1. Introduction
Odontogenic Sinusitis (ODS) is an infectious condition of the paranasal sinuses resulting from dental pathology or treatment. Historically, dental diseases such as periodontitis, periodontal abscesses, or periapical diseases, as well as dental trauma, have been reported to be responsible for 10-12% of maxillary sinusitis, but recent studies suggest a real incidence up to 30% [
1,
2] . The increased incidence of ODS is also probably trackable to an increase in the number of dental implant procedures [
3].
ODS usually involves the maxillary sinus monolaterally, because of the proximity of the teeth roots to the floor of the sinus. A dental infection or iatrogenic injuries (e.g. dental implants, oroantral communication following dental extractions and sinus floor elevation, foreign bodies) can violate the Schneiderian membrane, carrying infection and triggering a mucosal inflammatory response [
1,
4,
5]. This phenomenon causes a unilateral maxillary sinus mucosal thickening and radiological opacification. The infection and inflammation of the maxillary sinus causes the symptoms associated with ODS and eventually can also spread to other near paranasal structures [
2].
The diagnosis is often challenging due to diversified clinical presentation [
6]. One of the challenges with diagnosing ODS is that patients often require evaluations by both otolaryngologists and dental providers. When otolaryngologists are first consulted, the clinical presentations can mimic nonodontogenic rhinosinusitis, and odontogenic sources may not be investigated [
7]. Similarly, if patients present firstly to dental providers with maxillary dental pathology, sinusitis can be overlooked. Patients affected by classical ODS usually present symptoms of rhinosinusitis, but foul smell is more specific of ODS, while dental pain is unfrequently. Some patients will be asymptomatic [
6].
According to consensus statement on diagnosis of ODS, in presence of these elements is necessary a multidisciplinary evaluation with otolaryngologist and dental provider [
8]. The otolaryngologist should confirm sinusitis with nasal endoscopy by identifying unilateral purulence, oedema, or polyps in the middle meatus, or maxillary sinus. The dental provider confirms odontogenic sources of sinusitis evaluating the presence of necrotic o partially necrotic pulp or failing root canal therapy.
The multidisciplinary approach ensures a correct diagnosis and consequently an appropriate therapy. Otolaryngologists and dental providers should check for dental discomfort, oroantral fistula (OAF), pathologies, or previous treatments as well as sinusitis symptoms and dental pain. In cases with ODS otolaryngologists should typically confirm the sinusitis, and dental specialists should typically confirm the odontogenic pathology [
9].
The otolaryngologist, dental provider, and patient should collaborate on management decisions and talk about the advantages and disadvantages of endoscopic sinus surgery (ESS) and dental care. When both dental procedures and ESS are carried out for ODS brought on by endodontic disease, periodontitis, permanent OAF, and dental implants, the majority of case series have reported high success rates of 90% to 100% [
4] . Oral antibiotics alone has been shown a low efficacy [
7]. Patient with strong sinonasal symptoms and few dental complaints may benefit from primary ESS to relieve symptoms rapidly, followed by eventual any necessary dental care [
10]. It is advisable to prioritize the district causing the least tolerable symptoms for the patient. ESS is often required following primary dental care either to relieve sinonasal symptoms or to prevent risk orbital or cerebral consequences of ODS [
11], but also hybrid approaches such as the osteoplastic surgical approach (OPSA) to the maxillary sinus can be effective [
12].
The heterogeneity of causes, clinical presentation, and treatment requires a different clinical strategy than "classic" rhinosinusitis. The literature on ODS is varied, this is due both to its clinical heterogeneity and the involvement of different professional figures [
8]. The creation of uniform classification standards is necessary given the lack of defined guidelines.
The aim of our study is to create a classification that considers the clinical-instrumental aspects, to be able to identify all the characteristics using a simple and compact alphanumeric code.
2. Materials and Methods
A retrospective study was performed considering 124 patients visited and operated in the department of integrated therapies in otolaryngology Rome Biomedical Campus University Foundation from December 2020 to September 2023 and that have consented to the use of the clinical data reported in this article by signing a specific consent form. This retrospective analysis was performed in compliance with the World Medical Association Declaration of Helsinki on medical research protocols and ethics, being a retrospective analysis it was exempted from institutional review board approval.
A 3-year retrospective analysis was conducted, considering clinical results, demographic variables (age and sex), disease etiology and progression, imaging, and surgical and medicinal interventions [
Table A1].
The inclusion criteria applied were: (1) clinical diagnosis of sinusitis with suspected odontogenic etiology, supported by radiological and/or endoscopic findings and with medical treatment resistance; (2) specialist (ENT/maxillofacial surgeon or dentist) agreement on the odontogenic focus; (3) presence of maxillofacial computer tomography (CT) scan executed before the surgery.
The exclusion criterion was a history of chronic rhinosinusitis with or without polyps.
Clinically, patients referred purulent rhinorrhea, unilateral and bilateral nasal blockage, maxillary discomfort, and postnasal drip, which occurred later than dental treatments or disease. These symptoms did not respond to steroid (topical and systemic) and antibiotic therapy.
ENT examination is performed with flexible endoscope to examine the sinuses and discover areas of inflammation, displaced dental implants, or anatomical anomalies (turbinate anomalies, nasal polyps, septal deviation).
Dentist examination evaluates presence of OAF or dental lesions.
A CT scan of the paranasal sinuses without contrast material which revealed the location, extent, and severity of the disease, presence of foreign body in maxillary sinus, obstruction of ostiomeatal complex, OAF.
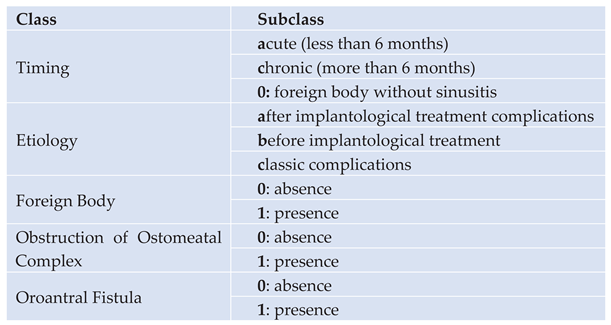
Our classification considers five factors: timing, etiology, presence of oro-antral fistula, obstruction of ostiomeatal complex and presence of foreign body.
Timing
The first factor that is evaluated with this classification is the duration of the symptoms (T= timing), dividing the ODS into two subclasses:
subclass A: when the symptoms have been present for less than 6 months (a = acute)
subclass C: when the symptoms last more than 4 months (c = chronic)
subclass 0: when a foreign body at the level of the maxillary sinus can be seen even when the patient does not have any sinusitis symptoms (0 = without sinusitis)
Etiology
The second factor is the cause of ODS (
E= etiology). For this factor we have resumed the classification of Felisati [
1] using the relation with oral surgery or disease:
subclass A includes sinusitis which occurs as a complication of a dental implant (a= after)
subclass B includes those which occur as a complication of treatments preceding a dental implant, such as sinus lift (b= before)
subclass C those that occur as a complication of a dental disease (c=classical complication)
Foreign Body, Obstruction, Fistula
The third, fourth and fifth factors evaluate the clinical pattern that is observed through fibroscopy performed by the ENT, dental examination, and CT of the facial mass. Specifically, is evaluated the absence (0) or the presence (1) of three elements:
Each factor is identified with a letter, generally the first letter, thus obtaining an acronym: TEBOF [
Table 1].
Additionally, each letter has a neighbouring letter or number that designates a subclass for each factor.
Examples
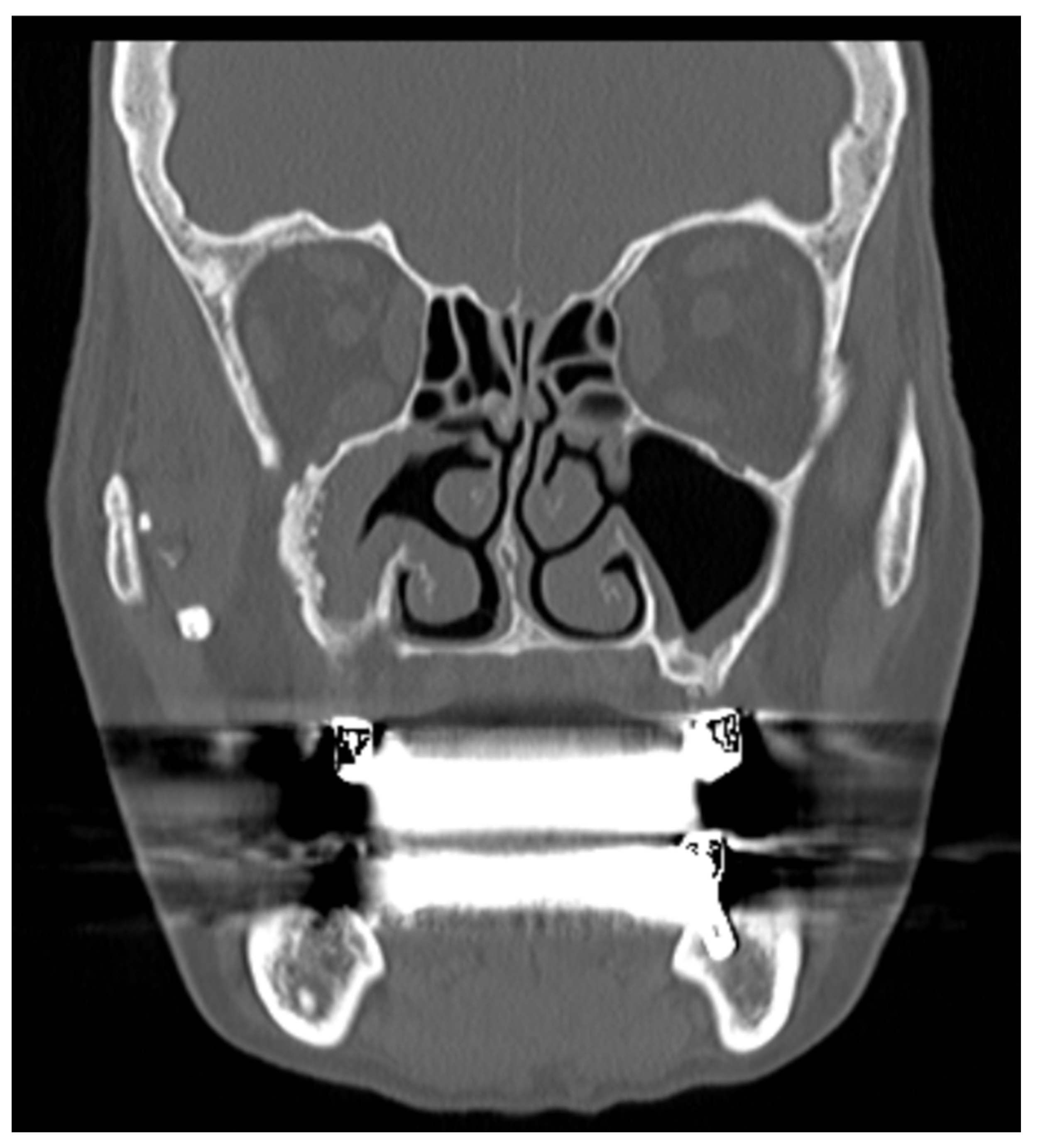
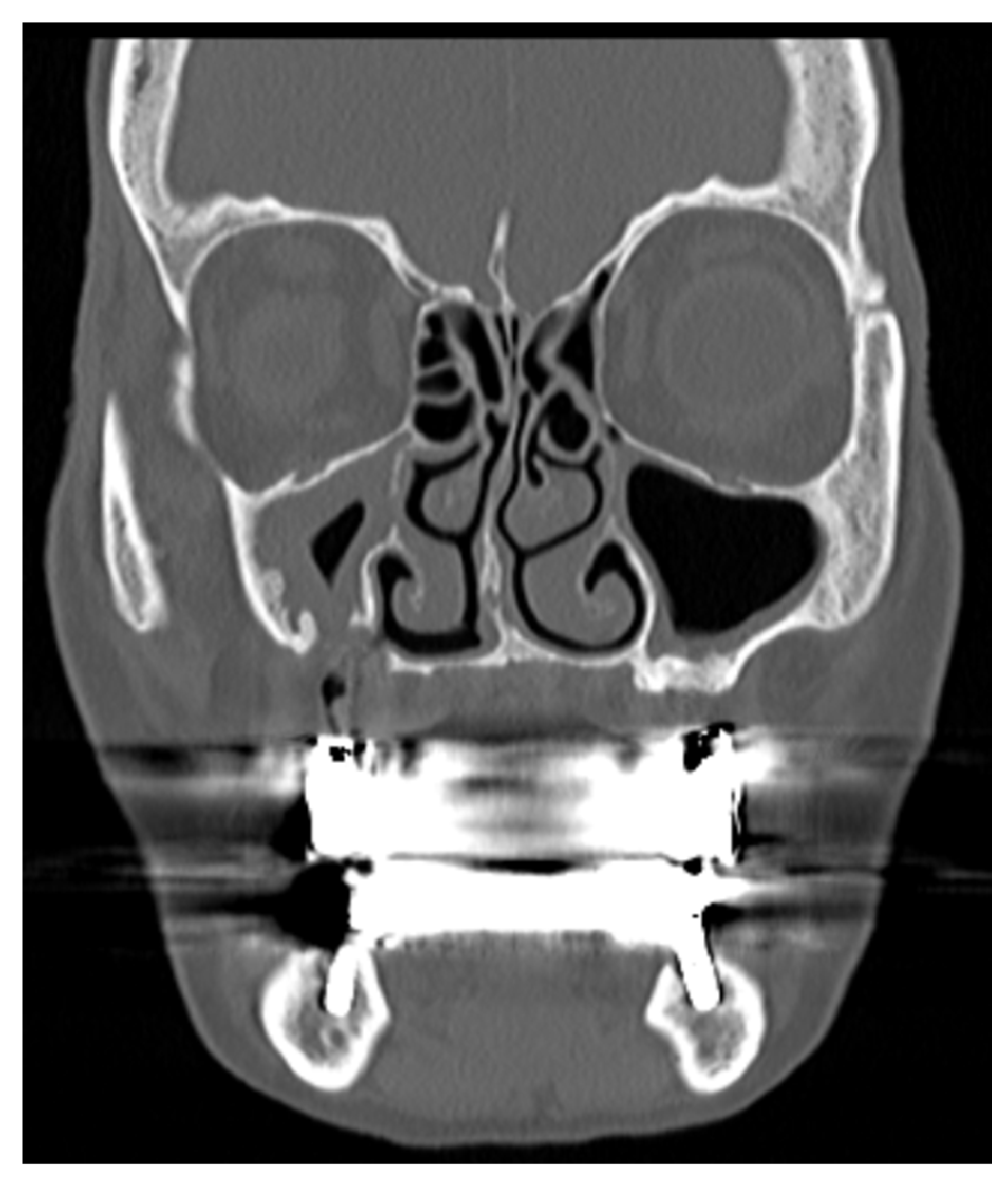
A patient suffering from sinusitis due to a complication of implantological treatment for at least 4 months, with OAF, without obstruction of ostiomeatal complex and without foreign body can be identified as: T
cE
aB
0O
0F
1 [
Figure 1] [
Figure 2]
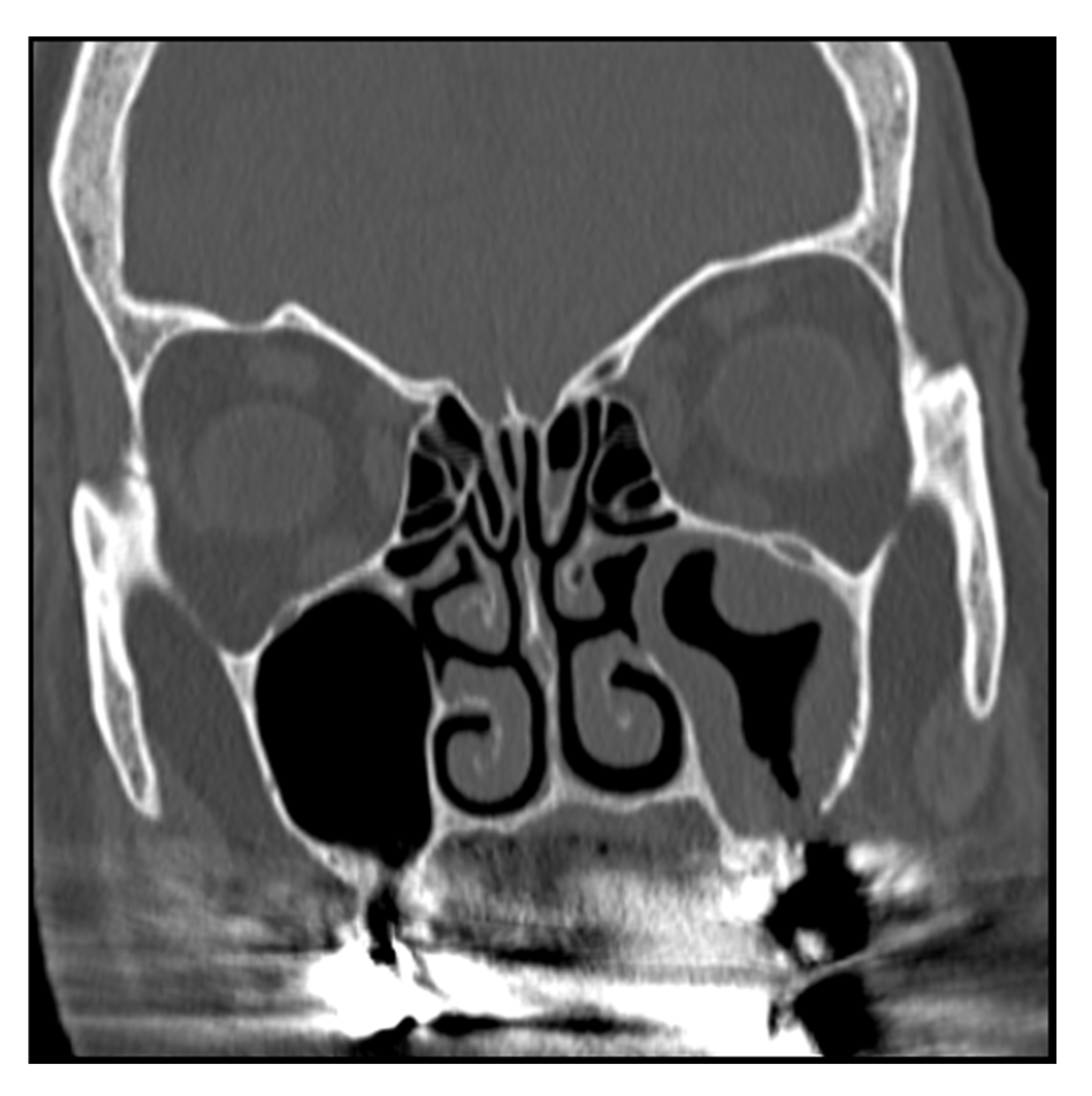
A patient presenting sinusitis symptoms for more than 4 months, after an implantological treatment, without a foreign body in the maxillary sinus, without obstruction of the OMC and with OAF, can be identified as: T
aE
aB
0O
1F
1 [
Figure 3]
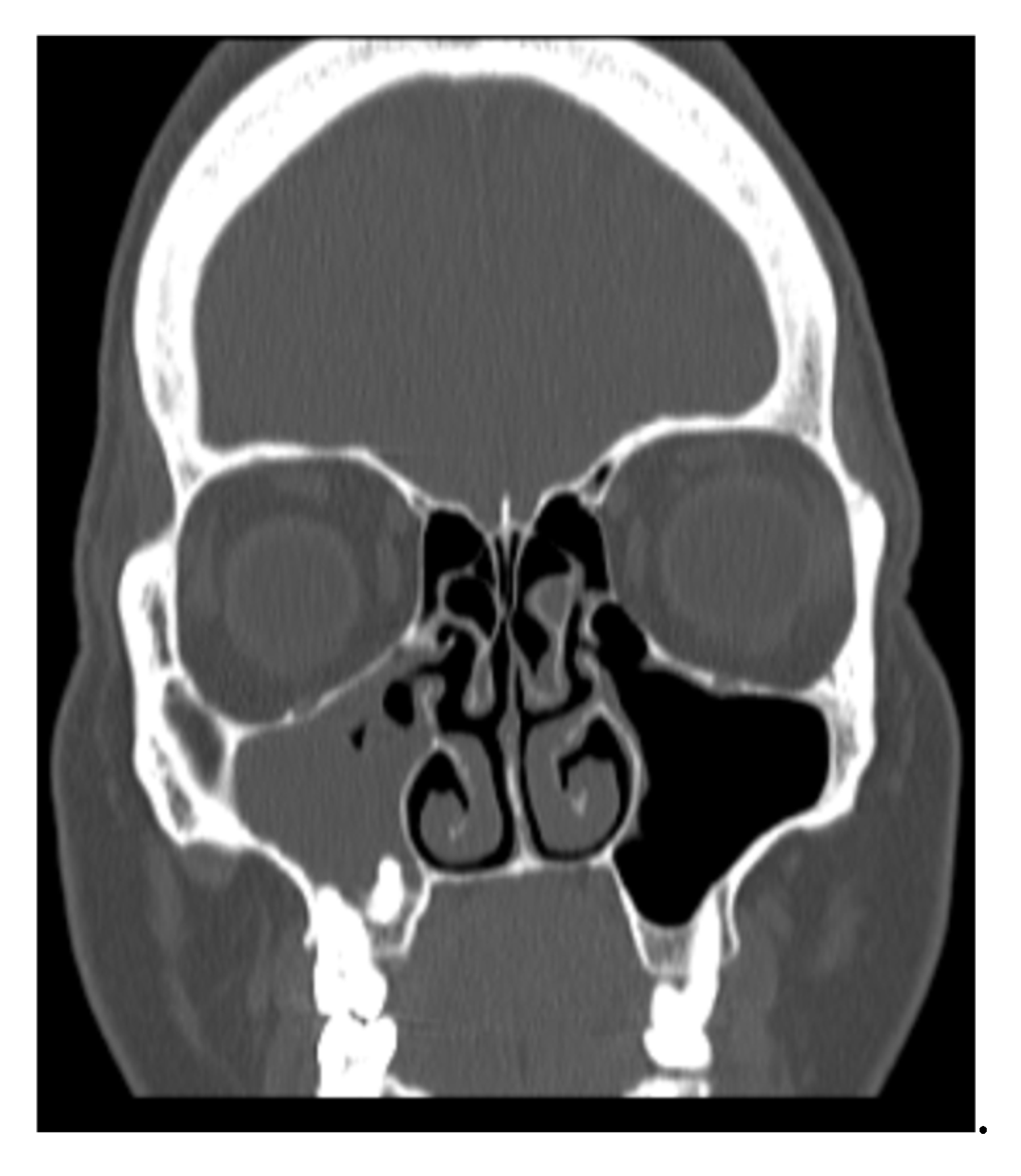
A patient with chronic sinusitis as complication of dental pathology, with foreign body in the maxillary sinuses, without obstruction of the OMC and with OAF, can be identified as: T
cE
cB
1O
0F
1 [
Figure 4]
3. Results
This retrospective study includes 124 patients with clinical and/or radiological signs of maxillary sinusitis operated in the department of integrated therapies in otolaryngology (Polyclinic Campus Bio-Medico, Rome, Italy) from December 2020 to December 2023. Patients with a CT scan showing a foreign body but without sinusitis symptoms, are also included in this database because a foreign body is a trigger for sinusitis.
Of these 124 patients, 64 are women (51,6%) and 60 men (48,4%), a male to female ratio of 0.94:1. The mean age was 57.2 ± 13 years, with the youngest patient 26 years and the oldest 87 years. Every patient disclosed a history of oral surgery or dental disease.
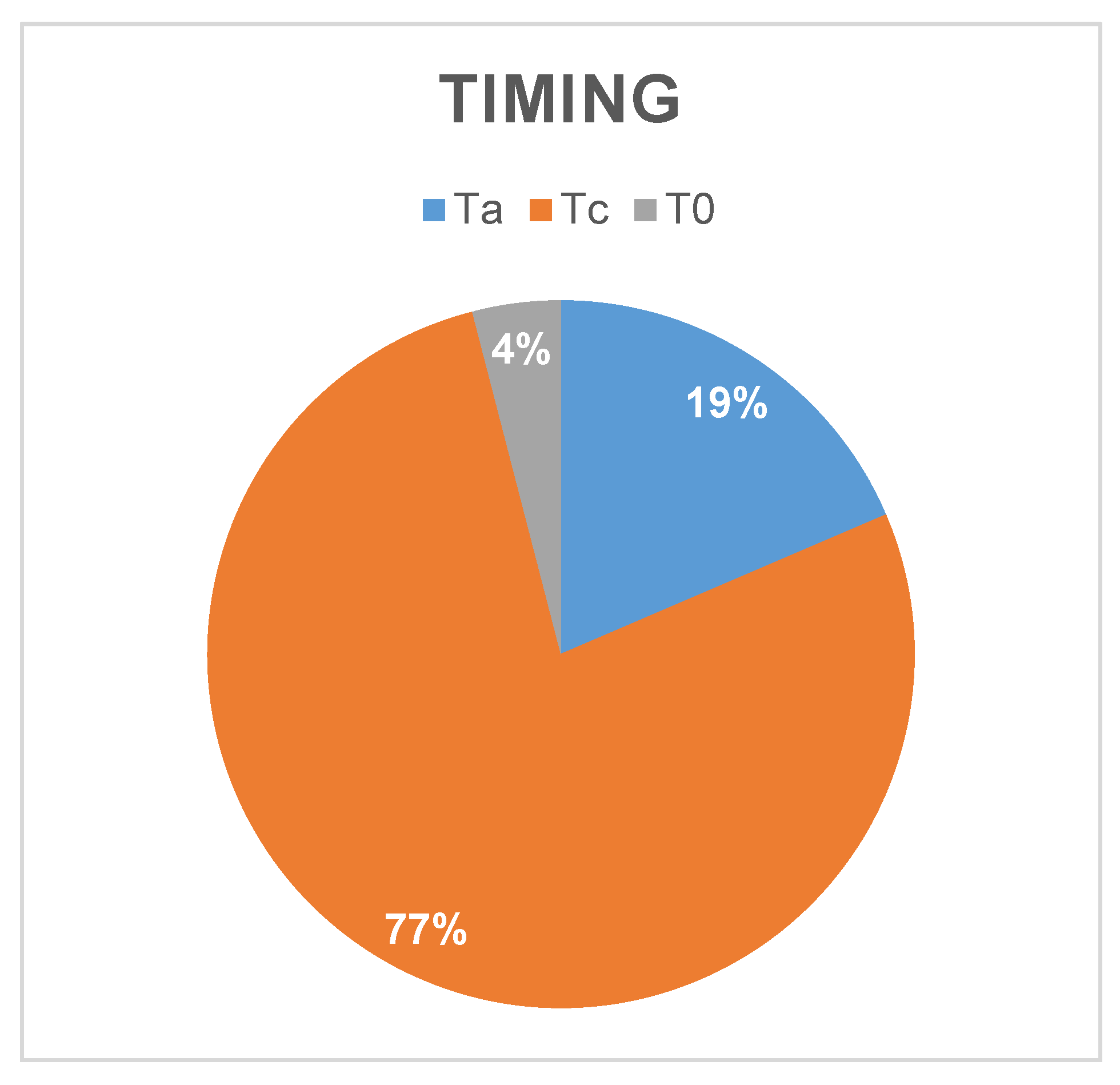
The duration of symptoms is reported by the patient during the visit with the ENT or dentist. 96 out of 124 patients (76,8%), who had symptoms for longer than four months, were classified as chronic sinusitis patients (Tc group). 23 patients (18,4%) were classified as acute sinusitis patients (Ta group) because they had symptoms for less than four months (
Graph 1). A tiny percentage of patients (4,00%), 5 in 122, were diagnosed the presence of a foreign body rather than sinusitis symptoms, placing them in the T
0 group.
All patients had an odontogenic cause.
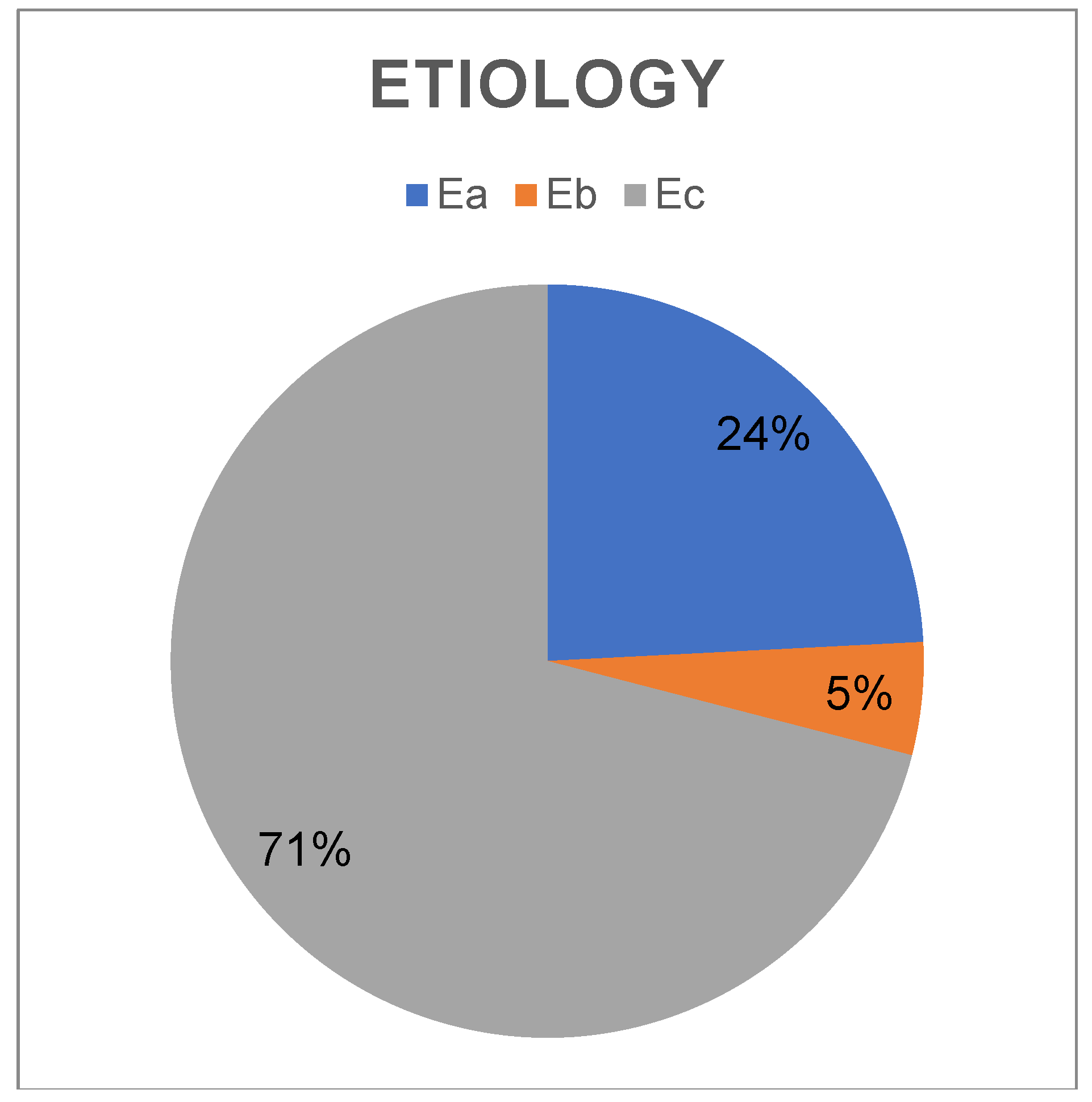
Most patients (88; 70,04%) were included in the E
c group, where
sinusitis is a side effect of a primary dental pathology. These patients
frequently visit the ENT for sinus problems without being aware that there is a
dental issue. On the other side, 30 (24,00%) patients were included to the “E
a”
group because they reported the onset of symptoms after having had dental
implants performed, while 6 (4,80%) were included to the “E
b” group
because they reported the onset of symptoms before a dental implant but after
an oral procedure such as a sinus lift (
Graph 2). Patients of these two groups, usually comes to ENT
specialist after they had seen the dentist.
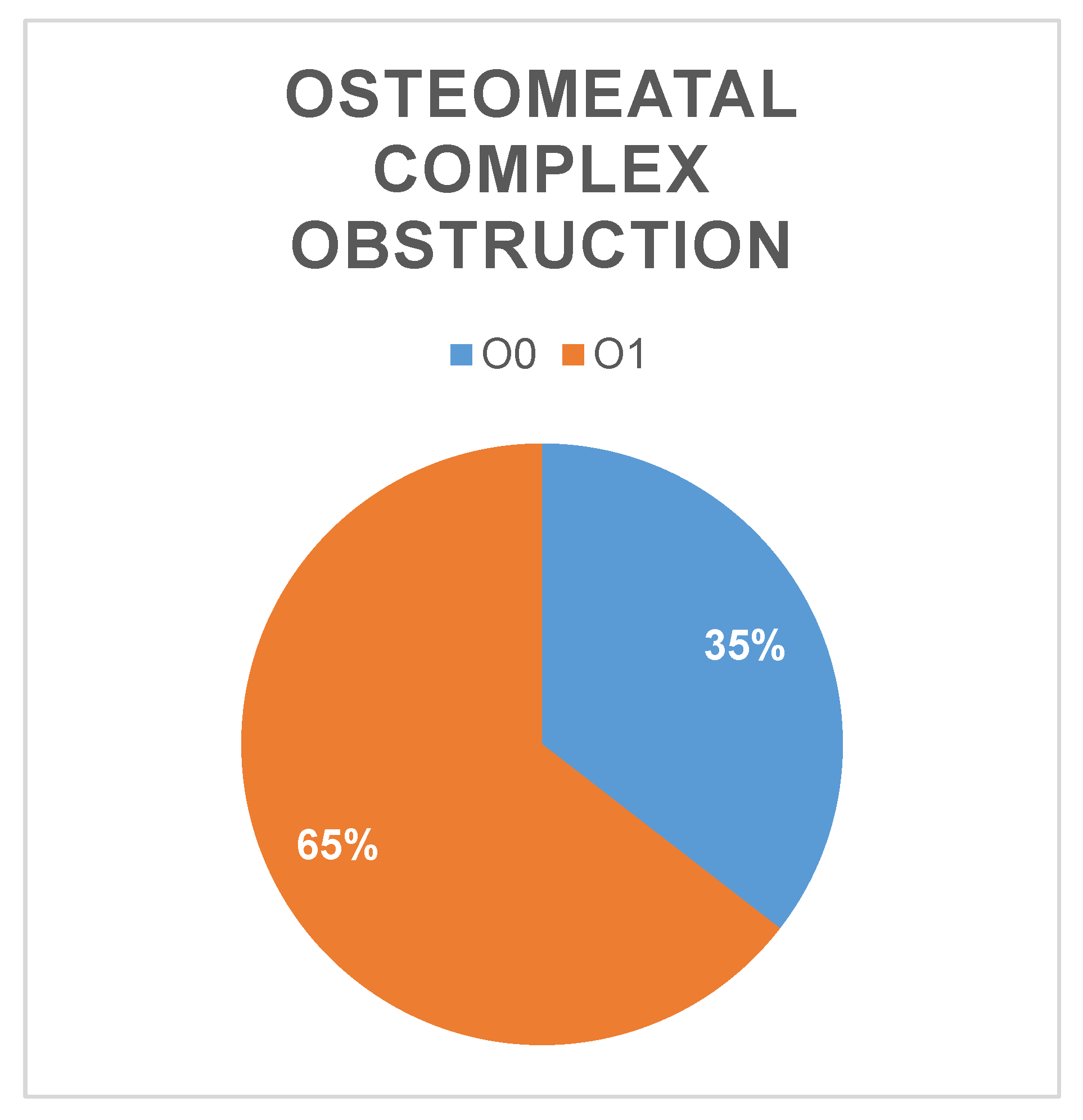
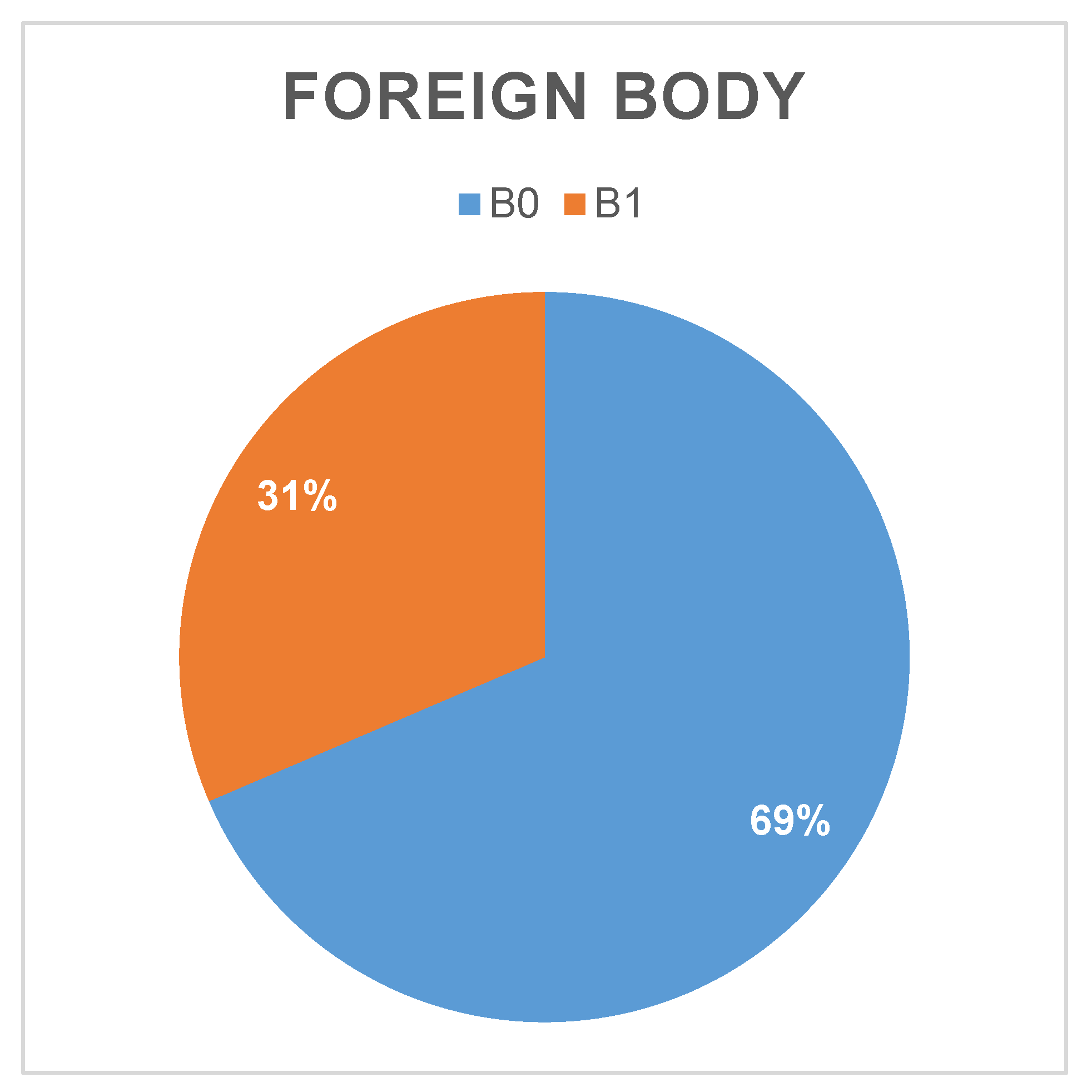
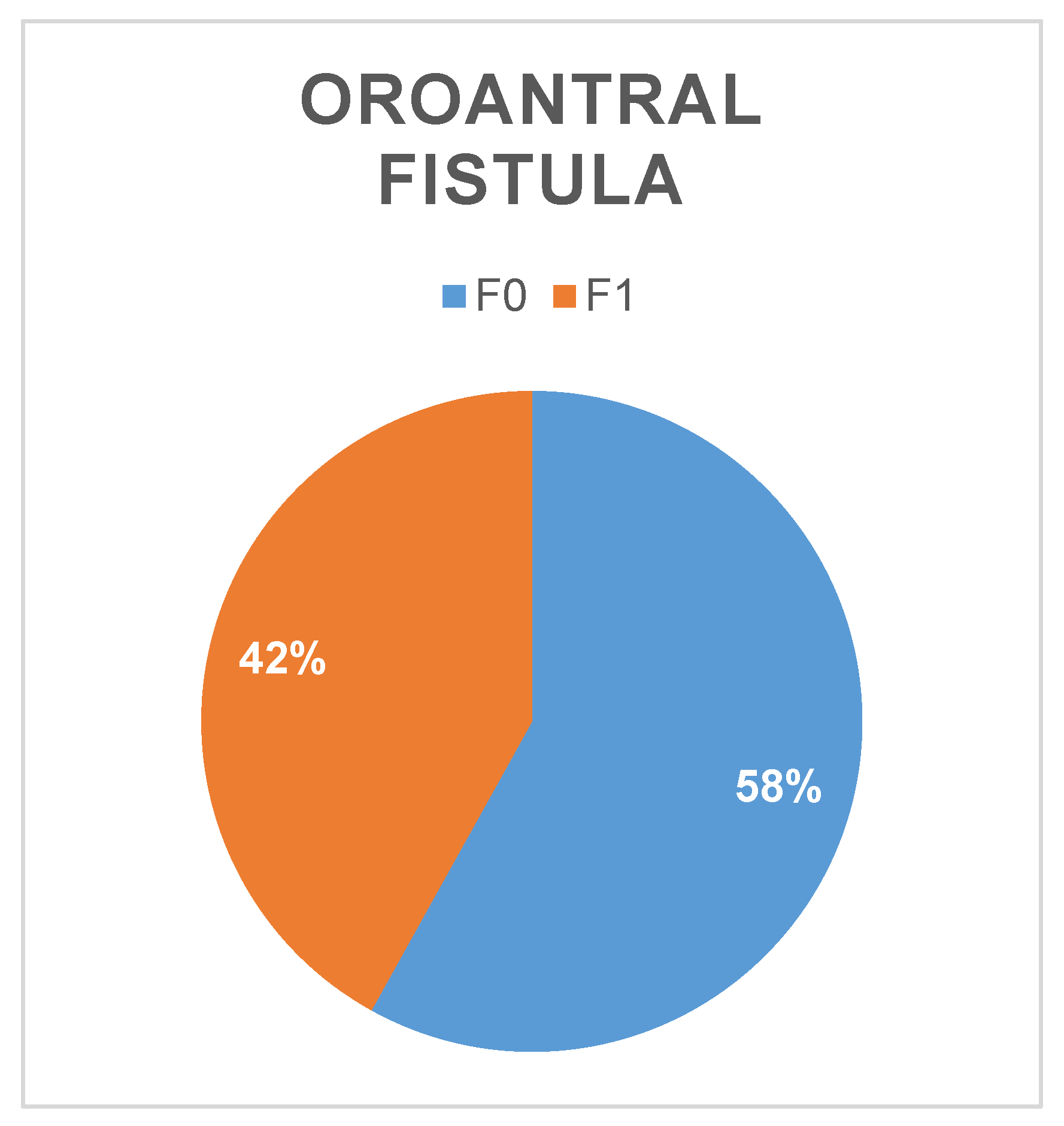
Through clinical examination and imaging, 39 foreign bodies (B
1 group), 80 (64,5%) patients with obstruction of the ostiomeatal complex (O
1 group) were observed (
Graph 3). A patient may have more than one of these conditions at the same time. Most of patients presented a foreign body in the maxillary sinus (85 – 69%) (
Graph 4). Oroantral fistula was observed in almost half of patients (52 – 42%). (
Graph 5)
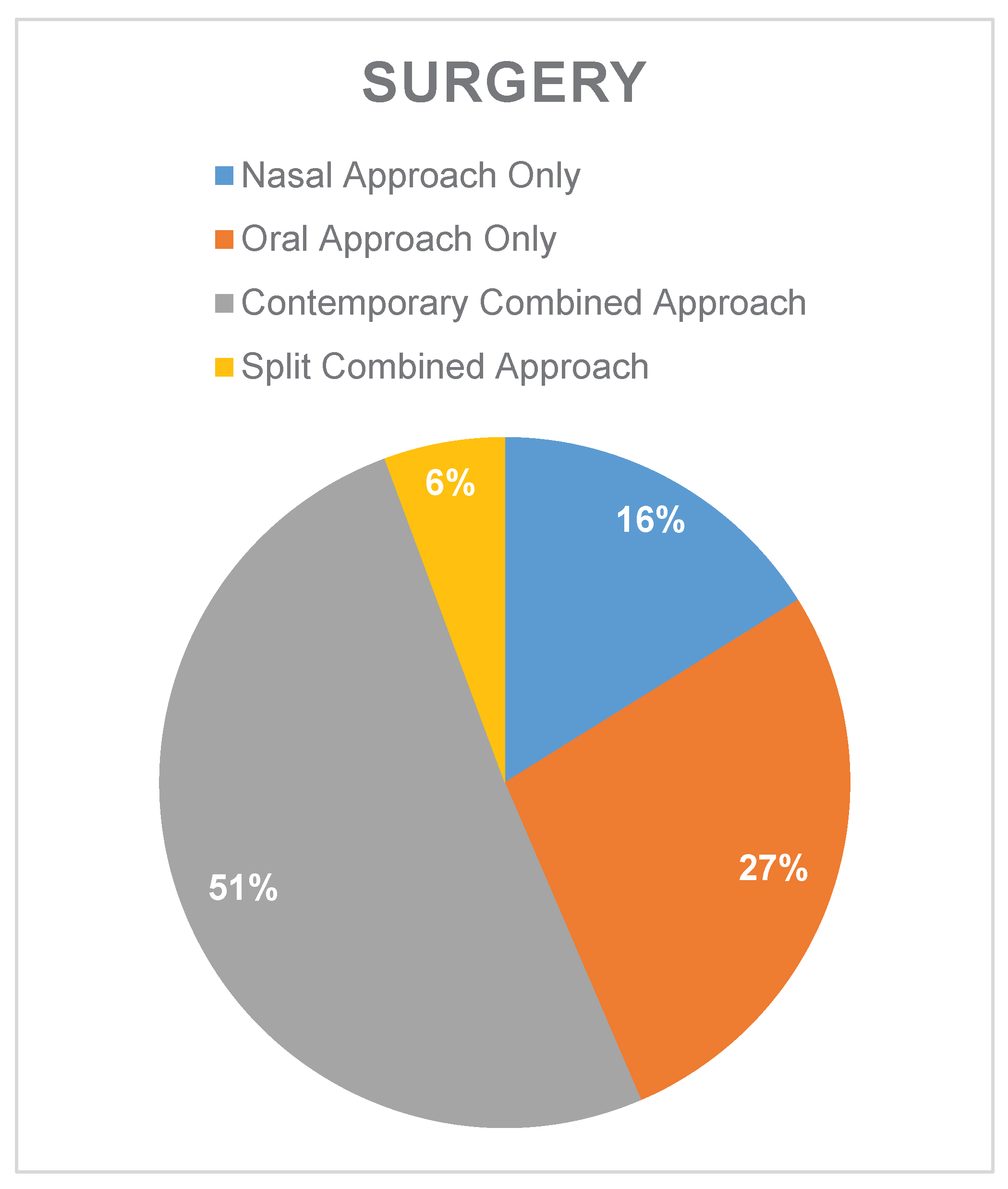
All patients included in this study had already been treated with medical therapy alone, without satisfying results. Every patient received surgical care. Anatomical features such as the presence of a foreign body, an OAF, and obstruction of the ostiomeatal complex are the main factors used to determine surgical treatment. To repair OAFs and execute dental extractions, the surgical therapy can be performed by the ENT specialist alone with a FESS (20 – 16%), by the dentist alone (34 – 28%), or by a combination of methods that involves simultaneous endoscopic sinus surgery and oral procedures (63 – 51%). In some instances, a fractional combination treatment plan was implemented (7 – 5%), in which the dentist and ENT treat the pertinent issues independently of one another. (
Graph 6) This flexibility of methods allows to treat this condition in a tailored fashion.
4. Discussion
Other classification of odontogenic sinusitis has been proposed to identify homogenous groups of treatment [
13] or radiological features [
14], are already in use [
1]. The classification proposed in this publication uses the basis laid on this previous works and is intended to allow for a global assessment, considering not only the primary pathology but also its etiology. By adopting a classification system that promotes a global perspective, healthcare professionals can collaborate more effectively, gain insights from different specialties, and improve the overall quality of care. This multidisciplinary approach contributes to a more nuanced and thorough representation of the patient's health status and paves the way for a tailored and effective treatment strategies.
The authors noted that the patients selected for a combined and split contemporary surgical approach presented roughly equal portion of patients with and without OAF and Foreign Body in the maxillary sinus. A more pronounced majority of patient presented obstruction of the ostiomeatal complex than in the general sample.
The subgroup of patients that were treated with intranasal approach alone reported a predictable shift towards cases without OAF or foreign body, while almost all of them presented ostiomeatal complex obstruction.
The ratio of patients with OAF and without resulted substantially even in the subgroup undergoing only intraoral approach while most of the patients in this subgroup did not present foreign body or obstruction of the ostiomeatal complex.
The portion of patient presenting classical etiology and a chronic condition is similar to the general sample, this is probably caused by selection of only patients where medical therapy resulted ineffective, this resulted in a selection bias for patient with a chronic condition.
5. Conclusions
This classification is useful for characterization of the sinusitis. Anamnesis is used to assess the duration and cause of the symptoms [
15]; clinical examination by otolaryngologist and dental provider reveals sinusitis signs and the presence of an OAF; imaging reveals the presence of a foreign body and obstruction of the ostiomeatal complex [
16].
This classification aims to provide a simple and compact combination of letters and numbers to provide to different specialists a full insight of different features of ODS in an easy and fast way, allowing easier communication between the different health professionals necessary for the proper care of this condition [
17]. The presence of one or more features can guide the choice of treatment. Antibiotic therapy, surgical therapy, or a combination of the two may be used, depending on how long the symptoms last and their etiology. Of course, the best surgical method for each patient must also consider the radiological parameters as dimension and position of the foreign body [
18].
The phenomenon of foreign bodies without sinusitis is also considered in this classification. The existence of a foreign body is always a trigger to inflammatory response within the sinus that may lead to sinusitis. So, in agreement with current literature, authors suggest removing the foreign body in most of the cases, even without clear sinusitis symptoms [
19].
The developing of different heterologous and autologous biomaterials for the closure of the OAF presents the challenge to select the right type for the specific patient, currently the only criteria considered has been the OAF dimension [
20,
21,
22,
23], the TEBOF classification could provide a wider contest for the evaluation and indication of these devices.
Dividing the sample in subgroups based on the therapeutical approach selected highlighted some elements that could induce a therapeutic approach over another, but this preliminary analysis presents important biases derived from the retrospective nature of this paper and the size of the sample.
Funding
This research received no external funding.
Informed Consent Statement
Any research article describing a study involving humans should contain this statement. Please add “Informed consent was obtained from all subjects involved in the study.” OR “Patient consent was waived due to REASON (please provide a detailed justification).” OR “Not applicable.” for studies not involving humans. You might also choose to exclude this statement if the study did not involve humans. Written informed consent for publication must be obtained from participating patients who can be identified (including by the patients themselves). Please state “Written informed consent has been obtained from the patient(s) to publish this paper” if applicable.
Data Availability Statement
We encourage all authors of articles published in MDPI journals to share their research data. In this section, please provide details regarding where data supporting reported results can be found, including links to publicly archived datasets analyzed or generated during the study. Where no new data were created, or where data is unavailable due to privacy or ethical restrictions, a statement is still required. Suggested Data Availability Statements are available in section “MDPI Research Data Policies” at
https://www.mdpi.com/ethics.
Acknowledgments
In this section, you can acknowledge any support given which is not covered by the author contribution or funding sections. This may include administrative and technical support, or donations in kind (e.g., materials used for experiments). Where GenAI has been used for purposes such as generating text, data, or graphics, or for study design, data collection, analysis, or interpretation of data, please add “During the preparation of this manuscript/study, the author(s) used [tool name, version information] for the purposes of [description of use]. The authors have reviewed and edited the output and take full responsibility for the content of this publication.”
Conflicts of Interest
The authors declare no conflicts of interest.
Abbreviations
The following abbreviations are used in this manuscript:
| ODS |
Odontogenic Sinusitis |
| OAF |
Oroantral Fistula |
| ESS |
Endoscopic Sinus Surgery |
| OPSA |
Osteoplastic Surgical Approach |
| CT |
Computer Tomography |
Appendix A
Appendix A.1
Table A1.
Patients considered in this study. M: male, F: female; Ta: symptoms< for < 6 months, Tc:symptoms >6 months; Ea:after dental impantation , Eb:before dental impantation , Ec: classical complication of dental condition; B0: foreign body absent in the maxillary sinus, B1: foreign body present in the maxillary sinus; O0: free osteomeatal complex, O1: closed osteomeatal complex; F0 absence of oroantral fistula, F1: presence of oroantral fistula.
Table A1.
Patients considered in this study. M: male, F: female; Ta: symptoms< for < 6 months, Tc:symptoms >6 months; Ea:after dental impantation , Eb:before dental impantation , Ec: classical complication of dental condition; B0: foreign body absent in the maxillary sinus, B1: foreign body present in the maxillary sinus; O0: free osteomeatal complex, O1: closed osteomeatal complex; F0 absence of oroantral fistula, F1: presence of oroantral fistula.
| Number |
Age (years) |
Sex |
Timing (T) |
Etiology (E) |
Foreign Body (B) |
Obstruction of Ostomeatal Complex (O) |
OroAntral Fistula (F) |
Surgical Approach |
| 1 |
43 |
F |
T0 |
Ea |
B1 |
O1 |
F1 |
Oral Approach Only |
| 2 |
79 |
F |
T0 |
Ea |
B1 |
O1 |
F1 |
Oral Approach Only |
| 3 |
40 |
M |
T0 |
Ec |
B1 |
O1 |
F0 |
Oral Approach Only |
| 4 |
26 |
F |
T0 |
Ec |
B1 |
O1 |
F0 |
simultaneous Combined Approach |
| 5 |
52 |
M |
Ta |
Ec |
B0 |
O1 |
F1 |
Split Combined Approach |
| 6 |
43 |
M |
Ta |
Ec |
B1 |
O1 |
F1 |
simultaneous Combined Approach |
| 7 |
72 |
M |
Ta |
Ec |
B0 |
O1 |
F1 |
simultaneous Combined Approach |
| 8 |
78 |
F |
Ta |
Ea |
B0 |
O1 |
F0 |
Nasal Approach Only |
| 9 |
70 |
M |
Ta |
Ec |
B0 |
O1 |
F0 |
Nasal Approach Only |
| 10 |
66 |
F |
Ta |
Eb |
B0 |
O1 |
F0 |
Nasal Approach Only |
| 11 |
87 |
F |
Ta |
Ec |
B0 |
O1 |
F0 |
Oral Approach Only |
| 12 |
48 |
M |
Ta |
Ea |
B0 |
O0 |
F1 |
Oral Approach Only |
| 13 |
43 |
M |
Ta |
Ec |
B0 |
O0 |
F0 |
Oral Approach Only |
| 14 |
37 |
F |
Ta |
Ea |
B0 |
O0 |
F0 |
Oral Approach Only |
| 15 |
69 |
F |
Ta |
Ea |
B0 |
O0 |
F1 |
Oral Approach Only |
| 16 |
59 |
F |
Ta |
Ea |
B0 |
O0 |
F1 |
Oral Approach Only |
| 17 |
64 |
M |
Ta |
Ec |
B0 |
O0 |
F1 |
Oral Approach Only |
| 18 |
43 |
F |
Ta |
Ec |
B0 |
O0 |
F1 |
Split Combined Approach |
| 19 |
42 |
F |
Ta |
Ec |
B0 |
O0 |
F0 |
Oral Approach Only |
| 20 |
33 |
M |
Ta |
Ec |
B0 |
O0 |
F0 |
Oral Approach Only |
| 21 |
55 |
M |
Ta |
Ec |
B0 |
O1 |
F0 |
Nasal Approach Only |
| 22 |
30 |
M |
Ta |
Ec |
B1 |
O1 |
F1 |
simultaneous Combined Approach |
| 23 |
63 |
F |
Tc |
Ec |
B0 |
O1 |
F0 |
simultaneous Combined Approach |
| 24 |
64 |
M |
Tc |
Ea |
B1 |
O1 |
F0 |
simultaneous Combined Approach |
| 25 |
83 |
F |
Tc |
Ec |
B1 |
O1 |
F0 |
Nasal Approach Only |
| 26 |
72 |
M |
Tc |
Ec |
B0 |
O0 |
F1 |
Oral Approach Only |
| 27 |
72 |
M |
Tc |
Ec |
B0 |
O0 |
F1 |
Oral Approach Only |
| 28 |
79 |
M |
Tc |
Ea |
B0 |
O0 |
F0 |
Split Combined Approach |
| 29 |
64 |
F |
Tc |
Ea |
B1 |
O1 |
F1 |
simultaneous Combined Approach |
| 30 |
47 |
M |
Tc |
Ec |
B0 |
O1 |
F1 |
Split Combined Approach |
| 31 |
29 |
M |
Tc |
Ec |
B0 |
O1 |
F0 |
Split Combined Approach |
| 32 |
66 |
M |
Tc |
Ec |
B0 |
O1 |
F0 |
simultaneous Combined Approach |
| 33 |
73 |
M |
Tc |
Ea |
B1 |
O1 |
F0 |
simultaneous Combined Approach |
| 34 |
58 |
F |
Tc |
Ea |
B1 |
O1 |
F1 |
simultaneous Combined Approach |
| 35 |
49 |
F |
Tc |
Eb |
B1 |
O1 |
F0 |
simultaneous Combined Approach |
| 36 |
57 |
F |
Tc |
Ec |
B0 |
O1 |
F0 |
simultaneous Combined Approach |
| 37 |
45 |
F |
Tc |
Ec |
B1 |
O0 |
F0 |
simultaneous Combined Approach |
| 38 |
72 |
M |
Tc |
Ea |
B1 |
O1 |
F0 |
simultaneous Combined Approach |
| 39 |
65 |
M |
Tc |
Ea |
B1 |
O1 |
F0 |
simultaneous Combined Approach |
| 40 |
54 |
M |
Tc |
Ea |
B1 |
O1 |
F0 |
Nasal Approach Only |
| 41 |
62 |
M |
Tc |
Ec |
B0 |
O1 |
F0 |
Split Combined Approach |
| 42 |
48 |
F |
Tc |
Ec |
B0 |
O1 |
F0 |
simultaneous Combined Approach |
| 43 |
57 |
F |
Tc |
Ea |
B0 |
O1 |
F1 |
simultaneous Combined Approach |
| 44 |
70 |
F |
Tc |
Ea |
B1 |
O0 |
F1 |
simultaneous Combined Approach |
| 45 |
58 |
M |
Tc |
Ec |
B0 |
O0 |
F0 |
simultaneous Combined Approach |
| 46 |
64 |
F |
Tc |
Ec |
B0 |
O1 |
F0 |
simultaneous Combined Approach |
| 47 |
76 |
M |
Tc |
Ec |
B0 |
O1 |
F0 |
simultaneous Combined Approach |
| 48 |
48 |
M |
Tc |
Ec |
B0 |
O1 |
F0 |
Nasal Approach Only |
| 49 |
51 |
F |
Tc |
Ec |
B1 |
O0 |
F0 |
Nasal Approach Only |
| 50 |
57 |
M |
Tc |
Ec |
B0 |
O1 |
F0 |
Nasal Approach Only |
| 51 |
73 |
M |
Tc |
Ec |
B0 |
O0 |
F0 |
Oral Approach Only |
| 52 |
61 |
|
Tc |
Ec |
B0 |
O0 |
F0 |
Oral Approach Only |
| 53 |
48 |
M |
Tc |
Ec |
B0 |
O0 |
F0 |
Nasal Approach Only |
| 54 |
69 |
M |
Tc |
Ec |
B0 |
O1 |
F0 |
Nasal Approach Only |
| 55 |
55 |
F |
Tc |
Ec |
B0 |
O1 |
F0 |
Nasal Approach Only |
| 56 |
53 |
F |
Tc |
Eb |
B1 |
O0 |
F0 |
simultaneous Combined Approach |
| 57 |
67 |
F |
Tc |
Ec |
B1 |
O1 |
F1 |
Oral Approach Only |
| 58 |
63 |
M |
Tc |
Ec |
B1 |
O0 |
F1 |
Oral Approach Only |
| 59 |
42 |
M |
Tc |
Eb |
B1 |
O0 |
F0 |
Oral Approach Only |
| 60 |
70 |
M |
Tc |
Ec |
B0 |
O1 |
F0 |
Oral Approach Only |
| 61 |
51 |
M |
Tc |
Ec |
B0 |
O0 |
F1 |
Oral Approach Only |
| 62 |
46 |
M |
Tc |
Ec |
B0 |
O0 |
F0 |
Oral Approach Only |
| 63 |
78 |
M |
Tc |
Ec |
B0 |
O0 |
F0 |
Oral Approach Only |
| 64 |
39 |
M |
Tc |
Ec |
B0 |
O0 |
F0 |
simultaneous Combined Approach |
| 65 |
52 |
M |
Tc |
Ec |
B0 |
O0 |
F0 |
Nasal Approach Only |
| 66 |
76 |
F |
Tc |
Ec |
B0 |
O1 |
F0 |
Nasal Approach Only |
| 67 |
59 |
F |
Tc |
Ec |
B0 |
O1 |
F0 |
Nasal Approach Only |
| 68 |
48 |
M |
Tc |
Ec |
B0 |
O0 |
F1 |
simultaneous Combined Approach |
| 69 |
42 |
M |
Tc |
Ec |
B0 |
O1 |
F0 |
simultaneous Combined Approach |
| 70 |
57 |
F |
Tc |
Ea |
B1 |
O0 |
F1 |
simultaneous Combined Approach |
| 71 |
45 |
F |
Tc |
Ec |
B0 |
O1 |
F1 |
simultaneous Combined Approach |
| 72 |
72 |
F |
Tc |
Ec |
B0 |
O1 |
F1 |
simultaneous Combined Approach |
| 73 |
65 |
M |
Tc |
Ec |
B0 |
O1 |
F0 |
simultaneous Combined Approach |
| 74 |
49 |
M |
Tc |
Ec |
B0 |
O1 |
F0 |
simultaneous Combined Approach |
| 75 |
51 |
F |
Tc |
Eb |
B1 |
O1 |
F1 |
simultaneous Combined Approach |
| 76 |
48 |
F |
Tc |
Ec |
B0 |
O1 |
F0 |
Nasal Approach Only |
| 77 |
38 |
F |
Tc |
Ec |
B0 |
O1 |
F1 |
simultaneous Combined Approach |
| 78 |
66 |
F |
Tc |
Ec |
B0 |
O0 |
F1 |
simultaneous Combined Approach |
| 79 |
34 |
M |
Tc |
Ea |
B1 |
O1 |
F1 |
simultaneous Combined Approach |
| 80 |
69 |
F |
Tc |
Ec |
B0 |
O1 |
F1 |
Oral Approach Only |
| 81 |
53 |
F |
Tc |
Ea |
B0 |
O1 |
F0 |
Nasal Approach Only |
| 82 |
60 |
F |
Tc |
Ea |
B1 |
O1 |
F1 |
simultaneous Combined Approach |
| 83 |
74 |
M |
Tc |
Ec |
B0 |
O1 |
F1 |
simultaneous Combined Approach |
| 84 |
59 |
F |
Tc |
Ec |
B0 |
O1 |
F0 |
simultaneous Combined Approach |
| 85 |
45 |
F |
Tc |
Ea |
B1 |
O1 |
F1 |
simultaneous Combined Approach |
| 86 |
67 |
M |
Tc |
Ec |
B0 |
O0 |
F0 |
simultaneous Combined Approach |
| 87 |
62 |
F |
Tc |
Ec |
B0 |
O0 |
F0 |
simultaneous Combined Approach |
| 88 |
33 |
F |
Tc |
Ec |
B0 |
O0 |
F1 |
simultaneous Combined Approach |
| 89 |
49 |
M |
Tc |
Ec |
B1 |
O1 |
F0 |
simultaneous Combined Approach |
| 90 |
37 |
F |
Tc |
Ea |
B1 |
O0 |
F0 |
Oral Approach Only |
| 91 |
71 |
M |
Tc |
Ec |
B0 |
O1 |
F1 |
simultaneous Combined Approach |
| 92 |
54 |
M |
Tc |
Ec |
B0 |
O1 |
F1 |
simultaneous Combined Approach |
| 93 |
57 |
M |
Tc |
Ea |
B1 |
O1 |
F1 |
simultaneous Combined Approach |
| 94 |
66 |
F |
Tc |
Ea |
B1 |
O0 |
F1 |
simultaneous Combined Approach |
| 95 |
35 |
M |
Ta |
Eb |
B0 |
O1 |
F0 |
Nasal Approach Only |
| 96 |
33 |
M |
Tc |
Ec |
B0 |
O0 |
F0 |
Oral Approach Only |
| 97 |
75 |
F |
Tc |
Ec |
B0 |
O0 |
F0 |
Oral Approach Only |
| 98 |
49 |
F |
T0 |
Ea |
B1 |
O0 |
F1 |
Oral Approach Only |
| 99 |
51 |
F |
Tc |
Ec |
B1 |
O0 |
F0 |
Oral Approach Only |
| 100 |
61 |
F |
Tc |
Ec |
B1 |
O0 |
F0 |
Oral Approach Only |
| 101 |
61 |
M |
Tc |
Ec |
B0 |
O1 |
F0 |
Nasal Approach Only |
| 102 |
82 |
F |
Tc |
Ec |
B0 |
O1 |
F1 |
simultaneous Combined Approach |
| 103 |
52 |
F |
Tc |
Ec |
B0 |
O1 |
F0 |
simultaneous Combined Approach |
| 104 |
48 |
F |
Tc |
Ec |
B0 |
O1 |
F1 |
simultaneous Combined Approach |
| 105 |
66 |
M |
Tc |
Ec |
B0 |
O1 |
F1 |
simultaneous Combined Approach |
| 106 |
52 |
F |
Tc |
Ec |
B0 |
O1 |
F1 |
simultaneous Combined Approach |
| 107 |
57 |
M |
Tc |
Ec |
B1 |
O1 |
F1 |
simultaneous Combined Approach |
| 108 |
50 |
M |
Ta |
Ec |
B0 |
O1 |
F0 |
simultaneous Combined Approach |
| 109 |
74 |
F |
Tc |
Ec |
B0 |
O0 |
F1 |
Oral Approach Only |
| 110 |
55 |
M |
Tc |
Ec |
B0 |
O1 |
F0 |
simultaneous Combined Approach |
| 111 |
77 |
M |
Tc |
Ec |
B0 |
O0 |
F1 |
Oral Approach Only |
| 112 |
72 |
F |
Tc |
Ec |
B0 |
O0 |
F0 |
Oral Approach Only |
| 113 |
56 |
F |
Tc |
Ec |
B0 |
O0 |
F1 |
Oral Approach Only |
| 114 |
49 |
F |
Tc |
Ec |
B1 |
O1 |
F0 |
simultaneous Combined Approach |
| 115 |
58 |
F |
Tc |
Ec |
B0 |
O1 |
F0 |
simultaneous Combined Approach |
| 116 |
49 |
M |
Tc |
Ea |
B1 |
O1 |
F0 |
simultaneous Combined Approach |
| 117 |
43 |
F |
Tc |
Ec |
B0 |
O1 |
F1 |
Split Combined Approach |
| 118 |
54 |
M |
Tc |
Ec |
B0 |
O1 |
F1 |
simultaneous Combined Approach |
| 119 |
57 |
F |
Ta |
Ec |
B0 |
O1 |
F1 |
simultaneous Combined Approach |
| 120 |
74 |
F |
Ta |
Ea |
B0 |
O1 |
F0 |
Nasal Approach Only |
| 121 |
52 |
F |
Tc |
Ec |
B0 |
O1 |
F0 |
simultaneous Combined Approach |
| 122 |
67 |
F |
Ta |
Ea |
B0 |
O1 |
F1 |
simultaneous Combined Approach |
| 123 |
67 |
F |
Tc |
Ea |
B1 |
O1 |
F1 |
simultaneous Combined Approach |
| 124 |
69 |
M |
Tc |
Ec |
B1 |
O1 |
F0 |
simultaneous Combined Approach |
References
- M. Molteni et al., ‘Odontogenic sinusitis and sinonasal complications of dental treatments: a retrospective case series of 480 patients with critical assessment of the current classification’, Acta Otorhinolaryngol. Ital., vol. 40, no. 4, pp. 282–289, Aug. 2020. [CrossRef]
- U. Aksoy and K. Orhan, ‘Association between odontogenic conditions and maxillary sinus mucosal thickening: a retrospective CBCT study’, Clin. Oral Investig., vol. 23, no. 1, pp. 123–131, Jan. 2019. [CrossRef]
- T. Brandstaetter et al., ‘Perforating dental implants and maxillary sinus pathology’, Oral Maxillofac. Surg., vol. 28, no. 2, pp. 715–721, Nov. 2023. [CrossRef]
- L. Sabatino et al., ‘Odontogenic Sinusitis from Classical Complications and Its Treatment: Our Experience’, Antibiotics, vol. 12, no. 2, p. 390, Feb. 2023. [CrossRef]
- M. Troeltzsch et al., ‘Etiology and clinical characteristics of symptomatic unilateral maxillary sinusitis: A review of 174 cases’, J. Cranio-Maxillofac. Surg., vol. 43, no. 8, pp. 1522–1529, Oct. 2015. [CrossRef]
- A. Wuokko-Landén, K. Blomgren, A. Suomalainen, and H. Välimaa, ‘Odontogenic causes complicating the chronic rhinosinusitis diagnosis’, Clin. Oral Investig., vol. 25, no. 3, pp. 947–955, Mar. 2021. [CrossRef]
- K. L. Wang, B. G. Nichols, D. M. Poetker, and T. A. Loehrl, ‘Odontogenic sinusitis: a case series studying diagnosis and management’, Int. Forum Allergy Rhinol., vol. 5, no. 7, pp. 597–601, Jul. 2015. [CrossRef]
- J. R. Craig et al., ‘Diagnosing odontogenic sinusitis: An international multidisciplinary consensus statement’, Int. Forum Allergy Rhinol., vol. 11, no. 8, pp. 1235–1248, Aug. 2021. [CrossRef]
- L. Sabatino et al., ‘Odontogenic Sinusitis with Oroantral Communication and Fistula Management: Role of Regenerative Surgery’, Medicina (Mex.), vol. 59, no. 5, p. 937, May 2023. [CrossRef]
- F. Costa, E. Emanuelli, L. Franz, A. Tel, and M. Robiony, ‘Single-step surgical treatment of odontogenic maxillary sinusitis: A retrospective study of 98 cases’, J. Cranio-Maxillofac. Surg., vol. 47, no. 8, pp. 1249–1254, Aug. 2019. [CrossRef]
- J. E. Douglas et al., ‘Odontogenic Sinusitis is a Common Cause of Operative Extra-Sinus Infectious Complications’, Am. J. Rhinol. Allergy, vol. 36, no. 6, pp. 808–815, Nov. 2022. [CrossRef]
- M. Zirk et al., ‘Odontogenic sinusitis maxillaris: A retrospective study of 121 cases with surgical intervention’, J. Cranio-Maxillofac. Surg., vol. 45, no. 4, pp. 520–525, Apr. 2017. [CrossRef]
- G. Felisati et al., ‘Sinonasal Complications Resulting from Dental Treatment: Outcome-Oriented Proposal of Classification and Surgical Protocol’, Am. J. Rhinol. Allergy, vol. 27, no. 4, pp. e101–e106, Jul. 2013. [CrossRef]
- S. Di Girolamo et al., ‘Odontogenic Maxillary Sinusopathies: a Radiological Classification’, J. Maxillofac. Oral Surg., vol. 21, no. 1, pp. 141–149, Mar. 2022. [CrossRef]
- A. Oreški, T. Gregurić, P. Gulin, N. Prica Oreški, D. Brajdić, and D. Vagić, ‘Differences in self-reported symptoms in patients with chronic odontogenic and non-odontogenic rhinosinusitis’, Am. J. Otolaryngol., vol. 41, no. 2, p. 102388, Mar. 2020. [CrossRef]
- H. A. Newsome and D. M. Poetker, ‘Odontogenic Sinusitis’, Immunol. Allergy Clin. North Am., vol. 40, no. 2, pp. 361–369, May 2020. [CrossRef]
- B. J. Yoo, S. M. Jung, H. N. Lee, H. G. Kim, J. H. Chung, and J. H. Jeong, ‘Treatment Strategy for Odontogenic Sinusitis’, Am. J. Rhinol. Allergy, vol. 35, no. 2, pp. 206–212, Mar. 2021. [CrossRef]
- R. Aukštakalnis, R. Simonavičiūtė, and R. Simuntis, ‘Treatment options for odontogenic maxillary sinusitis: a review’, Stomatologija, vol. 20, no. 1, pp. 22–26, 2018.
- Y. Hara et al., ‘A large-scale study of treatment methods for foreign bodies in the maxillary sinus’, J. Oral Sci., vol. 60, no. 3, pp. 321–328, 2018. [CrossRef]
- M. A. Lopez et al., ‘Closure of oroantral communications using heterologous biomaterials stabilized by porcine cortical lamina: A case series’, Am. J. Dent., vol. 37, no. SIA, pp. 33A-36A, Sep. 2024.
- P. C. Passarelli et al., ‘Closure of small oroantral communications using heterologous biomaterials: A case series’, Am. J. Dent., vol. 37, no. SIA, pp. 29A-32A, Sep. 2024.
- R. R. Y Baena, S. M. Lupi, R. Pastorino, C. Maiorana, A. Lucchese, and S. Rizzo, ‘Radiographic Evaluation of Regenerated Bone Following Poly(Lactic-Co-Glycolic) Acid/Hydroxyapatite and Deproteinized Bovine Bone Graft in Sinus Lifting’:, J. Craniofac. Surg., vol. 24, no. 3, pp. 845–848, May 2013. [CrossRef]
- K. Nelke et al., ‘Anatomical and Surgical Implications of the Usage of Bichat Fat Pad in Oroantral Communication, Maxillary, Palatal, and Related Surgeries—Narrative Review’, J. Clin. Med., vol. 12, no. 15, p. 4909, Jul. 2023. [CrossRef]
|
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2025 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (http://creativecommons.org/licenses/by/4.0/).