Submitted:
04 June 2025
Posted:
05 June 2025
You are already at the latest version
Abstract
Keywords:
1. Introduction
1.1. Self-Injurious Behaviors in Children and Adolescents with ASD
1.2. Prevalence and Relevance of the Problem
1.3. Treatment
1.4. Review of the State of Art
1.5. Limitations and Gaps
1.6. The Current Study
2. Materials and Methods
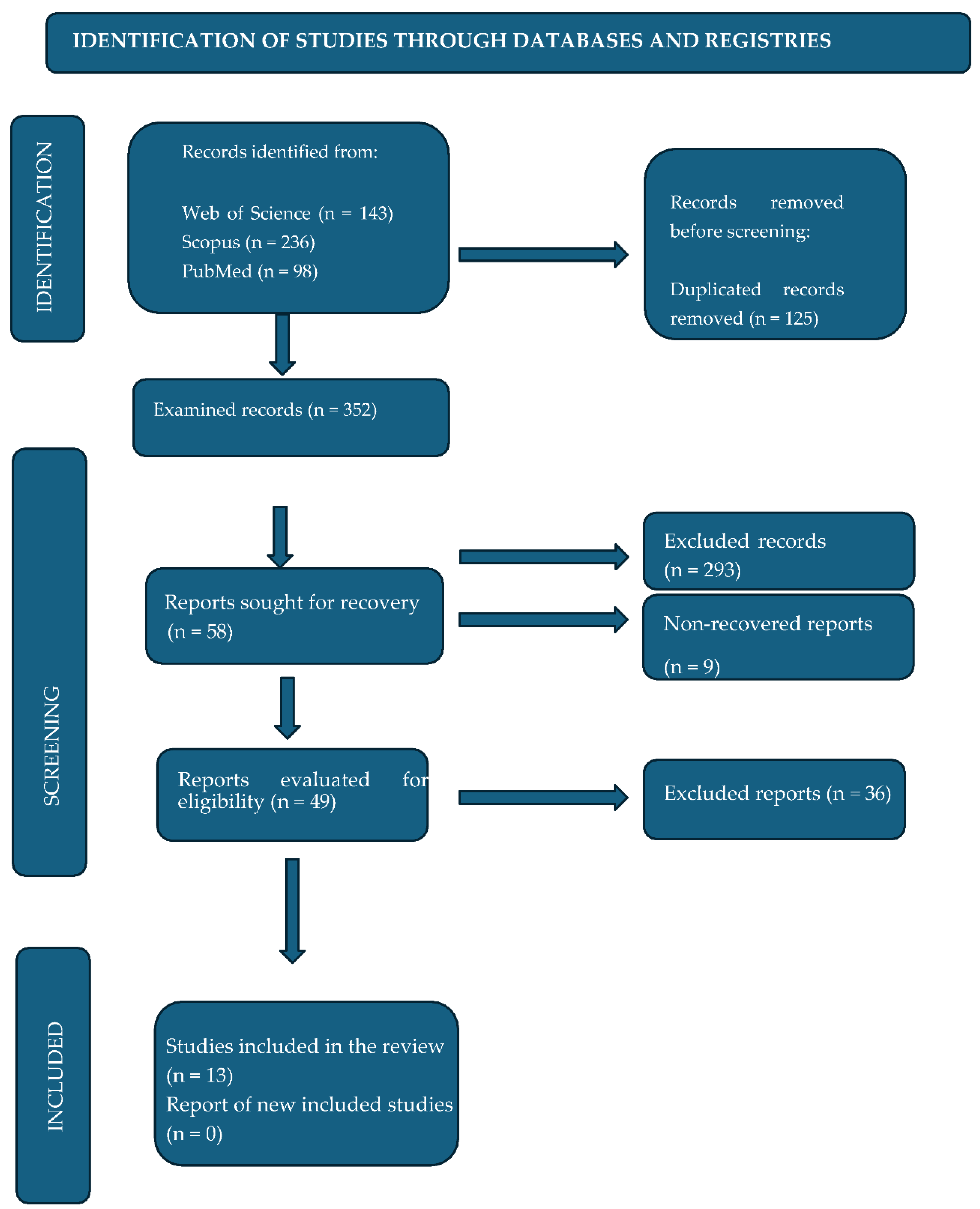
2.1. Selection of Studies
2.2. Extraction of Studies
3. Results
3.1. Study and Sample Characteristics
3.2. Overview of Interventions
3.2.1. Identified Limitations
3.2.2. Characteristics of the Interventions
3.2.3. Effectiveness of Interventions
4. Discussion
Author Contributions
Funding
Institutional Review Board Statement
Acknowledgments
Conflicts of Interest
References
- Celis Alcalá, G., & Ochoa Madrigal, M. G. (2022). Trastorno del espectro autista (TEA). Revista de la Facultad de Medicina(México), 65(1),7–20. [CrossRef]
- American Psychiatric Association (2013). Diagnostic and statistican manual of mental disorders (5th ed.). [CrossRef]
- Hervas, A. (2017). Psicofarmacología del TEA. En C. Soutullo (Ed.), Guía Esencial de Psicofarmacología del niño y del adolescente (2ª ed., pp. 200-220). Editorial Médica Panamericana.
- Tudela Torras, M., & Abad Más, L. (2019). Reducción de las conductas autolesivas y autoestimulatorias disfuncionales en los trastornos del espectro del autismo a través de la terapia ocupacional. Medicina (Buenos Aires), 79(1, Supl. 1), 38–43. https://www.scielo.org.ar/scielo.php?script=sci_arttext&pid=S0025-76802019000200009.
- Villarroel, G., Jerez, C., Montenegro, M., Montes, A., M., Mirko, I. M., & Silva, I. (2013). Conductas autolesivas no suicidas en la práctica clínica: Primera parte: conceptualización y diagnóstico. Revista Chilena de Neuro-Psiquiatría, 51(1), 38-45.
- Alakhzami, M., & Chitiyo, M. (2022). Using functional communication training to reduce self-injurious behavior for individuals with autism spectrum disorder. Journal of Autism and Developmental Disorders, 52(8), 3586–3597. [CrossRef]
- Matson, J. L., & Lovullo, S. V. (2008). A review of behavioral treatments for self-injurious behaviors of persons with autism spectrum disorders. Behavior Modification, 32(1), 61–76. [CrossRef]
- Erturk, B., Machalicek, W., & Drew, C. (2018). Self-injurious behavior in children with developmental disabilities: A systematic review of behavioral intervention literature. Behavior Modification, 42(4), 498–542. [CrossRef]
- Schaaf, R. C., Benevides, T., Leiby, B., Hunt, J., van Hooydonk, E., Faller, P., Mailloux, Z., & Kelly, D. (2013). An intervention for sensory difficulties in children with autism: A randomized trial. Journal of Autism and Developmental Disorders, 44(7), 1493–1506. [CrossRef]
- Iffland, M., Livingstone, N., Jorgensen, M., Hazell, P., & Gillies, D. (2023). Pharmacological interventions for irritability, aggression, and self-injury in autism spectrum disorder. Cochrane Database of Systematic Reviews, 2023(10), CD011769. [CrossRef]
- Fernández-Menéndez, E., Piqueras, J., & Soto-Sanz, V. (2022). Intervenciones cognitivo-conductuales para reducir conductas autolesivas en niños y jóvenes con TEA: Una revisión sistemática. Revista de Psicología Clínica con Niños y Adolescentes, 84–91. [CrossRef]
- World Health Organization (2023, November 15). Autism spectrum disorders. https://www.who.int/news-room/fact-sheets/detail/autism-spectrum-disorders.
- Fonseca-Pedrero, E., Pérez-Álvarez, M., Al-Halabí, S., Inchausti, F., López-Navarro, E. R., Muñiz & Montoya-Castilla, I. (2021). Tratamientos psicológicos empíricamente apoyados para la infancia y adolescencia: Estado de la cuestión. Psicothema, 33(3), 386–398. [CrossRef]
- Kanzari, C., Hawani, A., Ayed, K. B., Mrayeh, M., Marsigliante, S., & Muscella, A. (2025). The impact of a music-and movement-based intervention on motor competence, social engagement, and behavior in children with autism spectrum disorder. Children, 12(1), 87. [CrossRef]
- Flujas-Contreras, J. M., Chávez-Askins, M., & Gómez, I. (2023). Efectividad de las intervenciones psicológicas en Trastorno del Espectro Autista: una revisión sistemática de meta-análisis y revisiones sistemáticas. Revista de Psicología Clínica con Niños y Adolescentes, 10(1), 99-115. [CrossRef]
- Boesch, M. C., Taber-Doughty, T., Wendt, O., & Smalts, S. (2015). Using a behavioral approach to decrease self-injurious behavior in an adolescent with severe autism: A data-based case study. Behavioral Interventions, 30(2). [CrossRef]
- Reaven, J., Blakeley-Smith, C. K., & LeGrand, L. J. (2012). Cognitive-behavioral therapy for children and adolescents with autism spectrum disorders: A systematic review. Journal of Autism and Developmental Disorders, 53(4), 410–419. [CrossRef]
- Morano, S., Ruiz, S., Hwang, J., Wertalik, J. L., Moeller, J., Karal, M. A., & Mulloy, A. (2017). Meta-analysis of single-case treatment effects on self-injurious behavior for individuals with autism and intellectual disabilities. Autism & Developmental Language Impairments, 2. [CrossRef]
- Stepanova, E., Dowling, S., Phelps, M., & Findling, R. L. (2022). Pharmacotherapy of emotional and behavioral symptoms associated with autism spectrum disorder in children and adolescents. Dialogues in Clinical Neuroscience, 19(4), 395–402 . [CrossRef]
- Lucyshyn, J., Albin, R. W., Horner, R. H., & Mann, J. C. (2007). Family implementation of positive behavior support for a child with autism. Journal of Positive Behavior Interventions, 9(3), 131-150. [CrossRef]
- Howlin, P., Magiati, I., & Charman, T. (2009). Systematic review of early intensive behavioral interventions for children with autism. American Journal on Intellectual and Developmental Disabilities, 114(1), 23–41. [CrossRef]
- Rodgers, M., Simmonds, M., Marshall, D., Hodgson, R., Stewart, L. A., Rai, D., & Wright, K. (2016). Intensive behavioural interventions based on applied behaviour analysis for young children with autism: A systematic review and cost-effectiveness analysis. Health Technology Assessment, 20(10), 1–106. [CrossRef]
- Smith, T., Groen, A. D., & Wynn, J. W. (2000). Randomized trial of intensive early intervention for children with pervasive developmental disorder. American Journal on Mental Retardation, 105(4), 269285. [CrossRef]
- Pellicano, E., Dinsmore, A., & Charman, T. (2014). What should autism research focus upon? Community views and priorities from the United Kingdom. Autism, 18(7), 756–770. [CrossRef]
- Ghaleiha, A., Mohammadi, M. R., Mohammadi, E., et al. (2013). Riluzole como terapia adyuvante a risperidona para el tratamiento de la irritabilidad en niños con trastorno autista: un ensayo aleatorizado, doble ciego y controlado con placebo. Paediatric Drugs, 15(6), 505–514. [CrossRef]
- Izurieta-Cossio, M. (2023). Programa de intervención conductual para reducir conductas autolesivas en una niña con diagnóstico de autismo [Trabajo de titulación, Universidad Peruana Cayetano Heredia]. Repositorio Institutional UPCH. https://hdl.handle.net/20.500.12866/15083.
- Oshima, F., Mandy, W., Seto, M., Hongo, M., Tsuchiyagaito, A., Hirano, Y., Sutoh, C., Guan, S., Nitta, Y., Ozawa, Y., Kawasaki, Y., Ohtani, T., Masuya, J., Takahashi, N., Sato, N., Nakamura, S., Nakagawa, A., & Shimizu, E. (2023). Cognitive behavior therapy for autistic adolescents, awareness and care for my autistic traits program: a multicenter randomized controlled trial. BMC Psychiatry, 23, 661. [CrossRef]
- Weiss, J. A., Thomson, K., Burnham Riosa, P., Albaum, C., Chan, V., Maughan, A., Tablon, P., & Black, K. (2018). A randomized waitlist-controlled trial of cognitive behavior therapy to improve emotion regulation in children with autism. Journal of Child Psychology and Psychiatry, 59(11), 1180–1191. [CrossRef]
- Wood, J. J., Kendall, P. C., Wood, K. S., Kerns, C. M., Seltzer, M., Small, B. J., Lewin, A. B., & Storch, E. A. (2019). Cognitive behavioral treatments for anxiety in children with autism spectrum disorder: A randomized clinical trial. JAMA Psychiatry, 77(5), 474–483. [CrossRef]
- Minshawi, N. F., Hurwitz, S., Fodstad, J. C., Biebl, S., Morriss, D. H., & McDougle, C. J. (2014). The association between self-injurious behaviors and autism spectrum disorders. Psychology Research and Behavior Management, 7, 125–136. [CrossRef]
- Peterson, T., Dodson, J., & Strale, F. Jr. (2024). Impact of Applied Behavior Analysis on Autistic Children Target Behaviors: A Replication Using Repeated Measures. Cureus, 16(2). [CrossRef]
- Sabus, A., Feinstein, J., Romani, P., Goldson, E., & Blackmer, A. (2019). Management of self-injurious behaviors in children with neurodevelopmental disorders: A pharmacotherapy overview. Pharmacotherapy, 39(6), 645–664. [CrossRef]
- Robinson, J., Gershwin, T., & London, D. (2019). Maintaining Safety and Facilitating Inclusion: Using Applied Behavior Analysis to Address Self-Injurious Behaviors Within General Education Classrooms. Beyond Behavior, 28(3), 154-167. [CrossRef]
- Fuentes, C., Gómez, S., De Stasio, S., & Berenguer, C. (2025). Augmented reality and learning-cognitive outcomes in autism spectrum disorder: A systematic review. Children, 12, 493. [CrossRef]
| Study topic | Narrative review of effective interventions for the treatment of self-injurious behaviors in children and adolescents with ASD |
| Population | Children and adolescents with ASD |
| Intervention | Interventions for self-injurious behaviors in ASD (behavioral therapy, occupational therapy-based interventions, ABBA method, etc.) |
| Comparison | Comparison of different types of interventions considering their effectiveness |
| Outcome | The results of the interventions will be evaluated in terms of reduction or decrease in self-harming behaviors, improvements in quality of life, or adaptive behavior. |
| Study - Design | Controlled clinical trials, cohort studies, case-control studies. Longitudinal studies and intervention studies with control groups are the most appropriate for evaluating the long-term effectiveness of interventions. |
| Pattern | WoS | Scopus | PubMed |
| ("adolescents") AND (“children”) AND ("autism spectrum disorder ") AND (“self-injurious behaviors") AND (" Intervention" OR "Psychological Interventions" OR “cognitive behavioral therapy” OR “TCC” OR "Psychotherapy" OR "Clinical Psychology" OR "Intervention program*" OR "intervention*" OR "treatment program*" OR "therapeutic program*" OR "therapy program*" OR "clinical intervention*" OR "clinical treatment*" OR "psychological treatment*" OR "cognitive behavioral therapy*" OR "ABA therapy" OR " behavioral therap*" OR "ABA" OR "occupational therapy" OR "sensory therapy" OR "sensory integration" OR “effective interventions” OR "ABA behavioral therapy ” OR “Family based therapy" OR "asperger" OR "self-harm" OR "self-injurious behavior" OR "interpersonal therapy" OR "Cognitive therapy" OR "behavioral therapy). | 143 | 236 | 98 |
| Inclusion criteria | Exclusion criteria |
| Children and adolescents (up to 18 years old) diagnosed with autism spectrum disorder. Publication must be dated no more than 10 years ago to ensure the relevance and timeliness of the approaches. Studies evaluating interventions designed to reduce or manage self-injurious behaviors. Includes different types of interventions, such as behavioral, cognitive, sensory integration, and educational therapies, among others. Articles presenting quantitative and qualitative results on the effectiveness of interventions. Research directly addressing interventions to treat self-injurious behaviors in children and adolescents with ASD. Studies that clearly describe the methodology used in the intervention (behavioral, pharmacological, sensory, etc.). Articles that include data on the effectiveness of the intervention. No language restrictions |
Studies that focus exclusively on adults with ASD or populations not diagnosed with ASD. Studies that primarily investigate medical or psychological conditions other than ASD, unless they include a significant subgroup of participants with ASD. Studies that do not specifically evaluate interventions targeting self-injurious behaviors in children and adolescents with ASD. Articles not directly related to self-injurious behaviors in ASD. Studies of other disorders or interventions not applicable to ASD. Research without empirical evidence or studies that have not been peer-reviewed. Systematic reviews. |
|
Author(s), year, country |
Type of study | Intervention/therapy | Key findings |
| Weiss et al. (2018) Canada |
Randomized controlled | Cognitive Behavioral Therapy | Improvement in emotional regulation and reduction of self-harming behaviors. |
| Peterson et al. (2024) USA |
Experimental | Applied behavior analysis and other behavioral interventions | Reduction in self-harming behaviors and other problematic behaviors. |
| Alakhzami & Chitiyo (2022) USA |
Experimental | Functional Communication Training | Reduction in self-harming behaviors. |
| Robinson et al. (2019) USA |
Case | Behavioral interventions | Reduction in self-harming behaviors. |
| Sabus et al. (2019) USA |
Review | Pharmacotherapy | Pharmacological strategies; effectiveness of risperidone; pharmacotherapy should be combined with behavioral therapy. |
| Wood et al. (2019) USA |
Randomized controlled | Cognitive Behavioral Therapy | Reducción de ansiedad y conductas autolesivas. TCC adaptada al TEA con efecto indirecto. |
| Morano et al. (2017) USA |
Meta-analysis | Bhavioral treatments | Reduction in self-harming behaviors. |
| Boesch et al. (2015) USA |
Case | Behavioral approach | 50% reduction in self-injurious behaviors and effectiveness in severe cases. |
| Minshawi et al. (2014) USA |
Observational | Association analysis | Relationship between self-harm and clinical features; key functional assessment for intervention. |
| Schaaf et al. (2013) USA |
Randomized controlled | Sensory integration therapy | 40% reduction in self-injurious behaviors; improvement in self-regulation. |
| Izurieta Cossio (2023) Peru |
Case | Behavioral intervention | Reduction of self-injurious behaviors; effective individualized intervention. |
| Ghaleiha et al. (2013) Iran |
Randomized controlled | Pharmacotherapy | Improvement in irritability and indirect reduction in self-harm. |
| Oshima et al. (2023) Japan |
Randomized controlled | Cognitive Behavioral Therapy | Improvements in emotional self-regulation and reduction of self-harm. |
| Type of Therapy | Overall Effectiveness |
| Behavioral Therapies | Highly effective in reducing self-injurious behaviors, especially with applied behavioral intervention (ABA). The best results are seen in young children, although it is also useful in adolescents with moderate self-injurious behaviors. It is especially effective for higher-functioning individuals who can learn new behavioral skills quickly. |
| Cognitive-Behavioral Therapies | Positive effectiveness in emotional regulation, with significant reductions in self-injurious behaviors, particularly in managing frustration and anxiety. They are especially effective in children and adolescents with greater functional and verbal ability, who can benefit from problem-solving and the development of emotional coping skills. |
| Occupational Therapy/Sensory Integration | Moderately effective, they are especially useful for people with sensory overreactions. These therapies help reduce self-injurious behaviors related to sensory overload. They are most useful for children and adolescents with sensory difficulties and can also be applied to people with a wider range of functional abilities. |
| Combined interventions with Medications |
Effective for severe cases of ASD, especially those with emotional or neuropsychiatric comorbidities. Pharmacological interventions may be necessary in combination with other therapies to manage severe or neurochemical symptoms, and are more common in adolescents with severe self-injurious behaviors. |
| Combined Interventions (ABA + CBT, SI) |
Highly effective in the combined management of behaviors and emotions, offering integrated improvements that address multiple factors. These interventions are ideal for children and adolescents with ASD, especially those with emotional difficulties and severe self-injurious behaviors, who require a comprehensive approach that addresses both behavioral and emotional aspects. |
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2025 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (http://creativecommons.org/licenses/by/4.0/).





