Submitted:
19 June 2025
Posted:
23 June 2025
You are already at the latest version
Abstract
Keywords:
1. Introduction
2. Materials and Methods
2.1. Study Design, Settings, and Ethical Approval
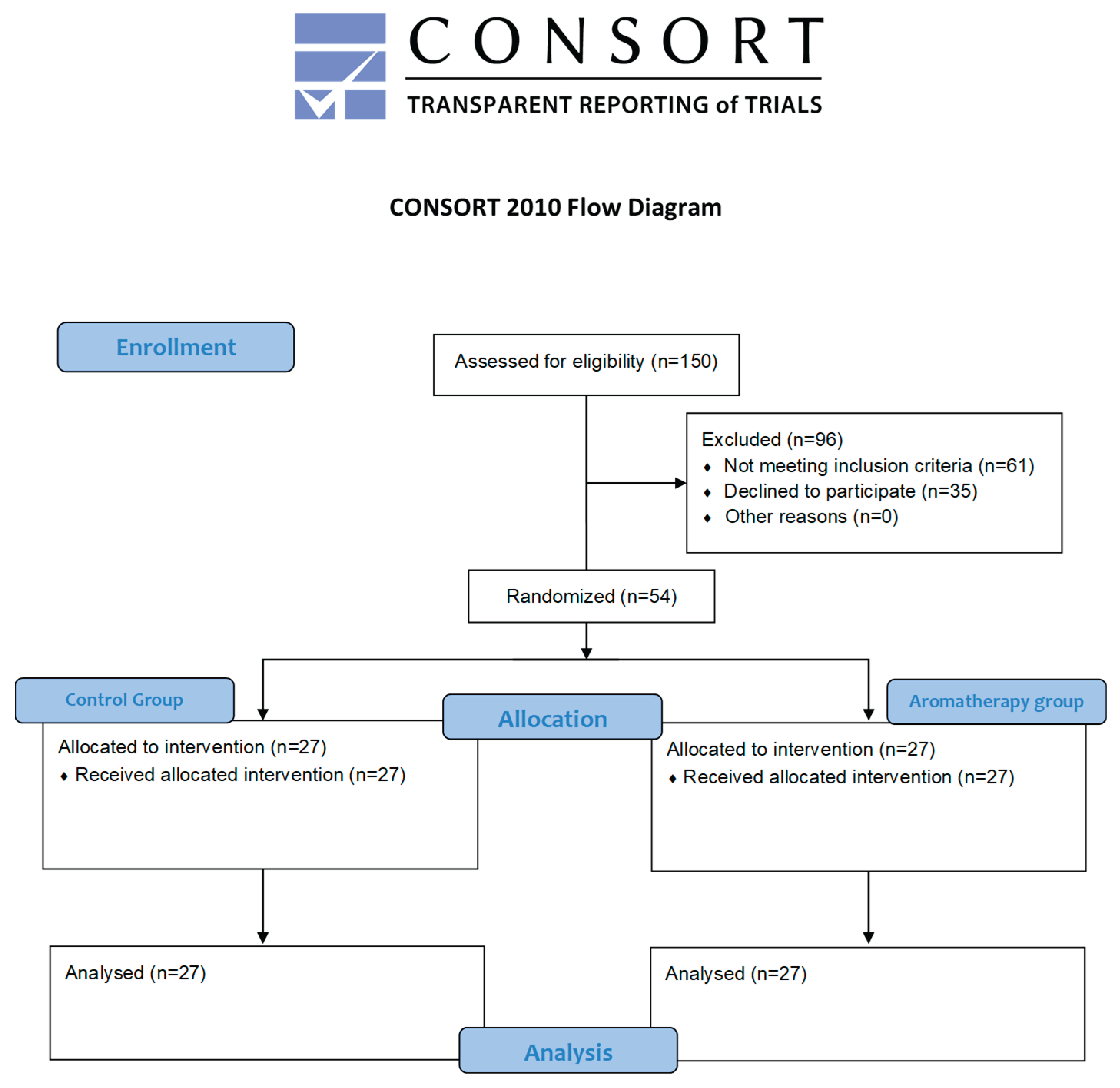
2.2. Sample Size Calculation
2.3. Recruitment and Eligibility Criteria
2.4. Randomization
2.5. Blinding
2.6. Intervention Procedures
2.7. Outcomes and Measurements
2.8. Statical Analysis
3. Results
4. Discussion
5. Conclusions
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Acknowledgments
Conflicts of Interest
References
- Grisolia BM, Dos Santos APP, Dhyppolito IM, Buchanan H, Hill K, Oliveira BH. Prevalence of dental anxiety in children and adolescents globally: A systematic review with meta-analyses. Int J Paediatr Dent. 2021 Mar;31(2):168-183. [CrossRef] [PubMed]
- Crellin DJ, Harrison D, Santamaria N, Huque H, Babl FE. The Psychometric Properties of the FLACC Scale Used to Assess Procedural Pain. J Pain. 2018 Aug;19(8):862-872. [CrossRef] [PubMed]
- Shukla H, Kulkarni S, Wasnik MB, Rojekar N, Bhattad D, Kolekar P. Acceptance of Parents for Behavior Management Technique with Reference to Previous Dental Expertise and Dental Anxiety. Int J Clin Pediatr Dent. 2021;14(Suppl 2):S193-S198. [CrossRef] [PubMed] [PubMed Central]
- Shindova MP, Belcheva AB. Dental fear and anxiety in children: a review of the environmental factors. Folia Med (Plovdiv). 2021 Apr 30;63(2):177-182. [CrossRef] [PubMed]
- Appukuttan, DP. Strategies to manage patients with dental anxiety and dental phobia: literature review. Clin Cosmet Investig Dent. 2016 Mar 10;8:35-50. [CrossRef] [PubMed] [PubMed Central]
- Zinke A, Hannig C, Berth H. Comparing oral health in patients with different levels of dental anxiety. Head Face Med. 2018 Nov 20;14(1):25. [CrossRef] [PubMed] [PubMed Central]
- Seangpadsa K, Smutkeeree A, Leelataweewud P. Parental acceptance of behavior management techniques for preschool children in dental practice: Revisited. J Indian Soc Pedod Prev Dent. 2020 Jul-Sep;38(3):274-279. [CrossRef] [PubMed]
- Coté CJ, Wilson S. Guidelines for Monitoring and Management of Pediatric Patients Before, During, and After Sedation for Diagnostic and Therapeutic Procedures. Pediatr Dent. 2019 Jul 15;41(4):259-260. [PubMed]
- Bikmoradi A, Khaleghverdi M, Seddighi I, Moradkhani S, Soltanian A, Cheraghi F. Effect of inhalation aromatherapy with lavender essence on pain associated with intravenous catheter insertion in preschool children: A quasi-experimental study. Complement Ther Clin Pract. 2017 Aug;28:85-91. [CrossRef] [PubMed]
- Moslemi F, Alijaniha F, Naseri M, Kazemnejad A, Charkhkar M, Heidari MR. Citrus aurantium Aroma for Anxiety in Patients with Acute Coronary Syndrome: A Double-Blind Placebo-Controlled Trial. J Altern Complement Med. 2019 Aug;25(8):833-839. [CrossRef] [PubMed]
- Reyes MCGM, Reyes MCGM, Ribay KGL, Paragas ED Jr. Effects of sweet orange aromatherapy on pain and anxiety during needle insertion among patients undergoing hemodialysis: A quasi-experimental study. Nurs Forum. 2020 Jul;55(3):425-432. [CrossRef] [PubMed]
- Babar Ali, Naser Ali Al-Wabel, Saiba Shams, Aftab Ahamad, Shah Alam Khan, Firoz Anwar, Essential oils used in aromatherapy: A systemic review, Asian Pacific Journal of Tropical Biomedicine. 2015 Aug; 5(8): 601-611. ISSN 2221-1691. [CrossRef]
- Alkanan SAM, Alhaweri HS, Khalifa GA, Ata SMS. Dental pain perception and emotional changes: on the relationship between dental anxiety and olfaction. BMC Oral Health. 2023 Mar 26;23(1):175. [CrossRef] [PubMed] [PubMed Central]
- Wang ZJ, Heinbockel T. Essential Oils and Their Constituents Targeting the GABAergic System and Sodium Channels as Treatment of Neurological Diseases. Molecules. 2018 May 2;23(5):1061. [CrossRef] [PubMed] [PubMed Central]
- MICHALAK, Monika. Aromatherapy and methods of applying essential oils. Archives of Physiotherapy and Global Researches, 2018, 22.2: 25-31.
- Lv XN, Liu ZJ, Zhang HJ, Tzeng CM. Aromatherapy and the central nerve system (CNS): therapeutic mechanism and its associated genes. Curr Drug Targets. 2013 Jul;14(8):872-9. [CrossRef] [PubMed]
- Wajda M, Gover A, Franco L, blanck T. 2017. “Review of Lavender Aromatherapy: Past, Present, and Future.” Austin Therapeutics 4(1). www.austinpublishinggroup.com.
- Donelli D, Antonelli M, Bellinazzi C, Gensini GF, Firenzuoli F. Effects of lavender on anxiety: A systematic review and meta-analysis. Phytomedicine. 2019 Dec;65:153099. [CrossRef] [PubMed]
- Scandurra C, Mezzalira S, Cutillo S, Zapparella R, Statti G, Maldonato NM, Locci M, Bochicchio V. The Effectiveness of Neroli Essential Oil in Relieving Anxiety and Perceived Pain in Women during Labor: A Randomized Controlled Trial. Healthcare (Basel). 2022 Feb 14;10(2):366. [CrossRef] [PubMed] [PubMed Central]
- Mannucci, C., Calapai, F., Cardia, L., Inferrera, G., D'Arena, G., Di Pietro, M.,... & Calapai, G. (2018). Clinical Pharmacology of Citrus aurantium and Citrus sinensis for the Treatment of Anxiety. Evidence-based complementary and alternative medicine: eCAM, 2018.
- Venkataramana, M., Pratap, K. V. N. R., Padma, M., Kalyan, S., Reddy, A. A., & Sandhya, P. (2016). Effect of aromatherapy on dental patient anxiety: A randomized controlled trial. Journal of Indian Association of Public Health Dentistry, 14(2), 131-134.
- Zabirunnisa M, Gadagi JS, Gadde P, Myla N, Koneru J, Thatimatla C. Dental patient anxiety: Possible deal with Lavender fragrance. J Res Pharm Pract. 2014 Jul;3(3):100-3. [CrossRef] [PubMed] [PubMed Central]
- Arslan I, Aydinoglu S, Karan NB. Can lavender oil inhalation help to overcome dental anxiety and pain in children? A randomized clinical trial. Eur J Pediatr. 2020 Jun;179(6):985-992. [CrossRef] [PubMed]
- Nirmala K, Kamatham R. Effect of Aromatherapy on Dental Anxiety and Pain in Children Undergoing Local Anesthetic Administrations: A Randomized Clinical Trial. J Caring Sci. 2021 Aug 23;10(3):111-120. [CrossRef] [PubMed] [PubMed Central]
- Jafarzadeh M, Arman S, Pour FF. Effect of aromatherapy with orange essential oil on salivary cortisol and pulse rate in children during dental treatment: A randomized controlled clinical trial. Adv Biomed Res. 2013 Mar 6;2:10. [CrossRef] [PubMed] [PubMed Central]
- SONI, Sheena; BHATIA, Rupinder; OBEROI, Jyoti. Evaluation of the efficacy of aromatherapy on anxiety level among pediatric patients in a dental setting: a randomized control trial. International Journal of Oral Care and Research, 2018, 6.2: 44-9.
- Ghaderi, Faezeh, and Neda Solhjou. 2020. “The Effects of Lavender Aromatherapy on Stress and Pain Perception in Children during Dental Treatment: A Randomized Clinical Trial.” Complementary Therapies in Clinical Practice 40.
- Abdalhai, R., Kouchaji, C., & Alkhatib, R. (2024). The effect of aromatherapy with Lavender-Neroli oil and music in management of pediatric dental anxiety: a randomized control trial. BDJ open, 10(1), 5.
- PRADOPO, Seno; SINAREDI, Betadion Rizki; JANUARISCA, Bernadeth Vindi. Pandan Leaves (Pandanus Amaryllifolius) aromatherapy and relaxation music to reduce dental anxiety of pediatric patients. Journal of International Dental and Medical Research, 2017, 10.3: 933-937.
- McHugh, ML. Interrater reliability: the kappa statistic. Biochem Med (Zagreb). 2012;22(3):276-82. [PubMed] [PubMed Central]
- Dean, Jeffrey A. 2021. Mcdonald and Avery’s Dentistry for the Child and Adolescent. 11 Edition. ed. Jeffrey A. Dean. Elsevier Health Science pp 327-330.
- Tiwari S, Kulkarni P, Agrawal N, Mali S, Kale S, Jaiswal N. Dental Anxiety Scales Used in Pediatric Dentistry: A Systematic Review and Meta-analysis. J Contemp Dent Pract. 2021 Nov 1;22(11):1338-1345. [PubMed]
- FATHIMA, Faazila; JEEVANANDAN, Ganesh. Validation of a facial image scale to assess child dental anxiety. Drug Invent Today, 2018, 10: 2825-8.
- Dak Albab, Rahaf, and Hisham Shakhashero. 2016. “The Validity and Reliability of the Arabic Version of FLACC Scale: A Clinical Trial.” Journal of Anesthesia & Clinical Research 7(8).
- Aditya PVA, Prasad MG, Nagaradhakrishna A, Raju NS, Babu DN. Comparison of effectiveness of three distraction techniques to allay dental anxiety during inferior alveolar nerve block in children: A randomized controlled clinical trial. Heliyon. 2021 Sep 29;7(9):e08092. [CrossRef] [PubMed] [PubMed Central]
- O'Flaherty LA, van Dijk M, Albertyn R, Millar A, Rode H. Aromatherapy massage seems to enhance relaxation in children with burns: an observational pilot study. Burns. 2012 Sep;38(6):840-5. [CrossRef] [PubMed]
- Harada H, Kashiwadani H, Kanmura Y, Kuwaki T. Linalool Odor-Induced Anxiolytic Effects in Mice. Front Behav Neurosci. 2018 Oct 23;12:241. [CrossRef] [PubMed] [PubMed Central]
- Eddin LB, Jha NK, Meeran MFN, Kesari KK, Beiram R, Ojha S. Neuroprotective Potential of Limonene and Limonene Containing Natural Products. Molecules. 2021 Jul 27;26(15):4535. [CrossRef] [PubMed] [PubMed Central]
- Hyde J, Ryan KM, Waters AM. Psychophysiological Markers of Fear and Anxiety. Curr Psychiatry Rep. 2019 Jun 4;21(7):56. [CrossRef]
- Malcolm BJ, Tallian K. Essential oil of lavender in anxiety disorders: Ready for prime time? Ment Health Clin. 2018 Mar 26;7(4):147-155. [CrossRef] [PubMed] [PubMed Central]
- Nwosu ADG, Ossai EN, Onwuasoigwe O, Ahaotu F. Oxygen saturation and perceived discomfort with face mask types, in the era of COVID-19: a hospital-based cross-sectional study. Pan Afr Med J. 2021 Jul 16;39:203. [CrossRef] [PubMed] [PubMed Central]
- Raglio, A. (2023). A noval music-based theraeutic approach: the therapeutic music listening. Front in Human Nerouscience, 17:1204593-1204593. [CrossRef]
- Toet A, Smeets MA, van Dijk E, Dijkstra D, van den Reijen L. Effects of Pleasant Ambient Fragrances on Dental Fear: Comparing Apples and Oranges. Chemosens Percept. 2010 Dec;3(3-4):182-189. [CrossRef] [PubMed] [PubMed Central]
- van der Weijden, F. N., etal. (2022). The effect of playing background music during dental treatment on dental anxiety and physiological parameters: A systematic review and meta-analysis. Psychology of Music, 50(2):365–388. [CrossRef]
- Nord D, Belew J. Effectiveness of the essential oils lavender and ginger in promoting children's comfort in a perianesthesia setting. J Perianesth Nurs. 2009 Oct;24(5):307-12. [CrossRef] [PubMed]
- Attar RH, Baghdadi ZD. Comparative efficacy of active and passive distraction during restorative treatment in children using an iPad versus audiovisual eyeglasses: a randomised controlled trial. Eur Arch Paediatr Dent. 2015 Feb;16(1):1-8. [CrossRef] [PubMed]
- Baghdadi, ZD. Evaluation of audio analgesia for restorative care in children treated using electronic dental anesthesia. J Clin Pediatr Dent. 2000 Fall;25(1):9-12. [PubMed]
- Baghdadi, ZD. Evaluation of electronic dental anesthesia in children. Oral Surg Oral Med Oral Pathol Oral Radiol Endod. 1999 Oct;88(4):418-23. [CrossRef] [PubMed]
- Haralambidis C, Nicozisis J. High-frequency neuromodulation with the dental pain eraser for nonpharmacologic pain relief in orthodontic practice. J Clin Orthod. 2024 Septemeber;58(9):567-572. [PubMed]

| Before anesthesia | After anesthesia | |||||
|---|---|---|---|---|---|---|
| Variables | Control group | Aromatherapy group | P-Value | Control Group | Aromatherapy group | p-Value |
| FIS* | 58.34 | 55.11 | 0.916 | 79.88 | 51.7 | 0.001S |
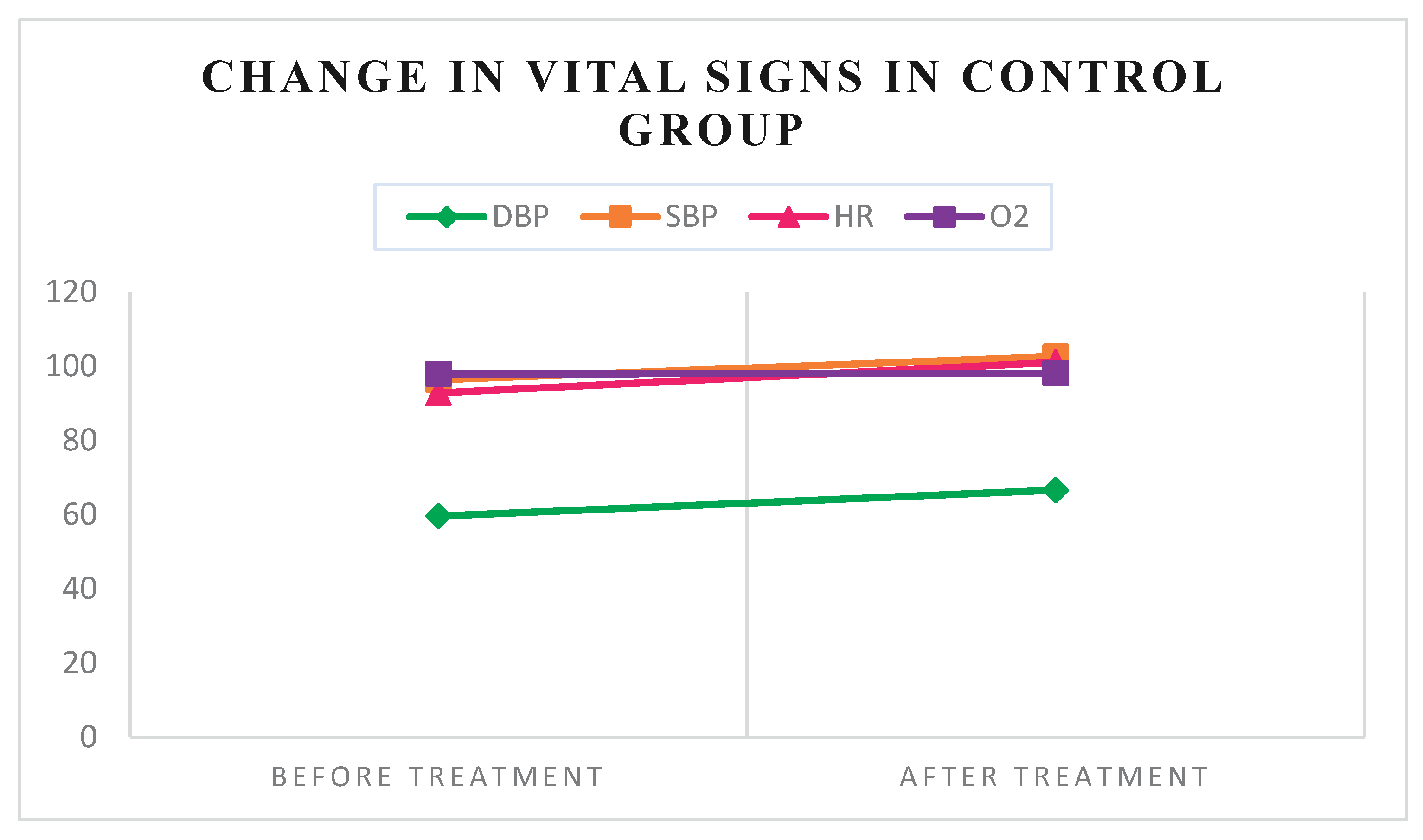
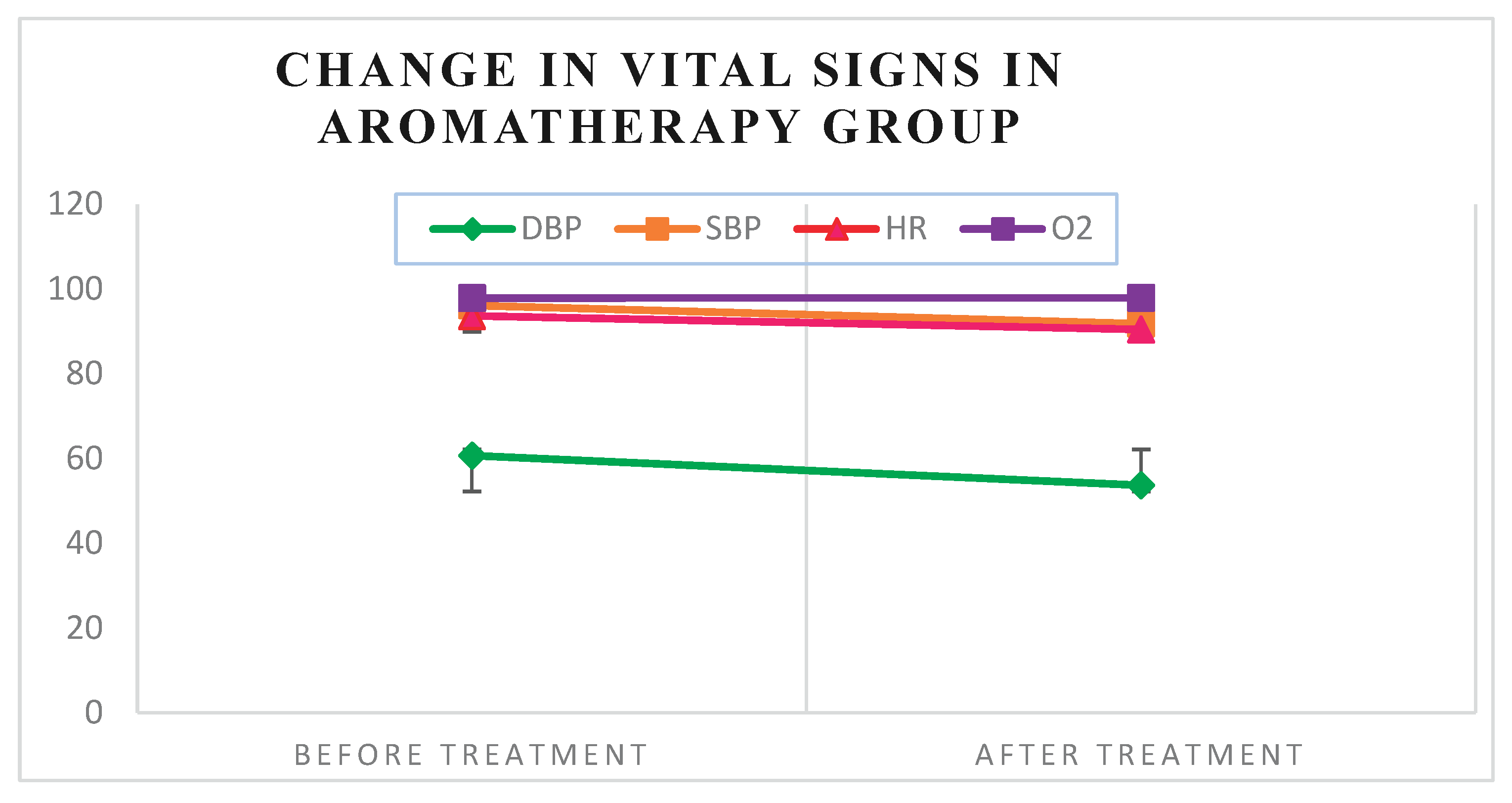
| DBP$ | 59.57 ±11.59 | 60.7 ±12.07 | 0.182 | 66.61 ±16.31 | 53.67 ±10.34 | 0.013S |
| SBP$ | 96.36 ±9.97 | 96.11 ±13.46 | 1.00 | 102.61 ±11.33 | 91.81 ±12.57 | 0.038S |
| HR$ | 92.79 ±15.76 | 93.63 ±16.83 | 0.825 | 101.04 ±19.43 | 90.48 ±17.11 | 0.000S |
| SPO2$ | 98.07 ±1.24 | 97.85 ±1.61 | 0.563 | 98.11±1.13 | 97.93 ±1.33 | 0.744 |
| FLACC$ | ----- | ----- | ----- | 3.11 ±2.42 | 1.51 ±1.87 | 0.042S |
| FIS: Facial Image Scale, DBP: Diastolic blood pressure, SBP: Systolic blood pressure, HR: Heart rate, SPO2: O2 Oxygen saturation, FLACC: Face-Legs-Activity-Cry-Consolability.Mean ranks were used for the FIS scale, whereas means ±Standard Deviation (SD) was used for vital signs and the FLACC scale. *: Differences in mean ranks of FIS between groups were analyzed using the Mann-Whitney U test. $: Differences in means of vital signs and FLACC scale between groups were analyzed using an independent T-test. S: Significant differences between groups. | ||||||
| Variables | Before treatment | After treatment | After-beforeMean differences ±SD | p-value | |
|---|---|---|---|---|---|
| Control group | FIS* | 58.34 | 79.88 | 0.000S | |
| DBP$ | 59.57 ±11.59 | 66.61 ±16.31 | 7.04 ±15.57 | 0.024S | |
| SBP$ | 96.36 ±9.97 | 102.61 ±11.33 | 6.25 ±10.46 | 0.004S | |
| HR$ | 92.79 ±15.76 | 101.04 ±19.43 | 8.25 ±10.17 | 0.000S | |
| SPO2$ | 97.93 ±1.09 | 98.11 ±1.13 | 0.18 ±1.33 | 0.485 | |
| Aromatherapy group | FIS* | 55.11 | 51.7 | 0.6 | |
| DBP$ | 60.7 ±12.07 | 53.67 ±10.34 | -7.04 ±13.32 | 0.011S | |
| SBP$ | 96.11 ±13.46 | 91.81 ±12.57 | -4.30 ±13.47 | 0.109 | |
| HR$ | 93.63 ±16.83 | 90.48 ±17.11 | -3.15 ±7.69 | 0.043S | |
| O2$ | 97.85 ±1.61 | 97.93 ±1.33 | 0.07 ±1.44 | 0.791 | |
|
*: FIS Means rank Differences in value before and after treatment were analyzed using the Wilcoxon signed-rank test. $: Means differences in value before and after treatment were analyzed using paired t-test. S: Significant differences were found within the group | |||||
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2025 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (http://creativecommons.org/licenses/by/4.0/).




