1. Introduction
A worsening during anti-tuberculosis therapy is often synonymous of therapeutic failure. However, in some cases the worsening of the patient’s clinical picture as well as the appearance of new signs and/or symptoms constitutes the so-called paradoxical reaction [
1]. Paradoxical reaction after the initiation of anti-tubercular treatment is defined as increased inflammation following effective antimycobacterial treatment. This is a phenomenon that can severely complicate a patient’s recovery, potentially leading to further morbidity and residual deficits. Paradoxical reaction remains poorly understood regarding its pathophysiology and management [
2]. These reactions are more commonly observed in patients coinfected with human immunodeficiency virus (HIV) after the initiation of antiretroviral therapy (ART) [
3]. Paradoxical reactions can also occur in immunocompetent individuals and the syndrome includes a variety of manifestations, such as intestinal perforation, vertebral tuberculosis, tubercular liver abscess, retropharyngeal abscess, endobronchial obstruction, skin abscess and other various syndromes [
4]. This phenomenon is usually diagnosed by excluding other causes of TB worsening, such as drug resistance, treatment failure, adherence issues. The paradoxical reaction represents an important challenge for clinicians as it inevitably leads to a prolonged hospitalization. We report a case of a 25-year-old immunocompetent man who suffered from paradoxical worsening of disseminated TB during anti-TB treatment manifested as osteomyelitis of the foot and disseminated subcutaneous abscesses. Finally, we report a review of the literature regarding the cases described of paradoxical reactions in the last ten years.
2. Case Presentation
A 25-year-old man reported onset of fever, cough and weight loss starting from June 2024. He is an immigrant from Bangladesh and arrived in Italy in November 2023 where he lives in a community together with other immigrated people. However, before arriving in Italy, he faced a long journey crossing several countries including Libya where he spent a certain period in prison with poor sanitary conditions. On July 4th he went to the emergency room, where blood tests showed anemia (Hb 7.4 g/dl) which required blood transfusions. The blood count showed no alterations in the leukocyte formula: WBC 5380/mmc with neutrophils 3500/mmc and lymphocytes 1200/mmc. Renal and liver function were within limits of normal (creatinine 0.94 mg/dl, AST 31 U/L, ALT 30 U/L), with altered inflammation biomarkers (C-reactive protein 7.06 mg/dl). In the emergency room, a CT scan of the chest and abdomen was performed with findings of multiple colliquated lymphadenopathies in the mediastinum, thickening with cavitation in the apical segment of the right upper lung lobe, and multiple hypodense lesions of the spleen. The interferon-gamma release assay (IGRA) was positive. Subsequently, a fibrobronchoscopy was performed with a positive result for Mycobacterium tuberculosis on direct examination, polymerase chain reaction and cultural examination. The same result was obtained from a fine needle aspiration of an hilar lymph node. The search for resistance to first-line anti-tuberculosis drugs has given negative results. Considering the microbiological result, the patient was admitted to the infectious diseases department of Pesaro hospital where antituberculosis therapy was started with isoniazid 300 mg, rifampicin 600 mg, ethambutol 1200 mg and pyrazinamide 1500 mg daily, with consequent clinical improvement and resolution of cough and fever. On 31 July the patient was discharged home with instructions to continue anti-tuberculosis therapy and with the scheduling of blood tests and check-ups.
On August 14th the patient came for a check-up complaining of severe pain in the left foot and ankle with difficult walking. The patient was hospitalized again at the infectious diseases department in Pesaro in order to carry out a series of tests.
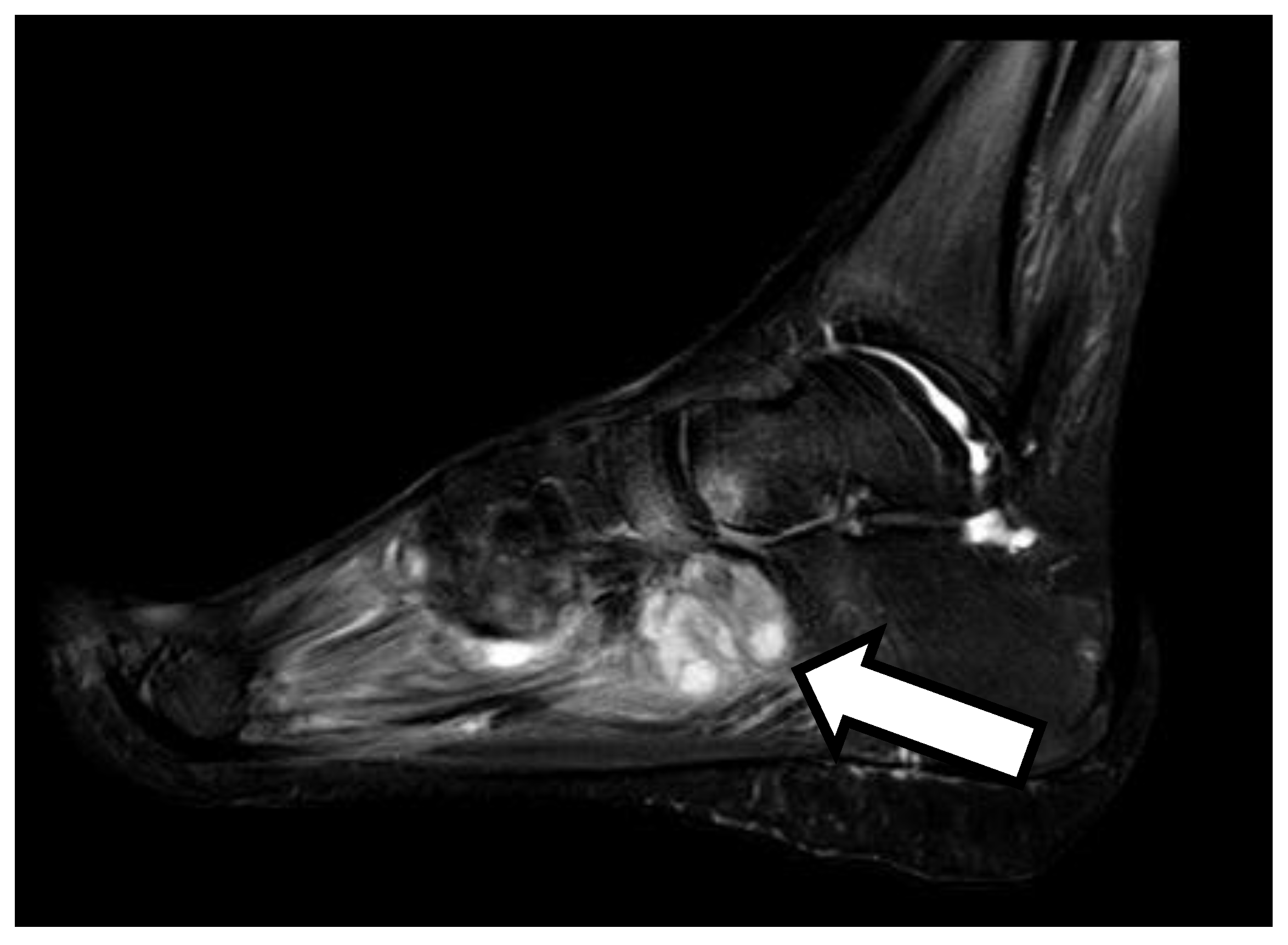
On September 4th, the patient underwent an MRI scan of the foot with findings of osteomyelitis affecting the cuboid bone. A fine needle aspiration of the ankle joint fluid was performed which showed a positive result for Mycobacterium tuberculosis. In consideration of the widespread tuberculosis (lymph nodes, lungs and bones), the anti-tuberculosis therapy was strengthened with a fifth antibiotic with good penetration into the bone tissue, i.e. levofloxacin 750 mg daily, with subsequent resolution of pain and resumption of normal walking.
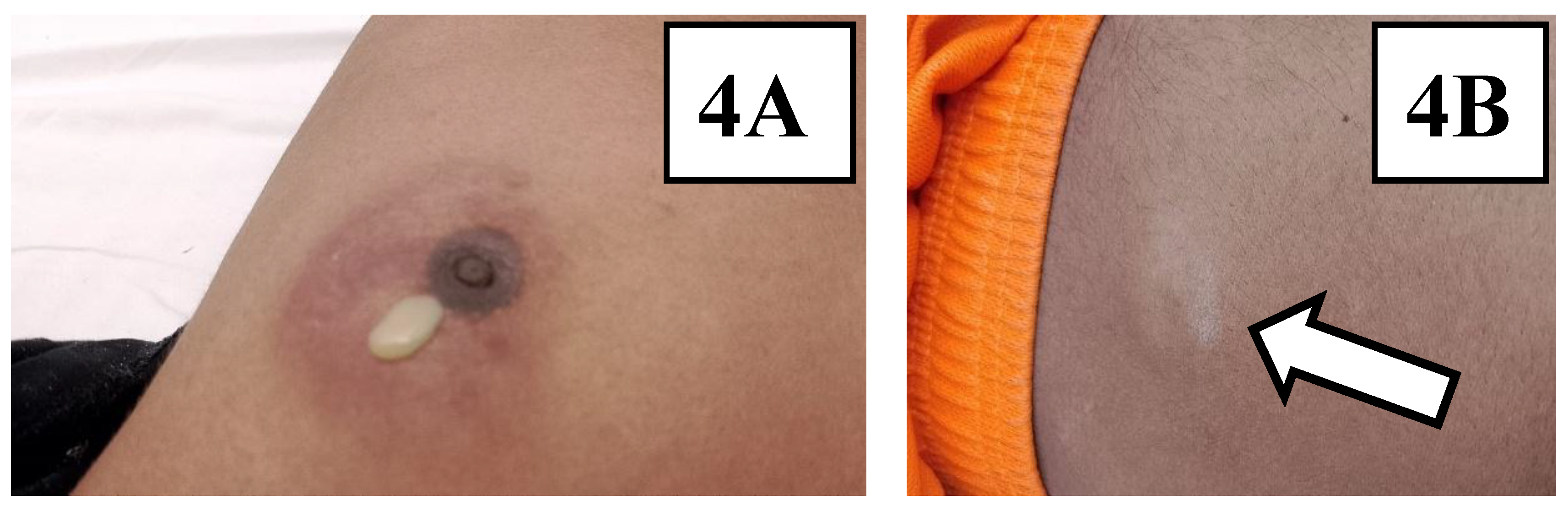
Within a few days the patient showed the appearance of subcutaneous swellings at the left periareolar, right subareolar and right paraumbilical levels. Subsequently, swellings also appeared at the right supraclavicular and left subscapular levels. The swellings appeared with varying degrees of size, erythematous and painful. At the level of the left periareolar swelling, a needle aspiration of purulent fluid was performed with a positive result again for Mycobacterium tuberculosis with the same good drug-sensitivity profile.
The anti-tuberculosis therapy was continued with five drugs (isoniazid, rifampicin, ethambutol, pyrazinamide and levofloxacin) for a period of 6 months and subsequently the therapy with two drugs (isoniazid and rifampicin) was continued with only isoniazid and rifampicin. In January 2025 and February 2025, the skin and subcutaneous swellings were repeatedly drained with the absence of mycobacterium tuberculosis on bacteriological examination.
3. Literature Review
Several cases are described in the literature about immunocompetent people with tuberculosis infection who develop a paradoxical reaction during treatment are described. Here we have selected the cases of paradoxical reactions described in the literature in the last ten years (2014-2024) and concerning immunocompetent adult subjects with tuberculosis infection. We used Pubmed as a search engine. We used the words “paradoxical reaction”, “immunocompetent”, “adult”, “tuberculosis infection”. We subsequently excluded all clinical cases that did not meet our inclusion criteria (e.g. clinical cases concerning tuberculosis infections in immunosuppressed subjects, or cases of tuberculosis infection in pediatric patients). We found 8 cases of paradoxical reactions following the start of anti-tuberculosis therapy in immunocompetent adults [TAB 1]. One of these cases concerns a 19-year-old girl with a significant state of malnutrition. The girl showed cervical lymphadenopathy fistulized, cough, fever and weight loss. Microbiological tests showed positivity for Mycobacterium tuberculosis, so therapy was started first with isoniazid, rifampicin, ethambutol and pyrazinamide, then isoniazid, rifampcin, ethambutol and moxifloxacin for initial alteration of liver function. After 4 weeks of therapy the girl showed the appearance of skin abscesses and new lymphadenopathies. The microbiological tests conducted on the new lesions showed positivity for Mycobacterium tuberculosis, therefore the anti-tuberculosis therapy was continued for 10 months with final resolution of the clinical picture [
5]. In another case, a young 39-year-old man with a history of alcoholism presented with pulmonary and meningeal tuberculosis. During therapy with isoniazid, rifampicin, ethambutol, pyrazinamide and dexamethasone, the patient developed osteoarticular tuberculosis in the thoracic spine. Anti-tuberculosis therapy was continued for 12 months with clinical resolution [
7]. Another case describes a 26-year-old boy with pulmonary tuberculosis who developed intestinal tuberculosis during anti-tuberculosis therapy. In this case, surgery and the continuation of medical therapy made it possible to achieve complete recovery [
8].
4. Discussion
A worsening of the symptoms during tuberculosis, with the appearance of new signs and/or symptoms generally implies therapeutic failure. This occurs in case of failure to take the therapy, in the presence of drug-resistant Mycobacterium tuberculosis or in immunosuppressed patients (for example with HIV infection [
12]). However, in some cases this phenomenon defined as a paradoxical reaction can also occur in otherwise healthy patients and often does not require additional therapy. Similar pictures are described in the literature especially linked to forms of lymph node tuberculosis (LNTB) [
13]. The prevalence of paradoxical reactions associated with LNTB varies from as low as 13.3% to as high as 35.3% [
14]. Paradoxical reaction may occur during antitubercular treatment or be reported even after completion of treatment called post-therapy paradoxical reaction. An onset of paradoxical reaction may occur within a month of therapy to even 12 months from the initiation of an anti-tubercular drug. It is important to consider paradoxical reaction when other causes of clinical or radiological worsening have been ruled out [
15]. In conclusion we report the case of a paradoxical reaction in a healthy patient without risk factors for immunosuppression. The paradoxical reaction must be taken into consideration as a differential diagnosis in all those situations in which the patient shows a worsening of the clinical picture despite the ongoing therapy. In these situations, it is essential to continue anti-tuberculosis therapy despite the apparent clinical worsening. However, further studies are needed to define the pathogenetic mechanisms underlying the paradoxical reaction to find therapeutic targets to counteract this phenomenon.
Supplementary Materials
The following supporting information can be downloaded at the website of this paper posted on Preprints.org.
Author Contributions
all authors contributed to the writing and reviewing of the submitted manuscript.
Funding
No funding was received for this report.
Acknowledgments
Not applicable.
Conflicts of Interest
All the authors report no conflicts of interest
References
- Azoulay, L.-D.; Houist, A.-L.; Feredj, E.; Vindrios, W.; Gallien, S. Réaction paradoxale tuberculeuse. La Rev. de Médecine Interne 2024, 45, 279–288. [Google Scholar] [CrossRef]
- Done, M.M.; Akkerman, O.W.; Al-Kailany, W.; de Lange, W.C.M.; de Jonge, G.; Kleinnijenhuis, J.; Stienstra, R.; van der Werf, T.S. Corticosteroid therapy for the management of paradoxical inflammatory reaction in patients with pulmonary tuberculosis. Infection 2020, 48, 641–645. [Google Scholar] [CrossRef] [PubMed]
- E Namale, P.; Abdullahi, L.H.; Fine, S.; Kamkuemah, M.; Wilkinson, R.J.; Meintjes, G. Paradoxical TB-IRIS in HIV-infected Adults: a Systematic Review and Meta-analysis. Futur. Microbiol. 2015, 10, 1077–1099. [Google Scholar] [CrossRef]
- Alharbi, A.; Aljahdali, A.; Ahamed, M.F.; Almarhabi, H. Left hand abscess as a paradoxical reaction during treatment of disseminated tuberculosis in immunocompetent patient: case report and review of literature. BMC Infect. Dis. 2024, 24, 1186. [Google Scholar] [CrossRef] [PubMed]
- Alharbi, A.; Aljahdali, A.; Ahamed, M.F.; Almarhabi, H. Left hand abscess as a paradoxical reaction during treatment of disseminated tuberculosis in immunocompetent patient: case report and review of literature. BMC Infect. Dis. 2024, 24, 1186. [Google Scholar] [CrossRef] [PubMed]
- Samad, M.; Dallevet, C.A.; Tandjaoui-Lambiotte, Y.; Bourgarit, A.; Jaquet, P. Spectacular Improvement of Paradoxical Reaction in Tuberculosis after Tumor Necrosis Factor-Alpha Antagonist Therapy. Cureus 2023, 15, e50596. [Google Scholar] [CrossRef] [PubMed]
- Volpe-Chaves, C.E.; Lacerda, M.L.G.G.; Castilho, S.B.; Fonseca, S.S.O.; Saad, B.A.A.; Franciscato, C.; Tibana, T.K.; Nunes, T.F.; Venturini, J.; de Oliveira, S.M.D.V.L.; et al. Vertebral tuberculosis as a paradoxical reaction to the treatment of pulmonary and meningeal tuberculosis in an immunocompetent patient. Medicine 2020, 99, e20012. [Google Scholar] [CrossRef] [PubMed]
- Shinga, B.W.; Dièye, A.; Badiane, N.M.D.; Lakhe, N.A.; Diallo, V.M.-P.C.; Mbaye, K.D.; Ka, D.; Badiane, A.S.; Diouf, A.; Déguénonvo, L.F.; et al. Tuberculose intestinale révélée par une occlusion intestinale aigüe au cours d’une réaction paradoxale au traitement anti-tuberculeux chez un patient immunocompétent: à propos d’un cas et revue de la littérature [Intestinal tuberculosis revealed by acute bowel obstruction during paradoxical reaction to antituberculosis treatment in an immunocompetent patient: about a case and literature review]. Pan Afr. Med J. 2019, 32, 173. [Google Scholar] [CrossRef] [PubMed]
- Kabra, M.N.; Kunapareddy, T. Paradoxical Upgradation Response in Non-HIV Tuberculosis: Report of Two Cases. Indian J. Med Microbiol. 2019, 37, 450–453. [Google Scholar] [CrossRef] [PubMed]
- Neki, Nirankar & Joshi, Neeraj & Shergill, Gagandeep & Singh, Amritpal & Meena, Narendra & Shergill, Amanpreet & Dhanju, Amandeep & Vaid, Aarti & Kausahal, Deepali & Resident, Junior & Resident, Senior. (2017). Paradoxical Reaction in an Immunocompetent Internal Medicine Resident Suffering from Tubercular Lymphadenitis.
- Chaskar, P. Treatment Paradox in Musculo- Skeletal Tuberculosis in An Immunocompetent Adult Male; A Case Report from A Tertiary Care Hospital. J. Clin. Diagn. Res. 2015, 9, DD01–2. [Google Scholar] [CrossRef] [PubMed]
- Breen, R.A.M.; Smith, C.J.; Bettinson, H.; Dart, S.; Bannister, B.; A Johnson, M.; I Lipman, M.C. Paradoxical reactions during tuberculosis treatment in patients with and without HIV co-infection. Thorax 2004, 59, 704–707. [Google Scholar] [CrossRef] [PubMed]
- Rai, D.K.; Kant, S.; Gupta, V.B. Paradoxical reaction in peripheral lymph node tuberculosis: a review for its prevalence, clinical characteristics, and possible treatment. Monaldi Arch. Chest Dis. 2023; Epub ahead of print. [Google Scholar] [CrossRef]
- Rai, D.K.; Kant, S.; Gupta, V.B. Paradoxical reaction in peripheral lymph node tuberculosis: a review for its prevalence, clinical characteristics, and possible treatment. Monaldi Arch. Chest Dis. 2023; Epub ahead of print. [Google Scholar] [CrossRef]
- Gallego, B.C.; Moreno-Pérez, D.; Cuadros, E.N.; Fernandez, A.M.; Cantero, M.M.; Pacheco, P.O.; Cardona, A.U. Paradoxical reaction in immunocompetent children with tuberculosis. Int. J. Infect. Dis. 2016, 51, 15–18. [Google Scholar] [CrossRef] [PubMed]
|
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2025 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (http://creativecommons.org/licenses/by/4.0/).