1. Introduction
Breastfeeding in the early postpartum period is widely recognized as critical to both maternal and infant health, yet it is also a time when mothers face significant challenges. Among these, nipple trauma is one of the most common issues, reported in over 60% of breastfeeding women [
1]. Painful nipple injuries can undermine maternal confidence and contribute to premature cessation of breastfeeding [
2,
3]. Despite the importance of early support, in-person care is often limited during the first postpartum month due to healthcare system constraints and social factors such as nuclear family structures [
4].
In Japan, for instance, although nearly all mothers express an intention to breastfeed, the exclusive breastfeeding rate drops to just over 50% by one month postpartum [
5]. A shortage of skilled lactation support, especially among midwives with increasing responsibilities, exacerbates this problem. Technological interventions may help bridge this gap. Since the COVID-19 pandemic, the expansion of online support tools has shown potential to enhance maternal confidence and improve breastfeeding outcomes [
6].
Recent advances in artificial intelligence (AI), particularly deep learning, have made it possible to automate the classification of medical images with high accuracy [
7,
8]. In a previous study, we developed a deep learning-based system that analyzes photographs of the nipple taken by postpartum mothers and automatically classifies the degree of nipple trauma using convolutional neural networks (CNNs) trained on clinical image data [
9]. This system offers objective assessments, which can complement clinical judgment and reduce variability in caregiver evaluations [
10].
While the system's technical validity has been demonstrated in prior research, its practical feasibility and acceptability in real-world clinical settings remain unclear. As digital-native generations of mothers become more prevalent, it is essential to understand how such AI-assisted tools are received by users, and whether they can be safely and effectively integrated into postpartum care.
Therefore, the aim of this study was to evaluate the feasibility and acceptability of a deep learning–based nipple trauma assessment system implemented during postpartum hospitalization. In addition, maternal perceptions of the intervention, including subjective experiences and breastfeeding self-efficacy, were explored.
2. Materials and Methods
2.1. Study Design and Setting
This quasi-experimental study was conducted at a single obstetric hospital in City A, Japan, between July and November 2024. Participants were allocated to an intervention or control group based on their expected month of delivery (August or September 2024, respectively). To minimize bias from caregiver variability, only one facility was used.
2.2. Participants
Eligible participants were Japanese women aged 18 years or older who were in the late stage of pregnancy and planned to breastfeed. Women were excluded if direct breastfeeding was not feasible due to factors such as maternal mental illness, risk of mother-infant infection, anticipated long-term separation, or if they were unable to operate a smartphone.
2.3. Intervention
Participants in both groups received standard postpartum care, including lactation support during hospitalization and home visits. In addition, the intervention group received feedback based on a deep learning-based assessment of nipple images.
During hospitalization, mothers in the intervention group used a dedicated, offline smartphone to take close-up photographs of their nipples. These images were then analyzed using the deep learning system, which classified nipple conditions into “mild,” “moderate,” or “severe” categories. Feedback and breastfeeding advice were provided through the official research LINE account based on the system’s results. To assess user impressions, participants in the intervention group were asked to complete four Likert-scale items and one open-ended question.
The smartphone model used was Black view A95, with a resolution of 720×1600 pixels. All images were collected and analyzed in an offline environment to ensure data security.
2.4. Data Collection
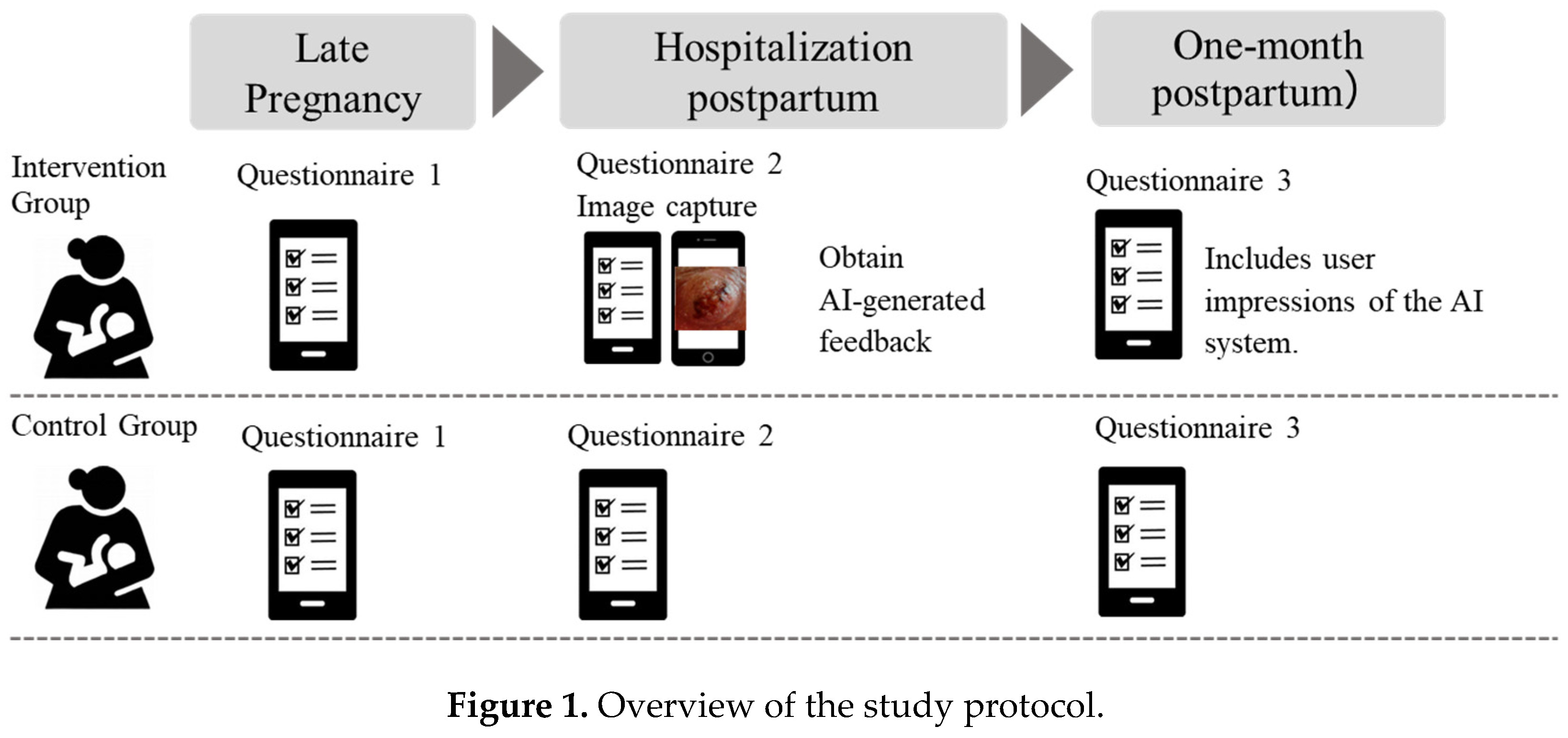
Figure 1 shows the overview of the study protocol. Three self-administered questionnaires were distributed via Google Forms through the LINE platform at three time points:
•T1 (Late pregnancy): breastfeeding intention, maternal demographics, obstetric history.
•T2 (Hospitalization postpartum): delivery details, feeding method, breastfeeding self-efficacy (BSES-SF) [
11,
12], and breastfeeding satisfaction.
•T3 (One-month postpartum): intervention feedback (intervention group only), current feeding method, breastfeeding self-efficacy (BSES-SF), and breastfeeding satisfaction.
2.5. Measures
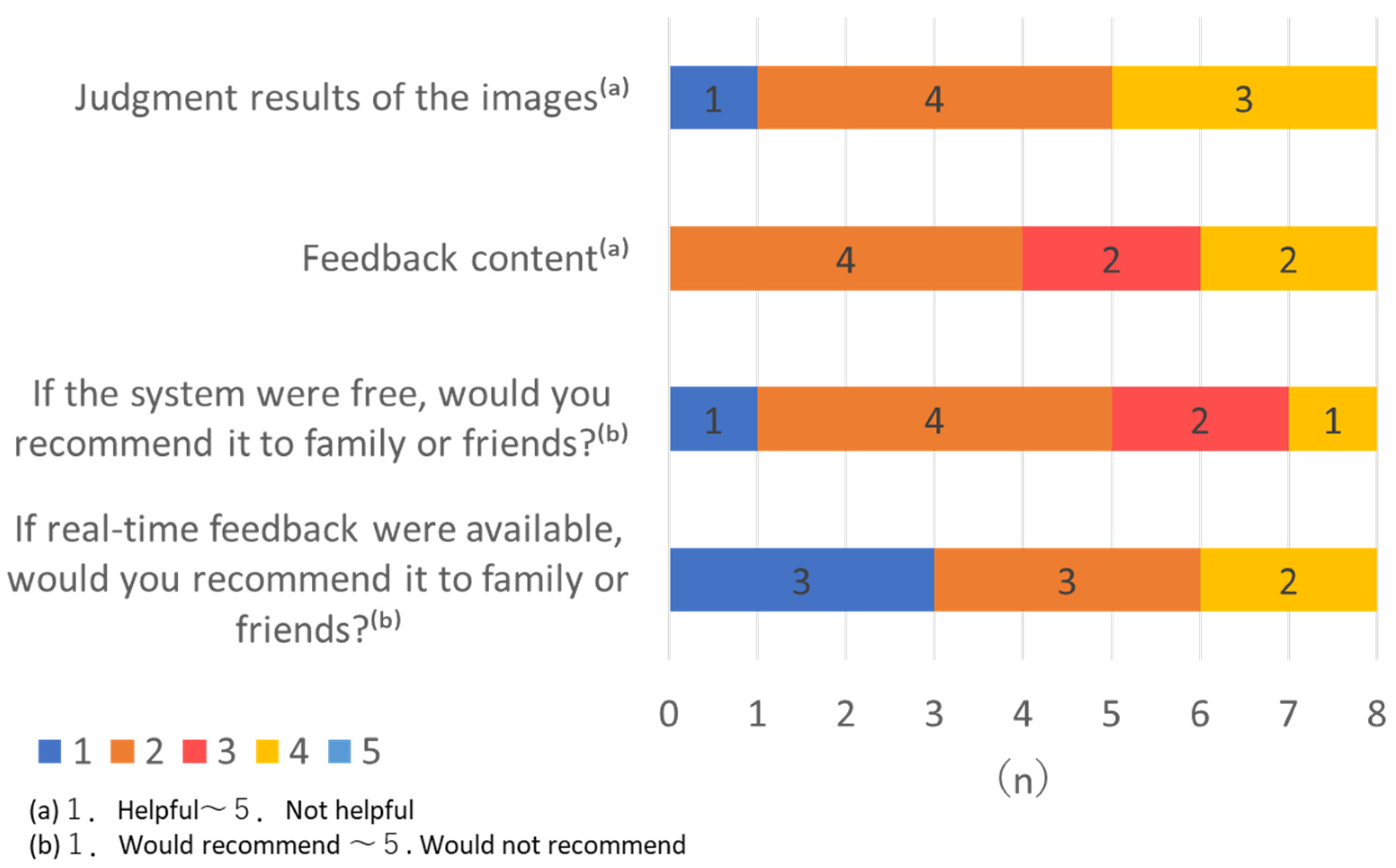
Impressions of using the deep learning system were assessed among participants in the intervention group using four single-item, 5-point Likert scales.
•Usefulness evaluations: Participants rated the usefulness of the AI-generated im age classification results and the helpfulness of the feedback content. Response options ranged from 1 ("Helpful") to 5 ("Not helpful").
•Recommendation intent: Participants were asked whether they would recommend the system to family or friends if it was free of charge, and if real-time feedback were available. Response options ranged from 1 ("Would recommend") to 5 ("Would not recommend").
•Breastfeeding Self-Efficacy Scale – Short Form (BSES-SF): A 14-item, 5-point Likert scale validated in Japanese [
11,
12]. A score of 50 or below is considered indicative of low breastfeeding confidence [
12].
•Breastfeeding satisfaction: A single-item, 3-point Likert scale assessing overall satisfaction with the current breastfeeding experience. Participants selected one of the following responses: "Satisfied," "Somewhat satisfied," or "Not satisfied."
2.6. Ethical Considerations
The study was approved by the Ethics Committee of the Faculty of Health Sciences, Hokkaido University (Approval No. 24-18). Written informed consent was obtained from all participants. All data were anonymized and managed securely, and nipple images were transferred directly from the dedicated device to an offline computer to prevent online data leakage.
3. Results
3.1. Participant Flow
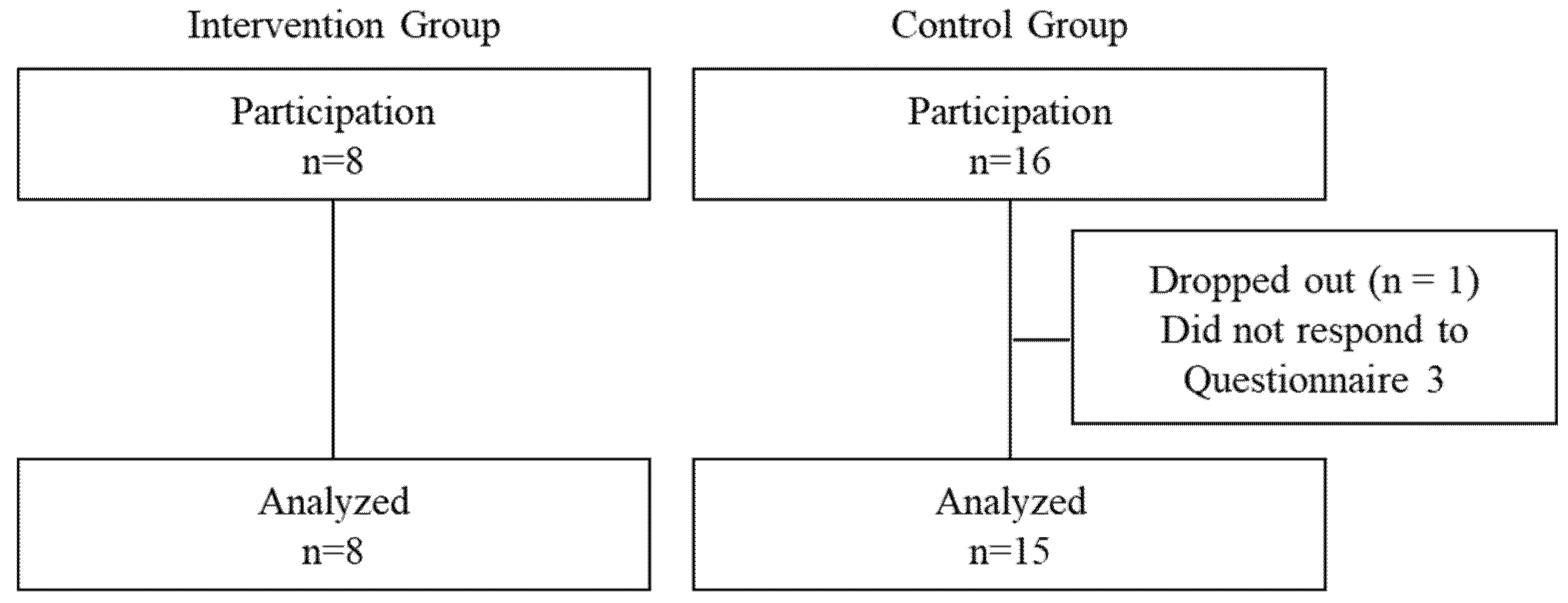
Figure 2 shows study flow. A total of 24 participants consented to join study 8 in the intervention group (expected delivery in August 2024) and 16 in the control group (expected delivery in September 2024). One control participant did not complete the final questionnaire at the one-month check-up and was excluded. Thus, 23 participants (intervention group: n = 8; control group: n = 15) were included in the final analysis. The complete response rate was 95.8%.
3.2. Participant Characteristics
Table 1 shows the demographic characteristics of the participants. The majority were primiparous (intervention group: 62.5%; control group: 80.0%). Approximately 75% of all participants were employed. There were no significant differences between groups except for age; the control group was significantly younger (p < 0.01). All participants delivered at term, with a mean gestational age of approximately 39 weeks. Most births were vaginal, with a few cesarean sections observed in the control group. Regarding breastfeeding intentions during pregnancy, participants in the control group were more likely to respond “Willing to breastfeed if milk is available” (n = 13, 86.6%). In contrast, in the intervention group, three participants (37.5%) selected either “I intend to use formula” or “No specific plan,” indicating a relatively lower baseline intention to exclusively breastfeed.
3.3. Analysis of AI Feedback and User Evaluation
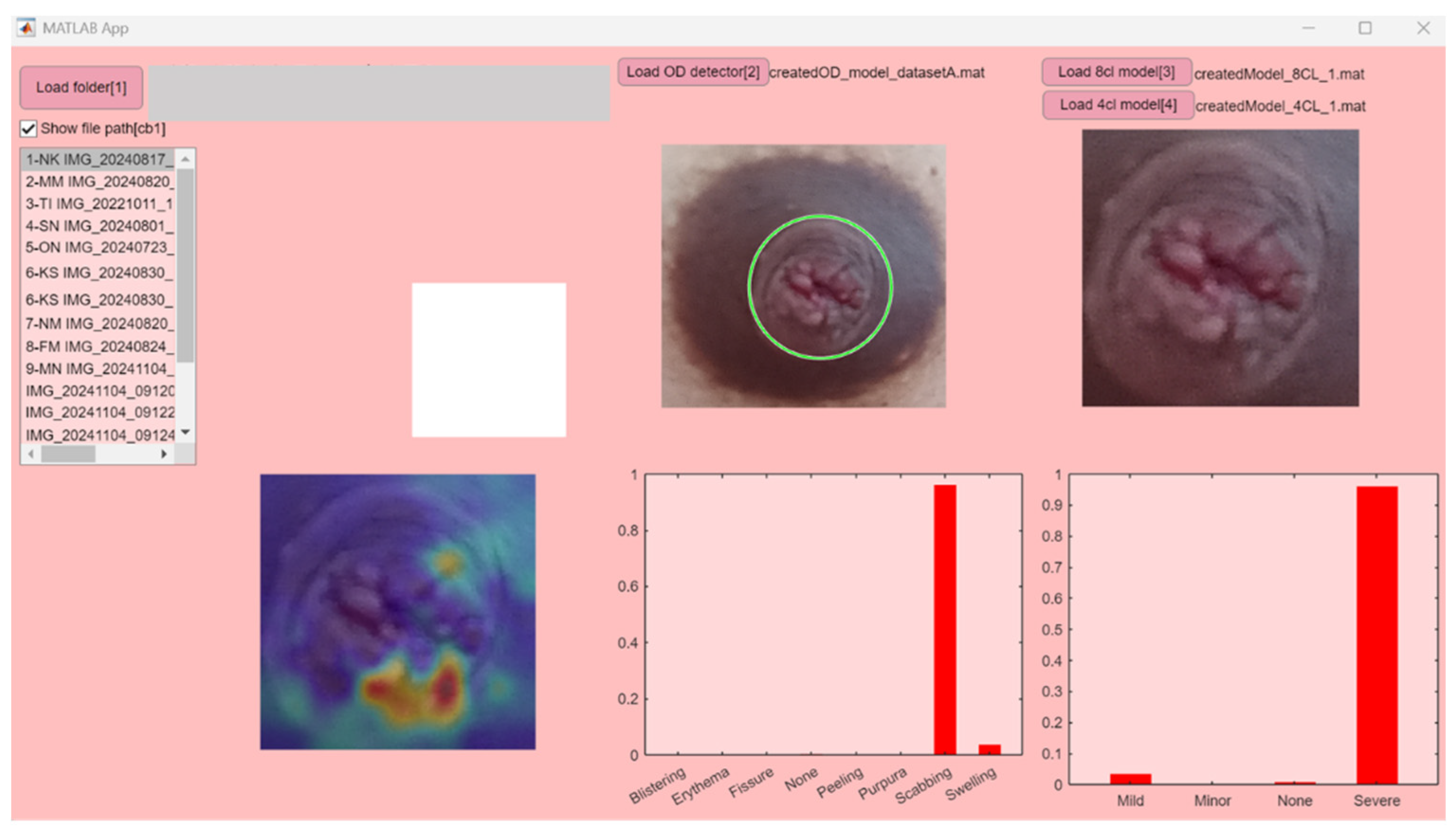
Figure 3 presents an example interface displaying the AI analysis results, and
Table 2 summarizes image-related information and the corresponding deep learning outputs. The class-wise posterior probabilities for each image were visualized on the software. The posterior class probabilities returned by MATLAB’s predict function were displayed as a bar chart, with class labels on the x-axis and probability values (ranging from 0 to 1) on the y-axis. In the intervention group, all submitted images were successfully analyzed by the AI system without technical errors, and no adverse events were reported by participants.
Based on the system’s classification, 12.5% of participants received a “green” result, indicating no visible nipple damage; 25.0% received a “yellow” result, indicating mild damage; and 62.5% received a “red” result, indicating severe damage.
Notably, the majority of participants (75%) received high-probability diagnostic outputs from the system (i.e., predicted class probability ≥ 60%). This suggests that the AI system not only functioned reliably but also provided results with a high level of certainty, potentially enhancing user trust in the feedback.
Figure 4 presented mothers’ feedback regarding the AI system. Ratings on usefulness and recommendation intention were moderate (means around 2–3 on a 5-point scale). Two mothers provided open-ended comments noting that the AI helped them recognize nipple trauma and made it easier to apply ointment effectively. Overall, participants rated the system as helpful (mean score for image judgment = 2.62; for feedback content = 2.75; on a 5-point Likert scale where 1 = helpful and 5 = not helpful). In terms of perceived value, most participants indicated they would recommend the system to others if it were free (mean = 2.37), and even more favorably if real-time feedback were available (mean = 2.12).
In addition, open-ended responses were collected from two participants (25%) in the intervention group. One mother expressed a desire to receive support not only during hospitalization but also in the early postpartum period at home (e.g., 4 days to 2 weeks after birth). Another mother noted that identifying the exact location of nipple trauma made it easier to apply ointment appropriately, especially when pain was widespread and the lower part of the nipple was difficult to visualize. These qualitative responses support the potential utility of AI-based image feedback for improving mothers' self-care and access to timely support.
These findings highlight the system’s operational feasibility and suggest strong user interest in enhanced features such as real-time analysis and post-discharge usability.
3.4. Breastfeeding Status at Hospitalization and One-Month Check-Up
Table 3 summarizes changes in breastfeeding practices. At hospitalization, none of the mothers in the intervention group exclusively breastfed, whereas 13.3% in the control group did. At one month postpartum, the percentage of mothers exclusively breastfeeding increased in both groups, with 46.6% in the control group and 12.5% in the intervention group.
3.5. Maternal Perception of Breastfeeding
Table 4 presents maternal evaluation scores. At hospitalization, 66.6% of the control group reported being satisfied with their feeding method, compared to only 25.0% in the intervention group. By one month, 62.5% of the intervention group also reported satisfaction.
The BSES-SF scores increased in both groups over time. Although the differences were not statistically significant, the control group consistently showed higher mean scores. The mean score increased by about 10 points in the intervention group and 8 points in the control group.
4. Discussion
This study explored the feasibility and acceptability of a deep learning-based nipple trauma assessment system implemented during postpartum hospitalization. Despite the small sample size, the findings offer important insights into the system’s potential clinical application and user perception.
4.1. Participant Characteristics and Baseline Trends
The characteristics of participants in this study were generally consistent with previous reports on Japanese postpartum women [
13]. Most participants were primiparous, employed, and part of nuclear families, reflecting contemporary maternal demographics in Japan. Although the control group was significantly younger, all participants were of the digital-native generation, and the influence of age differences was considered minimal.
However, previous research has suggested that older maternal age may be associated with higher breastfeeding satisfaction [
14]. Therefore, age should be taken into consideration when interpreting the results.
4.2. System Feasibility and Safety
The AI system was successfully implemented without technical errors or adverse events, supporting its feasibility for clinical use during postpartum hospitalization. All images submitted by mothers were correctly analyzed, and diagnostic results were consistent with previously reported distributions of nipple trauma severity in postpartum women [
15]. Notably, 75% of the intervention group received high-probability outputs (≥60%), suggesting the system’s robustness and potential to inspire user confidence. These results confirm that AI-based assessments can be effectively integrated into real-world maternity care under secure, offline conditions.
4.3. Maternal Feedback and Usability
Overall, participants rated the system as helpful, and many expressed interests in using similar tools post-discharge. Ratings on usefulness and recommendation intent were moderate to favorable, with lower scores (i.e., stronger interest) reported for a version offering real-time feedback. These findings are consistent with earlier reports indicating that timely, interactive support enhances breastfeeding satisfaction and self-efficacy [
16].
Open-ended responses further supported the system’s value: one mother appreciated the ability to locate trauma sites for accurate ointment application, while another requested continued support during the early post-discharge period. These responses suggest that AI-based visual feedback may empower mothers to manage nipple care more independently, especially when professional support is not readily accessible.
4.4. Impact on Breastfeeding Experience
While no statistically significant group differences were observed, improvements in breastfeeding self-efficacy (BSES-SF) were noted in both groups, with a slightly greater increase in the intervention group. This trend aligns with the hypothesis that personalized feedback could reinforce maternal confidence. Notably, the intervention group started with lower prenatal breastfeeding intention and satisfaction during hospitalization, potentially influencing post-intervention outcomes. These baseline differences should be considered when interpreting the results.
Importantly, due to the lack of a security system for transmitting sensitive images from home, the intervention was conducted during hospitalization rather than after discharge, as originally planned. Ideally, the impact of such an AI-based system should be evaluated during the post-discharge period, when professional support is limited and mothers are managing breastfeeding more independently. Therefore, the observed changes in self-efficacy and satisfaction should be regarded as secondary outcomes, reflecting the feasibility and preliminary effects of inpatient implementation, rather than the full potential of post-discharge intervention.
4.5. Practical and Ethical Challenges
Several practical and ethical challenges emerged during the implementation of this study. Initially, we aimed to enable prompt AI-based diagnosis by allowing participants to submit images remotely, including after hospital discharge. However, we were compelled to revise our study protocol because no image transmission system currently available in Japan met the necessary standards for privacy, security, and user confidence. As a result, several limitations arose. First, the time lag (0–2 days) between image submission and feedback delivery limited the immediacy of support. Second, the use of sensitive images may have discouraged some potential participants, particularly multiparous women. In future studies, ensuring secure yet user-friendly remote data transmission will be essential especially for post-discharge use. Real-time feedback functionality, end-to-end encryption, and automated anonymization could enhance both effectiveness and acceptability.
Moreover, the number of participants was substantially lower than originally planned, particularly among multiparous women. This limited recruitment may have reduced the diversity of maternal needs captured by the study. To enhance the appeal and practicality of the system for a broader range of mothers, future iterations should consider expanding its functionality beyond nipple trauma—for example, to include support for managing mastitis, guidance on formula supplementation, and general breastfeeding consultation. Such enhancements may increase the system’s relevance, particularly for experienced mothers who may have different support expectations and preferences.
4.6. Clinical Implications and Future Directions
The present study demonstrates that a deep learning–based nipple trauma assessment system can be safely and feasibly implemented during postpartum hospitalization. While the intervention was limited to a single image submission during inpatient care, the results suggest that even minimal AI-assisted feedback can positively influence maternal perceptions of breastfeeding. This is particularly relevant in modern maternity care contexts, where staffing shortages and shorter hospital stays often reduce opportunities for in-person breastfeeding support.
The integration of AI into postpartum care offers a promising strategy to supplement midwife-led interventions, especially during the critical transition from hospital to home. Given that many participants expressed interest in continued support after discharge, future iterations of the system should prioritize real-time functionality and remote usability. These advancements will require the development of secure image transfer protocols, user-friendly mobile applications, and ethical frameworks for handling sensitive health data. Importantly, such features must be designed to align with maternal preferences for privacy, usability, and timeliness.
In addition, this study highlights the need to diversify and strengthen recruitment strategies. The underrepresentation of multiparous women suggests that broader system appeal—through expanded features such as mastitis detection or personalized feeding advice—may be necessary to engage a wider demographic. Tailoring AI feedback to maternal experience levels, breastfeeding goals, and psychosocial context could improve both uptake and sustained use.
Finally, future research should aim for larger, more diverse samples and longitudinal designs to assess the long-term impact of AI-assisted support on breastfeeding duration, maternal confidence, and infant health outcomes. As the population of digital-native mothers continues to grow, the integration of AI into maternal health services must evolve in parallel, ensuring accessibility, equity, and clinical relevance across care settings.
5. Conclusions
This study demonstrated the feasibility and acceptability of a deep learning–based nipple trauma assessment system implemented during postpartum hospitalization. The system functioned safely and reliably for all participating mothers, with no adverse events reported. Most participants found the feedback helpful, and many expressed interest in future use beyond hospitalization.
To enhance clinical applicability, future development should focus on secure remote access, real-time analysis, and expanded features to support broader breastfeeding concerns. These improvements may increase usability and meet the diverse needs of postpartum mothers.
In summary, AI-assisted image analysis shows promise as a supportive tool in maternal care and warrants further research for broader implementation.
Author Contributions
Conceptualization, M.N. and E.Y.; methodology, M.N., E.Y. and H.S.; software, H.S. and M.N.; validation, M.N., E.Y. and H.S; formal analysis, M.N.; investigation, M.N.; data curation, M.N.; writing—original draft preparation, M.N.; writing—review and editing, E.Y. and H.S; supervision, E.Y.; project administration, M.N. and E.Y.; funding acquisition, M.N.
Funding
This research was funded by JST SPRING, Grant Number JPMJSP2119.
Institutional Review Board Statement
The study was conducted in accordance with the Declaration of Helsinki and approved by the Institutional Review Board of the National University Hospital Directors Conference (ID: UMIN000054751, 1. Jul. 2024.) and the Ethical Review Board of the Department of Health Sciences of Hokkaido University (Approval number: 24-18, 1. Jul. 2024.).
Informed Consent Statement
Informed consent was obtained from all subjects involved in the study. Written informed consent has been obtained from the patient(s) to publish this paper.
Acknowledgments
The authors thank the staff of the participating hospital and all mothers who took part in the study. The authors also acknowledge the support of the research collaborators who contributed to data collection and system development.
Conflicts of Interest
The authors declare no conflicts of interest.
Abbreviations
The following abbreviations are used in this manuscript:
| AI |
Artificial Intelligence |
| BSES-SF |
Breastfeeding Self-Efficacy Scale–Short Form |
References
- Buck, M. L., Amir, L. H., Cullinane, M., & Donath, S. M. Nipple pain, damage, and vasospasm in the first 8 weeks postpartum. Birth 2014, 41(2), 125–132. [CrossRef]
- Kent, J. C., Ashton, E., Hardwick, C. M., & Rowan, M. K. Nipple pain during breastfeeding. Breastfeed Med 2015, 10(9), 453–458. [CrossRef]
- Odom, E. C., Li, R., Scanlon, K. S., Perrine, C. G., & Grummer-Strawn, L. Reasons for earlier than desired cessation of breastfeeding. Pediatrics 2013, 131(3), e726–e732. [CrossRef]
- Yamakawa, S., Haga, C., Ogino, Y., et al. Characteristics and challenges of breastfeeding support in Japanese nuclear families: A qualitative study. Jpn J Public Health 2020, 67(4), 312–319. [in Japanese].
- Ministry of Health, Labour and Welfare. National Survey on Child Health and Development 2021. Available online: https://www.mhlw.go.jp/toukei/list/85-1a.html (accessed on 1 May 2025).
- Sun, Y., Gao, Y., Zhu, Z. et al. (2023). Effect of online intervention mode on breastfeeding results: a systematic review and meta-analysis. Reproductive Health, 20, 164. [CrossRef]
- Liu, Y., Jain, A., Eng, C., et al. A deep learning system for differential diagnosis of skin diseases. Nat Med 2020, 26(6), 900–908. 6. [CrossRef]
- Esteva, A., Kuprel, B., Novoa, R. A., et al. Dermatologist-level classification of skin cancer with deep neural networks. Nature 2017, 542(7639), 115–118. [CrossRef]
- Nakamura, M.; Sugimori, H.; Ebina, Y. Development of Nipple Trauma Evaluation System With Deep Learning. J. Hum. Lact. 2025, 41(1), 105–114. [CrossRef]
- Cirico, M. O. Cirico, M. O., Shimoda, G. T., & Oliveira, R. N. Healthcare quality in breastfeeding: Implementation of the nipple trauma index. Rev Gaucha Enferm 2017, 37(4), e60546. [CrossRef]
- Otsuka, K., Dennis, C. L., Tatsuoka, H., & Jimba, M. (2008). The relationship between breastfeeding self-efficacy and perceived insufficient milk among Japanese mothers. Journal of Obstetric, Gynecologic, and Neonatal Nursing, 37(5), 546–555. 1. [CrossRef]
- Nanishi K, Green J, Taguri M, Jimba M. Determining a Cut-Off Point for Scores of the Breastfeeding Self-Efficacy Scale-Short Form: Secondary Data Analysis of an Intervention Study in Japan. PLoS One. 2015;10(6):e0129698. Published 2015 Jun 24. [CrossRef]
- Hongo, H., Green, J., Shibanuma, A., Nanishi, K., & Jimba, M. (2020). The Influence of Breastfeeding Peer Support on Breastfeeding Satisfaction Among Japanese Mothers: A Randomized Controlled Trial. Journal of human lactation: official journal of International Lactation Consultant Association, 36(2), 337–347. [CrossRef]
- Ericson, J.; Flacking, R. Mothers' experiences and perceptions of breastfeeding support in neonatal intensive care units. J Clin Nurs 2021, 30(3–4), 400–409. [CrossRef]
- Nakamura, M., Sugimori, H., Asaka, Y., & Ebina, Y. (2025). Role of Silver Nipple Protectors in Treating Nipple Trauma: A Non-Randomized Comparative Trial. Journal of human lactation: official journal of International Lactation Consultant Association, 41(3), 382–391. [CrossRef]
- Ahmed, A. H., & Roumani, A. M. (2020). Breastfeeding Monitoring Improves Maternal Self-Efficacy and Satisfaction. MCN: The American Journal of Maternal Child Nursing, 45(6), 357–363. [CrossRef]
|
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2025 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).