1. Introduction
Cotyledonoid dissecting leiomyoma (CDL), also known as Sternberg tumour, is a rare variant of leiomyoma that was first reported by Roth et al. [
1]. It is typically found in women of reproductive or menopausal age between 23-65 years old, with common symptoms including lower abdominal pain and abnormal uterine bleeding [
2]. The pathogenesis of CDL is not well understood, but it is believed to arise from a stem cell population in the myometrium. Although it can be locally invasive and extend to neighbouring organs such as the bladder, rectum and fallopian tubes, it typically does not invade them and is considered a benign tumour with good prognosis [
3]. However, CDL can easily be mistaken for a malignant neoplasm on clinical and radiological examination, posing a diagnostic challenge for clinicians [
4]. Therefore, it is essential to recognize and differentiate this variant from other malignancies to avoid misdiagnosis and overtreatment, especially in women who wish to preserve their fertility. Herein, we report a rare case of CDL misdiagnosed pre-operatively as an ovarian tumour and explore the diagnostic challenges associated with CDL as well as the approach for its laparoscopic removal.
2. Case Presentation
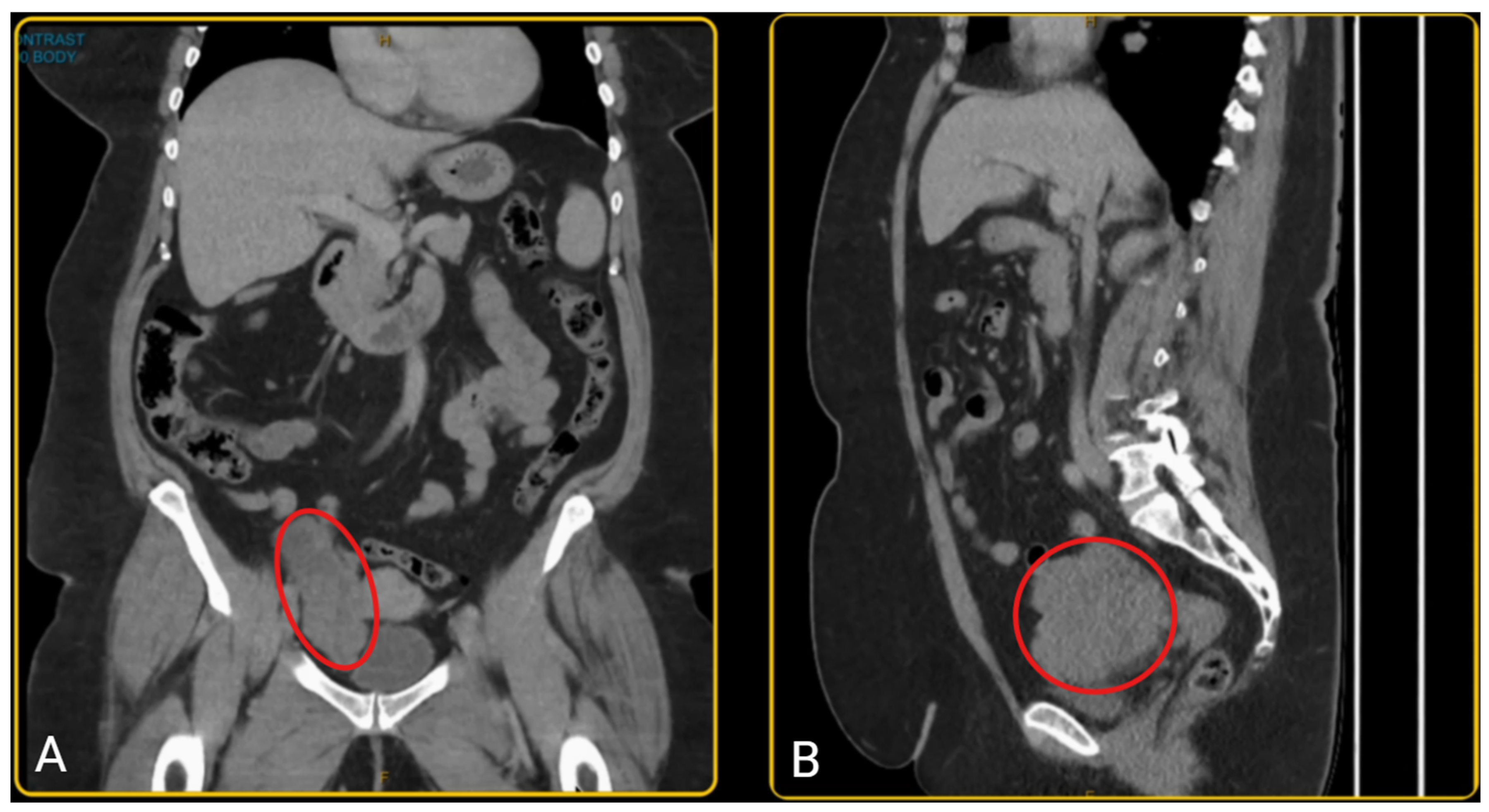
A woman in her late-50s presented with a history of post-menopausal bleeding and pelvic pressure. Pelvic ultrasound and CT scan showed a right adnexal mass with a solid component measuring 103 x 98 x 50 mm (
Figure 1). However, her tumour markers were normal (CA 125 = 13; Ca 19-9 = 22; CEA = 2.5, AFP = 7; RMI = 111). She was pre-emptively diagnosed with an ovarian tumour, however since the diagnosis was not established, pre-operative biopsy was not performed due to risk of tumour seeding and technical challenges. Hence, the patient was planned for a diagnostic laparoscopy and laparoscopic oophorectomy.
Endometrial cancer was ruled out with a hysteroscopy dilation & curettage and polypectomy immediately prior to the laparoscopy and oophorectomy, revealing an atrophic endometrium and a benign endometrial polyp.
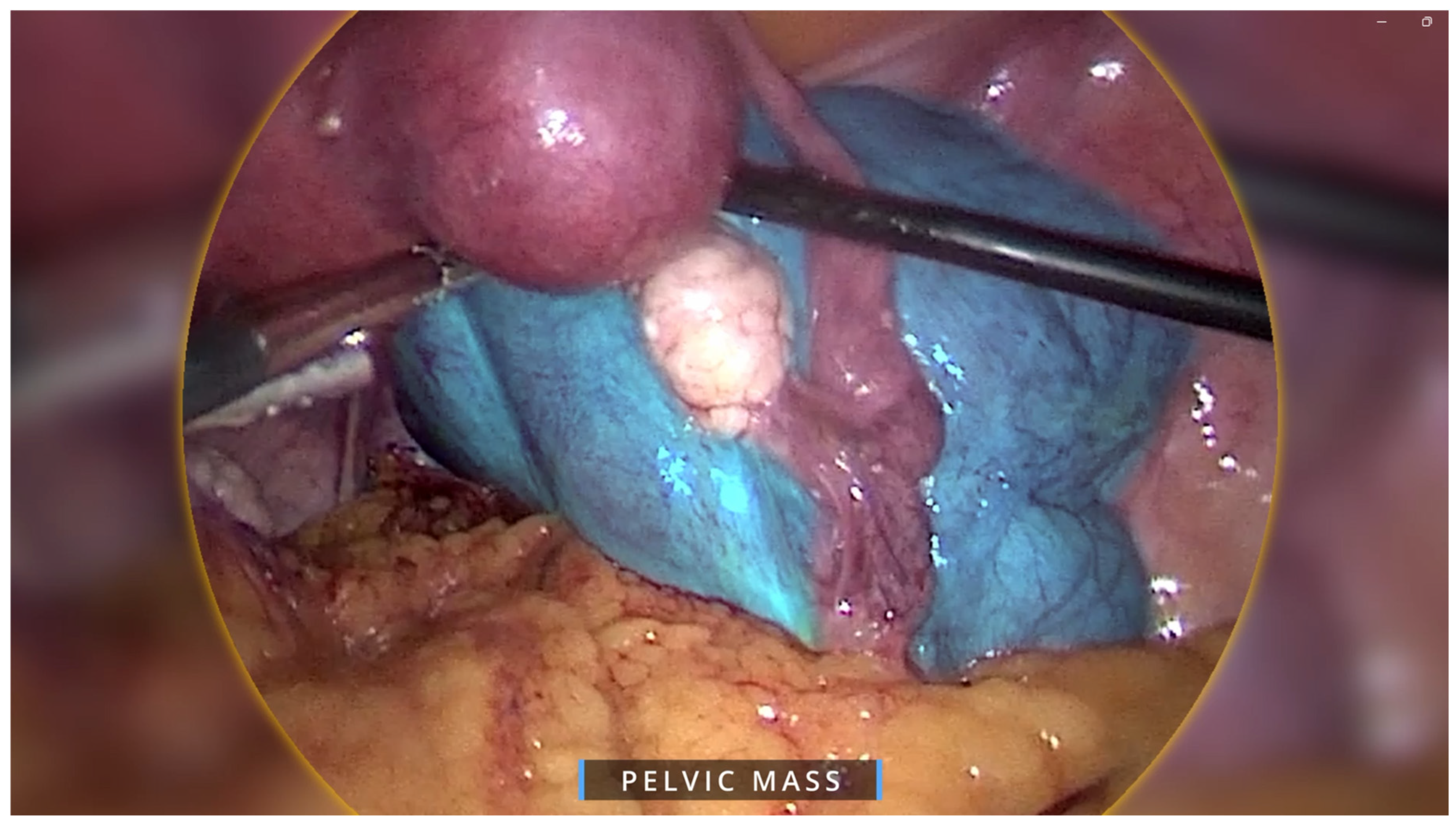
Regarding the ovarian tumour, the patient underwent a diagnostic laparoscopy using a 4-port laparoscopic technique with an ipsilateral configuration, during which we were met with an intra-operative surprise. A retroperitoneal pelvic mass of unknown origin was found and further explored. The mass measured around 8 x 8 cm and was found to be attached to the uterus laterally, anteriorly extending up to the paravesical space, laterally to the external iliac vessels, and posteriorly in the pararectal space (
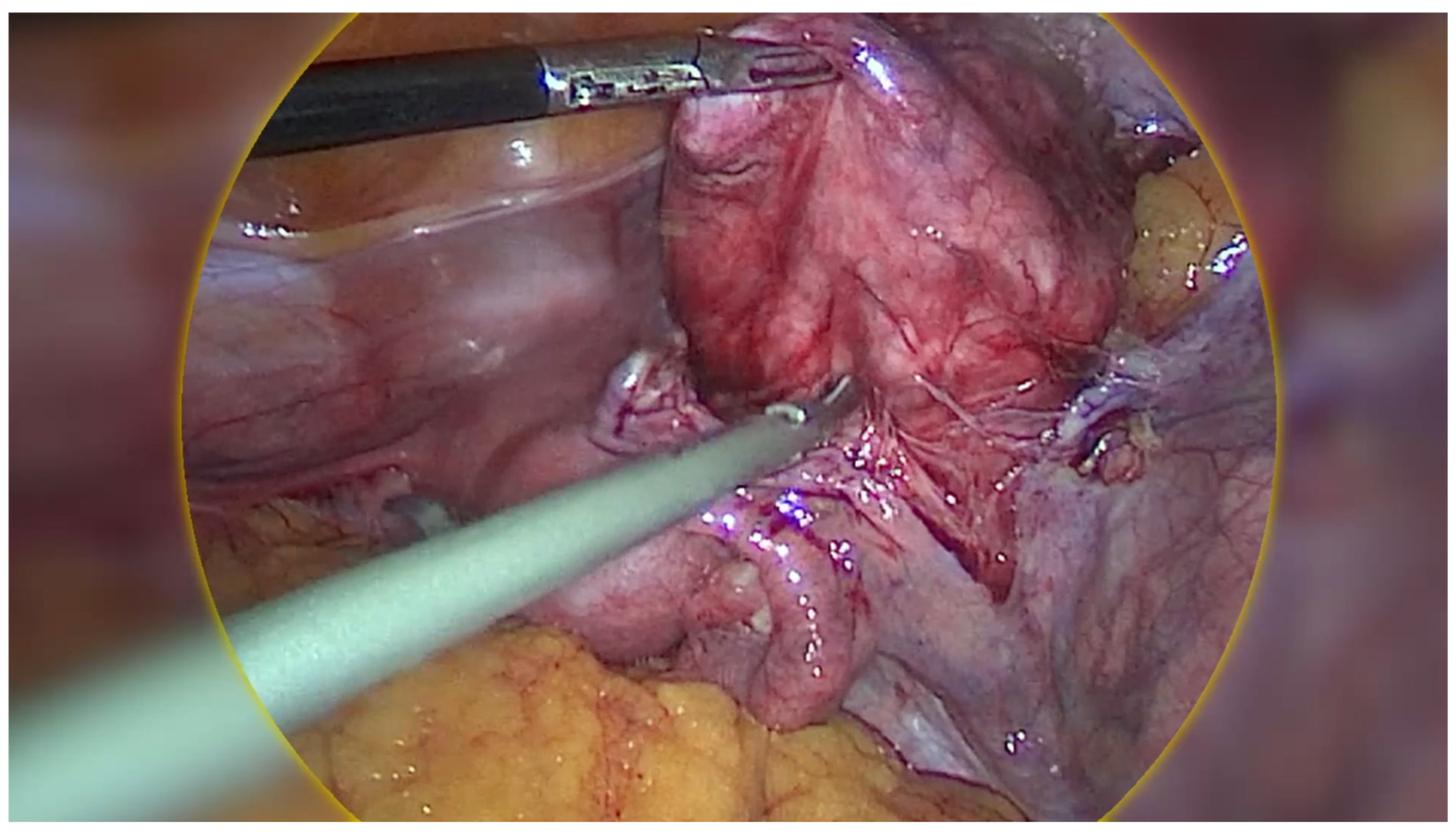
Figure 2). Initially, the mass was thought to be a fibroid, however on palpation the consistency of the mass was different to that of a usual fibroid and was soft, almost jelly-like. The gross features also resembled cotyledons of the placenta (
Figure 3). Due to the unique pattern of growth and inconclusive appearance of the retroperitoneal mass, we consulted with a gynaecology oncologist intra-operatively via telehealth and proceeded with their recommendation to perform an excisional biopsy.
The mass’ jelly-like consistency and attachment to the iliac vessels laterally required us to develop a plane between the lymph nodes of the pelvic side wall and the tumour in order to prevent injury to the iliac vessels. This demonstrates that the tumour is unique in the sense that it almost dissects its way into surrounding structures however does not invade them. Once the mass was carefully dissected and fully mobilised, it was placed in a laparoscopic bag and removed from the abdominal cavity. Surprisingly the bag was able to be extracted through the 15 mm port site via the umbilicus without any extension due to the jelly-like nature of the mass.
The excised mass was sent for testing, which revealed a CDL, a rare variant of leiomyoma. Macroscopically, it appeared to have a smooth peritonealised surface with a solid, lobulated, white, fibrotic cut surface, with the lobules ranging from 2-22mm in diameter. Areas of haemorrhage and increased vascularity were also noted. Histopathological examination of the mass demonstrated moderate vascularity and prominent oedematous areas separating the lobules of smooth muscle. There was no atypia of the smooth muscle cells, mitotic activity or evidence of necrosis. No malignant cells were seen in the peritoneal washings sent for cytology, hence supporting its benign status.
The patient recovered well and was discharged the following day without complications. During her follow up in a year the patient was well with no evidence of clinical symptoms or disease progression.
3. Discussion
CDL is an extremely rare variant of leiomyoma with less than 70 cases reported in English literature. Although it is benign and carries a good prognosis, its rarity and non-specific, alarming features often lead to its misdiagnosis for more sinister differentials including ovarian tumours, leiomyosarcomas, endometrial stromal sarcoma [
5]. This poses a diagnostic challenge for clinicians, especially in the pre-operative setting, and can lead to overtreatment. Therefore, recognition and awareness of CDL is essential to prevent such misdiagnosis and overtreatment.
Pre-operative diagnostic techniques for CDL often yield an inconclusive or incorrect diagnosis. The diagnostic work-up for CDL consists of clinical evaluation and screening for signs and symptoms similar to those of typical leiomyomas including lower abdominal pain/pressure, abnormal uterine bleeding, and a palpable pelvic mass. Radiological evaluation can include pelvic ultrasound and CT as well as MRI where CDL often presents as heterogenous mass, raising concerns of malignancies such as leiomyosarcomas. However, to date these imaging modalities cannot clearly differentiate malignant differentials from CDL [
6]. An incisional core biopsy can be valuable for pre-operative diagnosis but is limited by sampling errors and insufficient information, where the biopsy may not capture the representative tissue, especially in heterogeneous tumours. Additionally, the risk of tumour seeding discourages the use of incisional core biopsies in situations where the diagnosis has not been confirmed [
7]. In our case, since the pre-operative diagnosis was not established, an incisional core biopsy was not applicable.
CDL is often found incidentally in the intra-operative setting based on its unusual macroscopic appearance and pattern of growth. CDL typically appears as a multinodular, grape-like mass that is red-brown in colour, and has a placenta-like appearance resembling cotyledons. Despite being able to dissect its way adjacent organs such as the bladder, rectum, and fallopian tubes, CDL does not invade these surroundings structures [
4,
8,
9]. Thus, despite its atypical gross appearance and pattern of growth which can raise suspicions of sarcomas, CDL is considered a benign tumour that does not metastasise and carries a good prognosis. This demonstrates how careful intra-operative exploration and recognition of CDL based on its unique features can prompt consideration of alternative diagnoses rather than malignancies, hence guiding intraoperative decision-making to avoid overtreatment.
When in doubt, intraoperative frozen sections may be considered as they can provide immediate information to guide surgical decisions on whether a more conservative approach is sufficient or if more extensive surgery is required but may have limitations in accuracy due to the presence of artefacts and can prolong surgery [
10]. In this case, the facility where the surgery was performed did not have intraoperative frozen section capabilities. Instead, we consulted with a gynaecologic oncologist, and decided to proceed with an excisional biopsy instead of the initial intended oophorectomy, thus sparing the patient from unnecessary overtreatment.
Ultimately, histopathological examination remains the only diagnostic tool for a definitive diagnosis of CDL, whereby it is uniquely characterized by the presence of irregular nodular dissections of smooth muscle cells within the myometrium [
9].
The treatment options for CDL depend on several factors, including the patient’s age, symptoms, and desire for future fertility. In many cases, observation may be appropriate, especially in postmenopausal women who are asymptomatic. For symptomatic women, surgical resection may be recommended [
5].
4. Conclusions
CDL is is a rare, benign variant of leiomyoma with a good prognosis. However, it can be easily misdiagnosed as ovarian tumours, posing a diagnostic challenge for clinicians. This case and accompanying surgical video is among the first to feature a laparoscopic surgery of CDL and highlights the importance of thorough intraoperative exploration and careful consideration of uncommon differential diagnoses for ovarian tumours. Recognition and awareness of CDL by clinicians and pathologists can prevent misdiagnosis for a more sinister malignant condition, and consequently overtreatment, especially in fertility-seeking women. Further research may be required to gain a more comprehensive understanding of this pathological variant and develop more robust pre- and intra-operative diagnostic techniques.
Supplementary Materials
The following supporting information can be downloaded at the website of this paper posted on Preprints.org. Supplementary File 1: Surgical video depicting the case presentation and laparoscopic discovery and excision of the rare Cotyledonoid Dissecting Leiomyoma (CDL), initially misdiagnosed as an ovarian tumour.
Author Contributions
K.N.: Drafting the manuscript, narrating and editing of surgical video, critical review and editing of manuscript. T.R: Supervision, conceptualisation, lead clinician responsible for patient care including diagnosis and surgical treatment, recording of surgical video, critical review of manuscript. All authors have read and agreed to the published version of the manuscript.
Funding
This research received no external funding.
Data Availability Statement
The original contributions presented in this study are included in the article/supplementary material. Further inquiries can be directed to the corresponding author(s).
Conflicts of Interest
The authors declare no conflicts of interest. The article complies with institutional ethics guidelines.
References
- Roth, L.M., Reed, R.J. and Sternberg, W.H. (1996) ‘Cotyledonoid dissecting leiomyoma of the uterus’, The American Journal of Surgical Pathology, 20(12), pp. 1455–1461. [CrossRef]
- Xu, T. et al. (2016) ‘Cotyledonoid dissecting leiomyoma of the uterus: A report of four cases and a review of the literature’, Oncology Letters, 11(4), pp. 2865–2868. [CrossRef]
- Jamal, I. et al. (2019) ‘Cotyledonoid dissecting leiomyoma: An uncommon form of a common disease’, Obstetrics & Gynecology Science, 62(5), p. 362. [CrossRef]
- Abreu, R.F. et al. (2023) ‘Cotyledonoid dissecting leiomyoma of the uterus: A gross and radiologic malignancy mimicker’, International Journal of Gynecologic Cancer, 33(11), pp. 1827–1829. [CrossRef]
- Chahkandi, M. et al. (2023) ‘Cotyledonoid dissecting leiomyoma of the uterus: A case report and review of the literature’, Journal of Medical Case Reports, 17(1). [CrossRef]
- Asghari, K.M., Tabrizi, A.D. and Madani, P.S. (2024) ‘Unraveling the mystery of uterine cotyledonoid dissecting leiomyoma: A case report’, European Journal of Gynaecological Oncology, 45(3), p. 167. [CrossRef]
- Yarram, S.G. et al. (2007) ‘Evaluation of imaging-guided core biopsy of pelvic masses’, American Journal of Roentgenology, 188(5), pp. 1208–1211. [CrossRef]
- Saeed, A.-S. et al. (2006) ‘Cotyledonoid dissecting leiomyoma of the uterus’, International Journal of Gynecological Pathology, 25(3), pp. 262–267. [CrossRef]
- Fernandez, K., Cheung, L. and Taddesse-Heath, L. (2022) ‘Cotyledonoid dissecting leiomyoma: A rare variant of leiomyoma of the uterus’, Cureus [Preprint]. [CrossRef]
- Karki, D., Shrestha, G. and Joshi, S.L. (2024) ‘A case of cotyledonoid dissecting leiomyoma with associated disseminated peritoneal leiomyomatosis: The significance of frozen section in identification of this unusual entity’, Cureus [Preprint]. [CrossRef]
|
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2025 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (http://creativecommons.org/licenses/by/4.0/).