Submitted:
02 July 2025
Posted:
03 July 2025
You are already at the latest version
Abstract
Keywords:
Introduction
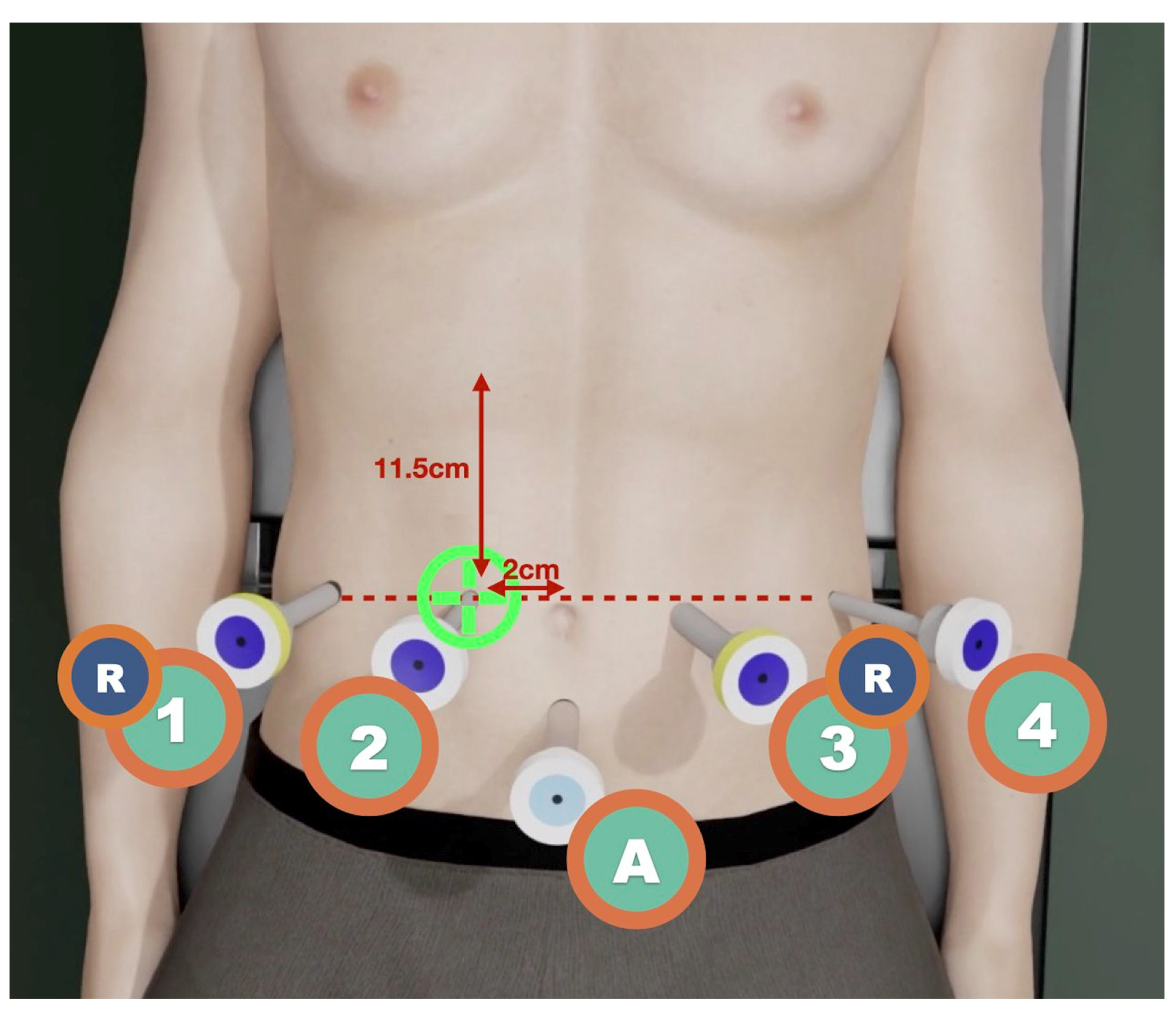
Stepwise Dissection Approach
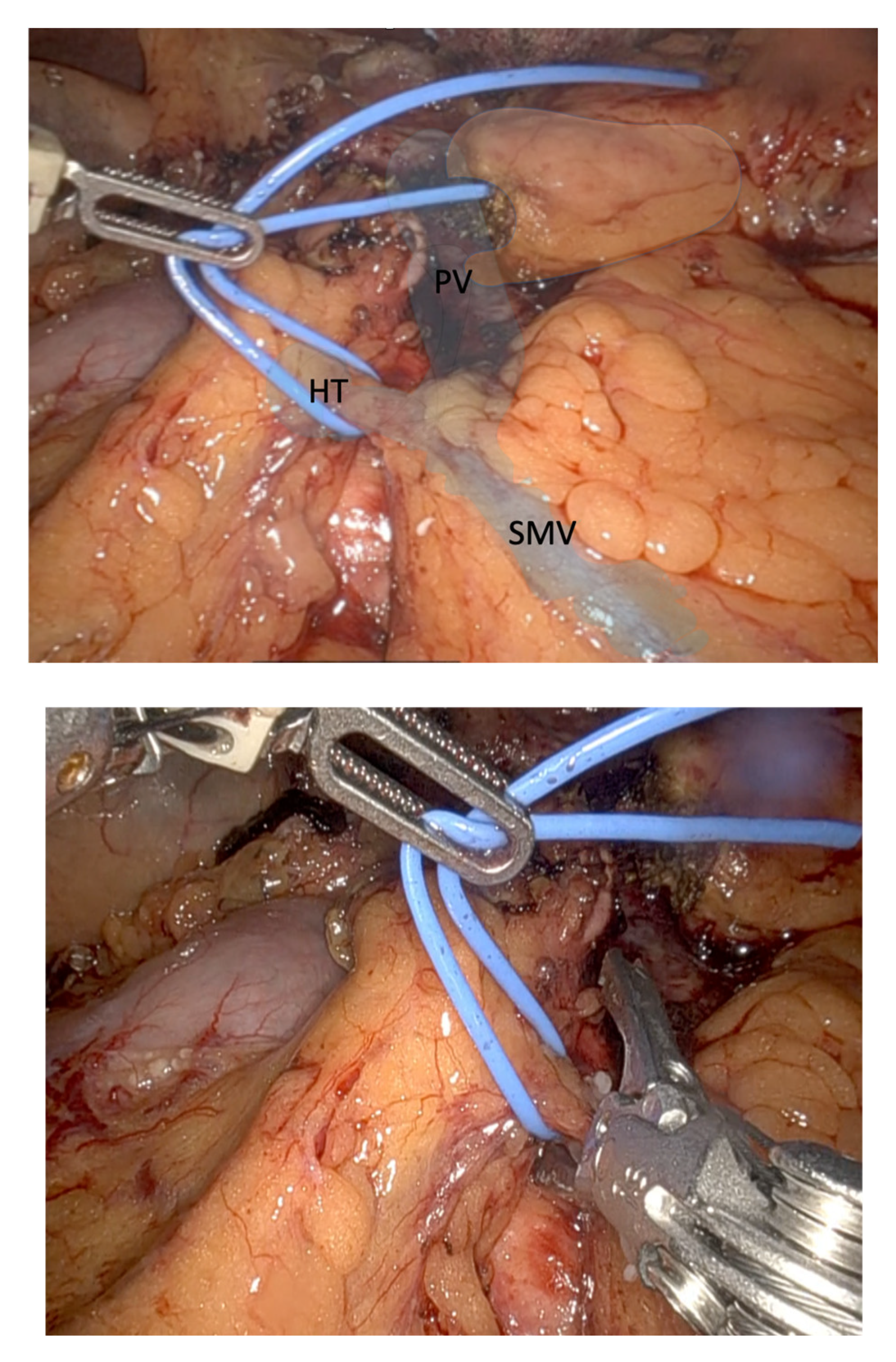
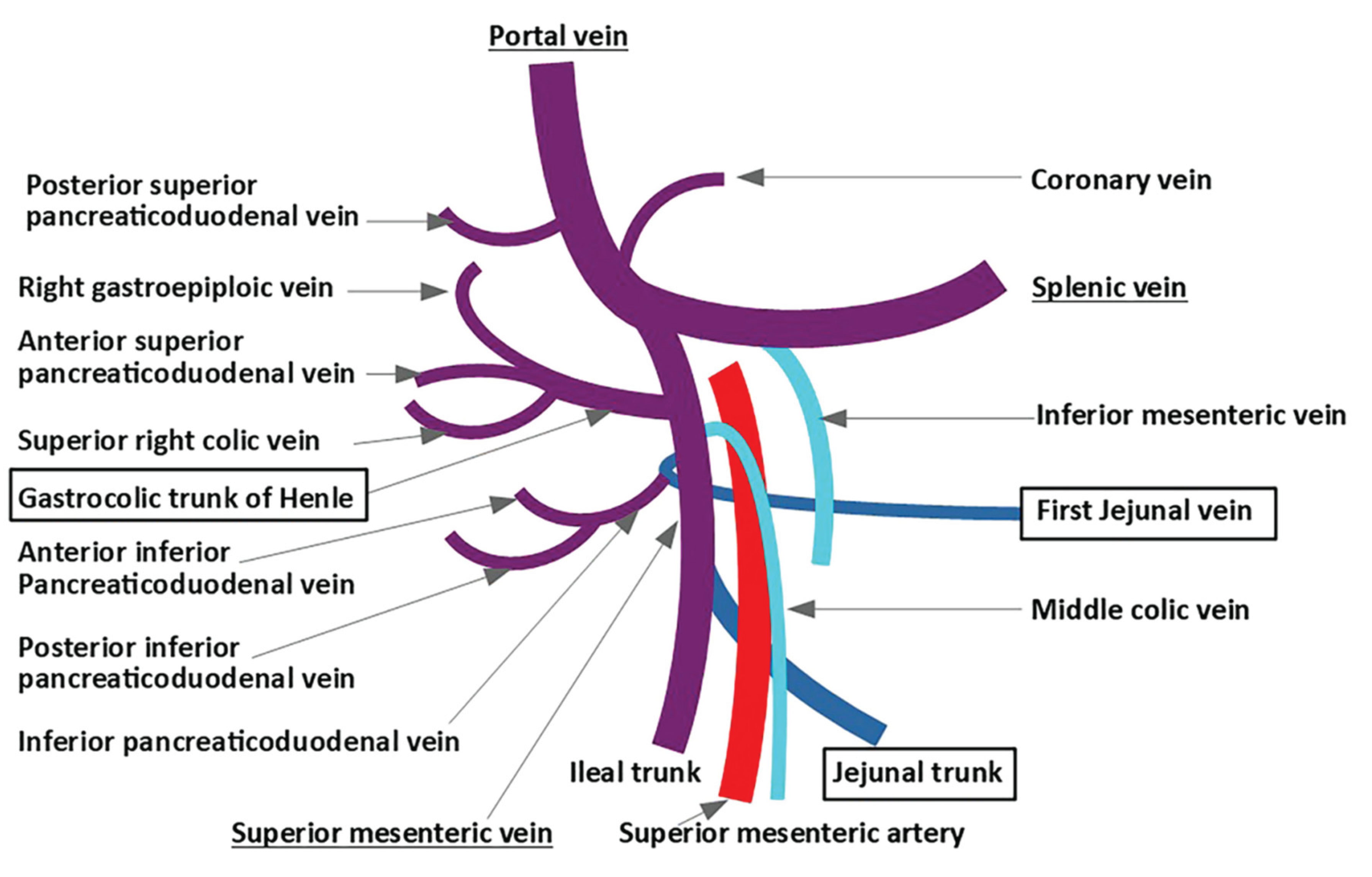
Trunk of Henle (TH)
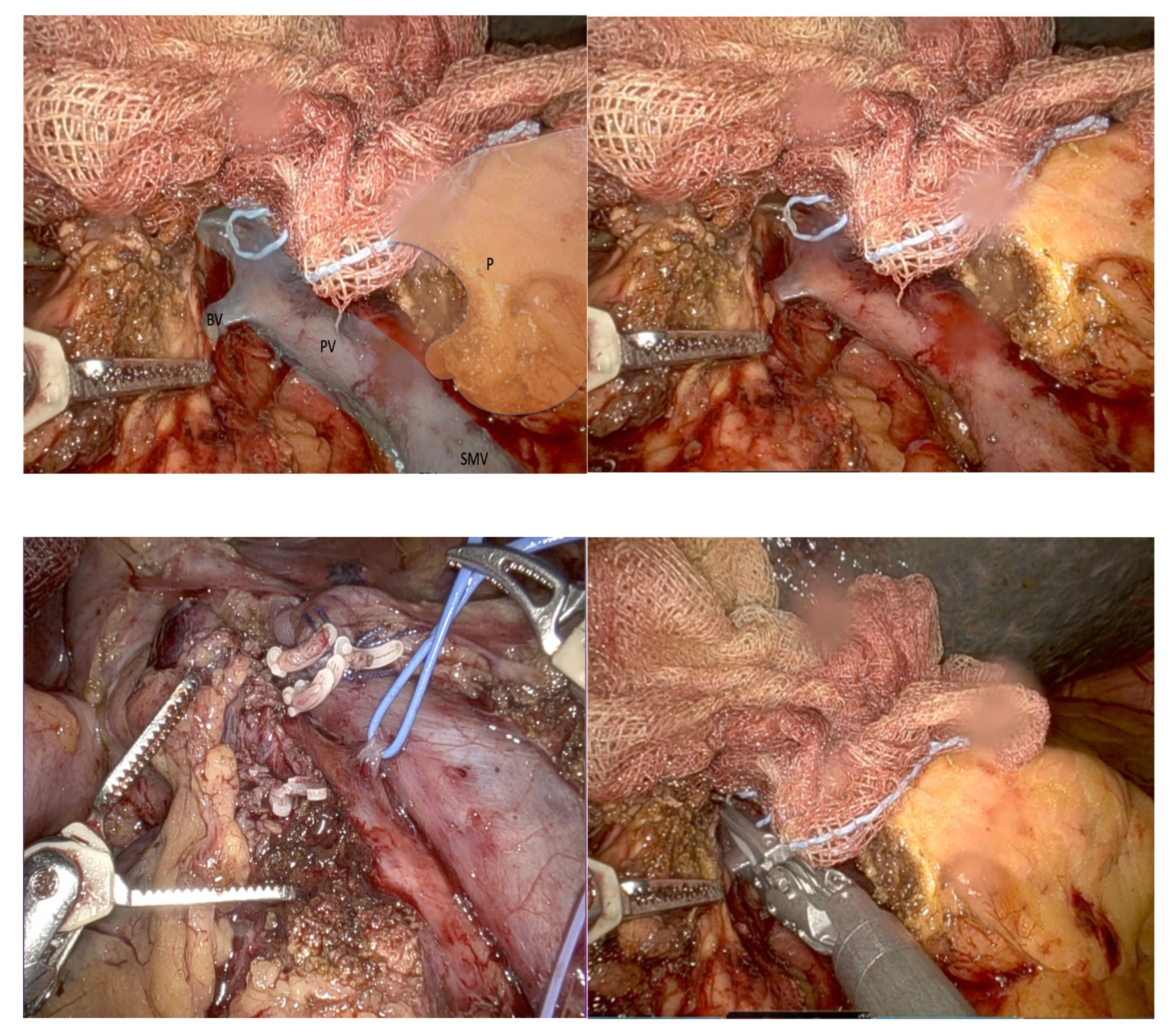
Belcher’s Vein (BV)
Discussion
Conclusion
References
- Giulianotti PC, Mangano A, Bustos RE, Gheza F, Fernandes E, Masrur MA, et al. Operative technique in robotic pancreaticoduodenectomy (RPD) at University of Illinois at Chicago (UIC): 17 steps standardized technique. Surg Endosc. 2018;32(10):4329–36.
- Jones LR, Zwart MJW, de Graaf N, Wei K, Qu L, Jiabin J, et al. Learning curve stratified outcomes after robotic pancreatoduodenectomy: International multicenter experience. Surgery. 2024 Dec;176(6):1721–9.
- Cugat Andorrà E, Cremades Perez M, Navinés López J, Matallana Azorín C, Zárate Pinedo A, Pardo Aranda F, et al. Challenge and future of liver and pancreatic robotic surgery. Analysis of 64 cases in a specialized unit. Cir Esp (Engl Ed). 2022 Mar;100(3):154–60.
- Giulianotti PC, Sbrana F, Bianco FM, Elli EF, Shah G, Addeo P, et al. Robot-assisted laparoscopic pancreatic surgery: single-surgeon experience. Surg Endosc. 2010 Jul 1;24(7):1646–57.
- Negoi I, Beuran M, Hostiuc S, Negoi RI, Inoue Y. Surgical Anatomy of the Superior Mesenteric Vessels Related to Pancreaticoduodenectomy: a Systematic Review and Meta-Analysis. J Gastrointest Surg. 2018 May;22(5):802–17.
- Stefura T, Kacprzyk A, Droś J, Pędziwiatr M, Major P, Hołda MK. The venous trunk of henle (gastrocolic trunk): A systematic review and meta-analysis of its prevalence, dimensions, and tributary variations. Clin Anat. 2018 Nov;31(8):1109–21.
- Negoi I, Beuran M, Hostiuc S, Negoi RI, Inoue Y. Response of the Authors to the Letter of the Editor Surgical Anatomy of the Superior Mesenteric Vessels Related to Pancreaticoduodenectomy: a Systematic Review and Meta-Analysis. J Gastrointest Surg. 2018 Aug 1;22(8):1457–1457.
- Katz MHG, Fleming JB, Pisters PWT, Lee JE, Evans DB. Anatomy of the Superior Mesenteric Vein With Special Reference to the Surgical Management of First-order Branch Involvement at Pancreaticoduodenectomy. Annals of Surgery. 2008 Dec;248(6):1098–102.
- Toya K, Tomimaru Y, Kobayashi S, Sasaki K, Iwagami Y, Yamada D, et al. Investigation of the variation of vessels around the pancreatic head based on the first jejunal vein anatomy at pancreaticoduodenectomy. Langenbecks Arch Surg. 2023 Aug 28;408(1):340.
- Klompmaker S, van Hilst J, Wellner UF, Busch OR, Coratti A, D’Hondt M, et al. Outcomes After Minimally-invasive Versus Open Pancreatoduodenectomy: A Pan-European Propensity Score Matched Study. Annals of Surgery. 2020 Feb;271(2):356.
- Pran L, Baijoo S, Dan D, Maharaj R. The Vein of Belcher: Revisited. J Gastrointest Surg. 2018 Jul 1;22(7):1303–4.
- AlMasri S, Kraftician J, Zureikat A, Paniccia A. Management of Intra-Operative Hemorrhage and Safe Venous Resection in Robotic-Assisted Pancreaticoduodenectomy: Techniques to Avoid Open Conversion. J Gastrointest Surg. 2023 Aug;27(8):1753–6.
- Bruna CL, Emmen AMLH, Wei K, Sutcliffe RP, Shen B, Fusai GK, et al. Effects of Pancreatic Fistula After Minimally Invasive and Open Pancreatoduodenectomy. JAMA Surg. 2025 Feb 1;160(2):190–8.
- Negoi I, Beuran M, Hostiuc S, Negoi RI, Inoue Y. Surgical Anatomy of the Superior Mesenteric Vessels Related to Colon and Pancreatic Surgery: A Systematic Review and Meta-Analysis. Sci Rep. 2018 Mar 8;8(1):4184.
- Desai G, Wagle PK. First jejunal vein, jejunal trunk, and pancreatico-duodenectomy: resolving the literature conundrum. Langenbecks Arch Surg. 2023 Feb 24;408(1):104.
- Cirocchi R, Matteucci M, Randolph J, Boselli C, Davies J, Scarselletti G, et al. Anatomical Variants of the Jejunal Veins and Their Technical Implications in Pancreaticoduodenectomy: A Systematic Review and Meta-Analysis. Dig Surg. 2024;41(5–6):245–55.
- Nagakawa Y, Hosokawa Y, Sahara Y, Takishita C, Hijikata Y, Osakabe H, et al. Approaching the superior mesenteric artery from the right side using the proximal-dorsal jejunal vein preisolation method during laparoscopic pancreaticoduodenectomy. Surg Endosc. 2018 Sep 1;32(9):4044–51.
- Kang MJ, Han SS, Park SJ, Park HM, Kim SW. Do jejunal veins matter during pancreaticoduodenectomy? Ann Hepatobiliary Pancreat Surg. 2022 Aug 31;26(3):229–34.
- Miyazawa M, Kawai M, Hirono S, Okada K ichi, Shimizu A, Kitahata Y, et al. Preoperative evaluation of the confluent drainage veins to the gastrocolic trunk of Henle: understanding the surgical vascular anatomy during pancreaticoduodenectomy. Journal of Hepato-Biliary-Pancreatic Sciences. 2015;22(5):386–91.
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2025 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (http://creativecommons.org/licenses/by/4.0/).




