Introduction
Ensuring patient safety and enhancing healthcare quality are fundamental goals in healthcare systems worldwide. A strong patient safety culture, defined by organizational beliefs and values, plays a critical role in promoting safe practices and accountability [
1].
Active Occurrence Variance Reporting (OVR) and Safety Huddles are two pivotal components of quality improvement initiatives aimed at fostering a culture of transparency and reducing adverse events. OVR systems, which document deviations from standard procedures, enable healthcare organizations to identify patterns, determine root causes, and implement targeted interventions [
2,
3]. Research in high-risk industries highlights the benefits of active reporting systems, where fostering a reporting culture has been associated with improved safety outcomes [
4].
OVR systems capture a wide range of incidents, including deviations from protocols and expected outcomes. These systems often work alongside Medication Error Reports, which focus specifically on medication-related incidents, highlighting critical areas for targeted interventions within patient care [
5,
6]. Understanding the impact of these reporting mechanisms on patient experiences and perceptions of healthcare quality is essential for continuous improvement. Effective OVR implementation depends on timely and accurate reporting, thorough data analysis, root cause identification, and a structured approach to intervention and monitoring, which all play a role in sustaining patient safety and healthcare quality [
7].
In healthcare, active OVR systems have shown potential in reducing adverse events, length of stay, and mortality rates, while promoting transparency and accountability [
8]. Safety Huddles, brief structured meetings aimed at enhancing team communication and reviewing safety incidents, provide a framework for healthcare teams to collaboratively address patient safety risks [
9]. Together, OVR and Safety Huddles emphasize the importance of timely intervention, preventive action, and interprofessional collaboration, which are essential in addressing complex healthcare safety issues [
10]. However, the effectiveness of these interventions depends on factors such as staff engagement, organizational support, and a non-punitive reporting environment, highlighting the need for further investigation [
11,
12].
For an OVR system to be effective, several strategies should be implemented. Key strategies include clear communication of the purpose and benefits of variance reporting to all staff, supported by comprehensive training and education [
13,
17]. A user-friendly and accessible reporting system, whether electronic or paper-based, encourages consistent reporting. Establishing a blame-free reporting culture further ensures that staff can report incidents openly without fear of reprisal [
14]. Guidelines for reporting, including incident definitions and timelines, maintain consistency and accuracy in reporting. Additionally, regular review and analysis of incidents allow early detection of trends and identification of improvement areas. Employing data analysis tools aids in root cause identification and designing targeted interventions [
14]. Continuous education, such as safety walk-rounds and commendations for high reporting, reinforces the importance of reporting and strengthens adherence to best practices [
3,
15].
This study investigates the impact of OVR and Safety Huddles on key patient outcomes, including average length of stay (ALOS), mortality rates, sepsis mortality, hospital-acquired infection rates, and patient satisfaction. By employing a quantitative retrospective design, this research examines how these safety interventions may influence patient outcomes and improve the quality of care. Conducted in Imam Abdulrahman Al Faisal Hospital, Riyadh, Saudi Arabia, this study provides insights into the role of active OVR and Safety Huddles in enhancing healthcare performance and patient experience.
The findings are intended to inform healthcare stakeholders about the effectiveness of integrating variance reporting systems and team-based safety initiatives, offering evidence-based recommendations for fostering a safety-focused, transparent culture within healthcare settings.
Conceptual Framework
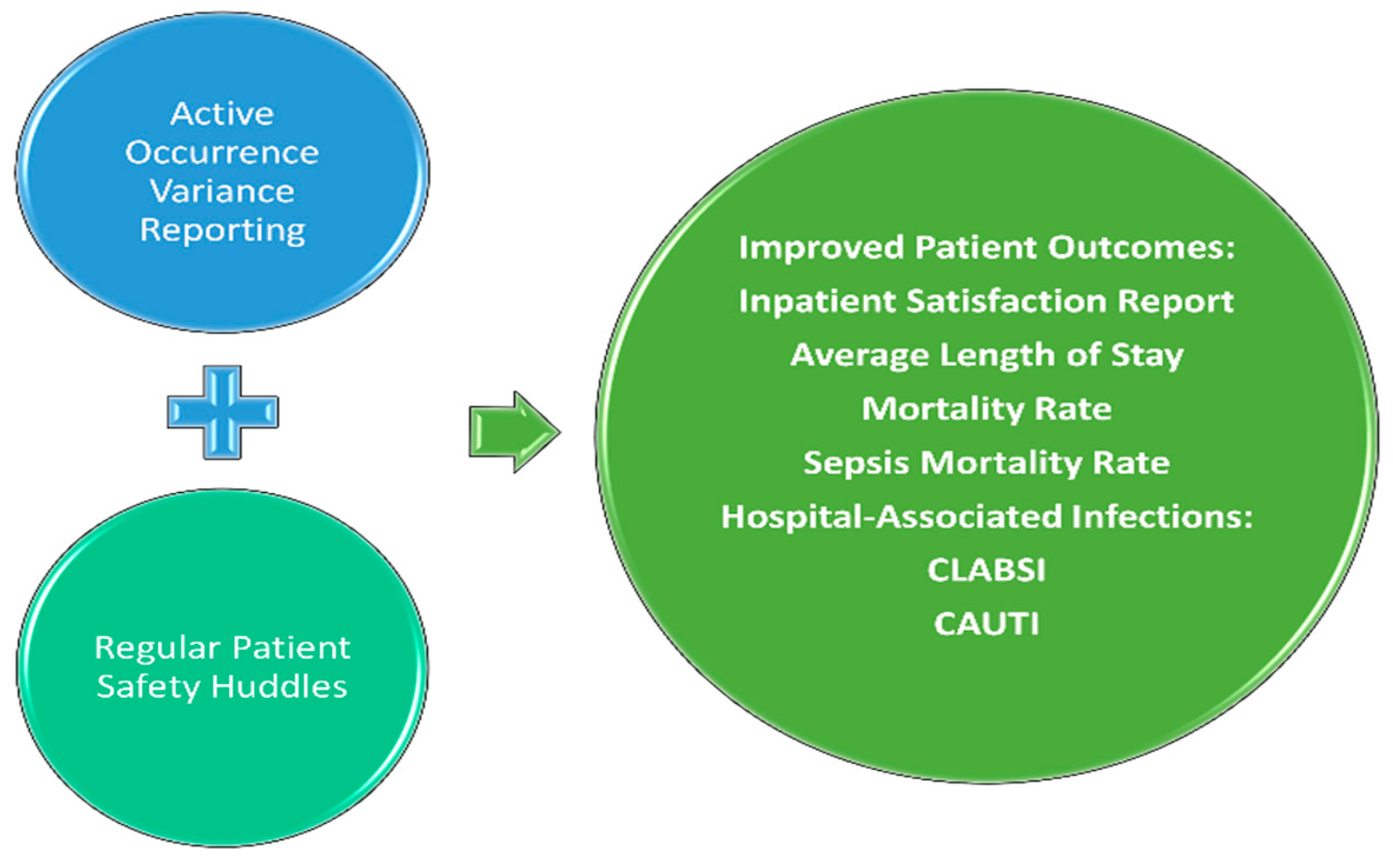
This study’s conceptual framework (
Figure 1) posits that
Active Occurrence Variance Reporting (OVR) and
Regular Patient Safety Huddles work synergistically to improve patient outcomes by fostering a proactive safety culture. OVR systems capture deviations from standard protocols, enabling targeted interventions, while Safety Huddles facilitate team-based communication and rapid response to safety issues. Together, these interventions are expected to enhance inpatient satisfaction, reduce average length of stay, lower mortality rates, and decrease hospital-associated infections such as CLABSI and CAUTI. This framework highlights the role of OVR and Safety Huddles in promoting transparency and accountability, ultimately contributing to improved clinical outcomes.
Aim of the Study
The primary aim of this study is to evaluate the impact of Active Occurrence Variance Reporting (OVR) and Safety Huddles on key patient outcomes, specifically focusing on average length of stay (ALOS), overall and sepsis-specific mortality rates, hospital-acquired infection rates (CLABSI and CAUTI), and patient satisfaction within a healthcare setting. By employing a quantitative retrospective design, this study seeks to explore potential correlations between these patient safety initiatives and clinical outcomes, offering insights into the effectiveness of OVR and Safety Huddles in fostering a transparent, safety-oriented culture. Ultimately, the findings aim to provide evidence-based recommendations to healthcare stakeholders for integrating these safety practices to improve patient outcomes and quality of care.
Methods
Study Design and Setting
This retrospective observational cohort study was conducted at Imam Abdulrahman Al Faisal Hospital, a Ministry of Health-affiliated government hospital in Riyadh, Saudi Arabia, over a two-year period from January 2022 to December 2023. The hospital operates as a regional referral center in an urban setting, offering comprehensive healthcare services. The study aims to evaluate the impact of Active Occurrence Variance Reporting (OVR) and Regular Patient Safety Huddles on patient outcomes, including length of stay, mortality rates, sepsis-specific mortality, hospital-associated infections, and patient satisfaction.
Data Collection
A census approach was used to collect data, ensuring the inclusion of all available OVR incidents, Safety Huddles, and relevant patient outcome data within the study period. Data on 10,736 OVR reports, 2,437 Safety Huddles, and outcome measures for 13,092 discharged patients were retrospectively extracted from the hospital’s incident reporting and clinical databases. Additional data on patient satisfaction were obtained through surveys administered by an independent third-party organization, covering a total of 2,471 patients.
Variables and Measures
The primary variables of interest included:
Active Occurrence Variance Reporting (OVR): Frequency of reported variance incidents.
Safety Huddles: Frequency of structured, team-based meetings focused on patient safety.
The outcome variables measured were:
Average Length of Stay (ALOS): Defined as the average number of days from patient admission to discharge.
Mortality Rate: Total in-hospital mortality rate and sepsis-specific mortality rate.
Hospital-Associated Infections: Incidence of central line-associated bloodstream infections (CLABSI) and catheter-associated urinary tract infections (CAUTI).
Patient Satisfaction: Percentage of patients reporting high satisfaction, as measured by standardized satisfaction surveys.
Data Analysis
Pearson correlation analysis was employed to examine the associations between OVR frequency, Safety Huddles, and patient outcome variables, with correlation coefficients calculated to assess relationships across various outcomes (ALOS, mortality rate, sepsis mortality, CLABSI, CAUTI, and patient satisfaction). While Pearson correlation was selected for its relevance to linear associations observed in initial data screening, future research may benefit from non-parametric or alternative regression models for outcomes that do not meet linear assumptions. All analyses were conducted using SPSS, with statistical significance set at p < 0.05.
Ethical Considerations
The study protocol was approved by the Institutional Review Board (IRB) of Imam Abdulrahman Al Faisal Hospital through King Saud Medical City. Patient confidentiality and data security were maintained in accordance with institutional guidelines and ethical standards. All patient data were anonymized before analysis, and data access was restricted to authorized personnel only.
Results
This study analyzed data from 2022 to 2023, capturing significant improvements in patient outcomes and safety activities at Imam Abdulrahman Al Faisal Hospital. Patient volume increased from 5,512 in 2022 to 7,580 in 2023, alongside a marked rise in Occurrence Variance Reporting (OVR) from 2,914 reports in 2022 to 7,822 in 2023, and Safety Huddles from 909 to 1,528 during the same period (
Table 1).
Key patient outcomes showed notable improvements, with the Average Length of Stay (ALOS) decreasing from 5.02 days in 2022 to 4.17 days in 2023, while mortality rate reduced from 3.56% to 2.19% and in-hospital sepsis mortality rate dropped significantly from 23% to 1.19%. Infection rates also showed favorable trends, with CLABSI and CAUTI rates declining from 1.4 to 0.61 and from 0.60 to 0.24, respectively. Patient satisfaction improved from 85.47% in 2022 to 88.12% in 2023, indicating enhanced patient experience as safety measures intensified (
Table 2).
Monthly Trends in Patient Outcomes
The study captured monthly trends in patient outcomes, showing significant improvements across key indicators such as length of stay and mortality rates, visualized in control charts (
Figure 2 and
Figure 3). While Pearson correlation provided insight into key associations, control charts helped verify trends over time, supporting the validity of observed relationships between OVR, Safety Huddles, and patient outcomes.
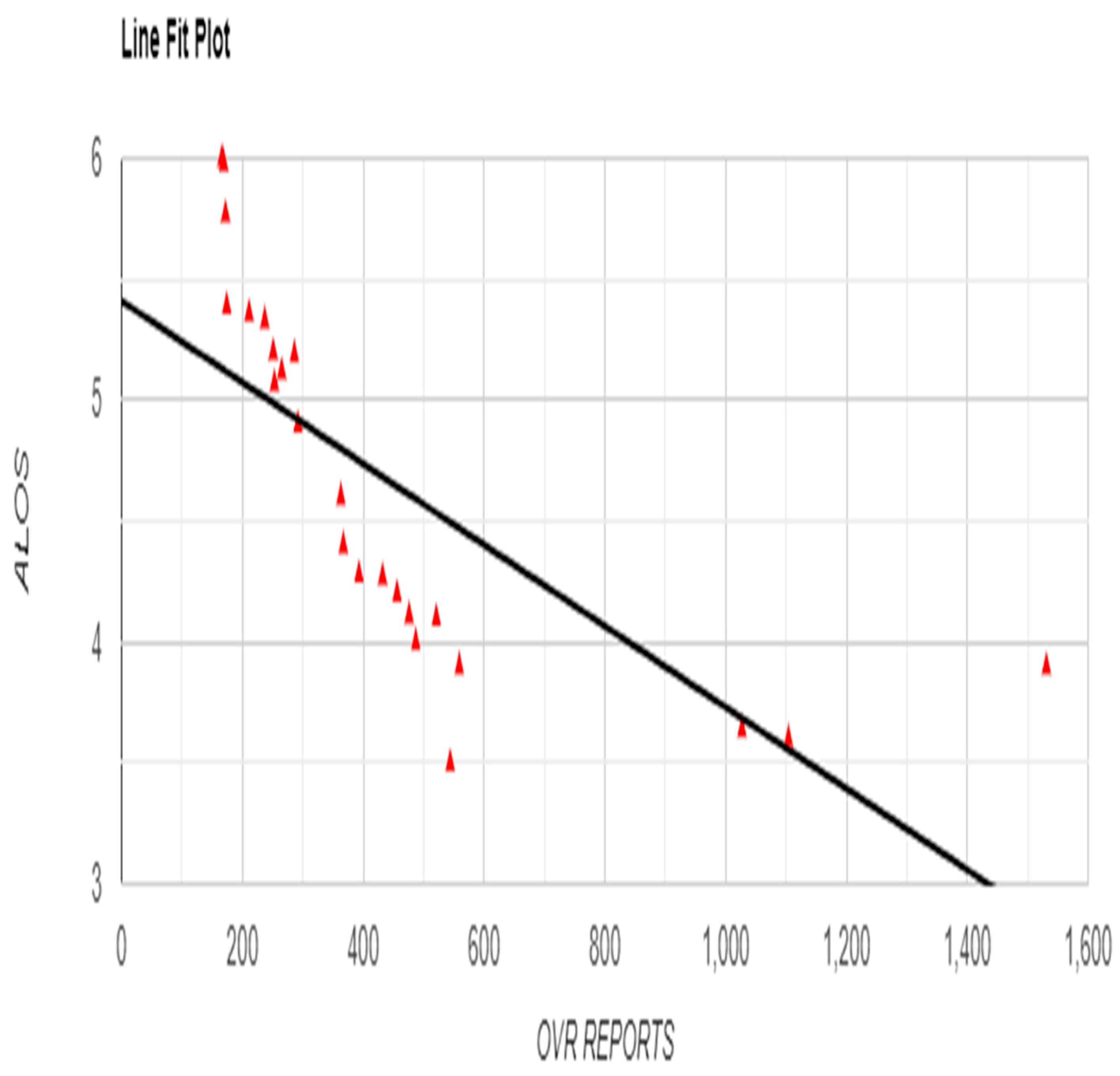
Pearson correlation analysis demonstrated significant relationships between OVR, Safety Huddles, and various patient outcomes. OVR was strongly negatively correlated with ALOS (r = -0.7293, p < 0.001), suggesting that increased OVR activity was associated with shorter hospital stays (
Figure 2).
Figure 2.
Relationship between Occurrence Variance Reporting (OVR) Frequency and Average Length of Stay (ALOS) with Line Fit Plot.
Figure 2.
Relationship between Occurrence Variance Reporting (OVR) Frequency and Average Length of Stay (ALOS) with Line Fit Plot.
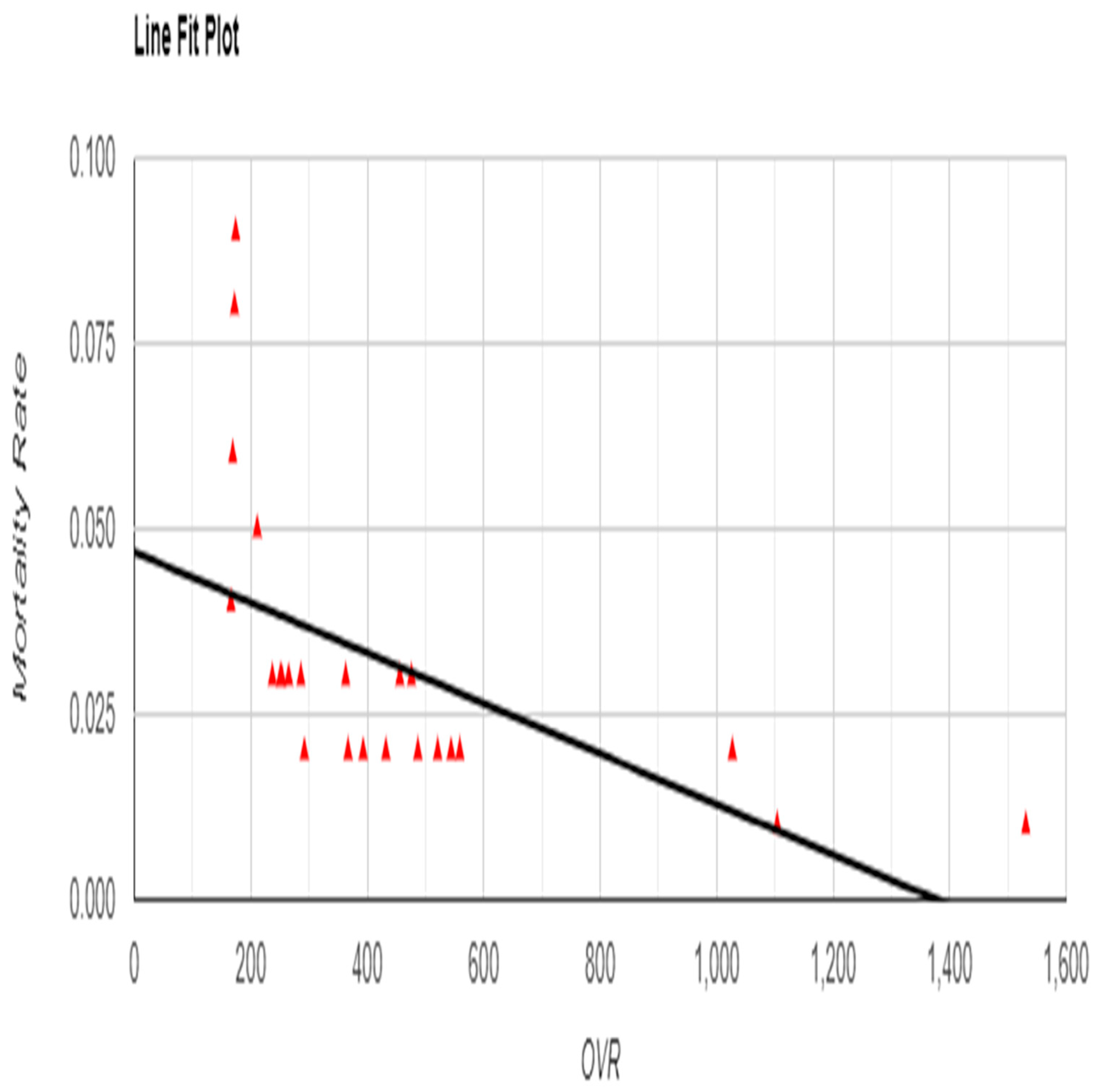
Similarly, a moderate negative correlation was found between OVR and overall mortality rate (r = -0.5684, p = 0.004), indicating that higher reporting correlated with lower mortality (
Figure 3).
Figure 3.
Relationship between Occurrence Variance Reporting (OVR) Frequency and Mortality Rate with Line Fit Plot.
Figure 3.
Relationship between Occurrence Variance Reporting (OVR) Frequency and Mortality Rate with Line Fit Plot.
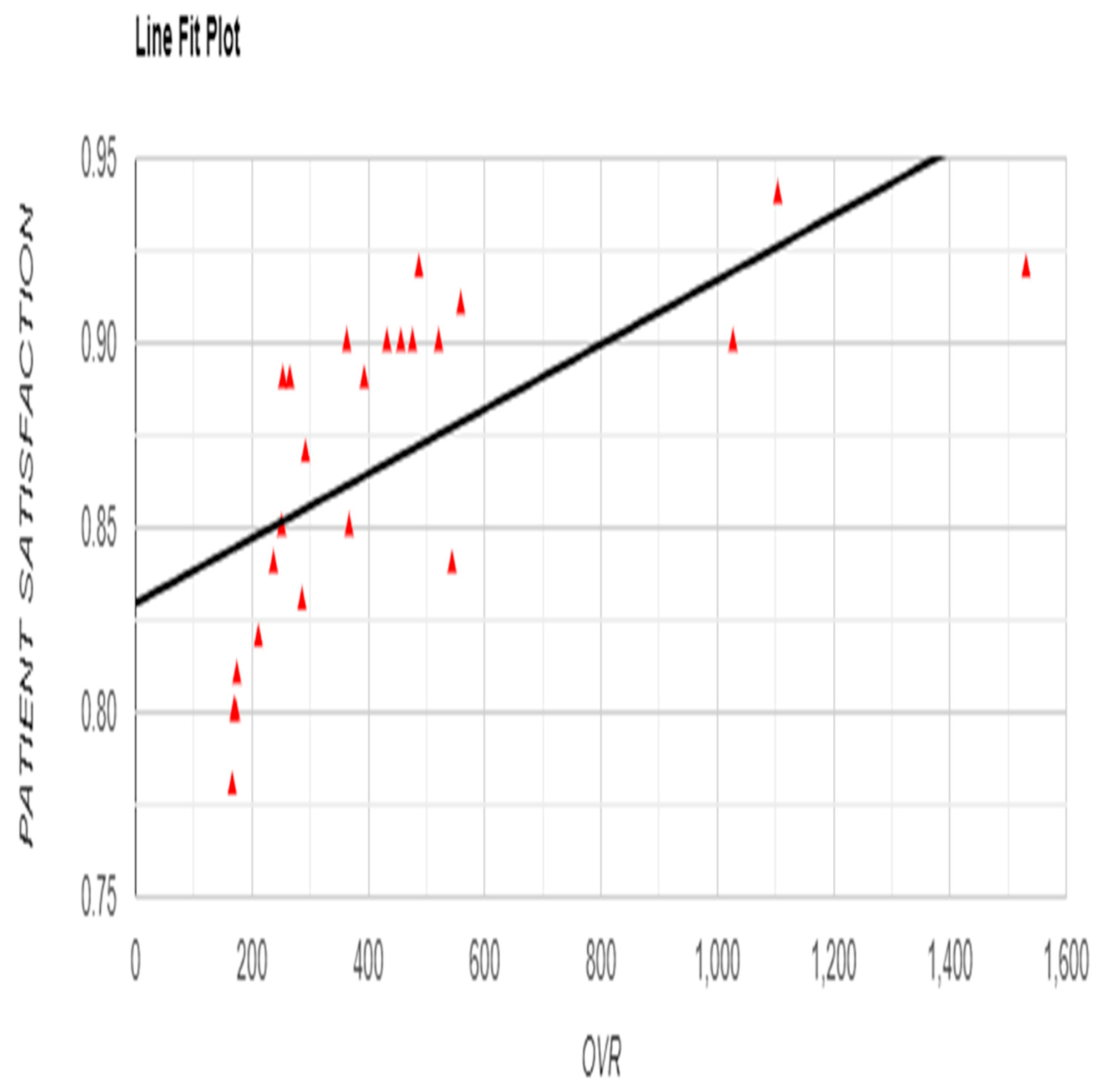
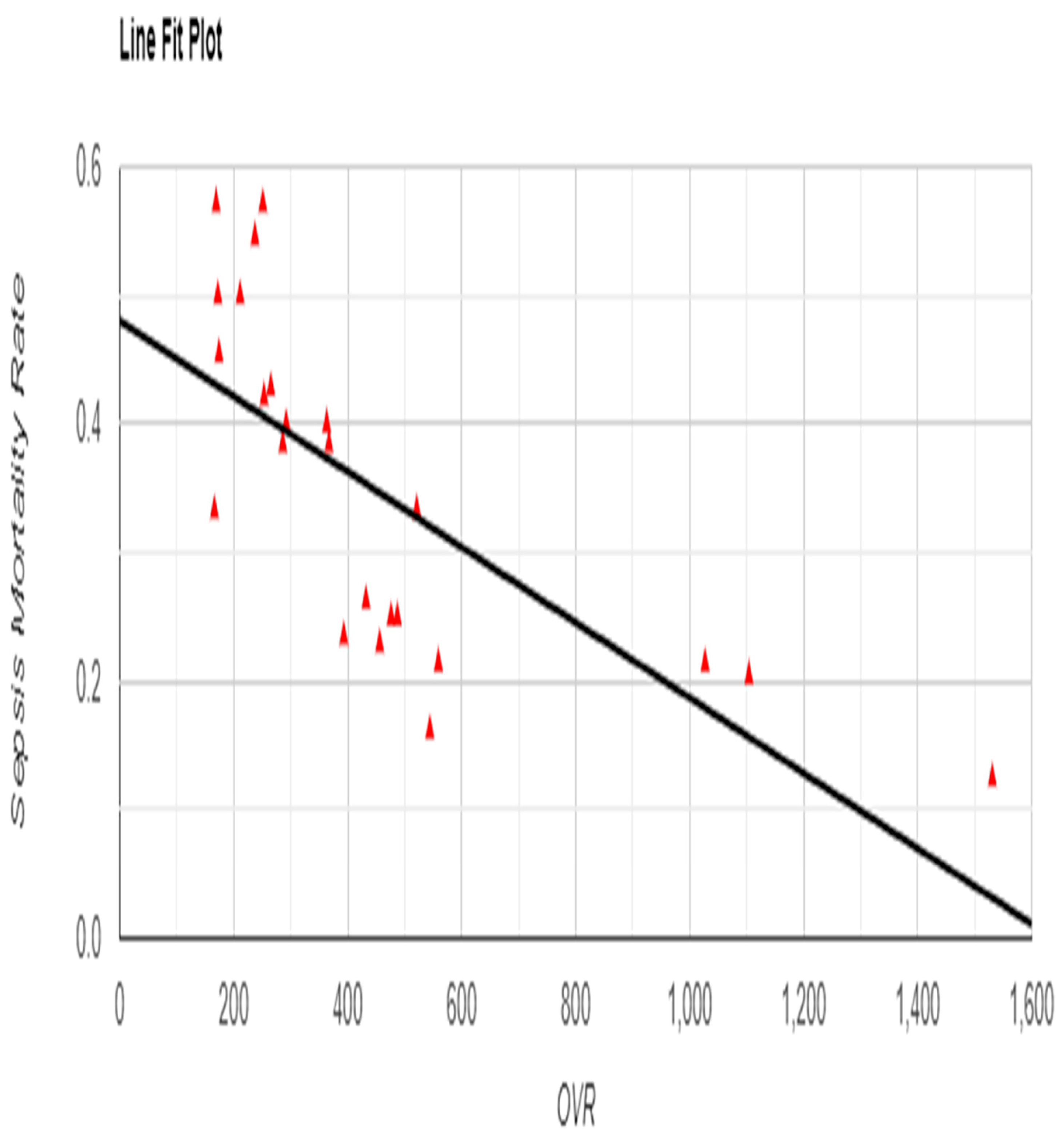
A strong negative correlation between OVR and sepsis-specific mortality rate (r = -0.7305, p = 0.001) further emphasized the association between frequent reporting and reduced sepsis-related deaths (
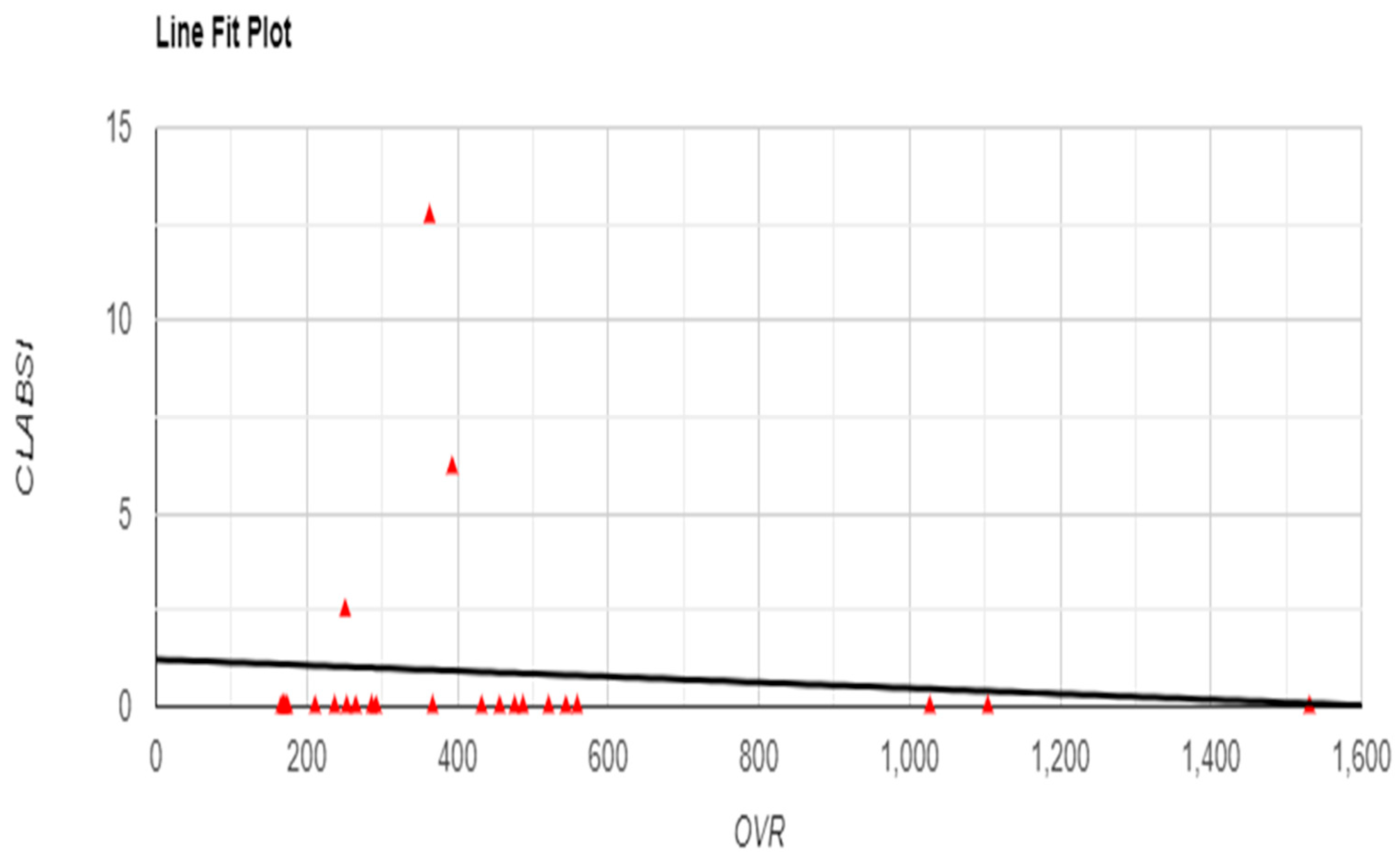
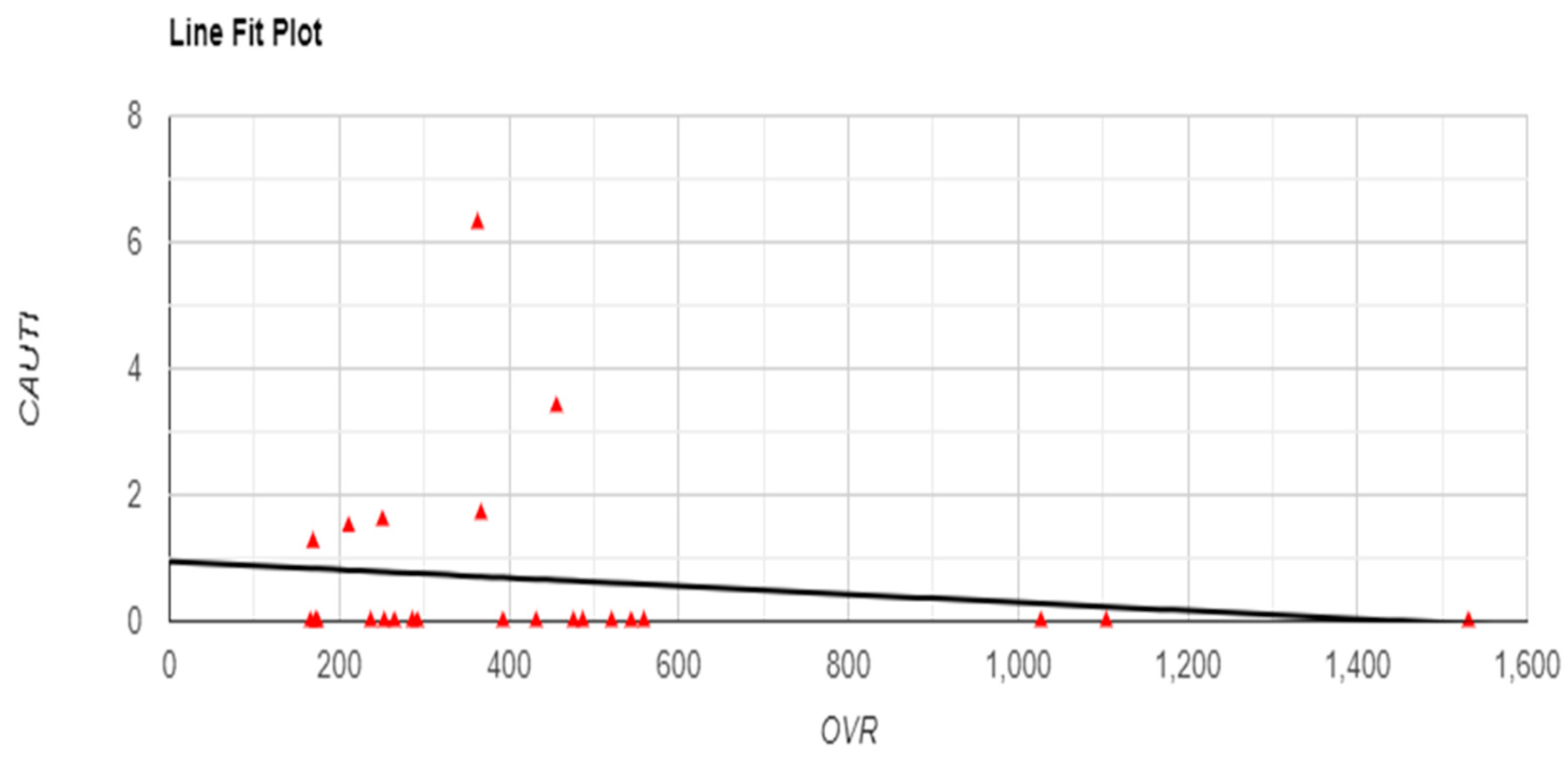
Figure 5). Although no significant correlations were found between OVR and infection rates, with non-significant relationships for CLABSI (r = -0.0869, p = 0.686) and CAUTI (r = -0.1462, p = 0.496) (
Figure 6 and
Figure 7), a significant positive correlation was observed between OVR and patient satisfaction (r = 0.6498, p < 0.001), suggesting that higher reporting levels align with enhanced patient satisfaction (
Figure 4).
Figure 4.
Relationship between Occurrence Variance Reporting (OVR) Frequency and Satisfaction Rate with Line Fit Plot.
Figure 4.
Relationship between Occurrence Variance Reporting (OVR) Frequency and Satisfaction Rate with Line Fit Plot.
Figure 5.
Relationship between Occurrence Variance Reporting (OVR) Frequency and Sepsis Mortality Rate with Line Fit Plot.
Figure 5.
Relationship between Occurrence Variance Reporting (OVR) Frequency and Sepsis Mortality Rate with Line Fit Plot.
Figure 6.
Relationship between Occurrence Variance Reporting (OVR) Frequency and CLABSI with Line Fit Plot.
Figure 6.
Relationship between Occurrence Variance Reporting (OVR) Frequency and CLABSI with Line Fit Plot.
Figure 7.
Relationship between Occurrence Variance Reporting (OVR) Frequency and CAUTI with Line Fit Plot.
Figure 7.
Relationship between Occurrence Variance Reporting (OVR) Frequency and CAUTI with Line Fit Plot.
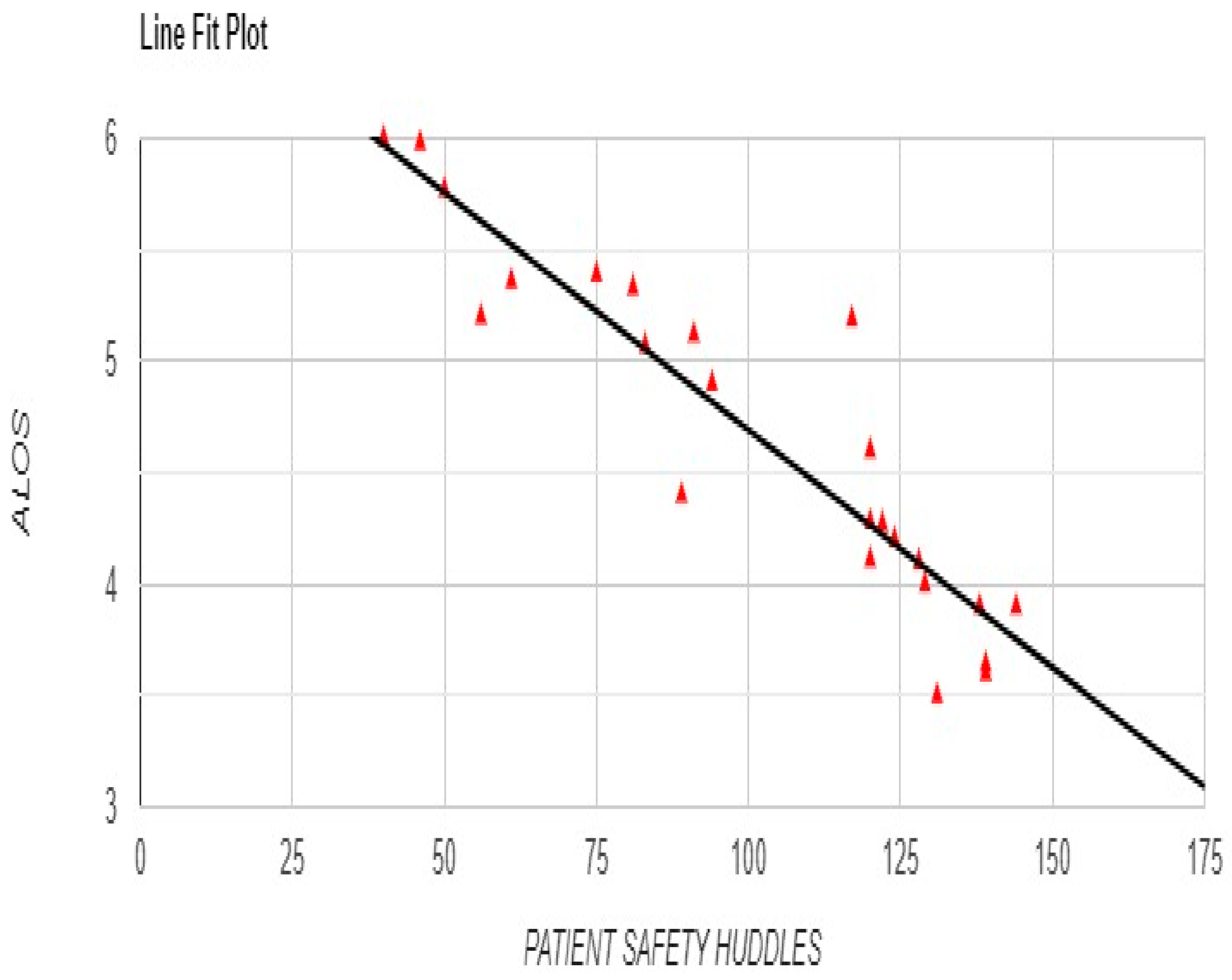
Safety Huddles also showed strong associations with improved patient outcomes. A robust negative correlation between Safety Huddles and ALOS (r = -0.9249, p < 0.001) indicated that more frequent huddles were linked to shorter hospital stays (
Figure 8).
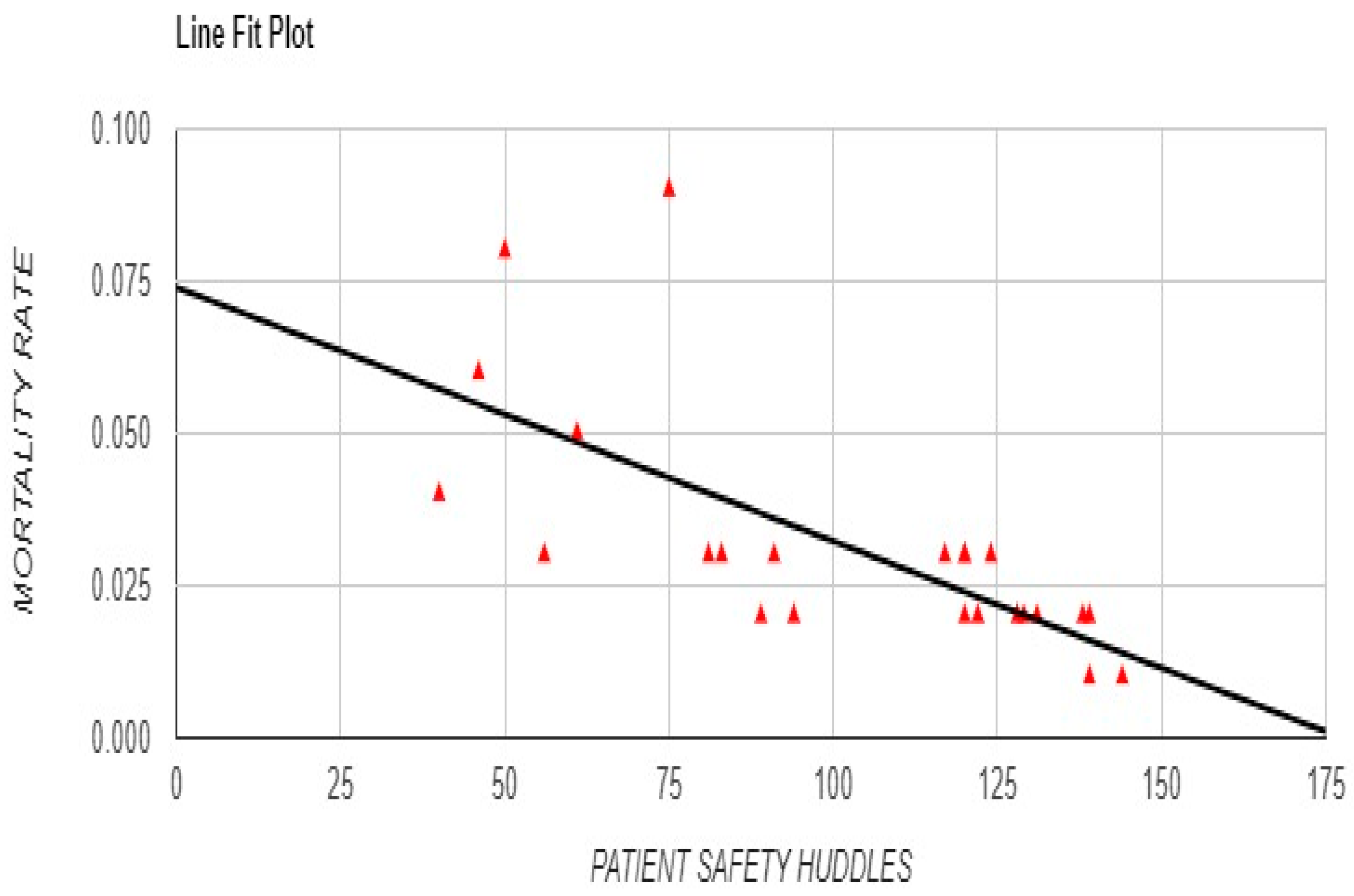
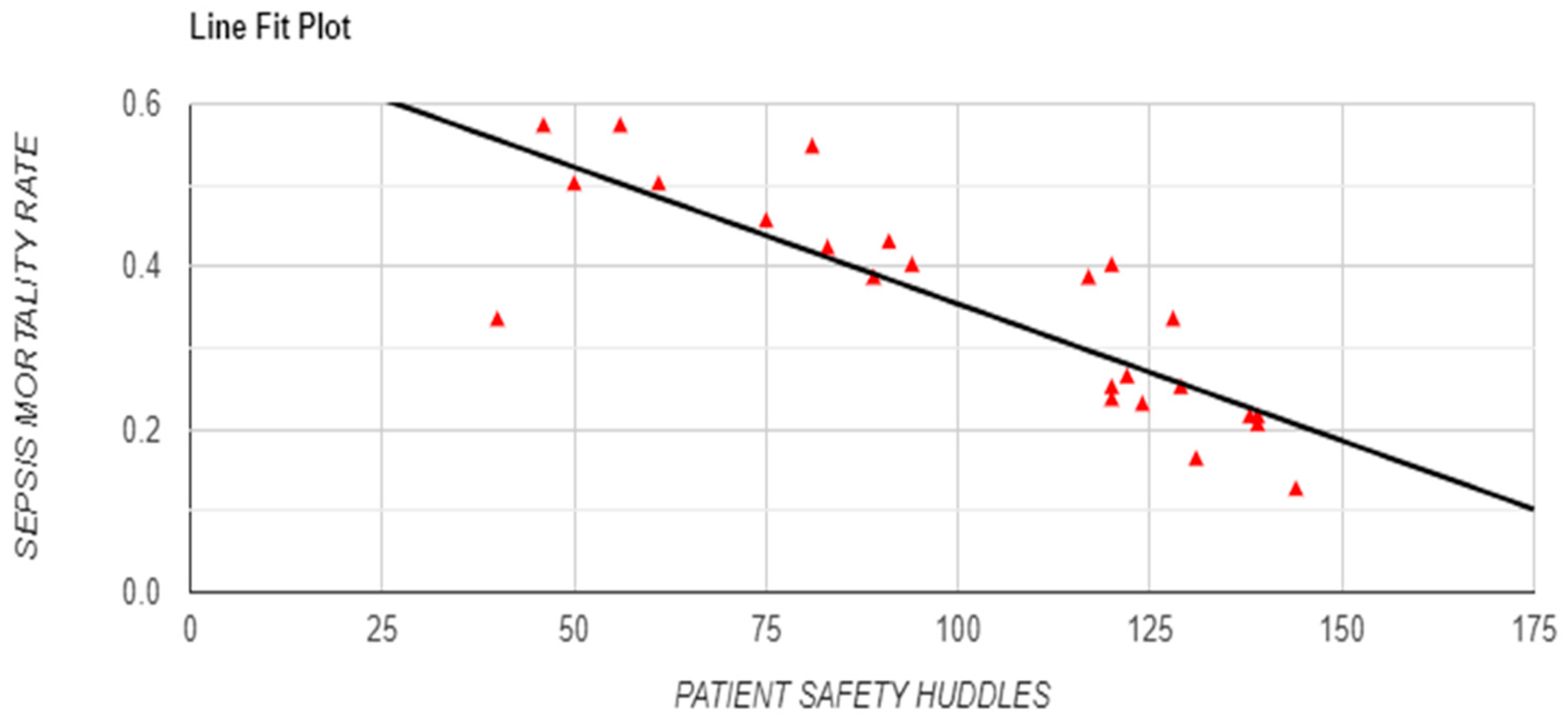
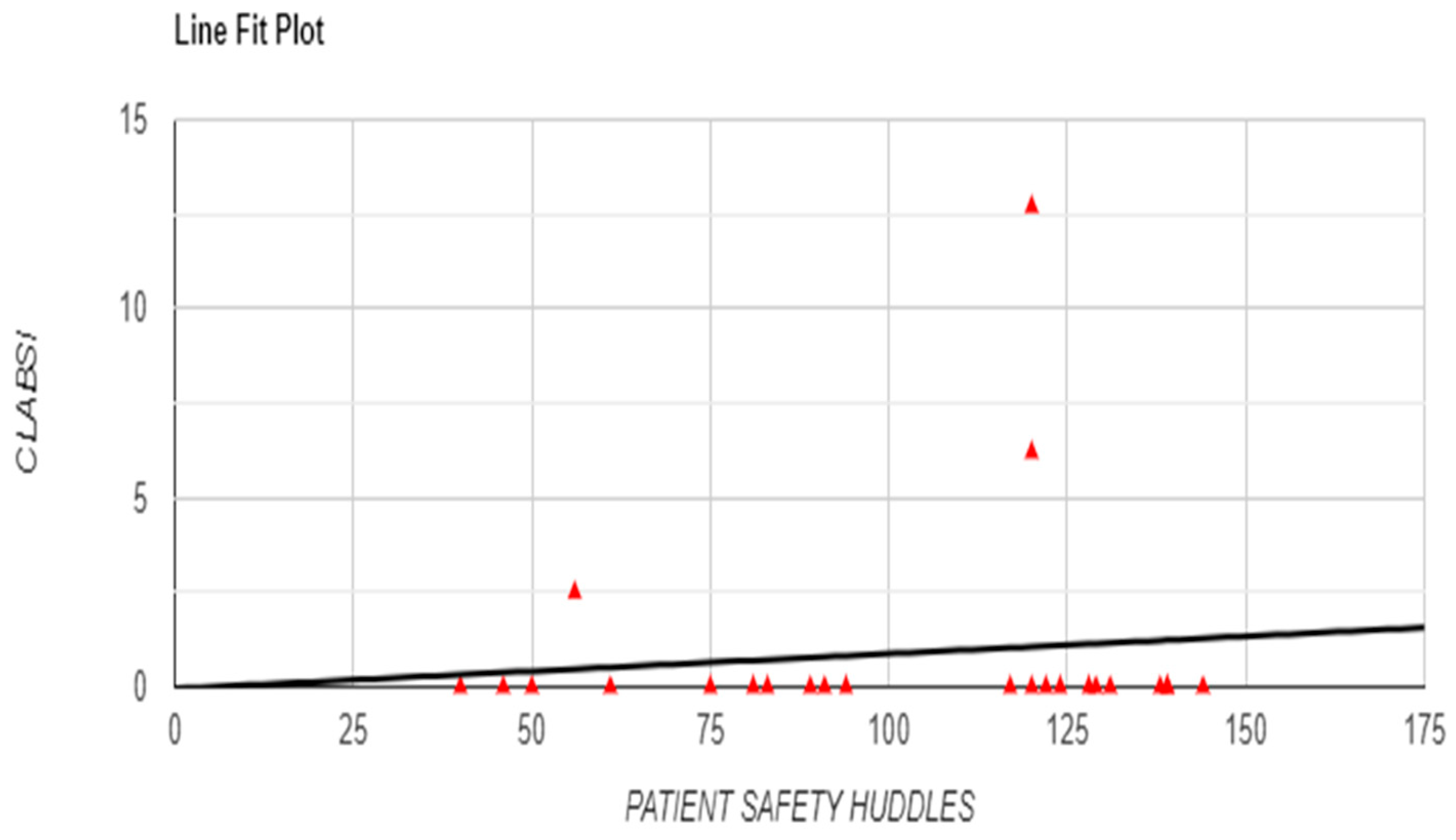
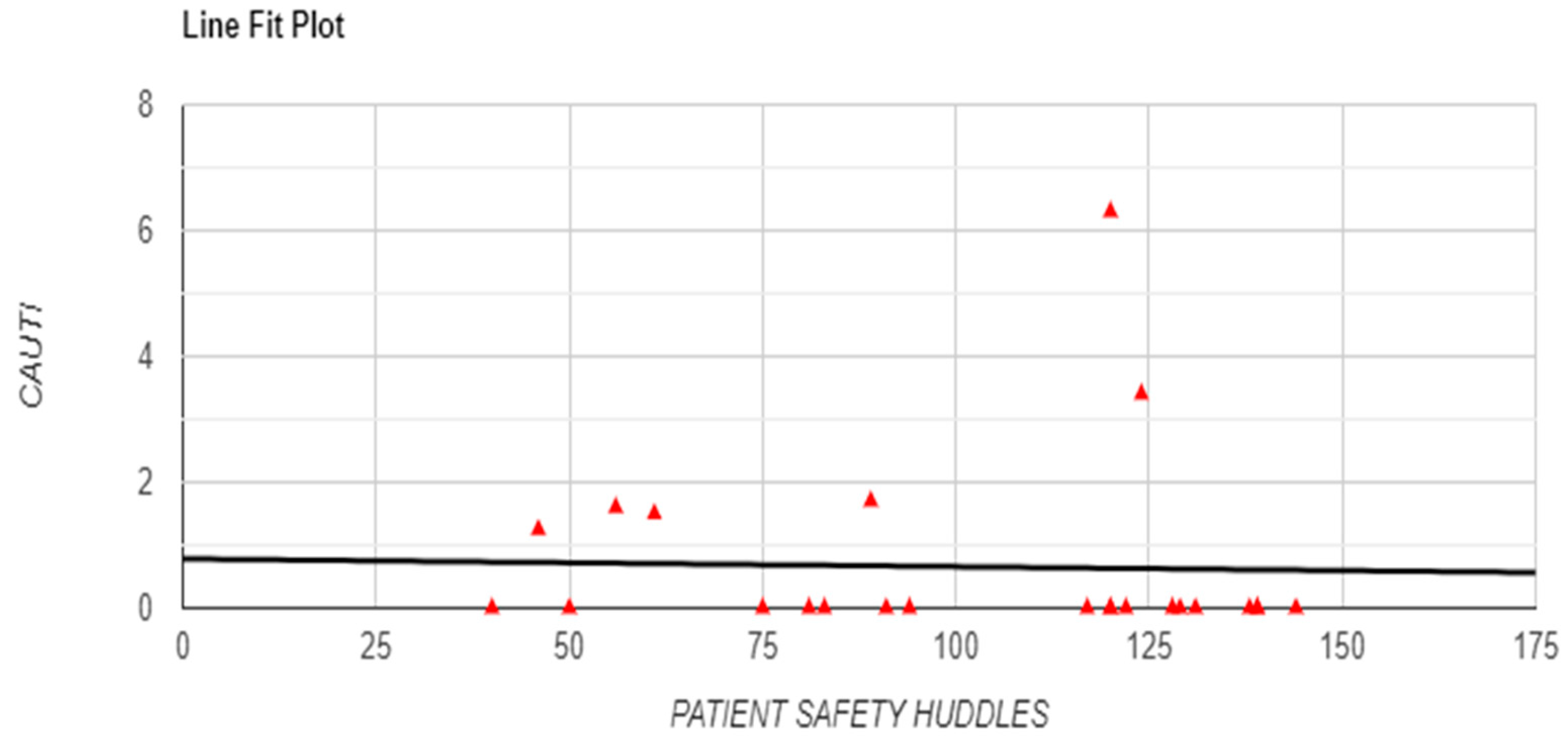
Additionally, Safety Huddles demonstrated a significant negative correlation with overall mortality rate (r = -0.6962, p < 0.001) and a similarly strong negative relationship with sepsis-specific mortality rate (r = -0.8375, p < 0.001), underscoring the potential of team-based interventions to improve survival outcomes (
Figure 9 and
Figure 11). Although no significant associations were found between Safety Huddles and infection rates, with non-significant correlations for CLABSI (r = 0.1077, p = 0.617) and CAUTI (r = -0.0281, p = 0.896) (
Figure 12 and
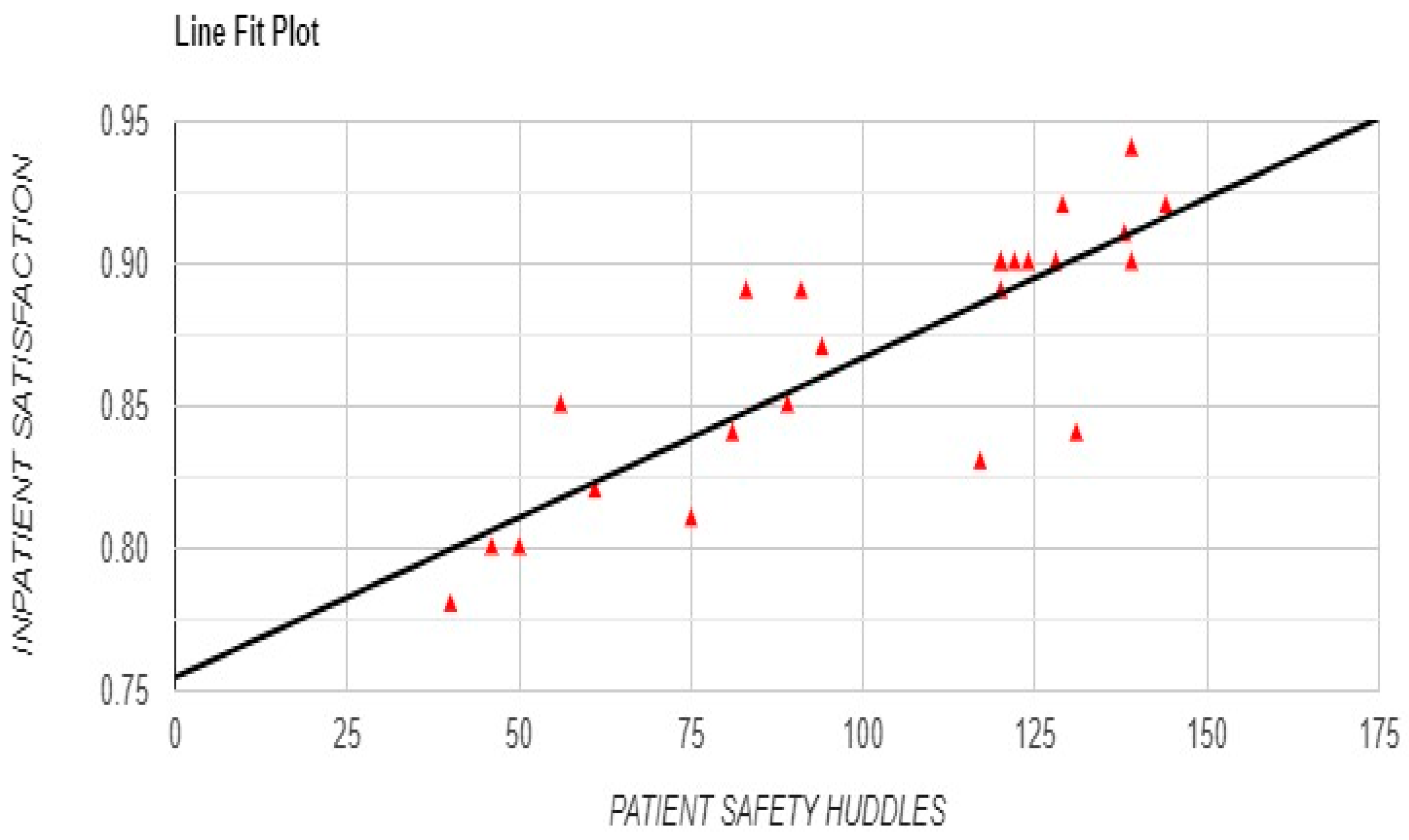
Figure 13), a strong positive correlation between Safety Huddles and patient satisfaction (r = 0.8331, p < 0.001) reinforced the impact of Safety Huddles on enhancing patient experience (
Figure 10).
Overall, these findings underscore the effectiveness of Active Occurrence Variance Reporting and Safety Huddles in driving improvements in patient outcomes, particularly in reducing ALOS, lowering mortality rates, and increasing patient satisfaction. However, the lack of significant correlations with infection rates suggests that other factors may influence these specific outcomes.
Table 1 and
Table 2 provide a detailed summary of monthly and annual data trends, while Figures 2 through 13 visually represent the significant correlations identified in the analysis.
Figure 9.
Correlation between Frequency of Patient Safety Huddles and Mortality Rate)with Line Fit Plot.
Figure 9.
Correlation between Frequency of Patient Safety Huddles and Mortality Rate)with Line Fit Plot.
Figure 10.
Correlation between Frequency of Patient Safety Huddles Frequency and Patient Satisfaction with Line Fit Plot.
Figure 10.
Correlation between Frequency of Patient Safety Huddles Frequency and Patient Satisfaction with Line Fit Plot.
Figure 11.
Correlation between Frequency of Patient Safety Huddles and Sepsis Mortality Rate with Line Fit Plot.
Figure 11.
Correlation between Frequency of Patient Safety Huddles and Sepsis Mortality Rate with Line Fit Plot.
Figure 12.
Correlation between Frequency of Patient Safety Huddles and CLABSI with Line Fit Plot.
Figure 12.
Correlation between Frequency of Patient Safety Huddles and CLABSI with Line Fit Plot.
Figure 13.
Correlation between Frequency of Patient Safety Huddles and CAUTI with Line Fit Plot.
Figure 13.
Correlation between Frequency of Patient Safety Huddles and CAUTI with Line Fit Plot.
Discussion
This study demonstrates the significant impact of Active Occurrence Variance Reporting (OVR) and Safety Huddles on key patient outcomes, specifically in reducing Average Length of Stay (ALOS) and mortality rates while enhancing patient satisfaction. These findings align with existing literature that emphasizes the importance of a proactive safety culture in healthcare, where transparent reporting and collaborative team interventions contribute to improved patient outcomes and organizational performance [
2,
8].
Similar findings were observed in a study by Bashir [
16], where healthcare professionals in a tertiary hospital identified that a well-established patient safety culture positively influences reporting practices. Higher scores in nonpunitive response to errors were associated with lower rates of adverse outcomes, such as medication errors and hospital-acquired infections. Furthermore, increased frequency of event reporting correlated with reduced incidences of pressure ulcers, falls, and surgical site infections, highlighting the direct impact of safety culture on patient outcomes. These findings reinforce the importance of cultivating a nonpunitive environment in fostering effective reporting and ultimately improving patient safety.
The strong negative correlation between OVR frequency and ALOS suggests that regular variance reporting may expedite the identification and resolution of safety issues, contributing to shorter hospital stays. This result is consistent with studies indicating that active incident reporting systems allow for timely intervention and preventive action [
4]. Similarly, the significant relationship between OVR and overall and sepsis-specific mortality rates highlights the role of systematic reporting in early detection of critical incidents, which can reduce mortality and improve survival outcomes. These findings support the idea that OVR can be a valuable tool for reducing risks and improving care quality when effectively implemented within a supportive, non-punitive culture [
7,
17].
Safety Huddles were also associated with favorable outcomes, including reductions in ALOS and mortality rates and increased patient satisfaction. The significant correlation between Safety Huddles and patient satisfaction suggests that regular, structured team meetings may foster a more responsive and patient-centered care environment. This aligns with research indicating that Safety Huddles improve team communication and engagement, which is crucial for addressing patient needs promptly [
9]. Furthermore, the observed decrease in sepsis-specific mortality with increased Safety Huddles underscores the potential of these huddles as a proactive measure in high-risk areas, facilitating early recognition of sepsis and enabling timely interventions.
Our results echo findings by Binkheder et al. [
18], who showed that a positive patient safety culture—especially in domains like teamwork within units, communication openness, and a nonpunitive approach to errors—was associated with lower occurrences of sentinel events in Saudi hospitals. Binkheder et al. emphasized the importance of a blame-free culture, similar to our study’s approach with OVR and Safety Huddles, as a means of encouraging open incident reporting and reducing adverse events. Their findings, together with ours, suggest that fostering a supportive and blame-free environment is integral to enhancing patient safety by enabling healthcare teams to identify risks early and implement effective interventions.
Moreover, Cooper et al. [
19] highlight that a culture of blame within healthcare settings often impedes the successful reporting of incidents, as fear of retribution discourages individuals from sharing potentially valuable safety information. In their analysis of incident reports, blame was commonly attributed to specific individuals, undermining the potential for system-based improvements. This underscores the importance of fostering a blame-free environment, as achieved through OVR and Safety Huddles, which encourages staff to report errors openly and focus on learning rather than assigning fault. Establishing such a supportive culture is essential for translating incident reporting into meaningful safety improvements and system-based solutions.
The observations of Forster et al. (2012) underline a critical gap in patient safety efforts: the absence of a systematic approach to measuring patient safety, which they argue has contributed to limited progress in reducing preventable harm. They suggest that without structured patient safety measurement systems, healthcare systems struggle to gauge or advance their safety efforts effectively. This study’s reliance on OVR and Safety Huddles as part of a consistent reporting and review framework addresses this gap by actively tracking and assessing safety events. By systematically tracking incidents and outcomes, OVR and Safety Huddles not only foster a blame-free culture but also serve as tools for ongoing quality measurement and improvement.
Interestingly, neither OVR nor Safety Huddles showed significant correlations with hospital-acquired infection rates, specifically CLABSI and CAUTI. This finding suggests that while OVR and Safety Huddles positively impact various patient outcomes, they may not directly influence infection rates. It is possible that infection control is more directly related to strict adherence to specific protocols and environmental hygiene standards, which are crucial factors in preventing such infections. Future research could explore additional variables that impact infection rates to determine how OVR and Safety Huddles might be integrated with other infection control measures for comprehensive patient safety strategies.
Limitations
This study has several limitations. As a retrospective analysis based on existing data, there may be inconsistencies or reporting bias. Additionally, focusing on a single healthcare institution limits generalizability to other settings. The correlational design does not establish causation, warranting prospective studies or randomized controlled trials to confirm these findings. Uncontrolled confounding factors, such as concurrent quality improvement efforts or staffing changes, could have influenced outcomes. Future research with a controlled design would help isolate the effects of OVR and Safety Huddles on patient outcomes.
Implications for Practice
Despite these limitations, the study provides important insights for healthcare administrators and practitioners. Implementing OVR and Safety Huddles within a supportive, non-punitive framework promotes a culture of transparency and continuous improvement. To maximize their effectiveness, healthcare organizations should prioritize accessible reporting systems, regular staff training, and a reporting-friendly environment. By embedding these practices into institutional structures, hospitals can enhance patient outcomes, satisfaction, and overall safety culture.
Conclusions
This study highlights the significant impact of Active Occurrence Variance Reporting (OVR) and Safety Huddles in improving key patient outcomes within a healthcare setting. The findings reveal that increased OVR and frequent Safety Huddles are associated with reduced average length of stay, lower overall and sepsis-specific mortality rates, and enhanced patient satisfaction, underscoring the importance of structured variance reporting and team-based safety interventions in fostering a culture of transparency and accountability. Although no significant correlations with infection rates (CLABSI and CAUTI) were observed, these interventions play a critical role in enhancing patient-centered care by promoting prompt identification and management of potential risks.
The insights from this research underscore the value of OVR and Safety Huddles in advancing patient safety and healthcare quality. To fully harness their benefits, healthcare institutions should establish a supportive framework that encourages open communication and non-punitive reporting. Further studies in diverse healthcare settings are warranted to assess the generalizability of these findings and to explore their impact on additional safety outcomes, informing strategies that can drive continuous improvement in patient care and hospital performance.
Institutional Review Board Statement
This research was approved by the King Saud Medical City Institutional Review Board (IRB) Committee (Reference Number: H1RE-09-Dec24-01).
Consent to Participate
NA.
Consent for Publication
NA.
Conflicts of Interest
The authors declare no conflict of interest.
Data Availability
The data that support the findings of this study are available from the corresponding author upon reasonable request.
References
- Garay S, Haeger M, Kühnlein L, Sulmann D, Suhr R. Interventions to enhance safety culture for nursing professionals in long-term care: a systematic review. International Journal of Nursing Studies Advances [Internet]. 2023 Feb;5:100119. Available from: https://pubmed.ncbi.nlm.nih.gov/38746586/. [CrossRef]
- Albarrak AI, Almansour AS, Alzahrani AA, Almalki AH, Alshehri AA, Mohammed R. Assessment of patient safety challenges and electronic occurrence variance reporting (e-OVR) barriers facing physicians and nurses in the emergency department: a cross sectional study. BMC Emergency Medicine [Internet]. 2020 Dec;20(1). Available from: https://bmcemergmed.biomedcentral.com/articles/10.1186/s12873-020-00391-2. [CrossRef]
- El-Sayed Aly RI, Ahmed Mohamed ELBahlawan G, Aly MR, Mohamed Elsayed BK. Enhancing the Occurrence Variance Reporting System Implementation at one of the Hospitals of the Egyptian Universal Health Insurance. SAGE Open Nursing [Internet]. 2022 Jan;8:237796082211421. Available from: https://journals.sagepub.com/doi/10.1177/23779608221142157. [CrossRef]
- Hawazen Rawas, Abou Hashish EA. Predictors and outcomes of patient safety culture at King Abdulaziz Medical City, Jeddah, Saudi Arabia. A nursing perspective. BMC nursing [Internet]. 2023 Jul 3;22(1). Available from: https://bmcnurs.biomedcentral.com/articles/10.1186/s12912-023-01391-w. [CrossRef]
- Wolf ZR, Hughes RG. Error Reporting and Disclosure [Internet]. National Library of Medicine. Agency for Healthcare Research and Quality (US); 2019. Available from: https://www.ncbi.nlm.nih.gov/books/NBK2652/.
- Al-Abri R, Al-Balushi A. Patient Satisfaction Survey as a Tool Towards Quality Improvement. Oman Medical Journal [Internet]. 2014;29(1):3–7. Available from: https://www.ncbi.nlm.nih.gov/pmc/articles/PMC3910415/. [CrossRef]
- Singh G, Patel RH, Boster J. Root cause analysis and medical error prevention [Internet]. PubMed. Treasure Island (FL): StatPearls Publishing; 2024. Available from: https://www.ncbi.nlm.nih.gov/books/NBK570638/.
- Boysen PG. Just culture: A foundation for balanced accountability and patient safety. The Ochsner journal [Internet]. 2013;13(3):400–6. Available from: https://www.ncbi.nlm.nih.gov/pmc/articles/PMC3776518/.
- Buljac-Samardzic M, Doekhie KD, Wijngaarden JDH. Interventions to improve team effectiveness within health care: A systematic review of the past decade. Human Resources for Health [Internet]. 2020;18(2):1–42. Available from: https://human-resources-health.biomedcentral.com/articles/10.1186/s12960-019-0411-3. [CrossRef]
- Health Education England. Improving safety through education and training [Internet]. Health Education England; 2016. Available from: https://www.hee.nhs.uk/sites/default/files/documents/Improving%20safety%20through%20education%20and%20training.pdf.
- Alsulami A, A’aqoulah A, Almutairi N. Patient safety culture awareness among healthcare providers in a tertiary hospital in Riyadh, Saudi Arabia. Frontiers in Public Health [Internet]. 2022 Jul 18;10(1). Available from: https://www.frontiersin.org/journals/public-health/articles/10.3389/fpubh.2022.953393/full. [CrossRef]
- Kohanová D, Bartoníčková D. Barriers to reporting adverse events from the perspective of ICU nurses: A mixed-method study. Enfermería Intensiva (English ed) [Internet]. 2024 Oct;35(4):287–98. Available from: https://www.sciencedirect.com/science/article/abs/pii/S2529984024000430?via%3Dihub.
- Pham JC, Girard T, Pronovost PJ. What to do with healthcare Incident Reporting Systems. Journal of Public Health Research [Internet]. 2013 Dec 1;2(3):27. Available from: https://www.ncbi.nlm.nih.gov/pmc/articles/PMC4147750/. [CrossRef]
- Ayed Awadh AlReshidi. Improving Occurrence Variance Reporting System through Implementing An Educational Program For Staff At King Saud Hospital,Unaizah, Al –Qassim, KSA. Journal of Natural Sciences Research [Internet]. 2025 [cited 2025 Jan 22];4(22):49–60. Available from: https://www.iiste.org/Journals/index.php/JNSR/article/view/17626.
- Elsehrawy MG, Samia Gaballah, Ateya Megahed, Mohamed A. Healthcare Providers’ Awareness of Occurrence Variance Reports and Their Magnitude at Accredited Versus Non-Accredited Hospitals: A Cross-Sectional Descriptive Study [Internet]. 2023. p. 2023–41. Available from: https://www.researchgate.net/publication/374090945.
- Bashir H, Barkatullah M, Raza A, Mushtaq M, Khanzada Sheraz Khan, Saber A, et al. Practices Used to Improve Patient Safety Culture Among Healthcare Professionals in a Tertiary Care Hospital. Global journal on quality and safety in healthcare [Internet]. 2024 Feb 1 [cited 2024 Mar 1];7(1):9–14. Available from: https://meridian.allenpress.com/innovationsjournals-JQSH/article/7/1/9/498915/Practices-Used-to-Improve-Patient-Safety-Culture. [CrossRef]
- Hughes R. Tools and strategies for quality improvement and patient safety [Internet]. National Library of Medicine. Agency for Healthcare Research and Quality (US); 2020. Available from: https://www.ncbi.nlm.nih.gov/books/NBK2682/.
- Binkheder S, Alaska YA, Albaharnah A, AlSultan RK, Alqahtani NM, Amr AA, et al. The relationships between patient safety culture and sentinel events among hospitals in Saudi Arabia: a national descriptive study. BMC Health Services Research [Internet]. 2023 Mar 18;23(1). Available from: https://bmchealthservres.biomedcentral.com/articles/10.1186/s12913-023-09205-0. [CrossRef]
- Cooper J, Edwards A, Williams H, Sheikh A, Parry G, Hibbert P, et al. Nature of Blame in Patient Safety Incident Reports: Mixed Methods Analysis of a National Database. The Annals of Family Medicine [Internet]. 2017 Sep;15(5):455–61. Available from: https://www.ncbi.nlm.nih.gov/pmc/articles/PMC5593729/pdf/0150455.pdf. [CrossRef]
- Forster A, Dervin G, Martin Jr. C, Papp S. Improving patient safety through the systematic evaluation of patient outcomes. Canadian Journal of Surgery [Internet]. 2012 Dec 1;55(6):418–25. Available from: https://www.canjsurg.ca/content/55/6/418.
|
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2025 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (http://creativecommons.org/licenses/by/4.0/).