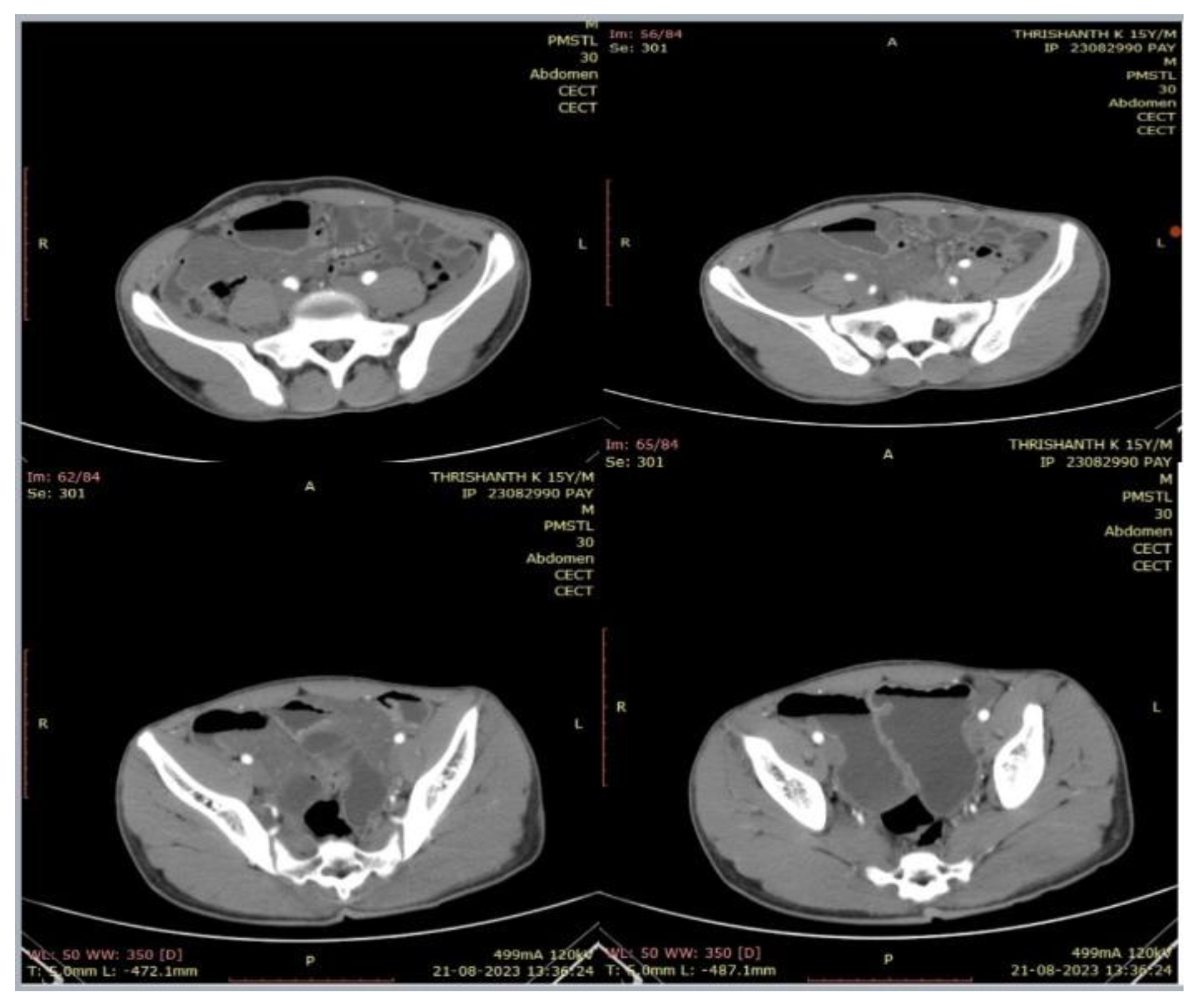
Figure 1]. On the abdominal ultrasound the bowel was dilated and distended with air. On enhanced CT image, there is evidence of ill-defined mass like soft tissue thickening noted involving the mesentery of the small bowel [
Figure 3].
On ophthalmology examination patient have multiple lisch nodules on iris.
Figure 1.
A 15-year-old male patient with NF-1 presented with abdominal pain and distension. (A) supine abdominal x ray, (B) erect x ray abdomen showing multiple air fluid levels.
Figure 1.
A 15-year-old male patient with NF-1 presented with abdominal pain and distension. (A) supine abdominal x ray, (B) erect x ray abdomen showing multiple air fluid levels.
Figure 2.
multiple Café-au-lait spots, the largest measuring approximately 2x1cm on the neck along with several smaller spots distributed over the abdomen.
Figure 2.
multiple Café-au-lait spots, the largest measuring approximately 2x1cm on the neck along with several smaller spots distributed over the abdomen.
Figure 3.
A 15-year-old male patient with NF-1 presented with abdominal pain and distension. Ill defined mass like soft tissue thickening noted involving the mesentery.
Figure 3.
A 15-year-old male patient with NF-1 presented with abdominal pain and distension. Ill defined mass like soft tissue thickening noted involving the mesentery.
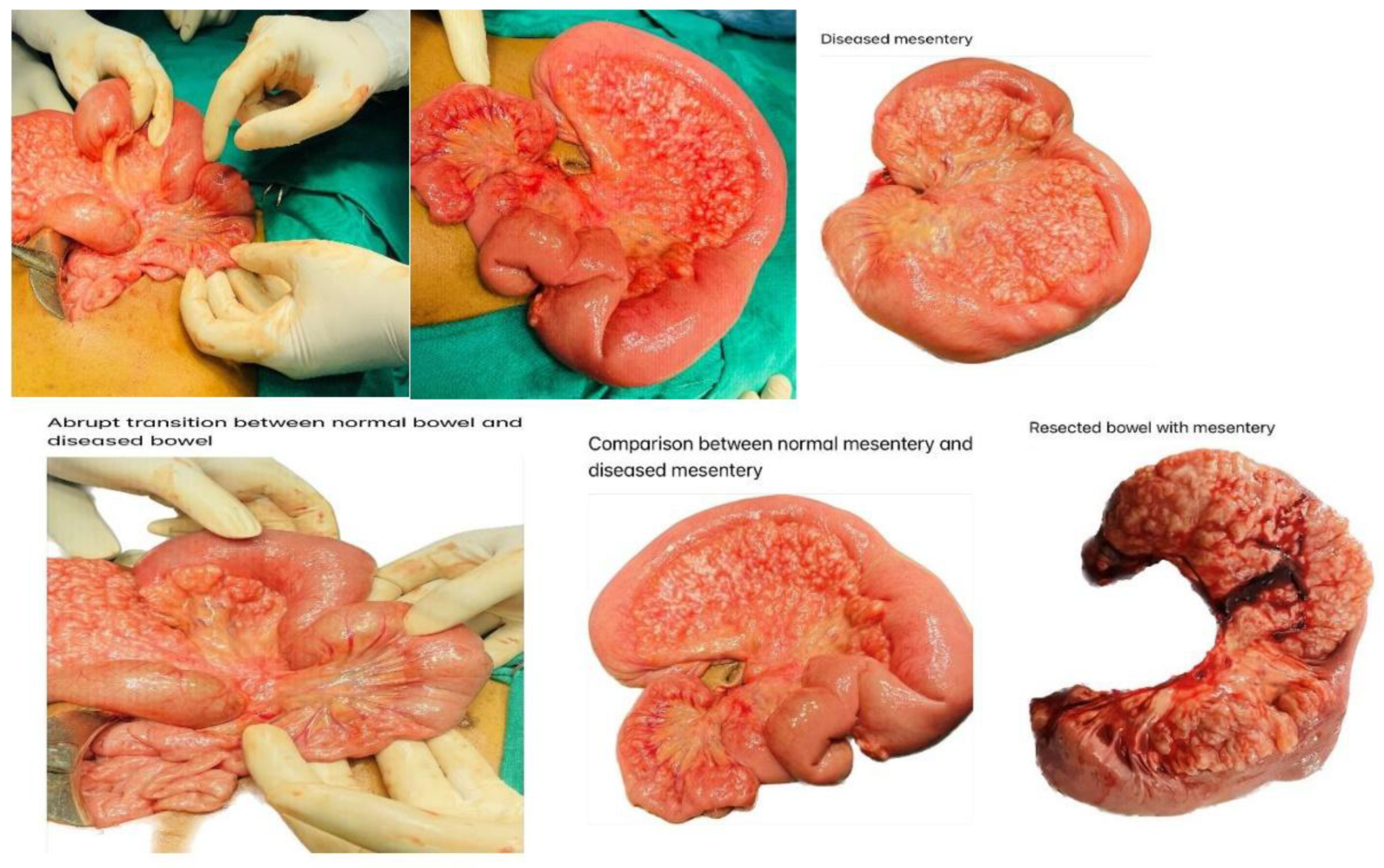
The patient underwent an exploratory laparotomy. Intraoperative observation showed that the bowel loops were dilated about 5cm diameter involving the ileum and caecum and colon are soft in palpation without dilation. The entire mesentery of the ileum is thickened with yellow nodular cord like structures, there is abrupt cut-off between the abnormal mesentery and normal mesentery [
Figure 4]. Entire involved mesentery along with the involved bowel is resected and end to end anastomosis of normal bowel is done.
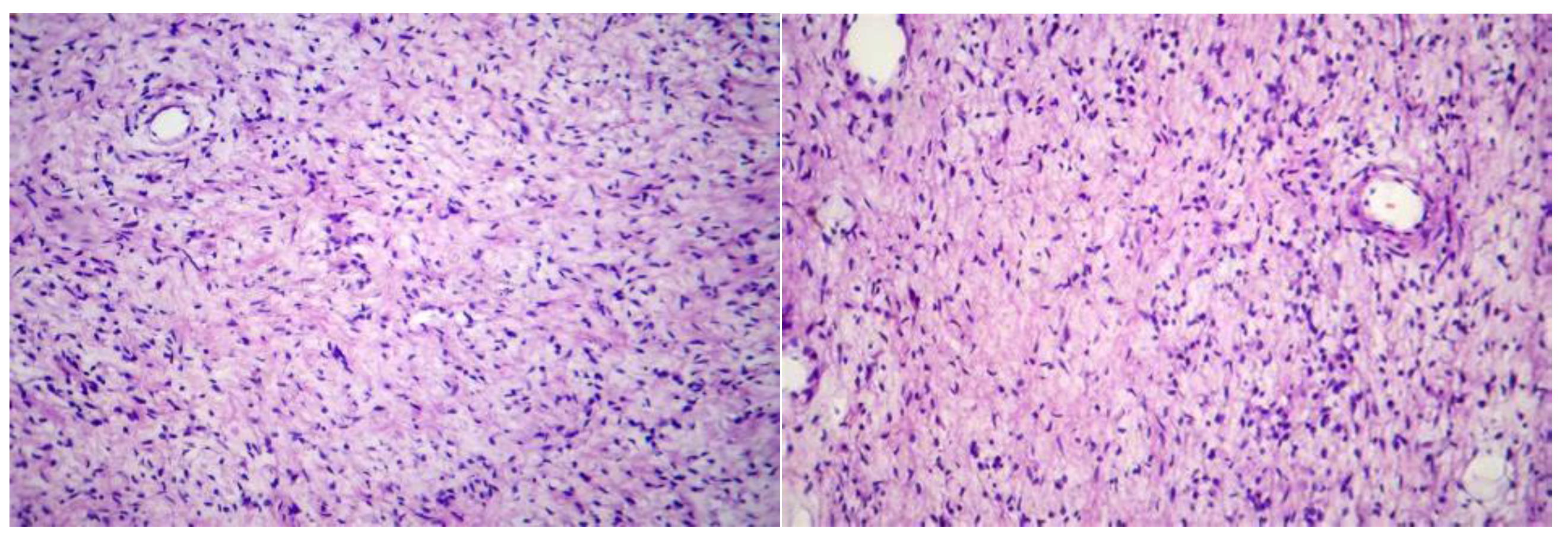
The patient performed biopsy on the lesion of the mesentery and dilated ileum. The H&E staining on the mesenteric lesions showed tumor tissue structure consisting of clusters of long slender spindle cells with wavy cytoplasm and slightly mucoid basal substance. No evidence of malignant transformation was seen. The final pathologic diagnosis was benign neurofibromatosis.
Figure 5.
A 15-year-old male patient with NF-1 presented with abdominal pain and distension. Pathologic images of mesenteric lesions: H&E stain showed tumor tissue structure consisting of clusters of long slender spindle cells with wavy cytoplasm.
Figure 5.
A 15-year-old male patient with NF-1 presented with abdominal pain and distension. Pathologic images of mesenteric lesions: H&E stain showed tumor tissue structure consisting of clusters of long slender spindle cells with wavy cytoplasm.
3. Discussion
Neurofibromatosis type I (NF-1), also known as Von Recklinghausen disease, is an autosomal dominant neurocutaneous syndrome resulting from mutations in the NF1gene located on chromosome 17q11.2. The disorder has a global prevalence of approximately 0.033% and affects all genders and ethnicities equally. Although NF-1 is inherited in an autosomal dominant manner, around 50% of cases arise from de novo mutations without a family history. Our patient similarly had no known family history, consistent with this high rate of spontaneous mutation.
NF-1 predominantly affects the peripheral nervous system and skin. Common clinical features include café-au-lait macules, intertriginous freckling (axillary or inguinal), neurofibromas, and iris hamartomas (Lisch nodules). Café-au-lait spots are often the earliest manifestation, sometimes present at birth, while freckling typically appears by ages 3 to 5. These cutaneous findings form part of the NIH diagnostic criteria and can help establish an early diagnosis.
Abdominal involvement occurs in 10–25% of NF-1 patients and is usually localized to the retroperitoneum or paraspinal areas. Mesenteric neurofibromatosis, however, is a rare manifestation. Gastrointestinal neurofibromas are often asymptomatic, with lesions identified incidentally during imaging or surgery. When symptomatic, the stomach and jejunum are the most common sites of involvement. Symptoms can vary depending on lesion size, location, and degree of mucosal involvement and may include gastrointestinal bleeding or abdominal discomfort. Approximately 65% of small mesenteric neurofibromas remain clinically silent.
Imaging is essential for diagnosis and follow-up. On ultrasonography, neurofibromas typically appear as homogenous or heterogeneous hypoechoic masses. A barium study may reveal mucosal or submucosal polyps, ulcerations, or external mass effects. CT scan findings include smooth, well-circumscribed, hypoattenuating lesions with precontrast Hounsfield units ranging from 20–30 and mild venous phase enhancement (30–50 HU). This appearance is attributed to the mucin-rich stroma of neurofibromas. Infiltrative lesions in the perirectal region may demonstrate fatty stranding and potential spread to adjacent pelvic structures such as the uterus or vagina.
MRI is especially useful for characterizing soft tissue lesions and differentiating benign from potentially malignant masses. Neurofibromas generally appear hypointense on T1-weighted and hyperintense on T2-weighted images due to their high water content and myxoid matrix. Central hypointensity on T2W may represent fibrosis, while gadolinium contrast typically produces mild enhancement. Heterogeneous signal intensity with cystic degeneration or necrosis on T2W images may suggest malignant transformation, which warrants histological evaluation through multiple biopsies.
Management of mesenteric neurofibromatosis should be individualized. Complete surgical excision remains the treatment of choice when feasible. However, in cases where resection would carry significant morbidity, as in our case, conservative management with biopsy and close clinical and radiologic follow-up is appropriate. Regular imaging is essential to detect signs of progression or malignant change. Indicators of transformation include rapid growth, increasing pain, or new-onset symptoms.
Adjuvant therapies such as ketotifen fumarate, cis-retinoic acid, interferon, and thalidomide have been explored for symptom control and tumor stabilization in inoperable or progressive lesions. Nevertheless, early detection and longitudinal monitoring remain the cornerstone of management to prevent complications associated with advanced or malignant disease.
4. Conclusions
Mesenteric neurofibromatosis is a rare benign lesion that can transform into malignancy. It often does not show specific clinical symptoms, easily confused with other digestive disorders. Therefore, diagnostic imaging methods for early detection of GI lesions in patients with NF-1 or patients at risk are necessary. If detected at an early stage, the lesion can be completely removed by surgery. In cases of total resection impossible, the tumor should be periodically followed both clinically and radiologically to detect early signs of malignant transformation.
Consent
Written informed consent was obtained from the patient/patient's family for publication of this case report and accompanying images. A copy of the written consent is available for review by the Editor-in-Chief of this journal on request.
Ethical approval
Ethical approval is not a requirement at our institution for reporting individual cases or case series.
References
- Zulfiqar M, Lin M, Ratkowski K, Gagnon MH, Menias C, Siegel CL. Imaging features of neurofibromatosis type 1 in the abdomen and pelvis. AJR Am J Roentgenol. 2021;216:241–51. [CrossRef]
- Cavallaro G, Basile U, Polistena A, Giustini S, Arena R, Scorsi A, et al. Surgical management of abdominal manifestations of type 1 neurofibromatosis: Experience of a single center. Am Surg. 2010;76:389–96.
- Rajiah P, Sinha R, Cuevas C, Dubinsky TJ, Bush WH, Jr, Kolokythas O. Imaging of uncommon retroperitoneal masses. Radiographics. 2011;31:949–76. [CrossRef]
- Ozcan HN, Karcaaltincaba M, Oguz B, Haliloglu M. Radiological manifestations of abdominopelvic nerve tumours seen in neurofibromatosis type 1. Clin Radiol. 2014;69:431–5. [CrossRef]
- Koşucu P, Ahmetoĝlu A, Cobanoĝlu U, Dinç H, Ozdemir O, Gümele HR. Mesenteric involvement in neurofibromatosis type 1: CT and MRI findings in two cases. Abdom Imaging. 2003;28:822–6. [CrossRef]
- Imamoğlu M, Cay A, Yariş N, Yayla S, Sarihan H. Intestinal mesenteric involvement with plexiform neurofibroma in neurofibromatosis type 1. Pediatr Int. 2006;48:337–9. [CrossRef]
- Gorbounova I, Lenahan A, Wenger T, Rudzinski E, Tang E, Smith C, et al. Mesenteric plexiform neurofibroma as a cause of weight loss and chronic diarrhea in a patient with YPEL3 variant. JPGN Reports. 2021;2:e098. [CrossRef]
- Li YT, Chen H, Ding X, Wu Q, Guo QC, Hu DM, et al. Features of CT and EUS in mesenteric plexiform neurofibroma with Neurofibromatosis type I: A case report. Radiol Case Rep. 2021;16:2103–7. [CrossRef]
- Levy AD, Patel N, Dow N, Abbott RM, Miettinen M, Sobin LH. From the archives of the AFIP: Abdominal neoplasms in patients with neurofibromatosis type 1: Radiologic-pathologic correlation. Radiographics. 2005;25:455–80. [CrossRef]
- Fortman BJ, Kuszyk BS, Urban BA, Fishman EK. Neurofibromatosis type 1: A diagnostic mimicker at CT. Radiographics. 2001;21:601–12. [CrossRef]
|
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2025 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (http://creativecommons.org/licenses/by/4.0/).