Submitted:
10 March 2025
Posted:
12 March 2025
You are already at the latest version
Abstract
Keywords:
1. Introduction
2. Materials and Methods
2.1. Study Design and Setting
2.2. Data Collection
2.3. Data Analysis
2.4. Operational Definitions
3. Results
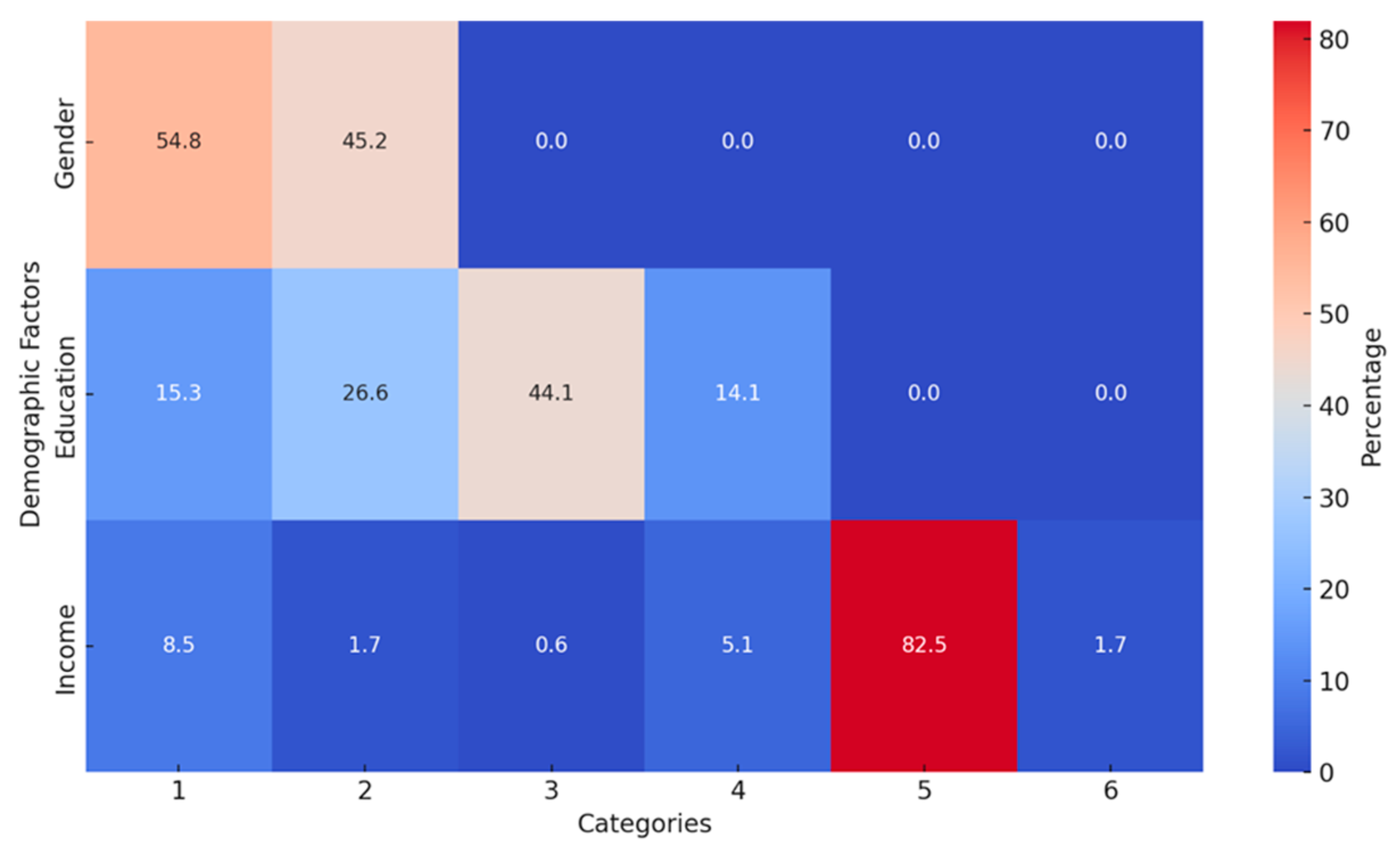
3.1. Demographic Analysis
3.2. Comorbidity and Sputum Conversion
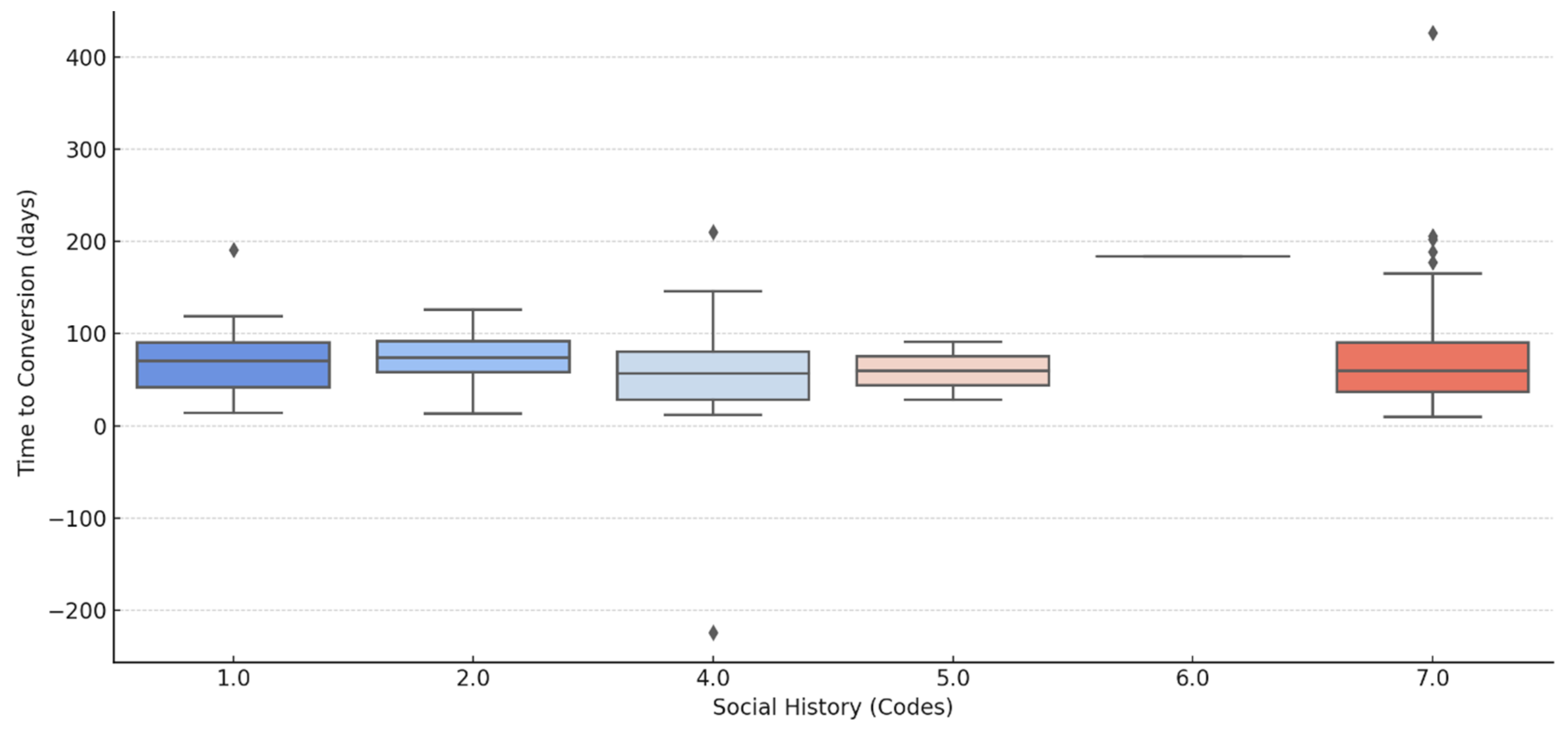
3.3. Social History Factors and Sputum Conversion Times
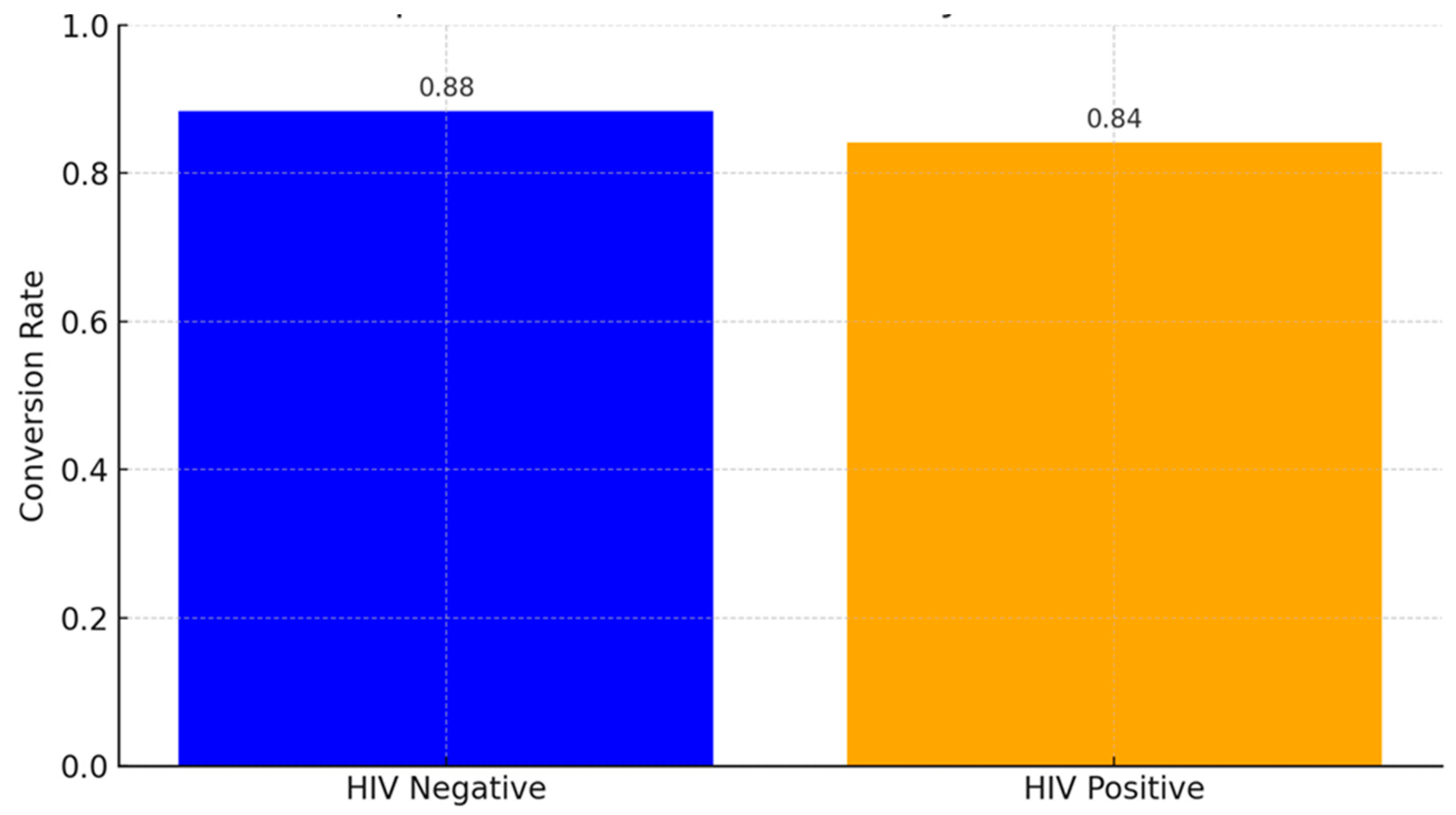
3.4. HIV Status and Sputum Conversion
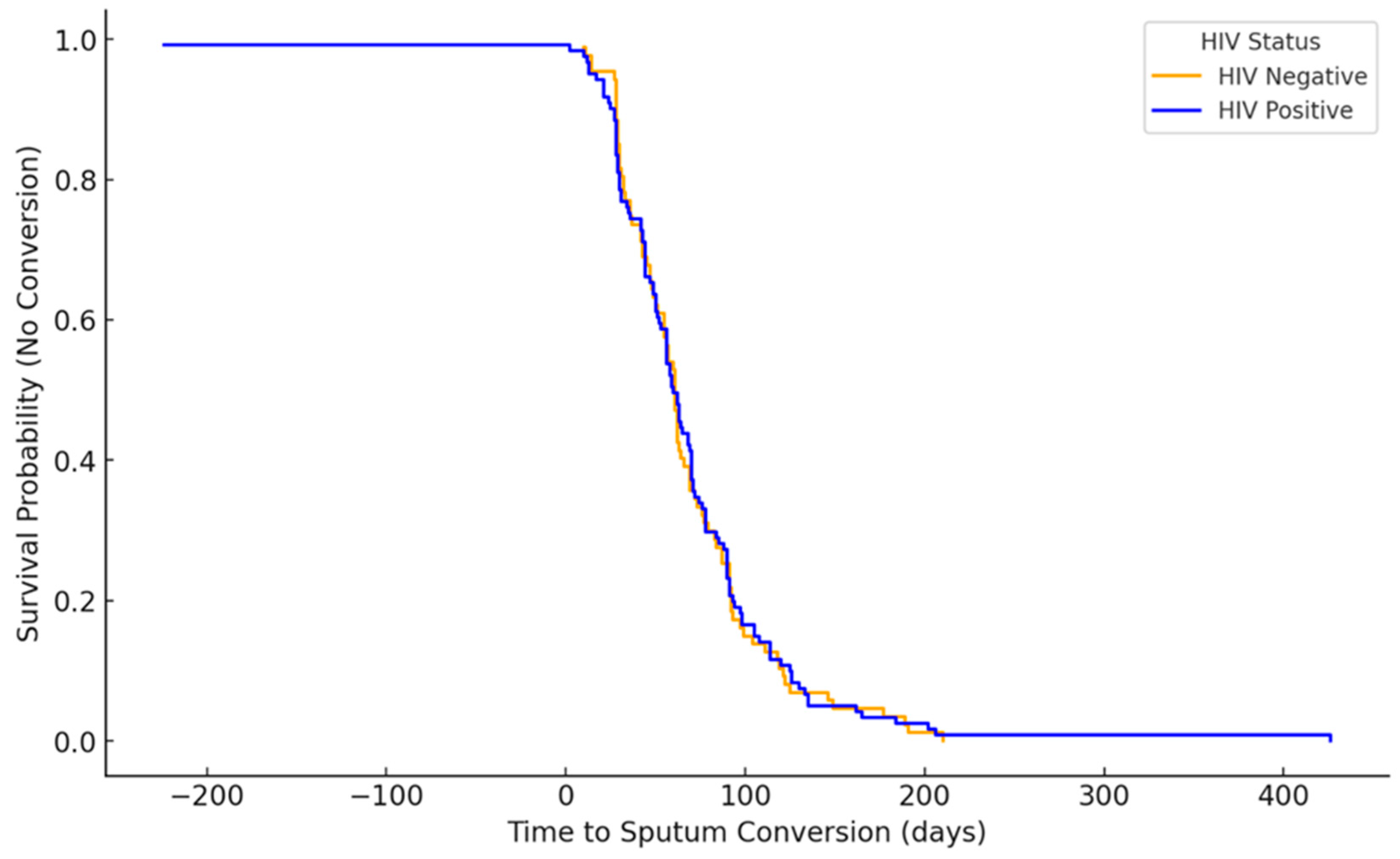
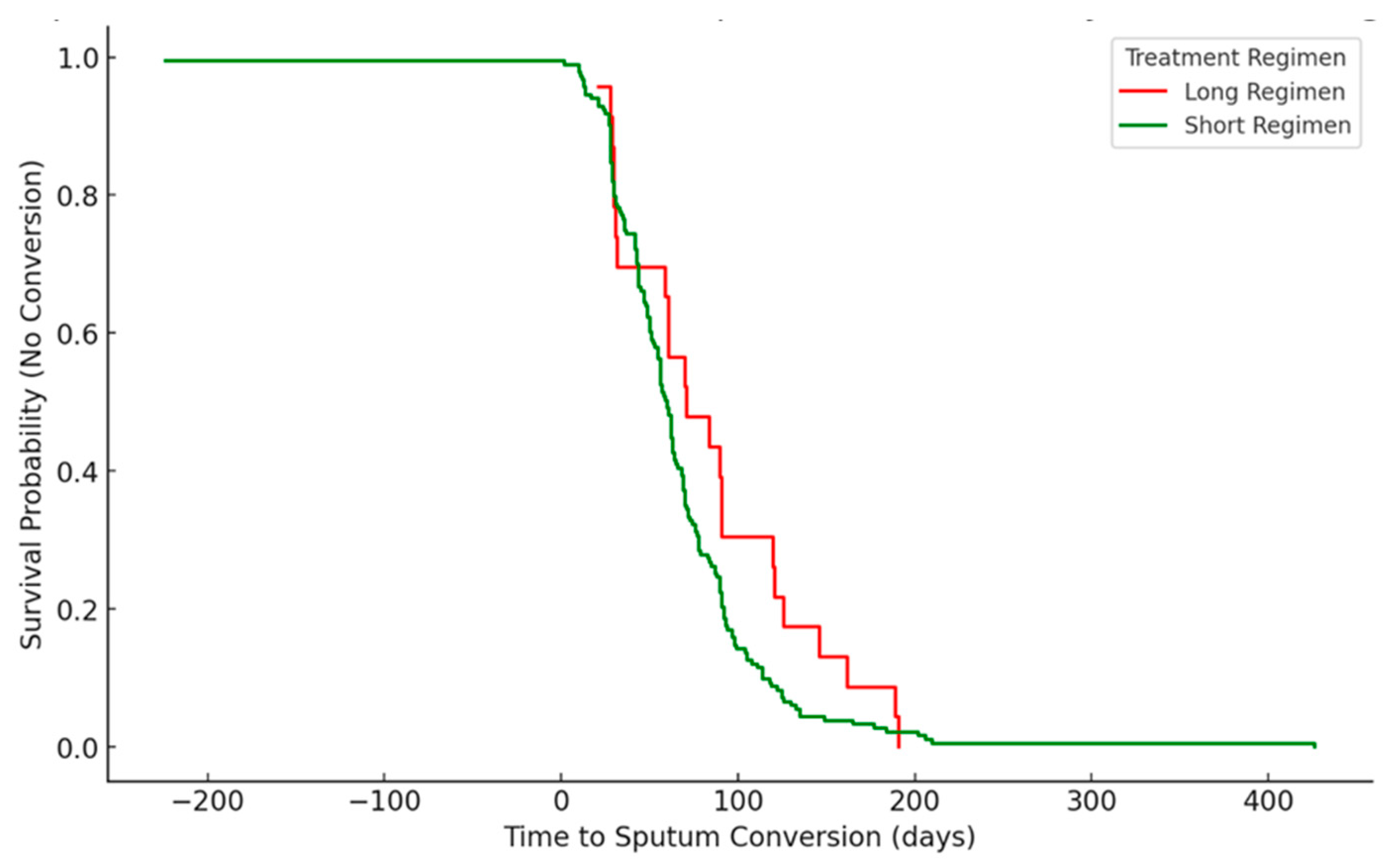
3.5. Time to Sputum Conversion Stratified by HIV Status (Kaplan-Meier Survival Curve)
3.6. Treatment Regimen
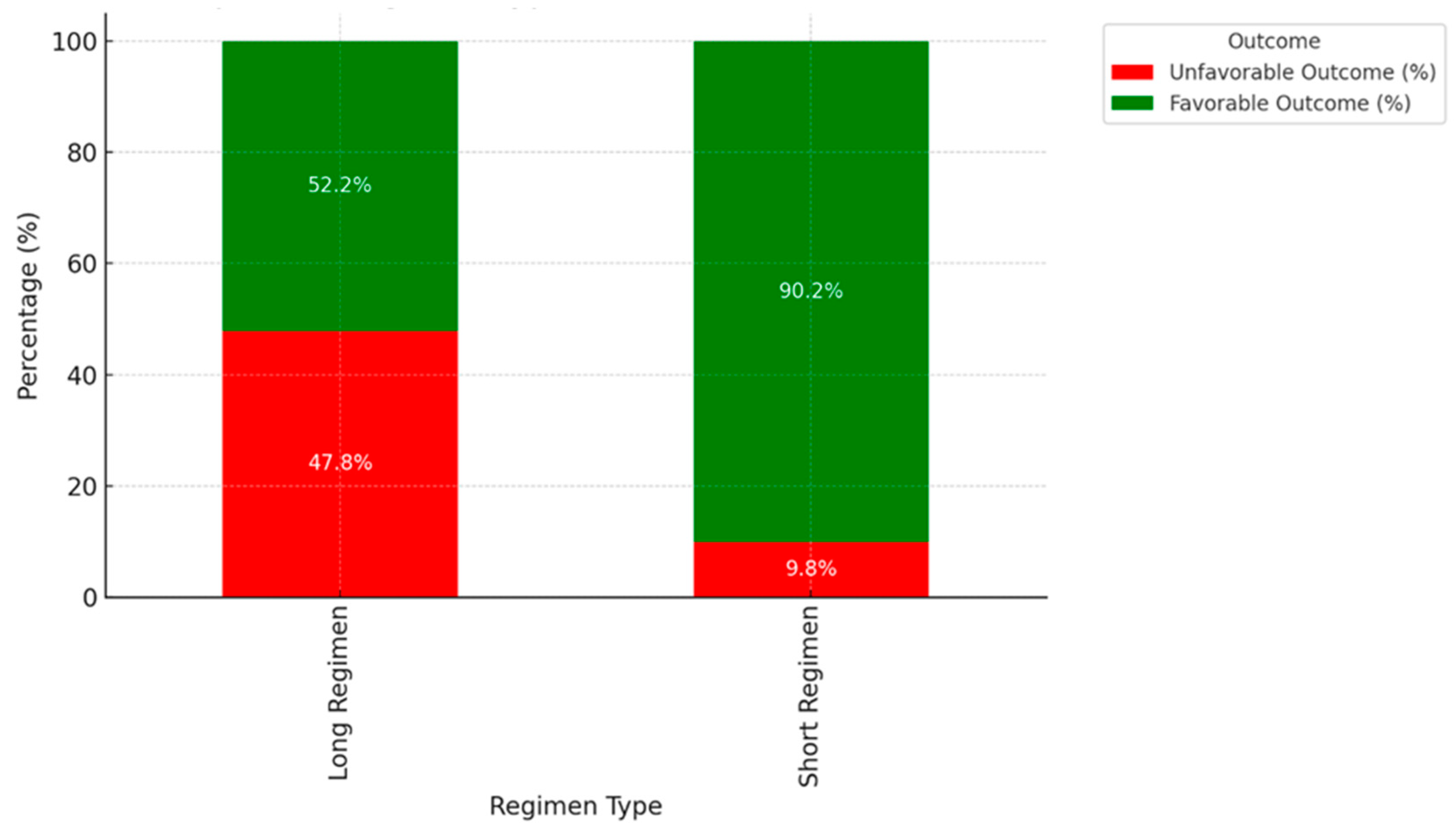
3.7. Impact of Regimen Type on Treatment Outcome
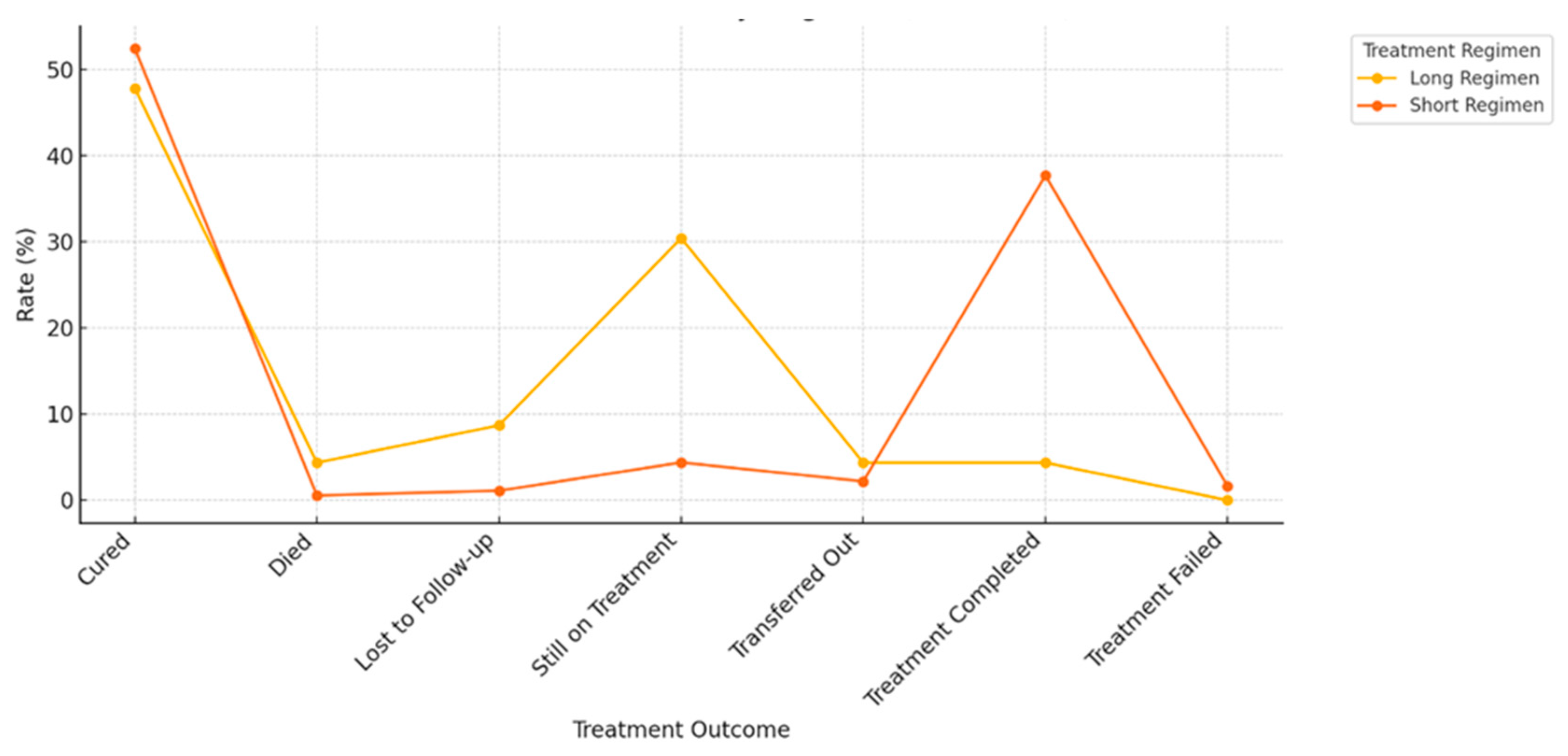
3.8. Treatment Outcomes Based on Different Types of Drug Regimen
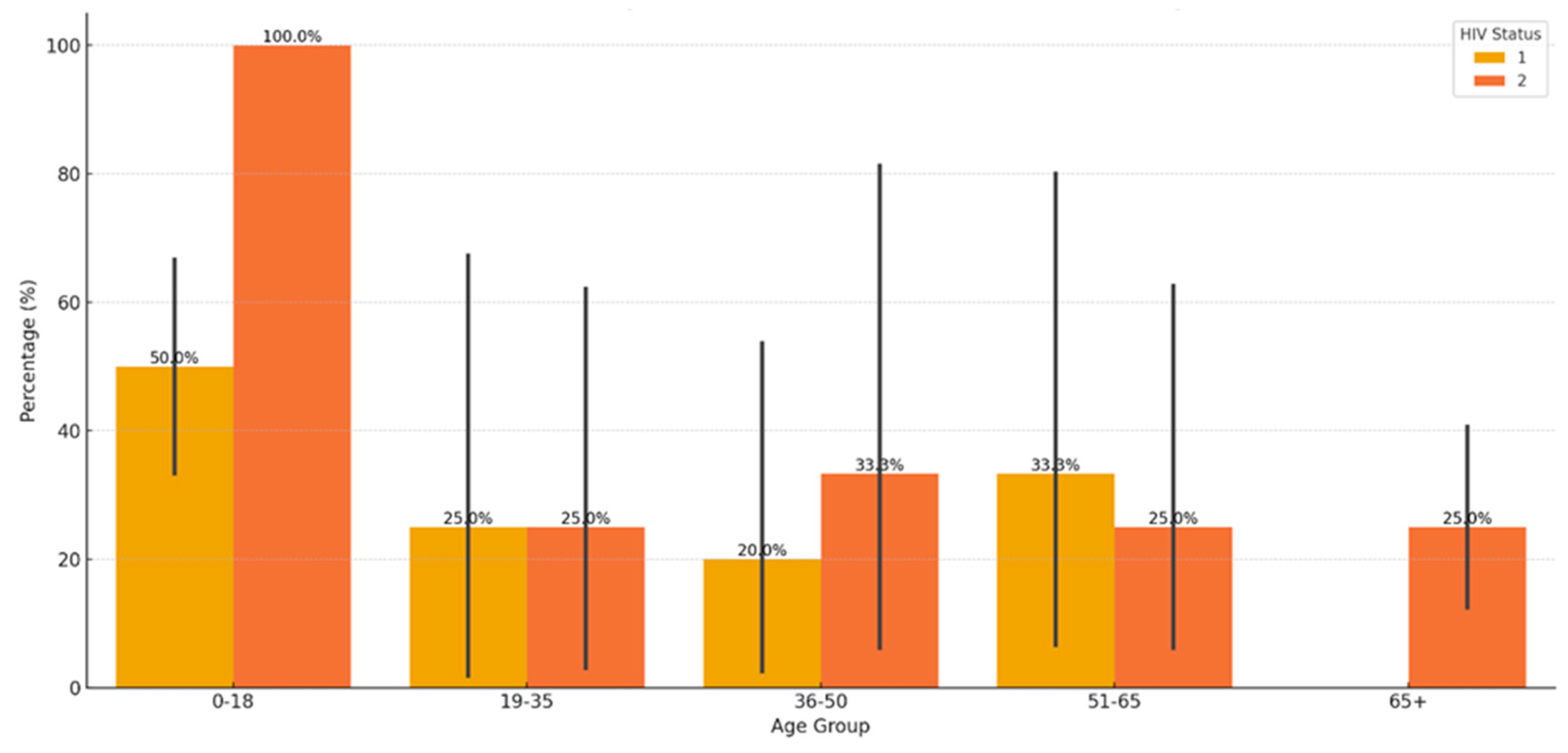
3.9. Relationship Between Age, HIV-Status and Comorbidities
3.10. Logistic Regression Results
4. Discussion
5. Conclusions
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Acknowledgments
Conflicts of Interest
Abbreviations
| TB | Tuberculosis |
| MDR-TB | Multidrug-resistant tuberculosis |
| XDR-TB | Extensively drug-resistant tuberculosis |
| AFB | Acid-fast bacilli |
| DCSPs | Delayed sputum conversion patients |
| PTB | Pulmonary tuberculosis |
| STR | short treatment regimen |
| LTR | longer treatment regimen |
| SCC | sputum culture conversion |
| SLR | standard longer regimen |
| ART | Antiretroviral therapy |
References
- Ordonez, A.A.; Tucker, E.W.; Anderson, C.J.; Carter, C.L.; Ganatra, S.; Kaushal, D.; Kramnik, I.; Lin, P.L.; Madigan, C.A.; Mendez, S.; Rao, J. Visualizing the dynamics of tuberculosis pathology using molecular imaging. J Clin Invest. 2021, 131(5).
- Shah, M., Dansky, Z., Nathavitharana, R., Behm, H., Brown, S., Dov, L., Fortune, D., Gadon, N.L., Gardner Toren, K., Graves, S, Haley, C.A., 2024. NTCA Guidelines for Respiratory Isolation and Restrictions to Reduce Transmission of Pulmonary Tuberculosis in Community Settings. Clin. Infect. Dis. 2024, ciae199.
- Weldemhret L.; Atsbaha A.H.; Bekuretsion H.; Desta A.; Legesse L.; Kahsay, A.G., Hagos, D. Time to Sputum Culture Conversion and Its Predictors Among Multidrug Resistant Tuberculosis Patients in Tigray, Northern Ethiopia: Retrospective Cohort Study. Infect. Drug Resist, 2023,16, 3671–3681. [CrossRef]
- Global tuberculosis report 2024. Geneva: World Health Organization; 2024. Licence: CC BY-NC-SA 3.0 IGO (Accessed 5th Januar, 2025).
- World Health Organization. Global tuberculosis report 2021. Geneva,Switzerland: World Health Organization; 2021 (Accessed 5th January 2025).
- Paradkar, M.S.; Pradhan, N.N.; Balaji, S.; Gaikwad, S.N.; Chavan, A.; Dharmashale, S.N.; Sahasrabudhe, T.; Lokhande, R.; Deshmukh, S.A.; Barthwal, M.; Atre, S. Early microbiologic markers of pulmonary tuberculosis treatment outcomes. Ann Am Thorac Soc, 2023, 20(12), 1760-1768.
- Abebe, M.; Atnafu, A.; Tilahun, M.; Sero, N.; Neway, S.; Alemu, M.; Tesfaye, G.; Mihret, A.; Bobosha, K.; Wan, C. Determinants of sputum culture conversion time in multidrug-resistant tuberculosis patients in ALERT comprehensive specialized hospital, Addis Ababa, Ethiopia: A retrospective cohort study. Plos One, 2024, 19(5), p.e0304507.
- Assemie, M. A.; Alene, M.; Petrucka, P.; Leshargie, C. T.; Ketema, D. B. Time to sputum culture conversion and its associated factors among multidrug-resistant tuberculosis patients in Eastern Africa: a systematic review and meta-analysis. Int. J. Infect. Dis. 2020, 98, 230–236. [CrossRef]
- Ncha, R.; Variava, E.; Otwombe, K.; Kawonga, M.; Martinson, N.A. Predictors of time to sputum culture conversion in multi-drug-resistant tuberculosis and extensively drug-resistant tuberculosis in patients at Tshepong-Klerksdorp Hospital. Southern Afr J Infect Dis, 2019, 34(1),1-8.
- Lee, H.H.; Jo, K.W.; Yim, J.J.; Jeon, D.; Kang, H.; Shim, T.S. Interim treatment outcomes in multidrug-resistant tuberculosis patients treated sequentially with bedaquiline and delamanid. Int J Infect Dis, 2020, 98, 478-485.
- Djouma, F.N.; Noubom, M.; Ateudjieu, J.; Donfack, H. Delay in sputum smear conversion and outcomes of smear-positive tuberculosis patients: a retrospective cohort study in Bafoussam, Cameroon. BMC Infect Dis. 2015, 15:1-7.
- Kateete, D.P.; Mbabazi, M.M.; Nakazzi, F.; Katabazi, F.A.; Kigozi, E.; Ssengooba, W.; Nakiyingi. L.; Namiiro, S.; Okwera, A.; Joloba, M.L.; Muwonge, A. Sputum microbiota profiles of treatment-naïve TB patients in Uganda before and during first-line therapy. Sci. Rep. 2021, 11:24486 . [CrossRef]
- Bisognin, F., Amodio, F., Lombardi, G., Reggiani, M.L.B., Vanino, E., Attard, L., Tadolini, M., Carla, R. M., Monte, P.D. Predictors of time to sputum smear conversion in patients with pulmonary tuberculosis under treatment. New Microbiologica, 2018, 42, 3, 171-175.
- Ibrahim, M.N.; Nik Husain, N.R.; Daud, A.; Chinnayah, T. Epidemiology and risk factors of delayed sputum smear conversion in Malaysian aborigines with smear-positive pulmonary tuberculosis. Int J Env Res Public Health, 2022, 19(4), 2365.
- Gamachu, M.; Deressa, A.; Birhanu, A.; Ayana, G.M.; Raru, T.B.; Negash, B.; Merga, B.T.; Alemu, A.; Ahmed, F.; Mohammed, A.; Abdulahi, I.M.; Regassa, L.D. Sputum smear conversion and treatment outcomes among drug-resistant pulmonary tuberculosis patients in eastern Ethiopia: A 9-years data analysis. Front. Med. 2022, 9:1007757. [CrossRef]
- Pang, M.; Dai, X.; Wang, N.; Yi, J.; Sun, S.; Miao, H.; Zhang, J.; Zhang, H.; Li, J.; Ding, B.; Yang, X. A study on factors influencing delayed sputum conversion in newly diagnosed pulmonary tuberculosis based on bacteriology and genomics. Sci Rep. 2024, 9;14(1):18550.
- Asemahagn, M. A. Sputum smear conversion and associated factors among smear-positive pulmonary tuberculosis patients in East Gojjam Zone, Northwest Ethiopia: a longitudinal study. BMC Pulm. Med. 2021, 21, 118–210. [CrossRef]
- .
- Kim, J.; Kwak, N.; Lee, H. Y.; Kim, T. S.; Kim, C. K.; Han, S. K.; Yim, J.J. Effect of drug resistance on negative conversion of sputum culture in patients with pulmonary tuberculosis. Int. J. Infect. Dis. 2016, 42, 64–68. [CrossRef]
- Tierney, D.B.; Franke, M.F.; Becerra, M.C.; Alcántara, Virú, F.A., Bonilla, C.A.; Sánchez, E.; Guerra, D.; Muñoz, M.; Llaro, K.; Palacios, E.; Mestanza, L. Time to Culture Conversion and Regimen Composition in Multidrug-Resistant Tuberculosis Treatment. PLoS ONE, 2014, 9, e108035. [CrossRef] [PubMed]
- Rieu, R.; Chang, C.; Collin, S. M.; Fazekas, J.; Dassanaike, S.; Abbara, A.; Davidson, R.N. Time to detection in liquid culture of sputum in pulmonary MDR-TB does not predict culture conversion for early discharge. J. Antimicrob. Chemother. 2016, 71 (3), 803–806. [CrossRef]
- Putri, F. A.; Burhan, E.; Nawas, A.; Soepandi, P. Z.; Sutoyo, D. K.; Agustin, H.; Isbaniah, F.; Dowdy, D.W. Body mass index predictive of sputum culture conversion among MDR-TB patients in Indonesia. Int. J. Tuberc. Lung Dis. 2014, 18 (5), 564–570. [CrossRef]
- Parikh, R.; Nataraj, G.; Kanade, S.; Khatri, V.; Mehta, P. Time to sputum conversion in smear positive pulmonary TB patients on category I DOTS and factors delaying it. J. Assoc. Physicians India, 2012, 60, 22–26.
- Shah, N.S.; Pratt, R.; Armstrong, L.; Robison, V.; Castro, K.G.; Cegielski, J.P. Extensively drug-resistant tuberculosis in the United States, 1993-2007. JAMA, 2008, 300(18), 2153-2160.
- Alzarea A.I.; Saifullah, A.; Khan, Y.H.; Alanazi, A.S.; Alatawi, A.D.; Algarni, M.A.; Almalki, Z.S.; Alahmari, A.K.; Alhassan, H.H.; Mallhi, T.H. Evaluation of time to sputum smear conversion and its association with treatment outcomes among drug-resistant tuberculosis patients: a retrospective record-reviewing study. Front. Pharmacol. 2024, 5;15:1370344.
- Holtz, T.H.; Sternberg, M.; Kammerer, S.; Laserson, K.F.; Riekstina, V.; Zarovska, E.; Skripconoka, V.; Wells, C.D.; Leimane, V. Time to sputum culture conversion in multidrug-resistant tuberculosis: predictors and relationship to treatment outcome. Ann Intern. Med. 2006, 144, 650–659. [CrossRef]
- Rodriguez, M.; Monedero, I.; Caminero, J.A.; Encarnación, M.; Dominguez, Y.; Acosta, I.; Muñoz, E.; Camilo, E.; Martinez-Selmo, S.; De Los Santos, S.; Del Granado, M. Successful management of multidrug-resistant tuberculosis under programme conditions in the Dominican Republic. Int. J. Tuberc Lung Dis, 2013, 17(4), 520-525.
- Basit, A.; Ahmad, N.; Khan, A.H.; Javaid, A.; Sulaiman, S.A.S.; Afridi, A.K.; Adnan, A.S.; Haq, I.U.; Shah, S.S.; Ahadi, A.; Ahmad, I. Predictors of two months culture conversion in multidrug-resistant tuberculosis: findings from a retrospective cohort study. PLOS One, 2014, 9: e93206. [CrossRef]
- Velayutham, B., Nair, D., Kannan, T., Padmapriyadarsini, C., Sachdeva, K.S., Bency, J., Klinton, J.S., Haldar, S., Khanna, A., Jayasankar, S., Swaminathan, S. Factors associated with sputum culture conversion in multidrug-resistant pulmonary tuberculosis. Int J Tuberc Lung Dis, 2016, 20, 1671–1676. [PubMed]
- Joseph, P.; Desai, V.B.R.; Mohan, N.S.; Fredrick, J.S.; Ramachandran, R.; Raman, B.; Wares, F.; Ramachandran, R.; Thomas, A. Outcome of standardized treatment for patients with MDR-TB from Tamil Nadu, India. Indian J Med. Res. 2011, 133(5), 529-534.
- Singla, R.; Sarin, R.; Khalid, U.; Mathuria, K.; Singla, N.; Jaiswal, A.; Puri, M.M.; Visalakshi, P.; Behera, D. Seven-year DOTS-Plus pilot experiencein India: results, constraints and issues. Int J Tuberc Lung Dis, 2009, 13: 976–981.
- Brust, J.C.M.; Lygizos, M.; Chaiyachati, K.; Scott, M.; van der Merwe, T.L.; Moll, A.P.; Li, X.; Loveday, M.; Bamber, S.A.; Lalloo, U.G.; Friedland, G.H. Culture Conversion Among HIV Co-Infected Multidrug- Resistant Tuberculosis Patients in Tugela Ferry, South Africa. PLoS One, 2011, 6, e15841. [CrossRef] [PubMed]
- Akalu, Y.T.; Muchie K.F.; Gelaye, K.A. Time to sputum culture conversion and its determinants among Multi-drug resistant Tuberculosis patients at public hospitals of the Amhara Regional State: A multicenter retrospective follow up study. PLoS One, 2018, 13(6), e0199320. [CrossRef]
- Shibabaw, A.; Gelaw, B.; Wang, S.H.; Tessema, B. Time to sputum smear and culture conversions in multidrug resistant tuberculosis at University of Gondar Hospital, Northwest Ethiopia. PLoS ONE, 2018, 13(6), e0198080. [CrossRef]
- Wenlu, Y.; Xia, Z.; Chuntao, W.; Qiaolin, Y.; Xujue, X.; Rong, Y.; Dan, S.; Xi, Y.; Bin, W. Time to sputum culture conversion and its associated factors among drug-resistant tuberculosis patients: a systematic review and meta-analysis. BMC Infect. Dis. 2024, 24(1), 169. [CrossRef]
- Kurbatova, E.V.; Cegielski, J.P.; Lienhardt, C.; Akksilp, R.; Bayona, J.; Becerra, M.C.; Caoili, J.; Contreras, C.; Dalton, T.; Danilovits, M.; Demikhova, O.V. Sputum culture conversion as a prognostic marker for end-of-treatment outcome in patients with multidrug-resistant tuberculosis: a secondary analysis of data from two observational cohort studies. Lancet Respir Med, 2015, 3(3), 201-209.
- Senkoro, M.; Mfinanga, S.G.; Mørkve, O. Smear microscopy and culture conversion rates among smear positive pulmonary tuberculosis patients by HIV status in Dar es Salaam, Tanzania. BMC Infect Dis. 2010, 10, 210. [CrossRef]
- Hafkin, J.; Modongo, C.; Newcomb, C.; Lowenthal, E.; MacGregor, R.R.; Steenhoff, A.P.; Friedman, H.; Bisson, G.P. Impact of the human immunodeficiency virus on early multidrug-resistant tuberculosis treatment outcomes in Botswana. Int J Tuberc Lung Dis, 2013, 17(3), 348-353.
- Alakaye, O.J. Time to sputum culture conversion of Multi-Drug Resistant Tuberculosis in HIV positive versus HIV negative patients in Lesotho. University of Pretoria (South Africa). 2018.
- Wahid, A.; Ghafoor, A.; Khan, A.W.; Al-Worafi, Y.M.; Latif, A.; Shahwani, N.A.; Atif, M.; Saleem, F.; Ahmad, N. Comparative effectiveness of individualized longer and standardized shorter regimens in the treatment of multidrug resistant tuberculosis in a high burden country. Front Pharmacol, 2022,13, 973713.
- Abidi, S.; Achar, J.; Neino, M.M.A.; Bang, D.; Benedetti, A.; Brode, S.; Campbell, J.R.; Casas, E.C.; Conradie, F.; Dravniece, G.; du Cros, P. Standardised shorter regimens versus individualised longer regimens for rifampin-or multidrug-resistant tuberculosis. Eur Resp J, 2020, 55(3).
- Karnan, A.; Jadhav, U.; Ghewade, B.; Ledwani, A.; Shivashankar, P. A Comprehensive Review on Long vs. Short Regimens in Multidrug-Resistant Tuberculosis (MDR-TB) Under Programmatic Management of Drug-Resistant Tuberculosis (PMDT). Cureus, 2024, 16(1).
- Lotz, J.K.; Porter, J.D.; Conradie, H.H.; Boyles, T.H.; Gaunt, C.B.; Dimanda, S.; Cort, D. Treating drug-resistant tuberculosis in an era of shorter regimens: Insights from rural South Africa. S. Afr Med J, 2023, 113(11), 1491-1500.
- Mleoh, L.; Mziray, S.R.; Tsere, D.; Koppelaar, I.; Mulder, C.; Lyakurwa, D. Shorter regimens improved treatment outcomes of multidrug-resistant tuberculosis patients in Tanzania in 2018 cohort. Trop Med Int Health, 2023, 28(5), 357-366.
- Hayre, K.; Takele, M.K.; Birri, D.J. Tuberculosis treatment outcomes and associated factors at Alemgena Health Center, Sebeta, Oromia, Ethiopia. PLoS One, 2024, 19(5): e0303797. [CrossRef]
- Leketa, M.M.; Zondi, S.; Cele, L.; Mathibe, M.; Ngwepe, P. Factors associated with unfavourable treatment outcomes among tuberculosis patients at health facilities of Maseru, Lesotho. S Afr Fam Pract. 2024, 66(1),6004.
- Massud, A.; Khan, A.H.; Syed Sulaiman, S.A.; Ahmad, N.; Shafqat, M.; Ming, L.C. Unsuccessful treatment outcome and associated risk factors. A prospective study of DR-TB patients from a high burden country, Pakistan. PLoS One, 2023, 18(8), e0287966.
- Osório, D.; Munyangaju, I.; Nacarapa, E.; Nhangave, A.V.; Ramos-Rincon, J.M. Predictors of unfavourable tuberculosis treatment outcome in Bilene District, Gaza Province, Mozambique: A retrospective analysis, 2016-2019. S Afr Med. J., 2022, 112(3), 234-239.
- Limenh, L.W.; Kasahun, A.E.; Sendekie, A.K.; Seid, A.M.; Mitku, M.L.; Fenta, E.T.; Melese, M.; Workye, M.; Simegn, W.; Ayenew, W. Tuberculosis treatment outcomes and associated factors among tuberculosis patients treated at healthcare facilities of Motta Town, Northwest Ethiopia: a five-year retrospective study. Sci Rep, 2024, 14(1), 7695.
- Hosu, M.C.; Faye, L.M.; Apalata, T. Comorbidities and Treatment Outcomes in Patients Diagnosed with Drug-Resistant Tuberculosis in Rural Eastern Cape Province, South Africa. Diseases, 2024, 12(11), 296.
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2025 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).




