Submitted:
20 February 2025
Posted:
21 February 2025
You are already at the latest version
Abstract
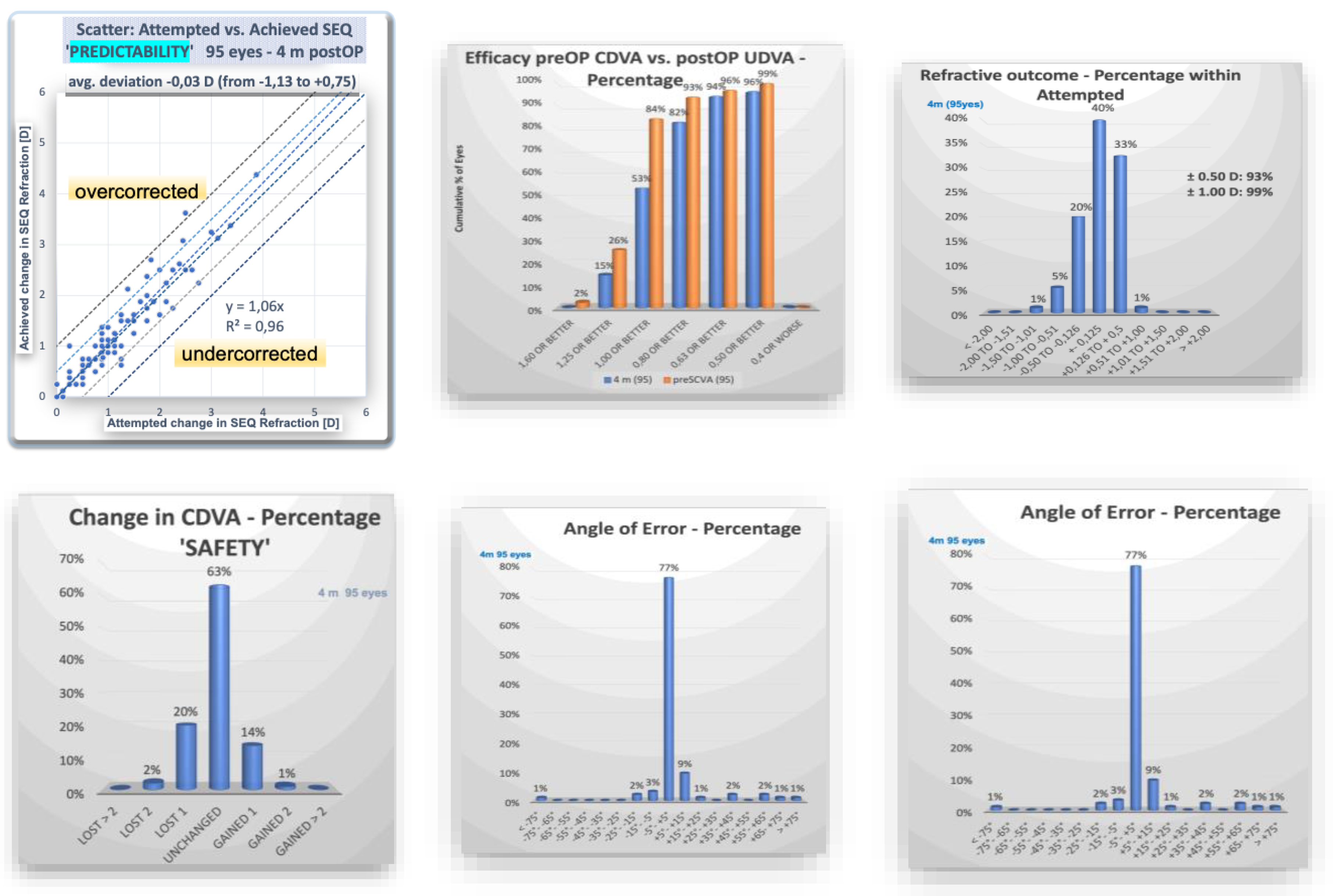
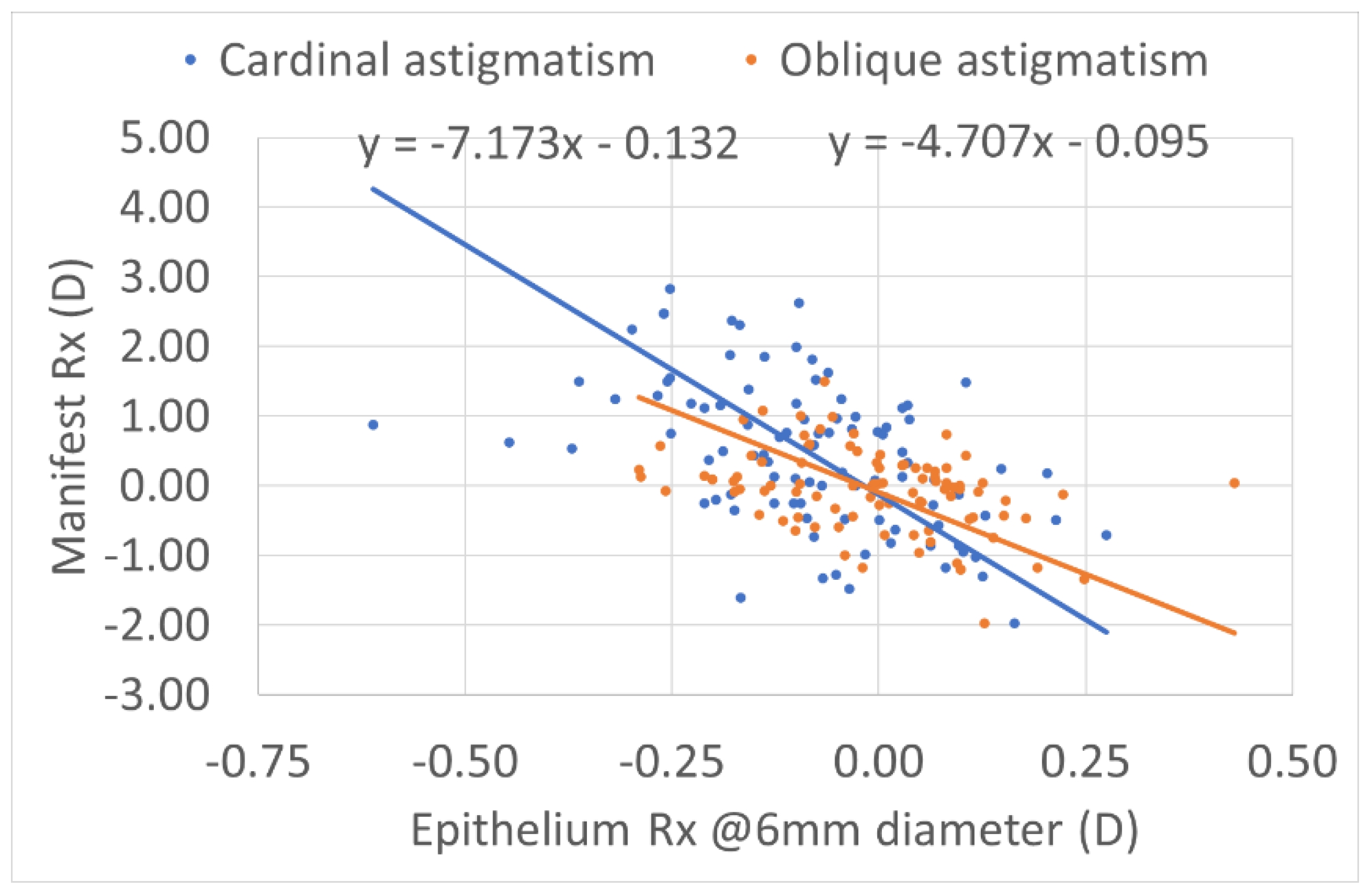
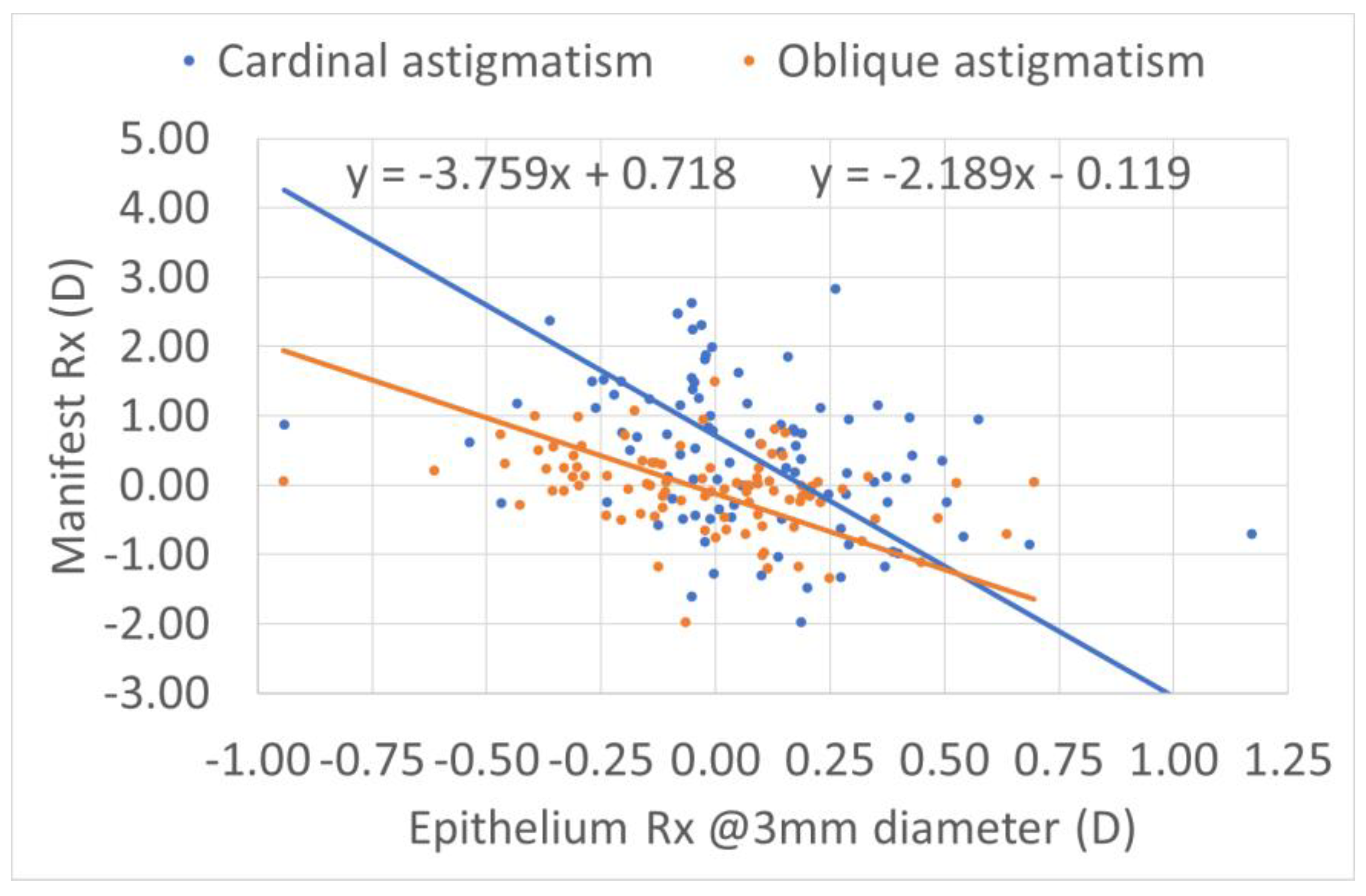
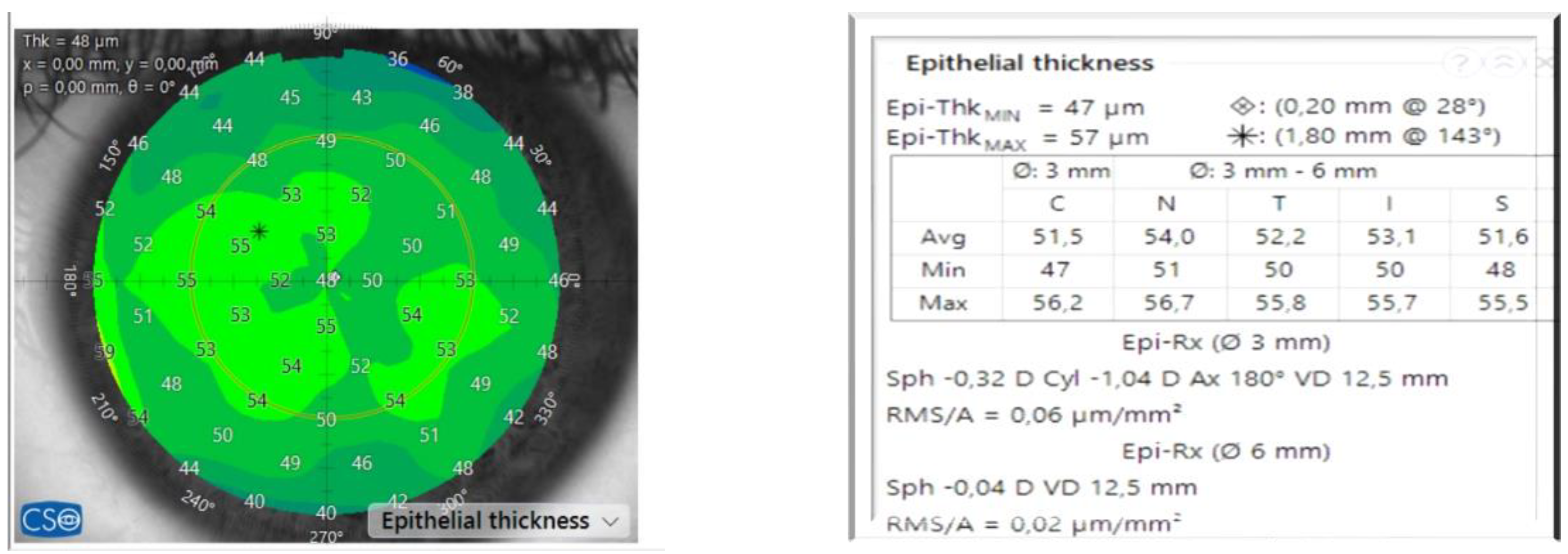
Purpose: To calculate the impact of the refractive power associated with the epithelial thickness in transepithelial refractive corrections Setting: Aurelios Augenzentrum Recklinghausen, Germany Methods: We analyzed the impact of the epithelium in a consecutive retrospective group of hiperopic eyes treated with TransPRK with the AMARIS 1050 RS laser platform (Schwind Eye-Tech Solutions, Kleinhostheim, Germany) with a minimal follow-up of 4 months. The group of 95 treated eyes had an average age of 36 years. The preoperative mean sphere was +1.6 dioptres (D) with a range till +5D, and the mean cylinder was -2.16 D with a range till -5.75D. For the epithelium measurements, we used the anterior segment optical coherence tomography MS-39 (CSO, Florence, Italy). Results: The refractive outcome showed a mean sphere of -0.03 D (range -0.5 to 1 D) and a mean cylinder of -0.33 (range -1.75 to 0 D). 93% and 98% of the cases had 0.5D, 1D, respectively, or less of spherical equivalent refractive error. The epithelium showed preoperative toricity, correlating to the preoperative manifest astigmatism. Preoperatively, at 6 mm, the epithelium showed compensational effect of ~15% of the refractive astigmatism (12% for cardinal and 18% for oblique astigmatism); whereas for 3mm the compensation accounted for ~25% of the refractive astigmatism (21% for cardinal and 31% for oblique astigmatism). No correlation was found postoperatively. Conclusions: The preoperative toricity of the epithelium is correlated with the amount of preoperative refractive astigmatism. No systematic correlation was found between preoperative epithelium and refractive deviations after hyperopia transepithelial treatments.
Keywords:
1. Introduction
2. Materials and Methods
3. Results
4. Discussion
5. Conclusions
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Conflicts of Interest
References
- Aslanides IM, Kymionis GD. Trans advanced surface laser ablation (TransPRK) outcomes using SmartPulseTechnology. Cont Lens Anterior Eye. 2017;40(1):42-46. [CrossRef]
- Seiler T, Kriegerowski M, Schnoy N, Bende T. Ablation rate of human corneal epithelium and Bowman’s layer with the excimer laser (193 nm). Refract Corneal Surg. 1990;6(2):99-102.
- Arba-Mosquera S, de Ortueta D. Geometrical analysis of the loss of ablation efficiency at non-normal incidence. Opt Express. 2008;16(6):3877-3895. [CrossRef]
- Reinstein DZ, Archer TJ, Gobbe M, Silverman RH, Coleman DJ. Epithelial thickness in the normal cornea: three-dimensional display with Artemis very high-frequency digital ultrasound. J Refract Surg. 2008;24(6):571-581. [CrossRef]
- de Ortueta D, Arba Mosquera S, Baatz H. Comparison of standard and aberration-neutral profiles for myopic LASIK with the SCHWIND ESIRIS platform. J Refract Surg. 2009;25(4):339-349. [CrossRef]
- Savini G, Schiano-Lomoriello D, Hoffer KJ. Repeatability of automatic measurements by a new anterior segment optical coherence tomographer combined with Placido topography and agreement with 2 Scheimpflug cameras. Journal of Cataract & Refractive Surgery. 2018;44(4). https://journals.lww.com/jcrs/Fulltext/2018/04000/Repeatability_of_automatic_measurements_by_a_new.10.aspx.
- Reinstein DZ, Archer TJ, Randleman JB. JRS standard for reporting astigmatism outcomes of refractive surgery. J Refract Surg. 2014;30(10):654-659. [CrossRef]
- de Ortueta D, von Rüden D, Verma S, Magnago T, Arba-Mosquera S. Transepithelial Photorefractive Keratectomy in Moderate to High Astigmatism With a Non-wavefront–Guided Aberration-Neutral Ablation Profile. J Refract Surg. 2018;34(7):466-474. [CrossRef]
- de Ortueta D. Transepithelial Photorefractive Keratektomy after a Clear Lens Exchange. Vision (Basel). 2021;5(1). [CrossRef]
- de Ortueta D, von Rüden D, Arba-Mosquera S. Customized versus Standard Epithelium Profiles in Transepithelial Photorefractive Keratectomy. Optics. 2021;2(4):266-275. [CrossRef]
- Simon G, Ren Q, Kervick GN, Parel JM. Optics of the corneal epithelium. Refract Corneal Surg. 1993;9(1):42-50.
- Gatinel D, Racine L, Hoang-Xuan T. Contribution of the corneal epithelium to anterior corneal topography in patients having myopic photorefractive keratectomy. Journal of Cataract and Refractive Surgery. 2007;33(11):1860-1865. [CrossRef]
- Benito A, Redondo M, Artal P. Laser in situ keratomileusis disrupts the aberration compensation mechanism of the human eye. Am J Ophthalmol. 2009;147(3):424-431.e1. [CrossRef]
- Aslanides IM, Padroni S, Arba Mosquera S, Ioannides A, Mukherjee A. Comparison of single-step reverse transepithelial all-surface laser ablation (ASLA) to alcohol-assisted photorefractive keratectomy. Clin Ophthalmol. 2012;6:973-980. [CrossRef]
- Arba Mosquera S, Awwad ST. Theoretical analyses of the refractive implications of transepithelial PRK ablations. Br J Ophthalmol. 2013;97(7):905-911. [CrossRef]
- Luger MHA, Ewering T, Arba-Mosquera S. Consecutive myopia correction with transepithelial versus alcohol-assisted photorefractive keratectomy in contralateral eyes: one-year results. J Cataract Refract Surg. 2012;38(8):1414-1423. [CrossRef]
- Salah-Mabed I, Saad A, Gatinel D. Topography of the corneal epithelium and Bowman layer in low to moderately myopic eyes. Journal of Cataract and Refractive Surgery. 2016;42(8):1190-1197. [CrossRef]
| n=95 eyes | ||||
| Gender | female | 46.3% (44 eyes) | male | 53.7% (51) eyes) |
| eye | left | 51.6% (49 eyes) | right | 48.4% (46 eyes) |
| Preoperatively | range | Postop 4m | range | |
| SEQ | +0.53 +/- 1.34 D | (-1.75 to +3.88 D) | -0.03 +/- 0.3 D | (-1.13 D to +0.75 D) |
| Sphere | +1.6 +/- 1.16 D | (+0.12 to +6 D) | +0.13 +/- 0.29 D | (-0.5D to +1 D) |
| Cyl | -2.16 +/- 1.32 D | (-5.75 to -0 D) | -0.33 +/- 0.38D | (-1.75 D to 0 D) |
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2025 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (http://creativecommons.org/licenses/by/4.0/).





