Submitted:
10 July 2025
Posted:
11 July 2025
You are already at the latest version
Abstract
Keywords:
1. Introduction
2. Materials and Methods
Patients and Study Design
Detection of (1→3)-β-D-Glucan
Statistical Analysis
3. Results
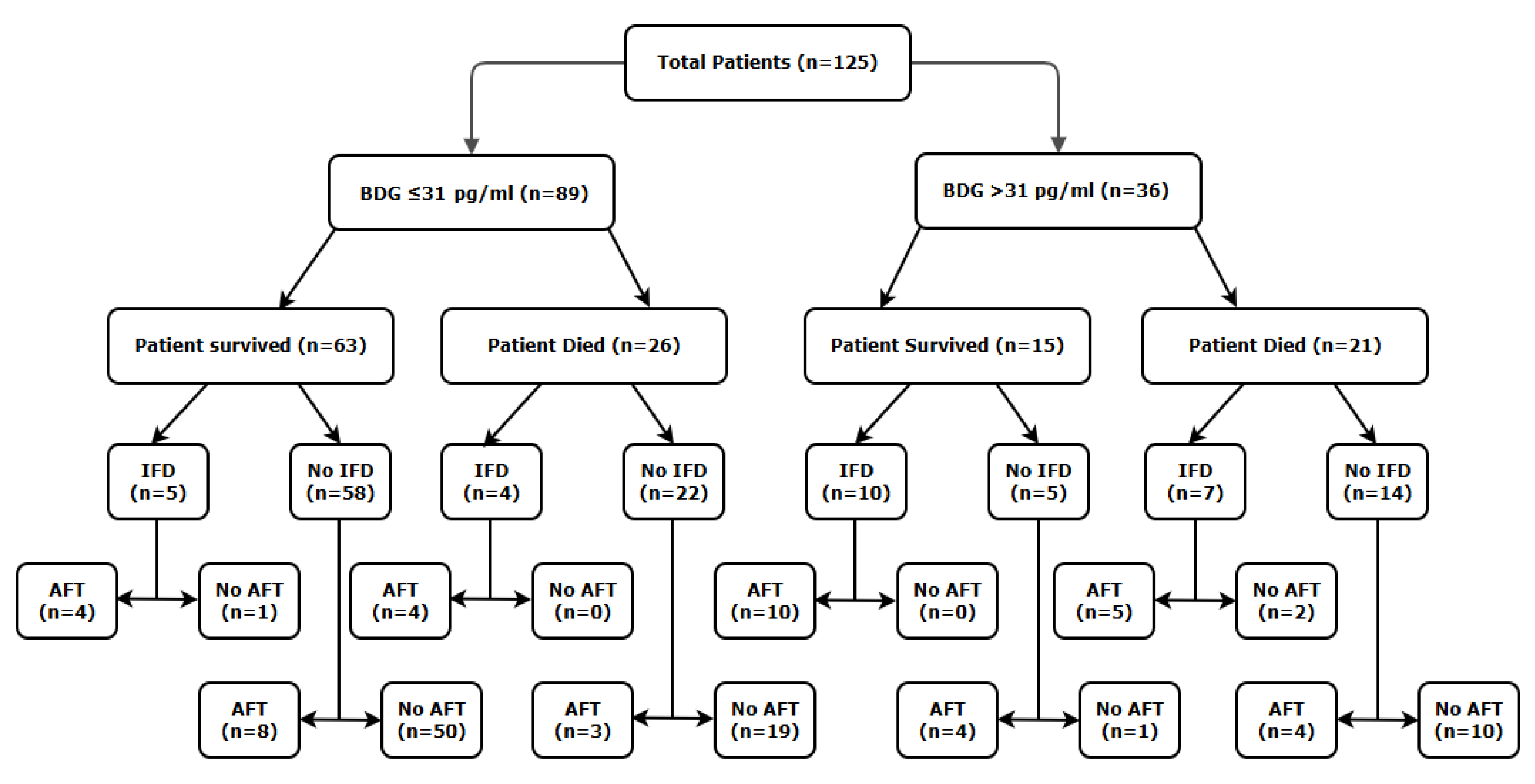
Population
(1→3)-β-D-Glucan Concentration and Mortality
Antifungal Therapy and Mortality
Mortality Associated with Invasive Fungal Disease
Mortality Associated with Invasive Fungal Disease and the Use of Antifungal Therapy
4. Discussion
5. Conclusions
Author Contributions
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Conflicts of Interest
Abbreviations
| IFD | Invasive fungal disease |
| PCT | Procalcitonin |
| BDG | (1-3)-β-D-Glucan |
| AFT | Antifungal therapy |
| EORTC | European Organization for the research and treatment of Cancer |
| MSGERC | Mycoses Study group Educational and Research Consortium |
| ECMM | European Confederation of Medical Mycology |
| ISHAM | International Society for Human and Animal Mycoses |
| CAPA | COVID-19 Associated pulmonary aspergillosis |
| 95% CI | 95% confidence intervals |
| PAMPs | pathogen-associated molecular pattern |
| LPS | Lipopolysaccharide |
| IC | Invasive candidiasis |
References
- Arnold DT, Attwood M, Barratt S, Morley A, Elvers KT, McKernon J, et al. Predicting outcomes of COVID-19 from admission biomarkers: a prospective UK cohort study. Emerg Med J. 2021 Jul;38(7):543–8. [CrossRef]
- Gold JAW, Adjei S, Gundlapalli AV, Huang YLA, Chiller T, Benedict K, et al. Increased Hospitalizations Involving Fungal Infections during COVID-19 Pandemic, United States, January 2020–December 2021. Emerg Infect Dis [Internet]. 2023 Jul [cited 2025 May 14];29(7). Available from: https://wwwnc.cdc.gov/eid/article/29/7/22-1771_article.
- Mittal R, Chourasia N, Bharti VK, Singh S, Sarkar P, Agrawal A, et al. Blood-based biomarkers for diagnosis, prognosis, and severity prediction of COVID-19: Opportunities and challenges. Journal of Family Medicine and Primary Care. 2022 Aug;11(8):4330–41.
- Giacobbe DR, Esteves P, Bruzzi P, Mikulska M, Furfaro E, Mesini A, et al. Initial serum (1,3)-β-d-glucan as a predictor of mortality in proven candidaemia: findings from a retrospective study in two teaching hospitals in Italy and Brazil. Clinical Microbiology and Infection. 2015 Oct;21(10):954.e9-954.e17. [CrossRef]
- Singh RP, Bhardwaj A. β-glucans: a potential source for maintaining gut microbiota and the immune system. Front Nutr. 2023 May 5;10:1143682. [CrossRef]
- Yamamoto T, Oishi K, Suizu J, Murakawa K, Hisamoto Y, Fujii T, et al. False-positive Elevation of Beta-D-glucan and Aspergillus Galactomannan Levels Due to Mendelson’s Syndrome after Rice Aspiration. Intern Med. 2022 Oct 1;61(19):2935–9.
- Carelli S, Posteraro B, Torelli R, De Carolis E, Vallecoccia MS, Xhemalaj R, et al. Prognostic value of serial (1,3)-β-d-glucan measurements in ICU patients with invasive candidiasis. Crit Care. 2024 Jul 12;28(1):236.
- Hardison SE, Brown GD. C-type lectin receptors orchestrate antifungal immunity. Nat Immunol. 2012 Sep;13(9):817–22.
- White PL, Posso R, Parr C, Price JS, Finkelman M, Barnes RA. The Presence of (1→3)-β-D-Glucan as Prognostic Marker in Patients After Major Abdominal Surgery. Clinical Infectious Diseases. 2021 Oct 5;73(7):e1415–22. [CrossRef]
- White L, Dhillon R, Cordey A, Hughes H, Faggian F, Soni S, et al. A National Strategy to Diagnose COVID-19 Associated Invasive Fungal Disease in the ICU. SSRN Journal [Internet]. 2020 [cited 2025 May 14]; Available from: https://www.ssrn.com/abstract=3644400.
- Koehler P, Bassetti M, Chakrabarti A, Chen SCA, Colombo AL, Hoenigl M, et al. Defining and managing COVID-19-associated pulmonary aspergillosis: the 2020 ECMM/ISHAM consensus criteria for research and clinical guidance. The Lancet Infectious Diseases. 2021 Jun;21(6):e149–62.
- Donnelly JP, Chen SC, Kauffman CA, Steinbach WJ, Baddley JW, Verweij PE, et al. Revision and Update of the Consensus Definitions of Invasive Fungal Disease From the European Organization for Research and Treatment of Cancer and the Mycoses Study Group Education and Research Consortium. Clinical Infectious Diseases. 2020 Sep 12;71(6):1367–76.
- Carolis ED, Marchionni F, Torelli R, Posteraro P, Pascale GD, Carelli S, et al. Comparable Serum and Plasma 1,3--D-Glucan Values Obtained Using the Wako -Glucan Test in Patients with Probable or Proven Fungal Diseases. 2019;57(5).
- De Pascale G, Posteraro B, D’Arrigo S, Spinazzola G, Gaspari R, Bello G, et al. (1,3)-β-d-Glucan-based empirical antifungal interruption in suspected invasive candidiasis: a randomized trial. Crit Care. 2020 Dec;24(1):550.
- De Pascale G, Tumbarello M. Fungal infections in the ICU: advances in treatment and diagnosis. Current Opinion in Critical Care. 2015 Oct;21(5):421–9.
- Amornphimoltham P, Yuen PST, Star RA, Leelahavanichkul A. Gut Leakage of Fungal-Derived Inflammatory Mediators: Part of a Gut-Liver-Kidney Axis in Bacterial Sepsis. Digestive Diseases and Sciences. 2019 Sep 1;64(9):2416–28.
- Giacobbe DR, Esteves P, Bruzzi P, Mikulska M, Furfaro E, Mesini A, et al. Initial serum (1,3)-β-d-glucan as a predictor of mortality in proven candidaemia: findings from a retrospective study in two teaching hospitals in Italy and Brazil. Clinical Microbiology and Infection. 2015 Oct;21(10):954.e9-954.e17.
- Carbonell R, Urgelés S, Rodríguez A, Bodí M, Martín-Loeches I, Solé-Violán J, et al. Mortality comparison between the first and second/third waves among 3,795 critical COVID-19 patients with pneumonia admitted to the ICU: A multicentre retrospective cohort study. The Lancet Regional Health - Europe. 2021 Dec;11:100243.
- Bakakos A, Koukaki E, Ampelioti S, Ioannidou I, Papaioannou AI, Loverdos K, et al. The Real Impact of Age on Mortality in Critically Ill COVID-19 Patients. JPM. 2023 May 29;13(6):908.
- Giron LB, Peluso MJ, Ding J, Kenny G, Zilberstein NF, Koshy J et al. Markers of fungal translocation are elevated during post-acute sequelae of SARS-CoV-2 and induce NF-κB signaling. JCI Insight. 2022 Aug 8;7(15):e160989. [CrossRef]
- Fasano, A. Zonulin and Its Regulation of Intestinal Barrier Function: The Biological Door to Inflammation, Autoimmunity, and Cancer. Physiological Reviews. 2011 Jan;91(1):151–75.
- Kitsios GD, Kotok D, Yang H, Finkelman MA, Zhang Y, Britton N, et al. Plasma 1,3-β-d-glucan levels predict adverse clinical outcomes in critical illness. JCI Insight. 2021 Jul 22;6(14):e141277.
- Hurt W, Youngs J, Ball J, Edgeworth J, Hopkins P, Jenkins DR, et al. COVID-19-associated pulmonary aspergillosis in mechanically ventilated patients: a prospective, multicentre UK study. Thorax. 2024 Jan;79(1):75–82.
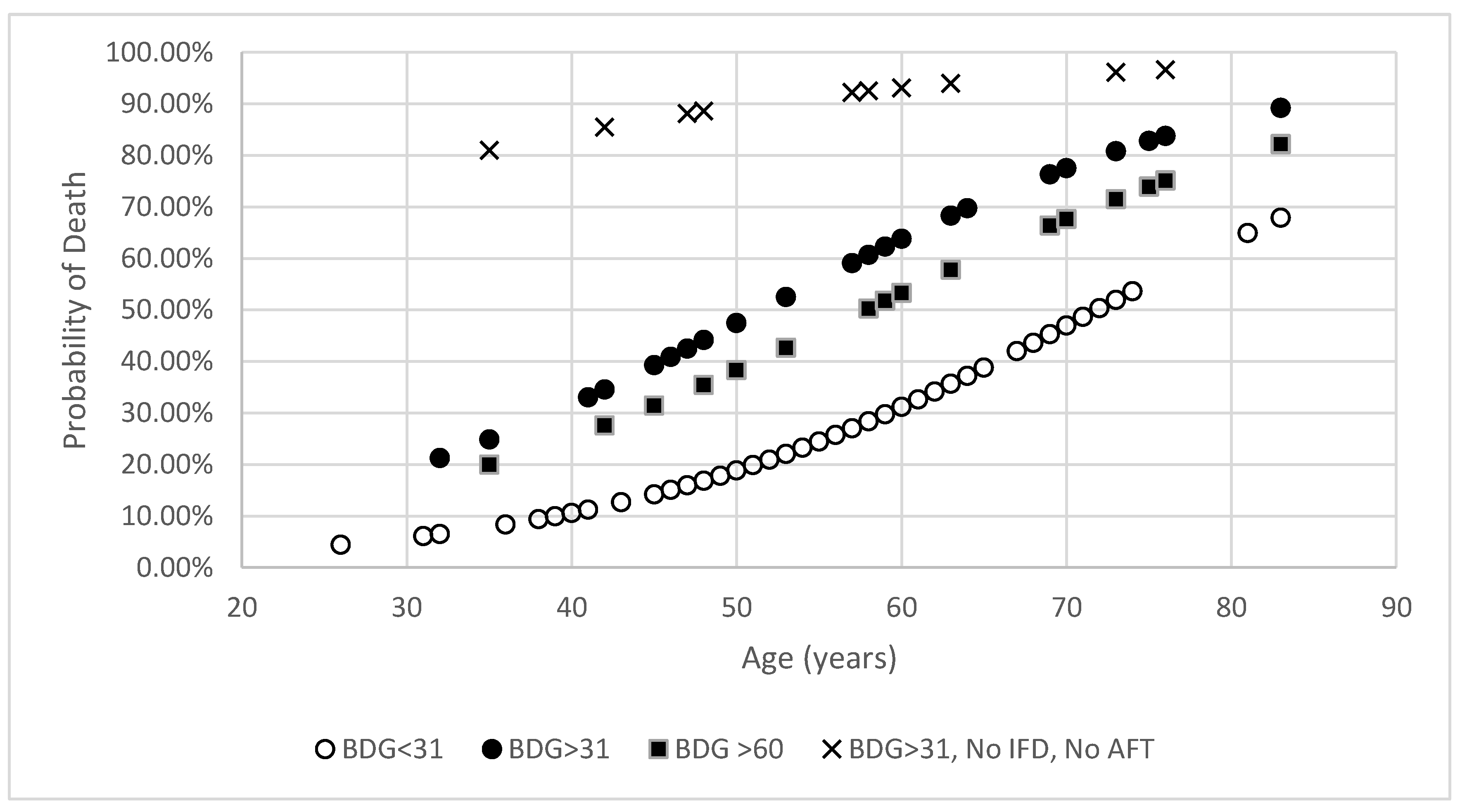
| Classification | Mortality rate (n/N, (%)) | |||
|---|---|---|---|---|
| BDG concentration | Difference in Mortality (95% CI) | Significance (P value) |
||
| ≤31 pg/mL | >31 pg/mL | |||
| Overall | 26/89 (29%) | 21/36 (58%) | 29% (10.0 to 45.9) | 0.0039 |
| AFT | 7/19 (37%) | 9/23 (39%) | 2% (29.1 to -25.6) | 1.0000 |
| No AFT | 19/70 (27%) | 12/13 (92%) | 65% (37.1 to 76.2) | <0.0001 |
| IFD | 4/9 (44%) | 7/17 (41%) | 3% (31.0 to -38.2) | 1.0000 |
| No IFD | 22/80 (28%) | 14/19 (74%) | 46% (21.3 to 63.0) | 0.0003 |
| IFD with AFT | 4/8 (50%) | 5/15 (33%) | 17% (21.2 to -50.4) | 0.6570 |
| IFD without AFT | 0/1 (0%) | 2/2 (100%) | 100% (30.5 to -100) | 0.3333 |
| No IFD with AFT | 3/11 (27%) | 4/8 (50%) | 23% (18.1 to -56.2) | 0.3765 |
| No IFD without AFT | 19/69 (28%) | 10/11 (91%) | 63% (32.5 to 75.2) | 0.0001 |
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2025 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (http://creativecommons.org/licenses/by/4.0/).





