1. Introduction
Wearable sensors are increasingly recognized as essential tools in the field of medicine, particularly for the management of chronic diseases. These devices effectively mon-itor a variety of chronic diseases, including diabetes, cardiovascular diseases, panic disorders, chronic obstructive pulmonary disease (COPD), arthritis, and Parkinson’s disease, which encompasses motor and nonmotor symptoms experienced by patients [
1]. Traditional methods for monitoring and managing chronic health conditions often prove to be inaccurate and time-consuming; thus, wearable technology is emerging as a transformative solution in this domain.
To optimize chronic disease management, healthcare systems must prioritize the establishment of patient-centric frameworks that allow people to participate in self-management strategies [
2]. Wearable sensors facilitate the continuous monitoring of vital parameters such as blood pressure, temperature, and blood glucose levels, pro-viding real-time data that improve the management of these conditions. Wearable devices commonly used include heart monitors, fitness trackers (for example, Fitbits), glucometers, and pedometers [
3]. These tools not only promote self-management, but also encourage patients to take an active role in their health care [
4].
The increasing prevalence of chronic diseases underscores the growing demand for effective wearable devices. Advances in wearable sensor technology are anticipated to significantly improve both the detection and management of these conditions [
5]. For example, cardiac rehabilitation programs have shown benefits in the prevention of heart disease [
6]. By integrating wearable devices into healthcare systems, a substan-tial transformation in patient care can be achieved. Future designs of these devices should prioritize efficiency and cost-effectiveness while ensuring that user privacy and comfort remain uncompromised.
The existing literature has documented various wearable devices used in chronic disease management, detailing their types and applications. The evolution of wearable technology encompasses both body-worn devices and supplementary add-ons [
7]. This review focuses exclusively on chronic diseases such as diabetes, cardiovascular dis-ease, Parkinson’s disease, and arthritis. The selection is based on the severity of these conditions, the existing literature, and the potential of wearable sensors to improve management strategies. This study serves as a valuable resource for healthcare profes-sionals, including scientists and clinicians, who seek to leverage wearable technology effectively [
8].
The paper discusses the management of chronic diseases through wearable sen-sors by following several key steps: an examination of various wearable devices and their applications in managing chronic conditions; an analysis of the effectiveness of these devices in patient behavior and treatment outcomes; a discussion of the chal-lenges faced while utilizing wearable technology for chronic disease management; and recommendations for future research directions.
2. Literature Review
Wearable sensors are advanced devices that monitor daily human activities and phys-iological parameters. They measure vital signs such as body temperature, blood pressure, heart rate, gait, and blood glucose levels. These sensors are widely utilized not only for fitness maintenance but also for capturing gait information, including speed, position, and acceleration. Their role is particularly crucial in the management of chronic diseases by continuously monitoring patient behaviors and activities. This paper explores the effectiveness of wearable sensors in the management of chronic diseases such as diabetes, cardiovascular disease, depression, and arthritis.
The prevalence of chronic diseases is increasing rapidly, necessitating effective mon-itoring and management strategies to mitigate their impact on individuals’ health and lifestyle. For example, cardiovascular diseases can cause lifelong health problems if not properly managed. Wearable sensors facilitate the monitoring of critical physiological parameters, such as temperature, blood sugar, blood pressure, and heart rate, provid-ing valuable data to manage these conditions. The massive development and impact of wearable technology in the management of chronic diseases have been extensively reviewed; however, challenges related to data accuracy and privacy remain significant issues that warrant further research [
9].
The importance of using wearable technology to monitor and manage chronic dis-eases cannot be overstated. According to Bain & Company, wearable devices such as fitness trackers, smartwatches, and step counters positively affect the performance of healthcare organizations by allowing the rapid detection, planning and treatment of patients with chronic diseases. These opportunities are well documented in the literature; however, future research must address critical aspects such as data secu-rity, privacy concerns, and compatibility of wearable sensors with existing healthcare systems [
10].
Globally, wearable technology-based telecare systems are gaining traction. Com-pared to traditional methods, wearable technology offers superior capabilities for predicting and preventing chronic diseases. Studies indicate that wearable technology has achieved approximately 46 percent accuracy in predictions; moreover, conditions such as panic disorders and diabetes benefit from more efficient data collection than traditional questionnaires. Implementing a model for managing chronic diseases with wearable technology requires data from various sources—including wearable sensors, mobile applications, environmental sensors—and the integration of deep learning algo-rithms. However, this model has limitations; it is not generalizable across diverse populations and may become less effective when applied to larger sample sizes. Future work should focus on expanding sample sizes and enhancing contextual feasibility [
11].
While the usability of wearable devices has been extensively studied, less attention has been devoted to understanding patients’ feelings regarding these technologies. This study addresses this gap by assessing usability through common patterns derived from surveys and questionnaires. Out of 37 papers reviewed, 71 percent exhibited biases in measuring mobility through wearable devices across various chronic conditions such as COPD and Parkinson’s disease. In some instances, usability was inadequately defined; thus, future research should aim to improve assessment quality through mixed methodologies and verified questionnaires [
12].
Wearable devices can effectively monitor communicable diseases at early stages when symptoms are minimal. They enable both individual- and community-level pre-vention strategies. Research indicates that these devices can gather real-time data on vital parameters like temperature, blood pressure, and blood glucose levels at a low cost. This real-time information can be integrated with healthcare systems to improve performance at the community level; however, ethical considerations require the establishment of clear criteria for appropriate use [
13].
There is a communication gap between chronic disease patients and their levels of physical activity. Thus, there is a need for strategic planning to improve physical activity through the efficient use of wearable sensors such as smartwatches and step counters. These devices provide users with health-related information tailored to their levels of usage. Patients with chronic disease are likely to benefit significantly from these technologies as they promote increased physical activity (AP). Further investi-gation into the impact and challenges of wearables—particularly regarding their role in enhancing PA among patients with chronic conditions—is warranted [
14].
Although wearables designed for activity tracking are beneficial in chronic disease management, they have yet to be fully integrated into self-management programs due to insufficient continuous data regarding usage and results. The use of wearable technology enhances patient engagement by providing immediate real-time data feed-back. Establishing standards for patient-centered evaluations that focus on motivation and data privacy is essential. Concepts from behavioral science could be harnessed to optimize the use of wearable devices in clinical settings. Future research should address issues related to measurement accuracy, integration with patient care planning systems, and privacy concerns [
3].
There is a strong relationship between wearable devices and healthcare outcomes; managing chronic diseases through wearables fosters better self-care and patient engagement. Numerous studies have documented the positive effects of these devices on health outcomes, such as pain relief and improved quality of life, while some surveys report negligible impacts. Two main studies evaluating the effectiveness of wearables in chronic disease management include randomized control trials (RCTs) and observational studies (OBSs) conducted between January 2016 and July 2021. These investigations focus primarily on type 2 diabetes and Parkinson’s disease while evaluating usability based on cost effectiveness, viability for patients, and healthcare outcomes. Given the existing inconsistencies in current data, future studies should focus on improving the quality and authenticity of the findings to improve the efficacy of wearables in disease management [
15].
This study analyzes key points regarding the role of wearables in preventing the deterioration of chronic conditions. While evidence suggests that wearables are effective tools for managing chronic diseases, they also present challenges that hin-der treatment efficacy. Various analyzes were performed using partial least squares (PLS) software; unexpectedly negative associations were found between wearables and healthcare outcomes compared to anticipated benefits. Future research should inves-tigate these contradictions further to identify underlying issues that may impede the effectiveness of wearables in managing chronic diseases [
16].
Existing studies have focused primarily on the usability of wearable sensors in various medical fields related to both physical and mental health conditions. This research specifically examines chronic diseases such as diabetes, Parkinson’s disease, cardiovascular diseases, and COPD to assess the impact of wearable sensors on their management. The aim is to analyze relevant data that support the implementation of wearable devices to effectively manage these chronic conditions.
3. Methodology
In this review article, a systematic review approach is used to evaluate and ana-lyze the effectiveness of wearable sensors in the management of chronic diseases and the improvement of quality of life [
17]. This methodology has been selected to accu-rately summarize the existing literature, highlight limitations, and recommend future research directions.
To identify and evaluate relevant literature, a unique and systematic search strategy was developed, encompassing electronic databases such as Google Scholar, Sci-Hub, and IEEE Xplore [
18]. The search terms included “wearable”, “sen-sors”, “chronic”, “disease”, “management”, “effectiveness”, “monitoring”, “efficacy”, “health”, “devices”, “outcomes” and “improvement”. To focus on recent developments, only research papers published in the range of 2015 to 2024 were included. The databases used for this review were Google Scholar, Sci-Hub, and IEEE Xplore.
The inclusion criteria for the selection of research papers were based on their rele-vance to wearable sensors used in the management of chronic diseases, publication in the last ten years, and peer-reviewed status [
2]. In contrast, articles that were irrele-vant, published before 2015 or not reviewed by peers were excluded from consideration [
19]. Research papers were selected based on several criteria: preference was given to the most relevant papers concerning the effectiveness of wearable sensors in manag-ing chronic diseases; only papers published within the last ten years (2015–2024) were considered; articles with higher impact factors received greater preference; articles with a greater number of citations were favored; and selected articles were required to demonstrate high methodological quality.
Data were extracted on the basis of various parameters. The types of wearable sensors included wearable electrocardiography (ECG) devices such as smartwatches and wristbands, photoplethysmography (PPG) devices such as headbands, earphones and gloves, ballistocardiographs (BCG), biofluidic-based wearables, phonocardiogra-phy (PCG), fitness trackers, Fitbit devices, heart rate smart wristbands and Samsung charms [
20,
21]. The usage protocols varied between studies, with monitoring dura-tions reported as 6 weeks, 7 weeks, and 12 weeks [
6]. The key parameters monitored included blood pressure, body temperature, heart rate, pulse waveform, movement, step count, and calories burned [
15,
20].
The analysis involved classifying findings from the selected studies regarding the impact of wearable sensors on managing chronic diseases. Studies were grouped by types of wearable sensors and their applications [
4]. A comparative analysis was performed on the data obtained from the literature review to investigate patterns, advantages, and drawbacks associated with various types of sensors and their appli-cation approaches. Thematic analysis of the reviewed papers identified emerging wearable technologies. Some studies involved participants over 50 who had been diagnosed with one or more chronic diseases [
22].
To ensure the reliability of the review, the quality of each selected study was evaluated using defined criteria such as relevance, publication year, impact factor, and number of citations. Seventy percent of the articles reviewed were identified as the top-published articles; the remaining thirty percent were deemed most relevant regardless of publication year or impact factor.
Ethical considerations involved the responsible use of published data and appro-priate citation of sources. No primary data was collected for this review; all reviewed studies were cited in accordance with academic standards.
This review is limited by the heterogeneity of studies included, variability in sen-sor accuracy, and ongoing technological advancements. The inclusion criteria may also introduce selection bias towards more recent and high-impact publications. Addition-ally, access to digital libraries may not be readily available for quick resource retrieval [
19].
This review follows a systematic methodology to identify the literature, select relevant studies, extract data, analyze findings, and evaluate quality. The goal is to provide a comprehensive summary of the effectiveness of wearable sensors in managing chronic diseases. By maintaining methodological rigor throughout the review process, the reliability and relevance of the findings are ensured, thereby establishing a strong foundation for subsequent findings, discussions, and critical evaluations within this rapidly evolving field.
4. Results
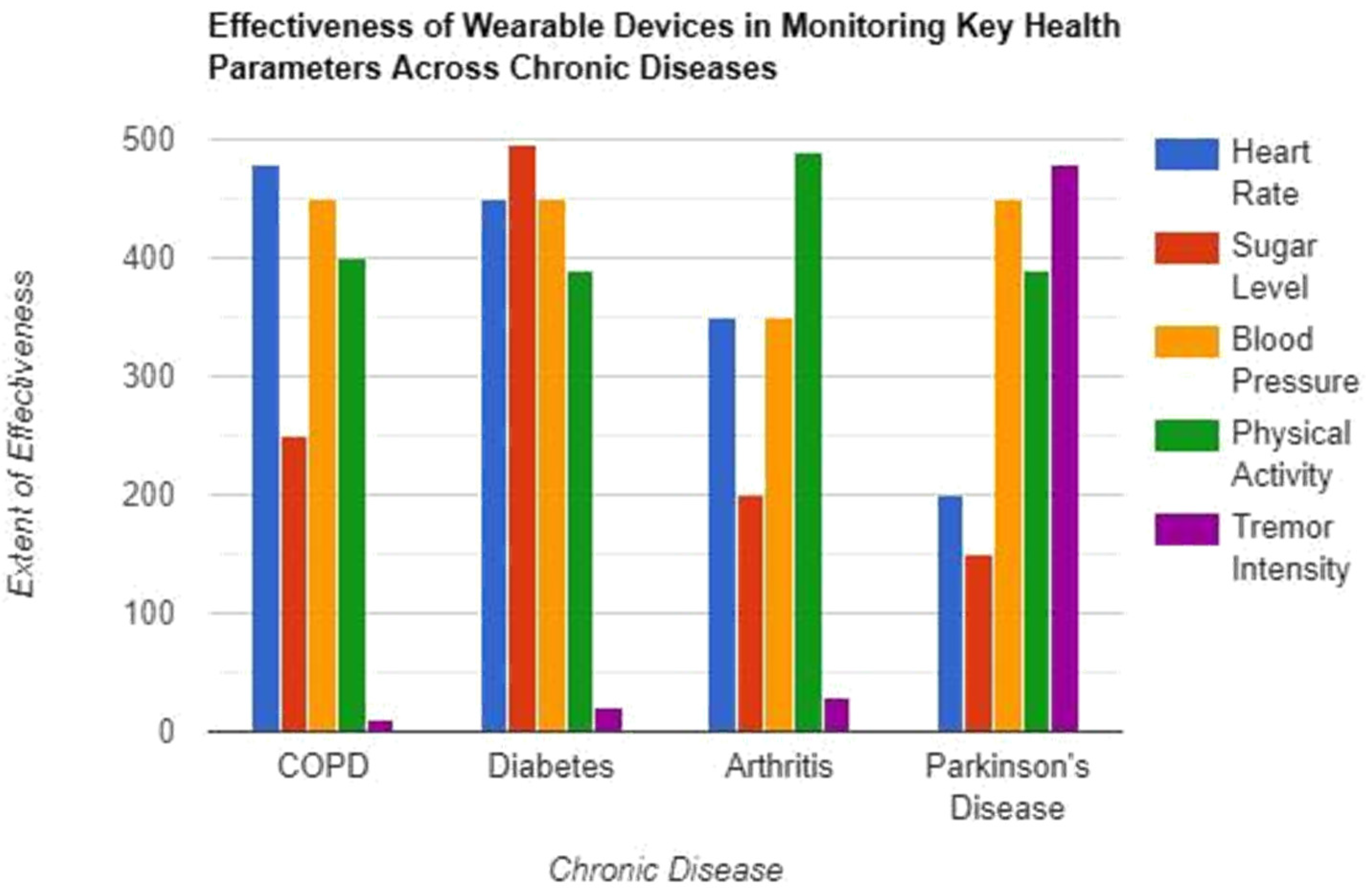
In chronic obstructive pulmonary disease (COPD), the most effectively monitored parameter is heart rate, followed by blood pressure, physical activity, and sugar level, with the intensity of tremors being monitored less effectively. In diabetes, the sugar level is most effectively monitored, followed by blood pressure and heart rate, with physical activity observed next and the intensity of the tremors tracked the least. For arthritis, physical activity is the most effectively monitored parameter, followed by blood pressure and heart rate, the sugar level is next monitored, and the intensity of the tremor is the least effectively tracked. In Parkinson’s disease, the intensity of tremors is monitored most effectively, followed by blood pressure, physical activity, heart rate, and sugar level, which is monitored the least (
Figure 1).
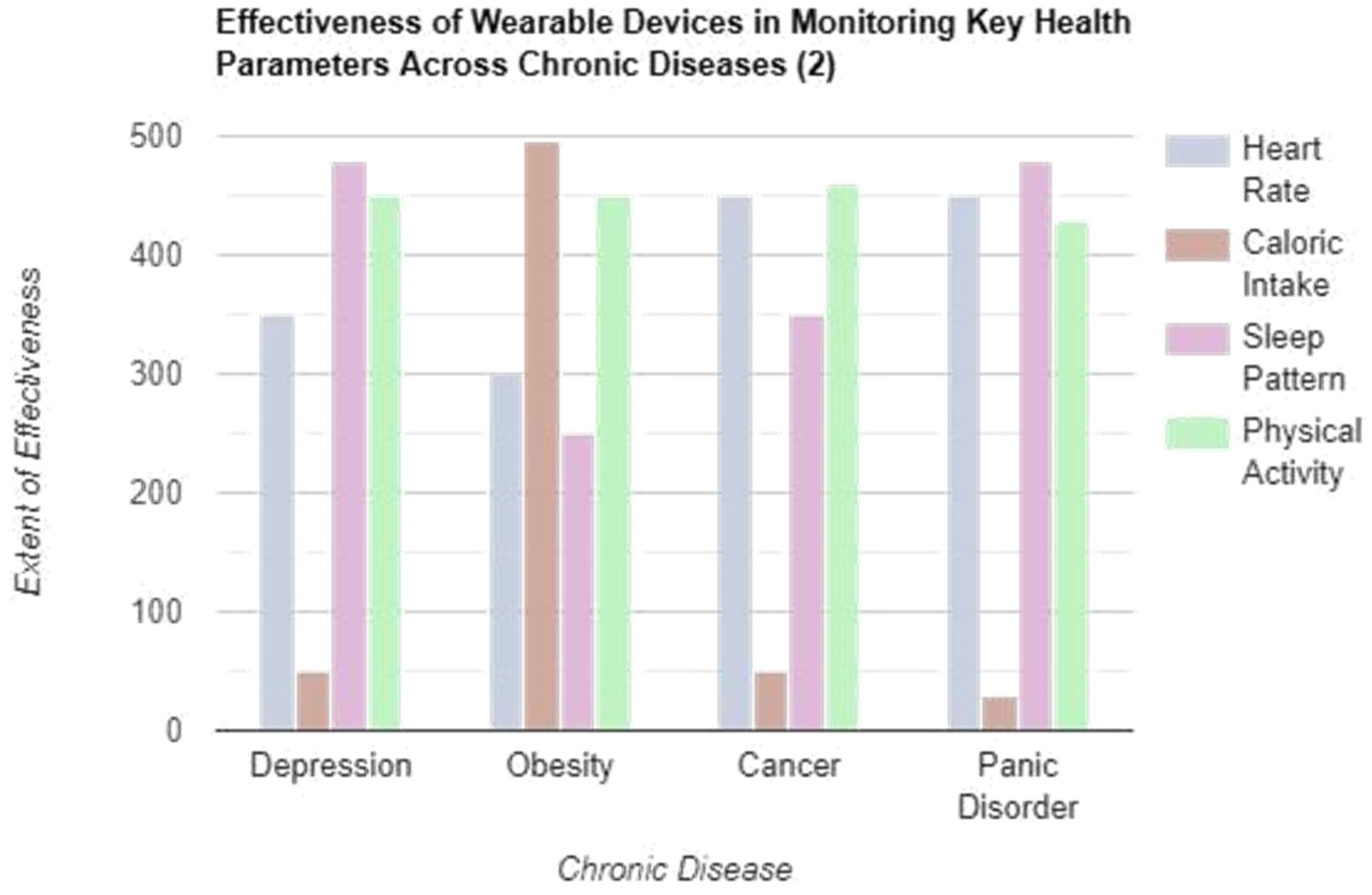
In depression, the most effectively monitored parameter is the sleep pattern, fol-lowed by physical activity, heart rate, and caloric intake. In obesity, caloric intake is monitored more effectively, followed by physical activity, heart rate, and sleep pattern that is most closely monitored. For cancer, physical activity is the most effectively monitored parameter, followed by heart rate, sleep pattern is next monitored, and caloric intake is the least efficiently tracked. In Panic disorder, sleep pattern is mon-itored most effectively, followed by heart rate, physical activity, and caloric intake, which is monitored least. This structured approach highlights the varying effective-ness of wearable devices in tracking specific health parameters across different chronic diseases, emphasizing the importance of customized monitoring strategies for optimal patient management (
Figure 2).
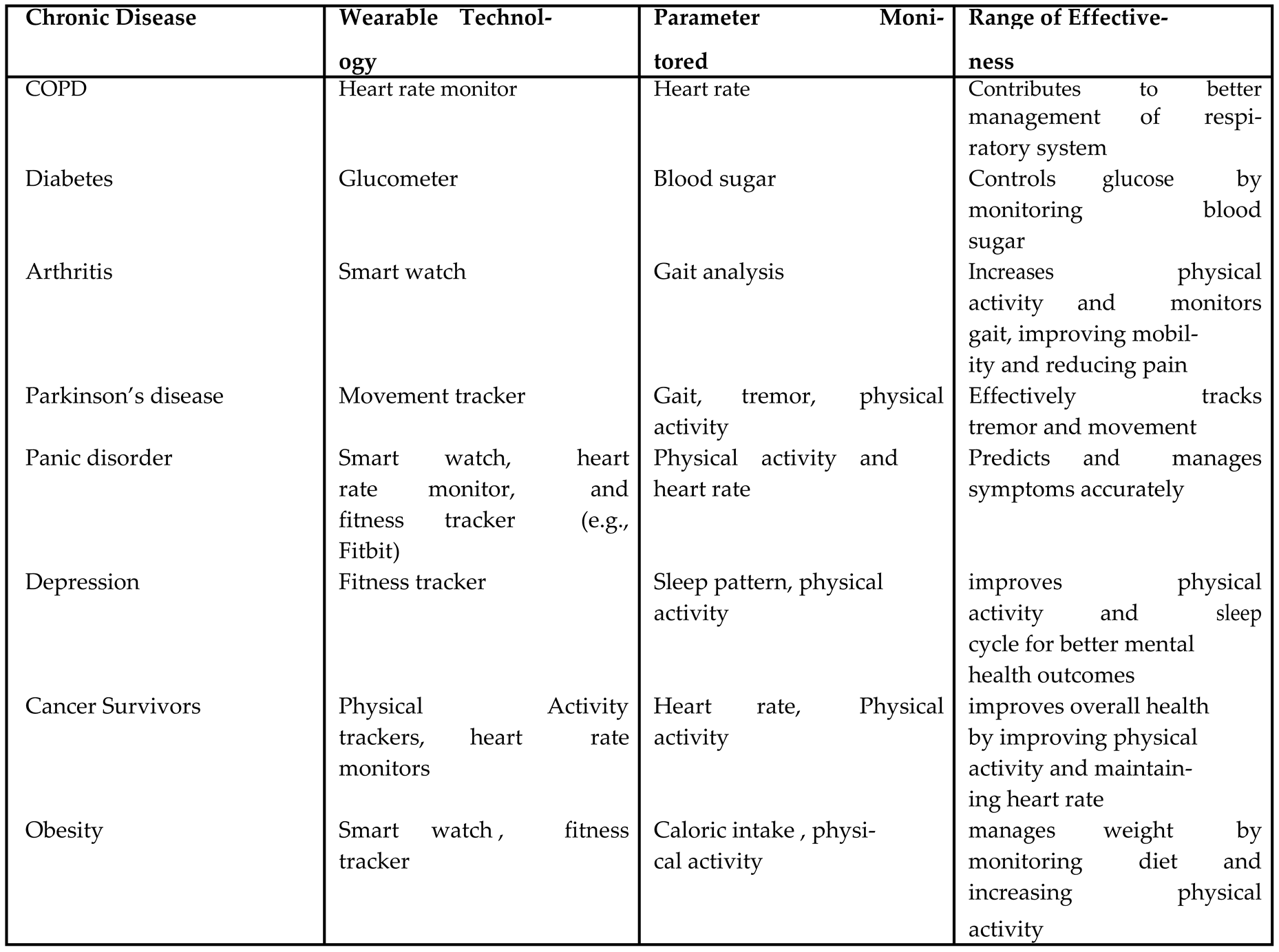
Various chronic diseases such as COPD, diabetes, Parkinson’s disease etc are man-aged effectively by different types of wearable devices including smart watch, heart rate monitor, glucometer, fitness trackers etc by monitoring key health parameters like blood sugar, heart rate, physical activity etc (
Table 1).
5. Discussion
The results underscore the critical role of wearable sensors in the management of chronic diseases. Wearable devices facilitate wireless communication with stationary gateway devices, enabling an effective and efficient transfer of sensor data [
23]. The advent of remote patient monitoring has made wearable sensors transformative tools in the monitoring and management of chronic diseases [
8]. This approach, utilizing wearable technology for chronic disease management, is more efficient and compre-hensive than traditional methods. Wearable technology continuously monitors vital physiological parameters, such as body temperature, blood glucose levels, and blood pressure, providing real-time data that improve disease management.
In diabetes management, maintaining optimal blood sugar levels is crucial. This is achieved through the use of wearable sensors, such as fitness trackers and glucometers, which promote increased physical activity and help regulate glucose levels in the body. Similarly, the management of cardiovascular diseases has been facilitated by wearable technology, including heart rate monitors. Furthermore, fitness trackers play an important role in promoting physical activity among patients and maintaining their blood pressure, thus contributing to general health and well-being [
24] .
Wearable technology has significantly revolutionized the management of chronic diseases. Research conducted by Bain and Company and other scholars has established that wearable sensors play a vital role in improving patient health outcomes [
10]. Although previous studies have examined the general application of wearable tech-nology in healthcare, this study specifically focuses on the impact of using wearable devices to manage chronic diseases. Chronic diseases considered include cardiovascu-lar diseases such as chronic obstructive pulmonary disease (COPD), panic disorder, diabetes, arthritis, and Parkinson’s disease, conditions characterized by motor and nonmotor symptoms that affect patient health [
25].
Wearable sensors incorporated with artificial intelligence (AI) exhibit substantial potential to predict and control chronic diseases, providing efficient methods to man-age these conditions. In contrast to traditional methods that rely on questionnaires for collecting data related to chronic diseases, portable devices have been shown to be more effective in collecting real-time data and managing these conditions [
11].
The findings reveal extensive practical implications for the integration of wearable sensors in the management of chronic diseases. Wearable devices have proven to be transformative in monitoring and managing chronic diseases by continuously track-ing vital physiological parameters in the bodies of patients and providing real-time data, facilitating efficient disease management [
26]. Furthermore, wearable technology enhances self-management capabilities and supports personalized treatment plans, ultimately contributing to improved quality of life. The economic advantages of uti-lizing wearable technology are notable, as they can reduce the frequency of medical visits, thereby alleviating the burden on healthcare systems.
By integrating wearable sensors into healthcare frameworks, resources can be uti-lized more efficiently. Individualized care is promoted through these sensors, as they enhance treatment plans and improve patient engagement. For instance, diabetes man-agement through wearable sensors exemplifies the Internet of Medical Things (IoMT), where devices are employed in a distributed manner to effectively manage health conditions [
27]. Fitness trackers play a significant role in improving physical activity levels, which can help reduce symptoms such as stiffness , while continuous glucose monitors provide real-time feedback based on ongoing patient monitoring, thereby facilitating effective diabetes management through wearable technology [
28].
Moreover, wearables are increasingly integrated into clinical trials aimed at pre-venting heart failure , and mobile cardiac telemetry (MCT) is utilized for cardiac monitoring through compact portable devices . These advancements underscore the potential of wearable technology to enhance patient outcomes and promote proactive health management [
29,
30].
The findings of this study reveal that there are unexpected outcomes associated with the use of wearable technology in chronic disease management. For certain spe-cific diseases, a negative relationship has been observed between wearable devices and treatment outcomes [
31]. Several studies have indicated that the implementation of wearable technology does not consistently yield beneficial results for healthcare out-comes and disease management. It is essential to employ alternative methods that consider the severity and type of disease, as anomalies have been noted in the efficacy of wearable technology.
The effectiveness of wearable technology can be significantly improved by its integration with existing healthcare systems [
3]. This integration facilitates seamless interoperability, allowing wearable-generated data, such as vital signs and patient activity, to become an integral part of electronic health records (EHRs). This inte-gration not only promotes data-driven clinical decision making, but also enables healthcare providers to monitor patients remotely. By ensuring that wearable data are effectively incorporated into clinical workflows, the overall efficiency and utility of these devices can be improved, thus maximizing their potential benefits for chronic disease management.
There is considerable variability in the scope and quality of existing studies, which highlights several limitations, including generalizability, sample size, and study design. The applicability of wearable technology to broader contexts and diverse popula-tions is constrained by issues related to generalizability. Discrepancies have also been observed in the effectiveness of wearable sensors in the management of chronic diseases such as Parkinson’s disease and chronic obstructive pulmonary disease (COPD) [
12].
To optimize the utilization of wearable technology in chronic disease management, there is a pressing need for more synthesized methodologies. This can be achieved by conducting comparative analyses of different wearable sensors to evaluate their usabil-ity and effectiveness comprehensively. Furthermore, the adoption of wearables can be hindered by ethical considerations and technical barriers, particularly in low- and middle-income countries (LMICs) . Addressing these challenges is crucial to improve the integration of wearable devices into healthcare systems, thus maximizing their potential benefits for chronic disease management.
This study makes a significant contribution to the advancing field of healthcare through the application of wearable technology. It emphasizes the utilization of wear-able technology for the management of chronic conditions. Chronic diseases considered include diabetes, chronic obstructive pulmonary disease (COPD), Parkinson’s dis-ease, panic disorder, and cardiovascular diseases. This research delineates how these wearable sensors can be used effectively to control and manage chronic diseases.
Not only can chronic diseases be managed using wearable technology, traditional methods can also be revolutionized through the integration of wearable sensors [
32]. Wearable devices precisely measure human movement and track the effects of disease [
33]. These devices provide crucial data that improve the efficiency of tools used to manage chronic diseases. The integration of wearable sensors with healthcare systems is highly emphasized. Through wearable technology, patients become more actively involved in disease management, promoting self-management practices. Patients must be actively involved in their treatment, as chronic diseases can become severe if not addressed effectively in 3 months [
34]. Wearable devices deliver real-time data and statistics, allowing patients to manage their health by monitoring physical activities and other vital parameters. Devices such as glucose monitors, Fitbits, heart rate mon-itors, and fitness trackers continuously monitor patients and provide real-time data to manage chronic conditions. Furthermore, wearable technology is beneficial for prevent-ing and managing COVID-19, as heart rate monitoring and physical activity analysis are critical for affected patients [
35,
36]. Through the use of wearables, patients’ quality of life is improved and healthcare organizations experience significant relief in various aspects, as sensors help at every stage of diagnosis and disease management.
Wearable technology is designed to be safe and standardized for its users. The design and applications of wearable devices can be innovated in the future through groundbreaking research [
37]. For certain diseases, such as diabetes and cardiovascular disease, wearables have been shown to be transformative. However, several challenges persist with wearable technology, including privacy concerns for users, data accuracy, and the integration of wearables with existing healthcare systems. These challenges must be addressed to scale up wearable technology and enhance its efficiency.
5.1. Remote Patient Monitoring through Wearable Sensors for Chronic Disease Management
Remote Patient Monitoring (RPM), enhanced by advances in Artificial Intelligence (AI), 5G, and the Internet of Things (IoT), is transforming healthcare. These tech-nologies support chronic disease management by enabling real-time tracking of vital health parameters through wearable devices. With a global aging population and an increase in chronic diseases, healthcare systems are facing significant strain. The integration of wearable sensors into healthcare infrastructures has the potential to alleviate this burden, providing a scalable approach to continuous patient monitoring [
38,
39,
40,
41].
RPM systems employ IoT-enabled wearable sensors to support chronic disease management by facilitating continuous monitoring and enabling early intervention. For instance, conditions such as diabetes, cardiovascular diseases, and other chronic ill-nesses have shown improved outcomes when managed with wearable sensors integrated with smartphone applications and biosensors [
42,
43,
44]. The synergy between wear-able devices and IoT can reduce healthcare costs, enhance patient quality of life, promote patient independence, and improve overall health outcomes through data-driven, personalized care. Elderly patients and those with chronic health conditions, in particular, benefit from RPM, as the ability to monitor essential health metrics like heart rate, blood pressure, and glucose levels is crucial for early detection and prevention [
45,
46,
47].
RPM technologies encompass various applications, including chronic disease man-agement, elderly care, and continuous health surveillance through Ambient Assisted Living (AAL) and wearable sensor networks. These systems enable patients to man-age their health conditions and receive timely intervention when necessary, thus improving both safety and autonomy [
48,
49,
50]. The versatility of wearable tech-nologies—ranging from body-mounted devices and textile-based sensors to contactless monitoring—facilitates customized solutions that address individual patient needs. RPM systems extend beyond vital sign monitoring; they also provide educational resources, support early disease detection, and strengthen patient engagement with healthcare providers [
46,
47,
51].
Despite the promising potential of RPM systems, several critical challenges remain. Key issues include data security, privacy, scalability, and data management. The inte-gration of wearable sensors with big data elements, such as high data velocity and volume, complicates data processing and patient prioritization [
38,
40,
48]. Many RPM systems are limited in scalability due to the lack of interoperability between various healthcare systems, restricting their greater integration and application capa-bilities [
43,
50]. Data privacy is also a paramount concern, as wearable technologies collect sensitive health information, necessitating the use of secure, compliant data transmission protocols [
42,
49]. Furthermore, achieving clinical acceptance and vali-dation of wearable devices remains challenging, particularly in conditions that demand precise data measurement and reliable data transmission [
30,
47].
To address these challenges, enhancing RPM system interoperability is essential. Integrating AI for predictive analysis, early detection, patient prioritization, and auto-mated decision-making can further improve the functionality of RPM systems. When supported by real-time data analysis and low-latency data transfer, wearable devices have the potential to significantly improve the accuracy, efficiency, and reliability of chronic disease management [
41,
44,
46]. Optimizing wearable technology to over-come limitations in data security, energy efficiency, and communication protocols will be crucial for achieving sustainable long-term chronic disease management. Further-more, widespread clinical validation and integration between healthcare systems are necessary to facilitate broader adoption in conventional healthcare settings [
45,
51].
In conclusion, wearable sensor technology-based RPM systems offer a transfor-mative approach to managing chronic diseases, enabling real-time monitoring and promoting patient self-care. Although RPM has already shown improved patient outcomes, more advances are needed to enhance security, scalability, and system inte-gration. Once these challenges are addressed, the full potential of IoT and wearable sensors can be realized in healthcare care, paving the way for more effective and sustainable chronic disease management [
38,
40,
50].
6. Conclusion
This review highlights the importance of using wearable sensors in the management of chronic diseases. The chronic diseases discussed include diabetes, chronic obstruc-tive lung disease (COPD), Parkinson’s disease, cardiovascular disease, panic disorder, and arthritis. The findings demonstrate that wearable technology is critical in the management of chronic diseases by monitoring vital parameters and providing real-time data. This capability assists in the early detection of symptoms and the design of personalized treatment plans for patients.
For certain chronic diseases, such as diabetes and cardiovascular conditions, wear-able technology has a significant impact, as these conditions require continuous monitoring and management based on real-time data. Conversely, for other condi-tions such as depression and anxiety, wearable technology has not proven to be as beneficial; however, this area can be improved in the future through further research.
There are several challenges that wearable technology faces in the management of chronic diseases that must be addressed to fully utilize wearable sensors within healthcare systems. Future researchers are encouraged to improve the quality of wear-able technology and integrate it with existing healthcare systems to revolutionize the medical field. In addition, data accuracy and user privacy concerns must be taken into account in future designs to develop better wearable devices that align with user comfort levels. Wearable technology can also help with the management of psycholog-ical disorders by accurately monitoring and responding to psychological changes. By exploring additional areas such as mental illnesses, future research could significantly enhance the utilization of wearable technology within healthcare systems.
Data Availability
Not applicable.
Declaration of interests
The authors declare that they have no known competing financial interests or personal relationships that could have appeared to influence the work reported in this paper. The participants consented to the publication.
Conflict of interest
The authors declare no conflict of interest.
References
- de Lima, A.L.S.; Hahn, T.; Evers, L.J.W.; de Vries, N.M.; Cohen, E.; Afek, M.; Bataille, L.; Daeschler, M.; Claes, K.; Boroojerdi, B.; et al. Feasibility of large-scale deployment of multiple wearable sensors in Parkinson's disease. PLOS ONE 2017, 12, e0189161. [Google Scholar] [CrossRef]
- Wulfovich, S.; Fiordelli, M.; Rivas, H.; Concepcion, W.; Wac, K. “I Must Try Harder”: Design Implications for Mobile Apps and Wearables Contributing to Self-Efficacy of Patients With Chronic Conditions. Front. Psychol. 2019, 10, 2388. [Google Scholar] [CrossRef] [PubMed]
- Chiauzzi, E.; Rodarte, C.; DasMahapatra, P. Patient-centered activity monitoring in the self-management of chronic health conditions. BMC Med. 2015, 13, 1–6. [Google Scholar] [CrossRef] [PubMed]
- Jiang, J.; Cameron, A.-F. IT-Enabled Self-Monitoring for Chronic Disease Self-Management: An Interdisciplinary Review. MIS Q. 2020, 44, 451–508. [Google Scholar] [CrossRef]
- Kario, K.: Management of hypertension in the digital era: small wearable monitor-ing devices for remote blood pressure monitoring. Hypertension 76(3), 640–650 (2020).
- Antoniou, V.; Xanthopoulos, A.; Giamouzis, G.; Davos, C.; Batalik, L.; Stavrou, V.; I Gourgoulianis, K.; Kapreli, E.; Skoularigis, J.; Pepera, G. Efficacy, efficiency and safety of a cardiac telerehabilitation programme using wearable sensors in patients with coronary heart disease: the TELEWEAR-CR study protocol. BMJ Open 2022, 12, e059945. [Google Scholar] [CrossRef]
- Guk, K.; Han, G.; Lim, J.; Jeong, K.; Kang, T.; Lim, E.-K.; Jung, J. Evolution of Wearable Devices with Real-Time Disease Monitoring for Personalized Healthcare. Nanomaterials 2019, 9, 813. [Google Scholar] [CrossRef]
- Appelboom, G.; Camacho, E.; E Abraham, M.; Bruce, S.S.; Dumont, E.L.; E Zacharia, B.; D’amico, R.; Slomian, J.; Reginster, J.Y.; Bruyère, O.; et al. Smart wearable body sensors for patient self-assessment and monitoring. Arch. Public Heal. 2014, 72, 28–28. [Google Scholar] [CrossRef]
- Guo, Y.; Liu, X.; Peng, S.; Jiang, X.; Xu, K.; Chen, C.; Wang, Z.; Dai, C.; Chen, W. A review of wearable and unobtrusive sensing technologies for chronic disease management. Comput. Biol. Med. 2021, 129, 104163–104163. [Google Scholar] [CrossRef]
- Adeghe, E.P.; Okolo, C.A.; Ojeyinka, O.T. A review of wearable technology in healthcare: Monitoring patient health and enhancing outcomes. Open Access Res. J. Sci. Technol. 2024, 7, 142–148. [Google Scholar] [CrossRef]
- Husnain, A., Hussain, H.K., Shahroz, H.M., Ali, M., Hayat, Y.: A precision health initiative for chronic conditions: Design and cohort study utilizing wearable tech-nology, machine learning, and deep learning. International Journal of Advanced Engineering Technologies and Innovations 1(2), 118–139 (2024).
- Keogh, A.; Argent, R.; Anderson, A.; Caulfield, B.; Johnston, W. Assessing the usability of wearable devices to measure gait and physical activity in chronic conditions: a systematic review. J. Neuroeng. Rehabilitation 2021, 18, 1–17. [Google Scholar] [CrossRef]
- Ming, D.K., Sangkaew, S., Chanh, H.Q., Nhat, P.T., Yacoub, S., Georgiou, P., Holmes, A.H.: Continuous physiological monitoring using wearable technology to inform individual management of infectious diseases, public health and outbreak responses. International Journal of Infectious Diseases 96, 648–654 (2020).
- Scheid, J.L.; West, S.L. Opportunities of Wearable Technology to Increase Physical Activity in Individuals with Chronic Disease: An Editorial. Int. J. Environ. Res. Public Heal. 2019, 16, 3124. [Google Scholar] [CrossRef] [PubMed]
- Mattison, G., Canfell, O., Forrester, D., Dobbins, C., Smith, D., T¨oyr¨as, J., Sul-livan, C.: The influence of wearables on health care outcomes in chronic disease: systematic review. Journal of Medical Internet Research 24(7), 36690 (2022).
- Yu, S.; Chen, Z.; Wu, X. The Impact of Wearable Devices on Physical Activity for Chronic Disease Patients: Findings from the 2019 Health Information National Trends Survey. Int. J. Environ. Res. Public Heal. 2023, 20, 887. [Google Scholar] [CrossRef] [PubMed]
- El-Amrawy, F., Nounou, M.I.: Are currently available wearable devices for activ-ity tracking and heart rate monitoring accurate, precise, and medically beneficial? Healthcare informatics research 21(4), 315–320 (2015).
- Rovini, E.; Maremmani, C.; Cavallo, F. How Wearable Sensors Can Support Parkinson's Disease Diagnosis and Treatment: A Systematic Review. Front. Neurosci. 2017, 11, 555–555. [Google Scholar] [CrossRef] [PubMed]
- Texas Tech University; Yu, S.; Chai, Y.; Hefei University of Technology; Chen, H.; University of Arizona; Sherman, S.J.; Brown, R.A.; Intelligence, L.H.M. Wearable Sensor-Based Chronic Condition Severity Assessment: An Adversarial Attention-Based Deep Multisource Multitask Learning Approach. MIS Q. 2022, 45, 1355–1394. [CrossRef]
- Cappon, G., Acciaroli, G., Vettoretti, M., Facchinetti, A., Sparacino, G.: Wear-able continuous glucose monitoring sensors: a revolution in diabetes treatment. Electronics 6(3), 65 (2017).
- Hickey, B.A.; Chalmers, T.; Newton, P.; Lin, C.-T.; Sibbritt, D.; McLachlan, C.S.; Clifton-Bligh, R.; Morley, J.; Lal, S. Smart Devices and Wearable Technologies to Detect and Monitor Mental Health Conditions and Stress: A Systematic Review. Sensors 2021, 21, 3461. [Google Scholar] [CrossRef]
- Mercer, K.; Giangregorio, L.; Schneider, E.; Chilana, P.; Li, M.; Grindrod, K. Acceptance of Commercially Available Wearable Activity Trackers Among Adults Aged Over 50 and With Chronic Illness: A Mixed-Methods Evaluation. JMIR mHealth uHealth 2016, 4, e7. [Google Scholar] [CrossRef]
- Aliverti, A. Wearable technology: role in respiratory health and disease. Breathe 2017, 13, e27–e36. [Google Scholar] [CrossRef]
- Iqbal, S.M.A.; Mahgoub, I.; Du, E.; Leavitt, M.A.; Asghar, W. Advances in healthcare wearable devices. npj Flex. Electron. 2021, 5, 1–14. [Google Scholar] [CrossRef]
- Mughal, H., Javed, A.R., Rizwan, M., Almadhor, A.S., Kryvinska, N.: Parkin-son’s disease management via wearable sensors: a systematic review. IEEE Access 10, 35219–35237 (2022).
- Ibrahim, T., Ali, H.: The impact of wearable iot devices on early disease detection and prevention. International Journal of Applied Health Care Analytics 8(8), 1–15 (2023).
- Bayo-Monton, J.-L.; Martinez-Millana, A.; Han, W.; Fernandez-Llatas, C.; Sun, Y.; Traver, V. Wearable Sensors Integrated with Internet of Things for Advancing eHealth Care. Sensors 2018, 18, 1851. [Google Scholar] [CrossRef]
- Singh, A., Bianchi-Berthouze, N., Williams, A.C.: Supporting everyday func-tion in chronic pain using wearable technology. In: Proceedings of the 2017 CHI Conference on Human Factors in Computing Systems, pp. 3903–3915 (2017).
- DeVore, A.D.; Wosik, J.; Hernandez, A.F. The Future of Wearables in Heart Failure Patients. JACC: Hear. Fail. 2019, 7, 922–932. [Google Scholar] [CrossRef]
- Sana, F., Isselbacher, E.M., Singh, J.P., Heist, E.K., Pathik, B., Armoundas, A.A.: Wearable devices for ambulatory cardiac monitoring: Jacc state-of-the-art review. Journal of the American College of Cardiology 75(13), 1582–1592 (2020).
- Ali, U.: The impact of wearable devices on the management and treatment of chronic medical conditions. Archives of Clinical Psychiatry 49(2) (2022).
- Lu, L.; Zhang, J.; Xie, Y.; Gao, F.; Xu, S.; Wu, X.; Ye, Z. Wearable Health Devices in Health Care: Narrative Systematic Review. JMIR mHealth uHealth 2020, 8, e18907. [Google Scholar] [CrossRef]
- Porciuncula, F.; Roto, A.V.; Kumar, D.; Davis, I.; Roy, S.; Walsh, C.J.; Awad, L.N. Wearable Movement Sensors for Rehabilitation: A Focused Review of Technological and Clinical Advances. PM&R 2018, 10, S220–S232. [Google Scholar] [CrossRef]
- Brown, M.S., Ashley, B., Koh, A.: Wearable technology for chronic wound monitoring: current dressings, advancements, and future prospects. Frontiers in bioengineering and biotechnology 6, 47 (2018).
- Justin, G., Nyenhuis, S.M.: Wearable technology and how this can be imple-mented into clinical practice. Current Allergy and Asthma Reports 20(8) (2020).
- Jiang, W.; Majumder, S.; Kumar, S.; Subramaniam, S.; Li, X.; Khedri, R.; Mondal, T.; Abolghasemian, M.; Satia, I.; Deen, M.J. A Wearable Tele-Health System towards Monitoring COVID-19 and Chronic Diseases. IEEE Rev. Biomed. Eng. 2021, 15, 61–84. [Google Scholar] [CrossRef] [PubMed]
- Sharma, A., Badea, M., Tiwari, S., Marty, J.L.: Wearable biosensors: an alter-native and practical approach in healthcare and disease monitoring. Molecules 26(3), 748 (2021).
- Al-Khafajiy, M.; Baker, T.; Chalmers, C.; Asim, M.; Kolivand, H.; Fahim, M.; Waraich, A. Remote health monitoring of elderly through wearable sensors. Multimedia Tools Appl. 2019, 78, 24681–24706. [Google Scholar] [CrossRef]
- Majumder, S.; Mondal, T.; Deen, M.J. Wearable Sensors for Remote Health Monitoring. Sensors 2017, 17, 130. [Google Scholar] [CrossRef]
- Kalid, N.; Zaidan, A.A.; Zaidan, B.B.; Salman, O.H.; Hashim, M.; Muzammil, H. Based Real Time Remote Health Monitoring Systems: A Review on Patients Prioritization and Related "Big Data" Using Body Sensors information and Communication Technology. J. Med Syst. 2017, 42, 30–30. [Google Scholar] [CrossRef]
- Soon, S.; Svavarsdottir, H.; Downey, C.; Jayne, D.G. Wearable devices for remote vital signs monitoring in the outpatient setting: an overview of the field. BMJ Innov. 2020, 6, 55–71. [Google Scholar] [CrossRef]
- Kakria, P.; Tripathi, N.K.; Kitipawang, P. A Real-Time Health Monitoring System for Remote Cardiac Patients Using Smartphone and Wearable Sensors. Int. J. Telemed. Appl. 2015, 2015, 373474. [Google Scholar] [CrossRef]
- Malasinghe, L.P., Ramzan, N., Dahal, K.: Remote patient monitoring: a compre-hensive study. Journal of Ambient Intelligence and Humanized Computing 10, 57–76 (2019).
- Farias, F.A.C.d., Dagostini, C.M., Bicca, Y.d.A., Falavigna, V.F., Falavigna, A.: Remote patient monitoring: a systematic review. Telemedicine and e-Health 26(5), 576–583 (2020).
- Baig, M.M., GholamHosseini, H., Moqeem, A.A., Mirza, F., Lind´en, M.: A sys-tematic review of wearable patient monitoring systems–current challenges and opportunities for clinical adoption. Journal of medical systems 41, 1–9 (2017).
- AlShorman, O.; AlShorman, B.; Al-Khassaweneh, M.; Alkahtani, F. A review of internet of medical things (IoMT) - based remote health monitoring through wearable sensors: a case study for diabetic patients. Indones. J. Electr. Eng. Comput. Sci. 2020, 20, 414–422. [Google Scholar] [CrossRef]
- Ch, R.; Sudheer, P.; Kumar, P.D. ; Department of CSE (AI&ML) - CVR college of Engineering-Hyderabad-India-501512 An Overview of Remote Patient Monitoring For Improved Patient Care and Cost Reduction: The Iot Revolutionizing Health Care. Int. J. Educ. Manag. Eng. 2023, 13, 33–40. [Google Scholar] [CrossRef]
- Vegesna, A.; Tran, M.; Angelaccio, M.; Arcona, S. Remote Patient Monitoring via Non-Invasive Digital Technologies: A Systematic Review. Telemed. e-Health 2017, 23, 3–17. [Google Scholar] [CrossRef]
- Mamdiwar, S.D.; R, A.; Shakruwala, Z.; Chadha, U.; Srinivasan, K.; Chang, C.-Y. Recent Advances on IoT-Assisted Wearable Sensor Systems for Healthcare Monitoring. Biosensors 2021, 11, 372. [Google Scholar] [CrossRef]
- Olmedo-Aguirre, J.O.; Reyes-Campos, J.; Alor-Hernández, G.; Machorro-Cano, I.; Rodríguez-Mazahua, L.; Sánchez-Cervantes, J.L. Remote Healthcare for Elderly People Using Wearables: A Review. Biosensors 2022, 12, 73. [Google Scholar] [CrossRef]
- Anzanpour, A., Azimi, I., G¨otzinger, M., Rahmani, A.M., TaheriNejad, N., Lil-jeberg, P., Jantsch, A., Dutt, N.: Self-awareness in remote health monitoring systems using wearable electronics. In: Design, Automation & Test in Europe Conference & Exhibition (DATE), 2017, pp. 1056–1061 (2017). IEEE.
|
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2025 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (http://creativecommons.org/licenses/by/4.0/).