1. Introduction
Partial-thickness rotator cuff tears (PTRCTs) are commonly pointed as a major cause of prevalent shoulder pain in middle-aged and elderly individuals. PTRCTs also frequently results in functional impairment, considerably affecting patients’ quality of life [
1]. However, such clinical presentation of PTRCTs is difficult to differentiate from other sorts of shoulder disorders, due to the similarity of their symptoms overlap with those of other conditions (e. g., impingement syndrome and tendinopathy). Moreover, regarding imaging modalities including MRI and ultrasound, there can be various interpretation among the interobservers, which consequently leads to continual debate about optimal management strategies [
2,
3].
To be specific, PTRCTs are classified into articular-sided, bursal-sided, and interstitial tears based on their location. According to the Ellman classification, when tendon thickness is less than 3 mm, these are categorized as Grade I tears. Similarly, Grade II tears involve from 3 to 6 mm, and Grade III tears exceed 6 mm [
4,
5]. Although the best treatment of PTRCTs remains controversial, patients with tears ranging more than 50% of the tendon thickness are often recommended for undergo surgery intervention in clinical practice. Otherwise, their symptoms may progress to more severe level and higher risk of full-thickness tears [
6]. However, in patients with low-grade PTRCTs (<50% thickness involvement), and particulary those experiencing from constant pain despite prolonged nonoperative therapy, the optimal treatment strategy remains a significant debate [
7].
For PTRCTs, many surgical alternatives such as acromioplasty, debridement, in situ repair, and completion repair have been suggested [
8]. Traditional rotator cuff repair is conducted mainly by anchor-based fixation of the tendon to the humerus. But this can be accompanied by severe postoperative pain, prolonged immobilization, and increase the risk of stiffness and retear [
9,
10]. Bioinductive collagen implants are a new treatment option which has gained attention recently in response to the above. This fresh solution particularly promotes tendon regeneration while avoiding direct tendon-bone attachment. The bioinductive collagen implant (REGENETEN, Smith & Nephew, London, UK) has already demonstrated promising clinical outcomes by stimulating new tissue formation and improving tendon integrity [
11].
Through prior studies, the efficacy of bioinductive collagen implants has been evaluated in various ways so far, but the studies have generally not distinguished between articular- and bursal-sided PTRCTs [
12]. Considering that bioinductive implants are positioned on the bursal surface, this study was designed specifically to focus on the clinical outcomes of applying a bioinductive collagen implant to bursal-sided PTRCTs without concurrent rotator cuff repair. Ultimately, this study aimed to evaluate the functional and radiological outcomes of this surgical strategy and determine its potential benefits as a middle-ground treatment between nonoperative management and traditional rotator cuff repair.
2. Methods
2.1. Study Design and Ethical Approval
This study populations consisted of patients with bursal-side partial-thickness rotator cuff tears who failed conservative treatment for at least six months and subsequently received surgery using Bioinductive Collagen Implant excluding rotator cuff repair. The study was approved by the Institutional Review Board (IRB), and all participants provided written informed consent.
2.2. Patient Selection and Exclusion Criteria
Patients with bursal-sided partial-thickness rotator cuff tears of Ellman grade I or II confirmed via MRI, were considered eligible for this study. To ensure homogeneity of the study population, patients were excluded if they had articular-side tears, required rotator cuff repair, or presented with conditions such as frozen shoulder, SLAP lesions, osteoarthritis, calcific tendinitis, or distal clavicle osteolysis.
2.3. Surgical Technique
Each procedure was performed with the patient under regional block anesthesia and placed in the beach chair position, allowing optimal access to the shoulder joint. To facilitate evaluation and instrument, anterior and lateral working portals were established following the initial arthroscopic examination through a posterior viewing portal.
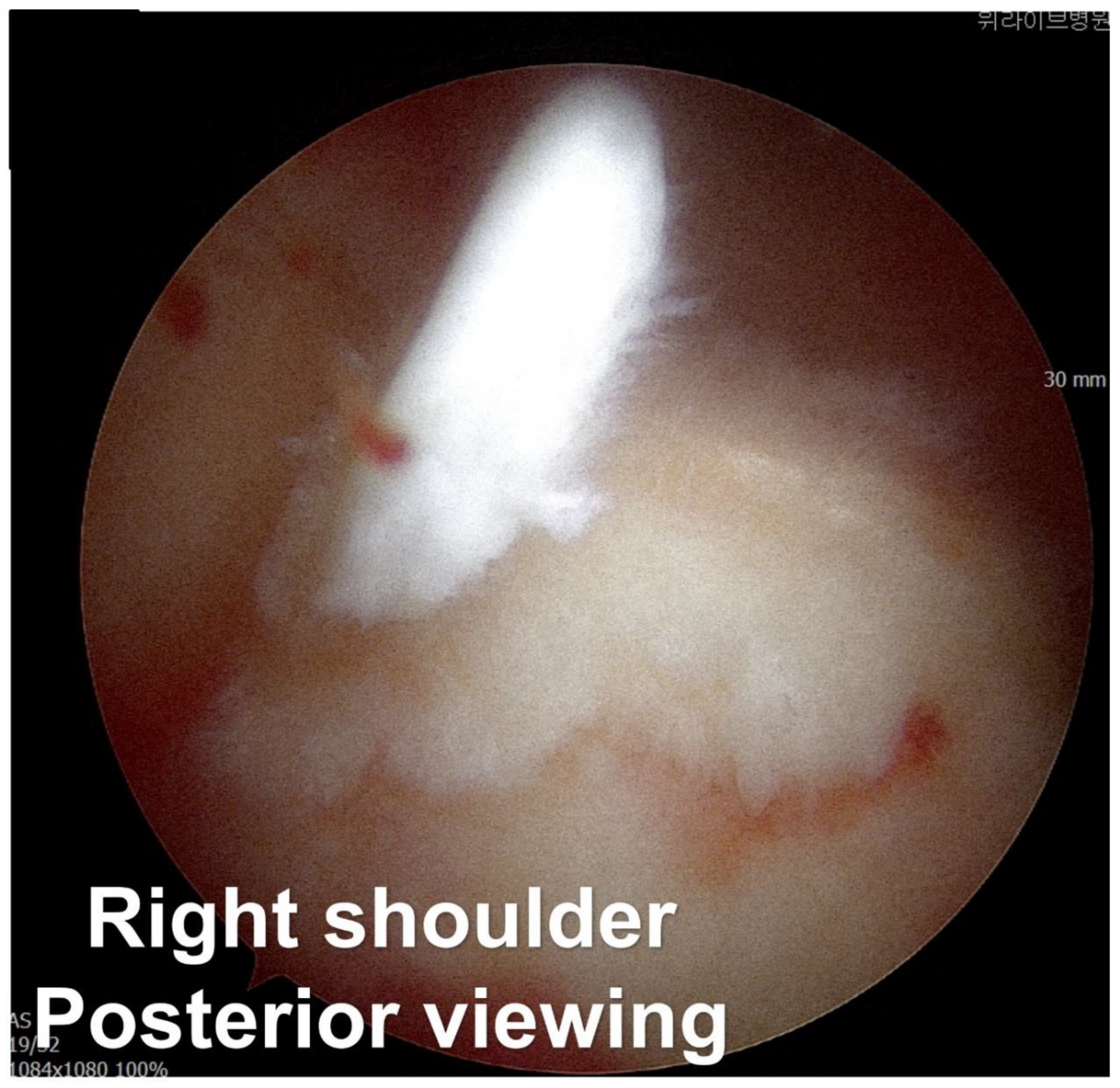
The surgeon identified a bursal-side partial-thickness rotator cuff tear and carefully examined the lesion to rule out full-thickness involvement (Fig. 1A). To preserve native rotator cuff, frayed tendon tissue was selectively removed using a shaver and radiofrequency alation device. Afterward, the coracoacromial ligament was released and acromioplasty was performed with a burr and high-speed shaver to address the acromial spur, which contributes to subacromial impingement and tendon degeneration [
13].
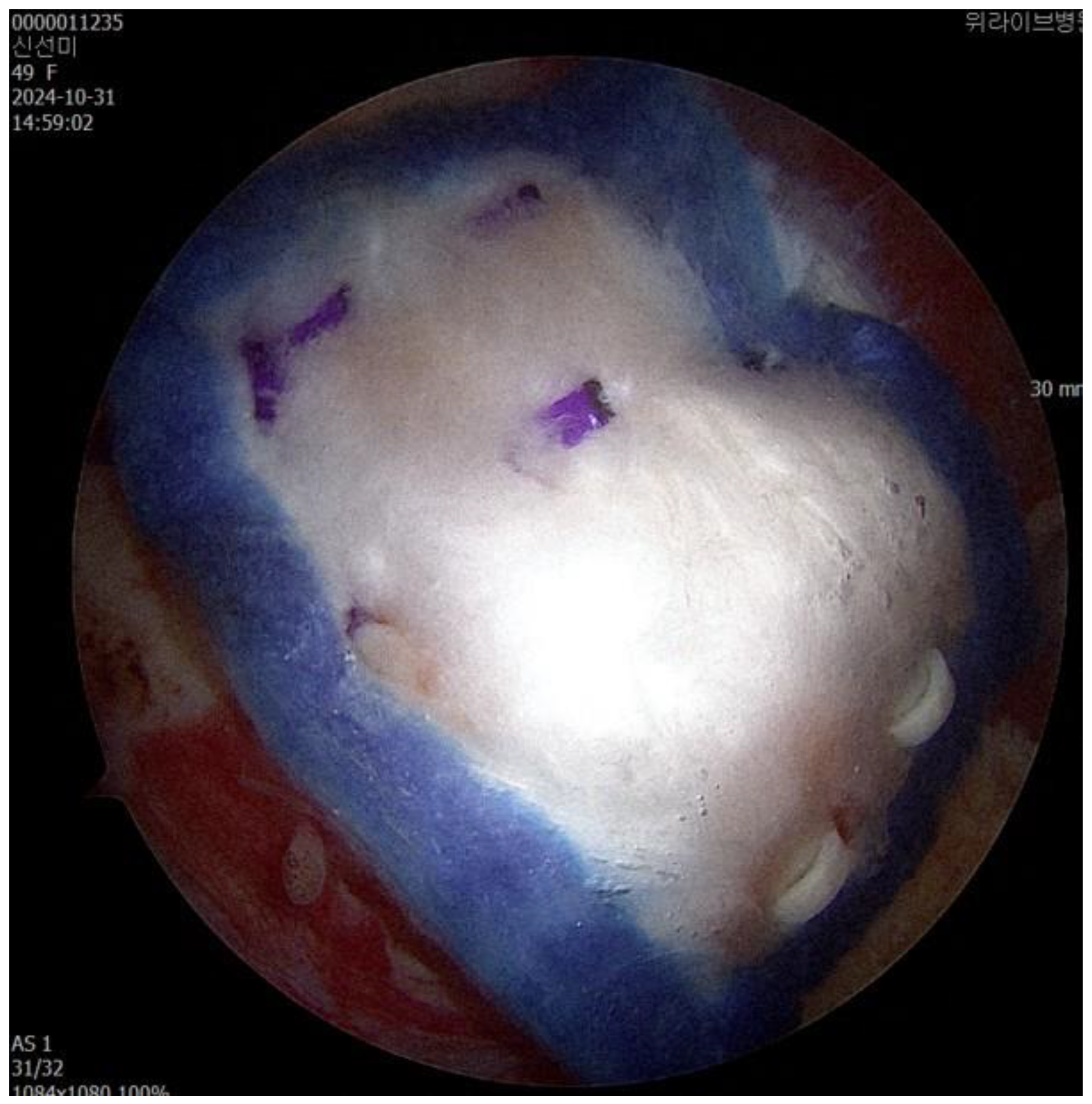
After establishing a superior anchor portal, a lateral working portal was created for insertion of the Bioinductive Collagen Implant (REGENETEN, Smith & Nephew, London, UK). Using the manufacturer-provided delivery system, the implant was deployed directly onto the degenerative rotator cuff tissue and secured in position. Final arthroscopic assessment confirmed stable positioning and adherence of the implant prior to closure (Fig 1B).
Figure 1.
(A) Bursal side partial thickness supraspinatus tear was observed. (B) The bioinductive collagen implant is fixed to cover the musculotendinous junction medially and the greater tuberosity laterally.
Figure 1.
(A) Bursal side partial thickness supraspinatus tear was observed. (B) The bioinductive collagen implant is fixed to cover the musculotendinous junction medially and the greater tuberosity laterally.
2.4. Postoperative Rehabilitation
For the first 48 hours after surgery, patients were instructed to use a shoulder sling to help protect the repair site and avoid putting stress on the implant. Once the shoulder had been immobilized for the initial period, the sling was taken off at intervals to gently begin moving the arm again, without interfering with the healing process. For the first two weeks, patients were allowed to do only passive range of motion (PROM) exercises, and movements like external rotation or lifting the arm overhead were strictly avoided.
From the second week after surgery, active-assisted range of motion (AAROM) exercises were introduced with supervision from a physical therapist, together with isometric excercises to help maintain muscle tone without overloading the healing tendon. In the weeks followed, active motion exercises were gradually included. By the sixth postoperative week, patients were guided to achieve full active motion, taking care not to overload the joint.
At about three months postoperatively, resistance training was stared using elastic bands and light weights to build strength in the shoulder. Depending on recovery progress, patients gradually resumed daily activities and sports over a period ranging from six to twelve months following surgery (Fig. 2).
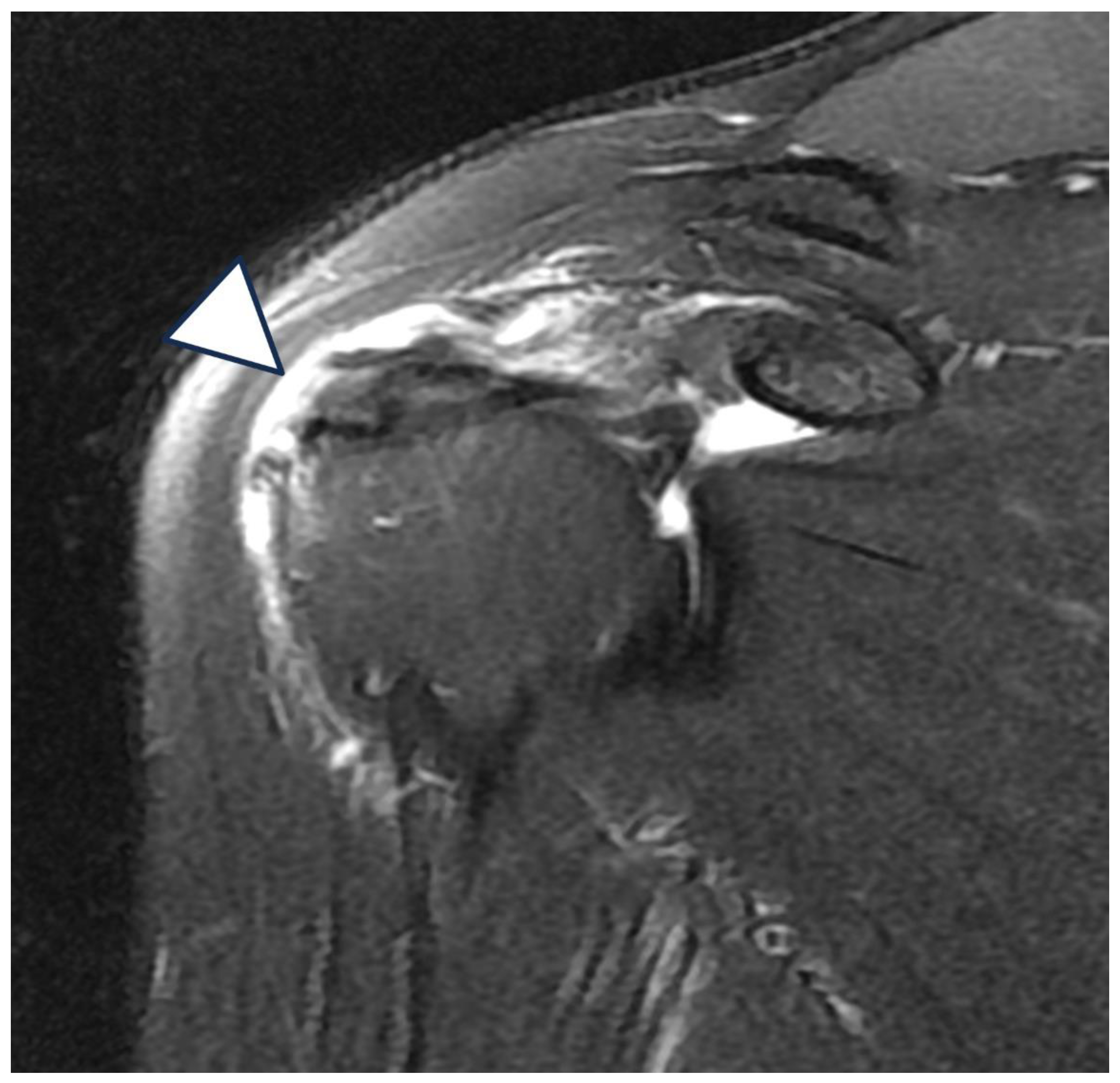
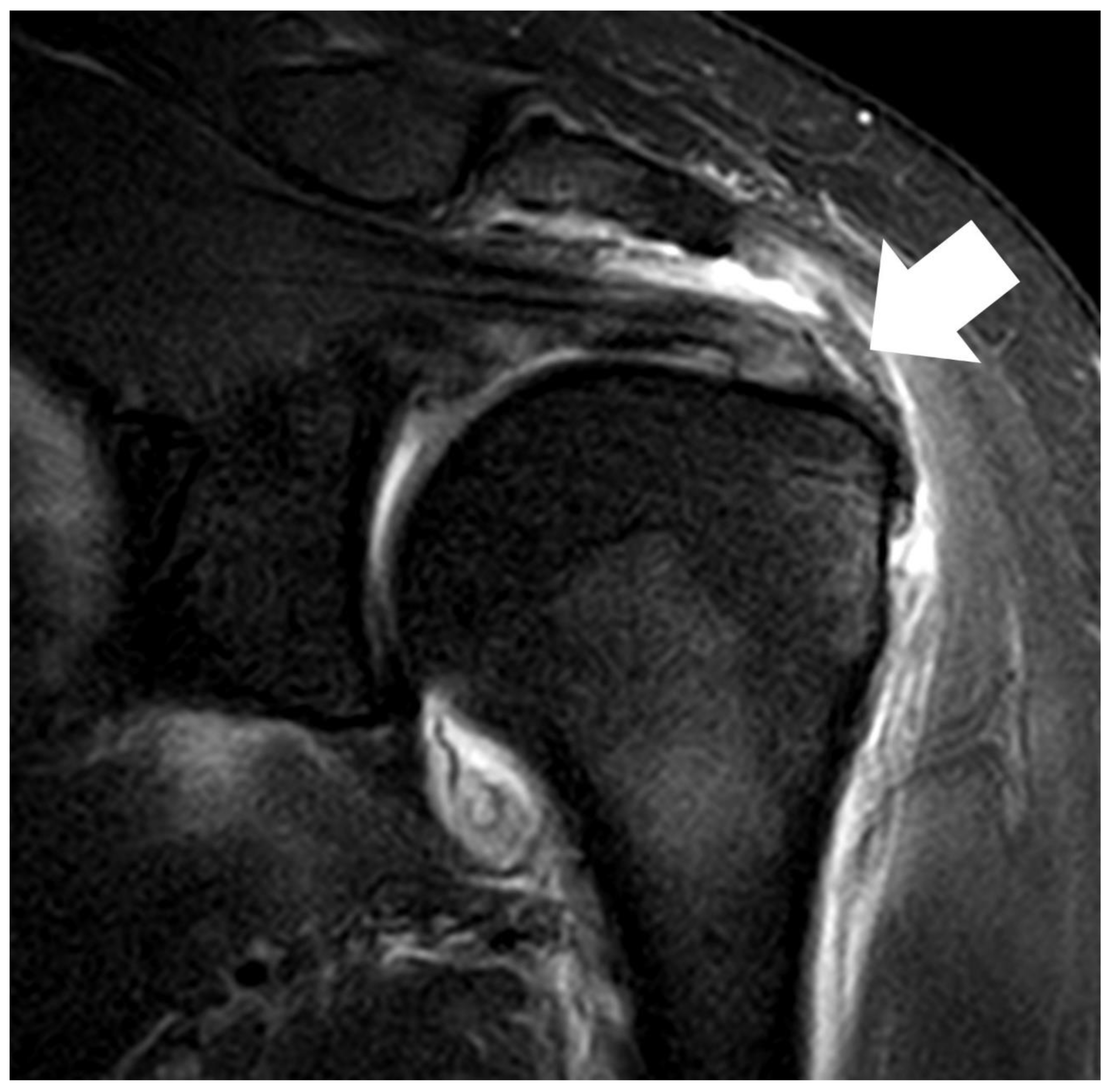
Figure 2.
(A) Bursal side partial thickness supraspinatus tear with subacromial spur was observed on the preoperative magnetic resonance imaging. (B) Bio-inductive collagen implant located on the tendon is observed in a post-operative magnetic resonance image. (C) A magnetic resonance image 6 months after surgery showed that the bio-inductive collagen implant was absorbed and the bursal side partial tear was fully recovered.
Figure 2.
(A) Bursal side partial thickness supraspinatus tear with subacromial spur was observed on the preoperative magnetic resonance imaging. (B) Bio-inductive collagen implant located on the tendon is observed in a post-operative magnetic resonance image. (C) A magnetic resonance image 6 months after surgery showed that the bio-inductive collagen implant was absorbed and the bursal side partial tear was fully recovered.
2.5. Clinical and Radiological Assessments
To track the clinical outcomes, functional assessments were performed before surgery and at 2 weeks, 6 weeks, 12 weeks, 24 weeks, and 52 weeks after surgery, using validated scoring tools for shoulder function. With regard to pain intensity, it was evaluated by the Visual Analog Scale (VAS). In addition, American Shoulder and Elbow Surgeons (ASES) score, the Single Assessment Numeric Evaluation (SANE), and the Western Ontario Rotator Cuff (WORC) index were used to measure patients’ shoulder performance and mobility.
At 6 months and 12 months after surgery, MRI and ultrasonography were used to examine bioinductive collagen implant integration and assess the condition of tendon tissue. MRI helped assess tendon integrity and healing, including continuity, signal changes, and possible problems such as delamination or re-tear. Ultrasonography was used to offer real-time imaging of the implant's condition.
2.6. Statistical Analysis
Based on prior studies, the sample size was calculated to ensure 80% power and an α level of 0.05 significance level, requiring at least 30 patients to detect a meaningful clinical difference.
Statistical analysis was carried out with SPSS Statistics version 21.0 (IBM Corp., Armonk, NY, USA) on a Windows platform. Continuous variables were examined using independent t-tests, and categorical variables were assessed with chi-square tests. A p-value below 0.05 was considered indicative of statistical significance.
3. Results
3.1. Patient Demographics and Baseline Characteristics
This study included 32 patients who underwent arthroscopic implantation of a bioinductive collagen patch (REGENETEN) for bursal-sided partial-thickness rotator cuff tears. The mean age of the enrolled patients was 53.2 years, with a standard deviation of 9.7 years. Among the 32 patients, 18 were female and 14 were male, showing a slight female predominance. Tears were more commonly observed in the dominant arm (19 patients, 59.4%) than in the non-dominant arm (13 patients, 40.6%). The patients had an average height of 169.4 ± 12.3 cm and and average weight of 68.6 ± 10.2 kg, corresponding to a mean body mass index (BMI) of 23.7 ± 4.1 kg/m².
As for health-related factors, 11 patients (34.4%) were smokers and 21 patients (65.6%) were non-smokers. Most belonged to ASA class 1 (29 patients, 90.6%), with 3 patients (9.4%) classified as ASA class 2. ASA class 3 was not observed in any case. Based on Ellman classification, 13 patients (40.6%) were classified as having grade I partial tears, and 19 patients (59.4%) as grade II. The mean follow-up period across all patients was 14.7 months (± 3.5) (Table I).
Table I.
Demographic data.
Table I.
Demographic data.
| Variable |
N=32 |
| Mean age |
53.2 ± 9.7 |
| Gender (Male: Female) |
14 : 18 |
| Dominant arm: Non-dominant arm |
19 : 13 |
| Height (cm) |
169.4 ± 12.3 |
| Weight (kg) |
68.6 ± 10.2 |
| Body mass index |
23.7 ± 4.1 |
| Smoking: Non-smoking |
11 : 21 |
| ASA class (1:2:3) |
29 : 3 : 0 |
| Ellman grade (1:2) |
13 : 19 |
| Mean follow-up (month) |
14.7 ± 3.5 |
3.2. Pain Improvement (VAS Score)
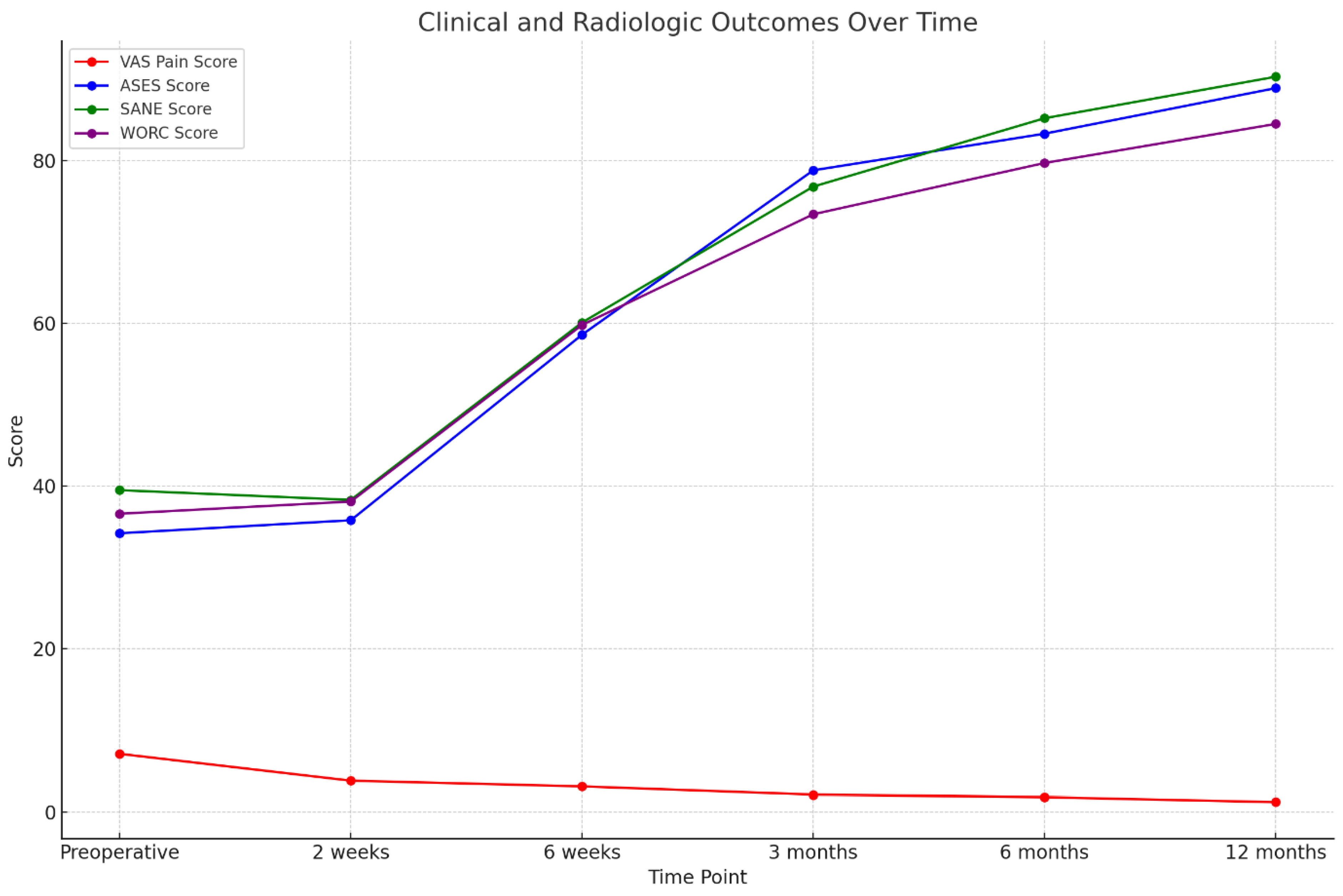
The Visual Analog Scale (VAS) pain scores significantly decreased after the surgical procedure, which can be interpreted as a positive impact on pain. Before surgery, the mean VAS score was 7.1 ± 4.4 and this shows that patients experienced considerable pain preoperatively. Just two weeks postoperatively, it dropped to 3.8 ± 2.9 (p < 0.001), showing a marked early improvement. Pain scores continued to decrease over time. At 6 weeks, the mean VAS score decreased to 3.1 ± 2.7, and by 3 months, it further declined to 2.1 ± 2.2 (p < 0.001 for both). At 6 months, the average score reached 1.8 ± 1.9, and by 12 months, most patients reported minimal residual pain, with a final VAS score of 1.2 ± 1.6 (p < 0.001 for all comparisons with baseline, Table II, Fig 3).
3.3. Functional Outcomes (ASES, SANE, and WORC Scores)
The American Shoulder and Elbow Surgeons (ASES) score improved significantly after surgery. Before surgery, the mean ASES score was 34.2 ± 17.5. No significant improvement was observed at 2 weeks (35.8 ± 18.2, p = 0.559). However, from 6 weeks onward, scores increased substantially: 58.6 ± 20.3 at 6 weeks, 78.8 ± 19.6 at 3 months, 83.3 ± 18.1 at 6 months, and 88.9 ± 17.5 at 12 months (all p < 0.001 compared to baseline).
The Single Assessment Numeric Evaluation (SANE) score, reflecting patients’ perception of shoulder function, also showed steady improvement throughout the follow-up period. The average preoperative SANE score was 39.5 ± 23.5. Although a slight decrease was recorded at 2 weeks (38.3 ± 20.8, p = 0.425), this difference did not reach stastical significance. From that point on, patients showed consistent improvement: 60.1 ± 23.2 at 6 weeks, 76.8 ± 19.8 at 3 months, 85.2 ± 21.5 at 6 months, and 90.3 ± 18.2 at 12 months (all p < 0.001).
The Western Ontario Rotator Cuff (WORC) index, which is used to assess quality of life in patients with rotator cuff disorders, showed a similar pattern to the result mentioned above. The average preoperative WORC score was 36.6 ± 23.4 and no statistically significant change was found at 2 weeks (38.1 ± 21.8, p = 0.174). However, significant improvement became evident from 6 weeks postoperatively (59.8 ± 22.4) and continued over time, with scores increasing to 73.4 ± 23.5 at 3 months, 79.7 ± 20.8 at 6 months, and 84.5 ± 22.7 at 12 months (all p < 0.001, Table II, Fig 3).
Table II.
Clinical and Radiologic outcomes.
Table II.
Clinical and Radiologic outcomes.
| Variable |
Preoperative |
2weeks |
6weeks |
3months |
6months |
12months |
| VAS pain score |
7.1±4.4 |
3.8±2.9 |
3.1±2.7 |
2.1±2.2 |
1.8±1.9 |
1.2±1.6 |
| |
|
<0.001 |
<0.001 |
<0.001 |
<0.001 |
<0.001 |
| ASES score |
34.2±17.5 |
35.8±18.2 |
58.6±20.3 |
78.8±19.6 |
83.3±18.1 |
88.9±17.5 |
| |
|
0.559 |
<0.001 |
<0.001 |
<0.001 |
<0.001 |
| SANE |
39.5±23.5 |
38.3±20.8 |
60.1±23.2 |
76.8±19.8 |
85.2±21.5 |
90.3±18.2 |
| |
|
0.425 |
<0.001 |
<0.001 |
<0.001 |
<0.001 |
| WORC |
36.6±23.4 |
38.1±21.8 |
59.8±22.4 |
73.4±23.5 |
79.7±20.8 |
84.5±22.7 |
| |
|
0.174 |
<0.001 |
<0.001 |
<0.001 |
<0.001 |
| Retear, % |
- |
0 (0%) |
0 (0%) |
0 (0%) |
0 (0%) |
0 (0%) |
Figure 3.
The clinical and radiologic outcomes following surgery over a 12-month period.
Figure 3.
The clinical and radiologic outcomes following surgery over a 12-month period.
3.4. Radiologic Outcomes and Graft Integrity
Radiologic assessments using MRI and ultrasonography revealed no evidence of graft failure or retear at any postoperative stage. Serial images demonstrated continuous tendon remodeling and integration of the Bioinductive Collagen Implant into the native rotator cuff tissue. At both 6 and 12 months postoperatively, all patients showed well-incorporated grafts with no signs of structural compromise.
4. Discussion
Partial-thickness rotator cuff tears (PTRCTs) are one of the most common shoulder pathologies, especially in middle-aged and older adults. These lesions can result in both functional limitations and diminished quality of life [
14]. Although many PTRCTs are asymptomatic, some patients continue to experience pain and functional impairments. In such cases, surgery may be required when conservative treatment fails [
15]. Among the traditional surgical options for treating PTRCTs - such as acromioplasty, debridement, in situ repair, and completion repair – many require tendon-bone reattachment using anchors, a technique that has been associated with prolonged immobilization, postoperative pain, and an increased incidence of stiffness [
16].
To address these limitations, bioinductive collagen implants such as REGENETEN have emerged as a promising alternative treatment that enables the tendon to heal without requiring direct suture repair or the use of anchors [
17]. Among these recent efforts, this study focused on evaluating the clinical outcomes of using a bioinductive collagen implant in patients with bursal-sided PTRCTs who were treated without tendon-to-bone fixation. The result demonstrated a significant reduction in postoperative pain, as evidenced by improved VAS scores observed at just two weeks postoperatively (p < 0.001). Moreover, functional outcomes, assessed by ASES, SANE, and WORC scores, showed significant improvement beginning at six weeks postoperatively (p < 0.001), with sustained improvement observed at later stages. These findings are consistent with earlier studies that have reported favorable clinical results using bioinductive collagen implants for rotator cuff pathology [
18].
Distinguishing between articular- and bursal-sided PTRCTs is essential, as they differ in both pain mechanism and healing potential—factors that directly influence treatment selection [
19]. Because bioinductive implants are placed on the bursal side—where they support collagen deposition and tendon regeneration—this study focused specifically on bursal-sided tears. As a result, we confirmed their effectiveness in promoting healing in these cases of PTRCTs and supported their use as a treatment option in appropriate situations [
20].
Since the subacromial bursa contains a higher density of sensory nerve endings, pain in bursal-sided PTRCTs follows a different mechanism than in that in articular-sided tears. According to previous research, neural structures in the bursal layer contribute to increased pain perception in these cases, so symptom relief is now considered a key treatment goal [
21]. In this study, the use of bioinductive collagen implants was found to aid in tendon healing and may help reduce pain, possibly because it lessens the mechanical contact between the acromion and the exposed tendon. The idea that bioinductive implants can influence tendon healing has also been supported by prior investigations, which observed changes in the local mechanics of the rotator cuff [
22].
A particular benefit observed with the use of bioinductive collagen implants is the way they may influence the course of postoperative rehabilitation, potentially allowing for a smoother and earlier return to activity. Patients treated with bioinductive collagen implants are able to begin rehabilitation earlier than those undergoing conventional repair. This may be because no tension is present at the site, unlike in suture-anchor constructs. As we observed in this study, early mobilization was well tolerated in all patients during the follow-up period. MRI and ultrasonography at 6 and 12 months showed no signs of implant failure or graft-related complications. Bioinductive collagen implants have been reported in previous studies to encourage tendon remodeling and integration. Unlike anchor-based techniques, no suture-related complications were observed [
23].
While the results are encouraging, several limitations should be considered. This was a retrospective study, which introduces the possibility of selection bias. In addition, potential confounding factors may have influenced the outcomes, as full control over such variables was not feasible in this study design. Another limitation lies in the small sample size, which may restrict broader interpretation of the results. Still, the power analysis suggests that the sample was sufficient to identify clinically relevant changes. A further concern relates to the follow-up period (12 months), which may not have been sufficient to assess long-term outcomes, such as the durability of the bioinductive implant or the possibility of delayed failure. Thus, longer-term follow-up and randomized controlled trials will be important to confirm the sustainability of these outcomes and to refine patient selection and surgical strategies.
Taken together, the findings of this study suggest that bioinductive collagen implants may provide effective pain relief and functional recovery in bursal-sided PTRCTs, while also supporting tendon healing and allowing for early rehabilitation. Bursal-sided tears may involve a distinct biological mechanism, which could influence healing potential. Further research will be necessary to clarify the long-term effectiveness of bioinductive implants and define their role in clinical practice.
5. Conclusion
Through this study, we looked at the actual clinical outcomes in patients with bursal-sided partial-thickness rotator cuff tears treated using a bioinductive collagen implant (REGENETEN) without formal rotator cuff repair. Following the results, early pain relief, improved shoulder function, and signs of tendon healing were observed in patients treated without anchor-based repair using this approach. After we performed surgery using a bioinductive collagen implant, pain scores went down (VAS, p < 0.001) and shoulder function got better across several measures (ASES, SANE, WORC, all p < 0.001). On MRI or ultrasound, no cases of graft failure were found.
While most prior research didn’t separate articular- from bursal-sided PTRCTs, here we looked only at the bursal ones based on the idea that the pain mechanism — including their anatomical and biomechanical characteristics — work differently in each type. We also believe that the decision to perform surgery should be made not only based on imaging findings but also, and more importantly, on each patient’s persistent symptoms that don’t improve with conservative care. Because distinguishing PTRCTs from early frozen shoulder remains difficult, and asymptomatic partial-thickness tears are still commonly seen in older patients in daily clinical practice.
References
- Lo, I.K.; Denkers, M.R.; More, K.D.; Nelson, A.A.; Thornton, G.M.; Boorman, R.S. Partial-thickness rotator cuff tears: Clinical and imaging outcomes and prognostic factors of successful nonoperative treatment. Open Access J. Sports Med. 2018, 9, 191–197.. [CrossRef]
- Kim, Y.K.; Jung, K.H.; Kang, S.W.; Hong, J.H.; Choi, K.Y.; Choi, J.U. Relationship of the shape of subacromial spur and rotator cuff partial thickness tear. Clin. Shoulder Elb. 2019, 22(3), 139–145. [CrossRef]
- Mihata, T.; Morikura, R.; Hasegawa, A.; Fukunishi, K.; Kawakami, T.; Fujisawa, Y.; et al. Partial-thickness rotator cuff tear by itself does not cause shoulder pain or muscle weakness in baseball players. Am. J. Sports Med. 2019, 47(14), 3476–3482. [CrossRef]
- Seo, J.; Heo, K.; Kwon, S.; Yoo, J. Critical shoulder angle and greater tuberosity angle according to the partial thickness rotator cuff tear patterns. Orthop. Traumatol. Surg. Res. 2019, 105(8), 1543–1548. [CrossRef]
- Wang, T.; Ren, Z.; Zhang, Y.; Zhao, X.; Liu, X.; Yu, T.; et al. Comparison of arthroscopic debridement and repair in the treatment of Ellman grade II bursal-side partial-thickness rotator cuff tears: A prospective randomized controlled trial. Orthop. Surg. 2021, 13(7), 2070–2080. [CrossRef]
- Zhang, Y.; Zhai, S.; Qi, C.; Chen, J.; Li, H.; Zhao, X.; et al. A comparative study of arthroscopic debridement versus repair for Ellman grade II bursal-side partial-thickness rotator cuff tears. J. Shoulder Elbow Surg. 2020, 29(10), 2072–2079. [CrossRef]
- Aydin, N.; Karaismailoglu, B. High-grade bursal-side partial rotator cuff tears: Comparison of mid- and long-term results following arthroscopic repair after conversion to a full-thickness tear. J. Orthop. Surg. Res. 2017, 12(1), 118. [CrossRef]
- Matthewson, G.; Beach, C.J.; Nelson, A.A.; Woodmass, J.M.; Ono, Y.; Boorman, R.S.; et al. Partial-thickness rotator cuff tears: Current concepts. Adv. Orthop. 2015, 2015, 458786. [CrossRef]
- Thangarajah, T.; Ling, F.K.; Lo, I.K. Isolated bioinductive arthroscopic repair of partial-thickness rotator cuff tears using a resorbable collagen implant. JBJS Essent. Surg. Tech. 2022, 12(1), e21.00073. [CrossRef]
- Fukuda, H. The management of partial-thickness tears of the rotator cuff. J. Bone Joint Surg. Br. 2003, 85(1), 3–11. [CrossRef]
- Sher, J.S.; Uribe, J.W.; Posada, A.; Murphy, B.J.; Zlatkin, M.B. Abnormal findings on magnetic resonance images of asymptomatic shoulders. J. Bone Joint Surg. Am. 1995, 77(1), 10–15. [CrossRef]
- Milgrom, C.; Schaffler, M.; Gilbert, S.; van Holsbeeck, M. Rotator-cuff changes in asymptomatic adults: The effect of age, hand dominance, and gender. J. Bone Joint Surg. Br. 1995, 77(2), 296–298.
- Yamanaka, K.; Matsumoto, T. The joint side tear of the rotator cuff: A follow-up study by arthrography. Clin. Orthop. Relat. Res. 1994, 304, 68–73.
- Mall, N.A.; Kim, H.M.; Keener, J.D.; Steger-May, K.; Teefey, S.A.; Middleton, W.D.; et al. Symptomatic progression of asymptomatic rotator cuff tears: A prospective study of clinical and sonographic variables. J. Bone Joint Surg. Am. 2010, 92(16), 2623–2633.
- Bushnell, B.D.; Connor, P.M.; Harris, H.W.; Ho, C.P.; Trenhaile, S.W.; Abrams, J.S. Two-year outcomes with a bioinductive collagen implant used in augmentation of arthroscopic repair of full-thickness rotator cuff tears: Final results of a prospective multicenter study. J. Shoulder Elbow Surg. 2022, 31(12), 2532–2541. [CrossRef]
- Hamada, K.; Tomonaga, A.; Gotoh, M.; Yamakawa, H.; Fukuda, H. Intrinsic healing capacity and tearing process of torn supraspinatus tendons: In situ hybridization study of alpha 1(I) procollagen mRNA. J. Orthop. Res. 1997, 15(1), 24–32. [CrossRef]
- Seo, J.B.; Kwak, K.Y.; Park, B.; Yoo, J.S. Anterior cable reconstruction using the proximal biceps tendon for reinforcement of arthroscopic rotator cuff repair to prevent retear and increase acromiohumeral distance. J. Orthop. 2021, 23, 246–249. [CrossRef]
- McIntyre, L.F.; Bishop, J.Y.; Jones, G.L.; McGarry, M.H.; Gupta, R.; Lee, T.Q. The biomechanical effect of a bioinductive collagen implant on rotator cuff healing. Orthop. J. Sports Med. 2021, 9(4), 23259671211004756.
- Kim, D.H.; Lee, H.J.; Kim, Y.J.; Jeong, W.K. Sensory innervation of the subacromial bursa and its potential role in shoulder pain: An anatomical study. J. Orthop. Res. 2023, 41(3), 741–748.
- Meislin, R.; Strauss, E.J.; Boorman, R.S.; Lo, I.K. Pain mechanisms in bursal-sided partial-thickness rotator cuff tears. Bull. Hosp. Jt. Dis. 2020, 78(1), 25–31.
- Ruiz Ibán, M.Á.; Lorenzini, M.; Lädermann, A.; Sánchez-Sotelo, J. Treatment strategies for partial-thickness rotator cuff tears. Knee Surg. Sports Traumatol. Arthrosc. 2024, 32(2), 145–157.
- McGarry, M.H.; McIntyre, L.F.; Bishop, J.Y.; Jones, G.L.; Gupta, R.; Lee, T.Q. The impact of bioinductive collagen implants on rotator cuff tendon healing: A biomechanical study. Orthop. J. Sports Med. 2021, 9(4), 23259671211004756.
- Thangarajah, T.; Ling, F.K.; Lo, I.K. Evaluation of bioinductive collagen implants for rotator cuff repair: Mechanisms and clinical outcomes. J. Shoulder Elbow Surg. 2020, 29(7), 1509–1516.
|
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2025 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).