Submitted:
03 April 2025
Posted:
07 April 2025
You are already at the latest version
Abstract
Keywords:
- a)
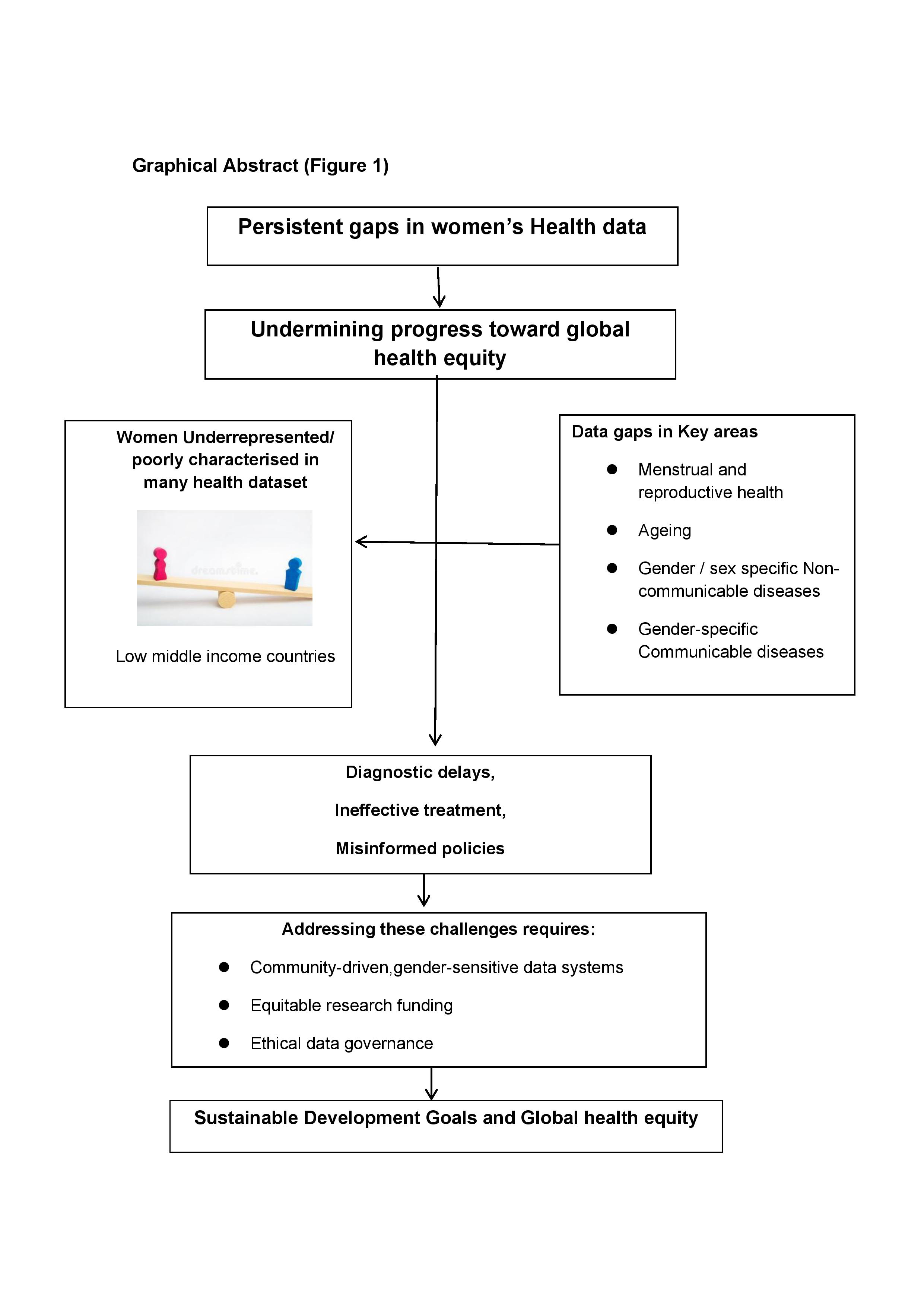
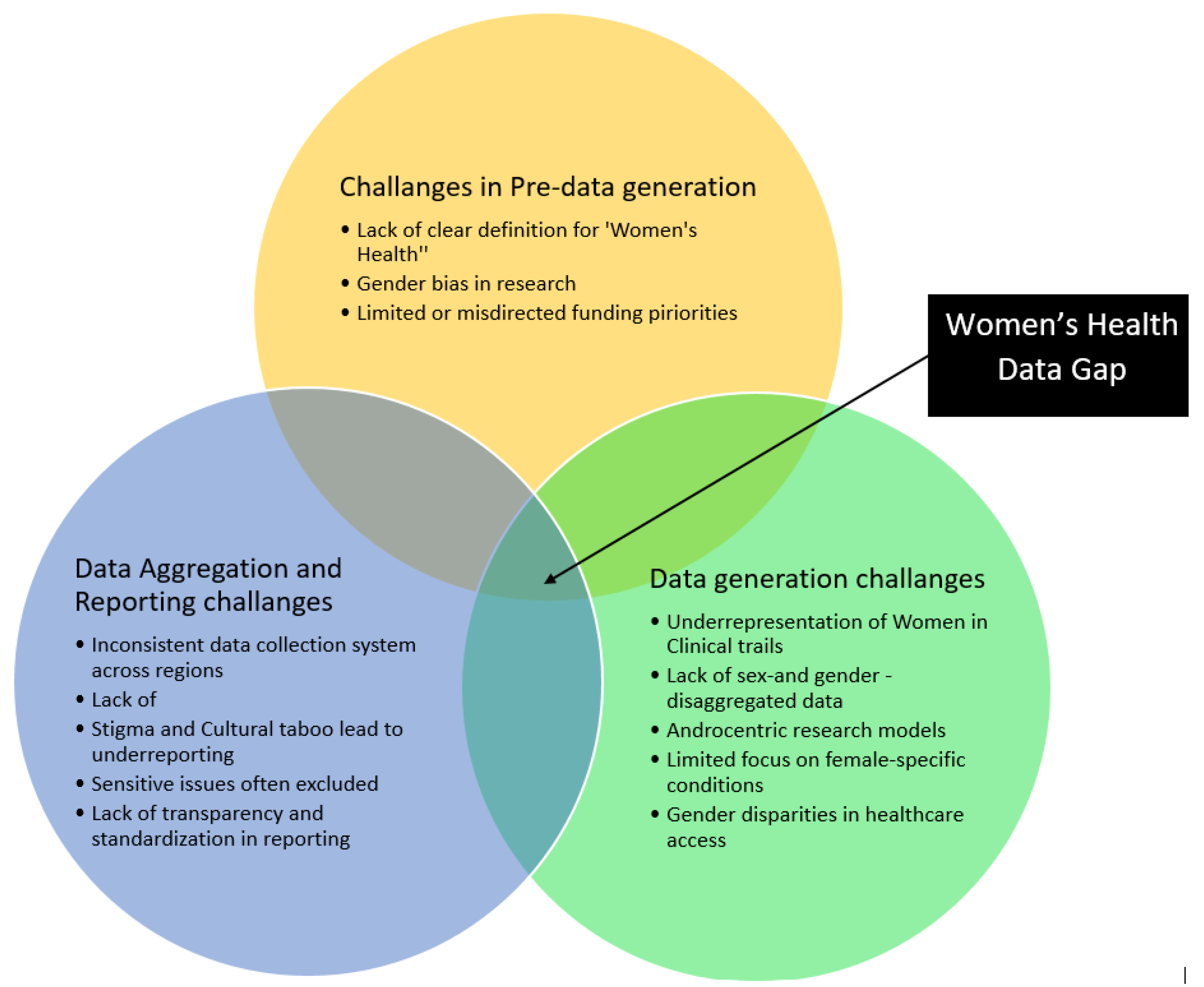
- Lack of Definition for Women’s Health: There is no universally accepted definition of women’s health, and most national systems focus only on reproductive health. This excludes LGBTQI+ individuals and overlooks diverse needs such as higher rates of mental health conditions and substance use [35,36].
- b)
- Gender Bias in Research Studies: The 1977 FDA ban on women in early-phase trials due to pregnancy risks led to long-term exclusion. As a result, many drugs were approved based solely on male physiology [37,38].Women experience more adverse drug reactions, often due to overmedication stemming from male-centric dosing protocols.
- c)
- Lack of Funding: Diseases that predominantly affect women receive less funding. A 2021 NIH study showed that male-dominated diseases are significantly overfunded, while female-dominated diseases are underfunded [30].
- a)
- b)
- a)
- Stigma and Cultural Barriers: Topics such as reproductive health, STIs, and mental health are taboo in many cultures. This leads to underreporting and inaccurate prevalence data. For example, WHO estimates the prevalence of endometriosis to be 6–13%, while global disease burden data suggests only 1–2% [42,43].
- b)
- c)
- Mandating Gender-Disaggregated Data Collection: Governments and health institutions must ensure collection across trials, research, and healthcare monitoring [78].
- Expanding Women’s Health Research Funding: Increase investment in non-reproductive health conditions [36].
- Regulating AI and Digital Health Bias: Enact ethical standards to prevent gender-biased machine learning tools [79].
- Strengthening Health Data in LMICs: Focus on context-specific, equitable, evidence-based interventions [17].
Author Contributions
Funding
Ethics Approval
Consent to Participate
Consent for Publication
Availability of Data and Material
Code Availability
Acknowledgments
Conflicts of Interest
References
- Women’s health research lacks funding – these charts show how [Internet]. [cited 2025 Apr 1]. Available from: https://www.nature.com/immersive/d41586-023-01475-2/index.html.
- FastStats [Internet]. 2024 [cited 2025 Apr 1]. Available from: https://www.cdc.gov/nchs/fastats/womens-health.htm.
- Gregory A, editor AGH. Women’s health being neglected worldwide, says Melinda French Gates. The Guardian [Internet]. 2024 Oct 9 [cited 2025 Apr 1]; Available from: https://www.theguardian.com/society/2024/oct/09/women-health-neglected-worldwide-melinda-french-gates.
- Women’s health [Internet]. [cited 2025 Apr 1]. Available from: https://www.who.int/health-topics/women-s-health.
- Langer, A.; Meleis, A.; Knaul, F.M.; Atun, R.; Aran, M.; Arreola-Ornelas, H. , et al. Women and Health: the key for sustainable development. The Lancet 2015, 386, 1165–210. [Google Scholar] [CrossRef] [PubMed]
- Tarpley, M. Invisible Women: Exposing Data Bias in a World Designed for Men: A Book for All. By Caroline Criado Perez. New York: Abrams Press, 2019. ISBN: 978-1-4197-2907-2 (hardcover). S Afr Med J. 2020, 110, 831. [Google Scholar] [CrossRef]
- World Health Organization. Closing data gaps in gender [Internet]. World Health Organization. 2021 [cited 2025 Mar 4]. Available from: https://www.who.int/activities/closing-data-gaps-in-gender.
- Differences I of M (US) C on U the B of S and G, Wizemann TM, Pardue ML. Every Cell Has a Sex. In: Exploring the Biological Contributions to Human Health: Does Sex Matter? [Internet]. National Academies Press (US); 2001 [cited 2025 Mar 28]. Available from: https://www.ncbi.nlm.nih.gov/books/NBK222291/.
- Plevkova, J.; Brozmanova, M.; Harsanyiova, J.; Sterusky, M.; Honetschlager, J.; Buday, T. Various Aspects of Sex and Gender Bias in Biomedical Research. Physiol Res. 2021, S367–78. [Google Scholar] [CrossRef]
- Holdcroft, A. Gender bias in research: how does it affect evidence based medicine? J R Soc Med. 2007, 100, 2–3. [Google Scholar] [CrossRef]
- Steering Committee of the Physicians’ Health Study Research Group*. Final Report on the Aspirin Component of the Ongoing Physicians’ Health Study. N Engl J Med. 1989, 321, 129–35. [CrossRef]
- Hanna, G.; Andrew, O. Gender differences in cardiovascular disease: Women are less likely to be prescribed certain heart medications - Harvard Health [Internet]. Harvard Health Publishing, Harvard Medical School. 2020 [cited 2025 Mar 28]. Available from: https://www.health.harvard.edu/blog/gender-differences-in-cardiovascular-disease-women-are-less-likely-to-be-prescribed-certain-heart-medications-2020071620553.
- Woodward, M. Cardiovascular Disease and the Female Disadvantage. IJERPH. 2019, 16, 1165. [Google Scholar] [CrossRef]
- Mehta, L.S.; Beckie, T.M.; DeVon, H.A.; Grines, C.L.; Krumholz, H.M.; Johnson, M.N. , et al. Acute Myocardial Infarction in Women: A Scientific Statement From the American Heart Association. Circulation 2016, 133, 916–47. [Google Scholar] [CrossRef]
- Results of the ‘Women’s Health – Let’s talk about it’ survey [Internet]. GOV.UK. [cited 2025 Apr 1]. Available from: https://www.gov.uk/government/calls-for-evidence/womens-health-strategy-call-for-evidence/outcome/3fa4a313-f7a5-429a-b68d-0eb0be15e696.
- Woods, W.A.; Watson, M.; Ranaweera, S.; Tajuria, G.; Sumathipala, A. Under-representation of low and middle income countries (LMIC) in the research literature: Ethical issues arising from a survey of five leading medical journals: have the trends changed? Global Public Health. 2023, 18, 2229890. [Google Scholar] [CrossRef]
- Jylhä, V.; Oikarainen, A.; Perälä, M.L.; Holopainen, A. Facilitating evidence-based practice in nursing and midwifery in the WHO European Region.
- Say, L.; Chou, D.; Gemmill, A.; Tunçalp, Ö.; Moller, A.B.; Daniels, J. , et al. Global causes of maternal death: a WHO systematic analysis. The Lancet Global Health. 2014, 2, e323–33. [Google Scholar] [CrossRef]
- Musarandega, R.; Nyakura, M.; Machekano, R.; Pattinson, R.; Munjanja, S.P. Causes of maternal mortality in Sub-Saharan Africa: A systematic review of studies published from 2015 to 2020. J Glob Health. 2021, 11, 04048. [Google Scholar] [CrossRef]
- Al Hamid, A.; Beckett, R.; Wilson, M.; Jalal, Z.; Cheema, E.; Al-Jumeily Obe, D. , et al. Gender Bias in Diagnosis, Prevention, and Treatment of Cardiovascular Diseases: A Systematic Review. Cureus. 2024, 16, e54264. [Google Scholar] [PubMed]
- Blanchard, D.C.; Griebel, G.; Blanchard, R.J. Gender bias in the preclinical psychopharmacology of anxiety: male models for (predominantly) female disorders. J Psychopharmacol. 1995, 9, 79–82. [Google Scholar] [CrossRef] [PubMed]
- Lee, E.; Wen, P. Gender and sex disparity in cancer trials. ESMO Open 2020, 5, e000773. [Google Scholar] [CrossRef] [PubMed]
- Carey, J.L.; Nader, N.; Chai, P.R.; Carreiro, S.; Griswold, M.K.; Boyle, K.L. Drugs and Medical Devices: Adverse Events and the Impact on Women’s Health. Clinical Therapeutics. 2017, 39, 10–22. [Google Scholar] [CrossRef]
- Eaton, N.R.; Keyes, K.M.; Krueger, R.F.; Balsis, S.; Skodol, A.E.; Markon, K.E. , et al. An invariant dimensional liability model of gender differences in mental disorder prevalence: Evidence from a national sample. Journal of Abnormal Psychology. 2012, 121, 282–8. [Google Scholar] [CrossRef]
- Castro-Aldrete, L.; Moser, M.V.; Putignano, G.; Ferretti, M.T.; Schumacher Dimech, A.; Santuccione Chadha, A. Sex and gender considerations in Alzheimer’s disease: The Women’s Brain Project contribution. Front Aging Neurosci. 2023, 15, 1105620. [Google Scholar] [CrossRef]
- Carter, C.L.; Resnick, E.M.; Mallampalli, M.; Kalbarczyk, A. Sex and Gender Differences in Alzheimer’s Disease: Recommendations for Future Research. Journal of Women’s Health. 2012, 21, 1018–23. [Google Scholar] [CrossRef]
- Angum, F.; Khan, T.; Kaler, J.; Siddiqui, L.; Hussain, A. The Prevalence of Autoimmune Disorders in Women: A Narrative Review. Cureus. 2020, 12, e8094. [Google Scholar] [CrossRef]
- Ross, L.; Ng, H.S.; O’Mahony, J.; Amato, M.P.; Cohen, J.A.; Harnegie, M.P. , et al. Women’s Health in Multiple Sclerosis: A Scoping Review. Front Neurol. 2022, 12, 812147. [Google Scholar] [CrossRef]
- Gerosa, M.; De Angelis, V.; Riboldi, P.; Meroni, P. Rheumatoid Arthritis: A Female Challenge. Womens Health (Lond Engl). 2008, 4, 195–201. [Google Scholar] [CrossRef]
- Mirin, A.A. Gender Disparity in the Funding of Diseases by the U. S. National Institutes of Health. Journal of Women’s Health. 2021, 30, 956–63. [Google Scholar] [CrossRef] [PubMed]
- Steinþórsdóttir, F.S.; Einarsdóttir, Þ.; Pétursdóttir, G.M.; Himmelweit, S. Gendered inequalities in competitive grant funding: an overlooked dimension of gendered power relations in academia. Higher Education Research & Development. 2020, 39, 362–75. [Google Scholar]
- Howard, L.M.; Ehrlich, A.M.; Gamlen, F.; Oram, S. Gender-neutral mental health research is sex and gender biased. The Lancet Psychiatry. 2017, 4, 9–11. [Google Scholar] [CrossRef]
- Delanerolle, G.; Phiri, P.; Elneil, S.; Talaulikar, V.; Eleje, G.U.; Kareem, R. , et al. Menopause: a global health and wellbeing issue that needs urgent attention. The Lancet Global Health. 2025, 13, e196–8. [Google Scholar] [CrossRef]
- Sarrel, P.; Portman, D.; Lefebvre, P.; Lafeuille, M.H.; Grittner, A.M.; Fortier, J. , et al. Incremental direct and indirect costs of untreated vasomotor symptoms. Menopause. 2015, 22, 260–6. [Google Scholar] [CrossRef]
- Closing the women’s health gap | McKinsey [Internet]. [cited 2025 Mar 31]. Available from: https://www.mckinsey.com/mhi/our-insights/closing-the-womens-health-gap-a-1-trillion-dollar-opportunity-to-improve-lives-and-economies.
- Snair, M.R. Overview of research gaps for selected conditions in women’s health research at the National Institutes of Health: proceedings of a workshop--in brief. Washington, DC: National Academies Press; 2024. 1 p. (Proceedings of a workshop--in brief).
- Merkatz, R.B. Inclusion of Women in Clinical Trials: A Historical Overview of Scientific Ethical and Legal Issues. Journal of Obstetric, Gynecologic & Neonatal Nursing. 1998, 27, 78–84. [Google Scholar]
- Zucker, I.; Prendergast, B.J. Sex differences in pharmacokinetics predict adverse drug reactions in women. Biol Sex Differ. 2020, 11, 32. [Google Scholar] [CrossRef]
- Waltz, M.; Lyerly, A.D.; Fisher, J.A. Exclusion of Women from Phase I Trials: Perspectives from Investigators and Research Oversight Officials. Ethics & Human Research. 2023, 45, 19–30. [Google Scholar]
- Salter-Volz, A.E.; Oyasu, A.; Yeh, C.; Muhammad, L.N.; Woitowich, N.C. Sex and Gender Bias in Covid-19 Clinical Case Reports. Front Glob Womens Health 2021, 2, 774033. [Google Scholar] [CrossRef]
- COVID-19 - PAHO/WHO Response, Report 72 (11 March 2022) - PAHO/WHO | Pan American Health Organization [Internet]. [cited 2025 Mar 31]. Available from: https://www.paho.org/en/documents/covid-19-pahowho-response-report-72-11-march-2022.
- Sexual and reproductive health for all: 20 years of the Global Strategy [Internet]. [cited 2025 Mar 31]. Available from: https://www.who.int/news/item/16-05-2024-sexual-and-reproductive-health-for-all-20-years-of-the-global-strategy.
- Rahmioglu, N.; Zondervan, K. Endometriosis: disease mechanisms and health disparities. Bull World Health Organ. 2024, 102, 919–21. [Google Scholar] [CrossRef]
- Shellenberg, K.M.; Moore, A.M.; Bankole, A.; Juarez, F.; Omideyi, A.K.; Palomino, N. , et al. Social stigma and disclosure about induced abortion: Results from an exploratory study. Global Public Health 2011, 6 (sup1), S111–25. [Google Scholar] [CrossRef] [PubMed]
- Norris, A.; Bessett, D.; Steinberg, J.R.; Kavanaugh, M.L.; De Zordo, S.; Becker, D. Abortion Stigma: A Reconceptualization of Constituents, Causes, and Consequences. Women’s Health Issues. 2011, 21, S49–54. [Google Scholar] [CrossRef] [PubMed]
- Harari, L.; Lee, C. Intersectionality in quantitative health disparities research: A systematic review of challenges and limitations in empirical studies. Soc Sci Med. 2021, 277, 113876. [Google Scholar] [CrossRef] [PubMed]
- Ezeamii, V.C.; Okobi, O.E.; Wambai-Sani, H.; Perera, G.S.; Zaynieva, S.; Okonkwo, C.C. , et al. Revolutionizing Healthcare: How Telemedicine Is Improving Patient Outcomes and Expanding Access to Care. Cureus. 2024, 16, e63881. [Google Scholar]
- Babatunde, A.O.; Abdulazeez, A.O.; Adeyemo, E.A.; Uche-Orji, C.I.; Saliyu, A.A. Telemedicine in Low and Middle Income Countries: Closing or Widening the Health Inequalities Gap? EUROPEAN J ENV PUBLI. 2021, 5, em0075. [Google Scholar] [CrossRef]
- Onsongo, S.; Kagotho, E. Telemedicine in Africa: Applications, Opportunities, and Challenges. In: R. Doarn C, F. Heston T, editors. Biomedical Engineering [Internet]. IntechOpen; 2024 [cited 2025 Mar 31]. Available from: https://www.intechopen.com/chapters/1176535.
- Empowered or Undermined? Women Entrepreneurs & the Digital Economy [Internet]. Cherie Blair Foundation for Women. [cited 2025 Mar 31]. Available from: https://cherieblairfoundation.org/what-we-do/research/2024-audit/.
- Van Kessel, R.; Wong, B.L.H.; Clemens, T.; Brand, H. Digital health literacy as a super determinant of health: More than simply the sum of its parts. Internet Interventions 2022, 27, 100500. [Google Scholar] [CrossRef]
- Chuma, K.; Sibiya, P. Digital Health Ecosystem Framework to Address Fragmentation of the Health System in South Africa. AJNM [Internet]. 2022 Nov 10 [cited 2025 Mar 31]; Available from: https://unisapressjournals.co.za/index.php/AJNM/article/view/11547.
- Zharima, C.; Griffiths, F.; Goudge, J. Exploring the barriers and facilitators to implementing electronic health records in a middle-income country: a qualitative study from South Africa. Front Digit Health 2023, 5, 1207602. [Google Scholar] [CrossRef]
- Improving Detection and Management of Postpartum Hypertension [Internet]. [cited 2025 Mar 31]. Available from: https://www.healthcatalyst.com/learn/success-stories/improving-detection-and-management-of-postpartum-hypertension.
- Hirshberg, A.; Downes, K.; Srinivas, S. Comparing standard office-based follow-up with text-based remote monitoring in the management of postpartum hypertension: a randomised clinical trial. BMJ Qual Saf. 2018, 27, 871–7. [Google Scholar] [CrossRef]
- Vudathaneni, V.K.P.; Lanke, R.B.; Mudaliyar, M.C.; Movva, K.V.; Mounika Kalluri, L.; Boyapati, R. The Impact of Telemedicine and Remote Patient Monitoring on Healthcare Delivery: A Comprehensive Evaluation. Cureus [Internet]. 2024 Mar 4 [cited 2025 Mar 31]; Available from: https://www.cureus.com/articles/227384-the-impact-of-telemedicine-and-remote-patient-monitoring-on-healthcare-delivery-a-comprehensive-evaluation.
- Mazaheri Habibi, M.R.; Moghbeli, F.; Langarizadeh, M.; Fatemi Aghda, S.A. Mobile health apps for pregnant women usability and quality rating scales: a systematic review. BMC Pregnancy Childbirth. 2024, 24, 34. [Google Scholar] [CrossRef]
- NHS App [Internet]. NHS England Digital. [cited 2025 Mar 31]. Available from: https://digital.nhs.uk/services/nhs-app.
- Reidy, C.; Papoutsi, C.; Kc, S.; Gudgin, B.; Laverty, A.A.; Greaves, F. , et al. Qualitative evaluation of the implementation and national roll-out of the NHS App in England. BMC Med. 2025, 23, 20. [Google Scholar] [CrossRef]
- England NHS. NHS England » Remote consulting [Internet]. [cited 2025 Mar 31]. Available from: https://www.england.nhs.uk/long-read/remote-consulting/.
- Delanerolle, G.; Phiri, P.; Cavalini, H.; Benfield, D.; Shetty, A.; Bouchareb, Y. , et al. Synthetic data & the future of Women’s Health: A synergistic relationship. International Journal of Medical Informatics 2023, 179, 105238. [Google Scholar] [PubMed]
- Locke, L.G.; Hodgdon, G. Gender bias in visual generative artificial intelligence systems and the socialization of AI. AI & Soc [Internet]. 2024 Nov 25 [cited 2025 Mar 31]; Available from: https://link.springer.com/10.1007/s00146-024-02129-1.
- Cirillo, D.; Catuara-Solarz, S.; Morey, C.; Guney, E.; Subirats, L.; Mellino, S. , et al. Sex and gender differences and biases in artificial intelligence for biomedicine and healthcare. npj Digit Med. 2020, 3, 81. [Google Scholar] [CrossRef] [PubMed]
- Cross, J.L.; Choma, M.A.; Onofrey, J.A. Bias in medical AI: Implications for clinical decision-making. Cheungpasitporn W, editor. PLOS Digit Health. 2024, 3, e0000651. [Google Scholar] [CrossRef] [PubMed]
- Buolamwini, J. Study finds gender and skin-type bias in commercial artificial-intelligence systems [Internet]. MIT Media Lab. [cited 2025 Mar 31]. Available from: https://www.media.mit.edu/articles/study-finds-gender-and-skin-type-bias-in-commercial-artificial-intelligence-systems/.
- UNESCO, EQUALS Skills Coalition. I’d blush if I could: closing gender divides in digital skills through education [Internet]. UNESCO; 2019 Jan [cited 2025 Mar 31]. Available from: https://unesdoc.unesco.org/ark:/48223/pf0000367416.
- Perez, A.J.; Zeadally, S. Recent Advances in Wearable Sensing Technologies. Sensors. 2021, 21, 6828. [Google Scholar] [CrossRef]
- Delanerolle, G.; Yang, X.; Shetty, S.; Raymont, V.; Shetty, A.; Phiri, P. , et al. Artificial intelligence: A rapid case for advancement in the personalization of Gynaecology/Obstetric and Mental Health care. Womens Health (Lond Engl) 2021, 17, 17455065211018111. [Google Scholar] [CrossRef]
- Komodo Health Introduces New No-Code Analytics Application To Visualize Real-World Healthcare Data in Minutes [Internet]. [cited 2025 Mar 31]. Available from: https://www.businesswire.com/news/home/20240319355597/en/Komodo-Health-Introduces-New-No-Code-Analytics-Application-To-Visualize-Real-World-Healthcare-Data-in-Minutes.
- Lego V, di. Uncovering the gender health data gap. Cad Saude Publica. 2023, 39, e00065423. [Google Scholar] [CrossRef]
- Kirkby, K.; Bergen, N.; Baptista, A.; Schlotheuber, A.; Hosseinpoor, A.R. Data Resource Profile: World Health Organization Health Inequality Data Repository. International Journal of Epidemiology. 2023, 52, e253–62. [Google Scholar] [CrossRef]
- Schubert, K.G.; Bird, C.E.; Kozhimmanil, K.; Wood, S.F. To Address Women’s Health Inequity, It Must First Be Measured. Health Equity. 2022, 6, 881–6. [Google Scholar] [CrossRef]
- European health interview survey - methodology [Internet]. [cited 2025 Apr 1]. Available from: https://ec.europa.eu/eurostat/statistics-explained/index.php?title=European_health_interview_survey_-_methodology.
- E6(R2) Good Clinical Practice: Integrated Addendum to ICH E6(R1) | Guidance for Industry.
- World Development Report 2022: FINANCE for an Equitable Recovery [Internet]. World Bank. [cited 2025 Mar 31]. Available from: https://www.worldbank.org/en/publication/wdr2021.
- Kaewkungwal, J.; Adams, P.; Sattabongkot, J.; Lie, R.K.; Wendler, D. Issues and Challenges Associated with Data-Sharing in LMICs: Perspectives of Researchers in Thailand. The American Journal of Tropical Medicine and Hygiene. 2020, 103, 528–36. [Google Scholar] [CrossRef]
- Lieftink, N.; Ribeiro, C.D.S.; Kroon, M.; Haringhuizen, G.B.; Wong, A.; Van De Burgwal, L.H. The potential of federated learning for public health purposes: a qualitative analysis of GDPR compliance, Europe, 2021. Eurosurveillance [Internet]. 2024 Sep 19 [cited 2025 Mar 31];29(38). Available from: https://www.eurosurveillance.org/content/10.2807/1560-7917.ES.2024.29.38.2300695.
- Wenham, C.; Davies, S.E. WHO runs the world – (not) girls: gender neglect during global health emergencies. International Feminist Journal of Politics. 2022, 24, 415–38. [Google Scholar] [CrossRef]
- Palaniappan, K.; Lin, E.Y.T.; Vogel, S. Global Regulatory Frameworks for the Use of Artificial Intelligence (AI) in the Healthcare Services Sector. Healthcare. 2024, 12, 562. [Google Scholar] [CrossRef]
- Patwardhan, V.; Gil, G.F.; Arrieta, A.; Cagney, J.; DeGraw, E.; Herbert, M.E. , et al. Differences across the lifespan between females and males in the top 20 causes of disease burden globally: a systematic analysis of the Global Burden of Disease Study 2021. The Lancet Public Health. 2024, 9, e282–94. [Google Scholar] [CrossRef]
| Policy Recommendations for Women’s Health Equity | |||
|---|---|---|---|
| Mandating Gender-Disaggregated Data Collection | Expanding Women’s Health Research Funding | Regulating AI and Digital Health Bias | Strengthening Health Data in LMICs |
| Clinical trials | Non-reproductive health conditions | Ethical guidelines for AI in healthcare | Improving women’s health data collection |
| Epidemiological research | Addressing disparities in medical research | Preventing gender bias in machine learning models | Evidence-based interventions |
| Health system monitoring | Ensuring fairness in diagnostic tools | Contextually relevant solutions | |
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2025 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (http://creativecommons.org/licenses/by/4.0/).





