Introduction
Large macular holes present a profound and complex challenge within the domain of ocular pathology, particularly when they manifest as sizable, unresponsive entities, necessitating alternative treatment strategies. Despite significant advances in the technique of internal limiting membrane (ILM) inversion, the closure of these substantial macular defects continues to represent a formidable obstacle to therapeutic success [
1,
2]. The persisting intricacy in achieving closure for large macular holes has catalyzed exploration into diverse and innovative surgical methodologies aimed at augmenting treatment efficacy and outcomes [
3,
4]. Within this evolving landscape of inquiry and experimentation, the utilization of amniotic membrane coverage as a therapeutic modality for addressing intractable large macular holes has emerged as a promising avenue warranting further investigation and optimization. Against this nuanced backdrop, the primary objective of the ongoing research endeavor is to meticulously assess the therapeutic effectiveness of this novel approach in facilitating successful closure of macular holes and in improving visual outcomes in individuals afflicted with refractory stage 4 macular holes, thereby enhancing the scope of treatment options available for this challenging clinical entity.
Treating recurrent macular holes, especially those that are refractory, following prior internal limiting membrane (ILM) peeling can pose challenges. Previous reports have explored various treatment approaches beyond ILM flap transplantation, such as utilizing a lens capsule flap or embedding an amniotic membrane, similar to our study [
5,
6,
7,
8,
9,
10]. However, there have been no reports on in this Japanese subjects regarding this matter.
This study is the first to report the use of amniotic membranes for surgical treatment of refractory macular holes in Japanese patients.
Materials and Methods
Ethical Approval
This retrospective cohort study was approved by our institution’s committee (Tohankai Eye Institutions Ethics Committee, approval number 0003, April 30st, 2023) and adhered to the regulations of clinical practice and tenets of the Declaration of Helsinki. The authors had access to information that could identify individual participants during and after the data collection. Informed consent was obtained from all participants in the study. The data for our research purposes were accessed on June 1, 2024. During the data collection process, the authors did not have access to any information to identify individual participants. All the data were anonymized to ensure confidentiality.
Study Design
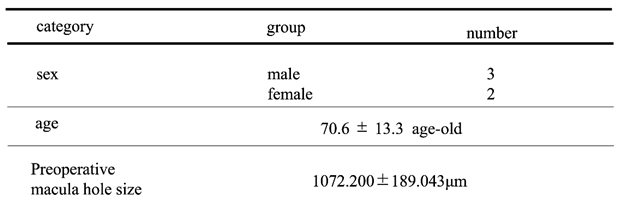
In a comprehensive retrospective analysis, five eyes of five patients were examined intricately. The demographic composition of the cohort included three males and two females, with an average age of 70.6 ± 13.3 years old. All patients presented with challenging large stage 4 macular holes (MH) > 400 μm that had exhibited resistance to closure despite undergoing the conventional procedure of internal limiting membrane (ILM) inversion (table1). This meticulous study spanned a significant duration from June 2022 to May 2024, with patients undergoing postoperative monitoring for a duration exceeding 6 months. Prior to the surgical intervention, thorough preoperative assessments of the macular hole dimensions were meticulously conducted leveraging the advanced imaging modality of optical coherence tomography (Cirrus HD-OCT; Carl Zeiss Meditec, Dublin, CA).
Surgical Procedure
The surgical protocol employed a precise 27-gauge transconjunctival vitrectomy approach using a Constellation Vision System (Alcon, Tokyo, Japan) without the customary step of ILM peeling, introducing a novel aspect to the operative technique. A sophisticated and innovative double-headed approach was adopted for the implementation of amniotic membrane coverage, showcasing a pioneering method in which two layers of amniotic membrane are delicately positioned at the precise center of the macular region under a dispersed viscoelastic material (Viscoat, Alcon). After sealing the macular hole with an amniotic membrane incorporating Viscoat, slow air exchange was performed, and the procedure was concluded with a 20% SF6 gas tamponade.
Statical Analysis
To assess the difference in visual acuity before and after surgery, we performed non-parametric statistical analysis using the Mann-Whitney U test. This test was chosen because of the small sample size and non-normal distribution of data. The statistical software used for these analyses was StatPlus (AnalystSoft Inc. Manhattan, New York).
Results
Table 1 presents a summary of patient demographics, including age, sex, and preoperative macular hole size. Preoperative evaluation of the patients in this study revealed intriguing findings that shed light on the intricate details of their ocular pathology. Specifically, the mean macular hole size was measured to be 1072.200 ± 189.043 μm, indicating significant variability within the patient cohort. This quantitative assessment provides a quantitative basis for understanding the extent of the macular holes and serves as a crucial parameter for tracking changes over time.
Furthermore, the preoperative logMAR visual acuity, a key metric of visual function, was reported to be 1.222 ± 0.278. This preoperative visual acuity data highlighted the challenges faced by individuals with stage 4 macular holes, underscoring the impact of these ocular abnormalities on visual acuity and quality of life.
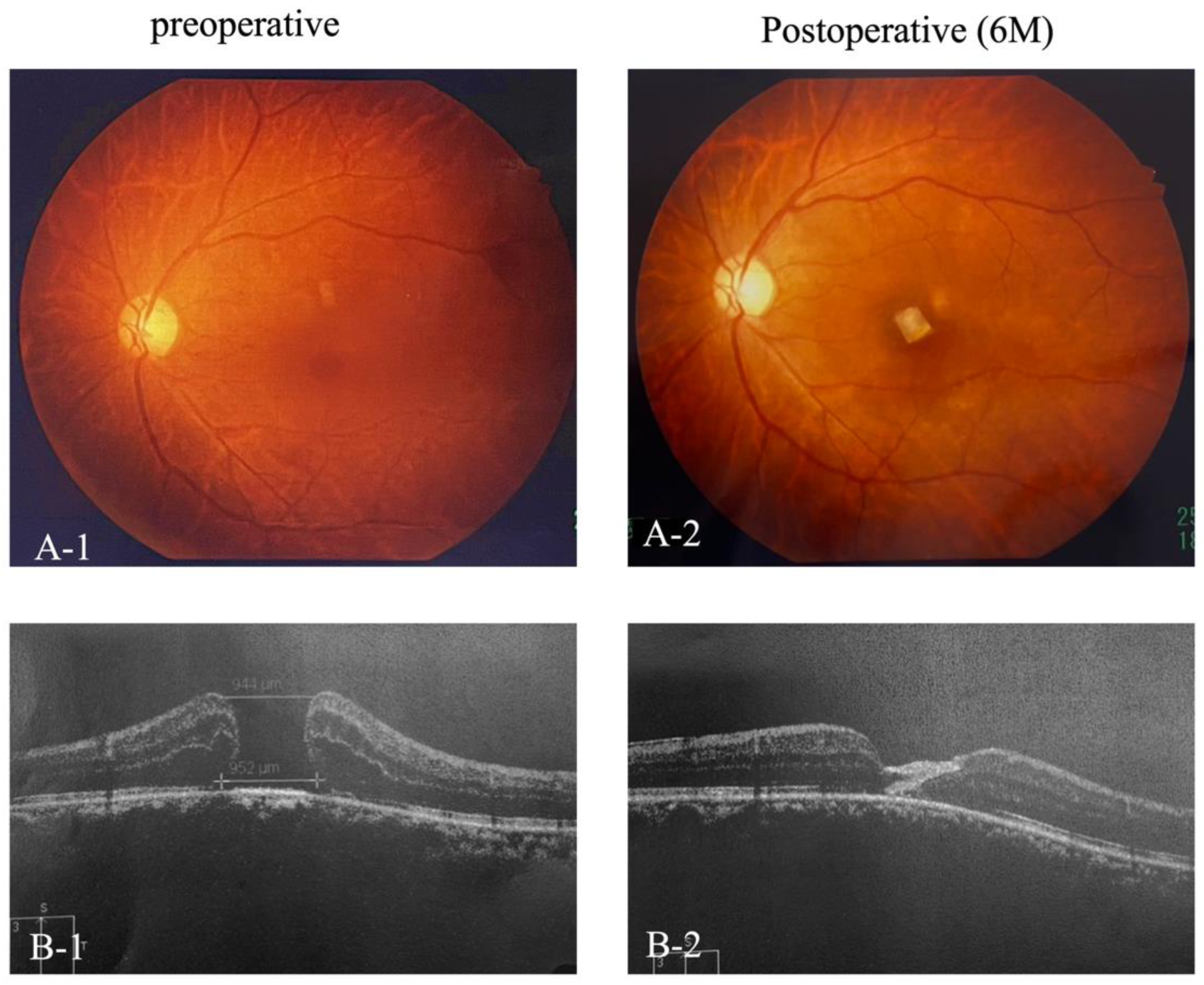
Following meticulous surgical interventions, all the macular holes in the study cohort achieved successful closure, marking a significant milestone in their clinical management. The fovea was covered by two layers of amniotic membrane, indicating closure of the macular hole on fundus photography and OCT (
Figure 1).
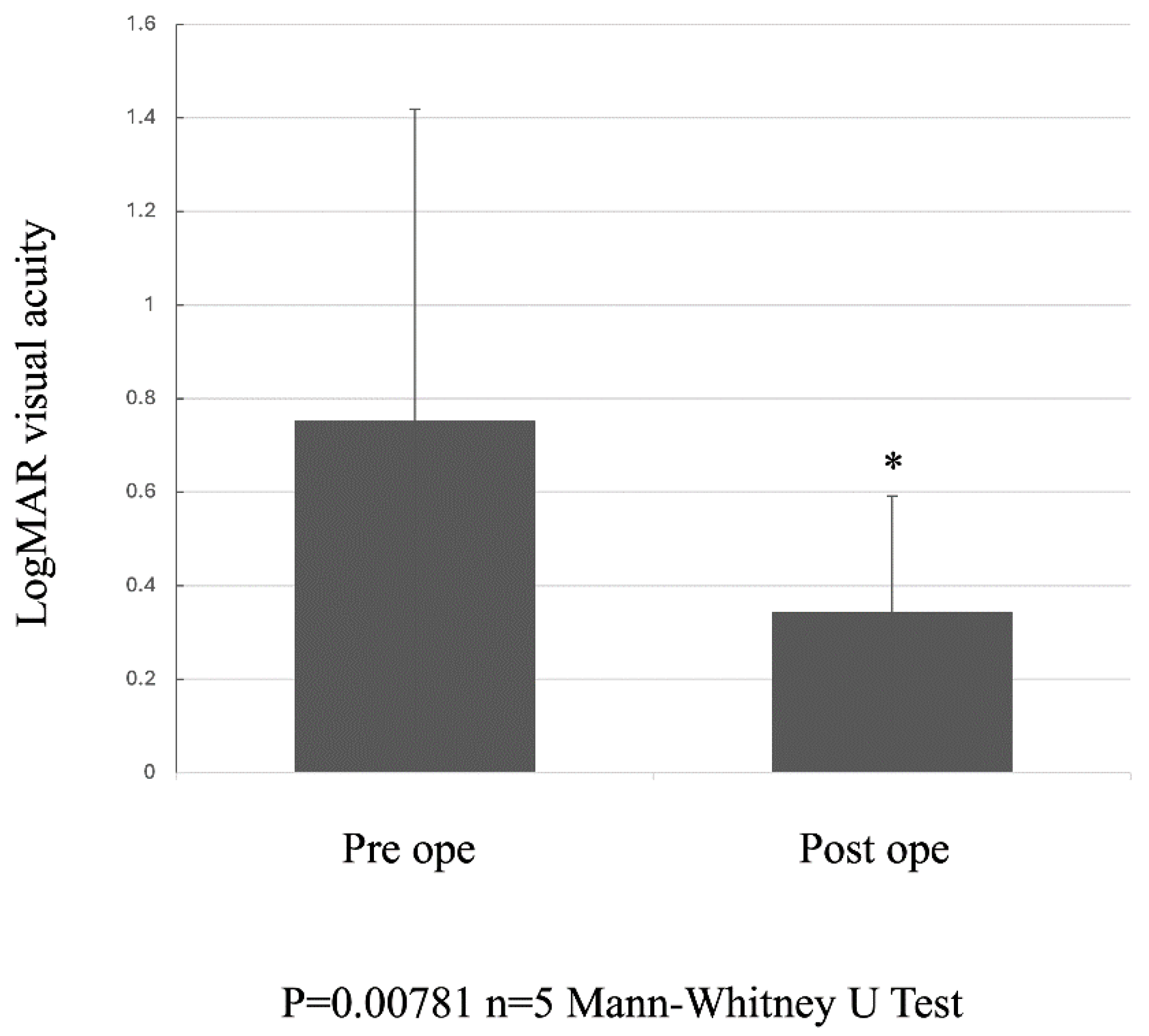
The postoperative logMAR visual acuity showed notable improvement, with a recorded value of 0.320 ± 0.110 at the 6-month follow-up period. The Mann-Whitney U was used to compare the medians of the two independent groups. The results showed a statistically significant difference between the preoperative (pre logMar) and postoperative (post logMar) visual acuity groups (U = 0.000, p = 0.00781) (
Figure 2).
This noteworthy enhancement in visual acuity underscores the positive outcomes resulting from the novel surgical approach employed in the treatment of these challenging cases.
The comprehensive data presented in this study provide valuable insights into the efficacy of the surgical techniques utilized and the resulting impact on visual outcomes in patients with stage 5 macular holes. These findings contribute to a growing body of knowledge aimed at enhancing the management and treatment of complex retinal pathologies, ultimately improving patient care and visual outcomes in this patient population.
Discussion
This study provides compelling evidence supporting the efficacy of amniotic membrane coverage as a novel surgical intervention for intractable large macular holes, particularly those that fail to close following internal limiting membrane (ILM) inversion. Our findings demonstrated a 100% closure rate with significant postoperative improvement in visual acuity, highlighting the potential of this approach to improve patient outcomes and expand the treatment options available for these challenging cases. This research represents a significant step forward in addressing the unmet needs of patients with intractable large macular holes, potentially offering a more effective and minimally invasive treatment modality.
Amniotic membrane is a multifaceted tissue that plays a crucial role in wound healing, particularly in ophthalmology. Its regenerative properties and anti-inflammatory effects make it a valuable tool for the treatment of various ocular conditions. The amniotic membrane promotes wound healing through a multifaceted mechanism involving the following:
Anti-inflammatory properties: The amnioticotic membrane effectively reduces inflammation by inhibiting the production of pro-inflammatory cytokines such as IL-1 and IL-6.. It also suppresses the release of chemoattractants, such as IL-8, which prevents the recruitment of inflammatory cells to the wound site. This anti-inflammatory effect minimizes the tissue damage caused by excessive inflammation, thus fostering a more conducive environment for healing [
11].
Growth factor and cytokine delivery: The amniotic membrane is a rich source of various growth factors such as epidermal growth factor (EGF), fibroblast growth factor (FGF), vascular endothelial growth factor (VEGF), and cytokines. These factors stimulate cell proliferation, migration, and differentiation, and promote tissue regeneration and angiogenesis. The presence of these bioactive molecules in the amniotic membrane expedites wound closure and tissue repair [
12].
Extracellular matrix remodeling: The amniotic membrane contains essential components of the extracellular matrix (ECM), such as collagen, elastin, and hyaluronic acid. These components provide structural support to the wound site and facilitate the formation of a new ECM, contributing to tissue repair and restoration of the normal tissue architecture [
13].
Immunomodulatory effects: Amniotic membranes have immunomodulatory properties that suppress immune responses and reduce the risk of rejection. This is achieved by inhibiting the activation of immune cells and promoting the production of anti-inflammatory cytokines. This makes it particularly useful for corneal transplantation, whichere rejection is a major concern [
14].
Anti-angiogenic effects: The amniotic membrane can suppress angiogenesis, which involves the formation of new blood vessels. This effect is particularly beneficial for treating conditions involving abnormal angiogenesis, such as diabetic retinopathy and corneal neovascularization [
15].
In essence, the amniotic membrane promotes wound healing through a multifaceted mechanism, including anti-inflammatory, growth factor delivery, extracellular matrix remodeling, immunomodulatory, and antiangiogenic effects. These properties make it a promising therapeutic tool for a variety of ocular conditions, particularly corneal wounds, inflammation, and neovascularization.
The successful closure of all macular holes in our study cohort underscores the potential of amniotic membrane coverage to overcome the limitations of conventional ILM peeling techniques in managing large, persistent macular holes. While previous studies have explored alternative treatment approaches, such as lens capsule flaps or amniotic membrane embedding, our findings demonstrate the efficacy of a unique double-headed technique, which involves placing two layers of amniotic membrane in the macular center [
16,
17,
18].
The postoperative improvement in visual acuity observed in our patient is particularly noteworthy. The significant reduction in LogMAR visual acuity suggests that amniotic membrane coverage not only promotes macular hole closure but also contributes to improved visual function. This finding aligns with the established benefits of the amniotic membrane in promoting tissue regeneration and reducing inflammation [
19,
20].
Although our results are promising, further investigations are needed to fully understand the mechanisms underlying the effectiveness of amniotic membrane coverage. It is essential to explore the role of amniotic membrane components such as growth factors and cytokines in promoting tissue healing and visual function recovery. Investigating the specific signaling pathways and cellular responses triggered by amniotic membrane components could provide valuable insights into the mechanisms of action [
21,22].
Furthermore, the optimal technique and placement of the amniotic membrane for intractable large macular holes require additional research. Investigating alternative techniques, such as single-layer placement or the use of different tamponade agents, could optimize the procedure and potentially improve the outcomes. Additionally, the use of different surgical approaches, such as combined ILM peeling and amniotic membrane coverage, could be investigated to maximize the benefits of this technique.
Although our study provides promising results, several limitations should be considered. The retrospective nature of this study limits the ability to draw definitive conclusions regarding the efficacy of amniotic membrane coverage. A prospective randomized controlled trial with a larger sample size would provide stronger evidence to support these findings and allow for a more robust assessment of the effectiveness and safety of this approach. A prospective study would also enable researchers to collect detailed data on patient demographics, preoperative characteristics, and long-term outcomes, thereby providing a more comprehensive understanding of the effects of treatment.
Additionally, our study included only five patients, which may not be representative of a broader patient population. Further research with larger and more diverse cohorts is necessary to validate the generalizability of our findings. Investigating the efficacy of amniotic membrane coverage in patients with different demographic characteristics such as age, sex, and underlying medical conditions would be valuable.
Despite these limitations, our findings contribute valuable information to the growing body of knowledge regarding the treatment of intractable large macular holes. The successful closure of all macular holes and the observed improvement in visual acuity in our study cohort warrants further investigation into amniotic membrane coverage as a promising surgical approach for treating these challenging cases.
Future research should address the limitations of this study. Prospective, randomized controlled trials with larger sample sizes are needed to confirm the efficacy of amniotic membrane coverage for intractable large macular holes and to elucidate the optimal surgical technique and placement. These trials should also include a comprehensive assessment of the long-term outcomes and safety of this approach, particularly with regard to potential complications such as retinal detachment or infection.
This research also underscores the importance of ongoing innovations in the field of ophthalmology, particularly in managing complex retinal pathologies. By exploring novel surgical approaches and leveraging the unique properties of materials such as amniotic membranes, we can continue to improve patient care and outcomes, ultimately enhancing the vision and quality of life of those suffering from challenging ocular conditions.
In conclusion, the application of amniotic membrane coverage in the treatment of intractable large macular holes demonstrates potential as an effective method for achieving macular hole closure and improving visual outcomes postoperatively. Further studies are warranted to confirm these findings and to elucidate the mechanisms underlying the success of this novel surgical approach. These studies could lead to significant advancements in the management of intractable large macular holes, providing patients with improved vision and quality of life.
Author Contributions
Y.H. performed surgery. Y. H. and T. I. conceived and designed the research and analyzed the data. Y. H. wrote the article. All the authors have read and approved the final manuscript.
Funding
This research received no external funding.
Institutional Review Board Statement
This retrospective cohort study was approved by our institution’s committee (approval number 0003, January 31,2023) and adhered to the regulations of clinical practice and the tenets of the Declaration of Helsinki.
Informed Consent Statement
Informed consent was obtained from all the participants.
Data Availability Statement
The datasets generated and analyzed during the current study are available from the corresponding author on reasonable request
Conflict of Interest Statement
The authors declare no conflicts of interest.
References
- Zong Y, Wu K, Yu J, Zhou C, Jiang C. Internal Limiting Membrane Peeling and Flap Inverting under Air in Large Idiopathic Macular Hole Surgery. J Ophthalmol. 2021;2021:2003001. Epub 2021 Sep 24. [CrossRef] [PubMed]
- Ramtohul P, Parrat E, Denis D, Lorenzi U. Inverted internal limiting membrane flap technique versus complete internal limiting membrane peeling in large macular hole surgery: a comparative study. BMC Ophthalmol. 2020;20(1):11. Epub 2020 Jan 6. [CrossRef] [PubMed]
- Liu L, Wang Z, Yu Y, Yang X, Qi B, Zhang K, Liu W. Microstructural and microperimetric comparison of internal limiting membrane peeling and insertion in large idiopathic macular hole. BMC Ophthalmol. 2023;23(1):274. Epub 2023 Jun 14. PMID: 37316769. [CrossRef]
- Galletero Pandelo L, Olaso Fernández H, Sánchez Aparicio JA, Rodríguez Vidal C, Martínez-Alday N. Results of large macular hole surgery using different interposition techniques. A report on 9 cases. Arch Soc Esp Oftalmol (Engl Ed). 2022;97(8):457-463. Epub 2022 Mar 21. [CrossRef]
- Zhang H, Li Y, Chen G, Han F, Jiang W. Human amniotic membrane graft for refractory macular hole: A single-arm meta-analysis and systematic review. J Fr Ophtalmol. 2023;46(3):276-286. Epub 2023 Feb 2. [CrossRef]
- Caporossi T, Tartaro R, Bacherini D, Pacini B, De Angelis L, Governatori L, Di Leo L, Oliverio L, Rizzo S. Applications of the Amniotic Membrane in Vitreoretinal Surgery. J Clin Med. 2020;9(8):2675. Epub 2020 Aug 18. [CrossRef] [PubMed]
- Bamberger MD, Felfeli T, Politis M, Mandelcorn ED, Galic IJ, Chen JC. Human Amniotic Membrane Plug for Chronic or Persistent Macular Holes. Ophthalmol Retina. 2022;6(5):431-433. Epub 2022 Jan 17. [CrossRef] [PubMed]
- Cisiecki S, Bonińska K, Bednarski M. Autologous Lens Capsule Flap Transplantation for Persistent Macular Holes. J Ophthalmol. 2021;2021:8148792. Epub 2021 Feb 27. [CrossRef] [PubMed]
- Yepez JB, Murati FA, De Yepez J, Petitto M, Arevalo JF. ANTERIOR LENS CAPSULE IN THE MANAGEMENT OF CHRONIC FULL-THICKNESS MACULAR HOLE. Retin Cases Brief Rep. 2018;12(4):286-290. Epub 2018 Fall. [CrossRef] [PubMed]
- Bhatia M, Pereira M, Rana H, Stout B, Lewis C, Abramson S, Labazzo K, Ray C, Liu Q, Hofgartner W, Hariri R. The Mechanism of Cell Interaction and Response on Decellularized Human Amniotic Membrane: Implications in Wound Healing. Wounds. 2007;19(8):207-17. Epub 2007 Aug. [PubMed]
- Grzywocz Z, Pius-Sadowska E, Klos P, Gryzik M, Wasilewska D, Aleksandrowicz B, Dworczynska M, Sabalinska S, Hoser G, Machalinski B, Kawiak J. Growth factors and their receptors derived from human amniotic cells in vitro. Folia Histochem Cytobiol. 2014;52(3):163-70. Epub 2014. [CrossRef] [PubMed]
- Rastegar Adib F, Bagheri F, Sharifi AM. Osteochondral regeneration in rabbit using xenograft decellularized ECM in combination with different biological products; platelet-rich fibrin, amniotic membrane extract, and mesenchymal stromal cells. J Biomed Mater Res B Appl Biomater. 2022;110(9):2089-2099. Epub 2022 Apr 5. [CrossRef] [PubMed]
- Kang JW, Koo HC, Hwang SY, Kang SK, Ra JC, Lee MH, Park YH. Immunomodulatory effects of human amniotic membrane-derived mesenchymal stem cells. J Vet Sci. 2012;13(1):23-31. Epub 2012 Mar. [CrossRef] [PubMed]
- Thomasen H, Pauklin M, Noelle B, Geerling G, Vetter J, Steven P, Steuhl KP, Meller D. The effect of long-term storage on the biological and histological properties of cryopreserved amniotic membrane. Curr Eye Res. 2011;36(3):247-55. Epub 2011 Jan 28. [CrossRef] [PubMed]
- Garcin T, Gain P, Thuret G. Femtosecond laser-cut autologous anterior lens capsule transplantation to treat refractory macular holes. Eye (Lond). 2023;37(6):1073-1079. Epub 2022 Apr. [CrossRef] [PubMed]
- Karanfil FC, Toklu Y, Yorgun MA. Amniotic Membrane Transplantation for Macular Hole Closure. Beyoglu Eye J. 2023;8(1):55-59. Epub 2023 Mar 1. [CrossRef] [PubMed]
- Felfeli T, Corrin M, Papanikolaou J, Mandelcorn ED. MACULAR HOLE HYDRODISSECTION TECHNIQUE WITH HUMAN AMNIOTIC MEMBRANE FOR REPAIR OF LARGE MACULAR HOLES. Retin Cases Brief Rep. 2023;17(6):767-770. Epub 2023 Oct 23. [CrossRef] [PubMed]
- Elkhenany H, El-Derby A, Abd Elkodous M, Salah RA, Lotfy A, El-Badri N. Applications of the amniotic membrane in tissue engineering and regeneration: the hundred-year challenge. Stem Cell Res Ther. 2022;13(1):8. Epub 2022 Jan 10. [CrossRef] [PubMed]
- Toda A, Okabe M, Yoshida T, Nikaido T. The potential of amniotic membrane/amnion-derived cells for regeneration of various tissues. J Pharmacol Sci. 2007;105(3):215-28. Epub 2007 Nov 6. [CrossRef] [PubMed]
- Ruiz-Cañada C, Bernabé-García Á, Liarte S, Insausti CL, Angosto D, Moraleda JM, Castellanos G, Nicolás FJ. Amniotic membrane stimulates cell migration by modulating transforming growth factor-beta signalling. J Tissue Eng Regen Med. 2018;12(3):808-820. Epub 2017 Oct 24. [CrossRef] [PubMed]
- Li JY, Ren KK, Zhang WJ, Xiao L, Wu HY, Liu QY, Ding T, Zhang XC, Nie WJ, Ke Y, Deng KY, Liu QW, Xin HB. Human amniotic mesenchymal stem cells and their paracrine factors promote wound healing by inhibiting heat stress-induced skin cell apoptosis and enhancing their proliferation through activating PI3K/AKT signaling pathway. Stem Cell Res Ther. 2019;10(1):247. Epub 2019 Aug 9. [CrossRef] [PubMed]
|
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2025 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (http://creativecommons.org/licenses/by/4.0/).