Introduction
Infectious diseases have shaped human history, causing devastating pandemics and ongoing health crisis worldwide. The Spanish flu pandemic of 1918-1919 is one of the most lethal outbreaks, killing between 50-100 million people due to the absence of antimicrobial agents, vaccines, and advanced critical care (Berche, 2022). Additionally, cholera, smallpox, bubonic plague, and influenza have caused major disease outbreaks in the past (Hoiby, 2021). Despite significant medical advancements, even today diseases such as tuberculosis, malaria, hepatitis and Covid - 19 continue to cause widespread morbidity and mortality as these diseases are infectious in nature (Kaur
et al., 2021). Moreover, impact of Covid - 19 pandemic is evident globally that led to both mortality and morbidity claiming over seven million lives worldwide leaving a great impact on society, environment and economic sector, causing widespread job losses, healthcare system collapse, learning disruptions, and economic recessions in multiple countries (Hotez, 2020; Cagino
et al., 2024; Nicola
et al., 2020). Besides the immediate loss of life, many infectious disease survivors suffer from long-term health issues which affects their quality of life and imposes heavy overload on healthcare systems (Morens
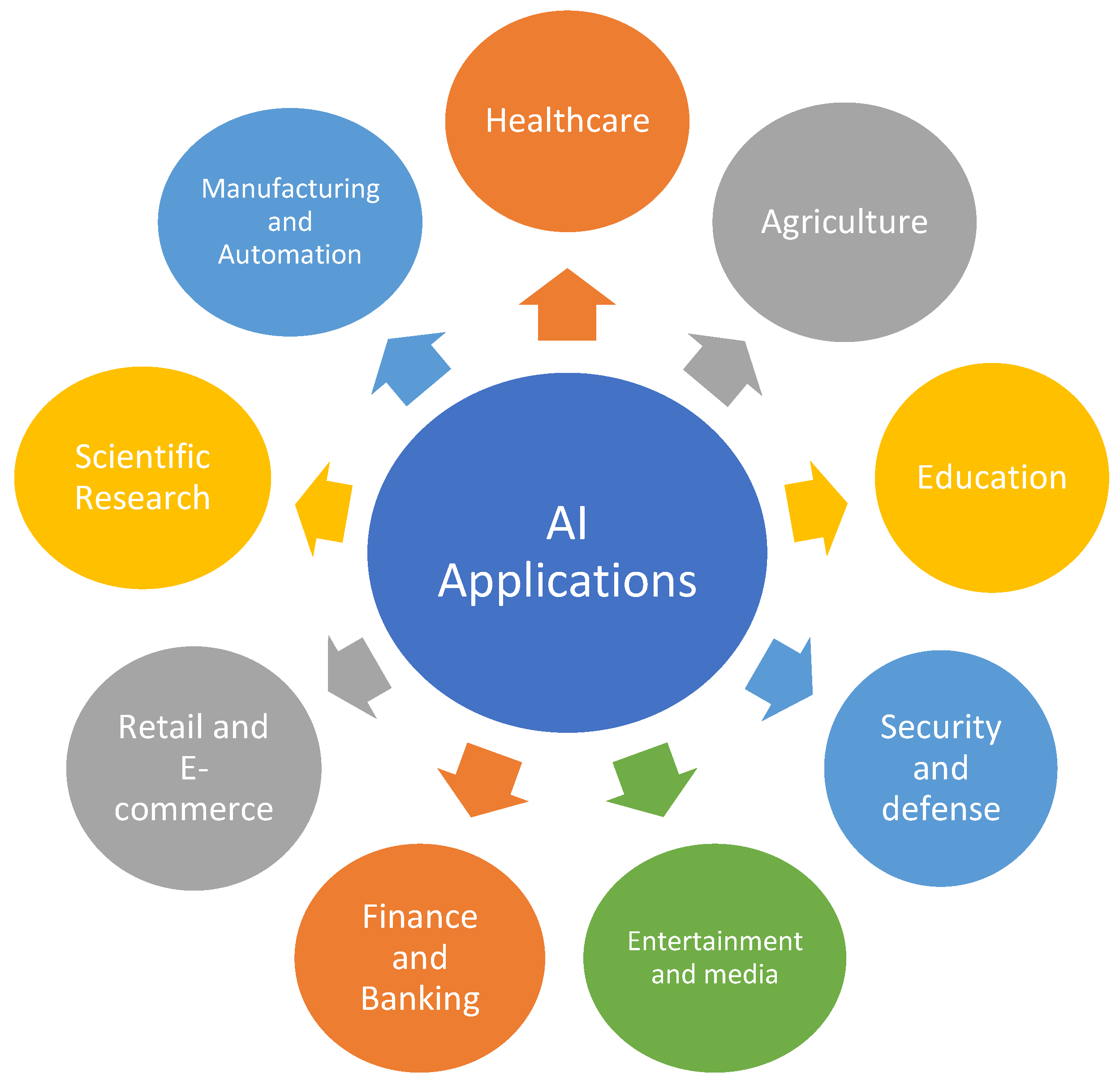
et al., 2004). More specifically, the burden of infectious illnesses increases due to socioeconomic variables such as poverty, poor sanitation, and limited access to healthcare especially in developing nations. Despite advancements in healthcare, the emergence of new pathogens, re-emergence of older infections, and the rise of antimicrobial resistance continue to complicate disease control and prevention efforts (Gupta and Garg, 2023). To overcome all these hurdles to combat infectious diseases, researchers and healthcare stakeholders have been continuously trying to discover innovative approaches to assist the medical field, particularly in identifying the spread of infectious illnesses (Dhar, 2014). Among various approaches, AI, the talk of day in every field particularly ML and DL, has transformed biomedical research in recent years (Topol, 2019; Brownstein
et al., 2023;
Figure 1.).
By using ML algorithms and data-driven insights, AI helps detect, predict, and manage epidemics more effectively, reducing their global impact while also assisting in diagnosis, precise treatment, threat detection, and lesion identification to minimize medical errors and improve healthcare efficiency (Kermany et al., 2018). AI has demonstrated impressive results in image-based diagnostics, especially in the interpretation of pathological and radiological images. For example, chest X-rays have been analyzed using deep Convolutional Neural Networks (CNNs) to diagnose tuberculosis (TB). In low-resource places where trained radiologists are mostly inaccessible, CNN model might diagnose TB from chest X-rays with diagnostic performance comparable to radiologists (Al-Hajjar, 2024). Similarly, AI models have been created to identify and categorize pathogens in blood smears e.g. CNNs have been used to detect malaria parasites on stained blood films. The AI system's accuracy was above 90% in case of CNN models, greatly lowering the diagnostic load in endemic areas (Liang et al., 2016). Beside these, ML techniques have also been used to evaluate the chances of infectious disease transmission at various geographical scales examining enormous databases, such as social media, medical records, and environmental data leading to early indication of disease in epidemics and also clearly demonstrating the significant role of AI in modern disease diagnostics and control, paving the way for more advanced and accessible healthcare solutions (McCall, 2020; Zhou et al., 2024). The gathering in knowledge concerned with AI for diagnosis and treatment is essential to ameliorate the current healthcare status. Therefore, the main aim of the present review is to describe the significance of AI in diagnosis and management of various infectious diseases.
Infectious Diseases
Infectious illnesses are caused by microscopic organisms such as bacteria, viruses, parasites or fungi that are spread from person to person either directly or indirectly. The direct mode of transmission involves physical touch, vertical transmission, sexual transmission or by vector bite. Besides these, SARS-CoV-2 and influenza are disseminated via aerosols or respiratory droplets whereas diseases like cholera and hepatitis A spread via contaminated food or water (Jones et al., 2020). These infectious diseases are paramount cause of mortality and morbidity worldwide, especially for young children in developing nations (King et al., 2006). Among various infectious diseases, malaria, diarrhea, and lower respiratory infections are some of the leading causes of death and have a great impact on health systems, economy, and society as evident by recent occurrence of Covid-19 pandemic (Layne et al., 2020; Simen-Kapeu et al., 2021). Moreover, infectious illnesses have a crucial effect on healthcare systems by putting a demand on resources, interfering with regular services, and revealing systemic weaknesses and making treatment more difficult due to the evolution of resistant strains. Substantial advancements in prevention and treatment of disease have led to some sort of reduction in life threatening infectious diseases. However, discovery of vaccination has played an instrumental role in eradicating, eliminating, or significantly reducing the burden of several infectious diseases like polio, smallpox, measles and rubella, but still there are many other diseases such as HIV, malaria are prevalent and needs much more attention so as to avoid the sufferings of the people (Zheng et al., 2018). World Health Organization (WHO), Global Alliance for Vaccines and Immunization (GAVI), and the Global Fund are among the organizations that use financing, research, and vaccination programs to reduce the burden of infectious illnesses (Jama et al., 2023). The most important impact of modern surveillance networks is to track outbreaks and carry out prompt treatments using digital technologies and artificial intelligence (Vaishya et al., 2020).
Artificial Intelligence
The term Artificial Intelligence (AI) describes the formation of algorithms and computer systems which can carry out operations that normally demand for human intellect and include learning, thinking, solving problems, making decisions and comprehending natural language (Hamet and Tremblay, 2017). The Turing test, which uses binary judgement criteria as its primary criterion, defines AI as the capacity of computers to interact with people (via electronic output devices) without revealing that they are not humans (Jiang et al., 2022). John McCarthy was the first to coin the term Artificial Intelligence during the Dartmouth Summer Research Project on AI in 1956 and is regarded as the father of AI (Andresen, 2002).
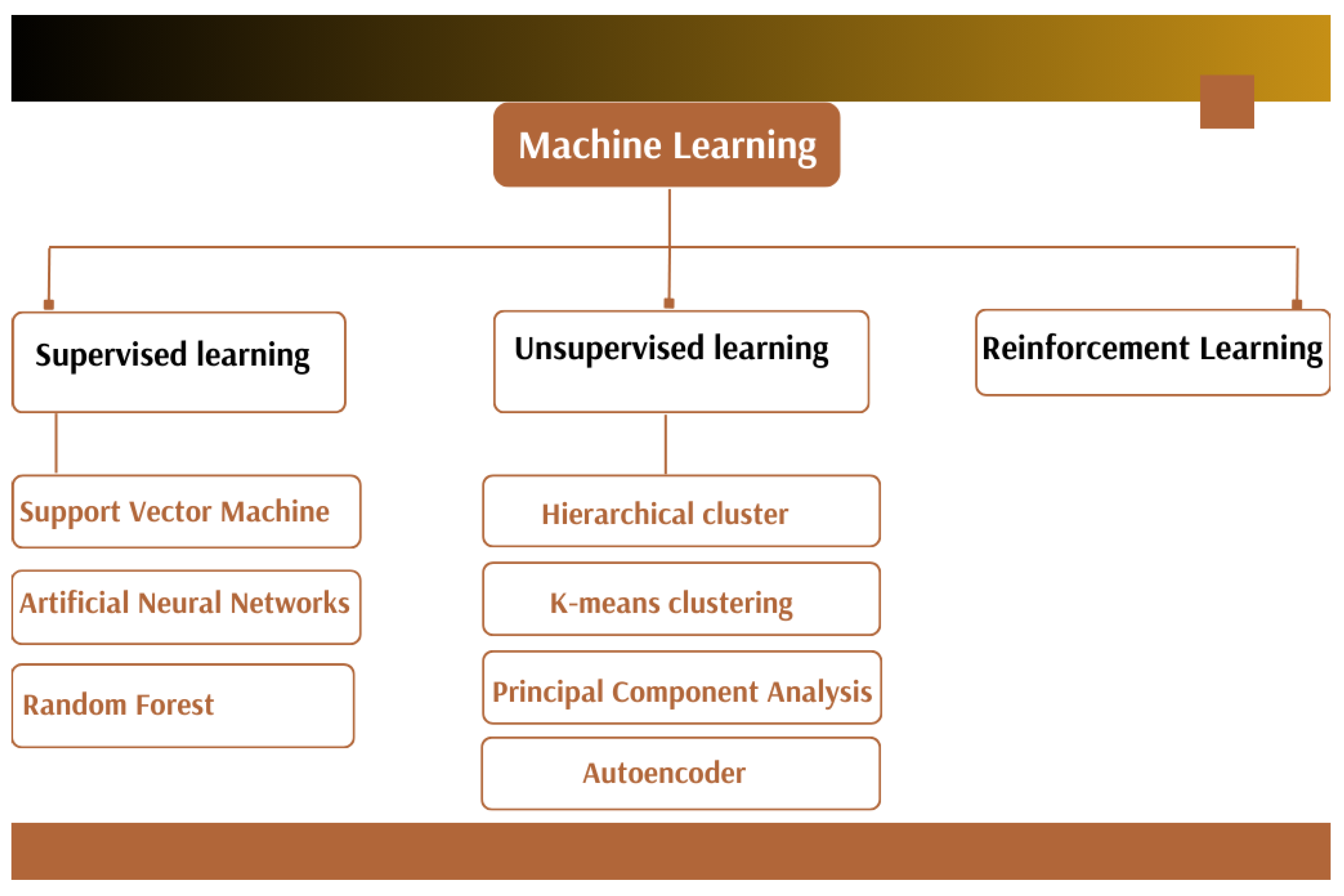
Machine learning (ML), a branch of AI, involves use of data as an input resource. Preset mathematical functions are used for classifying or regressing outcome that is often hard for people to achieve. ML is a rapid and cost-effective technique which is becoming more and more popular in a number of domains e.g., image recognition, autonomous vehicles, personalized medicine and medical diagnostics (Ahsan and Siddique, 2022). Traditionally, ML is divided into three main groups: (a) unsupervised learning, (b) supervised learning, which includes classification and regression techniques, and (c) reinforcement learning (Tran et al., 2021). ML techniques can be parametric (like logistic regression) or nonparametric (like neural networks and non-neural network approaches like logistic regression, Naïve Bayes, gradient boosting machine/decision tree, Support Vector Machine (SVM), k-nearest neighbour (k-NN), Random Forest (RF), and linear regression). However, selection of ML techniques depends on the type of data that provides better decisions during epidemic process to evaluate huge amounts of data and offer insight, and leads to a deeper understanding of the illness to both health and public officials (Thair et al., 2021). Furthermore, ML and AI make it simple to prevent, control, and monitor infectious diseases while for fatal and hazardous diseases, big data applications and deep learning (a subset of ML) can be very beneficial (Chrimes et al., 2017). As AI continues to advance, further innovations are expected to enhance the efficiency and precision of healthcare interventions.
Disease Surveillance Using AI
Disease surveillance mainly involves promptly identifying possible health risks, verifying, evaluating, and investigating them to support public health control recommendations (Paquet et al., 2006). Numerous disease monitoring initiatives have prioritized ML models which use the internet and open health data sources to enhance surveillance and prediction of infectious diseases including cholera, dengue fever, and malaria (Borda et al., 2022).
The "flu tracker" (an AI tool) employs crowd sourced platforms to report flu symptoms and enhance global influenza monitoring was created by the U.S. Centres for Disease Control and Prevention. It has become an essential tool to track the number of influenza cases and is based on the U.S. influenza-like illness surveillance network, which tracks the proportion of patients who visit outpatient clinics with influenza-like illness symptoms, such as fever, cough, or sore throat, over the total number of patient visits (Hart, 2019).
Several research teams, including Boston Children's Hospital's Computational Health Informatics Program (CHIP), have been using forecasting methods in conjunction with ML to produce more accurate estimations and predictive indications of local flu activity (Borda et al., 2022). Autoregression with general online information (ARGONet) is a program that uses data from Google searches linked to flu, Electronic Health Records (EHRs), and past flu activity in a specific area. ARGONet also uses the spatial-temporal patterns of flu propagation in nearby places to increase its accuracy (Smolinski et al., 2015). Huge amount of data from a variety of sources, such as social media, environmental data, news articles and medical records have been used by AI-powered systems to detect patterns that might be signs of disease outbreaks (Tripathi and Rathore, 2025).
Risk analysis firms equipped with AI-enabled the discovery of Covid-19 virus early before the notification of WHO. Moreover, in late December 2019, an AI epidemiologist from the Canadian business BlueDot has been the first to report on the COVID-19 epidemic. BlueDot expanded from places in China by analyzing data from news headlines, airline tickets, and animal illness outbreaks and helped in identifying locations that might be susceptible to the epidemic (McCall, 2020). San Francisco-based Metabiota is another firm utilizing AI that provides a near-term forecasting model of disease spread and an epidemic tracker. AI, combined with different tributaries, is considered helpful in depicting prediction of the agent responsible for causing diseases vis-à-vis place of its origin, as Coronavirus outbreak was predicted early by employing Metabiota in countries including Japan, Thailand, Taiwan, and South Korea (Allam et al., 2020).
AI for Diagnostics and Disease Detection
Controlling the impact and spread of infectious illnesses requires early and accurate diagnosis. Though conventional diagnostic techniques, such as Polymerase Chain Reaction (PCR), culture-based approaches, and serological testing provide good input about the diagnosis and treatment of infectious diseases but demands frequent specialized labs, skilled workers, and a substantial amount of time. Therefore, diagnosis of diseases has been transformed by artificial intelligence (AI), especially ML and deep learning (DL), that enhances accessibility, speed, and accuracy. Many diseases are predicted and diagnosed using AI techniques, particularly those whose diagnosis depends on imaging or signalling analysis (Uysal and Ozturk, 2020). Medical image analysis has been benefited greatly from ML approaches because of complex algorithms that allow for the automatic extraction of enhanced information (Nia et al., 2023). AI is already used to support medical professionals and enhance illness diagnosis; for instance, it helps gynaecologists to make judgements on the initial course of therapy and early detection of ectopic pregnancies (Fernández et al., 2019).
The field of ML also assists in detecting the diagnosis of an illness by using prior training data (Razia
et al., 2017). Numerous researchers have developed a variety of ML techniques that may effectively identify a range of diseases such as diabetes, cardiac syndrome, chronic kidney disease, breast cancer, and liver cancer having major influence on a person's health and can be fatal if left untreated (Ibrahim and Abdulazeez, 2021; Kohli and Arora, 2018). A number of classifiers and clustering algorithms, including K-nearest, Random Forest, Support Vector Machine (SVM), Decision Tree, Naïve Bayes and others can provide a solution to this problem as a result of advancements in ML and AI (Grampurohit and Sagarnal, 2020). Three main types of ML algorithms are utilized in disease diagnostics i.e. supervised learning, unsupervised learning and reinforcement learning as mentioned in
Figure 2.
Supervised Learning
This has been significant in the development of diagnostic algorithms for analyzing images in addition to various other decision supportive tasks in healthcare (Uddin et al., 2019). One effective supervised classifier is SVM (Cortes and Vapnik, 1995). SVMs work well for binary classification tasks like identifying infected and non-infected individuals from medical imaging e.g. SVMs have been used to accurately classify TB in chest X-rays (Perez-Barcena et al., 2023).
Artificial Neural Networks (ANNs), another supervised algorithm is primarily built on mathematical models that draw reference from biological nervous systems, including the information found in brain networks. American neurophysiologist Warren McCulloch initially defined ANN in 1943, which paved the way for Walter Pitts to create neural networks with electrical circuits. Various scientists have looked at the potential of ANN for the diagnosis and treatment of a range of infectious disorders, including COVID-19, dengue, diarrhoea, tuberculosis, and childhood blindness (Niazkar, 2020; Javaid and Saeed, 2021; Mbunge, 2022).
Random Forest is an ensemble learning technique which enhances diagnostic accuracy by combining many decision trees and has been used to analyze test findings and patient vital signs in order to diagnose sepsis. It uses an assembly of decision trees to give high classification accuracy by analyzing intricate relationships between clinical parameters (Touw et al., 2013). Wang et al. 2020 employed a RF prediction model to analyze the outcomes of COVID-19 patients alongwith their prognoses and the control techniques to protect these patients from SARS-Cov 2.
Unsupervised Learning
In unsupervised ML, the model uses unlabeled data to find information and hidden patterns that has played crucial role in diagnosis of infectious diseases. These are useful for classifying disease subtypes, detecting new diseases, and improving diagnostic accuracy when analyzing genetic sequences, patient health records, and epidemiological data (Sogandi, 2024). Commonly used unsupervised learning algorithms in disease diagnosis are hierarchical clustering, K-means clustering, Principal Component Analysis (PCA) and autoencoders.
Hierarchical cluster analysis pairs clusters, variables, or variables and clusters in a sequential manner to create a distinct set of nested categories or clusters. Starting with the correlation matrix, every cluster and unclustered variable is tested in every pair that may be formed. The pair that produces the highest average intercorrelation inside the trial cluster is selected as the new cluster (Valkenborg et al., 2023). Hierarchical clustering builds a tree-like structure (dendrogram) to represent data relationships and is useful in clustering patients with similar immune responses or disease progression patterns ((Ran et al., 2023; Aljohani, 2024). Papin et al. 2021 have used this algorithm for clinical and biological clustering of sepsis patients.
K- Means clustering is a simple type of unsupervised learning which sorts similar data points based on their features (Likas et al., 2003). It has been used to classify malaria infected and non infected RBCs from microscopic images which improved the efficiency of automated diagnosis of malaria (Abdul Nasir et al., 2012).
PCA for dimensionality reduction retains the most important information by reducing the complexity of high- dimensional medical datasets (Greenacre et al., 2023). It has been used in simplifying complex data of whole genome and protein sequences in Covid-19 studies (Wang and Jiang, 2024).
Autoencoder encodes information into a condensed and meaningful representation and then decodes it back in such a manner that the reconstructed input is as close to the original as
possible (Bank et al., 2023). Autoencoder CNNs are used to improve anomaly detection by uncovering hidden patterns in the data for pneumonia detection in chest X-rays (Nosa-Omoruyi and Oghenekaro, 2024).
Reinforcement Learning
The goal of reinforcement learning (RL) is to maximize rewards by decision-making through the use of agent-environment interaction and their possibly delayed feedbacks. RL concurrently addresses sampling, evaluative, and delayed feedbacks in sequential decision-making situations. However, in infectious disease diagnosis, RL models can optimize clinical decision-making, diagnostic strategies, and personalized treatment plans by continuously learning from patient data. Unlike supervised learning, which depends on labeled datasets, RL dynamically improves its performance based on feedback, making it well-suited for complex medical scenario. RL has been applied in automated medical diagnosis for analyzing ultrasound, Magnetic Resonance Imaging (MRI), Computed Tomography (CT) scan images (Yu et al., 2023).
Deep Learning
Deep learning (DL) is a subset of ML, but it makes use of a more sophisticated technique that mimics human thought and learning processes to allow computers to automatically extract, analyze, and comprehend the valuable information from the raw data (Khan et al., 2021). It has transformed infectious disease diagnosis by enabling automated, high-accuracy analysis of complex medical data. DL models, particularly CNNs, Long Short-Term Memory (LSTM) networks, Recurrent Neural Networks (RNNs) and Transformer-based models have wide application in medical imaging, genomic analysis, and clinical diagnostics. These models extract intricate patterns from radiology images, EHRs, genomic sequences and laboratory test results, enhancing early detection and precision medicine for infectious diseases (Alqaissi et al., 2022).
CNNs are widely used in the automated diagnosis of infectious diseases from medical images such as CT scans, X-rays and Magnetic Resonance Imaging (MRIs) by extracting hierarchical image features, distinguishing between infected and healthy tissues with high accuracy. DL technology may be applied to create an efficient diagnosis tool for COVID-19 and viral pneumonia using X-ray images (Keles et al., 2024).
Hochreiter and Schmidhuber (1997) initially presented the LSTMs structural architecture for RNNs in 1997 (Absar et al., 2022). An LSTM-based model was used to analyze EHRs for sepsis prediction, improving early diagnosis and intervention strategies (Absar et al., 2022). RNNs have been used in disease outbreak forecasting, analyzing past infection rates to predict the spread of influenza and dengue fever (Amin et al., 2020).
Transformer-based models like Bidirectional Encoder Representations from Transformers (BERT) and Generative Pre- training Transformer (GPT) have revolutionized NLP tasks in medical research. Transformers have been applied in SARS-CoV-2 genomic sequence analysis that helped in identifying mutations and new variants with improved accuracy (Feng et al., 2024). BioBERT, a domain-specific NLP model, has also been used to extract key information from scientific literature and clinical notes, aiding in real-time analysis of infectious disease reports (Lee et al., 2020).
NLP, a component of AI enables machines to understand, interpret, and analyze human language with the help of either ML or rule based approaches to understand the meaning and structure of text (Locke et al., 2021). NLP algorithms can process unstructured patient records for identifying main symptoms and risk factors related to infectious diseases. It can also enhance diagnostic accuracy by extracting assembled information from ML models. Ancochea et al. 2021 employed EHRead, a technology by Savana (an international, medical company) that uses NLP, DL and ML, to access and analyze the free-text, unstructured data that medical professionals enter into EHR.
AI in Point-of-Care Testing and Rapid Diagnostics
The term "point-of-care" (POC) diagnostics refers to a novel, innovative method for on-site, real-time, fast, and precise detection at the patient's point of need (Wang et al., 2021). AI enhances POC testing by integrating real-time analysis with portable diagnostic devices. AI-based mobile applications analyze images of Rapid Diagnostic Test (RDT) strips (e.g., for malaria or COVID-19), providing fast and accurate results without needing expert interpretation (Bermejo-Peláez et al., 2022). Biosensors are bioanalytical devices that interact and detect target analytes using biorecognition components. Wearable sensors combined with AI algorithms can detect early physiological changes, indicative of infections, such as fever, oxygen saturation drops, or heart rate variability (Flynn and Chang, 2024).
AI in Genomic and Molecular Diagnostics
AI speeds up pathogen diagnosis by genetic sequence analysis and mutations identification in real time. Next Generation Sequencing (NGS) has the potential to produce even more significant outcomes, insights, and results with the evolution of AI and ML. ML techniques analyze infectious agent genomic sequences quickly, improving pathogen identification and epidemic tracking (Ouanes, 2024). Algorithms for ML and AI have become effective weapons in the fight against AMR. Large datasets can now be analyzed efficiently due to recent advancements in AI/ML, which makes it possible to forecast AMR trends and treatment outcomes with minimum human assistance. Targeted treatment techniques can be developed by using ML algorithms to analyze genomic data and find genetic markers linked to antibiotic resistance. Furthermore, AI/ML approaches have potential for improving medication delivery and creating substitutes for conventional antibiotics (Lastra et al., 2024).
AI in Drug Discovery
Drug research and vaccine development have been transformed by AI, significantly reducing the cost and time required to identify effective treatments for infectious diseases. AI-driven methods improve vaccine development, optimize medication design, and speed up target identification whereas traditional drug discovery pipelines take 10–15 years and cost billions of dollars (Blanco-González et al., 2023).
Drug repurposing involves identifying existing FDA-approved drugs for new therapeutic uses. AI algorithms use DL and NLP to search through clinical trial data, medical literature, and molecular interactions to forecast repurposed medications. AI-driven drug repurposing identifies FDA-approved drugs that have unexpected antibacterial properties and saves years of development time compared to new drug discovery. Hence, it reduces clinical trial costs and expands the range of available treatments for MDR infections. AI repurposed metformin (the diabetes drug) for its potential antimicrobial activity against MDR tuberculosis (Jiang et al., 2024).
During the Covid-19 pandemic, remdesivir, baricitinib and dexamethasone have been used as potential treatment through AI powered drug repurposing. BenevolentAI used NLP and ML to identify baricitinib, a rheumatoid arthritis drug, as a potential COVID-19 treatment (Mohanty et al., 2020). To find possible therapeutic targets, AI systems examine enormous biological datasets, such as proteomic, metabolomic, and genomic data while DL models scan genomic sequences to identify essential viral and bacterial proteins that can serve as drug targets. AI-based network pharmacology helps uncover novel biomarkers for disease progression. AlphaFold, an AI-based protein structure prediction tool by DeepMind, accurately predicted the structures of SARS-CoV-2 proteins, accelerating drug development efforts (Torres et al., 2024)
AI models assist in predicting drug-protein binding affinities to identify promising compounds, optimizing molecular structures for better efficacy, lower toxicity; and virtual screening of millions of molecules to prioritize candidates for laboratory testing. Atomwise (a pharma company) used AI-driven virtual screening to identify small-molecule inhibitors for Ebola virus, reducing the time required for early-stage drug discovery, thus it is observed that through computational modeling and deep learning techniques, AI enables precise targeting of pathogens and accelerates the screening of potential compounds (Hemamalini et al., 2024).
AI in Personalized Treatment
AI models analyze proteomic, genomic, and metabolomic data to predict how an individual will respond to different treatments by identifying the host genetic factors that influence the disease susceptibility by optimizing both antiviral and antimicrobial therapies to minimize drug resistance (Johnson et al., 2021). AI models predicted patient-specific responses to HIV antiretroviral therapy, optimizing drug regimens for minimized side effects and maximum efficacy (Marcus et al., 2020).
AI helps in predicting which drugs will be most effective for a particular patient and identifying cases where pathogens develop drug resistance. ML algorithms analyze vast clinical datasets to predict patient-specific drug resistance patterns while AI assists in designing alternative drug regimens for patients with multidrug-resistant infections. Moreover, AI models have also been used to predict antibiotic resistance in TB patients, enabling doctors to choose effective second-line drugs for resistant strains (Geethalakshmi et al., 2024).
Sepsis, a life-threatening condition caused by severe infections, requires real-time monitoring and early intervention and AI have played a crucial role in early detection of sepsis using predictive algorithms on EHRs (Schinkel et al., 2019). AI-powered ICU management systems have been developed to optimize antibiotic dosages to improve survival rates, ventilator settings, fluid resuscitation, and vasopressor administration (Hakverdi et al., 2024). Google's DeepMind developed an AI model that predicted sepsis 48 hours in advance, reducing mortality rates in critically ill patients (Holcomb et al., 2018).
By utilizing patient-specific data, AI facilitates personalized treatment strategies that improve therapeutic outcomes and reduce adverse reactions. This method improves patient care by tailoring medical interventions based on individual genetic and physiological profiles.
AI in Novel Antibiotic Discovery
Traditional antibiotic discovery is slow and expensive, with most compounds failing in clinical trials. Interestingly, AI accelerates this process by screening millions of chemical compounds to identify potential antibiotics and can predict drug-target interactions and bacterial resistance mechanisms vis-à-vis can design novel synthetic antibiotics with enhanced efficacy (David et al., 2021). More specifically, AI discovered Halicin, a new antibiotic that is able to kill drug-resistant bacteria, including E. coli and Acinetobacter baumannii, within days of computational analysis (Booq et al., 2021).
AI for AMR Prediction and Early Detection
ML models analyze bacterial genomic data, clinical records, and patient demographics to predict which pathogens are resistant to specific antibiotics helping clinicians to select the most effective antibiotic therapy for individual patients. ML also reduces the unnecessary use of broad-spectrum antibiotics and helps in identifying high-risk patients likely to develop drug-resistant infections. Yang et al. 2019 developed a DL model that predicted tuberculosis drug resistance with an accuracy of 95% based on whole-genome sequencing data.
Traditional culture-based antibiotic susceptibility testing takes 24–72 hours, delaying critical treatment decisions but AI enhances rapid AMR detection through DL analysis of microscopic images to identify resistant bacteria, AI-driven mass spectrometry for detecting resistance-associated biomarkers and integration with POC diagnostic devices for real-time resistance profiling. DeepAMR, an AI-based framework, successfully identified resistant bacterial strains from genomic data within hours, aiding faster decision-making (Yang et al., 2019).
The application of AI in antimicrobial resistance helps in identifying resistance patterns and predicting new resistance mechanisms. By analyzing vast datasets, AI aids in optimizing antibiotic prescriptions and developing novel antimicrobial therapies to combat resistant infections.
AI in Patient Management and Remote Monitoring
Remote patient monitoring (RPM) using wearable devices, mobile health apps, and AI-powered chatbots improves patient outcomes by tracking symptoms and vitals in real-time, sending alerts for early intervention if a patient's condition worsens and hence ensuring treatment adherence through automated medication reminders (Jeddi and Bohr, 2020). AI-powered smartwatches detected early symptoms of COVID-19 based on physiological data like heart rate and oxygen levels, allowing for early isolation and treatment (Skibinska et al., 2021).
Digital therapeutics involve using AI-powered mobile applications to guide patients through treatment protocols, provide mental health support for infectious disease patients and offer dietary and lifestyle recommendations to support immune function. Ma et al. 2025 have also shown that AI-based chatbots and mobile apps were used to support mental health and medication adherence in HIV patients, improving their overall health outcomes.
Challenges
Despite the transformative potential of AI, it still faces several challenges in the management of infectious disease due to limited availability and quality of data, lack of expertise, privacy concerns, high costs, explainability issues, and regulatory barriers as AI models require large, high-quality datasets for training, but in many regions, patient data is incomplete, unstructured, or inconsistent that reduces the accuracy of AI predictions alongwith bias that remains a major issue (Badidi, 2023). More specifically, if AI systems are trained on data that does not represent diverse populations, can lead to inaccurate diagnosis and worsen healthcare disparities, particularly in low-income regions (Luengo-Oroz et al., 2021).
Another significant barrier is the lack of AI expertise among healthcare professionals. Many doctors and clinicians have limited training in AI, making it difficult to integrate AI-based tools into clinical workflows. Without proper understanding, there are a chances of misinterpreting AI-generated predictions. Furthermore, the use of AI in infectious disease management raises ethical and privacy concerns. AI systems rely on large amounts of patient data, and sharing this data for research and AI training often conflicts with privacy regulations (Rony et al., 2024).
The high cost and infrastructure challenges also limit AI adoption in many areas of the world. AI development and implementation require high-performance computing, reliable internet access and advanced software, which may not be available in low-resource settings (Iliashenko et al., 2019). Additionally, the lack of explainability in AI models makes it difficult for doctors to trust AI-based decisions. Finally, regulatory and legal barriers too slow down AI deployment in healthcare (Hassan et al., 2024). AI-powered diagnostic tools must undergo rigorous approval processes by regulatory agencies before clinical use, and many countries lack clear legal frameworks for AI in healthcare. However, addressing these challenges will need better data management, improved AI education for healthcare professionals, stronger privacy safeguards, cost-effective AI solutions, and clear regulatory guidelines. By overcoming these obstacles, AI can be more effectively integrated into infectious disease management, leading to better patient outcomes and stronger global health systems.
Conclusion
AI has emerged as an indispensable tool in various fields of human health i.e. diagnosis of infectious disease, surveillance, treatment, and pandemic response. Though, AI-driven solutions have streamlined diagnostics, accelerated drug discovery, and enhanced epidemiological monitoring, contributing to improved global health outcomes, however its implementation is still a point of concern due to various challenges in low-resource settings, AI-based point-of-care diagnostics and wearable health monitoring devices have expanded healthcare accessibility and have played a crucial role in AMR surveillance, guiding policymakers in antibiotic stewardship efforts.
Despite these successes, several challenges hinder the full-scale implementation of AI in healthcare due to data privacy, lack of standardization, algorithmic bias, and high computational requirements that needs to be addressed in detail. Moreover, ethical concerns regarding AI-based medical decision-making highlight the need for transparent and interpretable AI models.
Furthermore, collaborations between AI researchers, healthcare professionals, and policymakers are crucial for ensuring AI-driven healthcare solutions that are scalable, affordable, and equitable. However, with continued advancements in bioinformatics, AI is approaching to revolutionize the management of infectious diseases, reduce mortality rates, and strengthen global health security.
Future Perspectives
The future of AI in the management of infectious disease will rely on improving interpretability and transparency to ensure that AI-driven decisions are reliable and trusted in clinical settings. Developing explainable AI (XAI) models will guide healthcare professionals in understanding how AI systems generate predictions, making them more applicable in real-world scenarios. Additionally, federated learning and privacy-preserving AI will enable collaboration across multiple healthcare institutions while protecting patient data, addressing a major concern in AI-driven healthcare. More specifically, AI is also expected to play a key role in predicting emerging pathogens and tracking disease evolution by analyzing genomic sequences and epidemiological trends to anticipate viral mutations and potential outbreaks. Furthermore, integrating AI with wearable devices and remote health monitoring will allow real-time tracking of infectious diseases, improving early detection and personalized treatment. In drug discovery and vaccine development, AI will accelerate drug repurposing and optimize vaccine formulation, reducing the time needed for clinical trials and regulatory approvals. To expand the reach of AI-driven healthcare, efforts should focus on developing lightweight, offline-compatible AI models that can be deployed in resource-limited settings. Finally, ensuring ethical AI implementation by addressing issues of bias, fairness, and regulatory compliance will be essential for its responsible adoption. By overcoming these challenges and continuing to advance AI-driven innovations, the future of infectious disease management will become more effective, proactive, and globally accessible.
References
- Abdul Nasir, A.S.; Mashor, M.Y.; Mohamed, Z. Segmentation based approach for detection of malaria parasites using moving k-means clustering. 2012 IEEE-EMBS Conference on Biomedical Engineering and Sciences 2012, 653. [Google Scholar]
- Absar, N.; Uddin, N.; Khandaker, M.U.; Ullah, H. The efficacy of deep learning based LSTM model in forecasting the outbreak of contagious diseases. Infectious Disease Modelling 2022, 7, 170–183. [Google Scholar] [CrossRef] [PubMed]
- Ahsan, M.M.; Siddique, Z. Machine learning-based heart disease diagnosis: A systematic literature review. Artificial Intelligence in Medicine 2022, 128, 102289. [Google Scholar] [CrossRef] [PubMed]
- Al-Hajjar, S. Breakthroughs in Artificial Intelligence for Combating Infectious Diseases. International Journal of Pediatrics and Adolescent Medicine 2024, 11, 55–57. [Google Scholar] [CrossRef]
- Aljohani, A. Optimizing Patient Stratification in Healthcare: A Comparative Analysis of Clustering Algorithms for EHR Data. International Journal of Computational Intelligence Systems 2024, 17, 173. [Google Scholar] [CrossRef]
- Allam, Z.; Dey, G.; Jones, D. Artificial Intelligence (AI) Provided Early Detection of the Coronavirus (COVID-19) in China and Will Influence Future Urban Health Policy Internationally. AI 2020, 1, 156–165. [Google Scholar] [CrossRef]
- Alqaissi, E.Y.; Alotaibi, F.S.; Ramzan, M.S. Modern Machine-Learning Predictive Models for Diagnosing Infectious Diseases. Computational and Mathematical Methods in Medicine 2022, 2022, 1–13. [Google Scholar] [CrossRef]
- Amin, S.; Uddin, M.I.; Hassan, S.; Khan, A.; Nasser, N.; Alharbi, A.; Alyami, H. Recurrent Neural Networks With TF-IDF Embedding Technique for Detection and Classification in Tweets of Dengue Disease. IEEE Access 2020, 8, 131522–131533. [Google Scholar] [CrossRef]
- Ancochea, J.; Izquierdo, J.L.; Savana COVID-19 Research, G.r.o.u.p.; Soriano, J.B. Evidence of Gender Differences in the Diagnosis and Management of Coronavirus Disease 2019 Patients: An Analysis of Electronic Health Records Using Natural Language Processing and Machine Learning. Journal of Women’s Health 2021, 30, 393–404. [Google Scholar] [CrossRef]
- Andresen, S.L. John McCarthy: Father of AI. IEEE Intelligent Systems 2002, 17, 84–85. [Google Scholar] [CrossRef]
- Badidi, E. Edge AI for Early Detection of Chronic Diseases and the Spread of Infectious Diseases: Opportunities, Challenges, and Future Directions. Future Internet 2023, 15, 370. [Google Scholar] [CrossRef]
- Bank, D.; Koenigstein, N.; Giryes R (2023) Autoencoders In, L. Rokach, O. Maimon, & E. Shmueli (Eds.), Machine Learning for Data Science Handbook. 353–374.
- Berche, P. The Spanish flu. La Presse Médicale 2022, 51, 104127. [Google Scholar] [CrossRef] [PubMed]
- Bermejo-Peláez, D.; Marcos-Mencía, D.; Álamo, E.; Pérez-Panizo, N.; Mousa, A.; Dacal, E.; Lin, L.; Vladimirov, A.; Cuadrado, D.; Mateos-Nozal, J.; Galán, J.C.; Romero-Hernandez, B.; Cantón, R.; Luengo-Oroz, M.; Rodriguez-Dominguez, M. A Smartphone-Based Platform Assisted by Artificial Intelligence for Reading and Reporting Rapid Diagnostic Tests: Evaluation Study in SARS-CoV-2 Lateral Flow Immunoassays. JMIR Public Health and Surveillance 2022, 8, e38533. [Google Scholar] [CrossRef] [PubMed]
- Blanco-González, A.; Cabezón, A.; Seco-González, A.; Conde-Torres, D.; Antelo-Riveiro, P.; Piñeiro, Á.; Garcia-Fandino, R. The Role of AI in Drug Discovery: Challenges, Opportunities, and Strategies. Pharmaceuticals 2023, 16, 891. [Google Scholar] [CrossRef]
- Booq, R.Y.; Tawfik, E.A.; Alfassam, H.A.; Alfahad, A.J.; Alyamani, E.J. Assessment of the Antibacterial Efficacy of Halicin against Pathogenic Bacteria. Antibiotics 2021, 10, 1480. [Google Scholar] [CrossRef]
- Borda, A.; Molnar, A.; Neesham, C.; Kostkova, P. Ethical Issues in AI-Enabled Disease Surveillance: Perspectives from Global Health. Applied Sciences 2022, 12, 3890. [Google Scholar] [CrossRef]
- Brownstein, J.S.; Rader, B.; Astley, C.M.; Tian, H. Advances in Artificial Intelligence for Infectious-Disease Surveillance. New England Journal of Medicine 2023, 388, 1597–1607. [Google Scholar] [CrossRef]
- Cagino, L.; Seagly, K.; Noyes, E.; Prescott, H.; Valley, T.; Eaton, T.; McSparron, J.I. Outcomes and Management After COVID-19 Critical Illness. CHEST 2024, 165, 1149–1162. [Google Scholar] [CrossRef]
- Chrimes, D.; Kuo, M.H.; Moa, B.; Hu, W. Towards a real-time big data analytics platform for health applications. International Journal of Big Data Intelligence 2017, 4, 61. [Google Scholar] [CrossRef]
- Cortes, C.; Vapnik, V. Support-vector networks. Machine Learning 1995, 20, 273–297. [Google Scholar] [CrossRef]
- David, L.; Brata, A.M.; Mogosan, C.; Pop, C.; Czako, Z.; Muresan, L.; Ismaiel, A.; Dumitrascu, D.I.; Leucuta, D.C.; Stanculete, M.F.; Iaru, I.; Popa, S.L. Artificial Intelligence and Antibiotic Discovery. Antibiotics 2021, 10, 1376. [Google Scholar] [CrossRef] [PubMed]
- De La Lastra JM, P.; Wardell SJ, T.; Pal, T.; De La Fuente-Nunez, C.; Pletzer, D. From Data to Decisions: Leveraging Artificial Intelligence and Machine Learning in Combating Antimicrobial Resistance – a Comprehensive Review. Journal of Medical Systems 2024, 48, 71. [Google Scholar] [CrossRef] [PubMed]
- De Ramón Fernández, A.; Ruiz Fernández, D.; Prieto Sánchez, M.T. A decision support system for predicting the treatment of ectopic pregnancies. International Journal of Medical Informatics 2019, 129, 198–204. [Google Scholar] [CrossRef] [PubMed]
- Dhar, V. Big Data and Predictive Analytics in Health Care. Big Data 2014, 2, 113–116. [Google Scholar] [CrossRef]
- Feng, Y.; Goldberg, E.E.; Kupperman, M.; Zhang, X.; Lin, Y.; Ke, R. CovTransformer: A transformer model for SARS-CoV-2 lineage frequency forecasting. Virus Evolution 2024, 10, veae086. [Google Scholar] [CrossRef]
- Flynn, C.D.; Chang, D. Artificial Intelligence in Point-of-Care Biosensing: Challenges and Opportunities. Diagnostics 2024, 14, 1100. [Google Scholar] [CrossRef]
- Geethalakshmi, S.; Yadav, S. Advancements in artificial intelligence for the diagnosis of multidrug resistance and extensively drug-resistant tuberculosis: a comprehensive review. Cureus 2024, 16. [Google Scholar]
- Ghaffar Nia, N.; Kaplanoglu, E.; Nasab, A. Evaluation of artificial intelligence techniques in disease diagnosis and prediction. Discover Artificial Intelligence 2023, 3, 5. [Google Scholar] [CrossRef]
- Grampurohit, S.; Sagarnal, C. Disease Prediction using Machine Learning Algorithms. 2020 International Conference for Emerging Technology (INCET) 2020, 1–7. [Google Scholar]
- Greenacre, M.; Groenen PJ, F.; Hastie, T.; D’Enza, A.I.; Markos, A.; Tuzhilina, E. Publisher Correction: Principal component analysis. Nature Reviews Methods Primers 2023, 3, 22. [Google Scholar] [CrossRef]
- Gupta, V.; Garg, R. Emerging and Re-Emerging Infections: An Overview. Recent Advances in Pharmaceutical Innovation and Research 2023, 761–770. [Google Scholar]
- Hakverdi, Y. , Urve Gümüş, M., Taştekin, A., Idin, K., Kanḡın, M., Özyer, T., & Alhajj, R. Enhancing ICU Management and Addressing Challenges in Türkiye Through AI-Powered Patient Classification and Increased Usability With ICU Placement Software. IEEE Access 2024, 12, 146121–146136. [Google Scholar]
- Hamet, P.; Tremblay, J. Artificial intelligence in medicine. Metabolism 2017, 69, S36–S40. [Google Scholar] [CrossRef] [PubMed]
- Hart, A.M. Influenza: a clinical update following a century of influenza science. The Journal for Nurse Practitioners 2019, 15, 429–433. [Google Scholar] [CrossRef]
- Hassan, M.; Kushniruk, A.; Borycki, E. Barriers to and Facilitators of Artificial Intelligence Adoption in Health Care: Scoping Review. JMIR Human Factors 2024, 11, e48633. [Google Scholar] [CrossRef]
- Hemamalini, V.; Tyagi, A.K.; Vennila, V. ; Kumari S (2024) Revolutionizing drug Discovery With Cutting-Edge Technologies: Issue Challenges for the Next Decade In RK, P. Tripathi & S. Tiwari (Eds.), Advances in Healthcare Information Systems and Administration. 76–89.
- Høiby, N. Pandemics: past, present, future: that is like choosing between cholera and plague. Apmis 2021, 129, 352–371. [Google Scholar] [CrossRef]
- Holcomb, S.D.; Porter, W.K.; Ault, S.V.; Mao, G.; Wang, J. Overview on DeepMind and Its AlphaGo Zero AI. Proceedings of the 2018 International Conference on Big Data and Education 2018, 67–71. [Google Scholar]
- Hotez, P. J. NTDs in the 2020s: An epic struggle of effective control tools versus the Anthropocene. PLOS Neglected Tropical Diseases 2020, 14, e0007872. [Google Scholar] [CrossRef]
- Ibrahim, I.; Abdulazeez, A. The Role of Machine Learning Algorithms for Diagnosing Diseases. Journal of Applied Science and Technology Trends 2021, 2, 10–19. [Google Scholar] [CrossRef]
- Iliashenko, O.; Bikkulova, Z.; Dubgorn, A. Opportunities and challenges of artificial intelligence in healthcare. E3S Web of Conferences 2019, 110, 02028. [Google Scholar] [CrossRef]
- Jama, M.; Chakroun, M.; Atta, H.; Hasan, Q.; Hutin, Y.; Irtaza, A.; Mataria, A.; Hajjeh, R. Accelerating the prevention, control and elimination of communicable diseases through integration and optimization of the support from Gavi and Global Fund: A vision for the Eastern Mediterranean Region. Eastern Mediterranean Health Journal 2023, 29, 87–88. [Google Scholar] [CrossRef] [PubMed]
- Javaid, S. , & Saeed, N. (2021). Neural networks for infectious diseases detection: Prospects and challenges. Authorea Preprints.
- Jeddi, Z. , & Bohr, A. (2020). Remote patient monitoring using artificial intelligence. In Artificial Intelligence in Healthcare. 203–234.
- Jiang, Y.; Li, X.; Luo, H.; Yin, S.; Kaynak, O. Quo vadis artificial intelligence? Discover Artificial Intelligence 2022, 2, 4. [Google Scholar] [CrossRef]
- Johnson, K.B.; Wei, W.; Weeraratne, D.; Frisse, M.E.; Misulis, K.; Rhee, K.; Zhao, J.; Snowdon, J.L. Precision Medicine, AI, and the Future of Personalized Health Care. Clinical and Translational Science 2021, 14, 86–93. [Google Scholar] [CrossRef] [PubMed]
- Jones, N.; Bouzid, M.; Few, R.; Hunter, P.; Lake, I. Water, sanitation and hygiene risk factors for the transmission of cholera in a changing climate: using a systematic review to develop a causal process diagram. Journal of water and health 2020, 18, 145–158. [Google Scholar] [CrossRef]
- Kaur, I.; Behl, T.; Aleya, L.; Rahman, H.; Kumar, A.; Arora, S.; Bulbul, I.J. Artificial intelligence as a fundamental tool in management of infectious diseases and its current implementation in COVID-19 pandemic. Environmental Science and Pollution Research 2021, 28, 40515–40532. [Google Scholar] [CrossRef]
- Keles, A. , Keles, M. B., & Keles, A. COV19-CNNet and COV19-ResNet: Diagnostic Inference Engines for Early Detection of COVID-19. Cognitive Computation 2024, 16, 1612–1622. [Google Scholar]
- Kermany, D.S.; Goldbaum, M.; Cai, W.; Valentim CC, S.; Liang, H.; Baxter, S.L.; McKeown, A.; Yang, G.; Wu, X.; Yan, F.; Dong, J.; Prasadha, M.K.; Pei, J.; Ting MY, L.; Zhu, J.; Li, C.; Hewett, S.; Dong, J.; Ziyar, I.; … Zhang, K. Identifying Medical Diagnoses and Treatable Diseases by Image-Based Deep Learning. Cell 2018, 172, 1122–1131. [Google Scholar] [CrossRef]
- Khan, P. , Kader, Md. F., Islam, S. M. R., Rahman, A. B., Kamal, Md. S., Toha, M. U., & Kwak, K.-S. Machine Learning and Deep Learning Approaches for Brain Disease Diagnosis: Principles and Recent Advances. IEEE Access 2021, 9, 37622–37655. [Google Scholar]
- King, D.A.; Peckham, C.; Waage, J.K.; Brownlie, J.; Woolhouse ME, J. Infectious Diseases: Preparing for the Future. Science 2006, 313, 1392–1393. [Google Scholar] [CrossRef]
- Kohli, P.S.; Arora, S. Application of Machine Learning in Disease Prediction. 2018 4th International Conference on Computing Communication and Automation (ICCCA) 2018, 1–4. [Google Scholar]
- Layne, S.P.; Hyman, J.M.; Morens, D.M.; Taubenberger, J.K. New coronavirus outbreak: Framing questions for pandemic prevention. Science Translational Medicine 2020, 12, eabb1469. [Google Scholar] [CrossRef] [PubMed]
- Lee, J.; Yoon, W.; Kim, S.; Kim, D.; Kim, S.; So, C.H.; Kang, J. BioBERT: A pre-trained biomedical language representation model for biomedical text mining. Bioinformatics 2020, 36, 1234–1240. [Google Scholar] [CrossRef] [PubMed]
- Liang, Z. , Powell, A., Ersoy, I., Poostchi, M., Silamut, K., Palaniappan, K., Guo, P., Hossain, M. A., Sameer, A., Maude, R. J., Huang, J. X., Jaeger, S., & Thoma, G. CNN-based image analysis for malaria diagnosis. 2016 IEEE International Conference on Bioinformatics and Biomedicine (BIBM) 2016, 493–496. [Google Scholar]
- Likas, A.; Vlassis, N.; J Verbeek, J. The global k-means clustering algorithm. Pattern Recognition 2003, 36, 451–461. [Google Scholar] [CrossRef]
- Locke, S.; Bashall, A.; Al-Adely, S.; Moore, J.; Wilson, A.; Kitchen, G.B. Natural language processing in medicine: A review. Trends in Anaesthesia and Critical Care 2021, 38, 4–9. [Google Scholar] [CrossRef]
- Luengo-Oroz, M.; Bullock, J.; Pham, K.H.; Lam CS, N.; Luccioni, A. From Artificial Intelligence Bias to Inequality in the Time of COVID-19. IEEE Technology and Society Magazine 2021, 40, 71–79. [Google Scholar] [CrossRef]
- Ma, Y. , Achiche, S., Tu, G., Vicente, S., Lessard, D., Engler, K., Lemire, B., MARVIN chatbots Patient Expert Committee, Laymouna, M., De Pokomandy, A., Cox, J., & Lebouché, B. The first AI -based Chatbot to promote HIV self-management: A mixed methods usability study. HIV Medicine 2025, 26, 184–206. [Google Scholar]
- Marcus, J.L.; Sewell, W.C.; Balzer, L.B.; Krakower, D.S. Artificial Intelligence and Machine Learning for HIV Prevention: Emerging Approaches to Ending the Epidemic. Current HIV/AIDS Reports 2020, 17, 171–179. [Google Scholar] [CrossRef]
- Mbunge, E.; Batani, J.; Gaobotse, G.; Muchemwa, B. Virtual healthcare services and digital health technologies deployed during coronavirus disease 2019 (COVID-19) pandemic in South Africa: a systematic review. Global health journal 2022, 6, 102–113. [Google Scholar] [CrossRef]
- McCall, B. COVID-19 and artificial intelligence: Protecting health-care workers and curbing the spread. The Lancet Digital Health 2020, 2, e166–e167. [Google Scholar] [CrossRef]
- Mohanty, S.; Harun Ai Rashid, M.; Mridul, M.; Mohanty, C.; Swayamsiddha, S. Application of Artificial Intelligence in COVID-19 drug repurposing. Diabetes & Metabolic Syndrome: Clinical Research & Reviews 2020, 14, 1027–1031. [Google Scholar]
- Morens, D.M.; Folkers, G.K.; Fauci, A.S. The challenge of emerging and re-emerging infectious diseases. Nature 2004, 430, 242–249. [Google Scholar] [CrossRef] [PubMed]
- Niazkar, H.R.; Niazkar, M. Application of artificial neural networks to predict the COVID-19 outbreak. Global health research and policy 2020, 5, 1–11. [Google Scholar] [CrossRef] [PubMed]
- Nicola, M.; Alsafi, Z.; Sohrabi, C.; Kerwan, A.; Al-Jabir, A.; Iosifidis, C.; Agha, M.; Agha, R. The socio-economic implications of the coronavirus pandemic (COVID-19): A review. International Journal of Surgery 2020, 78, 185–193. [Google Scholar] [CrossRef]
- Nosa-Omoruyi, M. , & Oghenekaro, L. U. (2024). AutoEncoder Convolutional Neural Network for Pneumonia Detection. arXiv preprint arXiv:2409.02142, arXiv:2409.02142.
- Ouanes K (2024) The role of artificial intelligence machine learning in, N.G.S. Ouanes K (2024) The role of artificial intelligence machine learning in, N.G.S. In Next Generation Sequencing (NGS) Technology in DNA Analysis. 531–538.
- Papin, G. , Bailly, S., Dupuis, C., Ruckly, S., Gainnier, M., Argaud, L., Azoulay, E., Adrie, C., Souweine, B., Goldgran-Toledano, D., Marcotte, G., Gros, A., Reignier, J., Mourvillier, B., Forel, J.-M., Sonneville, R., Dumenil, A.-S., Darmon, M., Garrouste-Orgeas, M., … OUTCOMEREA study group. Clinical and biological clusters of sepsis patients using hierarchical clustering. PLOS ONE 2021, 16, e0252793. [Google Scholar]
- Paquet, C.; Coulombier, D.; Kaiser, R.; Ciotti, M. Epidemic intelligence: A new framework for strengthening disease surveillance in Europe. Eurosurveillance 2006, 11, 5–6. [Google Scholar] [CrossRef]
- Perez-Barcena, F.; Bayareh-Mancilla, R.; Hernández-Rodríguez, Y.M.; Murillo-Ortíz, B.; Cigarroa-Mayorga, O.E. Building an Extensive Database for Training Predictive Models in Image Classification of Mammography Views and Projections using Support Vector Machines. 2023 20th International Conference on Electrical Engineering, Computing Science and Automatic Control (CCE).
- Plotkin, S.; Robinson, J.M.; Cunningham, G.; Iqbal, R.; Larsen, S. The complexity and cost of vaccine manufacturing – An overview. Vaccine 2017, 35, 4064–4071. [Google Scholar] [CrossRef]
- Ran, X.; Xi, Y.; Lu, Y.; Wang, X.; Lu, Z. Comprehensive survey on hierarchical clustering algorithms and the recent developments. Artificial Intelligence Review 2023, 56, 8219–8264. [Google Scholar] [CrossRef]
- Ranney, M.L.; Griffeth, V.; Jha, A.K. Critical Supply Shortages—The Need for Ventilators and Personal Protective Equipment during the Covid-19 Pandemic. New England Journal of Medicine.
- Razia, S.; Prathyusha, P.S.; Krishna, N.V.; Sumana, N.S. A review on disease diagnosis using machine learning techniques. International Journal of Pure and Applied Mathematics 2017, 117, 79–85. [Google Scholar]
- Rony MK, K.; Numan, S. Md. , Akter, K., Tushar, H., Debnath, M., Johra, F. T., Akter, F., Mondal, S., Das, M., Uddin, M. J., Begum, J., & Parvin, Mst. R. Nurses’ perspectives on privacy and ethical concerns regarding artificial intelligence adoption in healthcare. Heliyon 2024, 10, e36702. [Google Scholar]
- Schinkel, M.; Paranjape, K.; Nannan Panday, R.S.; Skyttberg, N.; Nanayakkara PW, B. Clinical applications of artificial intelligence in sepsis: A narrative review. Computers in Biology and Medicine 2019, 115, 103488. [Google Scholar] [CrossRef] [PubMed]
- Simen-Kapeu, A.; Bogler, L.; Weber, A.-C.; Ntambi, J.; Zagre, N.M.; Vollmer, S.; Ekpini, R.E. Prevalence of diarrhoea, acute respiratory infections, and malaria over time (1995-2017): A regional analysis of 23 countries in West and Central Africa. Journal of Global Health 2021, 11, 13008. [Google Scholar] [CrossRef] [PubMed]
- Skibinska, J. , Burget, R., Channa, A., Popescu, N., & Koucheryavy, Y. COVID-19 Diagnosis at Early Stage Based on Smartwatches and Machine Learning Techniques. IEEE Access 2021, 9, 119476–119491. [Google Scholar]
- Smith, M.J.; Silva, D.S. Ethics for pandemics beyond influenza: Ebola, drug-resistant tuberculosis, and anticipating future ethical challenges in pandemic preparedness and response. Monash Bioethics Review.
- Smolinski, M.S.; Crawley, A.W.; Baltrusaitis, K.; Chunara, R.; Olsen, J.M.; Wójcik, O.; Santillana, M.; Nguyen, A.; Brownstein, J.S. Flu Near You: Crowdsourced Symptom Reporting Spanning 2 Influenza Seasons. American Journal of Public Health 2015, 105, 2124–2130. [Google Scholar] [CrossRef]
- Sogandi, F. Identifying diseases symptoms and general rules using supervised and unsupervised machine learning. Scientific Reports 2024, 14, 17956. [Google Scholar] [CrossRef]
- Thair, S.; Mewes, C.; Hinz, J.; Bergmann, I.; Büttner, B.; Sehmisch, S.; Meissner, K.; Quintel, M.; Sweeney, T.E.; Khatri, P.; Mansur, A. Gene Expression–Based Diagnosis of Infections in Critically Ill Patients—Prospective Validation of the SepsisMetaScore in a Longitudinal Severe Trauma Cohort. Critical Care Medicine 2021, 49, e751–e760. [Google Scholar] [CrossRef]
- Topol, E.J. High-performance medicine: The convergence of human and artificial intelligence. Nature Medicine 2019, 25, 44–56. [Google Scholar] [CrossRef]
- Torres, J.; Pervushin, K.; Surya, W. Prediction of conformational states in a coronavirus channel using Alphafold-2 and DeepMSA2: Strengths and limitations. Computational and Structural Biotechnology Journal 2024, 23, 3730–3740. [Google Scholar] [CrossRef]
- Touw, W.G.; Bayjanov, J.R.; Overmars, L.; Backus, L.; Boekhorst, J.; Wels, M.; Van Hijum SA, F.T. Data mining in the Life Sciences with Random Forest: A walk in the park or lost in the jungle? Briefings in Bioinformatics 2013, 14, 315–326. [Google Scholar] [CrossRef]
- Tran, N.K.; Albahra, S.; May, L.; Waldman, S.; Crabtree, S.; Bainbridge, S.; Rashidi, H. Evolving Applications of Artificial Intelligence and Machine Learning in Infectious Diseases Testing. Clinical Chemistry 2021, 68, 125–133. [Google Scholar] [CrossRef]
- Tripathi, A. ; Rathore R (2025) AI in Disease Surveillance—An Overview of How AICan Be Used in Disease Surveillance Outbreak Detection in Real-World Scenarios In, R. Singh, A. Gehlot, N. Rathour, & S. V. Akram (Eds.), AI in Disease Detection. 337–359.
- Uddin, S.; Khan, A.; Hossain, M.E.; Moni, M.A. Comparing different supervised machine learning algorithms for disease prediction. BMC Medical Informatics and Decision Making 2019, 19, 281. [Google Scholar] [CrossRef] [PubMed]
- Uysal, G.; Ozturk, M. Hippocampal atrophy based Alzheimer’s disease diagnosis via machine learning methods. Journal of Neuroscience Methods 2020, 337, 108669. [Google Scholar] [CrossRef]
- Vaishya, R.; Javaid, M.; Khan, I.H.; Haleem, A. Artificial Intelligence (AI) applications for COVID-19 pandemic. Diabetes & Metabolic Syndrome: Clinical Research & Reviews 2020, 14, 337–339. [Google Scholar]
- Valkenborg, D.; Rousseau, A.-J.; Geubbelmans, M.; Burzykowski, T. Unsupervised learning. American Journal of Orthodontics and Dentofacial Orthopedics 2023, 163, 877–882. [Google Scholar] [CrossRef] [PubMed]
- Wang, B.; Jiang, L. Principal Component Analysis Applications in COVID-19 Genome Sequence Studies. Cognitive Computation 2024, 16, 1637–1648. [Google Scholar] [CrossRef]
- Wang, C.; Liu, M.; Wang, Z.; Li, S.; Deng, Y.; He, N. Point-of-care diagnostics for infectious diseases: From methods to devices. Nano Today 2021, 37, 101092. [Google Scholar] [CrossRef]
- Wang, J.; Yu, H.; Hua, Q.; Jing, S.; Liu, Z.; Peng, X.; Cao, C.; Luo, Y. A descriptive study of random forest algorithm for predicting COVID-19 patients outcome. PeerJ 2020, 8, e9945. [Google Scholar] [CrossRef]
- Yang, Y. , Walker, T. M., Walker, A. S., Wilson, D. J., Peto, T. E. A., Crook, D. W., Shamout, F., CRyPTIC Consortium, Arandjelovic, I., Comas, I., Farhat, M. R., Gao, Q., Sintchenko, V., Van Soolingen, D., Hoosdally, S., Gibertoni Cruz, A. L., Carter, J., Grazian, C., Earle, S. G., … Clifton, D. A. DeepAMR for predicting co-occurrent resistance of Mycobacterium tuberculosis. Bioinformatics 2019, 35, 3240–3249. [Google Scholar]
- Yu, C.; Liu, J.; Nemati, S.; Yin, G. Reinforcement Learning in Healthcare: A Survey. ACM Computing Surveys 2023, 55, 1–36. [Google Scholar] [CrossRef]
- Zheng, Z.; Diaz-Arévalo, D.; Guan, H.; Zeng, M. Noninvasive vaccination against infectious diseases. Human Vaccines & Immunotherapeutics 2018, 14, 1717–1733. [Google Scholar]
- Zhou, H.-Y.; Li, Y.; Li, J.-Y.; Meng, J.; Wu, A. Harnessing the power of artificial intelligence to combat infectious diseases: Progress, challenges, and future outlook. The Innovation Medicine 2024, 2, 100091. [Google Scholar] [CrossRef]
|
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2025 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (http://creativecommons.org/licenses/by/4.0/).