The challenges observed in DTP3 vaccination coverage in Asia resonate with broader global issues, particularly those faced by African immunization programs, which are also striving to meet the 2030 Global Immunization Goals. In 2021, there were 25 million under-vaccinated children, of whom 18 million were zero-dose children[
28]. Despite progress, significant challenges persist, with 8.4% zero immunization coverage in the WHO African Region as of 2022 and approximately 67 million children in Africa missing routine vaccinations between 2019 and 2021. Key barriers in low- and middle-income countries are limited parental education, religious beliefs, inadequate healthcare systems, and vaccine hesitancy. Addressing these systemic issues often requires similar community-driven approaches, strengthening supply chains, and expanding financial resources, reflecting a shared global imperative for equitable access to vaccines.[
1]
4.1. Synthesis of Asian Trends
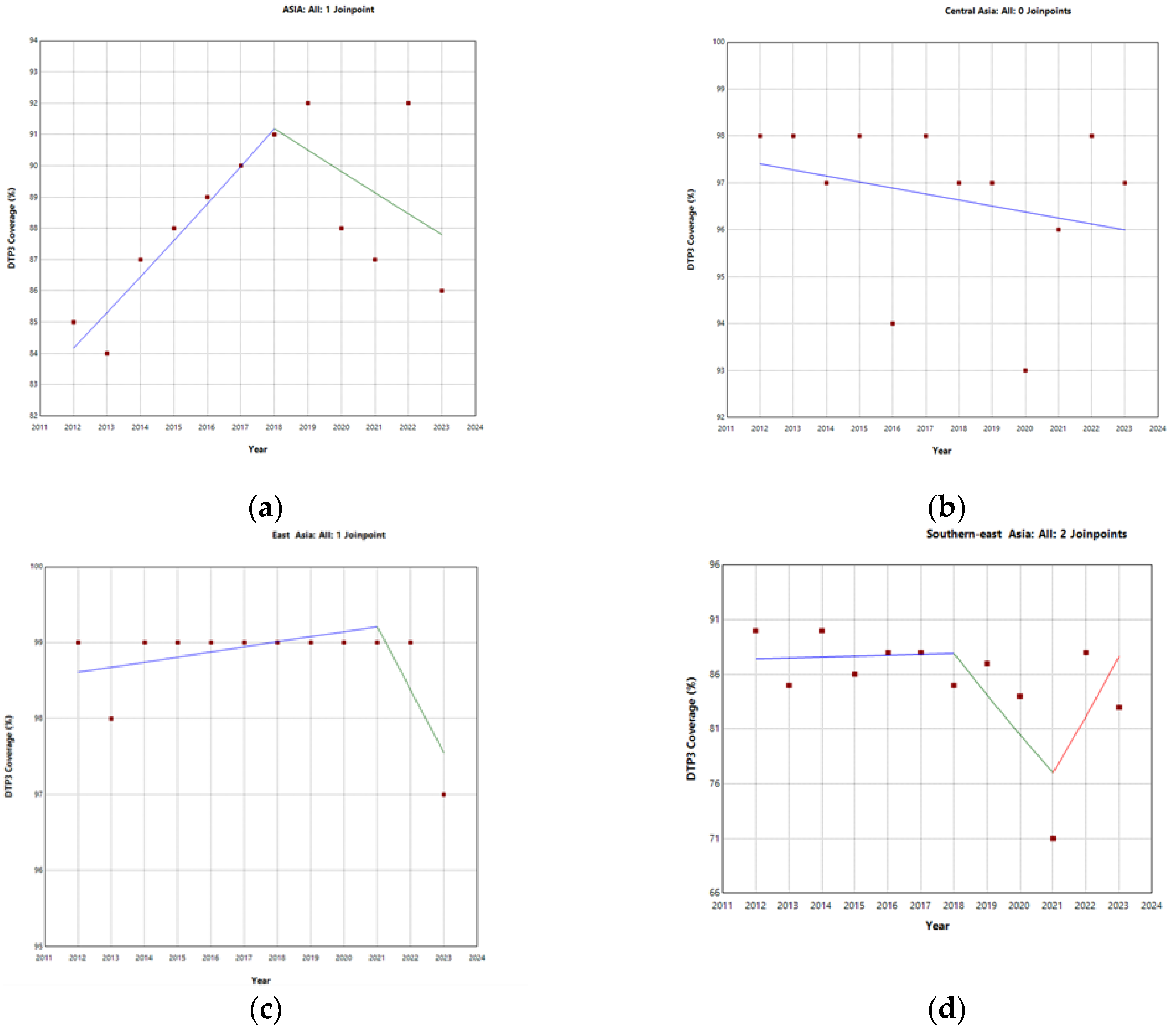
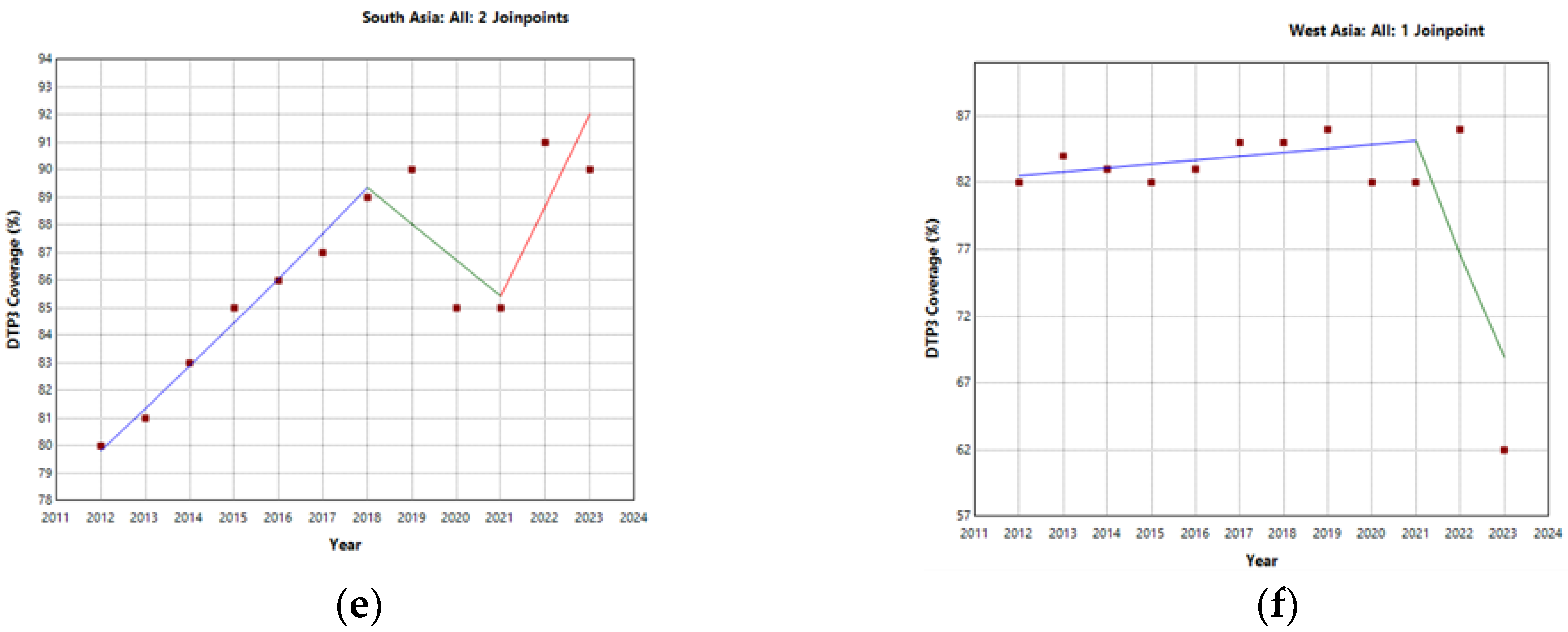
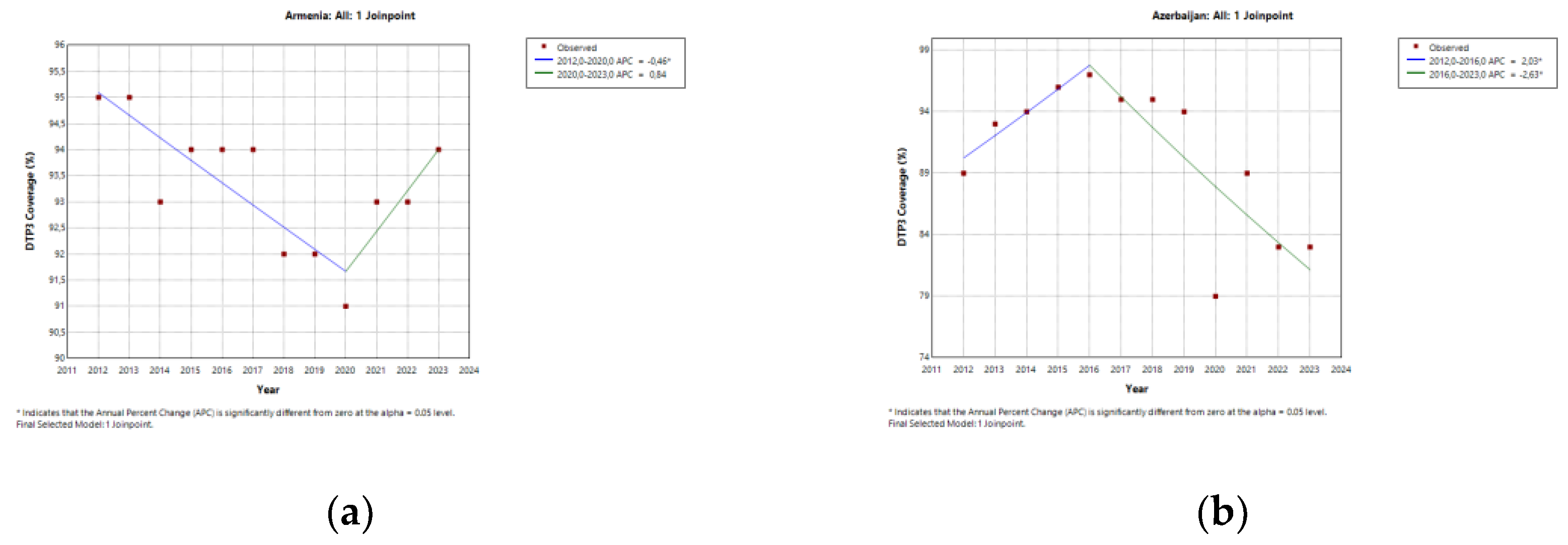
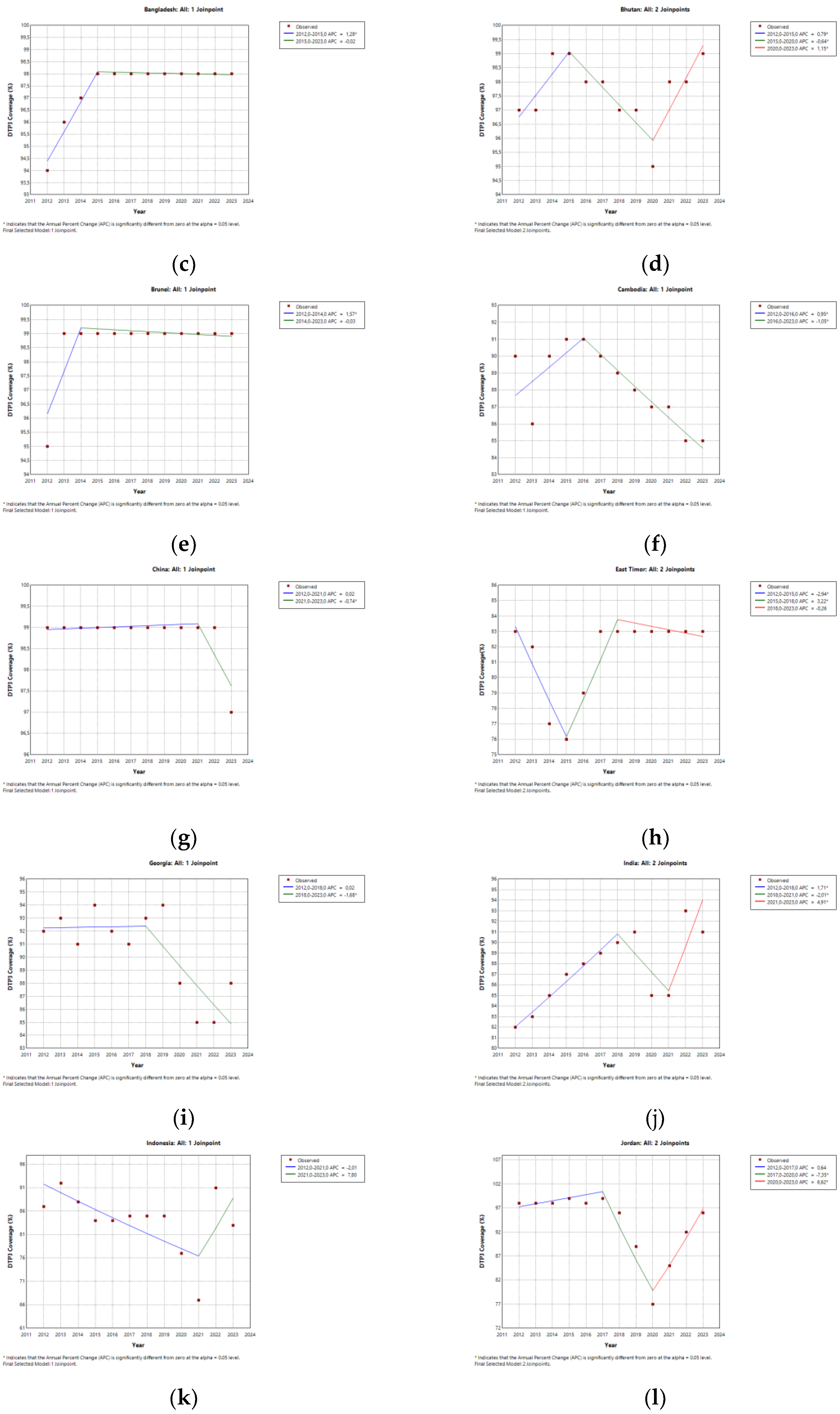
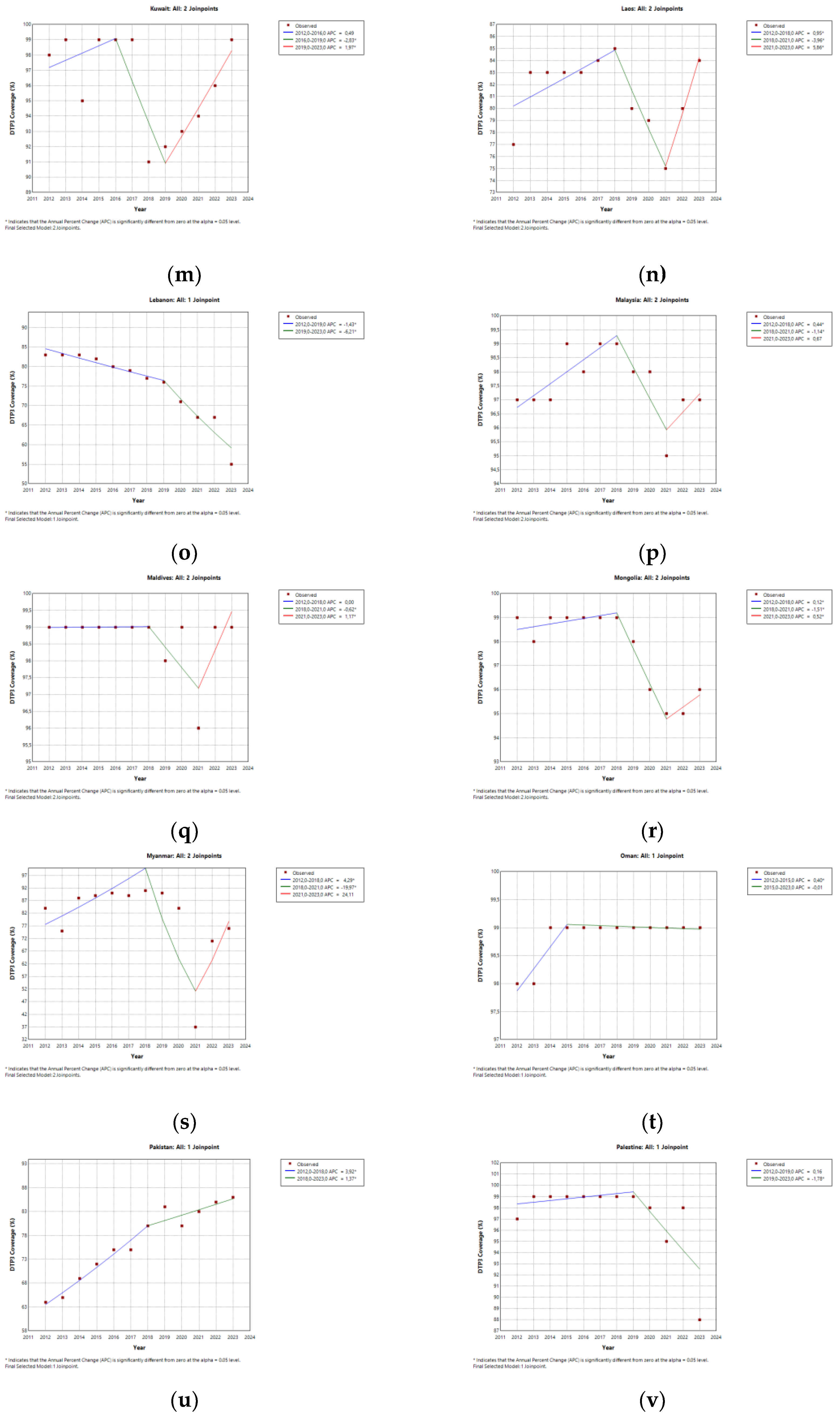
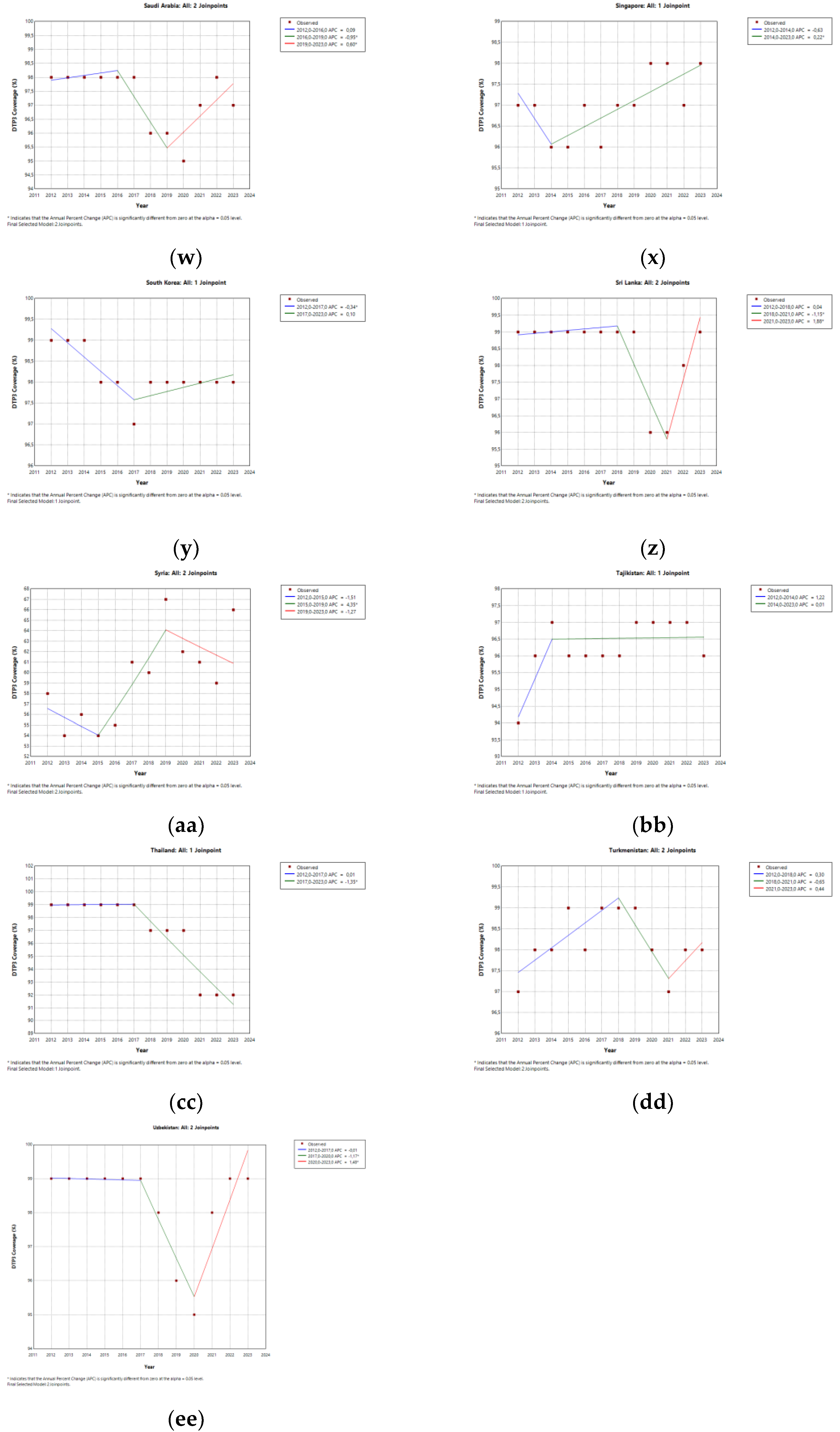
This study analyzed trends in DTP3 vaccination coverage across Asian countries and regions between 2012 and 2023 using Joinpoint regression. The main finding is that significant changes in vaccination trends were observed in multiple countries and regions during the period overlapping with the COVID-19 pandemic. At the continental level, a joinpoint was estimated in 2018, and several regional joinpoints were identified in 2019, 2020, or 2021, with confidence intervals overlapping the pandemic years.
Notably, Southeast Asia and South Asia showed declines in coverage, followed by signs of partial recovery, while other regions, such as Central Asia, showed no significant joinpoints. At the country level, several nations—including India, Malaysia, Indonesia, and Myanmar— exhibited joinpoints that coincided with the pandemic period, which may reflect disruptions in routine immunization services that temporally coincided with the pandemic.
Notably, some countries showed no significant joinpoints but displayed consistent upward or downward trends throughout the study period. For example, Iraq and Israel showed stable or improving coverage, while Afghanistan and Yemen experienced persistent declines.
To fully contextualize DTP3 coverage patterns, it is essential to distinguish between zero-dose children—those who have not received even the first dose of DTP—and children who begin but do not complete the series (i.e., drop-outs)[
29]. While zero-dose status highlights complete exclusion from the immunization system, DTP3 drop-off reflects system attrition, where access or engagement breaks down after initiation. Several countries in our dataset exhibited both phenomena: high zero-dose prevalence and substantial gaps between DTP1 and DTP3 vaccination coverage. This dual burden shows the need for tailored strategies, including outreach and demand generation for zero-dose populations, as well as continuity-focused interventions (e.g., follow-up mechanisms, trust-building, and service accessibility) to address drop-out. Future analyses should explore the proportion of DTP3 under-vaccinated children who are truly zero-dose versus drop-outs, to refine targeting and improve immunization system performance.
Our findings are further contextualized by recent global analyses, which highlight the multifaceted nature of vaccination inequalities. There has been a global increase in socioeconomic-related between-country inequalities in vaccination coverage during the initial years of the COVID-19 pandemic, followed by a recovery in 2022 [
30]. Countries with lower income or education levels were more likely to exhibit higher vaccine confidence, a trend that contrasts with within-country inequalities in high-income settings, suggesting that while external disruptions, such as pandemics, significantly impact coverage disparities, underlying socioeconomic factors and varying levels of vaccine confidence play complex and sometimes counterintuitive roles in shaping immunization landscapes across different regions[
30]. Although the SARS-CoV-2 pandemic caused global disruptions in immunization delivery, its impact was particularly severe in fragile settings already grappling with conflict or recovery, where baseline immunization deficits were exacerbated. For example, in Hadeetha, Anbar, Iraq, a region recovering from ISIS occupation, the pandemic shutdowns further compounded the challenge of returning to regular immunization services. There, 46.2% of children were missing their DTP3 vaccine doses due to pandemic-related disruptions, indicating a dual burden of conflict and health crises on vaccination completion[
31].
Our findings on DTP3 vaccination coverage align with qualitative studies that highlight persistent, localized barriers, particularly in rural and remote areas, which often stem from insufficient information, sociocultural limitations, and access challenges, as observed in Sindh, Pakistan [
32]. The concept of ‘zero-dose’ children, defined as those who have not received any DPT-containing vaccine [
33], serves as a critical indicator of access to routine immunization and is strongly associated with elevated risks of mortality, morbidity, and poorer human development throughout the life course. An analysis of 81 LMIC (low and middle-income countries) representing an estimated 21 million children revealed a prevalence of 12% zero-dose children between 2014 and 2023. [
33] Although an APC of 0.7% was observed, significant disparities persist across regions and countries, underscoring the ongoing challenge to achieve the Immunization Agenda 2030 targets. Beyond the established challenges of access and infrastructure, our understanding of ‘zero-dose’ children and incomplete vaccination schedules must also consider less-explored demographic and social factors, such as the significant association between unintended pregnancies and children not receiving their initial DPT vaccine doses.[
34] Beyond national policies and broader social determinants, localized studies, such as one conducted in a South Indian tertiary care hospital, reveal the nuanced interplay of socioeconomic factors, healthcare access points, and gender disparities in shaping childhood immunization utilization, even for mandatory vaccines [
35].
4.2. Interpretation of the Trends
Worldwide, the COVID-19 pandemic had a greater impact on vaccination coverage in 2021 than in 2020.[
36].Southeast Asia experienced significant reductions in DTP3 coverage during the COVID-19 pandemic, with observed rates consistently lower than predicted in both 2020 and 2021.[
36]. The decline in DTP3 coverage in Asia may reflect a broader global trend, indicating a vulnerability to multi-dose vaccine completion during health system crises.[
36] In particular, DTP3 coverage in 2021 showed a statistically significant drop of nearly three percentage points below expected levels, underscoring a sustained and worsening disruption across the region[
36]. Lower-than-expected DTP3 uptake across Southeast Asia may be attributed to a combination of healthcare facility closures, supply chain disruptions, and parental concerns about COVID-19 exposure, as identified in global analyses.[
36]
In regions such as South Asia, where DTP3 coverage has declined or struggled to recover, a deeper understanding of community-level barriers is crucial. A qualitative exploration in Sindh, Pakistan, identified several unexamined barriers from the perspective of community leaders, including an unsustainable communication system heavily reliant on polio mobile teams, discourteous healthcare personnel, cultural restrictions on women’s mobility, economic hardships, limited transportation, and security concerns[
32]. These findings demonstrate how local contexts, beyond national policies, significantly hinder routine immunization efforts and can contribute to the observed DTP3 coverage pattern.
The persistence of ‘zero-dose’ children, defined as those who have not received any DPT vaccine by 12 months of age, poses a significant challenge to global immunization agendas, such as IA 2030 and Gavi’s 5.0 strategy. However, in many settings, dropout between DTP1 and DTP3 also contributes significantly to underimmunization, particularly during periods of service disruption. Our analysis of DTP3 coverage trends reveals ongoing disparities, and one previously under-examined factor contributing to this burden is unintended pregnancy. Children born from unintended pregnancies consistently show a higher prevalence of zero-dose DPT vaccination, with adjusted odds 1.21 times higher compared to children from intended births. This novel finding underscores how a mother’s reproductive planning directly impacts a child’s likelihood of entering the immunization system, influencing overall population immunity and highlighting a critical area for targeted interventions[
34]
The observed trends in DTP3 coverage in Asia, including periods of decline and partial recovery, are further elucidated by regional studies on overall childhood immunization. For instance, a 5-year study conducted in a South Indian tertiary care hospital (2018-2022) revealed an overall 26.12% decline in vaccine utilization by 2022 compared to 2018, with a significant drop (53.01% of vaccinees and 25.72% of vaccine doses) in 2020, coinciding with the COVID-19 pandemic [
35]. While the use of mandatory vaccines generally rebounded, trends for optional vaccines exhibited mixed results, often shaped by their incorporation into national programs (such as the Rota and PCV vaccines) or by parents’ willingness to pay for additional immunity (like the MMR vaccine). These mixed results demonstrate the impact of global events, national policies, and local healthcare dynamics on immunization patterns. Therefore, the decline in overall vaccine uptake can be attributed to multiple factors rather than a single cause.
4.3. Asian Countries: Country-Specific Insights
Vaccines have contributed to reducing child mortality across Asia. Between 1990 and 2019, countries such as India, China, Ethiopia, Pakistan, and Bangladesh saw the largest absolute reductions in under-five mortality, primarily due to the widespread introduction of vaccines against diphtheria-tetanus-pertussis (DTP), measles, rotavirus, and Haemophilus influenzae type b [
37] In the South Asia Region, several countries—including Pakistan, Afghanistan, Iraq, Jordan, Syria, and Yemen—experienced significant disruptions in DTP3 coverage during the early phase of the COVID-19 pandemic in 2020. While countries such as Pakistan and Iraq demonstrated recovery by 2021, offsetting the setbacks of 2020, others like Afghanistan, Syria, and Jordan faced continued declines through both 2020 and 2021 [
38].
Within Southeast Asia, disparities in maternal and child health (MCH) services, including immunization coverage, persist as a significant challenge. An analysis of ASEAN member states highlights Thailand and Vietnam as regional models, with high MCH service coverage and substantial equity across populations. In contrast, countries such as Lao PDR and Timor-Leste face significant inequities, marked by low overall coverage and pronounced disparities across urban-rural divides, socioeconomic strata, and subnational regions. Myanmar and the Philippines also report low coverage levels, with structural inequities such as a pronounced pro-urban bias in Myanmar and worsening regional disparities in the Philippines. It is necessary to have targeted policies and investments tailored to each country’s unique challenges, leveraging successful regional experiences to bridge gaps and accelerate progress toward universal health coverage [
39,
40].
Immunization coverage, particularly for DTP3, has declined in parts of Asia—most notably in Southeast Asia—where the proportion of children with zero doses reached as high as 24% in 2020 [
41]. This decline is partly driven by vaccine hesitancy, fueled by misinformation and anti-vaccination content on social media platforms (SMPs). Reliance on SMPs for vaccine-related information is associated with increased fear of vaccines and a three-to-four-fold higher likelihood of delayed immunization among caregivers. Vaccine hesitancy and negative attitudes toward COVID-19 vaccines are prevalent in many Asian countries, with rates ranging from 20% to 55%. Particularly high levels of hesitancy have been reported in countries such as Jordan, Kuwait, and Russia. Similar concerns have also been documented for non-COVID-19 vaccines in Saudi Arabia, Israel, South India, Pakistan, China, Japan, Mongolia, and Korea [
41].
4.3.1. Afghanistan
Afghanistan experienced a challenging period, with the number of zero-dose children more than doubling throughout 2021, indicating a worsening of immunization performance in several districts.[
38].
4.3.2. Bangladesh
Bangladesh is actively engaged in initiatives aimed at better understanding and reaching zero-dose children, those who have not received their first diphtheria-tetanus-pertussis (DTP1)-containing vaccine. As a participant in the Zero-Dose Learning Hub (ZDLH) initiative, Bangladesh is exploring flexible age cohorts for targeted immunization surveys at the local level[
42]. to generate more timely and relevant insights into immunization timeliness and the factors affecting vaccine uptake in systematically missed communities, complementing global tracking efforts.. [
40]. Despite these efforts, some studies highlight persistent inequalities in coverage based on household characteristics and geographical location. Bangladesh also experienced significant absolute reductions in under-5 deaths associated with DTP, measles, rotavirus, and Hib vaccines between 1990 and 2019.[
40]
4.3.3. Cambodia
Cambodia has improved DTP3 coverage from 66% in 2000 to over 90% by 2014. [
43] National data show that children living in rural areas, from low-income households, or with mothers who have limited education are significantly more likely to miss the third DTP dose. Low birth weight and inadequate prenatal care are also risk factors for incomplete DTP3 immunization.[
44]
4.3.4. China
China has achieved 98% coverage for routine vaccines through its National Immunization Program (NIP) [
45,
46]. The first dose of DTaP coverage was exceptionally high in 2019, with a national median of 99.55% [
47]. However, significant disparities exist in completion rates. Dropout rates between the first and third doses of DTaP (DTaP1–DTaP3) ranged from 0.36% to 28.66% across provinces, with the highest levels recorded in Gansu (28.66%) and Guizhou (17.19%) [
45]. At the county level, disparities reached up to 39.22%, particularly in western provinces such as Gansu, Qinghai, and Guizhou. These intra-provincial differences were associated with lower overall DTaP3 coverage. [
45].
One documented contributor to incomplete immunization is the refusal by community health centers to vaccinate children with underlying conditions, such as cardiovascular disease, due to safety concerns. This has led to delays in DTP vaccination for this vulnerable group [
46].
Despite high overall national coverage, rural areas, particularly in Southwest China, face challenges with timely and complete immunization. While coverage for each vaccine dose remained above 90% during the COVID-19 pandemic, the rate of timely DTP3 vaccination dropped as low as 43.86% in some counties [
11]. Timely and complete coverage for multi-dose vaccines was often below 70%.
The COVID-19 pandemic impacted routine immunization services in China, particularly the timeliness of multi-dose vaccines, such as DTP3. Nevertheless, China’s immunization system demonstrated resilience. A large cohort study in Beijing reported an initial decline in timely DTP3 coverage during the pandemic’s early phase, followed by a rapid recovery that ultimately surpassed the 90% WHO target [
12].
While China’s public health infrastructure has ensured high overall coverage, vaccine hesitancy and access barriers persist for specific subpopulations. Parental concerns, amplified by safety rumors, have led some to delay or forego vaccinating children with chronic illnesses. [
46,
47]
There is a demand for more comprehensive immunization options. Surveys indicate a parental willingness to pay for hexavalent vaccines not included in the NIP [
48]. Understanding the drivers behind this demand could inform policy decisions on expanding the national immunization schedule.
Rising Pertussis and Policy Implications
Despite high and stable DTP3 coverage (consistently above 97%), China has witnessed a resurgence in pertussis. A 20-year ecological study in Chongqing documented a 283-fold increase in pertussis incidence between 2005 and 2024 [
48] This rise coincided with a national shift from whole-cell to acellular vaccines, which was associated with a 23.54-fold increase in reported cases. Additionally, the introduction of enhanced molecular diagnostics in 2023 led to an 82.65-fold increase in case detection. [
48].
Notably, school-aged children (6–7 years) emerged as key transmission nodes, exhibiting the highest relative risk among non-infant groups. These findings suggest that high coverage alone is insufficient to control pertussis, highlighting the need for booster dose strategies targeting older children. Furthermore, they underscore the importance of monitoring vaccine effectiveness over time and revisiting vaccine type selection as part of long-term immunization policy [
48].
4.3.5. India
In a similar way to the African continent, India faces a complex set of barriers contributing to zero-dose and under-vaccinated children. These include socioeconomic disparities, geographic access limitations, and sociocultural factors[
1].
India has made significant progress in its immunization efforts over the past two decades, reducing the prevalence of children who have not received any vaccinations, which declined from 33.4% in 1992 to 6.6% in 2021. Over this period, inter-state disparities also narrowed significantly, with the interquartile range decreasing from 30.1% in 1993 to 3.1%in 2021. In 2021, the highest zero-dose prevalence was recorded in Meghalaya (17.0%), while the lowest was in Kerala (0.1%)[
49].
This progress was exceptionally rapid between 2005–06 and 2015–16, coinciding with major health system reforms such as the National Rural Health Mission. Despite these gains, an estimated 2.88 million children remained zero-dose in 2016. These children were disproportionately from rural areas, the lowest wealth quintiles, and households with uneducated mothers. Notably, while many disparities narrowed, zero-dose prevalence among Muslim children showed slight improvement. Zero-dose children also had significantly higher rates of malnutrition, stunting, underweight, and wasting, indicating a cumulative disadvantage across multiple dimensions of child health. The geographic distribution was uneven in urban areas, particularly among migrant and informal sector populations.[
50].
Nationally, coverage of core vaccines such as DTP, BCG, polio, and MCV was found to be high in a survey conducted between 2019 and 2021, with DTP coverage ranging from 42% (for rotavirus) to 95% (for BCG) [
51]. A strong correlation was observed between district-level coverage estimates across different vaccines, with substantial spatial overlap in areas with low coverage. Integrated delivery strategies targeting full immunization coverage for core vaccines were projected to outperform single-vaccine approaches and could nearly double coverage of non-core vaccines such as rotavirus. These findings underscore the potential of integrated and geographically targeted strategies to accelerate progress toward full immunization and enhance the reach of broader child health interventions. [
51].
As a key contributor to the global zero-dose burden, India reported a 6.7% prevalence of children not receiving a DTP-containing vaccine in 2021, down from 25.1% in 2006. This represents an average annual decline of 1.2%, the fastest rate observed in South Asia, and reflects a broader trend among Low- and Middle-Income Countries (LMICs). The countries with higher initial burdens have made faster progress [
33].
However, given India’s large birth cohort, this translates into an estimated 3.056 million zero-dose children in 2021. A nationally representative survey further revealed that 9.14% of children from unintended pregnancies were zero-dose for DTP, compared to 6.69% among those from intended pregnancies. This suggests that unintended pregnancy is an important and often overlooked risk factor for incomplete immunization. [
34].
Zero-dose prevalence also varied widely across India, from 0.9% in Puducherry to 18.2% in Meghalaya. Thirteen states and Union Territories had rates above the national average of 6.8%. Additional risk factors included low wealth, maternal education, urban residence (in contrast to previous trends), and non-institutional deliveries. These findings show the need for integrated maternal and child health strategies that prioritize continuity of care. [
34]
Although DTP immunization coverage is high, India faces a significant gap in booster uptake. A study in Odisha found that only 60.68% of children aged six and above had received the second DTP booster dose, compared to approximately 90% for the primary series of vaccinations. Key barriers included parental misconceptions and procrastination. A single, clinic-based educational intervention significantly improved booster uptake, particularly in tribal areas, showing the value of culturally sensitive education and follow-up reminders. [
52].
In Mumbai, a study focused on zero-dose children among migrant and urban poor populations found that, despite hospital births and initial contact with the health system, follow-up vaccinations were often missed. This was due to limited parental awareness, operational challenges, and weak provider engagement, particularly in private facilities. These findings emphasize the need for targeted outreach and systemic improvements to prevent vaccine dropouts and support full immunization among the most vulnerable groups. [
53].
Despite ambitious national programs like EPI, UIP, and Mission Indradhanush, regional disparities persist. A five-year study (2018–2022) conducted at a tertiary hospital in South India, involving over 32,000 children, revealed a decline in vaccine utilization by 2022, with the sharpest drop occurring in 2020 due to the COVID-19 pandemic. While some recovery occurred for mandatory vaccines, optional vaccines—often paid out-of-pocket—displayed a marked male preference. Delayed or incomplete immunization was more common among females, older children, rural residents, and families with lower to middle incomes. These trends highlight persistent gender and socioeconomic inequalities in vaccine uptake, particularly for non-mandatory vaccines. .[
35]
An evaluation of the Intensified Mission Indradhanush (IMI) revealed that greater decision-making autonomy at the block and subcenter levels did not necessarily improve DTP3 coverage. Structural equation modeling indicated that broader local decision space, especially in community engagement, was paradoxically associated with fewer doses administered. This may reflect an inadequate infrastructure or competing responsibilities. Decentralization without adequate institutional support and accountability may undermine program effectiveness in complex settings such as India.[
54].
4.3.6. Indonesia
In Indonesia, coverage has increased in the last few decades, but there are still children who receive vaccinations at an inadequate age. The main factors influencing this are maternal education and maternal engagement with health services.[
55]
4.3.7. Irak
The case of Iraq provides a critical lens on the compounded challenges to childhood immunization in healthcare systems recovering from conflict while also navigating global health crises. A study conducted in Hadeetha, Anbar, a region affected by ISIS occupation, found that COVID-19-related shutdowns resulted in 46.2% of children missing their DTP3 vaccine doses. [
31] This shows that global disruptions exacerbate existing immunization gaps in fragile settings.
Unlike broader analyses that focus solely on pandemic-related disruptions or socioeconomic barriers, Iraq’s experience underscores the unique difficulties of sustaining immunization programs amid intermittent conflict. [
31]
Key predictors of incomplete DTP3 vaccination included the child’s age, the mother’s knowledge of the vaccination schedule, and the ongoing impact of regional conflict. Notably, vaccine availability was not reported as a primary barrier, and caregiver vaccine hesitancy was low. Instead, challenges were linked to systemic access issues and the reliance on mass vaccination campaigns.
Caregivers expressed openness to receiving phone reminders and television campaigns about vaccination schedules. Immunization strategies in conflict-recovery zones should prioritize consistent access to healthcare providers and leverage modern communication tools to address literacy gaps and improve schedule adherence.
Insights from mass COVID-19 vaccination efforts, such as retraining community health workers for door-to-door outreach and implementing electronic immunization registries, offer practical strategies to reinforce routine childhood immunization in complex, post-conflict environments.
4.3.8. Iran
According to a comparative cross-sectional study on SDG health indicators, Iran has achieved full DTP3 immunization coverage, outperforming both the global average and all WHO regional averages, highlighting the effectiveness of its national immunization efforts despite challenges in other mortality-related indicators.[
56].
4.3.9. Israel
Recent research in Israel has highlighted within-country disparities in DTP vaccination coverage, particularly among Ultra-Orthodox Jewish communities. A study conducted in Safed, a socioeconomically deprived city with a large underprivileged population, found significantly lower and delayed DTP vaccination coverage in underprivileged neighborhoods compared to non-underprivileged areas, as well as higher dropout rates between DTP1 and DTP4 [
57]. These disparities reflect vaccine hesitancy and structural and logistical barriers such as access limitations, large family sizes, and competing priorities. The narrowing of coverage gaps over time for certain vaccines (e.g., MMRV) but not for DTP points to vaccine-specific perceptions within the community, possibly linked to recent disease outbreaks.
4.3.10. Pakistan
Despite national improvements in childhood immunization coverage in Pakistan, disparities persist between urban and rural areas, particularly in remote and tribal regions such as Sindh. A qualitative study of community leaders in Shikarpur, Sindh, revealed numerous barriers to immunization [
32]. These included a fundamental lack of vaccine knowledge among the leaders themselves and fragmented, inconsistent information flows, often overly reliant on polio eradication campaign teams. Such findings illustrate how local contextual factors—beyond national policies—substantially hinder routine immunization efforts and help explain observed patterns in DTP3 coverage.
Between 2006 and 2018, research on Pakistan showed improvements in full vaccination coverage across three survey waves. However, persistent disparities were evident across provinces and wealth quintiles. Children in the poorest wealth quintile consistently had higher odds of under-vaccination, and provincial disparities widened over time. The provinces of Balochistan, Sindh, and Khyber Pakhtunkhwa showed a higher under-vaccination rate compared to Punjab [
58]. Sociocultural norms also play a critical role. Restrictions on women’s mobility, the disproportionate burden placed on mothers for ensuring vaccination, economic hardship, and limited transportation were identified as major impediments.
Tribal conflicts produce security concerns that restrict access to health facilities and impede outreach efforts by vaccinators. Community leaders proposed contextually tailored solutions, including structured community meetings for information dissemination, empathy-based training for healthcare workers, and subsidized, women-centered transportation services.
Subnational data further emphasize these issues. DTP3 coverage experienced major disruptions during the early phase of the COVID-19 pandemic in 2020. Although Pakistan demonstrated a recovery by 2021, reducing the number of zero-dose children, challenges remain. [
40].
Notably, DTP1 coverage dropped sharply in Q2 2020 but rebounded by Q4 of the same year, resulting in a substantial decrease in zero-dose children by Q4 2021. Pakistan and the Philippines, both of which offer vaccines during the second year of life, achieved increased coverage through catch-up campaigns using the pentavalent vaccine. [
38,
59]
The geographical distribution of unvaccinated children in Pakistan changed between 2020 and 2021. Ethnic disparities and household wealth are still associated with immunization coverage, and there are specific ethnic groups disproportionately affected.
4.3.11. Vietnam.
A seroepidemiological study conducted in 10 provinces of southern Vietnam between 2012 and 2016 found a high concentration, with more than 90% of tetanus antibodies in children under 4 years old. Differences among provinces were detected, which could be attributed to either coverage differences between provinces or variations in serum collection and conservation procedures [
60].
4.4. Global Context: Comparisons with Other Regions
This study is part of a broader research series assessing the impact of the COVID-19 pandemic on DTP3 vaccination coverage across different world regions.[
13,
14,
15] DTP3 trends in Asia align with findings from other continents, especially Africa, where DTP3 coverage declined from 77% in 2019 to 72% between 2021 and 2022, reflecting the global health challenges posed by the pandemic.
DTP3 trends in Asia during the pandemic are similar to those of Africa, where DTP3 coverage declined from 77% in 2019 to 72% between 2021 and 2022, reflecting the global health challenges posed by the pandemic. [
1].
Modifiable and non-modifiable factors contributing to low immunization rates in Africa—such as vaccine safety concerns, long waiting times, negative healthcare worker attitudes, and limited affordability—mirror the structural and attitudinal barriers identified in our Asian context. This cross-continental consistency suggests that many immunization challenges have a universal nature and that successful strategies, such as mobile clinics, door-to-door campaigns, improved coordination, and innovative financing, may be adaptable across diverse geographic settings. [
1].
In previous analyses of Africa, the Americas, and Europe, we identified a clear temporal alignment between the onset of the pandemic and significant disruptions in vaccination trends, often followed by only partial recoveries. In Africa, many countries experienced sharp and sustained declines in coverage [
13]. In the Americas, we observed considerable heterogeneity, with some countries maintaining stable coverage while others experienced dramatic declines [
14]. In Europe, although overall coverage remained relatively stable, several countries—such as Ireland, Poland, and Sweden—showed joinpoints temporally close to the pandemic, indicating modest but statistically significant shifts[
15]. Similarly, our analysis of Asia detected pandemic-associated disruptions, with joinpoints around 2020–2021 in most subregions. The internal diversity within Asia was also notable: while Southeast and West Asia experienced pronounced declines, other regions maintained relative stability. Beyond the challenge of addressing ‘zero-dose’ children (those who do not receive any DTP doses), ensuring completion of the immunization schedule, including booster doses, remains a critical public health concern. For example, a study in India reported that delays in administering the second DTP booster (the fifth dose) have contributed to the resurgence of vaccine-preventable diseases among older children. However, educational programs targeting parents have shown promise in accelerating vaccine uptake. [
52].
A multi-country analysis of 81 low- and middle-income countries (LMICs) reported an average annual decline of 0.7 percentage points in zero-dose DTP prevalence between 2005 and 2019, with South Asia exhibiting the fastest reduction at 1.1% per year [
33]. Recent improvements in South Asia, particularly in areas with initially high zero-dose rates, indicate a convergence trend toward more uniform vaccination coverage. Significantly, the strong association between zero-dose prevalence and child mortality—a 1.2 deaths per 1,000 live births increase for every one percentage point rise in zero-dose prevalence—highlights the far-reaching public health implications of vaccination gaps [
33].
Our findings resonate with broader challenges observed across LMICs, particularly the persistent inequities in immunization coverage. A systematic review with an equity impact analysis in Nigeria demonstrated that disparities in basic vaccination coverage are consistently associated with socioeconomic, geographic, maternal, child, and healthcare factors. Key determinants include household wealth, religion, ethnicity, maternal education, and age at childbirth, as well as access to antenatal care and facility-based delivery [
61]. Community-driven approaches and supply chain strengthening, which have proven successful in one region, offer adaptable solutions to similar systemic issues in other regions.
India’s longitudinal data further enriches our analysis. Between 1992 and 2016, India achieved a 23.3% absolute decline in zero-dose DTP prevalence, with reductions most pronounced among the most disadvantaged populations [
50]. The elimination of disparities by child sex and caste is particularly remarkable. However, zero-dose children are disproportionately concentrated in rural areas, lower wealth quintiles, and among mothers with limited education. Notably, gaps in coverage between Muslim and Hindu children have persisted, as has the association between zero-dose status and early childhood undernutrition. It is necessary to have comprehensive interventions addressing broader social, economic, and environmental determinants, as advocated by IA2030.[
50]
Moreover, a study covering 20 LMICs in Asia and Africa found that the COVID-19 pandemic worsened existing inequalities in immunization coverage, disproportionately affecting children from rural areas, low-income households, and those with less maternal education [
61] In India and Pakistan, service disruptions led to significant declines in DTP3 uptake, exacerbating equity gaps. Finally, our findings are further contextualized by studies from conflict-affected regions. For example, in Hadeetha, Iraq, the dual burden of ongoing conflict and pandemic-related service disruptions left many children unimmunized, especially those with caregivers lacking vaccine literacy. In Nasiriya, an area not directly affected by conflict, vaccination rates declined in different patterns during the pandemic. These cases illustrate how conflict can exacerbate the impact of global health crises, rendering already vulnerable populations even more susceptible to immunization gaps [
31].
4.5. Methodological Considerations
In previous studies from our series on DTP3 vaccination coverage in other continents, we applied both segmented regression and Joinpoint regression, consistently observing similar results regarding trend changes and their temporal alignment with the COVID-19 pandemic [
13,
14,
15]. Based on that experience, we chose to use only Joinpoint regression in the present analysis, as it offers a statistically robust and widely accepted method for detecting significant changes in temporal trends. Although we considered a chi-square test to compare DTP3 coverage between 2019 (pre-pandemic) and 2023, we ultimately excluded it, as the Joinpoint analysis already captures temporal changes, including those related to the pandemic, with greater analytical precision. This approach avoids redundancy while preserving clarity and methodological rigor. This study has several limitations that should be acknowledged. The World Bank/UNICEF estimates of DTP3 vaccination coverage are based on a combination of government-reported administrative data, household surveys, and statistical modeling. When estimates rely primarily on administrative reports, they may be subject to reporting bias[
36]. Additionally, in countries lacking updated data, estimates were extrapolated based on pre-pandemic trends, which may have led to an overestimation of coverage during the COVID-19 period. Notably, several countries for which extrapolated data were used—such as Bahrain, Brunei, and Iran, located in Asia—introduce potential uncertainty into regional trend analyses [
36].
Our analysis was conducted using national-level data. However, a shift toward subnational-level monitoring of immunization coverage is necessary. Annual national reports often obscure significant within-country disparities and fail to capture real-time performance, especially during crises [
38]. The surveillance of administrative data at the district or subdistrict level is crucial for identifying low-performing areas promptly, planning effective catch-up interventions, and tailoring strategies to address barriers and reach unvaccinated children throughout the year.
4.6. Implications for Policy and Practice
Considering recent trends and projections, particularly the ongoing challenges faced by low- and middle-income countries (LMICs) in achieving optimal age-appropriate vaccination coverage, several critical policy and practice implications emerge.
From a policy perspective, our findings align with recent analyses of vaccination trends across LMICs. While significant progress was made between 2000 and 2020, projections indicate that many countries will fall short of achieving the 2030 coverage goals. By 2030, only 5 out of 41 LMICs are expected to reach 90% coverage for DTP3 and none for MCV if current trends persist. Notably, urban-rural and socioeconomic disparities remain widespread, particularly in several African countries, where the poorest and rural populations continue to experience the largest gaps.
Although recent disruptions such as the COVID-19 pandemic did not significantly alter projected trends—due in part to resilient immunization programs and safer delivery protocols—sustained international and governmental advocacy remains essential. Challenges, including resource mobilization and concerns about infections, must be addressed to ensure the timely vaccination of children. There is a need for effective, equity-driven strategies to improve vaccine coverage in rural and underserved areas. Strengthening vaccine availability, enhancing community health worker (CHW) engagement, and implementing targeted policies to reduce disparities can improve child survival through better coverage and timeliness.
Cambodia offers a successful model, where catch-up campaigns for missed vaccinations, supported by community mobilization and expanded health services, helped overcome accessibility barriers.
Although recent disruptions such as the COVID-19 pandemic did not significantly alter projected trends—due in part to resilient immunization programs and safer delivery protocols—sustained international and governmental advocacy remains essential. Challenges, including resource mobilization and concerns about infections, must be addressed to ensure the timely vaccination of children.
Differences in DTP3 coverage recovery across Asian countries reflect variations in systemic resilience, baseline health infrastructure, and policy responses. Regulatory complexities around high-valent diphtheria-tetanus-pertussis combination vaccines (DTPCVs) further affect uptake. Diverse national licensing and regulatory requirements hinder the broader adoption of these efficient vaccine formulations. Accelerating regulatory convergence and harmonizing approval processes could improve access and uptake [
62].
Integrated vaccine delivery and geographic targeting—such as those demonstrated in India with DTP—can drive progress toward full immunization and broader child health interventions [
51]. Addressing disparities in DTP3 booster dose coverage and causes of non-compliance requires holistic and targeted strategies [
52]
A compelling link exists between unintended pregnancies and higher zero-dose DTP rates. Addressing unmet needs for family planning and integrating family planning services with immunization visits—particularly during postnatal care—can foster continuity of care.
This integrated approach promotes ongoing healthcare engagement, reduces missed vaccination opportunities, and improves both maternal and child health outcomes.[
34]
Experiences from conflict-affected regions, such as Hadeetha, Iraq, reveal that caregiver awareness and time constraints, not vaccine hesitancy, were significant barriers to immunization [
31]. Interventions should prioritize accessible healthcare providers and deploy technology, including cellphone reminders and mass media campaigns, to provide timely information. Lessons from COVID-19 mass vaccination efforts, such as retraining community health workers for home visits and implementing electronic immunization registries, can be adapted to strengthen routine immunization in fragile contexts. [
31].
In South India, gender (female), older age, rural residence, and lower socioeconomic status significantly predicted incomplete vaccination [
35]. Male children have a higher rate of optional vaccinations, which warrants targeted policies. Enhanced catch-up, public awareness, and educational campaigns may help promote equitable vaccine access, thereby reducing financial and social barriers. Health information interventions have shown persistent positive effects on vaccination uptake. In Uttar Pradesh, India, such interventions sustained improvements over 30 months without displacing vaccinations that would have occurred otherwise [
63]. These results affirm the long-term value of demand-side strategies.
Furthermore, treatment effects varied: children who were older and had prior DTP doses responded more strongly. This suggests targeted engagement with families of children in specific age groups through repeated outreach. Since improved maternal knowledge appears to be a key mechanism, leveraging low-cost delivery platforms—such as community health workers and digital tools—can amplify reach and impact.
High acceptance and willingness to pay for hexavalent vaccines among Chinese parents, even for non-EPI vaccines, suggest a strong demand [
64]. Acceptance could further increase with government coverage, insurance reimbursement, or price reductions. Economic analyses in Korea suggest that hexavalent vaccines may be cost-effective by reducing the number of administration visits and improving adherence. [
65] . In Malaysia, rural, low-income families valued the vaccine’s ability to reduce transportation costs [
66].
The incorporation into insurance schemes, reducing out-of-pocket costs, and addressing perceived financial barriers (primarily through parental education) could substantially improve vaccine uptake. Social media are becoming a growing health communication channel in Asia, and they could be used to combat misinformation and promote accurate vaccine information[
67]
Evidence from a Phase IV randomized controlled trial in China supports the co-administration of sIPV, DTaP, and MMR at 18 months as both safe and immunogenic. This offers a practical strategy for delivering missed DTP3 doses during scheduled MMR visits [
68].. Community and stakeholder involvement, as demonstrated in several African programs, remains vital to program success [
69].
We propose three key, actionable strategies for LMICs aiming to reduce zero-dose prevalence and improve DTP3 completion:
Community-Based Outreach: Deploy mobile vaccination teams and employ door-to-door strategies to reach children who are zero-dose, particularly in underserved rural and urban communities with low socioeconomic status.
Continuity of Care Mechanisms: Strengthen follow-up systems after initial immunization contact through electronic registries, SMS reminders, and integrated service delivery to reduce dropouts between DTP1 and DTP3.
Equity-Driven Targeting: Use disaggregated subnational data to identify the most disadvantaged populations. Tailor interventions to address local barriers linked to poverty, geography, gender, and cultural norms.
These strategies align with the Immunization Agenda 2030 and provide a scalable, evidence-based framework for post-pandemic recovery and long-term resilience in immunization systems.