1. Introduction
Multiple studies have demonstrated the efficacy of MARPE (Mini screw-Assisted Rapid Palatal Expander) in producing skeletal maxillary expansion in adult patients [
1,
2], as well as the stability [
3] of these outcomes. Other studies have shown that MARPE can reduce daytime sleepiness and improve symptoms in patients with obstructive sleep apnea (OSA) [
4,
5].
While the effects of MARPE expansion in adults are well documented, there is a wide variety of techniques and appliance designs used to achieve skeletal maxillary expansion in this population, resulting in variable efficiency and outcomes.
A meta-analysis by Liu et al. [
6] evaluated the short- and long-term effects of MARPE on the upper airway and alar dimensions in non-growing patients. The study reported significant increases in nasal cavity width (mean difference: 2.05 mm), nasal floor width (mean difference: 2.13 mm), nasal cavity volume (mean difference: 1.24 cm³), and alar width (mean difference: 1.47 mm). These findings suggest that MARPE effectively expands the nasal and maxillary structures, potentially improving nasal breathing. The study also found significant reductions in nasal resistance and increases in nasal airflow following MARPE treatment, likely attributed to the expanded nasal cavity dimensions.
Adjunct techniques such as midpalatal corticotomy and piezocorticotomy have been shown to facilitate suture separation, with measurements of 3.14 mm at the premolar area and 2.06 mm at the molar area of maxillary crest-to-crest bone separation. This approach effectively addresses transverse maxillary deficiency in adult patients. (7) Although systematic reviews favor the conclusion that MARPE produces significant clinical changes compared to conventional rapid palatal expander, surgically assisted rapid palatal expansion (SARPE), or controls, they highlight a lack of consistent methodology and outcome data [
6].
Guided MARPE insertion with a 3D-planned and pre-printed temporary anchorage device (TAD) guide was described in a case report by Minervini et al.[
7], which focused on the design and positioning of MARPE-supporting mini-screws rather than guided piezocorticotomy for midpalatal dissection.
The aim of this case series is to describe a novel 3D-printed and 3D-designed midpalatal piezocorticotomy guide and its benefits for MARPE-assisted midfacial skeletal expansion.
2. Materials and Methods
All study participants have signed a written consent to participate in the research prior to commencement of the study.
2.1. Description of MARPE Installation Procedure
The MARPE installation is preceded by a guide-assisted midpalatal piezocorticotomy (Piezosurgery touch, Mectron, Hilliard, OH, USA) under local anesthesia. The procedure begins with a fit check of the midpalatal piezocorticotomy guide, adjustment of the occlusal fit if needed, and the initial notch placement as specified by the guide design. The incisions are made to the depth of the palatine bone and the crests of the maxillary bones. Proprioceptive feedback and pre-measured bone depths help determine cortical plate penetration. Piezocorticotomy tips are pre-calibrated for various incision depths. One week of healing is allowed before MARPE activation begins. Activation proceeds at one turn/day for females over 8–9 weeks and at two turns/day for males until the initial midpalatal suture separation is achieved, followed by one turn/day for an additional 6–7 weeks (
Figure 1).
2.2. Description of the Novel Piezocorticotomy Guide for Midpalatal Skeletal Expansion
The midpalatal piezocorticotomy guide is an auxiliary appliance designed to enhance midpalatal piezocorticotomy results. This technique and design, filed under US and Canadian patent applications, provide a novel method for achieving predictable midfacial bone separation.
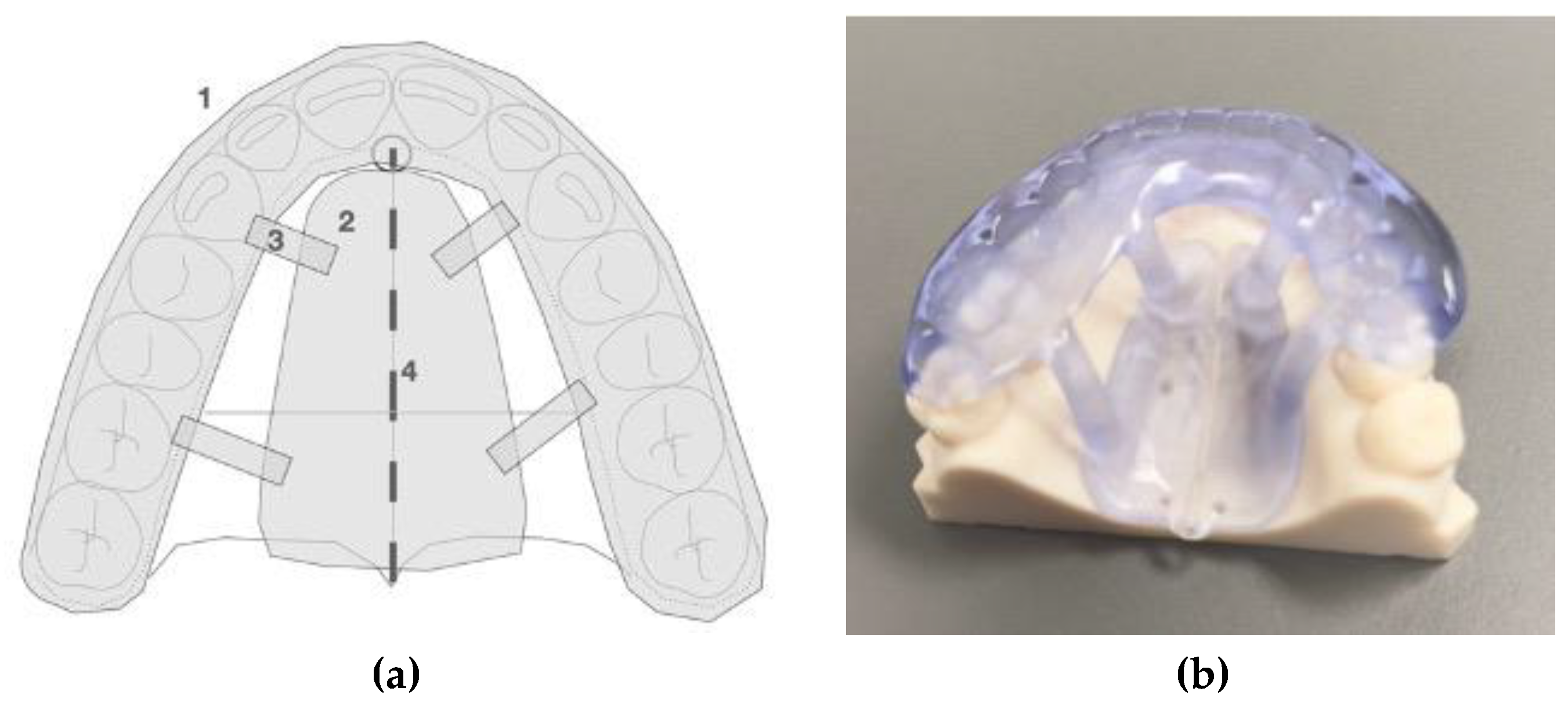
The guide is a custom-designed, 3D-printed, one-piece, unattached appliance that rests on the maxillary occlusal surfaces and palatal vault. It includes an occlusal splint, a palatal baseplate, and connectors attached to both. Printed from polymethyl methacrylate (PMMA) resin, the appliance is modifiable. The piezocorticotomy notch locations are determined via 3D planning and individualized patient anatomy (
Figure 2).
The appliance design and materials used for 3D printing are modifiable to improve retention, fit, and stability. The notch locations are determined through individualized 3D planning for each patient.
When PMMA resin is used as the printing material, a thickness of 2.5 mm is recommended. The appliance functions as a temporary guide during the piezocorticotomy incision procedure.
2.3. Technique of the 3D Printed Guide-Assisted Midpalatal Piezocortictomy
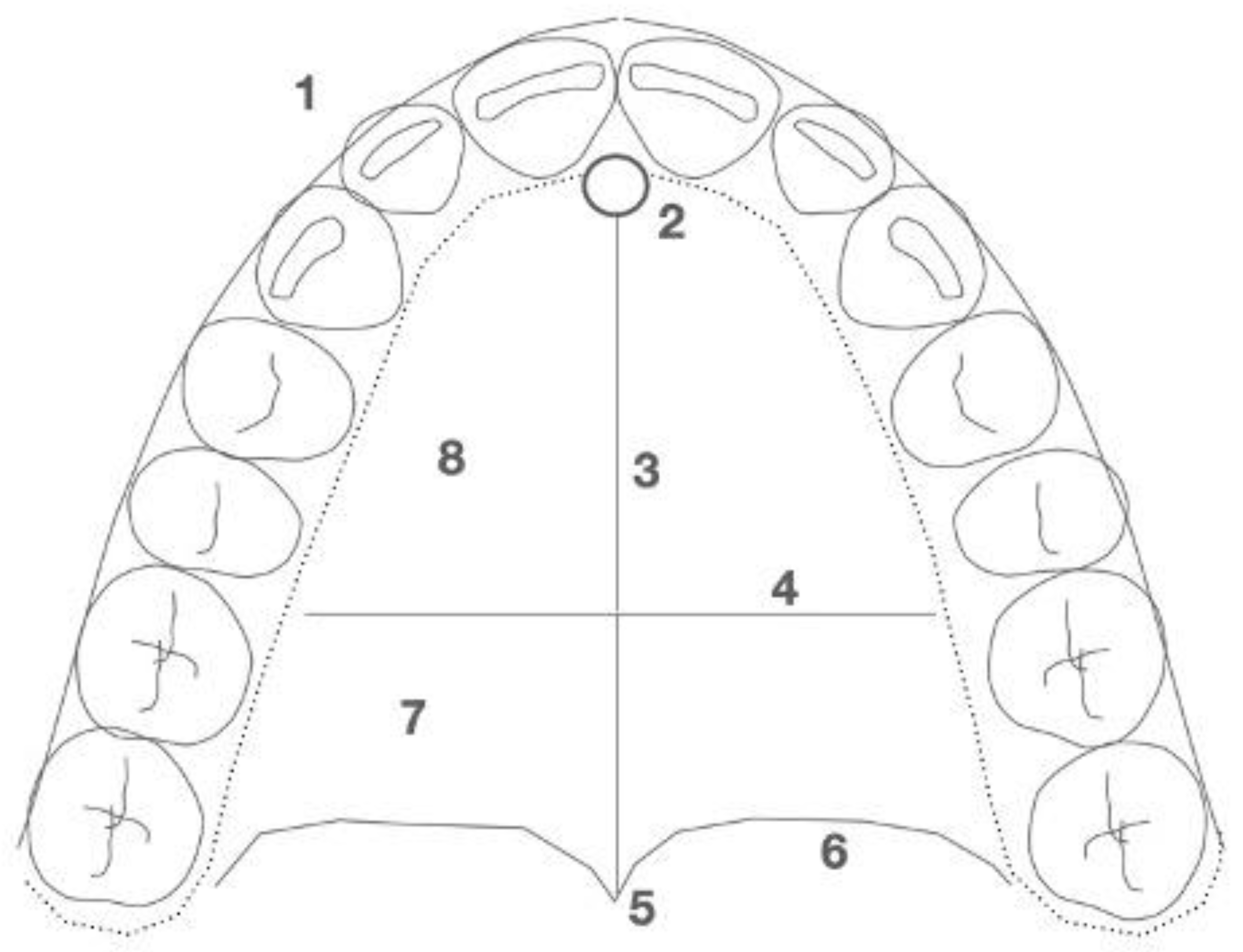
The midpalatal piezocorticotomy technique recommended by the authors involves guide-assisted piezocorticotomy utilizing CBCT-guided planning. This technique enables bilateral separation of the maxillary crests of the palatal processes and the palatine bones (
Figure 3).
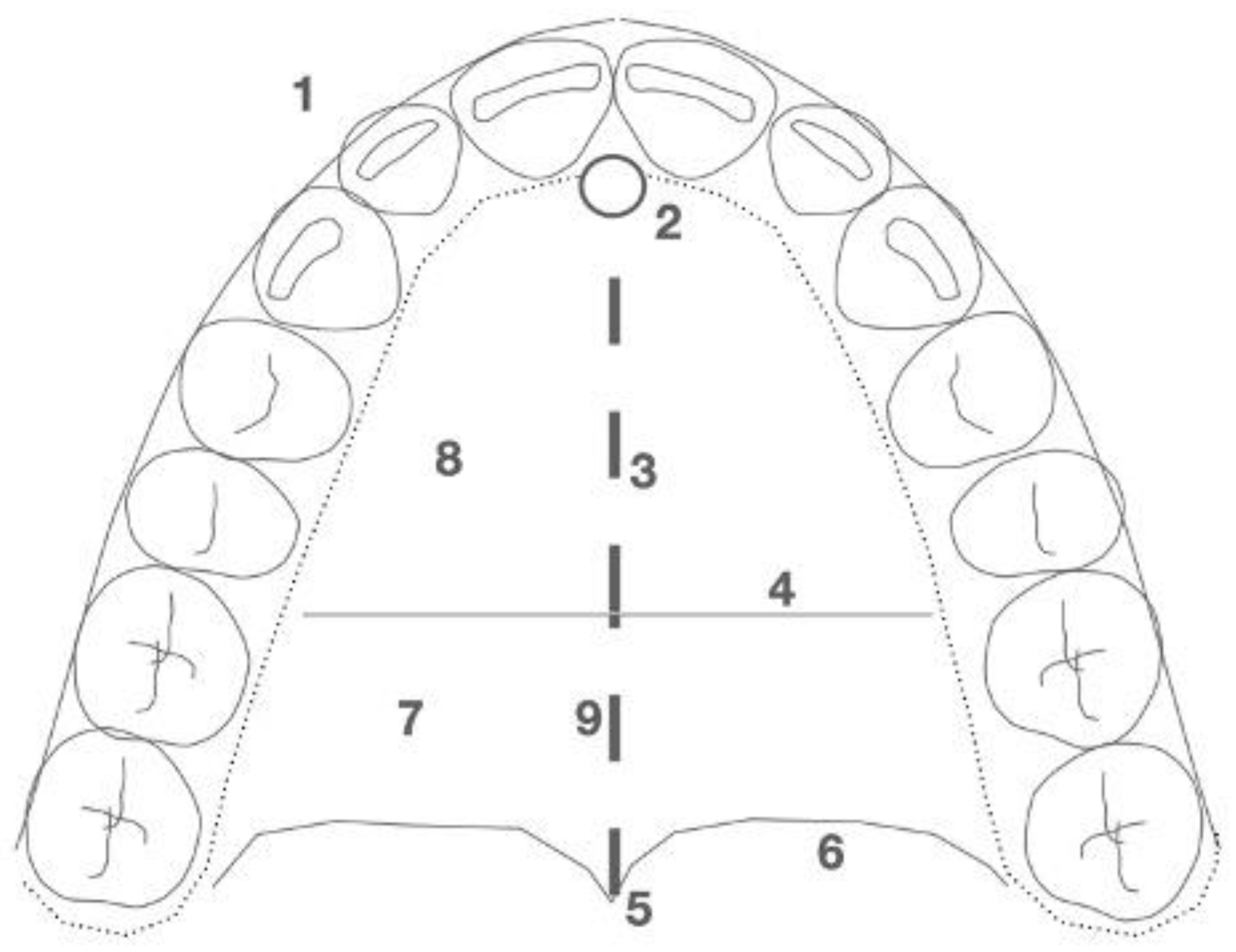
The incision extends from the distal aspect of the incisive foramen, in the projection of the nasal septum attachment, to the most distal margin of the palatine bone at the level of the posterior nasal spine (PNS) (
Figure 4).
2.4. Case A: Blind Midpalatal Piezocorticotomy with MARPE Expansion
A 25-year-old male patient underwent MARPE midfacial expansion with midpalatal piezocorticotomy, opting not to use the piezocorticotomy guide. The patient presented with a skeletal Class III base, anterior open bite, and posterior open bite. The procedure was performed under local anesthesia with topical and infiltrative application in the midpalatal area. Landmarks were visually positioned along the mucosal outline of the midpalatal suture, followed by piezotome incisions (Piezosurgery touch, Mectron, Hilliard, OH, USA). Expansion followed a one turn/day protocol over 12 weeks. The result (
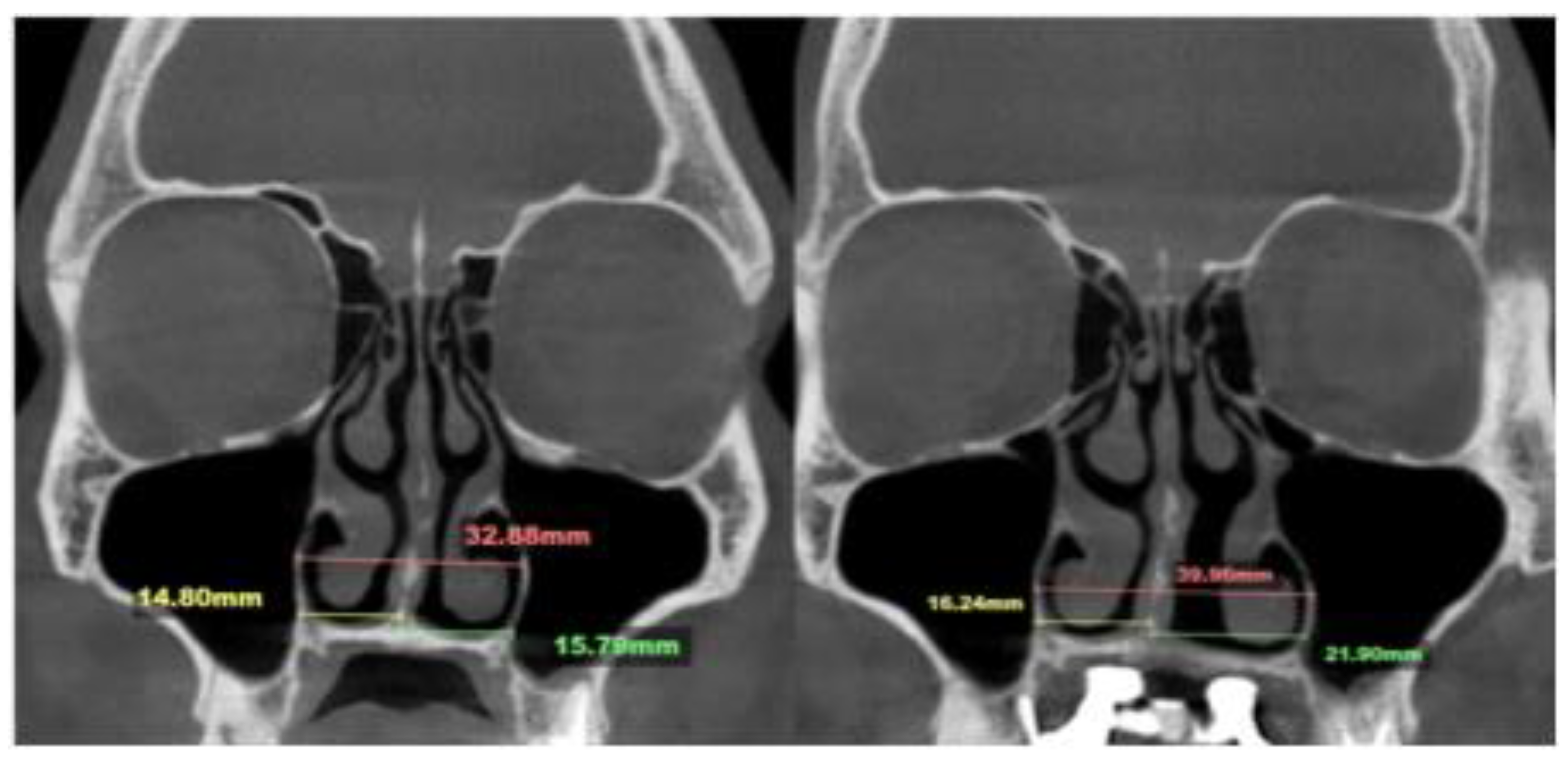
Figure 5) revealed unfavorable suture separation with asymmetrical nasal septum displacement and unilateral nasal airway expansion favoring the left side.
The total expansion 10. 5 mm was distributed unevenly, with approximately 75% of the total expansion occurring on the left passage (
Figure 6).
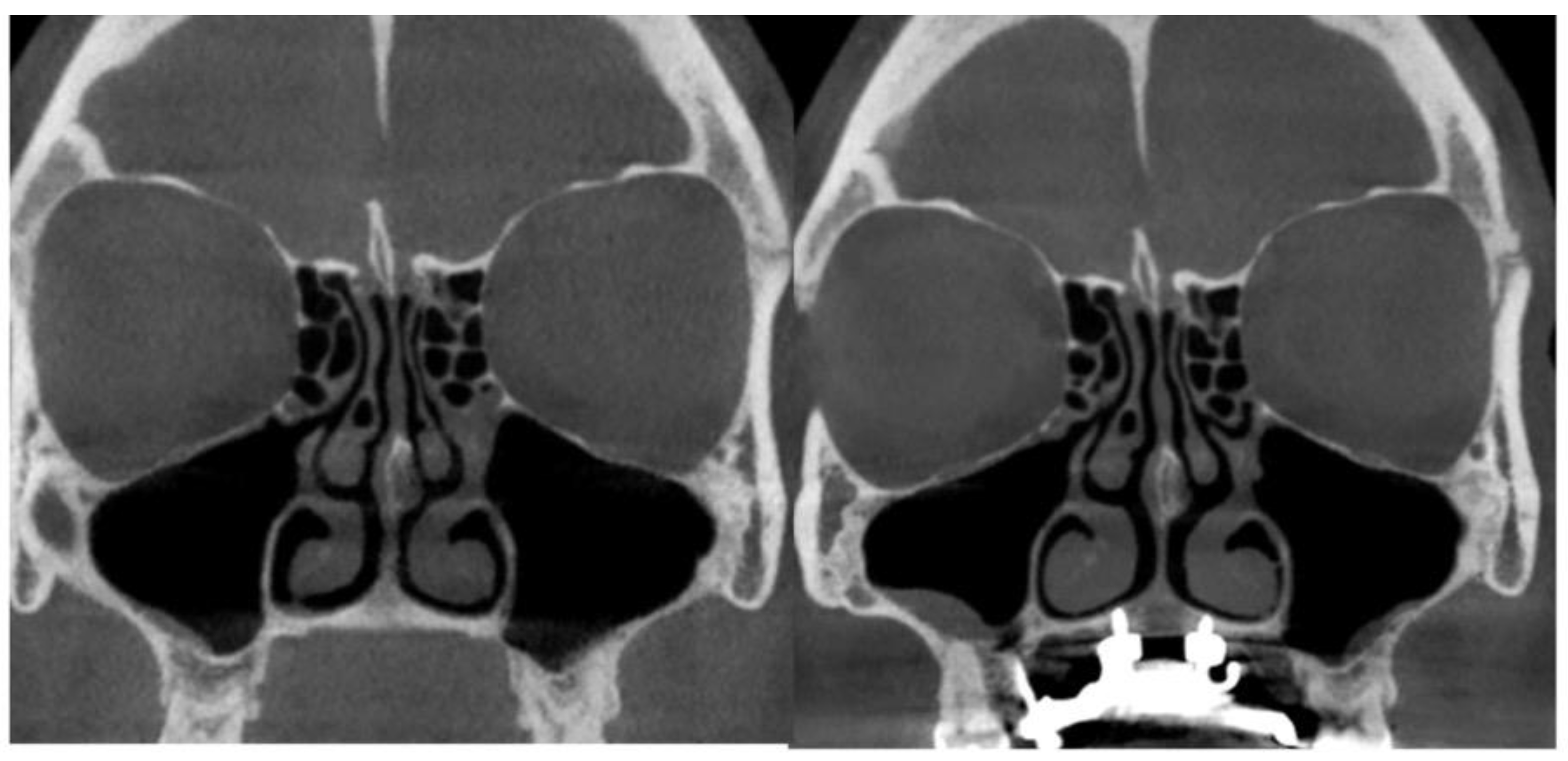
2.5. Case B: Guide-Assisted Midpalatal Piezocorticotomy
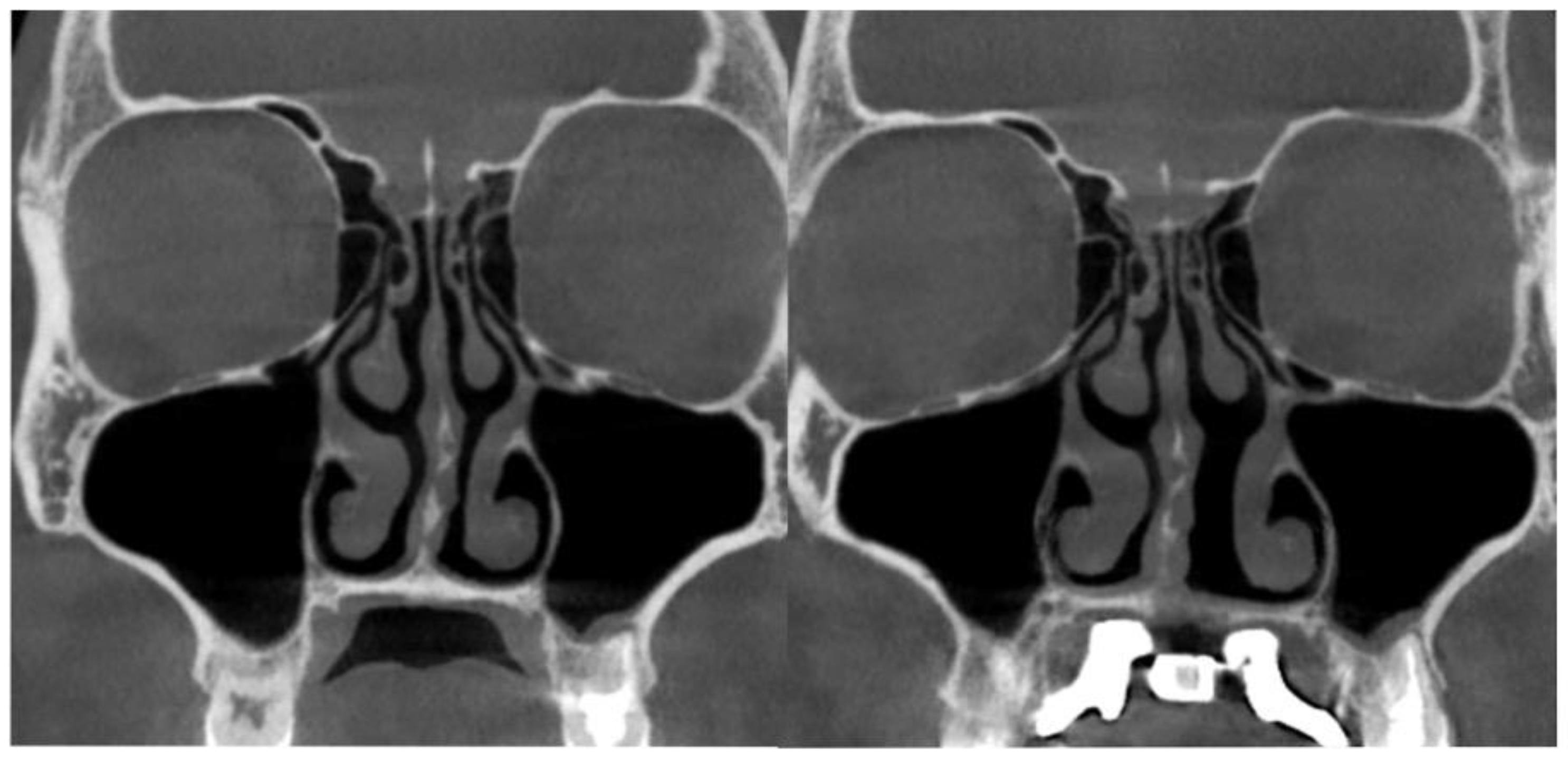
A 35-year-old female underwent midfacial skeletal expansion using a custom-milled MARPE appliance. The MARPE installation was preceded by guide-assisted midpalatal piezocorticotomy under local anesthesia. Incisions reached the palatine bone and maxillary crests, with proprioceptive feedback used to confirm cortical plate penetration. After 1 week of healing, MARPE activation began at one turn/day over 9 weeks, achieving 5.3 mm of maxillary crest-to-crest separation. Pre- and post-expansion CBCT images in coronal projection are shown in
Figure 7.
The case demonstrated precise 5.3 mm midpalatal suture separation and a post-expansion nasal septum position centered relative to the nasal base (
Figure 8).
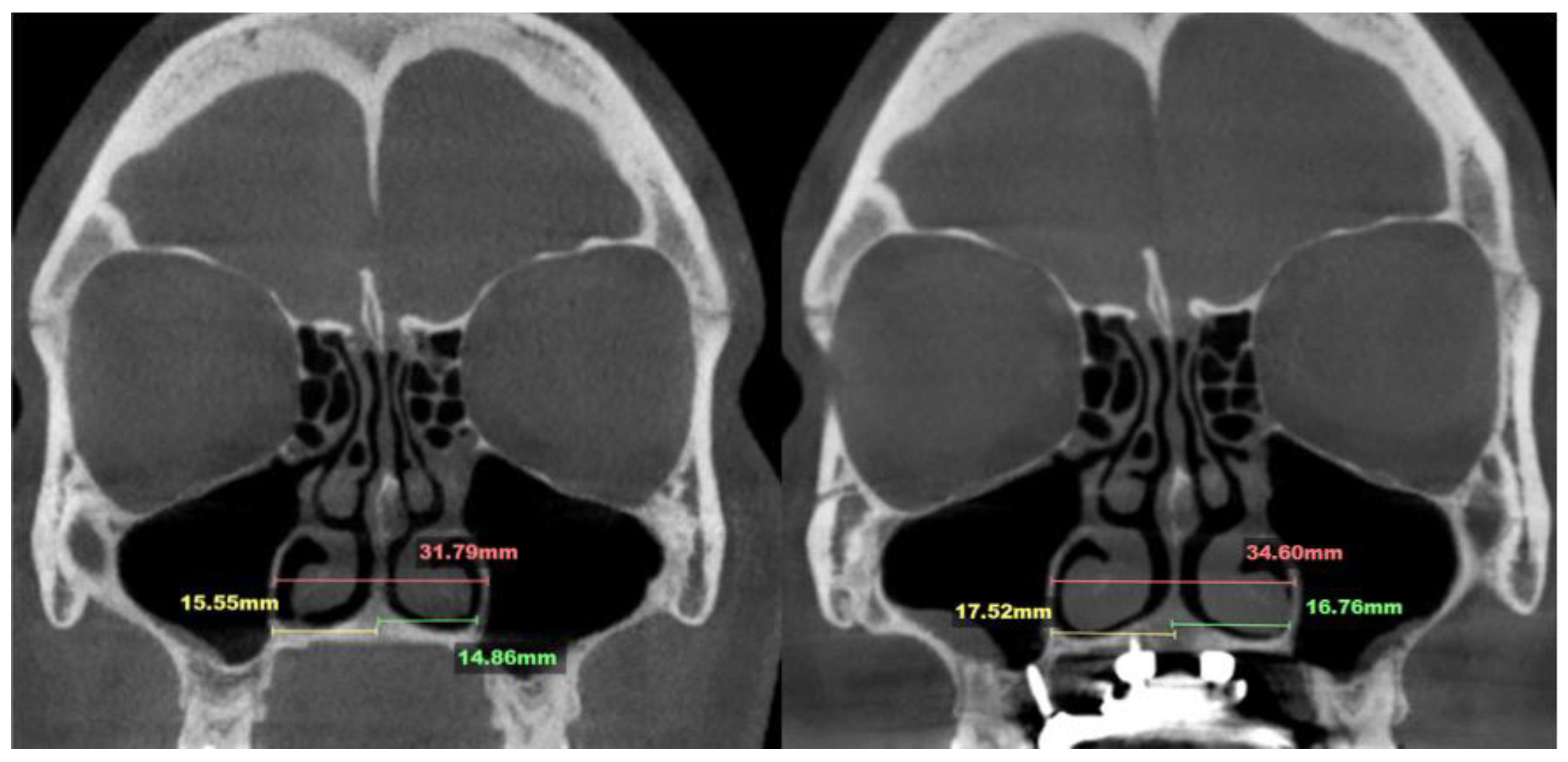
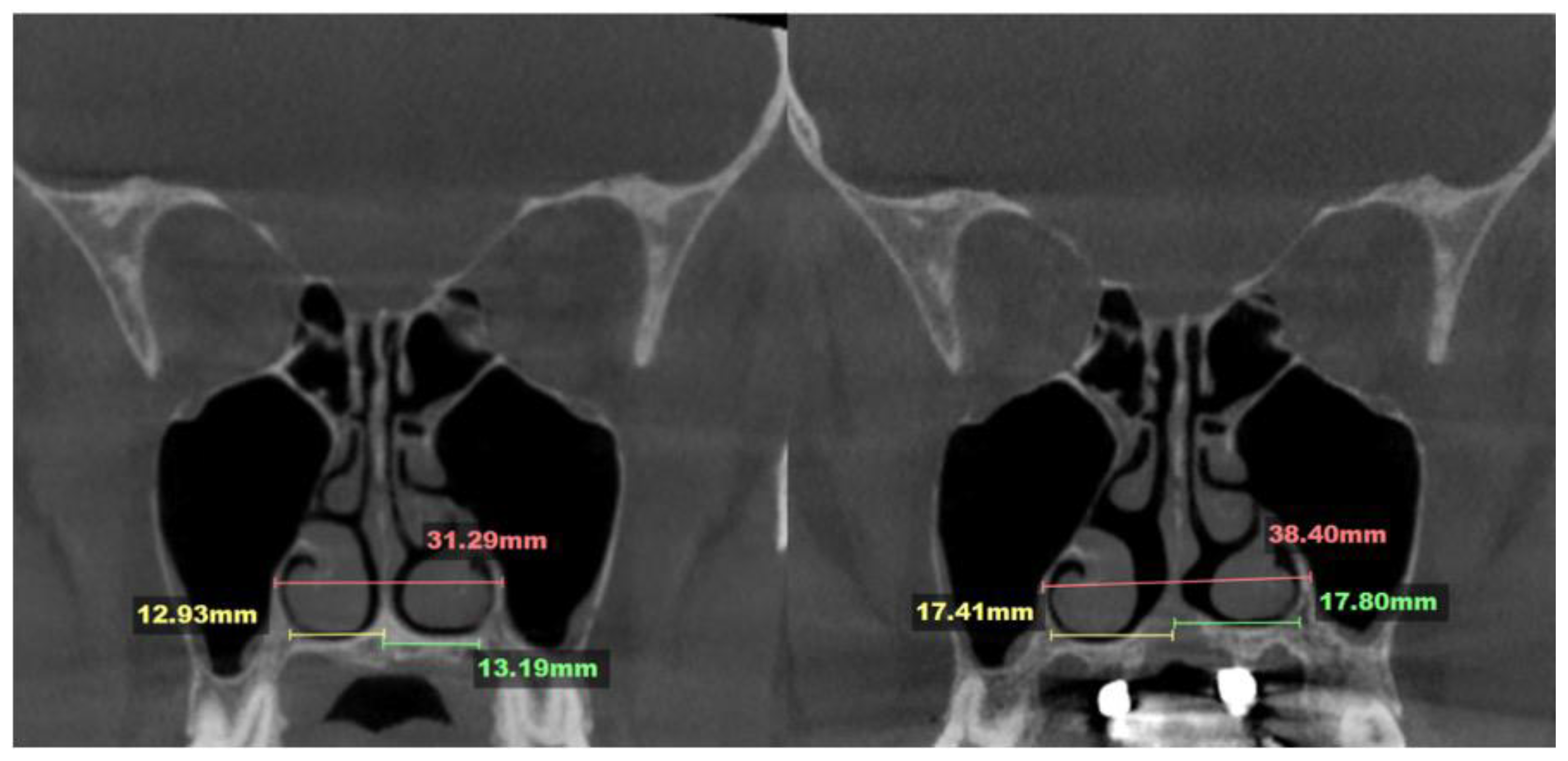
2.6. Case C: Bilateral Posterior Crossbite with Guide-Assisted Expansion
A 33-year-old male presented with an anterior open bite and bilateral posterior crossbite. He underwent MARPE expansion with guide-assisted midpalatal piezocorticotomy, performed under local anesthesia with topical and infiltrative applications. Antibiotic premedication was administered 1 hour before the procedure (
Figure 9).
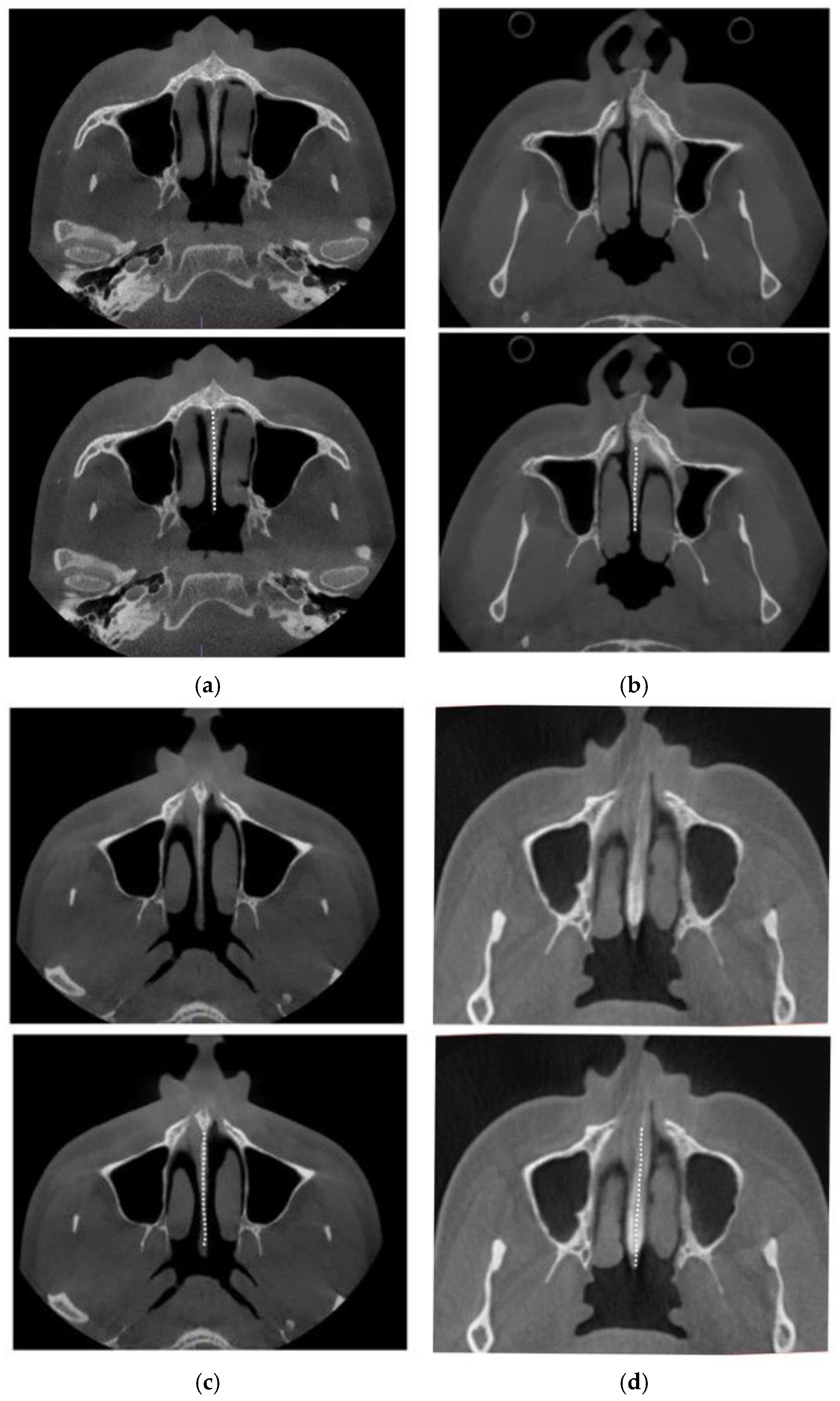
Expansion followed a one turn/day protocol for over 10 weeks, achieving a total crest-to-crest separation of 8.4 mm. The nasal septum remained centered, and nasal passages showed a relatively even increase in volume. The septum maintained alignment with surrounding structures, including the ethmoid cells, maxillary sinuses, and nasal cavity base (
Figure 10).
2.7. Case D: Midfacial Asymmetry Correction with Guided Expansion
A 40-year-old female presented with maxillary roll, with the left occlusal plane positioned inferior to the right. CBCT confirmed the palatal plane was not parallel to the orbital plane.
Midpalatal guide-assisted piezocorticotomy and MARPE insertion were performed in a single appointment, including antibiotic premedication and local anesthesia via topical and infiltrative methods. Activation began in week 2, after the initial mucosal healing period, and continued for 10 weeks (
Figure 11).
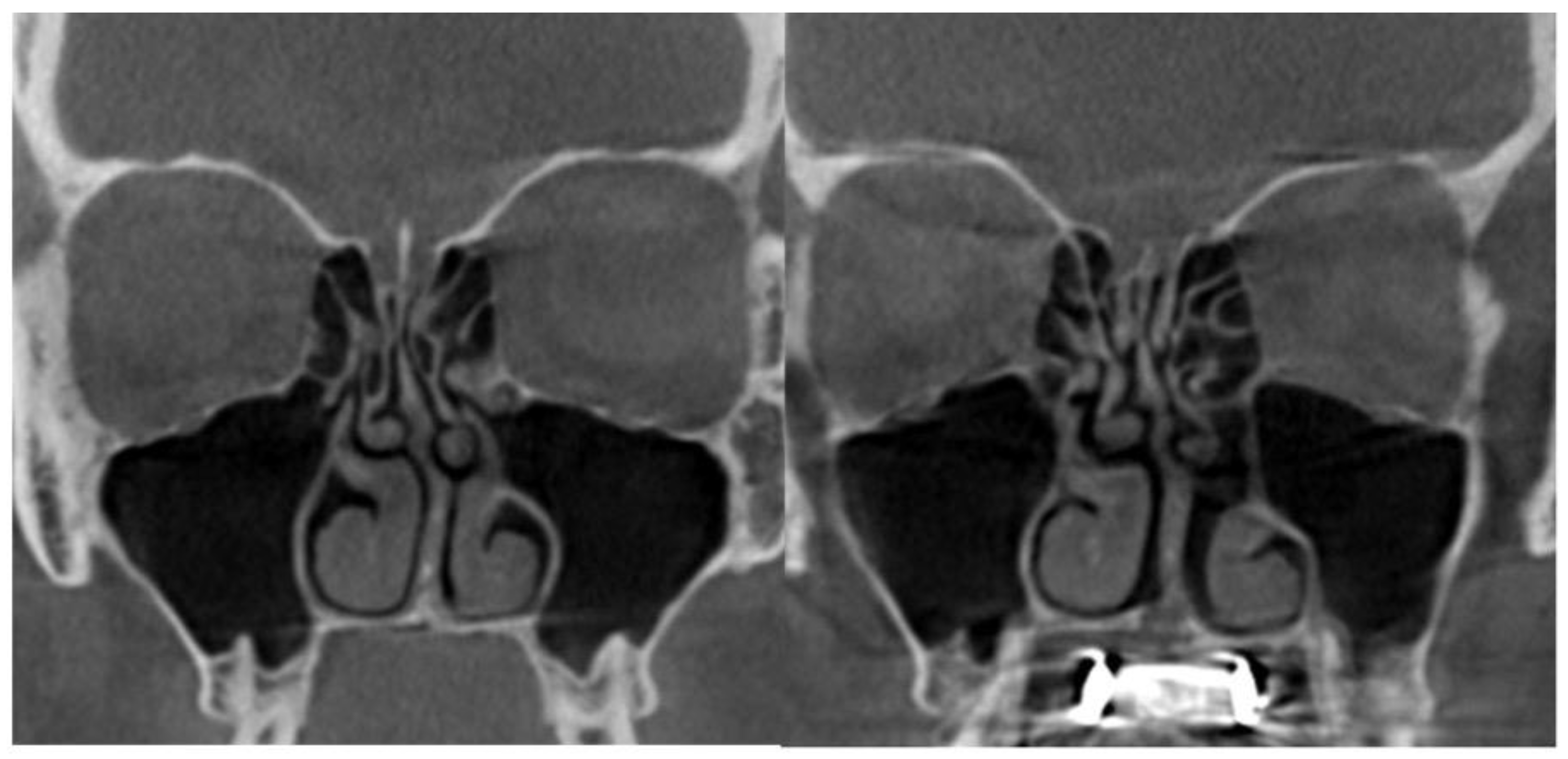
The total expansion exceeded 7 mm, resulting in symmetrical nasal base separation and alignment parallel to the original maxillary base plane inclination (
Figure 12).
3. Discussion
The skeletal component of maxillary expansion was first described by Haas and Isaacson [
8,
9]. Isaacson conducted measurements using a built-in dynamometer in a fixed skeletal expander appliance and demonstrated that the forces generated by the appliance, under consistent activation regimens, ranged from 2.5 to 10 pounds. He concluded that the primary resistance to skeletal activation originated from the peri-maxillary sutures rather than the midpalatal suture itself. He also emphasized that appliance activation may vary depending on the patient’s age and midpalatal suture resistance. Isaacson described retention as highly dependent on surrounding skeletal structures rather than tooth-borne retention alone. The key to retention lies in neutralizing external forces from peri-maxillary sutures, muscles, and ligaments, which otherwise could reduce the volume of newly formed bone. The study concluded that lower force levels with low load-deflection rates are preferable for expansion mechanisms.
A study by Weissheimer et al.[
10] comparing the effects of Haas and Hyrax expanders for skeletal maxillary expansion in individuals aged 9–14 supported previous findings of a V-shaped midpalatal suture separation pattern. This pattern was attributed to the resistance from the medial and lateral pterygoid plates of the sphenoid bone to the expansion-induced tipping moment. Both expander types achieved similar skeletal gains of approximately 40%, with the remaining 60% attributed to dentoalveolar changes. Notably, this study reported statistically greater skeletal expansion with the Haas expander compared to the Hyrax, contrary to earlier findings [
11].
The literature lacks consensus on adult midpalatal expansion techniques, including appliance types and activation protocols. Most studies indicate beneficial changes in upper airway volume and minimum cross-sectional area [
12,
13,
14]. A systematic review and meta-analysis by Kapetanovic et al. [
15] on MARPE effects in adults found skeletal width increases ranging from 1.63 to 3.03 mm and dentoalveolar increases from 5.50 to 7.59 mm, with significant dental tipping. A study by Tang et al. with similar skeletal separation demonstrated that MARPE outcomes in young adults were relatively stable. Greater stability was observed in individuals with thicker palatal bone and shallower palatal vaults [
16]. Naveda et al. measured midpalatal bone density 16 months post-MARPE in young adults [
17] , finding that the anterior region exhibited the highest bone repair rate. Specifically, 80.95% of the midpalatal suture length was repaired in all patients, with the middle third showing the least ossification. Similar findings were reported by Ceschi et al.[
18] who suggested that older patients may require longer retention periods for full ossification of the midpalatal suture.
Laudemann et al. reported a positive correlation between SARPE with pterygomaxillary disjunction and posterior skeletal and alveolar expansion [
19].
To the best of our knowledge, asymmetric expansion has not been addressed in previous studies.
Recent advances in airway-focused orthodontics have shown that nasal base expansion—particularly at the levels of the anterior nasal spine (ANS), posterior nasal spine (PNS), and piriform foramen—can significantly increase airway volumes in the nasal, nasopharyngeal, oropharyngeal, and hypopharyngeal regions [
14,
19,
20]. However, not all MARPE designs consistently achieve separation at both the ANS and PNS [
19].
The technique described below has consistently produced midpalatal suture separation at both the ANS and PNS, along with disjunction of the pterygomaxillary sutures. These outcomes result in forward and downward movement of the maxillary complex.
The current clinical case series presents a novel 3D-designed and 3D-printed midpalatal piezocorticotomy guide that enhances MARPE midfacial expansion through guided midpalatal piezocorticotomy.
Adult MARPE expansion—especially in males over 18 years—has historically been considered questionable, with alternative techniques often recommended to improve nasal airflow and address nasal breathing as a component of sleep-disordered breathing. For this age group, variations of piezocorticotomy have been suggested [
21].
The technique described in this article has proven effective and efficient for midfacial expansion in adult males and females over 18, achieving maxillary crest-to-crest separation exceeding 5 mm. Benefits of using the guided midpalatal piezocorticotomy include prevention of unilateral nasal septum displacement, asymmetric nasal cavity and volume expansion, maxillary base roll, and vertical discrepancies of the maxillary occlusal plane.
Rationale for the Use of the Midpalatal Piezocorticotomy Guide
Unfortunately, current research lacks prospective studies comparing adult MARPE expansion with and without midpalatal piezocorticotomy. As a result, the topic remains primarily within the domain of clinical observation, debate, and discussion.
Our clinical observations indicate that when midpalatal separation—measured at the level of the maxillary crest above the first molars—exceeds 5 mm of crest-to-crest distance, the following complications are frequently observed:
Asymmetric expansion with residual attachment of the nasal septum unilaterally to the maxillary crestal bone (
Figure 5,6);
Diagonal fractures of the palatine bone extending from the distal margin of the palatal process of the maxillary bone unilaterally, often associated with pain and tension;
Asymmetric displacement of the nasal base floor with unilateral downward and outward movement (
Figure 5,6)
Downward inclination and displacement of the alveolar process on the ipsilateral side (
Figure 5,6);
Unilateral soft tissue shift, including nasal ala and corner of the mouth displacement toward the side of unattached separation.
The midpalatal piezocorticotomy guide is designed to mitigate most of these complications. It accounts for each patient’s unique anatomy to enhance both the efficiency and symmetry of maxillary expansion. Key contributing anatomical variables include the position and symmetry of the nasal septum and variability in palatal bone thickness.
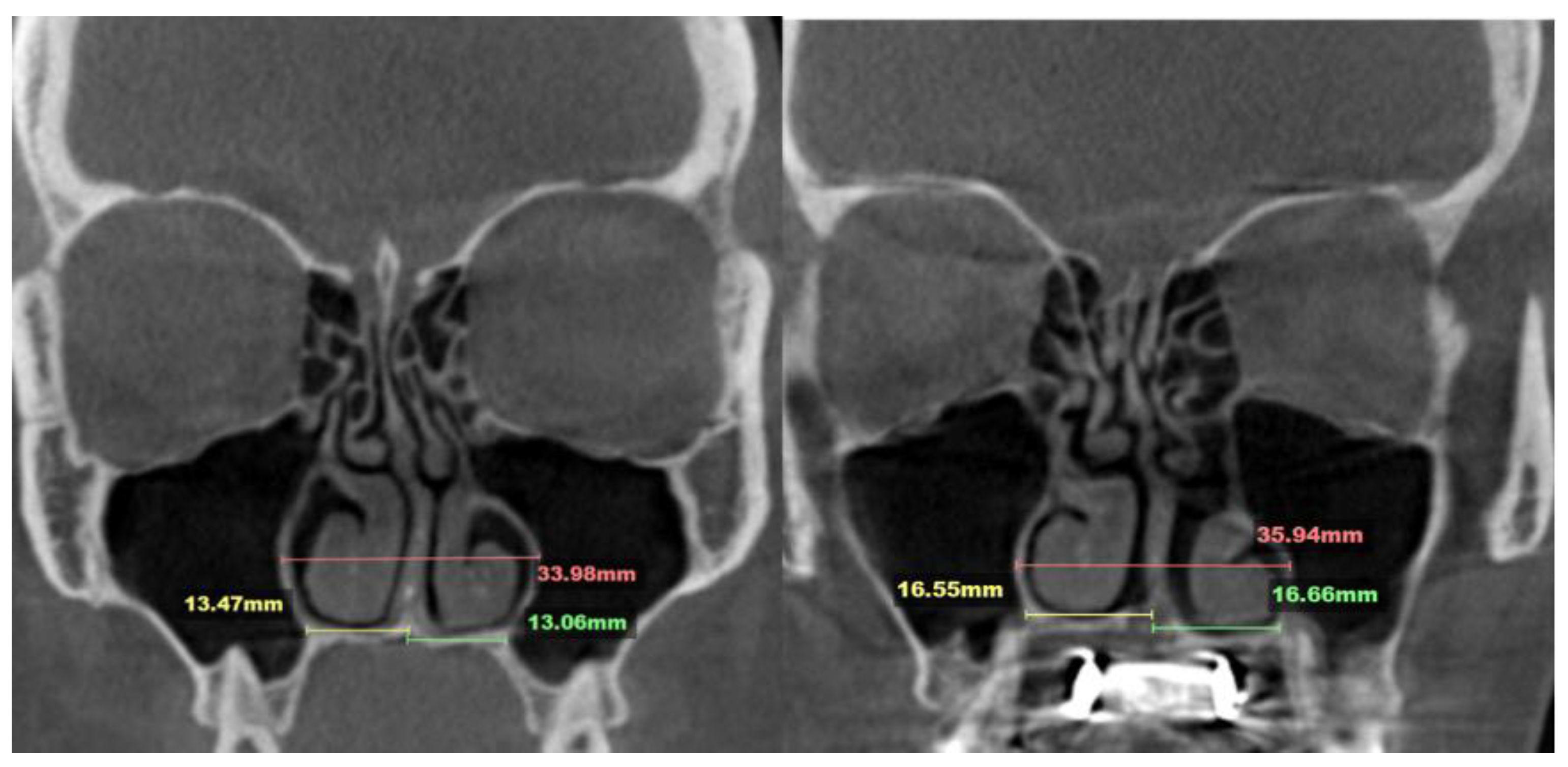
The nasal septum’s attachment projection is best visualized in axial CBCT views of the maxillofacial region.
Figure 13 illustrates variations in septal shape and attachment.
As shown in
Figure 13, nasal septum variability extends beyond the coronal plane and poses additional challenges when evaluated in the axial plane. This complexity contributed to the asymmetric nasal septum displacement observed in Case A.
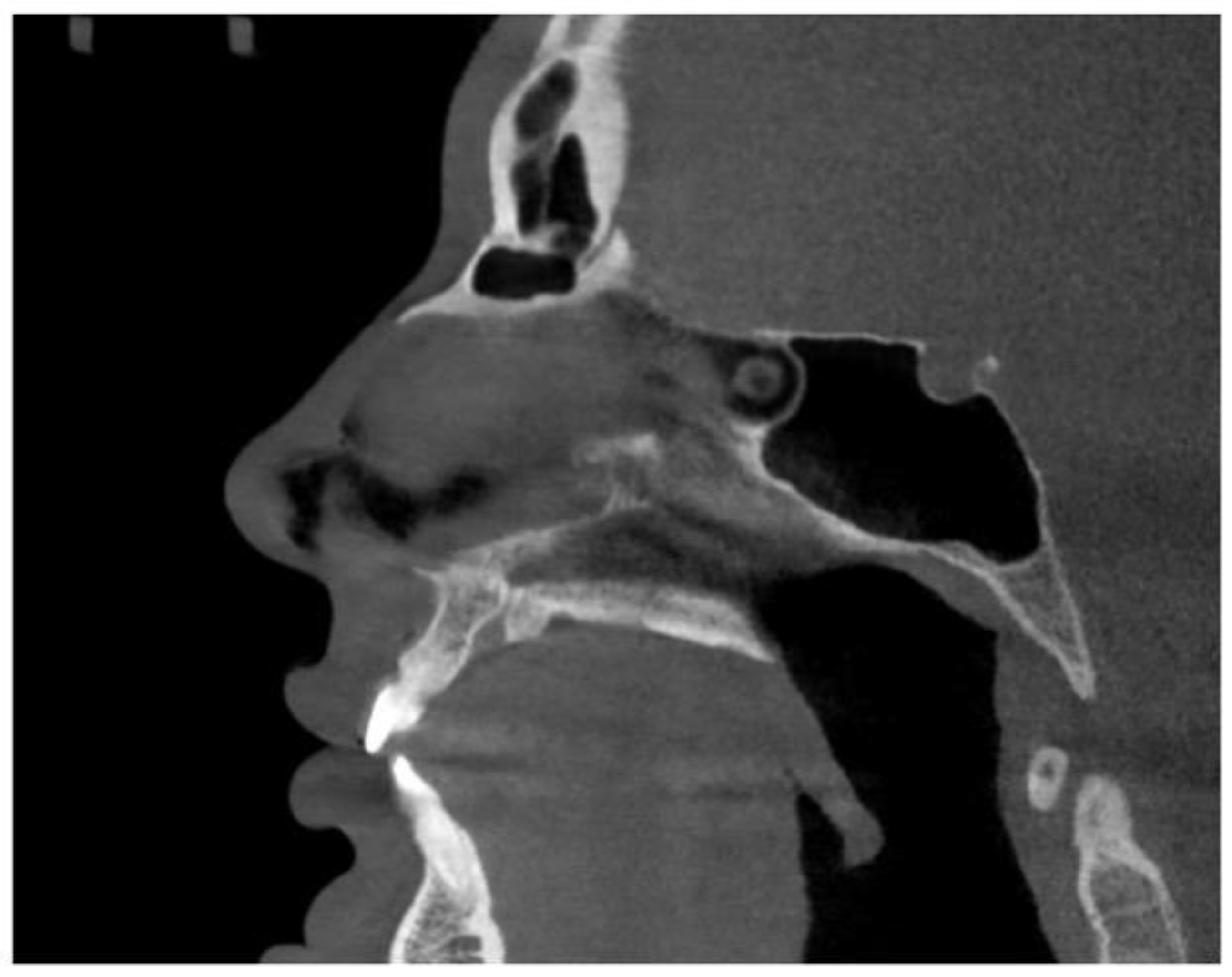
The depth of the piezocorticotomy incisions involves the full thickness of the palatine bone and the maxillary crest in the corresponding regions, as shown in the sagittal view (
Figure 14).
Case A, which involved midpalatal separation without guided piezocorticotomy, represents a typical outcome of blind piezocorticotomy. In our experience, such cases consistently lack expansion symmetry. Common findings include unilateral nasal septum attachment, asymmetrical lateralization of the nasal walls, uneven bone apposition on the contralateral side of the septum, vertical drop of the dental-alveolar complex, and other complications.
4. Conclusions
The novel midpalatal piezocorticotomy guide represents a significant advancement in adult midfacial expansion using the MARPE appliance. Guided piezocorticotomy of the midpalatal suture not only helps prevent major side effects but also improves the predictability and symmetry of maxillary expansion in adult male and female patients.
Funding
No funding is reported for this study.
Institutional Review Board Statement
Ethical review and approval were waived for this study due to the retrospective nature of the study and the exclusive use of fully de-identified data.
Informed Consent Statement
All patients provide informed consent for the use of their de-identified data prior to treatment.
Data Availability Statement
We encourage all authors of articles published in MDPI journals to share their research data. In this section, please provide details regarding where data supporting reported results can be found, including links to publicly archived datasets analyzed or generated during the study. Where no new data were created, or where data is unavailable due to privacy or ethical restrictions, a statement is still required. Suggested Data Availability Statements are available in section “MDPI Research Data Policies” at
https://www.mdpi.com/ethics.
Conflicts of Interest
The authors report there are no competing interests to declare.
References
- Kapetanović A, Theodorou CI, Bergé SJ, et al. Efficacy of miniscrew-assisted rapid palatal expansion (MARPE) in late adolescents and adults: a systematic review and meta-analysis. Eur J Orthod. 2021;43:313–323. [CrossRef]
- Tanaka O, Mota-Júnior SL. MARPE as an adjunct to orthodontic treatment. Dent Press J Orthod. 2023;27:e22bbo6. [CrossRef]
- Chun JH, de Castro ACR, Oh S, et al. Skeletal and alveolar changes in conventional rapid palatal expansion (RPE) and miniscrew-assisted RPE (MARPE): a prospective randomized clinical trial using low-dose CBCT. BMC Oral Health. 2022;22:114. [CrossRef]
- Brunetto DP, Sant’Anna EF, Machado AW, et al. Non-surgical treatment of transverse deficiency in adults using microimplant-assisted rapid palatal expansion (MARPE). Dent Press J Orthod. 2017;22:110–125. [CrossRef]
- Brunetto DP, Moschik CE, Dominguez-Mompell R, et al. Mini-implant assisted rapid palatal expansion (MARPE) effects on adult obstructive sleep apnea (OSA) and quality of life: a multi-center prospective controlled trial. Prog Orthod. 2022;23:3. [CrossRef]
- Ventura V, Botelho J, Machado V, et al. Miniscrew-assisted rapid palatal expansion (MARPE): an umbrella review. J Clin Med. 2022;11:1287. [CrossRef]
- Bud E, Vlasa A, Pacurar M, et al. A retrospective histological study on palatal and gingival mucosa changes during a rapid palatal expansion procedure. Biomedicines. 2023;11:3246. [CrossRef]
- Zimring JF, Isaacson RJ. Forces produced by rapid maxillary expansion. 3. Forces present during retention. Angle Orthod. 1965;35:178–186. [CrossRef]
- Handelman CS, Wang L, BeGole EA, et al. Nonsurgical rapid maxillary expansion in adults: report on 47 cases using the Haas expander. Angle Orthod. 2000;70:129–144. [CrossRef]
- Weissheimer A, de Menezes LM, Mezomo M, et al. Immediate effects of rapid maxillary expansion with Haas-type and hyrax-type expanders: a randomized clinical trial. Am J Orthod Dentofac Orthop Off Publ Am Assoc Orthod Its Const Soc Am Board Orthod. 2011;140:366–376. [CrossRef]
- Lione R, Ballanti F, Franchi L, et al. Treatment and posttreatment skeletal effects of rapid maxillary expansion studied with low-dose computed tomography in growing subjects. Am J Orthod Dentofac Orthop Off Publ Am Assoc Orthod Its Const Soc Am Board Orthod. 2008;134:389–392. [CrossRef]
- Altieri F, Cassetta M. Comparison of changes in skeletal, dentoalveolar, periodontal, and nasal structures after tooth-borne or bone-borne rapid maxillary expansion: a parallel cohort study. Am J Orthod Dentofac Orthop Off Publ Am Assoc Orthod Its Const Soc Am Board Orthod. 2022;161:e336–e344. [CrossRef]
- Oztürk M, Doruk C, Ozeç I, et al. Pulpal blood flow: effects of corticotomy and midline osteotomy in surgically assisted rapid palatal expansion. J Cranio-Maxillo-fac Surg Off Publ Eur Assoc Cranio-Maxillo-fac Surg. 2003;31:97–100. [CrossRef]
- Li J, Shi L, Zhang X, et al. Evaluating the effect of midpalatal corticotomy-assisted rapid maxillary expansion on the upper airway in young adults using computational fluid dynamics. J Zhejiang Univ Sci B. 2021;22:146–155. [CrossRef]
- Kapetanović A, Theodorou CI, Bergé SJ, et al. Efficacy of miniscrew-assisted rapid palatal expansion (MARPE) in late adolescents and adults: a systematic review and meta-analysis. Eur J Orthod. 2021;43:313–323. [CrossRef]
- Tang H, Liu P, Liu X, et al. Skeletal width changes after mini-implant-assisted rapid maxillary expansion (MARME) in young adults. Angle Orthod. 2021;91:301–306. [CrossRef]
- Naveda R, Dos Santos AM, Seminario MP, et al. Midpalatal suture bone repair after miniscrew-assisted rapid palatal expansion in adults. Prog Orthod. 2022;23:35. [CrossRef]
- Ceschi M, Riatti R, Di Leonardo B, et al. Skeletal expansion using a miniscrew-assisted rapid palatal expansion in a 50-year-old patient. Am J Orthod Dentofac Orthop Off Publ Am Assoc Orthod Its Const Soc Am Board Orthod. 2022;162:568–579. [CrossRef]
- Laudemann K, Santo G, Revilla C, et al. Assessment of surgically assisted rapid maxillary expansion regarding pterygomaxillary disjunction using thin volume-rendering technique: in variance analysis and in reliability, accuracy, and validity. J Oral Maxillofac Surg Off J Am Assoc Oral Maxillofac Surg. 2011;69:2631–2643. [CrossRef]
- Quo SD, Hyunh N, Guilleminault C. Bimaxillary expansion therapy for pediatric sleep-disordered breathing. Sleep Med. 2017;30:45–51. [CrossRef]
- Yoon A, Gozal D, Kushida C, et al. A roadmap of craniofacial growth modification for children with sleep-disordered breathing: a multidisciplinary proposal. Sleep. 2023 14;46:zsad095.
Figure 1.
MARPE expander before and after expansion. A – Guided midpalatal piezocorticotomy appointment with MARPE installation. B – MARPE expansion completed, midpalatal piezocorticotomy incision healed, MARPE framework was adjusted with reducing the tooth-borne components.
Figure 1.
MARPE expander before and after expansion. A – Guided midpalatal piezocorticotomy appointment with MARPE installation. B – MARPE expansion completed, midpalatal piezocorticotomy incision healed, MARPE framework was adjusted with reducing the tooth-borne components.
Figure 2.
A. Schematic image of the midpalatal piezoguide: 1 – occlusal splint, 2- baseplate, 3-connector, 4 – piezocortical incision notches. B. Piezoguide fitted on the model.
Figure 2.
A. Schematic image of the midpalatal piezoguide: 1 – occlusal splint, 2- baseplate, 3-connector, 4 – piezocortical incision notches. B. Piezoguide fitted on the model.
Figure 3.
Schematic image of the palatal anatomy: 1- alveolar process of the maxillary arch with the dental arch, 2- incisive foramen, 3- midpalatal suture, 4 – transverse suture, 5 – posterior nasal spine, 6 – posterior crest of the palatine bone, 7 – palatine bone, 8 – palatal process of the maxillary bone.
Figure 3.
Schematic image of the palatal anatomy: 1- alveolar process of the maxillary arch with the dental arch, 2- incisive foramen, 3- midpalatal suture, 4 – transverse suture, 5 – posterior nasal spine, 6 – posterior crest of the palatine bone, 7 – palatine bone, 8 – palatal process of the maxillary bone.
Figure 4.
Schematic image of the location of piezocortical incision: 1- alveolar process of the maxillary arch with the dental arch, 2- incisive foramen, 3- midpalatal suture, 4 – transverse suture, 5 – posterior nasal spine, 6 – posterior crest of the palatine bone, 7 – palatine bone, 8 – palatal process of the maxillary bone, 9 – incision location (indicated by a dashed line).
Figure 4.
Schematic image of the location of piezocortical incision: 1- alveolar process of the maxillary arch with the dental arch, 2- incisive foramen, 3- midpalatal suture, 4 – transverse suture, 5 – posterior nasal spine, 6 – posterior crest of the palatine bone, 7 – palatine bone, 8 – palatal process of the maxillary bone, 9 – incision location (indicated by a dashed line).
Figure 5.
Before (A) and after (B) MARPE Midfacial expansion without guide-assisted midpalatal piezocorticotomy. The Expansion of 10.5 mm was achieved over the 12 weeks of expansion with 1 turn/day.
Figure 5.
Before (A) and after (B) MARPE Midfacial expansion without guide-assisted midpalatal piezocorticotomy. The Expansion of 10.5 mm was achieved over the 12 weeks of expansion with 1 turn/day.
Figure 6.
Pre- and post-MARPE expansion measurements with the blind midpalatal piezocorticotomy. A. Nasal base measurements before MARPE expansion after blind midpalatal piezocorticitomy: lateral nasal width equals 32.88 mm, the right and left septum-lateral walls width equal 14.80 and 15.79 mm, correspondingly. B. Post -MARPE expansion measurements: lateral nasal width equals 39.96 mm, right and left septum-layteral wall widths resulted in 16.24 and 21.90 mm, respectively.
Figure 6.
Pre- and post-MARPE expansion measurements with the blind midpalatal piezocorticotomy. A. Nasal base measurements before MARPE expansion after blind midpalatal piezocorticitomy: lateral nasal width equals 32.88 mm, the right and left septum-lateral walls width equal 14.80 and 15.79 mm, correspondingly. B. Post -MARPE expansion measurements: lateral nasal width equals 39.96 mm, right and left septum-layteral wall widths resulted in 16.24 and 21.90 mm, respectively.
Figure 7.
Before and after MARPE Midfacial expansion with guide-assisted midpalatal piezocorticotomy. The Expansion of 5.3 mm was achieved over the 9 weeks of expansion with 1 turn/day.
Figure 7.
Before and after MARPE Midfacial expansion with guide-assisted midpalatal piezocorticotomy. The Expansion of 5.3 mm was achieved over the 9 weeks of expansion with 1 turn/day.
Figure 8.
Pre- and post-MARPE expansion measurements with the blind midpalatal piezocorticotomy. A. Nasal base measurements before MARPE expansion after guided midpalatal piezocorticitomy: lateral nasal width equals 31.79 mm, the right and left septum-lateral walls width equal 15.55 and 14.86 mm, correspondingly. B. Post -MARPE expansion measurements: lateral nasal width equals 34.60 mm, right and left septum-lateral wall widths resulted in 17.52 and 16.76 mm, respectively.
Figure 8.
Pre- and post-MARPE expansion measurements with the blind midpalatal piezocorticotomy. A. Nasal base measurements before MARPE expansion after guided midpalatal piezocorticitomy: lateral nasal width equals 31.79 mm, the right and left septum-lateral walls width equal 15.55 and 14.86 mm, correspondingly. B. Post -MARPE expansion measurements: lateral nasal width equals 34.60 mm, right and left septum-lateral wall widths resulted in 17.52 and 16.76 mm, respectively.
Figure 9.
Before (A) and after (B) MARPE Midfacial expansion with guide-assisted midpalatal piezocorticotomy. The Expansion of 8.4 mm was achieved over the 10 weeks of expansion with 1 turn/day.
Figure 9.
Before (A) and after (B) MARPE Midfacial expansion with guide-assisted midpalatal piezocorticotomy. The Expansion of 8.4 mm was achieved over the 10 weeks of expansion with 1 turn/day.
Figure 10.
Pre- and post-MARPE expansion measurements with the blind midpalatal piezocorticotomy. A. Nasal base measurements before MARPE expansion after guided midpalatal piezocorticitomy: lateral nasal width equals 31.29 mm, the right and left septum-lateral walls width equal 12.93 and 13.19 mm, correspondingly. B. Post -MARPE expansion measurements: lateral nasal width equals 38.40 mm, right and left septum-lateral wall widths resulted in 17.41 and 17.80 mm, respectively.
Figure 10.
Pre- and post-MARPE expansion measurements with the blind midpalatal piezocorticotomy. A. Nasal base measurements before MARPE expansion after guided midpalatal piezocorticitomy: lateral nasal width equals 31.29 mm, the right and left septum-lateral walls width equal 12.93 and 13.19 mm, correspondingly. B. Post -MARPE expansion measurements: lateral nasal width equals 38.40 mm, right and left septum-lateral wall widths resulted in 17.41 and 17.80 mm, respectively.
Figure 11.
Before (A) and after (B) MARPE Midfacial expansion with guide-assisted midpalatal piezocorticotomy. The Expansion of 7.5 mm was achieved over the 9 weeks of expansion with 1 turn/day.
Figure 11.
Before (A) and after (B) MARPE Midfacial expansion with guide-assisted midpalatal piezocorticotomy. The Expansion of 7.5 mm was achieved over the 9 weeks of expansion with 1 turn/day.
Figure 12.
Pre- and post-MARPE expansion measurements with the blind midpalatal piezocorticotomy. A. Nasal base measurements before MARPE expansion after guided midpalatal piezocorticitomy: lateral nasal width equals 33.98 mm, the right and left septum-lateral walls width equal 13.47 and 13.06 mm, correspondingly. B. Post -MARPE expansion measurements: lateral nasal width equals 35.94 mm, right and left septum-lateral wall widths resulted in 16.55 and 16.66 mm, respectively.
Figure 12.
Pre- and post-MARPE expansion measurements with the blind midpalatal piezocorticotomy. A. Nasal base measurements before MARPE expansion after guided midpalatal piezocorticitomy: lateral nasal width equals 33.98 mm, the right and left septum-lateral walls width equal 13.47 and 13.06 mm, correspondingly. B. Post -MARPE expansion measurements: lateral nasal width equals 35.94 mm, right and left septum-lateral wall widths resulted in 16.55 and 16.66 mm, respectively.
Figure 13.
Base of the nasal septum of a 40 yo female (A), 35 yo male (B), 23 yo male (C) , 35 yo female (D) in the axial plane (before intervention).
Figure 13.
Base of the nasal septum of a 40 yo female (A), 35 yo male (B), 23 yo male (C) , 35 yo female (D) in the axial plane (before intervention).
Figure 14.
Sagittal midline view of the hard palate with the incisive canal cross-section.
Figure 14.
Sagittal midline view of the hard palate with the incisive canal cross-section.
|
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2025 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (http://creativecommons.org/licenses/by/4.0/).