Introduction
Dental implants are the optimal treatment for replacing missing teeth. Widely employed in dentistry, they provide a reliable restorative solution after tooth extraction, offering high success and survival rates in terms of aesthetics and patient satisfaction. The success of dental implants is based on the principle of osseointegration, a concept introduced by Branemark, who defined it as "a functional and structural union between the living bone and the implant,which is considered a critical factor in implant stability [
1].
Although dental implants generally exhibit a high success rate, there remains a risk of implant failure. Implant failure occurs when an implant does not achieve its functional or aesthetic objectives due to biological or mechanical complications. Biological complications, which affect the supporting tissues of the dental implant include peri-implant mucositis. Mechanical complications, on the other hand, compromise the structural integrity of the implant or the abutment of the prosthesis superstructure and can be classified into three categories: (i) implant-related issues, such as implant fractures; (ii) connection-related issues, including loosening in the prosthesis or abutment, screw fractures, and abutment fractures; and (iii) supra-structure-related issues, such as metal framework fractures worn materials, acrylic resin base fractures in implant overdentures, veneer porcelain fractures and prosthetic material failure [
2].
Mechanical problems may occur due to occlusal overload, excessive muscle of mastication exertion, or design faults. Occlusal overload can be caused by factors such as immediate-loading designs, large cantilevers, steep cuspal inclinations, occlusal interferences, and parafunctional habits including bruxism. Although implants are structurally robust enough to withstand significant masticatory forces, implant abutment fractures have been seen, that is caused by screw loosening or abutment micromovements. The incidence of loosening has been observed in 25% of patients during routine follow-up, particularly with single-tooth implants. The reported incidence of abutment or screw fractures ranges from 0.35% to 0.5% [
3].
Screw loosening may be related to the tightening technique or insufficient torque. It considered one of most common mechanical complication which occurs initially due to external forces, such as masticatory forces applied to the screw, causing slippage and subsequent release of screw's preload. In the second stage a continuous reduction in preload below a critical permits thread rotation, ultimately resulting in the failure of intended screw joint connection. Posterior abutment screws exhibit a higher rate of loosening compared to anterior implants. This finding underscores the importance of unnecessary occlusal and off-axial forces on implant-supported restorations [
4,
5]
.
Factors influencing abutment screw loosening include:
Screw Length: Longer screws with more threads improve retention. A minimum screw length of 1.4 mm (0.5) was utilized.
Angulation of the Abutment: Angulated abutments show greater screw loosening compared to straight implants.
Implant Diameter: Implants with wider diameters tend to experience more screw loosening than standard ones.
Abutment Screw Retightening: Retightening the screw 10 minutes after the initial torque is recommended as a standardized implant placement protocol.
Lateral Screw Loosening: Lateral forces applied to implants increase the risk of screw loosening [
6].
One of the most frequent outcomes of screw loosening is the occurrence of biological complications at the implant abutment interface, permitting bacterial leakage through the interface. bacterial infiltration, coupled with the mechanical issues caused by screw loosening, can lead to peri-implant bone loss and the presence of infiltrates, ultimately resulting in implant fracture and subsequent implant failure [
7].
The present study highlights the importance of treatment abutment screw fracture to preserve integrity of implant.
Case Report
A 52-year-old female patient presented in March 2025 with complaints of mobility of the upper bridge supported implants caused by a fractured abutment screw, with its apical portion remaining threaded within the implant. Patients is good and fit systemic health with good oral hygiene. Clinical examination revealed that the remaining fragment of the screw was minimal, positioned far from the implant neck, and difficult to remove. The implant was placed one year ago. The portion of the implant was clinically visible; however, radiographic evaluation demonstrated a fracture in the apical one-third of the fixture. The images showed the presence of a cylindrical form implant, resembling an 10 mm long, 4 mm abutment with an internal hex implant, appearing to be well-positioned in all dimensions mesiodistal, buccolingual, and apicocoronally without any radiographic indication of damage to the implant.
Technique for Retrieval of Abutment Screw [7]:
Assess the location of the fractured abutment, either clinically or radiographically by determining whether the fracture part is above or below the implant head.
As the abutment screw fractures below the implant platform, Ultrasonic tip used counterclockwise for retrieving broken fragments under copious irrigation to avoid thermal damage to the surrounding bone. This is considering a straight forward noninvasive method.
If the fracture screw still difficult to remove it entirely from the fixture. A cotton swab employed to extract the fragment. Oblique fractures in cotton swab may be more easily managed to help wedging the screw within the oblique part of the wooden swab.
Finally healing abutment diameter 4 x 2 mm placed in implant to regain emergence profile until new restoration fabrication.
advantages of this technique: Cost-effective and readily available in every clinic.
Figure 1.
Clinical photograph showing dental implant placement surgically.
Figure 1.
Clinical photograph showing dental implant placement surgically.
Figure 2.
Clinical photograph showing dental implant placement surgically.
Figure 2.
Clinical photograph showing dental implant placement surgically.
Figure 3.
Radiographic photo of inserted implants with final abutment in place before fracture.
Figure 3.
Radiographic photo of inserted implants with final abutment in place before fracture.
Figure 4.
clinical photo showing final restoration.
Figure 4.
clinical photo showing final restoration.
Figure 5.
Radiographic photo show Fracture abutment screw after 1year of implant placement. .
Figure 5.
Radiographic photo show Fracture abutment screw after 1year of implant placement. .
Figure 6.
Ultrasonic tip and cotton picks application.
Figure 6.
Ultrasonic tip and cotton picks application.
Results
The ultrasonic tip technique has a significant impact by providing a safe and conservative method for removing fractured screw abutments from dental implants.
This approach allows reuse of the same implant without causing trauma or imposing burdens on the patient.
Managing fractured implant abutment screws poses a confusing situation for clinicians, particularly given the lack of established protocols regarding the treatment plan.
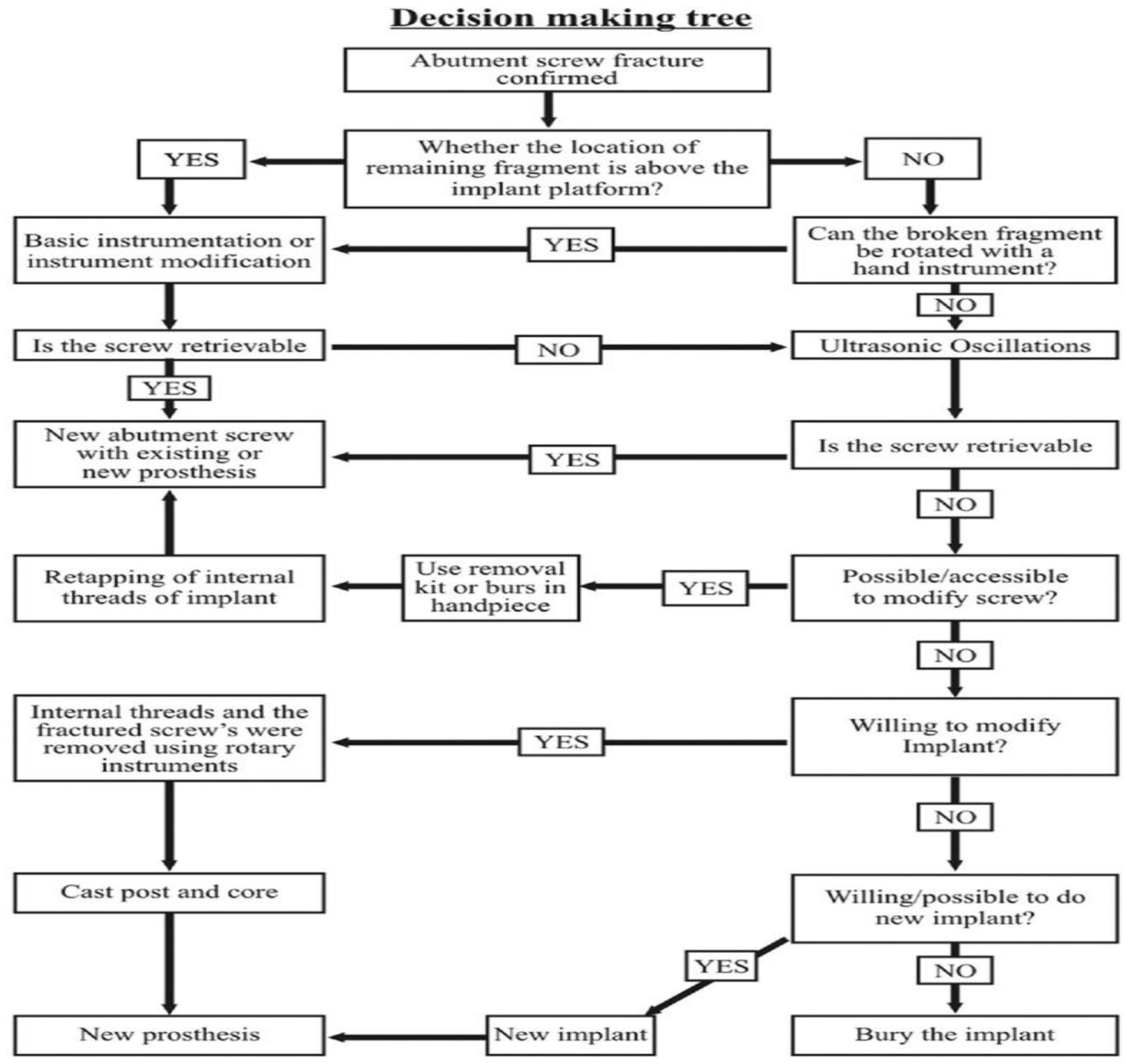
Implementing a decision-making framework may offer a structured approach to addressing fractured abutment screws. According to this framework, the techniques for retrieving the fractured site depend on its location relative to the screw head. If the fractured abutment screw fragment cannot be removed, clinicians may opt to either remove the implant and replace it with a new one or abandon the implant and cover it with soft tissue. However, many may avoid choosing a new implant due to its high cost and the need for another surgical procedures.
Figure 7.
Decision tree of retrieve fractured implant abutment screws.
Figure 7.
Decision tree of retrieve fractured implant abutment screws.
Discussion
The initial step in managing a fractured screw involves obtaining a detailed patient history and conducting a comprehensive clinical examination. Identifying the cause of the screw fracture is crucial to reducing the likelihood of subsequent complications. In most cases, abutment screw loosening precedes the fracture. The etiology is multifactorial and may include inadequate treatment planning and design, component misfit, insufficient screw tightening, excessive loading due to occlusion type, occlusal design, and parafunctional habits.
Tabrizi et al. and Lee et al. [
7,
8] have both highlighted impact of excessive occlusal load, particularly in molar and premolar regions, is a significant factor contributing to implant failure.
Inadequate treatment planning and design may arise from improper patient assessment or an insufficient number and placement of implants. After identifying the cause of the fracture, the next step is to verify presence of a fractured component and determine the fracture location. Fractures typically occur at junction between the screw head and the screw shank or between the screw shank and the screw thread. Confirmation a screw fracture can be through direct visualization, radiographic examination, tactile using an instrument, or comparing it with an intact screw from the same system to identify potential obstructions hindering complete seating. A fractured abutment screw must be removed without causing damage to the implant body, allowing it to be replaced with a new abutment so the implant can continue to retain the prothesis [
6].
Managing abutment screw fractures is challenging, occlusal forces can wedge the fractured abutment into the implant, necessitating a high pull-out force. The presence of saliva, blood, and limited surgical visibility further complicates access. In such cases, conservative retrieval is always the preferred initial treatment option. According to the proposed decision-making tree, the methods for retrieving broken fragments or screws depend on the location of the fractured abutment, whether it is above or below the implant head. If an abutment screw fractures above the implant head, tools such as an explorer, straight probe, or hemostat can be utilized. The tip of the instrument is carefully maneuvered in a counterclockwise direction over the surface of the screw segment until it loosens. When the abutment screw fractures below the implant platform, the recommended approach involves using instruments such as ultrasonic tip, sickle explorer, or orthodontic tool in a similar manner. Care must be taken to prevent tip breakage. Occasionally, even if the screw becomes loosened, it may still be difficult to remove it entirely from the fixture. In such cases, a cotton swab can be employed to extract the fragment. Oblique fractures may be more easily managed with technique, as a purchase point often exists where the instrument can engage. Ultrasonic, combined with hand instruments, serves as an auxiliary method for removing a fractured abutment screw fragment that cannot be retrieved with hand instruments alone. Thin scaler tips operating in counterclockwise oscillation may assist in backing out the fragment, but caution must be exercised to avoid wedging the screw further. These methods are gentle and pose minimal risk, as they do not damage the internal threads of the implant or raise the temperature, which could affect the surrounding bone. The procedure was deemed successful; the screw fragment was retrieved within 15 minutes without causing damage to the screw channel of the dental implant. If the internal component of the implant is damaged or the screw fragment cannot be retrieved, the clinician may need to remove the implant and replace it with a new one. However, this may depend on various factors, including the patient's experience and their willingness to undergo additional surgery [
9,
10,
11]. The level of operator experience was found to have no impact on their ability to retrieve fractured abutment screws. This finding further supports the notion that successful retrieval of abutment screw fragments primarily depends on visibility and access [
12].
To address screw fractures, prevention is essential. Implant planning, which includes considerations of implant design, diameter, and occlusal factors, plays a significant role in minimizing risks.
Preventive Management
In clinical practice, it is recommended to reduce the effect by retightening implant screws 10 minutes after the initial torque application.
Mechanical torque gauges should be used instead of hand drivers for consistently tightening of implant components to the recommended torque values.
The use of sealers to fill gaps between screws and implant threads, as well as adhesives to increase frictional resistance, has been suggested to minimize screw loosening. Ceka Bond (Preat, San Mateo, CA) is listed as an adhesive paste on the package.
Conclusion
The use of osseointegrated implants to replace missing natural teeth has become a well-established clinical protocol in dentistry.
Although implant fractures are rare, they are regarded as a serious complication that results in implant failure. Therefore, prevention is mandatory and depends on precise diagnosis, proper case selection, careful treatment planning, and thorough maintenance.
The retrieval of a fractured screw is considered one of the most challenging scenarios. A decision-making tree serves as a valuable tool to guide clinicians in managing abutment screw fractures and ensuring the successful rehabilitation of the implant.
Recommendation
To use dental loupes with a coaxial or light-emitting diode headlamp, or a dental surgical microscope, is highly recommended in cases of deep fractures to improve visualization.
Further research in this area is recommended to highlight the challenges or simplicity involved in retrieving fractured abutment screws with different techniques applied.
Funding
no external funding.
Ethics Statement
Ethical approval for the study was obtained according to the ethical committee Faculties of Dental Medicine, Al-Azhar University.
Statement of informed consent
was taken from the patient about the method of trial and the suspected publishing.
Data Availability
Public available.
Conflicts of Interest
The authors declare no conflict of interest.
References
-
Peitsinis, Panagiotis Rafail, et al. "Optimizing Implant Placement Timing and Loading Protocols for Successful Functional and Esthetic Outcomes: A Narrative Literature Review." Journal of Clinical Medicine 14.5 (2025): 1442. [CrossRef]
-
Pereira, Rafael & Sabri, Hamoun & Nava, Paolo & Alrmali, Abdusalam & Wang, Hom-Lay. Treatment Strategies for Peri-Implant Mucositis: The Final Stop for Preventing Peri-Implantitis. International Journal of Dentistry. 2025. [CrossRef]
-
Choi, Sunyoung, Young Suk Kang, and In-Sung Luke Yeo. "Influence of implant–abutment connection biomechanics on biological response: a literature review on interfaces between implants and abutments of titanium and zirconia." Prosthesis 5.2 (2023): 527-38. [CrossRef]
- Abdelfattah, MY. Abdelfattah MY. Different mechanical complications of implant prosthodontics. Int J Dent Res. 2014;2(6):190-6.
-
Barreiros P, Neves L, Aroso C, Mendes JM, Silva AS. Comparison in four different implant systems of mechanical resistance to maximal stress in prosthetic screws—an in vitro study. Dentistry Journal. 2020 Oct 9;8(4):116. [CrossRef]
-
Alsubaiy EF. Abutment screw loosening in implants: A literature review. Journal of Family Medicine and Primary Care. 2020 Nov 1;9(11):5490-4. [CrossRef]
-
Nayana P, Nayak SS, Chatterjee A, Sivaraman K, Srikanth G, Singh C. Retrieval of fractured implant abutment screws: a narrative review. Journal of International Society of Preventive and Community Dentistry. 2022 May 1;12(3):287-94.
-
Tabrizi, R.; Behnia, H.; Taherian, S.; Hesami, N. What Are the Incidence and Factors Associated With Implant Fracture? J. Oral Maxillofac. Surg.2017, 75, 1866–72. [CrossRef]
-
Lee, J.H.; Kim, Y.T.; Jeong, S.N.; Kim, N.H.; Lee, D.W. Incidence and pattern of implant fractures: A long-term follow-up multicenter study. Clin. Implant Dent. Relat. Res. 2018, 20, 463–9. [CrossRef]
-
Raju S, Nair VV, Karunakaran HK, Manjuran NG. Management of perishing implants with abutment screw fracture–A systematic review. The Journal of Indian Prosthodontic Society. 2021 Jul 1;21(3):229-39.
-
Martínez-Alcaraz P, Flores-Fraile J, Agustín-Panadero R, Senent-Vicente G, Gómez-Polo C, de la Cruz-Jiménez S, et al. Retrievability of Fractured Abutment Screws and Damage to Implant–Abutment Connections: An In Vitro Comparative Analysis of Conventional vs. Drilling Techniques. Applied Sciences. 2024 Dec 18;14(24):11846.
-
Moorthy A, Aljudaibi S, Donnelly-Swift E, Polyzois I, Grufferty B. An in vitro evaluation of 2 methods for retrieving fractured abutment screw fragments from the intaglio of 4 different implant systems. The Journal of Prosthetic Dentistry. 2024 Feb 1;131(2):282-90. [CrossRef]
-
Agustín-Panadero R, Baixauli-López M, Gómez-Polo M, Cabanes-Gumbau G, Senent-Vicente G, Roig-Vanaclocha A. In vitro comparison of the efficacy of two fractured implant-prosthesis screw extraction methods: Conventional versus mechanical. The Journal of Prosthetic Dentistry. 2020 Dec 1;124(6):720-6. [CrossRef]
-
Sane VD, Nair VS, Khandelwal S, Sane RV. A clinical tip for conservative retrieval of fractured abutment screw. The Journal of Indian Prosthodontic Society. 2023 Oct 1;23(4):398-400. [CrossRef]
|
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2025 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (http://creativecommons.org/licenses/by/4.0/).