Submitted:
07 March 2025
Posted:
07 March 2025
You are already at the latest version
Abstract
Keywords:
1. Introduction
2. Neuron-Specific Enolase (NSE) as a Prognostic Marker of Central Nervous System Damage and Poor Neurological Outcomes Following Cardiac Arrest
| Condition | Biological Mechanism | Cut-off NSE | Sensitivity (%) | Specificity (%) | Main Findings |
|---|---|---|---|---|---|
| Out-of-Hospital Cardiac Arrest (OHCA) | Cerebral ischemia & reperfusion injury. | >20 μg/L (Days 3–4) | 85 | 82 | - NSE >30 μg/L (Day 4) → 100% specificity for poor prognosis.- 48:24-hour NSE ratio ≥1.7 → 100% specificity. [3] |
| Sepsis-Associated Encephalopathy (SAE) | Neuronal damage due to inflammation and BBB disruption. | 14.36 μg/L (Day 3) | 61.1 | 73.9 | - NSE elevated in SAE vs. controls (Δ 7.79 ng/mL, 95% CI: 5.23–10.34).- Moderate diagnostic accuracy, improves with IL-6. [6] |
| Status Epilepticus (SE) | Neuronal damage from prolonged seizures. | 17.8 μg/L | 77.3 | 45.2 | - NSE alone: limited accuracy (AUC = 0.624).- With S100β → AUC = 0.748, better specificity. [2] |
| Delirium in ICU | Acute brain dysfunction, unclear NSE role. | Not defined | NA | NA | - NSE not a direct mortality predictor.- May indicate disease severity / ventilation need. [12] |
| Ischemic/Traumatic Brain Injury | Neuronal apoptosis and necrosis. | >25 μg/L | 76 | 80 | - NSE correlates with injury severity.- Specificity affected by sepsis, shock. [1] |
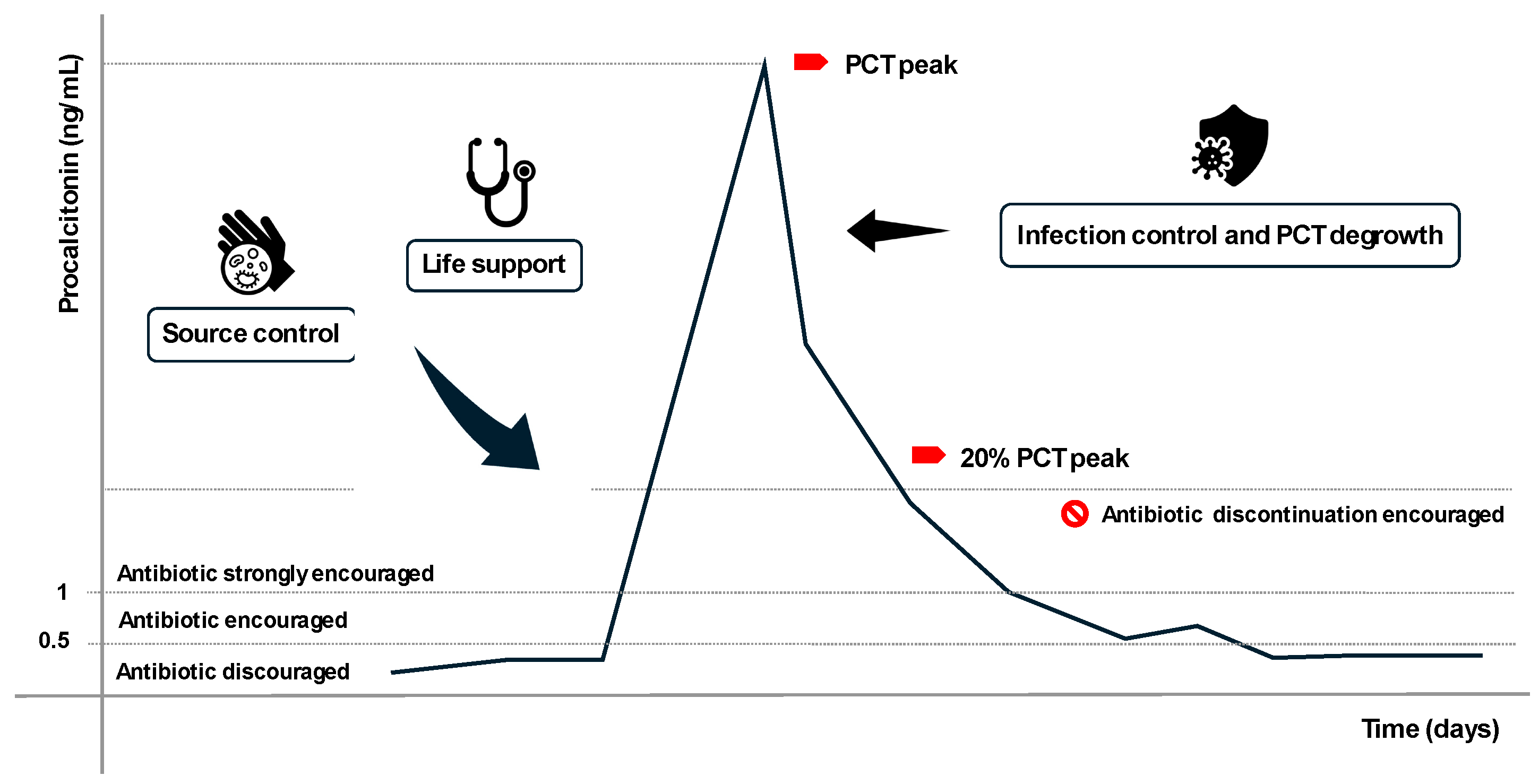
3. Procalcitonin (PCT): A Biomarker for Detecting Infections and Guiding Antibiotic Therapy
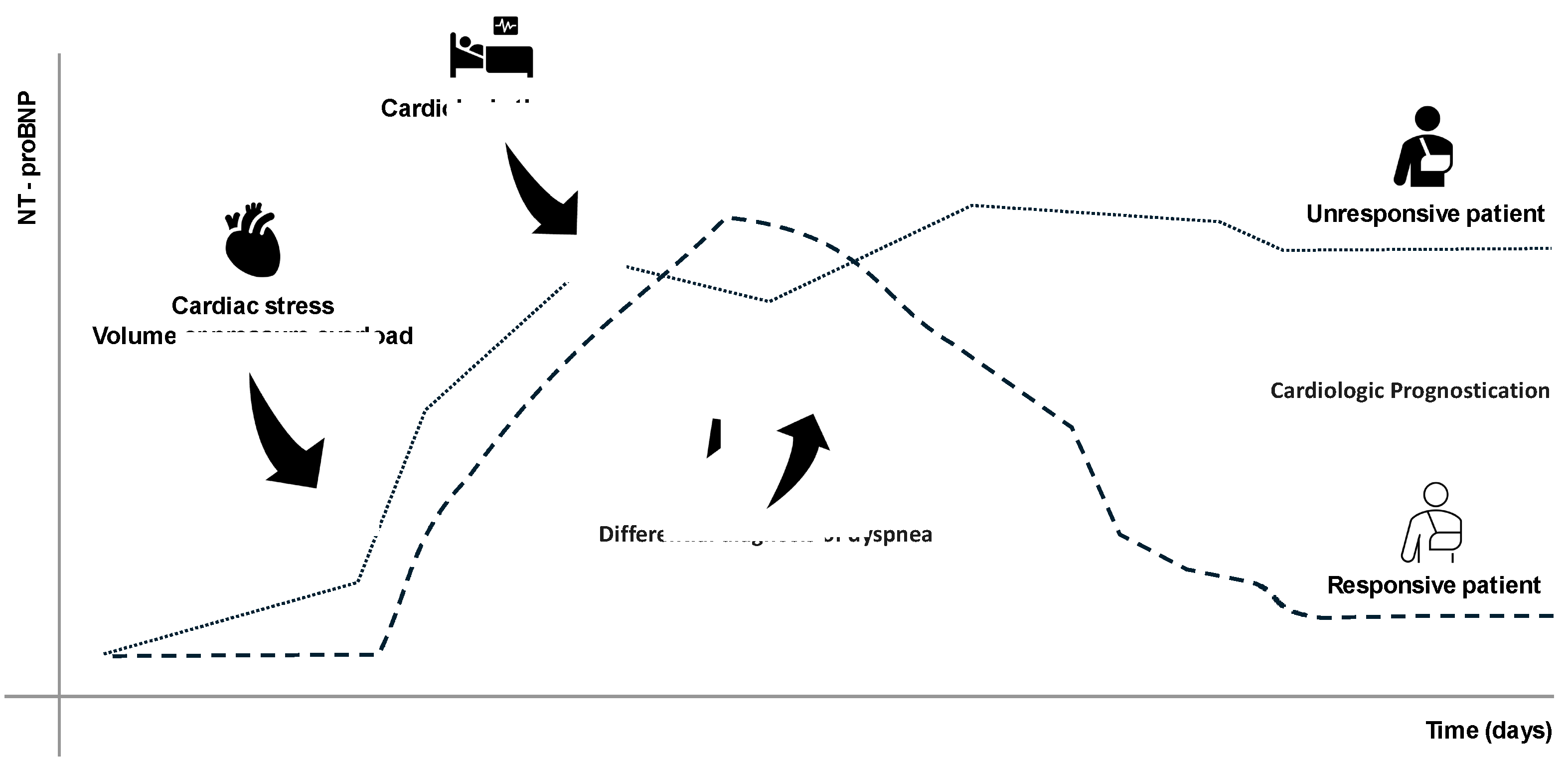
4. N-Terminal Pro-Brain Natriuretic Peptide (NT-proBNP): A Reliable Biomarker for Cardiac Failure Diagnosis and Management
5. Interleukin-6 (IL-6): A Key Biomarker of Systemic and Pulmonary Inflammation
6. Serum Creatinine (SCr) and Cystatin C (CysC): Essential Biomarkers for Renal Function Evaluation
| Characteristic | Serum Creatinine (SCr) | Cystatin C (CysC) |
|---|---|---|
| Production | Derived from muscle metabolism | Produced constantly by all nucleated cells |
| Elimination | Filtered by glomeruli; partially secreted by tubules | Filtered and fully metabolized in proximal tubules |
| Influencing Factors | Muscle mass, diet, age, hydration | Minimal; thyroid and inflammation influence |
| Cost | Low (<€5) | High (~10× SCr) |
| Half-Life | ~4 hours | ~1.5–2 hours; faster response to GFR changes |
| Sensitivity for AKI | Low; delayed detection | High; AUROC 0.89 for AKI |
| Specificity for CKD | Moderate | High; better predictor of CKD progression |
| Response to Therapy | Slow; lag in reflecting renal recovery | Fast; better indicator of therapy response |
| Utility in Pediatric Patients | Limited due to growth-related variability | Effective; reliable even in pediatric populations |
| Utility in Post-Transplant Monitoring | Limited; less accurate for dynamic GFR changes | Superior marker for post-transplant renal function monitoring |
| Utility in Critical Care | Limited in ICU; confounded by muscle wasting | High; preferred in ICU settings for early AKI detection |
| Correlation with Inflammation or Other Conditions | Minimal inflammation impact | May be influenced by systemic inflammation |
| Primary Applications | CKD monitoring, basic renal evaluation | Early AKI detection, ICU, cardiovascular risk prediction |
7. Activated clotting time (ACT): A Rapid and Reliable Marker for Monitoring Anticoagulation Therapy
8. Prealbumin: A Marker for Differentiating Catabolic and Anabolic Phases in Critically Ill Patients
9. Clinical Tips: Practical Use of Biomarkers in the ICU
10. Future Advances in Biomarker Utilization in the ICU
11. Conclusion
Author Contributions
Funding
Conflicts of Interest
Abbreviations
| NSE | Neuron-Specific Enolase |
| PCT | Procalcitonin |
| NT-proBNP | N-terminal pro-brain natriuretic peptide |
| SCr | Serum creatinine |
| CysC | Cystatin C |
| TTR | Prealbumin |
| ACT | Activated clotting time |
References
- Zhi M, Huang J and Jin X 2024 Clinical value of serum neuron-specific enolase in sepsis-associated encephalopathy: a systematic review and meta-analysis Syst Rev 13 191.
- Hanin A, Denis J A, Frazzini V, Cousyn L, Imbert-Bismut F, Rucheton B, Bonnefont-Rousselot D, Marois C, Lambrecq V, Demeret S and Navarro V 2022 Neuron Specific Enolase, S100-beta protein and progranulin as diagnostic biomarkers of status epilepticus J Neurol 269 3752–60.
- Vondrakova D, Kruger A, Janotka M, Malek F, Dudkova V, Neuzil P and Ostadal P 2017 Association of neuron-specific enolase values with outcomes in cardiac arrest survivors is dependent on the time of sample collection Crit Care 21 172.
- Sakimura K, Kushiya E, Takahashi Y and Suzuki Y 1987 The structure and expression of neuron-specific enolase gene Gene 60 103–13.
- Marangos P J and Schmechel D E 1987 Neuron Specific Enolase, A Clinically Useful Marker for Neurons and Neuroendocrine Cells Annu. Rev. Neurosci. 10 269–95.
- Feng Q, Wu L, Ai Y H, Deng S Y, Ai M L, Huang L, Liu Z Y and Zhang L N 2017 [The diagnostic value of neuron-specific enolase, central nervous system specific protein and interleukin-6 in sepsis-associated encephalopathy] Zhonghua Nei Ke Za Zhi 56 747–51.
- Kim Y-J, Kim Y H, Youn C S, Cho I S, Kim S J, Wee J H, Park Y S, Oh J S, Lee B K and Kim W Y 2023 Different neuroprognostication thresholds of neuron-specific enolase in shockable and non-shockable out-of-hospital cardiac arrest: a prospective multicenter observational study in Korea (the KORHN-PRO registry) Crit Care 27 313.
- Chung-Esaki H M, Mui G, Mlynash M, Eyngorn I, Catabay K and Hirsch K G 2018 The neuron specific enolase (NSE) ratio offers benefits over absolute value thresholds in post-cardiac arrest coma prognosis Journal of Clinical Neuroscience 57 99–104.
- Scarpino M, Lolli F, Lanzo G, Carrai R, Spalletti M, Valzania F, Lombardi M, Audenino D, Celani M G, Marrelli A, Contardi S, Peris A, Amantini A, Sandroni C, Grippo A, Amantini A, Carrai R, Grippo A, Lanzo G, Lolli F, Masi G, Moretti M, Peris A, Scarpino M, Spalletti M, Bandinelli C, Lombardi M, Contardi S, Marudi A, Audenino D, Rikani K, Ospedale Galliera E O, Marrelli A, Cantisani T A, Celani M G, Fiacca A, Sabadini R and Valzania F 2019 Neurophysiology and neuroimaging accurately predict poor neurological outcome within 24 hours after cardiac arrest: The ProNeCA prospective multicentre prognostication study Resuscitation 143 115–23.
- Mastroianni A, Panella R and Morelli D 2020 Invisible hemolysis in serum samples interferes in NSE measurement Tumori 106 79–81.
- Müller J, Bissmann B, Becker C, Beck K, Loretz N, Gross S, Amacher S A, Bohren C, Pargger H, Tisljar K, Sutter R, Marsch S and Hunziker S 2021 Neuron-Specific Enolase (NSE) Predicts Long-Term Mortality in Adult Patients after Cardiac Arrest: Results from a Prospective Trial Medicines 8 72.
- Macedo R C D, Tomasi C D, Giombelli V R, Alves S C, Bristot M D L U, Locks M F T, Petronilho F, Grandi C, Quevedo J, Dal-Pizzol F and Ritter C 2013 Lack of association of S100β and neuron-specific enolase with mortality in critically ill patients Rev. Bras. Psiquiatr. 35 267–70.
- Davies J 2015 Procalcitonin J Clin Pathol 68 675–9.
- Algeciras-Schimnich A, Preissner C M, Theobald J P, Finseth M S and Grebe S K G 2009 Procalcitonin: a marker for the diagnosis and follow-up of patients with medullary thyroid carcinoma J Clin Endocrinol Metab 94 861–8.
- Meisner M 2014 Update on Procalcitonin Measurements Ann Lab Med 34 263–73.
- Gaïni S, Koldkjaer O G, Pedersen C and Pedersen S S 2006 Procalcitonin, lipopolysaccharide-binding protein, interleukin-6 and C-reactive protein in community-acquired infections and sepsis: a prospective study Crit Care 10 R53.
- Bouadma L, Luyt C-E, Tubach F, Cracco C, Alvarez A, Schwebel C, Schortgen F, Lasocki S, Veber B, Dehoux M, Bernard M, Pasquet B, Régnier B, Brun-Buisson C, Chastre J and Wolff M 2010 Use of procalcitonin to reduce patients’ exposure to antibiotics in intensive care units (PRORATA trial): a multicentre randomised controlled trial The Lancet 375 463–74.
- Jona V, Bharadwaj R, Swindler J and Stokes C 2012 False Negative Procalcitonin Levels in Patients With Positive Blood Cultures Chest 142 230A.
- Chun K, Chung W, Kim A J, Kim H, Ro H, Chang J H, Lee H H and Jung J Y 2019 Association between acute kidney injury and serum procalcitonin levels and their diagnostic usefulness in critically ill patients Sci Rep 9 4777.
- Bayés-Genís A, Santaló-Bel M, Zapico-Muñiz E, López L, Cotes C, Bellido J, Leta R, Casan P and Ordóñez-Llanos J 2004 N-terminal probrain natriuretic peptide (NT-proBNP) in the emergency diagnosis and in-hospital monitoring of patients with dyspnoea and ventricular dysfunction European J of Heart Fail 6 301–8.
- Forfia P R, Watkins S P, Rame J E, Stewart K J and Shapiro E P 2005 Relationship Between B-Type Natriuretic Peptides and Pulmonary Capillary Wedge Pressure in the Intensive Care Unit Journal of the American College of Cardiology 45 1667–71.
- Christenson R H 2008 What is the value of B-type natriuretic peptide testing for diagnosis, prognosis or monitoring of critically ill adult patients in intensive care? Clinical Chemistry and Laboratory Medicine 46.
- Baggish A L, van Kimmenade R R J and Januzzi J L 2008 The differential diagnosis of an elevated amino-terminal pro-B-type natriuretic peptide level Am J Cardiol 101 43–8.
- Christ M and Mueller C 2008 Use of natriuretic peptide assay in dyspnea Dtsch Arztebl Int 105 95–100.
- Smit B, Spoelstra-de Man A M, Girbes A R and De Waard M C 2015 NT-proBNP in cardiopulmonary resuscitated patients treated with mild therapeutic hypothermia is not independently associated with mortality: a retrospective observational study BMC Anesthesiol 15 48.
- Hou J-L, Gao K, Li M, Ma J-Y, Shi Y-K, Wang Y and Zhao Y-F 2008 Increased N-terminal pro-brain natriuretic peptide level predicts atrial fibrillation after surgery for esophageal carcinoma World J Gastroenterol 14 2582–5.
- Kobayashi A, Hashimoto S, Kooguchi K, Kitamura Y, Onodera H, Urata Y and Ashihara T 1998 Expression of Inducible Nitric Oxide Synthase and Inflammatory Cytokines in Alveolar Macrophages of ARDS Following Sepsis Chest 113 1632–9.
- Tanaka T, Narazaki M and Kishimoto T 2014 IL-6 in Inflammation, Immunity, and Disease Cold Spring Harbor Perspectives in Biology 6 a016295–a016295.
- Matthay M A, Ware L B and Zimmerman G A 2012 The acute respiratory distress syndrome J. Clin. Invest. 122 2731–40.
- Chalmers J D, Singanayagam A and Hill A T 2008 C-Reactive Protein Is an Independent Predictor of Severity in Community-acquired Pneumonia The American Journal of Medicine 121 219–25.
- Ware L B, Koyama T, Zhao Z, Janz D R, Wickersham N, Bernard G R, May A K, Calfee C S and Matthay M A 2013 Biomarkers of lung epithelial injury and inflammation distinguish severe sepsis patients with acute respiratory distress syndrome Crit Care 17 R253.
- Gamarra-Morales Y, Molina-López J, Santiago-Ruiz F-C, Herrera-Quintana L, Vázquez-Lorente H, Gascón-Luna F and Planells E 2024 Efficiency of IL-6 in Early Prognosis and Follow-Up in Critically Ill Patients with Septic Shock Diseases 12 298.
- Li L, Yao Y, Feng X, Chen L, Wu R, Chang Y, Lou Q, Pan J and Wang Z 2022 Analysis of Clinical Manifestations and Imaging of COVID-19 Patients in Intensive Care ed M F Hashmi Contrast Media & Molecular Imaging 2022 9697285.
- Boretti A and Banik B 2022 Modulation of Covid-19 cytokine storm by tocilizumab Journal of Medical Virology 94 823–8.
- Zhou Y, Li C, Mei S, Xu Q, Qin S, Feng J, Wang J, Xing S, Wang W, Li F, Zhou Q, He Z, Gao Y, Zhang X and Zhang Z 2024 Identifying risk factors for acute respiratory distress syndrome in critically ill patients: a retrospective study Front. Med. 11 1469291.
- Wu Q, Yang H and Kang Y 2018 Comparison of diagnostic accuracy among procalcitonin, C-reactive protein, and interleukin 6 for blood culture positivity in general ICU patients Crit Care 22 339.
- De Rosa S, Samoni S and Ronco C 2016 Creatinine-based definitions: from baseline creatinine to serum creatinine adjustment in intensive care Crit Care 20 69.
- De Rosa S, Greco M, Rauseo M and Annetta M G 2023 The Good, the Bad, and the Serum Creatinine: Exploring the Effect of Muscle Mass and Nutrition Blood Purif 52 775–85.
- Baxmann A C, Ahmed M S, Marques N C, Menon V B, Pereira A B, Kirsztajn G M and Heilberg I P 2008 Influence of muscle mass and physical activity on serum and urinary creatinine and serum cystatin C Clin J Am Soc Nephrol 3 348–54.
- Lorenz G, Hettwer S, McCallum W, Angermann S, Wen M, Schmaderer C, Heemann U, Roos M, Renders L and Steubl D 2019 Plasma C-terminal agrin fragment and rapid kidney function decline in chronic kidney disease patients Medicine (Baltimore) 98 e15597.
- Shlipak M G, Mattes M D and Peralta C A 2013 Update on cystatin C: incorporation into clinical practice Am J Kidney Dis 62 595–603.
- Peng P, Fu X C, Wang Y, Zheng X, Bian L, Zhati N, Zhang S and Wei W 2024 The value of serum cystatin c in predicting acute kidney injury after cardiac surgery: A systematic review and meta-analysis PLoS One 19 e0310049.
- Ostermann M, Legrand M, Meersch M, Srisawat N, Zarbock A and Kellum J A 2024 Biomarkers in acute kidney injury Ann. Intensive Care 14 145.
- Poventud-Fuentes I, Garnett E, Akcan-Arikan A and Devaraj S 2022 Comparison of Cystatin C and Creatinine-Based Equations with Measured Glomerular Filtration Rate in a Diverse Pediatric Population J Appl Lab Med 7 1016–24.
- Miyazaki S, Iino N, Koda R, Narita I and Kaneko Y 2021 Brain-derived neurotrophic factor is associated with sarcopenia and frailty in Japanese hemodialysis patients Geriatr Gerontol Int 21 27–33.
- Nourie N, Ghaleb R, Lefaucheur C and Louis K 2024 Toward Precision Medicine: Exploring the Landscape of Biomarkers in Acute Kidney Injury Biomolecules 14 82.
- Chew J S C, Saleem M, Florkowski C M and George P M 2008 Cystatin C--a paradigm of evidence based laboratory medicine Clin Biochem Rev 29 47–62.
- Yong Z, Pei X, Zhu B, Yuan H and Zhao W 2017 Predictive value of serum cystatin C for acute kidney injury in adults: a meta-analysis of prospective cohort trials Sci Rep 7 41012.
- Kashani K, Cheungpasitporn W and Ronco C 2017 Biomarkers of acute kidney injury: the pathway from discovery to clinical adoption Clin Chem Lab Med 55 1074–89.
- Bufkin K B, Karim Z A and Silva J 2024 Review of the limitations of current biomarkers in acute kidney injury clinical practices SAGE Open Med 12 20503121241228446.
- Erkinaro T, Moilanen J, Lahtinen J, Mosorin M and Savolainen E-R 2022 The Standard Point-of-Care Hemochron Jr. ACT+ Test in Monitoring Heparin Administration for Cardiopulmonary Bypass in Severe Factor XII Deficiency Journal of Cardiothoracic and Vascular Anesthesia 36 2031–4.
- Chen Y, Phoon P H Y and Hwang N C 2022 Heparin Resistance During Cardiopulmonary Bypass in Adult Cardiac Surgery Journal of Cardiothoracic and Vascular Anesthesia 36 4150–60.
- Roosendaal L C, Hoebink M, Wiersema A M, Blankensteijn J D and Jongkind V 2024 Activated clotting time-guided heparinization during open AAA surgery: a pilot study Pilot Feasibility Stud 10 73.
- Wehner J E, Boehne M, David S, Brand K, Tiede A and Bikker R 2020 Activated Clotting Time (ACT) for Monitoring of Low-Dose Heparin: Performance Characteristics in Healthy Adults and Critically Ill Patients Clin Appl Thromb Hemost 26 1076029620975494.
- Hansen R, Koster A, Kukucka M, Mertzlufft F and Kuppe H 2000 A quick anti-Xa-activity-based whole blood coagulation assay for monitoring unfractionated heparin during cardiopulmonary bypass: a pilot investigation Anesth Analg 91 533–8.
- Yoshinaga K, Otsuka Y, Furukawa T, Amitani S, Kimura N and Sanui M 2021 Correlation between activated clotting time monitoring and heparin concentration measurement in a patient with antiphospholipid syndrome during cardiac valve surgery: a case report JA Clin Rep 7 24.
- Grewal N, Yousef D, Palmen M, Klautz R, Eikenboom J and Wink J 2022 Accuracy of point-of-care coagulation testing during cardiopulmonary bypass in a patient post COVID-19 infection J Cardiothorac Surg 17 108.
- Helin T, Tirri T, Korkala H, Lappalainen K and Joutsi-Korhonen L 2023 Laboratory Assessment of Unfractionated Heparin (UFH) with Activated Clotting Time (ACT) and Anti-Xa Activity during Peripheral Arterial Angiographic Procedure Diagnostics 13 1489.
- McLaughlin K, Rimsans J, Sylvester K W, Fanikos J, Dorfman D M, Senna P, Connors J M and Goldhaber S Z 2019 Evaluation of Antifactor-Xa Heparin Assay and Activated Partial Thromboplastin Time Values in Patients on Therapeutic Continuous Infusion Unfractionated Heparin Therapy Clin Appl Thromb Hemost 25 1076029619876030.
- Keller U 2019 Nutritional Laboratory Markers in Malnutrition JCM 8 775.
- Ingenbleek Y and Young V 1994 Transthyretin (prealbumin) in health and disease: nutritional implications Annu Rev Nutr 14 495–533.
- Dellière S and Cynober L 2017 Is transthyretin a good marker of nutritional status? Clin Nutr 36 364–70.
- Wajner S M, Goemann I M, Bueno A L, Larsen P R and Maia A L 2011 IL-6 promotes nonthyroidal illness syndrome by blocking thyroxine activation while promoting thyroid hormone inactivation in human cells J. Clin. Invest. 121 1834–45.
- Linden M A, Freitas R G B D O N, Teles L O D S, Morcillo A M, Ferreira M T and Nogueira R J N 2024 Transthyretin and Nutritional Status in Critically Ill Adults on Parenteral Nutrition: A Prospective Cohort Study Nutrients 16 2448.
- Devakonda A, George L, Raoof S, Esan A, Saleh A and Bernstein L H 2008 Transthyretin as a marker to predict outcome in critically ill patients Clin Biochem 41 1126–30.
- Sreedhara R, Avram M M, Blanco M, Batish R, Avram M M and Mittman N 1996 Prealbumin is the best nutritional predictor of survival in hemodialysis and peritoneal dialysis Am J Kidney Dis 28 937–42.
- Akashi M, Minami Y, Haruki S, Jujo K and Hagiwara N 2019 Prognostic implications of prealbumin level on admission in patients with acute heart failure referred to a cardiac intensive care unit J Cardiol 73 114–9.
- Lourenço P, Silva S, Friões F, Alvelos M, Amorim M, Torres-Ramalho P, Teles M J, Guimarães J T and Bettencourt P 2013 Does pre-albumin predict in-hospital mortality in heart failure? Int J Cardiol 166 758–60.
- Wang W, Ren D, Wang C-S, Li T and Yao H-C 2019 High sensitivity C-reactive protein to prealbumin ratio measurement as a marker of the prognosis in acute coronary syndrome Sci Rep 9 11583.
- Haltmeier T, Inaba K, Durso J, Khan M, Siboni S, Cheng V, Schnüriger B, Benjamin E and Demetriades D 2020 Transthyretin at Admission and Over Time as a Marker for Clinical Outcomes in Critically Ill Trauma Patients: A Prospective Single-Center Study World J Surg 44 115–23.
- Kim S H, Kim H J, Park K N, Choi S P, Lee B K, Oh S H, Jeung K W, Cho I S and Youn C S 2020 Neuron-specific enolase and neuroimaging for prognostication after cardiac arrest treated with targeted temperature management PLoS One 15 e0239979.
- Westwood M, Ramaekers B, Whiting P, Tomini F, Joore M, Armstrong N, Ryder S, Stirk L, Severens J and Kleijnen J 2015 Procalcitonin testing to guide antibiotic therapy for the treatment of sepsis in intensive care settings and for suspected bacterial infection in emergency department settings: a systematic review and cost-effectiveness analysis Health Technol Assess 19 v–xxv, 1–236.
- Cao Z, Jia Y and Zhu B 2019 BNP and NT-proBNP as Diagnostic Biomarkers for Cardiac Dysfunction in Both Clinical and Forensic Medicine Int J Mol Sci 20 1820.
- Lagos-Arevalo P, Palijan A, Vertullo L, Devarajan P, Bennett M R, Sabbisetti V, Bonventre J V, Ma Q, Gottesman R D and Zappitelli M 2015 Cystatin C in acute kidney injury diagnosis: early biomarker or alternative to serum creatinine? Pediatr Nephrol 30 665–76.
- Tanaka T, Narazaki M and Kishimoto T 2014 IL-6 in inflammation, immunity, and disease Cold Spring Harb Perspect Biol 6 a016295.
- Tolan N V, Vidal-Folch N, Algeciras-Schimnich A, Singh R J and Grebe S K G 2013 Individualized correction of neuron-specific enolase (NSE) measurement in hemolyzed serum samples Clin Chim Acta 424 216–21.
- Mat-Nor M B, Md Ralib A, Abdulah N Z and Pickering J W 2016 The diagnostic ability of procalcitonin and interleukin-6 to differentiate infectious from noninfectious systemic inflammatory response syndrome and to predict mortality J Crit Care 33 245–51.
- Michelhaugh S A and Januzzi J L 2022 Using Artificial Intelligence to Better Predict and Develop Biomarkers Heart Fail Clin 18 275–85.
- Johnson K B, Wei W-Q, Weeraratne D, Frisse M E, Misulis K, Rhee K, Zhao J and Snowdon J L 2021 Precision Medicine, AI, and the Future of Personalized Health Care Clin Transl Sci 14 86–93.
- Vitorino R 2024 Transforming Clinical Research: The Power of High-Throughput Omics Integration Proteomes 12 25.
- Metra M, Nodari S, Parrinello G, Specchia C, Brentana L, Rocca P, Fracassi F, Bordonali T, Milani P, Danesi R, Verzura G, Chiari E and Dei Cas L 2007 The role of plasma biomarkers in acute heart failure. Serial changes and independent prognostic value of NT-proBNP and cardiac troponin-T Eur J Heart Fail 9 776–86.
- C; Méndez Hernández R and Ramasco Rueda F 2023 Biomarkers as Prognostic Predictors and Therapeutic Guide in Critically Ill Patients: Clinical Evidence J Pers Med 13 333.
| Biomarker | Recommended Use | Use with Caution |
|---|---|---|
| NSE | Neurological outcomes after cardiac arrest; reliable with time-based measurements and multimodal tools (SSEPs, EEG, imaging). | Avoid standalone use; factors like hemolysis can inflate levels. Combine with other diagnostic tools. |
| PCT | Bacterial infections and antibiotic guidance; reduces unnecessary antibiotics in clinical algorithms. | Limited for non-bacterial inflammation (e.g., post-surgery, viral); always interpret within clinical context. |
| NT-proBNP | Heart failure diagnosis and management; differentiates cardiac vs. pulmonary dyspnea and monitors disease progression. | May be elevated due to non-cardiac causes (e.g., renal dysfunction, age); careful clinical correlation required. |
| CysC | Early detection of AKI in critically ill patients; more sensitive and specific than SCr. | SCr is slow to detect early AKI and influenced by muscle mass, limiting reliability in critical settings. |
| IL-6 | Systemic inflammation, sepsis, and ARDS tracking; useful for monitoring cytokine storms and treatment responses. | Lacks specificity: elevated levels in trauma, burns, or autoimmune diseases. Correlate with clinical signs. |
| TTR | Nutritional and inflammatory status in critically ill; identifies catabolic/anabolic phases for tailored nutritional interventions. | Not solely a nutritional marker; reflects inflammatory/metabolic changes, requiring contextual interpretation. |
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2025 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (http://creativecommons.org/licenses/by/4.0/).





