1. Introduction
Psoriatic arthritis (PsA) is a chronic inflammatory disease associated with psoriasis (Pso), affecting both peripheral joints and the axial skeleton, often leading to disability. The prevalence of psoriasis ranges between 0.5% and 5%, and PsA develops in 6–42% of psoriasis patients [
1,
2,
3].
PsA is characterized by heterogeneous musculoskeletal involvement and diverse clinical phenotypes. In 15% of patients, musculoskeletal manifestations occur in the absence of psoriasis [
3,
4]. Unlike rheumatoid arthritis (RA), PsA is often associated with milder joint pain and may present with normal acute phase reactants in nearly half of patients [
4,
5].
PsA can cause a wide range of radiological changes, including inflammatory, erosive, and osteoproliferative features, primarily in mechanically stressed regions. Due to its varied presentation, PsA is frequently misdiagnosed, leading to years of delay in diagnosis. A recent study reported that 96% of PsA patients received at least one incorrect diagnosis before their PsA diagnosis [
6]. Common misdiagnoses include osteoarthritis and axial skeletal pathologies [
6].
With recent advances in PsA pathogenesis, novel pharmacologic treatments have led to improved remission rates [
7,
8]. However, studies have shown that healthcare costs begin increasing approximately five years before diagnosis, with MSK surgeries contributing significantly to these costs [
9,
10,
11,
12,
13]. While previous studies have reported MSK surgery rates ranging between 2% and 48% in PsA patients, most focused on post-diagnosis surgery, leaving data from the pre-diagnosis period limited [
12,
13,
14,
15,
16,
17,
18,
19,
20].
Given the high frequency of MSK surgeries before PsA diagnosis, we hypothesize that delayed diagnosis may contribute to unnecessary surgical interventions. This study aims to compare the annual frequency of MSK surgeries in the period of diagnostic delay with that of the post-diagnosis period in PsA patients.
2. Materials and Methods
2.1. Study Design and Patients
This is a retrospective cohort study comparing the annual frequency of musculoskeletal operations in PsA patients in the symptomatic pre-diagnosis period compared to the post-diagnosis period. The study included 84 patients with PsA who met the CASPAR classification criteria and were followed up in the Rheumatology Clinic of Inonu University, Faculty of Medicine. Patients younger than 18 years and older than 65 years were excluded. Approval for the study was obtained from the Inonu University Faculty of Medicine Clinical Research Ethics Committee (Ethics Committee no: 2019/133). Informed consent was obtained from the patients participating in the study.
2.2. Collection of Musculoskeletal Surgery Data and Other Clinical Data
Demographic, medical, laboratory, radiological, and medical treatment data of the patients were recorded in the patient and follow-up files. Records of all previous musculoskeletal operations were obtained from the patient's clinical history and medical records. The pre-diagnosis symptomatic period was considered as the period of diagnostic delay. The total number of MSK operations in the pre-diagnosis period was divided by the number of years in that period to calculate the annual surgery rate. Similarly, the number of MSK operations in the post-diagnosis period was divided by the year of diagnosis, and the annual number of operations in the post-diagnosis period was calculated.
2.3. Statistical Analysis
Data were analyzed using SPSS software version 26 (SPSS Inc., Chicago, IL, USA). Descriptive statistics were used to summarise the data. The conformity of the variables to normal distribution was evaluated using the Kolmogorov-Smirnov test, and homogeneity of variance was evaluated using Levene's test. Categorical variables were expressed as number-percentage. Continuous variables with normal distribution were expressed as mean ± standard deviation (SD), while those without normal distribution were reported as median (minimum-maximum). McNemar Test was used to analyze categorical variables. In addition, Wilcoxon Signed Rank Test was used to compare ordinal nonparametric data between dependent groups. Statistical significance was set at a p-value of 0.05, and the results were supported by confidence intervals.
3. Results
3.1. Demographic Data or Baseline Characteristics
The study included 84 PsA patients. Demographic and clinical characteristics of the patients are summarised in
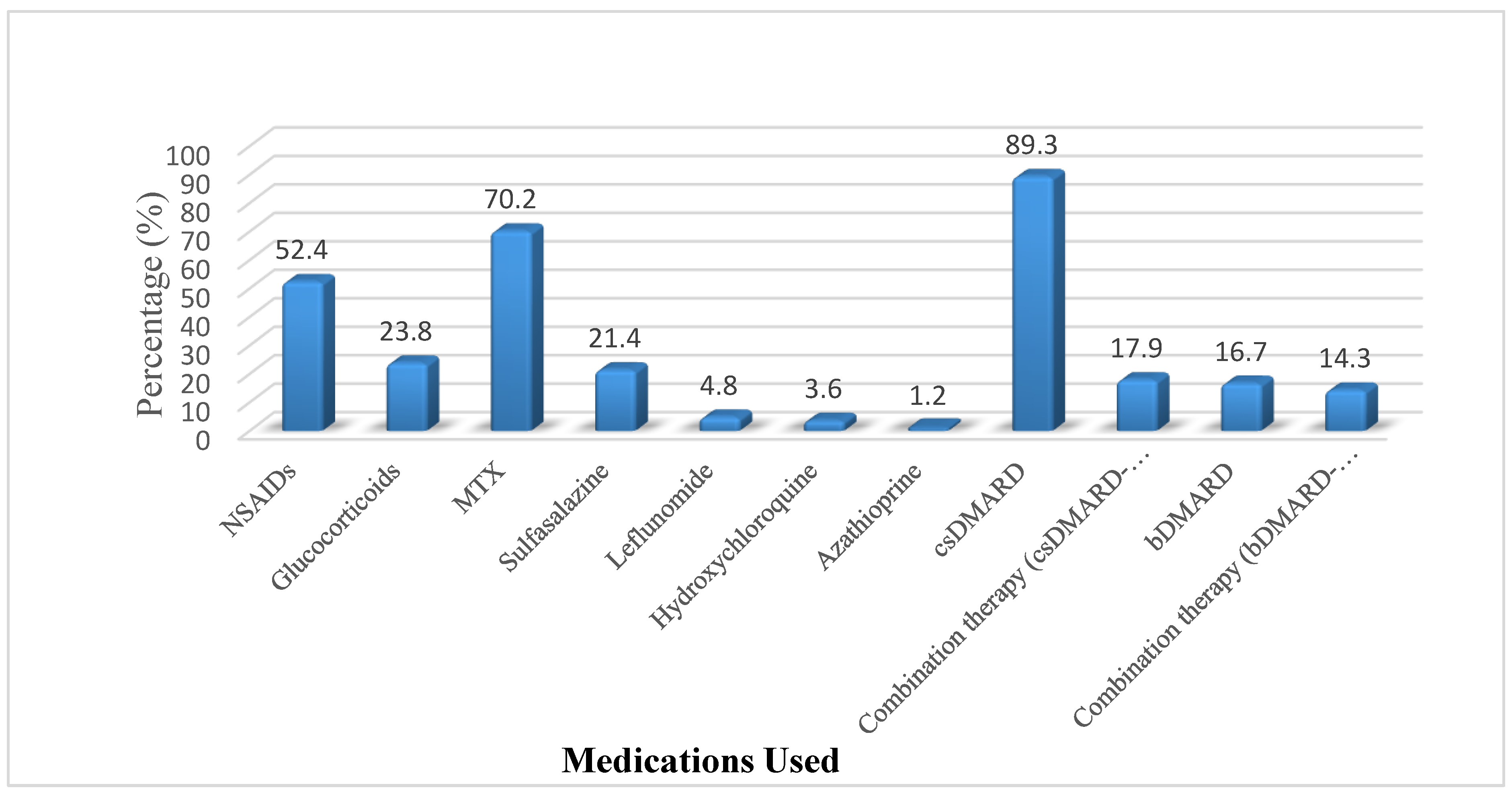
Table 1. The mean age of the patients was 47±11 years. 88.1% of the patients were female and 11.9% were male. PsA patients had a mean duration of diagnosis of 3.39 years. There was a mean diagnostic delay of 7.49 years. Both axial and peripheral involvement was present in 76.2% of patients. While 41.7% of the patients had psoriasis themselves, 67.9% had a family history of psoriasis. Nonsteroidal anti-inflammatory drugs (NSAIDs) were given in 52.4%, glucocorticoids in 23.8%, MTX in 70.2%, sulfasalazine in 21.4%, and biological disease-modifying drugs (bDMARDs) in 16.7% (
Figure 1).
3.2. MSK operation data:
A total of 23 patients (27.4%) had at least one MSK operation in the symptomatic period before and after the diagnosis (
Table 1). PsA patients had undergone a total of 39 operations, 36 in the pre-diagnosis symptomatic period and 3 in the post-diagnosis period. During the pre-diagnosis symptomatic period, 25% of the patients and 3.6% during the post-diagnosis treatment period had at least 1 MSK operation (
Table 2). During this period, one patient underwent five MSK surgeries, while two patients underwent three surgeries each. Only 1 of 21 patients who had undergone MSK operation during the delayed diagnosis period had undergone MSK operation again in the post-diagnosis period (medical treatment). The 2 patients who underwent surgery after the diagnosis did not have any MSK operation during the delayed diagnosis period.
The mean number of MSK operations in the pre-diagnosis symptomatic period of PsA patients was significantly higher than in the post-diagnosis period (<0.001, Z=-3.952). In addition, since the pre-diagnosis symptomatic period was longer than the post-diagnosis period, statistical tests were performed again after calculating the mean number of MSK operations per unit time (year). Thus, it was possible to compare the number of MSK operations per unit time. In this way, the mean number of MSK operations per year was significantly higher in the symptomatic period before diagnosis than in the treatment period after diagnosis (P=0.001, Z=-3.182) (
Table 2). No significant correlation was found between the number of operations and patient age, PsA symptom duration, PsA diagnosis duration and Pso rash duration among patients who underwent MSK operation during the diagnostic delay period (p>0.05 for all).
Demographic, clinical and treatment characteristics of patients with and without MSK operation were compared (
Table 3). The frequency of MTX intake was significantly higher in the group with MSK operation compared to the group without MSK operation (P=0.040). There was no significant difference between the 2 groups in terms of other data (p>0.05 for all) (
Table 3).
3.3. Subgroup Analyses
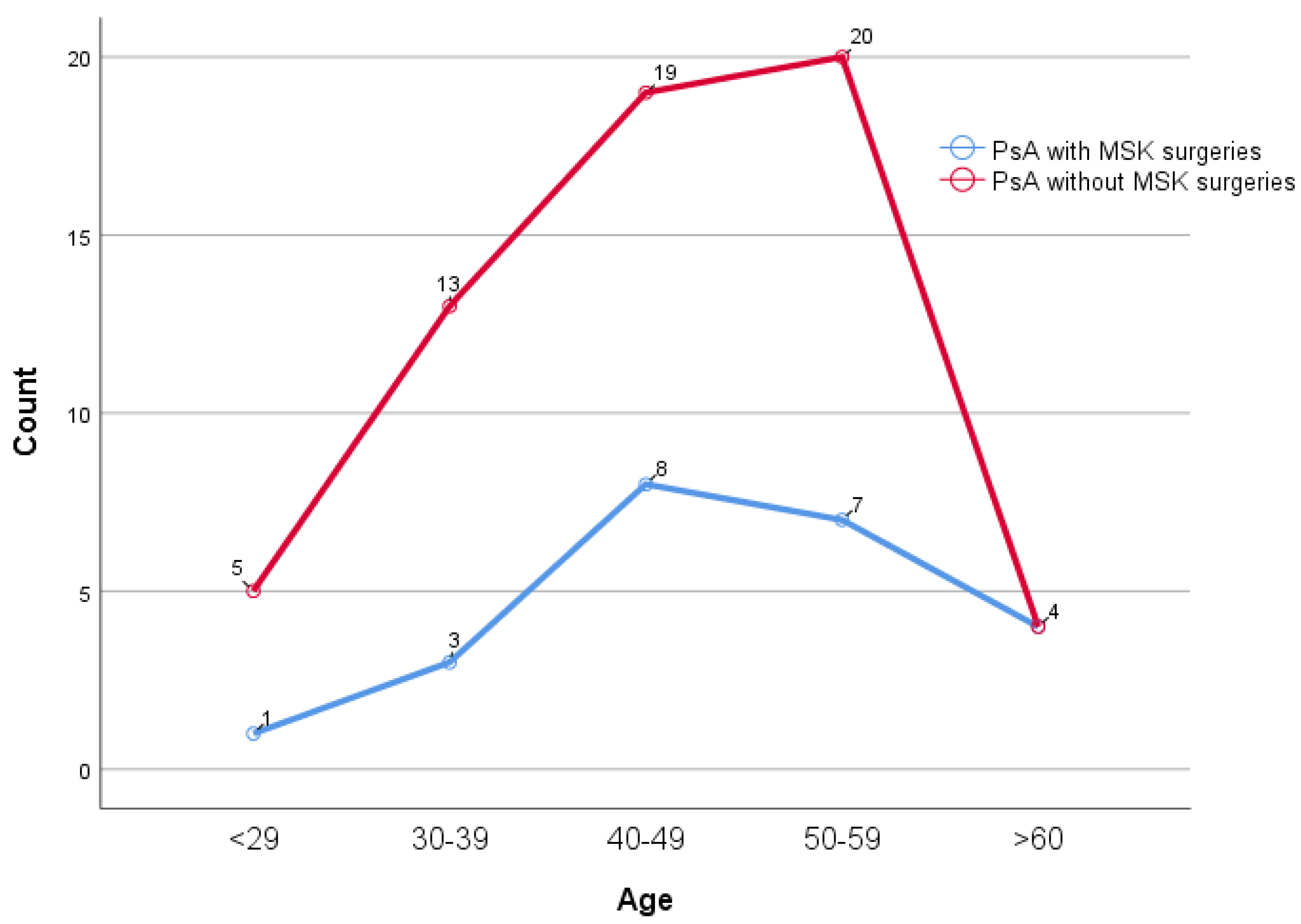
There was no significant difference in the number of MSK operations between age decades (p=0.677) (
Figure 2). The significant change observed in the presence of MSK surgeries before and after the diagnosis is especially evident in the female patient group (p<0.001, 25.68% to 4.05% decrease). In female PsA patients, the number of operations during the delayed diagnosis period was significantly higher than in the post-diagnosis period (P<0.001, Z=-3.748). The number of operations per year in the period of delayed diagnosis was significantly higher in female PsA patients than in the post-diagnosis period (P=0.001, Z=-2.923). In contrast, in male PsA patients, there was no significant difference between the pre-diagnosis symptomatic period and the post-diagnosis period in terms of the number of operations and the number of operations per year (p>0.005 for both) (
Table 4). In patients with axial + peripheral joint involvement, the change in MSK surgery rates before and after diagnosis was statistically significant (p=0.001, 25.00% vs 3.13%). Although a decrease in the post-diagnosis operation rates was also observed in patients with axial and peripheral involvement, this decrease did not reach statistical significance in axial involvement (p=0.250). (
Table 4). There was no association between psoriatic rash or nail involvement and MSK surgery (for all, p>0.05). In patients with a family history of psoriasis, the change in MSK surgery rates before and after diagnosis was quite prominent and statistically significant (p<0.001, decrease from 31.71% to 2.44%). In patients without a family history of psoriasis, a decrease in the operation rates was also observed, but the statistical significance level of this change was lower (p=0.109, decrease from 18.60% to 4.65%) (
Table 4). There was no association between bDMARD, csDMARD or their combined use and MSK surgeries (for all, p>0.05).
In general, a significant decrease in MSK operation rates was observed in all patient groups after diagnosis, and this decrease was found to be statistically more significant especially in female patients, patients with axial + peripheral joint involvement and patients with a family history of psoriasis.
4. Discussion
In our study, the mean number of MSK surgeries per year was significantly higher in the period of delayed diagnosis compared to the period of medical treatment after diagnosis. In addition, there was a 7.49 years delay in the diagnosis of PsA. This is the first study comparing the mean annual frequency of MSK surgeries in the period of delayed diagnosis with the post-diagnosis period in PsA patients.
PsA may affect all joints in the body and shows a variable clinical course [
21]. PsA may lead to different pictures developing as a result of intertwined inflammatory, erosive, or osteoproliferative changes in the musculoskeletal system. Therefore, it overlaps clinically with many degenerative and inflammatory diseases. This leads to the diagnosis of different mimetic diseases other than PsA and thus delays in the diagnosis of PsA for years [
4,
6,
19,
22,
23,
24].
Previously, PsA was considered to be a relatively benign disorder, but in recent years, it has been demonstrated that the majority of PsA patients develop erosive arthritis. Structural damage to the joints of PsA patients has been found to be similar in magnitude and effect to that seen in patients with RA [
16]. A delay in diagnosis in patients with PsA leads to a progression of the inflammatory process and permanent structural damage in the musculoskeletal structure over time [
13]. Since both peripheral and axial skeletal involvement may occur, structural and functional disorders may be observed in these areas. Approximately 2/3 of PsA patients with peripheral joint involvement followed up for 5 years showed radiographic erosions [
13]. In another study, it was shown that destructive arthritis occurred in approximately 25% of patients presenting with oligoarticular arthritis and in approximately 65% of patients presenting with polyarticular disease [
21]. Haroon et al. showed that a 6-month delay in diagnosis in PsA patients led to an increased risk of joint erosion and deterioration in long-term physical function outcomes and quality of life. The importance of early diagnosis and appropriate adequate treatment to slow the progression of PsA and improve quality of life has been emphasized in many studies [
25].
In the years preceding the diagnosis of PsA, it is important to identify, prevent or manage both PsA risk factors and PsA-related long-term complications. It has been suggested that there may be a critical period in which we can identify and intervene in patients with early PsA to improve PsA-related complications [
9]. Some of the musculoskeletal findings related to PsA may lead to irreversible structural damage, and some may lead to inflammatory changes that can be reversed with medical treatment. With the introduction of new advanced treatment options in the last few decades and the demonstration of their effects on radiological progression, this issue has become a focus of interest [
13,
16,
26].
PsA patients have an increased risk of MSK surgeries due to progressive MSK system involvement, which varies according to the methodology and location of the studies [
13,
14,
15,
16,
17,
18]. The use of joint surgery among PsA patients in the Danish registry was found to be twice as high compared with the general population cohort, and it was shown that this risk increased exponentially as the duration of PsA diagnosis increased. In addition, the risk of surgery was found to be higher among patients with diagnosed PsA aged 18-40 years (22%) compared to patients in the general population cohort aged over 60 years (20%) after 15 years of follow-up [
16].
A significant proportion of our patients with PsA underwent more MSK surgeries in the delayed diagnostic period compared to the post-diagnostic period. Thus, there was a significant decrease in the number of operations per year in the post-diagnosis and post-treatment periods. As mentioned previously, although there are many studies showing an increased risk of MSK surgeries in PsA patients, our study is the first to compare the annual frequency of operations in the pre-diagnosis symptomatic period and the post-diagnosis period. Here, the calculation of the number of MSK surgeries per unit of time made the frequency of operations more accurate and comparable. In previous studies, the number of operations of varying durations made objective evaluation very difficult.
In a study by Haque et al. the frequency of orthopaedic interventions in PsA patients before and after diagnosis was evaluated. In this study, 63.92% of all operations were performed after the diagnosis, and 36.07% were performed before the diagnosis of PsA. However, the duration of symptoms before the diagnosis was not specified in this study. In addition, the duration of these operations and the frequency of operations for a certain unit of time were not calculated [
18]. In our study, the frequency of MSK surgeries before and after diagnosis was determined and compared with each other per 1-year unit time. This provided a more objective and comparable advantage.
MSK surgeries in PsA patients are usually performed to relieve pain caused by inflammation or structural defects and to restore physical function [
13,
16]. In different studies, cumulative disease activity, number of tender/swollen areas, and high erythrocyte sedimentation rate (ESR), which are indicators of increased inflammation, have been associated with increased MSK surgical risk [
13,
17,
18]. In a study by Kwok et al. it was shown that a significant proportion of surgical indications were due to inflammatory variables (42%). High ESR and active inflamed joint numbers (high disease activity markers), which are indicators of uncontrolled inflammation in PsA, were found to be associated with the frequency of MSK surgeries and the risk of undergoing major operation [
13]. In the same study, 11% of the patients were subjected to revision surgery after the first operation. This was associated with the continuation of the inflammatory process [
13]. In another study, it was shown that operations were usually performed in the most severe disease state [
17]. Patients with PsA have an overall higher risk of undergoing total hip arthroplasty and total knee arthroplasty compared to the general population, but temporal trends suggest that the risk is decreasing for patients diagnosed in recent years. It has been emphasized that collaboration between rheumatologists and orthopaedic surgeons should be strengthened because interdisciplinary evaluation is very important to improve the outcomes of PsA patients undergoing orthopaedic surgery [
14].
Previous studies have found an increase in the frequency of MSK surgeries with disease year. In our study, lower annual MSK surgery frequencies were found after PsA diagnosis. In addition, the fact that more operations were performed in the early symptomatic period before the diagnosis in our study supports that some of these operations were related to inflammation and that suppression of inflammation and symptoms with medical treatment reduced the number of operations. This suggests that early diagnosis may prevent MSK surgeries associated with these reversible inflammatory conditions. A multidisciplinary approach may have a very important contribution here. In particular, units performing MSK surgeries such as orthopaedics and neurosurgery, evaluating patients with early diagnosis questionnaires for PsA risk before the operation, and referring risky patients to rheumatology clinics may contribute to early diagnosis of PsA and prevent MSK surgeries with treatment [
27]. Interestingly, one study showed a protective effect of the Psoriasis Area Severity Index on operations in PsA patients. In our study, no correlation was found between the presence of psoriatic rash and nail involvement and MSK operation status. However, since we did not have PASI scores of the patients during the MSK surgeries, no evaluation could be made on these scores [
13]. In some studies, the effect of biological treatments on MSK operations was not found to be statistically significant. It has been stated that this may be related to the gradual transition to these drugs, which increases the risk of structural damage in diagnosed patients and osteoarthritis accompanying PsA [
13,
17]. In our study, no significant relationship was found between medication use and MSK surgeries. This supports the idea that treatment, independent of drug type, has an effect on the frequency of operations.
In addition to these, our study had some limitations. First, the fact that our study was conducted in a single centre limits the generalizability of our findings to other populations. Second, the cross-sectional design prevents this study from evaluating any of the clinical outcomes in the long term. Third, our patient numbers were too small to assess different disease patterns and treatment subgroups of PsA. In addition, no detailed assessment was made of the types and aetiology of MSK surgeries. The fact that the majority of our patients were women limited the evaluation of the gender differences in this outcome.
Prospective studies with more patients can be conducted to investigate the effect of early diagnosis and treatment on the frequency of MSK surgeries. Studies evaluating the annual frequency of MSK surgeries in PsA patients may be useful in revealing the risks of operations and the association of different treatment options with MSK surgeries. For this purpose, the effect of early initiation of new advanced treatments on operations can be more accurately demonstrated.
In conclusion, while an increase in MSK surgeries is expected in PsA patients due to disease progression over time, in our study, we found a decrease in the frequency of MSK surgeries with medical treatment after diagnosis compared to the pre-diagnosis symptomatic period. These findings suggest that diagnostic delays contribute to an increased rate of MSK surgeries, many of which could have been prevented with early medical treatmen. In this respect, evaluation of patients scheduled for MSK surgeries for the presence of PsA and early diagnosis may prevent some reversible inflammation-related MSK surgeries in this patient group.
Our study provides strong evidence that diagnostic delays in PsA contribute to excessive MSK surgeries. Timely diagnosis and medical management could prevent avoidable surgical interventions, reducing both patient morbidity and healthcare costs. Future prospective studies should further investigate the impact of early biologic therapies on MSK surgery rates
Author Contributions
Conceptualization, S.Y., İ.G., M.K., E.Ç., G.Y., N.İ., E.İ., S.Z., and M.K.; Methodology, S.Y., İ.G., M.K., E.Ç., G.Y., and N.İ.; Software, None; Validation, S.Y., İ.G., M.K., E.Ç., G.Y., and N.İ.; Formal Analysis, S.Y., İ.P.C., and M.K.; Investigation, S.Y., İ.G., M.K., E.Ç., G.Y., and N.İ.; Resources, S.Y., İ.G., M.K., E.Ç., G.Y., and N.İ.; Data Curation, S.Y., İ.G., M.K., E.Ç., G.Y., N.İ., E.İ., S.Z., and M.K.; Writing – Original Draft Preparation, S.Y., E.İ., .Z., and M.K.; Writing – Review & Editing, S.Y., İ.G., M.K., E.Ç., G.Y., N.İ., E.İ., .Z., and M.K.; Visualization, S.Y., E.İ., .Z., and M.K.; Supervision, S.Y.; Project Administration, S.Y., İ.G., M.K., E.Ç., G.Y., N.İ., .Z., and M.K.; Funding Acquisition, S.Y.
Funding
This research received no external funding
Institutional Review Board Statement
This study was conducted in compliance with the ethical standards set forth in the Declaration of Helsinki and approved by the Institutional Review Board of İnönü University Faculty of Medicine (Approval code: 2019/133). Written informed consent was obtained from all participants in accordance with the requirements of the Institutional Review Board.
Informed Consent Statement
Informed consent was obtained from the patients participating in the study.
Acknowledgments
This study was assisted by İpek Balikçi Cicek, Biostatistics and Medical Informatics, as sub-investigator.
Conflict of Interest
The authors declare that there are no conflicts of interest regarding the conduct, results, or presentation of this study.
Abbreviations
| bDMARD |
Biologic disease-modifying antirheumatic drug |
| CsDMARD |
Conventional synthetic disease-modifying antirheumatic drug |
| ESR |
Erythrocyte sedimentation rate |
| MSK |
Musculoskeletal system |
| MTX |
Methotrexate |
| NSAID |
Nonsteroidal anti-inflammatory drug |
| PsA |
Psoriatic arthritis |
| Pso |
Psoriasis |
| RA |
Rheumatoid arthritis |
| SpA |
Spondyloarthritis |
References
- Ogdie, A.; Weiss, P. The Epidemiology of Psoriatic Arthritis. Rheum. Dis. Clin. North Am. 2015, 41(4), 545–568. [Google Scholar] [CrossRef] [PubMed]
- Alascio, L.; Azuaga-Piñango, A. B.; Frade-Sosa, B.; Sarmiento-Monroy, J. C.; Ponce, A.; et al. Axial Disease in Psoriatic Arthritis: A Challenging Domain in Clinical Practice. Diagnostics (Basel, Switzerland). 2024, 14(15), 1637. [CrossRef]
- Emmungil, H.; İlgen, U.; Direskeneli, R. H. Autoimmunity in Psoriatic Arthritis: Pathophysiological and Clinical Aspects. Turk. J. Med. Sci. 2021, 51(4), 1601–1614. [Google Scholar] [CrossRef]
- Ritchlin, C. T.; Colbert, R. A.; Gladman, D. D. Psoriatic Arthritis. N. Engl. J. Med. 2017, 376, 957–970. [Google Scholar] [CrossRef] [PubMed]
- Ogdie, A.; Coates, L. C.; Mease, P. Measuring Outcomes in Psoriatic Arthritis. Arthritis Care Res. (Hoboken) 2020, 10 Suppl 10(Suppl 10), 82–109. [Google Scholar] [CrossRef] [PubMed]
- Ogdie, A.; Nowell, W. B.; Applegate, E.; Gavigan, K.; Venkatachalam, S.; de la Cruz, M.; Flood, E.; Schwartz, E. J.; Romero, B.; Hur, P. Patient Perspectives on the Pathway to Psoriatic Arthritis Diagnosis: Results from a Web-Based Survey of Patients in the United States. BMC Rheumatol. 2020, 4, 2. [Google Scholar] [CrossRef]
- Gossec, L.; Kerschbaumer, A.; Ferreira, R. J. O.; Aletaha, D.; Baraliakos, X.; et al. EULAR Recommendations for the Management of Psoriatic Arthritis with Pharmacological Therapies: 2023 Update. Ann. Rheum. Dis. 2024, 83(6), 706–719. [Google Scholar] [CrossRef]
- Kerschbaumer, A.; Smolen, J. S.; Ferreira, R. J. O.; Bertheussen, H.; Baraliakos, X.; et al. Efficacy and Safety of Pharmacological Treatment of Psoriatic Arthritis: A Systematic Literature Research Informing the 2023 Update of the EULAR Recommendations for the Management of Psoriatic Arthritis. Ann. Rheum. Dis. 2024, 83(6), 760–774. [Google Scholar] [CrossRef]
- Ogdie, A. The Preclinical Phase of PsA: A Challenge for the Epidemiologist. Ann. Rheum. Dis. 2017, 76(9), 1481–1483. [Google Scholar] [CrossRef]
- Kristensen, L. E.; Jørgensen, T. S.; Christensen, R.; Gudbergsen, H.; Dreyer, L.; et al. Societal Costs and Patients' Experience of Health Inequities Before and After Diagnosis of Psoriatic Arthritis: A Danish Cohort Study. Ann. Rheum. Dis. 2017, 76(9), 1495–1501. [Google Scholar] [CrossRef]
- Caso, F.; Costa, L.; Megna, M.; Cascone, M.; Maione, F.; et al. Early Psoriatic Arthritis: Clinical and Therapeutic Challenges. Expert Opin. Investig. Drugs 2024, 33(9), 945–965. [Google Scholar] [CrossRef]
- Zangger, P.; Esufali, Z. H.; Gladman, D. D.; Bogoch, E. R. Type and Outcome of Reconstructive Surgery for Different Patterns of Psoriatic Arthritis. J. Rheumatol. 2000, 27, 967–974. [Google Scholar] [PubMed]
- Kwok, T. S. H.; Sutton, M.; Cook, R. J.; Pereira, D.; Chandran, V.; Gladman, D. D. Musculoskeletal Surgery in Psoriatic Arthritis: Prevalence and Risk Factors. J. Rheumatol. 2023, 50(4), 497–503. [Google Scholar] [CrossRef] [PubMed]
- Ciaffi, J.; Bianchi, L.; Di Martino, A.; Faldini, C.; Ursini, F. Is Total Joint Arthroplasty an Effective and Safe Option for Psoriatic Arthritis Patients? J. Clin. Med. 2024, 13(18), 5552. [Google Scholar] [CrossRef]
- Mazzucchelli, R.; Almodóvar, R.; Turrado-Crespí, P.; Crespí-Villarías, N.; Pérez-Fernández, E.; et al. Trends in Orthopaedic Surgery for Spondyloarthritis: Outcomes from a National Hospitalised Patient Registry (MBDS) over a 17-Year Period (1999–2015). RMD Open 2022, 8(1), e002107. [Google Scholar] [CrossRef] [PubMed]
- Guldberg-Møller, J.; Cordtz, R. L.; Kristensen, L. E.; Dreyer, L. Incidence and Time Trends of Joint Surgery in Patients with Psoriatic Arthritis: A Register-Based Time Series and Cohort Study from Denmark. Ann. Rheum. Dis. 2019, 78(11), 1517–1523. [Google Scholar] [CrossRef]
- Zangger, P.; Gladman, D. D.; Bogoch, E. R. Musculoskeletal Surgery in Psoriatic Arthritis. J. Rheumatol. 1998, 25(4), 725–729. [Google Scholar]
- Haque, N.; Lories, R. J.; de Vlam, K. Orthopaedic Interventions in Patients with Psoriatic Arthritis: A Descriptive Report from the SPAR Cohort. RMD Open 2016, 2(2), e000293. [Google Scholar] [CrossRef]
- Michet, C. J.; Mason, T. G.; Mazlumzadeh, M. Hip Joint Disease in Psoriatic Arthritis: Risk Factors and Natural History. Ann. Rheum. Dis. 2005, 64, 1068–1070. [Google Scholar] [CrossRef]
- Belsky, M. R.; Feldon, P.; Millender, L. H.; et al. Hand Involvement in Psoriatic Arthritis. J. Hand Surg. Am. 1982, 7, 203–207. [Google Scholar] [CrossRef]
- Strauss, E. J.; Alfonso, D.; Baidwan, G.; Di Cesare, P. E. Orthopedic Manifestations and Management of Psoriatic Arthritis. Am. J. Orthop. (Belle Mead NJ) 2008, 37(3), 138–147.
- McHugh, N. J.; Balachrishnan, C.; Jones, S. M. Progression of Peripheral Joint Disease in Psoriatic Arthritis: A 5-Year Prospective Study. Rheumatology 2003, 42, 778–783. [Google Scholar] [CrossRef]
- Kılıç, G.; Kılıç, E.; Tekeoğlu, İ.; Sargın, B.; Cengiz, G.; et al. Diagnostic Delay in Psoriatic Arthritis: Insights from a Nationwide Multicenter Study. Rheumatol. Int. 2024, 44(6), 1051–1059. [Google Scholar] [CrossRef] [PubMed]
- Sørensen, J.; Hetland, M. L.; all departments of rheumatology in Denmark. Diagnostic Delay in Patients with Rheumatoid Arthritis, Psoriatic Arthritis and Ankylosing Spondylitis: Results from the Danish Nationwide DANBIO Registry. Ann. Rheum. Dis. 2015, 74(3), e12. [CrossRef]
- Haroon, M.; Gallagher, P.; Fitzgerald, O. Diagnostic Delay of More than 6 Months Contributes to Poor Radiographic and Functional Outcome in Psoriatic Arthritis. Ann. Rheum. Dis. 2015, 74, 1045–1050. [Google Scholar] [CrossRef] [PubMed]
- Goulabchand, R.; Mouterde, G.; Barnetche, T.; Lukas, C.; Morel, J.; Combe, B. Effect of Tumour Necrosis Factor Blockers on Radiographic Progression of Psoriatic Arthritis: A Systematic Review and Meta-Analysis of Randomised Controlled Trials. Ann. Rheum. Dis. 2014, 73(2), 414–419. [Google Scholar] [CrossRef] [PubMed]
- Lajevardi, V.; Ghodsi, S. Z.; Shafiei, M.; Teimourpour, A.; Etesami, I. Evaluating the Persian Versions of Two Psoriatic Arthritis Screening Questionnaires Early Arthritis for Psoriatic Patients Questionnaire (EARP) and Psoriasis Epidemiology Screening Tool (PEST) in Iranian Psoriatic Patients. Turk. J. Med. Sci. 2021, 51(1), 159–166. [Google Scholar] [CrossRef]
|
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2025 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (http://creativecommons.org/licenses/by/4.0/).