Submitted:
18 March 2025
Posted:
18 March 2025
Read the latest preprint version here
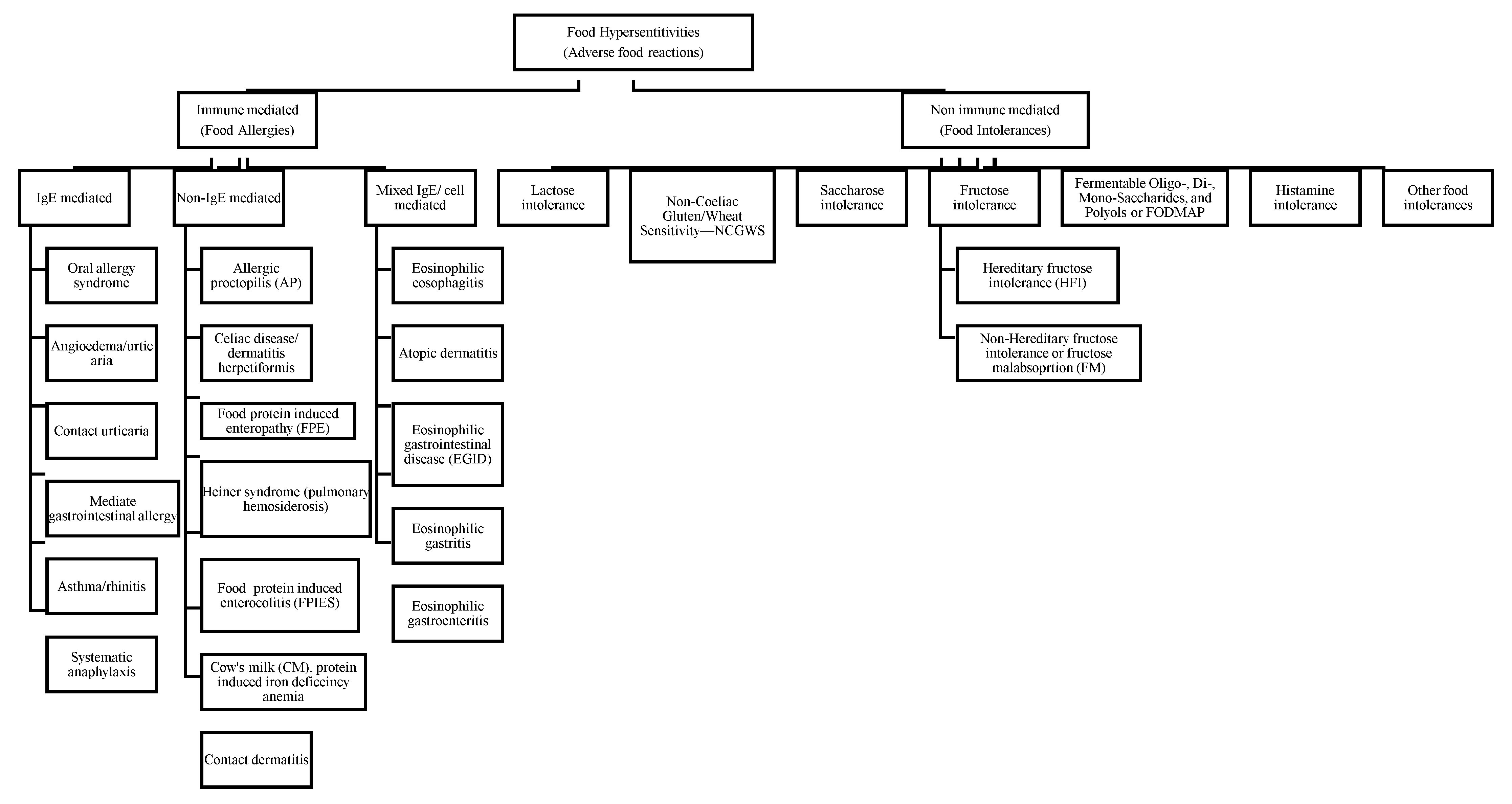
Abstract
Keywords:
1. Introduction
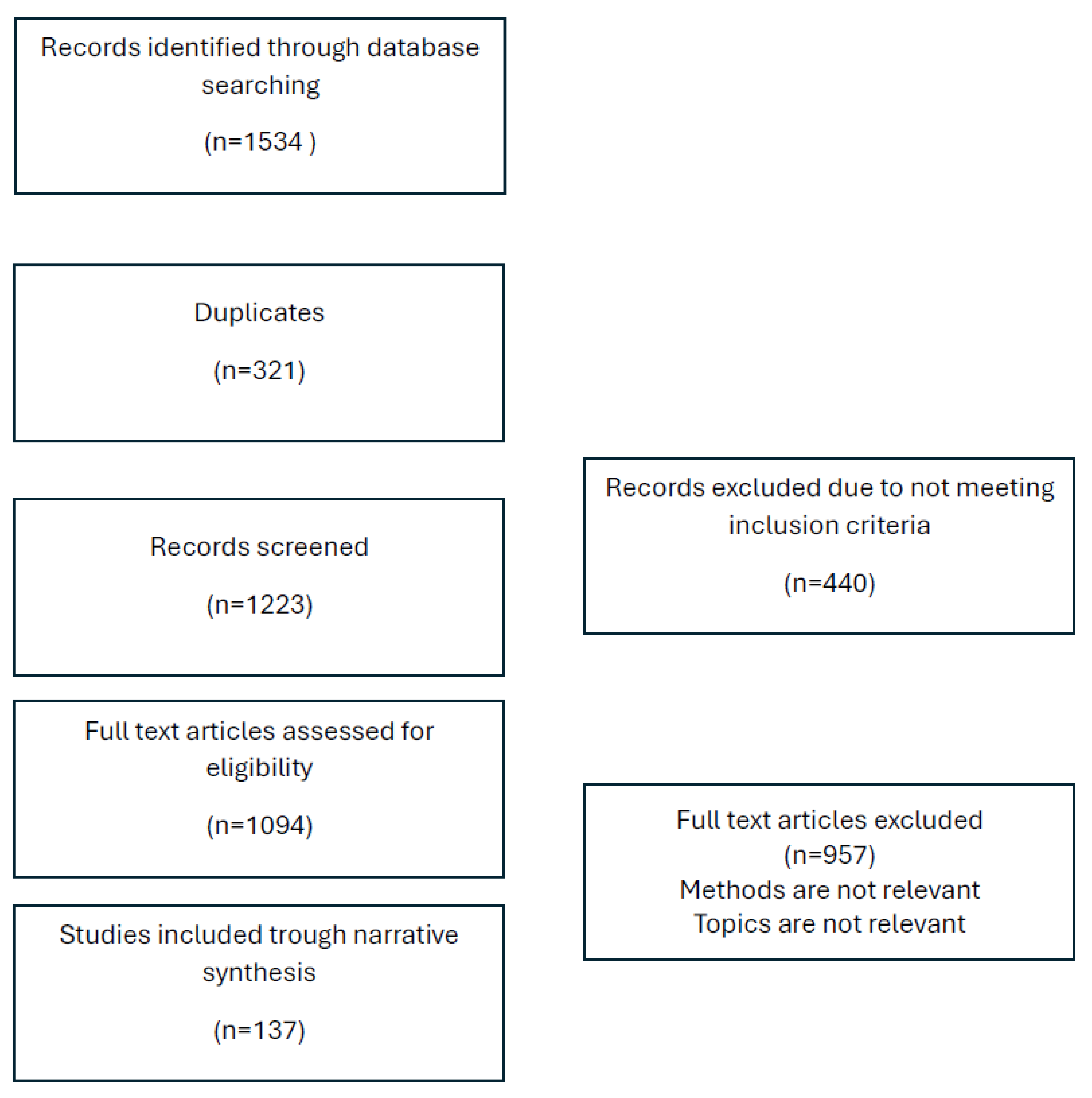
2. Material and Methods
3. Results
3.1. Food Allergies
| Author | Year | Study Type | Country | Sample Size | Duration of Intervention | Summary of Findings |
|---|---|---|---|---|---|---|
| Vassilopoulou et al. [5] | 2022 | Retrospective, observational, multicenter case-control study | Greece | 96 mothers of infants with and 141 mothers of infants without a history of FPIAP. | From May 2018 to November 2020 | Identified cow milk (83%), eggs (7.3%), wheat (6.4%), and beef (6.4%) as the main triggers for allergic proctocolitis in infants through maternal diet. |
| Ruffner et al. [6] | 2013 | Retrospective chart review | USA | 462 cases identified from the hospital patients | From 2007 until 2012 | FPIES reactions were observed more frequently than previously reported, though their presentation and clinical characteristics remained consistent with earlier findings. Milk- and soy-induced FPIES were prevalent, with 43.5% of patients who reacted to milk also experiencing a reaction to soy. |
| Pinto-Sánchez et al. [7] | 2021 | Prospective study | Canada | prospective study of 50 patients with IBS (ROME III, all subtypes), with and without serologic reactivity to gluten (antigliadin IgG and IgA), and 25 healthy subjects (controls) | Between 2012 and 2016 | Evaluated the effectiveness of a gluten-free diet in achieving mucosal healing for celiac patients. |
| Ford et al. [8] | 2014 | Cross Sectional | Canada | 4224 patients recruited | Between January 2008and December 2014 | Functional bowel disorders (FBDs) showed significant demographic and psychological differences among patients. The Rome III classification system did not clearly distinguish between different FBD subtypes. There was considerable symptom overlap among irritable Bowel syndrome (IBS), functional diarrhea, and chronic idiopathic constipation (CIC). The findings suggest a need for improved diagnostic criteria to differentiate FBDs more effectively. |
| Schink et al. [9] | 2018 | Cross sectional observational study | Germany | 64 participants 8 with histamine intolerance (HIT), 25 with food hypersensitivity (FH), 21 with food allergy and 10 healthy controls (HC) |
12 months | Suggested dietary modifications and DAO supplements for histamine intolerance. |
| Halmos et al. [10] | 2014 | Randomized, controlled, cross-over trial | Australia | 30 patients with IBS and 8 healthy individuals (controls, matched for demographics and diet) |
Between April 2009 and June 2011 | Confirmed the efficacy of the low FODMAP diet in IBS symptom reduction. |
| Nwaru et al. [11] | 2014 | Systematic review and meta-analysis | Europe | Not Applicable | Between 1 January 2000 and 30 September 2012 | Highlighted that early introduction of allergenic foods may reduce the risk of developing IgE-mediated food allergies. |
| West et al. [12] | 2014 | Observational population-based study | UK | 57 million | Between 1990 and 2011 | Found that the incidence of celiac disease is increasing, estimating 19.1 per 100,000 cases annually. |
3.1.1. Definition
3.1.2. Symptoms
3.1.3. IgE-Mediated Food Allergies
3.1.4. Mixed IgE/Non IgE Mediated Food Allergies
3.2. Food Intolerances
3.2.1. Lactose Intolerance
3.2.2. Non-Coeliac Gluten/Wheat Sensitivity (NCGWS)
| Celiac Disease | NCGWS | Wheat Allergy | |
|---|---|---|---|
| Prevalence | 0.5–1.7% | 0.6-10% | 0.5–9% in children |
| Pathogenesis | Autoimmune | Non-specific immune response | IgE mediated response |
| DQ2-DQ8 HLA haplotypes | Positive in 95% cases | Positive in 50% cases | Negative |
| Serological markers | IgA anti-EMA, IgA anti-tTG, IgG anti-DGP, IgA anti-gliadin | IgA/IgG anti-gliadin in 50% cases | specific IgE antibodies against wheat and gliadin |
| Duodenal biopsy * | Marsh I to IV with domination of Marsh III and IV | Marsh 0-II, but according to some experts Marsh III might also be in NCGS | Marsh 0-II |
| Duodenal villi atrophy | Present | Absent | Might be present or absent |
3.2.3. Fructose Intolerance
3.2.4. Saccharose Intolerance
3.2.5. Histamine Intolerance
3.2.6. FODMAP
3.3. Irritable Bowel Syndrome IBS
4. Conclusion
Author Contributions
Funding
Conflicts of Interest
References
- Gargano D, Appanna R, Santonicola A, De Bartolomeis F, Stellato C, Cianferoni A, Casolaro V, Iovino P. Food Allergy and Intolerance: A Narrative Review on Nutritional Concerns. Nutrients (2021) 13:1638. [CrossRef]
- Tedner SG, Asarnoj A, Thulin H, Westman M, Konradsen JR, Nilsson C. Food allergy and hypersensitivity reactions in children and adults—A review. Journal of Internal Medicine (2022) 291:283–302. [CrossRef]
- Connors L, O’Keefe A, Rosenfield L, Kim H. Non-IgE-mediated food hypersensitivity. Allergy, Asthma & Clinical Immunology (2018) 14:56. [CrossRef]
- Zingone F, Bertin L, Maniero D, Palo M, Lorenzon G, Barberio B, Ciacci C, Savarino EV. Myths and Facts about Food Intolerance: A Narrative Review. Nutrients (2023) 15:4969. [CrossRef]
- Vassilopoulou E, Feketea G, Konstantinou GN, Zekakos Xypolias D, Valianatou M, Petrodimopoulou M, Vourga V, Tasios I, Papadopoulos NG. Food Protein-Induced Allergic Proctocolitis: The Effect of Maternal Diet During Pregnancy and Breastfeeding in a Mediterranean Population. Front Nutr (2022) 9:. [CrossRef]
- Ruffner MA, Ruymann K, Barni S, Cianferoni A, Brown-Whitehorn T, Spergel JM. Food protein-induced enterocolitis syndrome: insights from review of a large referral population. J Allergy Clin Immunol Pract (2013) 1:343–349. [CrossRef]
- Pinto-Sanchez MI, Nardelli A, Borojevic R, De Palma G, Calo NC, McCarville J, Caminero A, Basra D, Mordhorst A, Ignatova E, et al. Gluten-Free Diet Reduces Symptoms, Particularly Diarrhea, in Patients With Irritable Bowel Syndrome and Antigliadin IgG. Clin Gastroenterol Hepatol (2021) 19:2343-2352.e8. [CrossRef]
- Ford AC, Bercik P, Morgan DG, Bolino C, Pintos-Sanchez MI, Moayyedi P. Characteristics of functional bowel disorder patients: a cross-sectional survey using the Rome III criteria. Aliment Pharmacol Ther (2014) 39:312–321. [CrossRef]
- Schink M, Konturek PC, Tietz E, Dieterich W, Pinzer TC, Wirtz S, Neurath MF, Zopf Y. Microbial patterns in patients with histamine intolerance. J Physiol Pharmacol (2018) 69:. [CrossRef]
- Halmos EP, Power VA, Shepherd SJ, Gibson PR, Muir JG. A diet low in FODMAPs reduces symptoms of irritable bowel syndrome. Gastroenterology (2014) 146:67-75.e5. [CrossRef]
- Nwaru BI, Hickstein L, Panesar SS, Muraro A, Werfel T, Cardona V, Dubois AEJ, Halken S, Hoffmann-Sommergruber K, Poulsen LK, et al. The epidemiology of food allergy in Europe: a systematic review and meta-analysis. Allergy (2014) 69:62–75. [CrossRef]
- West J, Fleming KM, Tata LJ, Card TR, Crooks CJ. Incidence and Prevalence of Celiac Disease and Dermatitis Herpetiformis in the UK Over Two Decades: Population-Based Study. Am J Gastroenterol (2014) 109:757–768. [CrossRef]
- Sicherer SH, Sampson HA. Food allergy: A review and update on epidemiology, pathogenesis, diagnosis, prevention, and management. Journal of Allergy and Clinical Immunology (2018) 141:41–58. [CrossRef]
- Waserman S, Bégin P, Watson W. IgE-mediated food allergy. Allergy, Asthma & Clinical Immunology (2018) 14:55. [CrossRef]
- Anvari S, Miller J, Yeh C-Y, Davis CM. IgE-Mediated Food Allergy. Clinic Rev Allerg Immunol (2019) 57:244–260. [CrossRef]
- Patel BY, Volcheck GW. Food Allergy: Common Causes, Diagnosis, and Treatment. Mayo Clinic Proceedings (2015) 90:1411–1419. [CrossRef]
- Sampson HA, Aceves S, Bock SA, James J, Jones S, Lang D, Nadeau K, Nowak-Wegrzyn A, Oppenheimer J, Perry TT, et al. Food allergy: a practice parameter update-2014. J Allergy Clin Immunol (2014) 134:1016-1025.e43. [CrossRef]
- Savage J, Sicherer S, Wood R. The Natural History of Food Allergy. J Allergy Clin Immunol Pract (2016) 4:196–203; quiz 204. [CrossRef]
- Heinzerling L, Mari A, Bergmann K-C, Bresciani M, Burbach G, Darsow U, Durham S, Fokkens W, Gjomarkaj M, Haahtela T, et al. The skin prick test – European standards. Clin Transl Allergy (2013) 3:3. [CrossRef]
- Heinzerling L, Mari A, Bergmann K-C, Bresciani M, Burbach G, Darsow U, Durham S, Fokkens W, Gjomarkaj M, Haahtela T, et al. The skin prick test – European standards. Clinical and Translational Allergy (2013) 3:3. [CrossRef]
- Bousquet J, Schünemann HJ, Samolinski B, Demoly P, Baena-Cagnani CE, Bachert C, Bonini S, Boulet LP, Bousquet PJ, Brozek JL, et al. Allergic Rhinitis and its Impact on Asthma (ARIA): achievements in 10 years and future needs. J Allergy Clin Immunol (2012) 130:1049–1062. [CrossRef]
- Ansotegui IJ, Melioli G, Canonica GW, Caraballo L, Villa E, Ebisawa M, Passalacqua G, Savi E, Ebo D, Gómez RM, et al. IgE allergy diagnostics and other relevant tests in allergy, a World Allergy Organization position paper. World Allergy Organ J (2020) 13:100080. [CrossRef]
- Wood RA, Kim JS, Lindblad R, Nadeau K, Henning AK, Dawson P, Plaut M, Sampson HA. A randomized, double-blind, placebo-controlled study of omalizumab combined with oral immunotherapy for the treatment of cow’s milk allergy. J Allergy Clin Immunol (2016) 137:1103-1110.e11. [CrossRef]
- Matricardi PM, Kleine-Tebbe J, Hoffmann HJ, Valenta R, Hilger C, Hofmaier S, Aalberse RC, Agache I, Asero R, Ballmer-Weber B, et al. EAACI Molecular Allergology User’s Guide. Pediatr Allergy Immunol (2016) 27 Suppl 23:1–250. [CrossRef]
- Zuberbier T, Aberer W, Asero R, Abdul Latiff AH, Baker D, Ballmer-Weber B, Bernstein JA, Bindslev-Jensen C, Brzoza Z, Buense Bedrikow R, et al. The EAACI/GA2LEN/EDF/WAO guideline for the definition, classification, diagnosis and management of urticaria. Allergy (2018) 73:1393–1414. [CrossRef]
- Ewan PW, Dugué P, Mirakian R, Dixon TA, Harper JN, Nasser SM. BSACI guidelines for the investigation of suspected anaphylaxis during general anaesthesia. Clinical & Experimental Allergy (2010) 40:15–31. [CrossRef]
- Gargano D, Appanna R, Santonicola A, De Bartolomeis F, Stellato C, Cianferoni A, Casolaro V, Iovino P. Food Allergy and Intolerance: A Narrative Review on Nutritional Concerns. Nutrients (2021) 13:1638. [CrossRef]
- Sicherer SH, Sampson HA. Food allergy: Epidemiology, pathogenesis, diagnosis, and treatment. J Allergy Clin Immunol (2014) 133:291–307; quiz 308. [CrossRef]
- Gupta RS, Warren CM, Smith BM, Jiang J, Blumenstock JA, Davis MM, Schleimer RP, Nadeau KC. Prevalence and Severity of Food Allergies Among US Adults. JAMA Netw Open (2019) 2:e185630. [CrossRef]
- Osborne NJ, Koplin JJ, Martin PE, Gurrin LC, Thiele L, Tang ML, Ponsonby A-L, Dharmage SC, Allen KJ, HealthNuts Study Investigators. The HealthNuts population-based study of paediatric food allergy: validity, safety and acceptability. Clin Exp Allergy (2010) 40:1516–1522. [CrossRef]
- Muir A, Falk GW. Eosinophilic Esophagitis: A Review. JAMA (2021) 326:1310–1318. [CrossRef]
- Dellon ES, Jensen ET, Martin CF, Shaheen NJ, Kappelman MD. Prevalence of eosinophilic esophagitis in the United States. Clin Gastroenterol Hepatol (2014) 12:589-596.e1. [CrossRef]
- Liacouras CA, Furuta GT, Hirano I, Atkins D, Attwood SE, Bonis PA, Burks AW, Chehade M, Collins MH, Dellon ES, et al. Eosinophilic esophagitis: Updated consensus recommendations for children and adults. Journal of Allergy and Clinical Immunology (2011) 128:3-20.e6. [CrossRef]
- Hirano I, Pandolfino JE, Boeckxstaens GE. Functional Lumen Imaging Probe for the Management of Esophageal Disorders: Expert Review From the Clinical Practice Updates Committee of the AGA Institute. Clin Gastroenterol Hepatol (2017) 15:325–334. [CrossRef]
- Lucendo AJ, Arias Á, Molina-Infante J. Efficacy of Proton Pump Inhibitor Drugs for Inducing Clinical and Histologic Remission in Patients With Symptomatic Esophageal Eosinophilia: A Systematic Review and Meta-Analysis. Clin Gastroenterol Hepatol (2016) 14:13-22.e1. [CrossRef]
- Boyce JA, Assa’ad A, Burks AW, Jones SM, Sampson HA, Wood RA, Plaut M, Cooper SF, Fenton MJ, Arshad SH, et al. Guidelines for the Diagnosis and Management of Food Allergy in the United States: Summary of the NIAID-Sponsored Expert Panel Report. Journal of Allergy and Clinical Immunology (2010) 126:1105–1118. [CrossRef]
- Barni S, Mori F, Giovannini M, Liotti L, Mastrorilli C, Pecoraro L, Saretta F, Castagnoli R, Arasi S, Caminiti L, et al. Allergic Proctocolitis: Literature Review and Proposal of a Diagnostic–Therapeutic Algorithm. Life (Basel) (2023) 13:1824. [CrossRef]
- Zubeldia-Varela E, Barker-Tejeda TC, Blanco-Pérez F, Infante S, Zubeldia JM, Pérez-Gordo M. Non-IgE-Mediated Gastrointestinal Food Protein-Induced Allergic Disorders. Clinical Perspectives and Analytical Approaches. Foods (2021) 10:. [CrossRef]
- Martin VM, Virkud YV, Seay H, Hickey A, Ndahayo R, Rosow R, Southwick C, Elkort M, Gupta B, Kramer E, et al. PROSPECTIVE ASSESSMENT OF PEDIATRICIAN-DIAGNOSED FOOD-PROTEIN INDUCED ALLERGIC PROCTOCOLITIS BY GROSS OR OCCULT BLOOD. J Allergy Clin Immunol Pract (2020) 8:1692-1699.e1. [CrossRef]
- Elizur A, Cohen M, Goldberg MR, Rajuan N, Cohen A, Leshno M, Katz Y. Cow’s milk associated rectal bleeding: a population based prospective study. Pediatr Allergy Immunol (2012) 23:766–770. [CrossRef]
- Mennini M, Fiocchi AG, Cafarotti A, Montesano M, Mauro A, Villa MP, Di Nardo G. Food protein-induced allergic proctocolitis in infants: Literature review and proposal of a management protocol. World Allergy Organ J (2020) 13:100471. [CrossRef]
- Nowak-Wegrzyn A, Warren CM, Brown-Whitehorn T, Cianferoni A, Schultz-Matney F, Gupta RS. Food protein-induced enterocolitis syndrome in the US population-based study. J Allergy Clin Immunol (2019) 144:1128–1130. [CrossRef]
- Caubet J-C, Szajewska H, Shamir R, Nowak-Węgrzyn A. Non-IgE-mediated gastrointestinal food allergies in children. Pediatr Allergy Immunol (2017) 28:6–17. doi: le.
- Lebwohl B, Rubio-Tapia A. Epidemiology, Presentation, and Diagnosis of Celiac Disease. Gastroenterology (2021) 160:63–75. [CrossRef]
- Al-Toma A, Volta U, Auricchio R, Castillejo G, Sanders DS, Cellier C, Mulder CJ, Lundin KEA. European Society for the Study of Coeliac Disease (ESsCD) guideline for coeliac disease and other gluten-related disorders. United European Gastroenterol J (2019) 7:583–613. [CrossRef]
- Alkalay MJ. Nutrition in Patients with Lactose Malabsorption, Celiac Disease, and Related Disorders. Nutrients (2021) 14:2. [CrossRef]
- Hadithi M, von Blomberg BME, Crusius JBA, Bloemena E, Kostense PJ, Meijer JWR, Mulder CJJ, Stehouwer CDA, Peña AS. Accuracy of Serologic Tests and HLA-DQ Typing for Diagnosing Celiac Disease. Ann Intern Med (2007) 147:294–302. [CrossRef]
- Singh P, Arora A, Strand TA, Leffler DA, Catassi C, Green PH, Kelly CP, Ahuja V, Makharia GK. Global Prevalence of Celiac Disease: Systematic Review and Meta-analysis. Clinical Gastroenterology and Hepatology (2018) 16:823-836.e2. [CrossRef]
- Lebwohl B, Rubio-Tapia A. Epidemiology, Presentation, and Diagnosis of Celiac Disease. Gastroenterology (2021) 160:63–75. [CrossRef]
- Ludvigsson JF, Murray JA. Epidemiology of Celiac Disease. Gastroenterol Clin North Am (2019) 48:1–18. [CrossRef]
- Rubio-Tapia A, Hill ID, Semrad C, Kelly CP, Greer KB, Limketkai BN, Lebwohl B. American College of Gastroenterology Guidelines Update: Diagnosis and Management of Celiac Disease. Official journal of the American College of Gastroenterology | ACG (2023) 118:59. [CrossRef]
- SALMI T, HERVONEN K. Current Concepts of Dermatitis Herpetiformis. Acta Derm Venereol (2020) 100:5664. [CrossRef]
- Collin P, Salmi TT, Hervonen K, Kaukinen K, Reunala T. Dermatitis herpetiformis: a cutaneous manifestation of coeliac disease. Annals of Medicine (2017) 49:23–31. [CrossRef]
- Nguyen CN, Kim S-J. Dermatitis Herpetiformis: An Update on Diagnosis, Disease Monitoring, and Management. Medicina (Kaunas) (2021) 57:843. [CrossRef]
- Antiga E, Maglie R, Quintarelli L, Verdelli A, Bonciani D, Bonciolini V, Caproni M. Dermatitis Herpetiformis: Novel Perspectives. Front Immunol (2019) 10:1290. [CrossRef]
- Reunala T, Hervonen K, Salmi T. Dermatitis Herpetiformis: An Update on Diagnosis and Management. Am J Clin Dermatol (2021) 22:329–338. [CrossRef]
- Mansikka E, Hervonen K, Kaukinen K, Collin P, Huhtala H, Reunala T, Salmi T. Prognosis of Dermatitis Herpetiformis Patients with and without Villous Atrophy at Diagnosis. Nutrients (2018) 10:641. [CrossRef]
- Collin P, Salmi TT, Hervonen K, Kaukinen K, Reunala T. Dermatitis herpetiformis: a cutaneous manifestation of coeliac disease. Ann Med (2017) 49:23–31. [CrossRef]
- Caproni M, Antiga E, Melani L, Fabbri P, Italian Group for Cutaneous Immunopathology. Guidelines for the diagnosis and treatment of dermatitis herpetiformis. J Eur Acad Dermatol Venereol (2009) 23:633–638. [CrossRef]
- Feuille E, Nowak-Węgrzyn A. Food Protein-Induced Enterocolitis Syndrome, Allergic Proctocolitis, and Enteropathy. Curr Allergy Asthma Rep (2015) 15:50. [CrossRef]
- Jenkins HR, Pincott JR, Soothill JF, Milla PJ, Harries JT. Food allergy: the major cause of infantile colitis. Arch Dis Child (1984) 59:326–329.
- Caubet JC, Ford LS, Sickles L, Järvinen KM, Sicherer SH, Sampson HA, Nowak-Węgrzyn A. Clinical features and resolution of food protein-induced enterocolitis syndrome: 10-year experience. J Allergy Clin Immunol (2014) 134:382–389. [CrossRef]
- Fernandes BN, Boyle RJ, Gore C, Simpson A, Custovic A. Food protein-induced enterocolitis syndrome can occur in adults. J Allergy Clin Immunol (2012) 130:1199–1200. [CrossRef]
- Koc AS, Sucu A, Celik U. A different clinical presentation of Heiner syndrome: The case of diffuse alveolar hemorrhage causing massive hemoptysis and hematemesis. Respir Med Case Rep (2019) 26:206–208. [CrossRef]
- Arasi S, Mastrorilli C, Pecoraro L, Giovannini M, Mori F, Barni S, Caminiti L, Castagnoli R, Liotti L, Saretta F, et al. Heiner Syndrome and Milk Hypersensitivity: An Updated Overview on the Current Evidence. Nutrients (2021) 13:1710. [CrossRef]
- Lee JY, Park M, Jung JH, Kim SY, Kim YH, Hahn SM, Kim S, Lee M-J, Shim HS, Sohn MH, et al. Children with Heiner Syndrome: A Single-Center Experience. Children (Basel) (2021) 8:1110. [CrossRef]
- Calvani M, Anania C, Bianchi A, D’Auria E, Cardinale F, Votto M, Martelli A, Tosca M, Chiappini E, Brambilla I, et al. Update on Food protein-induced enterocolitis syndrome (FPIES). Acta Biomed (2021) 92:e2021518. [CrossRef]
- Nowak-Węgrzyn A, Chehade M, Groetch ME, Spergel JM, Wood RA, Allen K, Atkins D, Bahna S, Barad AV, Berin C, et al. International consensus guidelines for the diagnosis and management of food protein–induced enterocolitis syndrome: Executive summary—Workgroup Report of the Adverse Reactions to Foods Committee, American Academy of Allergy, Asthma & Immunology. Journal of Allergy and Clinical Immunology (2017) 139:1111-1126.e4. [CrossRef]
- Mehr S, Frith K, Campbell DE. Epidemiology of food protein-induced enterocolitis syndrome. Curr Opin Allergy Clin Immunol (2014) 14:208–216. [CrossRef]
- Tuck CJ, Biesiekierski JR, Schmid-Grendelmeier P, Pohl D. Food Intolerances. Nutrients (2019) 11:1684. [CrossRef]
- Misselwitz B, Butter M, Verbeke K, Fox MR. Update on lactose malabsorption and intolerance: pathogenesis, diagnosis and clinical management. Gut (2019) 68:2080–2091. [CrossRef]
- Catanzaro R, Sciuto M, Marotta F. Lactose intolerance: An update on its pathogenesis, diagnosis, and treatment. Nutrition Research (2021) 89:23–34. [CrossRef]
- Bayless TM, Brown E, Paige DM. Lactase Non-persistence and Lactose Intolerance. Curr Gastroenterol Rep (2017) 19:23. [CrossRef]
- Deng Y, Misselwitz B, Dai N, Fox M. Lactose Intolerance in Adults: Biological Mechanism and Dietary Management. Nutrients (2015) 7:8020–8035. [CrossRef]
- Enattah NS, Sahi T, Savilahti E, Terwilliger JD, Peltonen L, Järvelä I. Identification of a variant associated with adult-type hypolactasia. Nat Genet (2002) 30:233–237. [CrossRef]
- Simrén M, Stotzer P. Use and abuse of hydrogen breath tests. Gut (2006) 55:297–303. [CrossRef]
- Simrén M, Barbara G, Flint HJ, Spiegel BMR, Spiller RC, Vanner S, Verdu EF, Whorwell PJ, Zoetendal EG. Intestinal microbiota in functional bowel disorders: a Rome foundation report. Gut (2013) 62:159–176. [CrossRef]
- Jo IH, Paik C-N, Kim Y-J, Lee JM, Choi SY, Hong KP. Lactase Deficiency Diagnosed by Endoscopic Biopsy-based Method is Associated With Positivity to Glucose Breath Test. J Neurogastroenterol Motil (2023) 29:85–93. [CrossRef]
- Swallow DM. Genetics of lactase persistence and lactose intolerance. Annu Rev Genet (2003) 37:197–219. [CrossRef]
- Shaukat A, Levitt MD, Taylor BC, MacDonald R, Shamliyan TA, Kane RL, Wilt TJ. Systematic review: effective management strategies for lactose intolerance. Ann Intern Med (2010) 152:797–803. [CrossRef]
- Roszkowska A, Pawlicka M, Mroczek A, Bałabuszek K, Nieradko-Iwanicka B. Non-Celiac Gluten Sensitivity: A Review. Medicina (Kaunas) (2019) 55:222. [CrossRef]
- Catassi C, Elli L, Bonaz B, Bouma G, Carroccio A, Castillejo G, Cellier C, Cristofori F, de Magistris L, Dolinsek J, et al. Diagnosis of Non-Celiac Gluten Sensitivity (NCGS): The Salerno Experts’ Criteria. Nutrients (2015) 7:4966–4977. [CrossRef]
- Carroccio A, Mansueto P, Iacono G, Soresi M, D’Alcamo A, Cavataio F, Brusca I, Florena AM, Ambrosiano G, Seidita A, et al. Non-Celiac Wheat Sensitivity Diagnosed by Double-Blind Placebo-Controlled Challenge: Exploring a New Clinical Entity. Official journal of the American College of Gastroenterology | ACG (2012) 107:1898. [CrossRef]
- Uhde M, Ajamian M, Caio G, De Giorgio R, Indart A, Green PH, Verna EC, Volta U, Alaedini A. Intestinal cell damage and systemic immune activation in individuals reporting sensitivity to wheat in the absence of coeliac disease. Gut (2016) 65:1930–1937. [CrossRef]
- Skodje GI, Sarna VK, Minelle IH, Rolfsen KL, Muir JG, Gibson PR, Veierød MB, Henriksen C, Lundin KEA. Fructan, Rather Than Gluten, Induces Symptoms in Patients With Self-Reported Non-Celiac Gluten Sensitivity. Gastroenterology (2018) 154:529-539.e2. [CrossRef]
- Ensari A, Marsh MN. Diagnosing celiac disease: A critical overview. Turk J Gastroenterol (2019) 30:389–397. [CrossRef]
- Singh SK, Sarma MS. Hereditary fructose intolerance: A comprehensive review. World J Clin Pediatr (2022) 11:321–329. [CrossRef]
- Debray F-G, Seyssel K, Fadeur M, Tappy L, Paquot N, Tran C. Effect of a high fructose diet on metabolic parameters in carriers for hereditary fructose intolerance. Clinical Nutrition (2021) 40:4246–4254. [CrossRef]
- Adamowicz M, Płoski R, Rokicki D, Morava E, Giżewska M, Mierzewska H, Pollak A, Lefeber DJ, Wevers RA, Pronicka E. Transferrin hypoglycosylation in hereditary fructose intolerance: Using the clues and avoiding the pitfalls. Journal of Inherited Metabolic Disease (2007) 30:407. [CrossRef]
- Ali M, Rellos P, Cox TM. Hereditary fructose intolerance. J Med Genet (1998) 35:353–365. [CrossRef]
- Tolan DR, Brooks CC. Molecular analysis of common aldolase B alleles for hereditary fructose intolerance in North Americans. Biochem Med Metab Biol (1992) 48:19–25. [CrossRef]
- Ebert K, Witt H. Fructose malabsorption. Mol Cell Pediatr (2016) 3:10. [CrossRef]
- Hammer HF, Fox MR, Keller J, Salvatore S, Basilisco G, Hammer J, Lopetuso L, Benninga M, Borrelli O, Dumitrascu D, et al. European guideline on indications, performance, and clinical impact of hydrogen and methane breath tests in adult and pediatric patients: European Association for Gastroenterology, Endoscopy and Nutrition, European Society of Neurogastroenterology and Motility, and European Society for Paediatric Gastroenterology Hepatology and Nutrition consensus. United European Gastroenterol J (2021) 10:15–40. [CrossRef]
- Komericki P, Akkilic-Materna M, Strimitzer T, Weyermair K, Hammer HF, Aberer W. Oral xylose isomerase decreases breath hydrogen excretion and improves gastrointestinal symptoms in fructose malabsorption – a double-blind, placebo-controlled study. Alimentary Pharmacology & Therapeutics (2012) 36:980–987. [CrossRef]
- Gibson PR, Shepherd SJ. Evidence-based dietary management of functional gastrointestinal symptoms: The FODMAP approach. Journal of Gastroenterology and Hepatology (2010) 25:252–258. [CrossRef]
- Tuck CJ, Biesiekierski JR, Schmid-Grendelmeier P, Pohl D. Food Intolerances. Nutrients (2019) 11:1684. [CrossRef]
- Frissora CL, Rao SSC. Sucrose intolerance in adults with common functional gastrointestinal symptoms. Proc (Bayl Univ Med Cent) (2022) 35:790–793. [CrossRef]
- Treem WR, McAdams L, Stanford L, Kastoff G, Justinich C, Hyams J. Sacrosidase therapy for congenital sucrase-isomaltase deficiency. J Pediatr Gastroenterol Nutr (1999) 28:137–142. [CrossRef]
- Robayo-Torres CC, Opekun AR, Quezada-Calvillo R, Villa X, Smith EO, Navarrete M, Baker SS, Nichols BL. 13C-breath tests for sucrose digestion in congenital sucrase isomaltase-deficient and sacrosidase-supplemented patients. J Pediatr Gastroenterol Nutr (2009) 48:412–418. [CrossRef]
- Latorre-Moratalla ML, Comas-Basté O, Bover-Cid S, Vidal-Carou MC. Tyramine and histamine risk assessment related to consumption of dry fermented sausages by the Spanish population. Food and Chemical Toxicology (2017) 99:78–85. [CrossRef]
- Comas-Basté O, Sánchez-Pérez S, Veciana-Nogués MT, Latorre-Moratalla M, Vidal-Carou M del C. Histamine Intolerance: The Current State of the Art. Biomolecules (2020) 10:1181. [CrossRef]
- Schwelberger HG, Feurle J, Houen G. Mapping of the binding sites of human diamine oxidase (DAO) monoclonal antibodies. Inflamm Res (2018) 67:245–253. [CrossRef]
- Schnedl WJ, Lackner S, Enko D, Schenk M, Holasek SJ, Mangge H. Evaluation of symptoms and symptom combinations in histamine intolerance. Intest Res (2019) 17:427–433. [CrossRef]
- Reese I, Ballmer-Weber B, Beyer K, Dölle-Bierke S, Kleine-Tebbe J, Klimek L, Lämmel S, Lepp U, Saloga J, Schäfer C, et al. Guideline on management of suspected adverse reactions to ingested histamine: Guideline of the German Society for Allergology and Clinical Immunology (DGAKI), the Society for Pediatric Allergology and Environmental Medicine (GPA), the Medical Association of German Allergologists (AeDA) as well as the Swiss Society for Allergology and Immunology (SGAI) and the Austrian Society for Allergology and Immunology (ÖGAI). Allergologie Select (2021) 5:305. [CrossRef]
- Hasler WL, Grabauskas G, Singh P, Owyang C. Mast cell mediation of visceral sensation and permeability in irritable bowel syndrome. Neurogastroenterol Motil (2022) 34:e14339. [CrossRef]
- Schnedl WJ, Schenk M, Lackner S, Enko D, Mangge H, Forster F. Diamine oxidase supplementation improves symptoms in patients with histamine intolerance. Food Sci Biotechnol (2019) 28:1779–1784. [CrossRef]
- Maintz L, Novak N. Histamine and histamine intolerance. Am J Clin Nutr (2007) 85:1185–1196. [CrossRef]
- Ispiryan L, Zannini E, Arendt EK. FODMAP modulation as a dietary therapy for IBS: Scientific and market perspective. Comprehensive Reviews in Food Science and Food Safety (2022) 21:1491–1516. [CrossRef]
- Morariu I-D, Avasilcai L, Vieriu M, Lupu VV, Morariu B-A, Lupu A, Morariu P-C, Pop O-L, Starcea IM, Trandafir L. Effects of a Low-FODMAP Diet on Irritable Bowel Syndrome in Both Children and Adults—A Narrative Review. Nutrients (2023) 15:2295. [CrossRef]
- Lenhart A, Chey WD. A Systematic Review of the Effects of Polyols on Gastrointestinal Health and Irritable Bowel Syndrome. Adv Nutr (2017) 8:587–596. [CrossRef]
- Sultan N, Varney JE, Halmos EP, Biesiekierski JR, Yao CK, Muir JG, Gibson PR, Tuck CJ. How to Implement the 3-Phase FODMAP Diet Into Gastroenterological Practice. J Neurogastroenterol Motil (2022) 28:343–356. [CrossRef]
- Bellini M, Tonarelli S, Nagy AG, Pancetti A, Costa F, Ricchiuti A, de Bortoli N, Mosca M, Marchi S, Rossi A. Low FODMAP Diet: Evidence, Doubts, and Hopes. Nutrients (2020) 12:148. [CrossRef]
- Gwioździk W, Krupa-Kotara K, Całyniuk B, Helisz P, Grajek M, Głogowska-Ligus J. Traditional, Vegetarian, or Low FODMAP Diets and Their Relation to Symptoms of Eating Disorders: A Cross-Sectional Study among Young Women in Poland. Nutrients (2022) 14:4125. [CrossRef]
- So D, Loughman A, Staudacher HM. Effects of a low FODMAP diet on the colonic microbiome in irritable bowel syndrome: a systematic review with meta-analysis. Am J Clin Nutr (2022) 116:943–952. [CrossRef]
- Staudacher HM, Lomer MCE, Farquharson FM, Louis P, Fava F, Franciosi E, Scholz M, Tuohy KM, Lindsay JO, Irving PM, et al. A Diet Low in FODMAPs Reduces Symptoms in Patients With Irritable Bowel Syndrome and A Probiotic Restores Bifidobacterium Species: A Randomized Controlled Trial. Gastroenterology (2017) 153:936–947. [CrossRef]
- Oka P, Parr H, Barberio B, Black CJ, Savarino EV, Ford AC. Global prevalence of irritable bowel syndrome according to Rome III or IV criteria: a systematic review and meta-analysis. The Lancet Gastroenterology & Hepatology (2020) 5:908–917. [CrossRef]
- Lacy BE, Mearin F, Chang L, Chey WD, Lembo AJ, Simren M, Spiller R. Bowel Disorders. Gastroenterology (2016) 150:1393-1407.e5. [CrossRef]
- Ford AC, Sperber AD, Corsetti M, Camilleri M. Irritable bowel syndrome. The Lancet (2020) 396:1675–1688. [CrossRef]
- Ford AC, Forman D, Bailey AG, Axon ATR, Moayyedi P. Irritable bowel syndrome: a 10-yr natural history of symptoms and factors that influence consultation behavior. Am J Gastroenterol (2008) 103:1229–1239; quiz 1240. [CrossRef]
- Yarandi SS, Nasseri-Moghaddam S, Mostajabi P, Malekzadeh R. Overlapping gastroesophageal reflux disease and irritable bowel syndrome: Increased dysfunctional symptoms. World J Gastroenterol (2010) 16:1232–1238. [CrossRef]
- Ford AC, Moayyedi P, Lacy BE, Lembo AJ, Saito YA, Schiller LR, Soffer EE, Spiegel BMR, Quigley EMM, Task Force on the Management of Functional Bowel Disorders. American College of Gastroenterology monograph on the management of irritable bowel syndrome and chronic idiopathic constipation. Am J Gastroenterol (2014) 109 Suppl 1:S2-26; quiz S27. [CrossRef]
- Matheis A, Martens U, Kruse J, Enck P. Irritable bowel syndrome and chronic pelvic pain: A singular or two different clinical syndrome? World J Gastroenterol (2007) 13:3446–3455. [CrossRef]
- Barsky AJ. Assessing the New DSM-5 Diagnosis of Somatic Symptom Disorder. Psychosom Med (2016) 78:2–4. [CrossRef]
- Koloski NA, Jones M, Weltman M, Kalantar J, Bone C, Gowryshankar A, Walker MM, Talley NJ. Identification of early environmental risk factors for irritable bowel syndrome and dyspepsia. Neurogastroenterol Motil (2015) 27:1317–1325. [CrossRef]
- Biesiekierski JR, Peters SL, Newnham ED, Rosella O, Muir JG, Gibson PR. No effects of gluten in patients with self-reported non-celiac gluten sensitivity after dietary reduction of fermentable, poorly absorbed, short-chain carbohydrates. Gastroenterology (2013) 145:320-328.e1–3. [CrossRef]
- Czaja-Bulsa G. Non coeliac gluten sensitivity - A new disease with gluten intolerance. Clin Nutr (2015) 34:189–194. [CrossRef]
- Enck P, Aziz Q, Barbara G, Farmer AD, Fukudo S, Mayer EA, Niesler B, Quigley EMM, Rajilić-Stojanović M, Schemann M, et al. Irritable bowel syndrome. Nat Rev Dis Primers (2016) 2:16014. [CrossRef]
- Hamer HM, Jonkers D, Venema K, Vanhoutvin S, Troost FJ, Brummer R-J. Review article: the role of butyrate on colonic function. Aliment Pharmacol Ther (2008) 27:104–119. [CrossRef]
- Rajilić-Stojanović M, de Vos WM. The first 1000 cultured species of the human gastrointestinal microbiota. FEMS Microbiol Rev (2014) 38:996–1047. [CrossRef]
- Spiller RC. Inflammation as a basis for functional GI disorders. Best Pract Res Clin Gastroenterol (2004) 18:641–661. [CrossRef]
- Pimentel M, Gunsalus R, Rao S, Zhang H. Methanogens in Human Health and Disease. Am J Gastroenterol (2012) 1:28–33. [CrossRef]
- Rajilić-Stojanović M, Biagi E, Heilig HGHJ, Kajander K, Kekkonen RA, Tims S, de Vos WM. Global and deep molecular analysis of microbiota signatures in fecal samples from patients with irritable bowel syndrome. Gastroenterology (2011) 141:1792–1801. [CrossRef]
- Attaluri A, Jackson M, Paulson J, Rao SS. Methanogenic flora is associated with altered colonic transit but not stool characteristics in constipation without IBS. Am J Gastroenterol (2010) 105:10.1038/ajg.2009.655. [CrossRef]
- Longstreth GF, Thompson WG, Chey WD, Houghton LA, Mearin F, Spiller RC. Functional bowel disorders. Gastroenterology (2006) 130:1480–1491. [CrossRef]
- Drossman DA, Tack J, Ford AC, Szigethy E, Törnblom H, Van Oudenhove L. Neuromodulators for Functional Gastrointestinal Disorders (Disorders of Gut-Brain Interaction): A Rome Foundation Working Team Report. Gastroenterology (2018) 154:1140-1171.e1. [CrossRef]
- Lacy BE, Mearin F, Chang L, Chey WD, Lembo AJ, Simren M, Spiller R. Bowel Disorders. Gastroenterology (2016) 150:1393-1407.e5. [CrossRef]
- Quigley EMM. Prebiotics and Probiotics in Digestive Health. Clin Gastroenterol Hepatol (2019) 17:333–344. [CrossRef]
| Pathology | Disorder | Key features | Most common causal foods |
|---|---|---|---|
| IgE-mediated (acute onset) | Acute urticaria/angioedema | Food commonly causes acute (20%) but rarely chronic urticaria | Cow milk, gluten, eggs, wheat, beans, soybean, nuts, and seafood |
| Contact urticaria | Direct skin contact results in lesions. Histamine release, in rare cases, can cause urticaria. (I change the sentence) (nonimmunologic) |
Multiple | |
| Anaphylaxis | Rapidly progressive, multiple organs system reactions can include cardiovascular collapse | Any but more commonly peanut, Tree nuts, shellfish, fish, milk, and egg | |
| Food-associated, exercise-induced anaphylaxis | Food triggers anaphylaxis only if ingestion is followed temporally by exercise | Wheat, shellfish, and celery are most often described | |
| Oral allergy syndrome (pollen-associated food allergy syndrome) | Pruritus and mild edema are confined to the oral cavity and uncommonly progress beyond the mouth (w7%) and rarely to anaphylaxis (1% to 2%). It might increase after the pollen season. | Raw fruit/vegetables; cooked forms tolerated; examples of relationships: birch (apple, peach, pear, carrot), ragweed (melons) | |
| Immediate gastrointestinal hypersensitivity | Immediate vomiting, pain | Cow milk, gluten, eggs, wheat, beans, soybean, nuts, and seafood | |
| Combined IgE and cell-mediated (delayed onset/chronic) | Atopic dermatitis | Associated with food allergy in 35% of children with moderate-to-severe rash | Major allergens, particularly egg, milk |
| Eosinophilic esophagitis | Symptoms might include feeding disorders, reflux symptoms, vomiting, dysphagia, and food impaction. | Multiple | |
| Eosinophilic gastroenteritis | Vary on site(s)/degree of eosinophilic inflammation; might include ascites, weight loss, edema, obstruction | Multiple | |
| Cell-mediated (delayed onset/chronic) | Food protein-induced enterocolitis syndrome Cow’s milk, soy, rice, oat, meat | Primarily affects infants; chronic exposure: emesis, diarrhea, poor growth, lethargy; re-exposure after restriction: emesis, diarrhea, hypotension (15%) 2 hours after ingestion | Cow’s milk, soy, rice, oat, meat |
| Food protein induced allergic proctocolitis | Mucus-laden, bloody stools in infants Milk (through breast-feeding) | Milk (through breast-feeding) | |
| Allergic contact dermatitis | Often occupational because of chemical moieties, oleoresins. Systemic contact dermatitis is a rare variant because of ingestion | Spices, fruits, vegetables | |
| Heiner syndrome | Pulmonary infiltrates, failure to thrive, iron deficiency anemia | Cow’s milk |
|
Microbiota species increased in IBS -Enterobacteriaceae -Veillonella -Streptococcus* -Dorea -Blautia -Roseburia -Ruminococcus -Methanobrevibacter‡ |
|
Microbiota species decreased in IBS -Bifidobacterium -Collinsella -Streptococcus‡ -Faecalibacterium -Christensenellaceae -Clostridiales -Methanobrevibacter§ |
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2025 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (http://creativecommons.org/licenses/by/4.0/).