1. Introduction
One of the leading challenges in laser refractive surgery is the postoperative corneal ectasia. In order to avoid this, it was the most important to detect keratoconus (KC) in its earlier stage, named forme fruste KC (FFKC), preclinical or subclinical KC, and keratoconus suspect (KCS) [
1,
2,
3,
4,
5]. FFKC was the fellow eye of a clinical KC without any clinical findings [
1,
4,
5,
6]. Preclinical or subclinical KC was the fellow eye of a clinical KC, but some clinical findings such as I-S asymmetry and/or bowtie pattern [
2,
5]. KCS showed several findings such as focal steep keratmetric curvature more than 47.0D, peripheral corneal asymmetry, etc. but do not result in visual impairment compared to keratoconus (KC) resulting in visual impairment [
1,
2,
3,
4,
5,
6]. Until now definition of KCS is not defined [
5,
6,
7,
8,
9]. Recently Scheimpflug corneal topography and epithelial mapping by corneal OCT were currently used [
10,
11,
12]. Of suspected findings of KCS, steep keratometric curvature greater than 47.0 D and peripheral corneal thickness asymmetry (SUM ≥80 µm) could be the most important to determine laser refractive surgery in myopic patients with KCS [
1][
18], because of an absolute contraindication to LASIK or photorefractive keratectomy (PRK) due to postoperative ectasia [
1][
29], possibly because the postoperative thinner cornea could be moved forward due to corneal biomechanical interaction of corneal thickness, corneal stiffness and IOP, resulting in optical aberrations [
22,
23,
24,
25,
26,
27,
28,
29].
Recently asymmetric corneal ablation methods were tried to make asymmetric cornea of KC, corneal ectasia or KCS be symmetric postoperatively with selective ablation of the thicker portion of the cornea [
30,
31,
32,
33]. In KC, a novel approach to reshape the ectatic cornea by means of crescent keratectomy performed with an excimer laser using a mask showed improvement in visual acuity, keratometry and corneal topography at 1 year postoperatively [
30]. In corneal ectasia,8-mm diameter keratectomy (180°, 270°, or 360°) with femtosecond laser platform and the edges of the resection and sutured showed corneal flattening, reduction of anterior chamber, and decreased optical aberrations at 3 year postoperatively [
31]..And also in myopic patients of KCS with peripheral asymmetry of corneal thickness (SUM) ≥80 µm) and focally steep keratometric curvature greater than 47.0D of the thinner corneal portion, asymmetric corneal crescentic ablation (customized ablation) on the thicker peripheral cornea quantitively, and customizedly with LAK and original ablation of the refractive errors simultaneously to make the symmetric cornea and correct the refractive errors postoperatively could be safe postoperative and showed good outcomes without postoperative ectasia and focal corneal steepening [
32,
33]. Postoperative corneal symmetry was the important facter in clinical outcomes. DISTANCE and SUM on an Orbscan map as the evaluating indices featured a central visual axis and, thus, they are very useful for measuring symmetry [
13,
14,
15,
16,
17,
18].
LAK as a customization method reported excellent clinical outcomes with symmetric cornea in patients with peripheral asymmetric cornea with only selective ablation of thicker peripheral cornea analysed with the Vision-Up software (WellC, Busan, Republic of Korea) approved in the Republic of Korean, Food and Drug Administration (FDA) in 2021 [
13,
14,
15,
16,
17,
18,
32,
33].
L-LAK could correct the refractive errors (original ablation) and make the cornea be symmetric simultaneously by decreasing the SUM and DISTANCE with customization ablation (crescentic customized ablation), decreased the steep keratometric curvature of the cornea (Kmax) [
13,
14,
15,
16,
17,
18,
32,
33], and could show good postoperative corneal symmetry and visual outcomes without postoperative corneal ectasia in myopic patients with KCS [
32,
33].
The purpose of our study was to report the change in corneal symmetry and clinical outcomes after L-LAK in myopic patients with KCS manifesting peripheral corneal asymmetry (SUM) ≥80 µm) and steep keratometric curvature greater than 47.0 D on the thinner corneal portion by evaluating corneal regularity regularity in order to avoid the postoperative corneal ectasia which is one of the leading challenges in laser refractive surgery without LAK.
2. Materials and Methods
This study included 20 eyes of 14 patients who received L-LAK at the Woori Eye Clinic between March 2021 and December 2021. KCS was diagnosed as corneal topography findings with abnormal localized steep keratometric curvature greater than 47.0 D or an asymmetric bowtie pattern, a normal-appearing cornea on slit lamp biomicroscope, and at least 1 of the following signs: peripheral corneal thickness asymmetry (SUM≥80 µm), oblique cylinder greater than 1.50 D, central corneal thickness less than 500 µm, or clinical KC in the fellow eye [
1,
2,
3,
4,
5,
6,
7,
8,
9].
The inclusion criteria were patients with KCS manifesting both steep keratometric curvature greater than 47.0 D on the thinner corneal portion and a SUM of ≥80 µm [
1][
18], receiving operation of L-LAK, also manifesting myopia >-1.50 diopter, 20/20 or better in CDVA, and postoperative follow-up check over 1 year. Patients with follow-up examination under 1 year, and history of other ocular operations, corneal scarring, pregnancy, glaucoma, and causes of ocular astigmatism were excluded.
Refractive errors were corrected with L-LAK using excimer laser (Kera Havest Inc,Taiwan) by the same doctor (BM Min) and with the same method (L-LAK) under topical anesthesia (Alcaine, Alcon NV, Belgium). for all patients [
13,
14,
15,
16,
17,
18,
32,
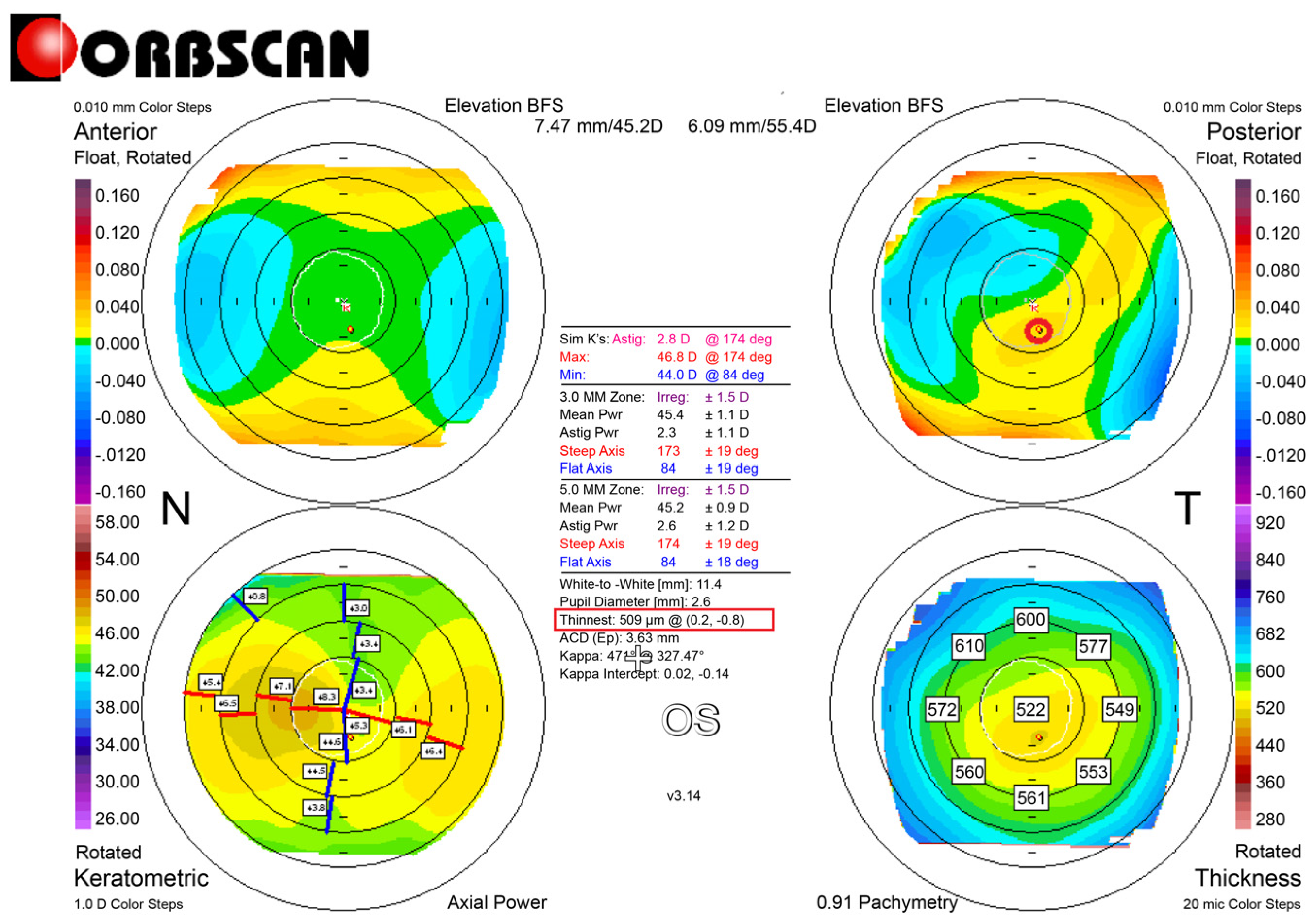
33]. The 7.0 mm optic zone and 7-9 mm in transitional zone were ablated for correcting refractive errors without epithelium of a 10.0–10.5mm in diameter for LASEK. After analyzing the thicker corneal regions with the Vision-Up software (WellC, Republic of Korea) on topography (
Figure 1) [
13,
14,
15,
16,
17,
18,
32,
33], we operated original ablation for original refractive errors (
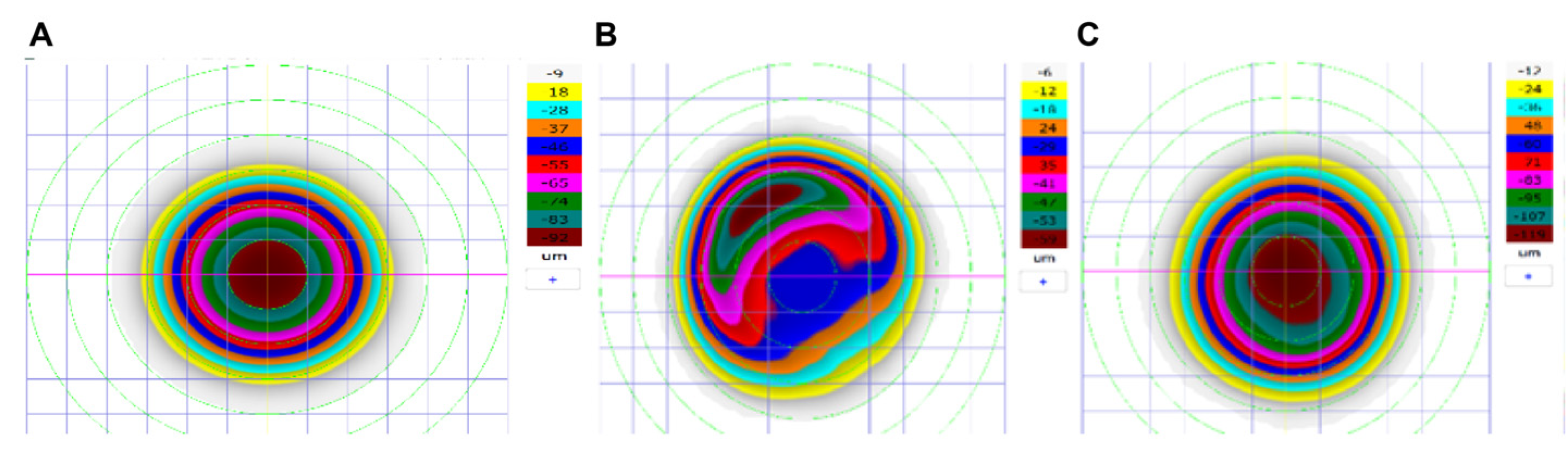
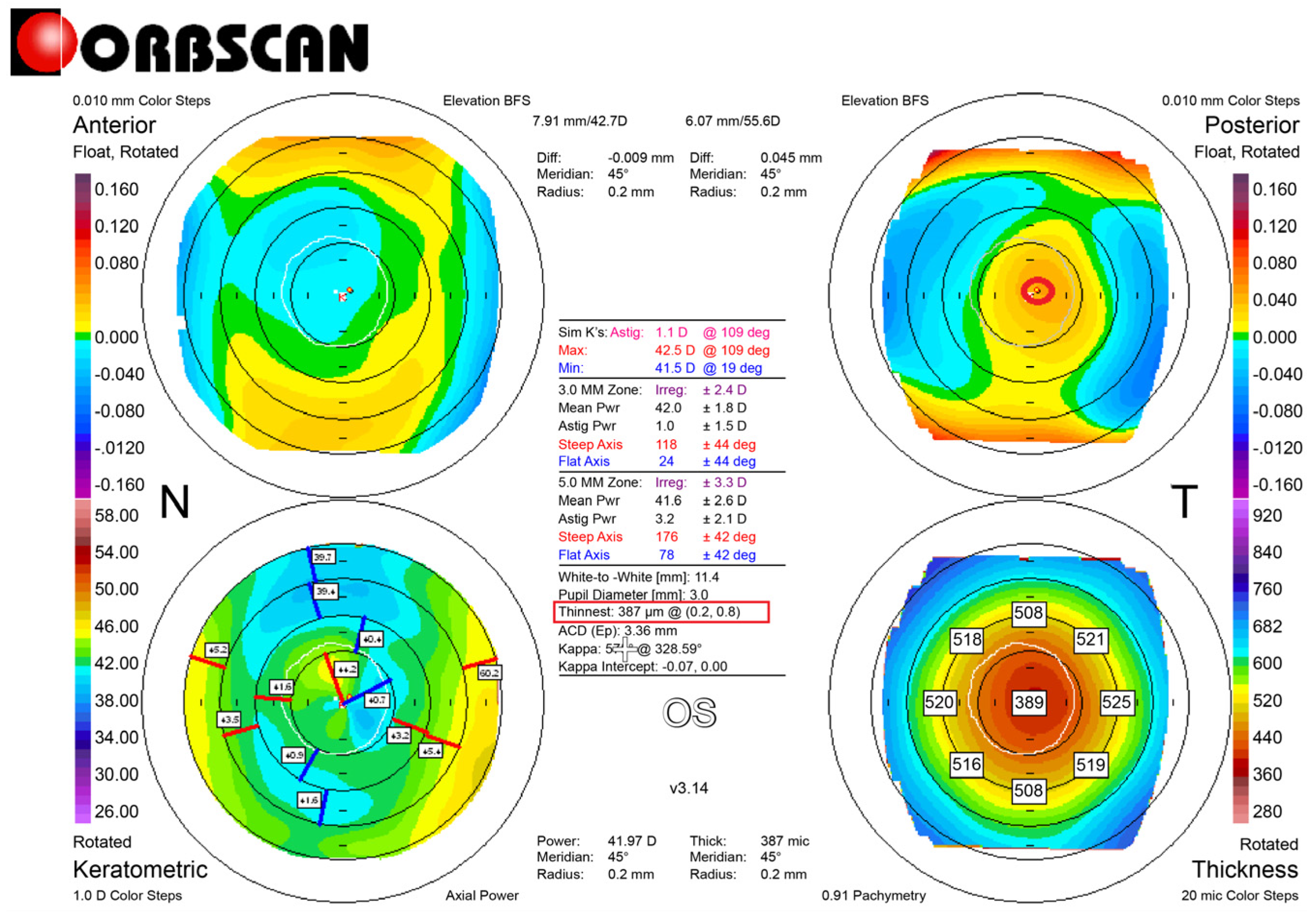
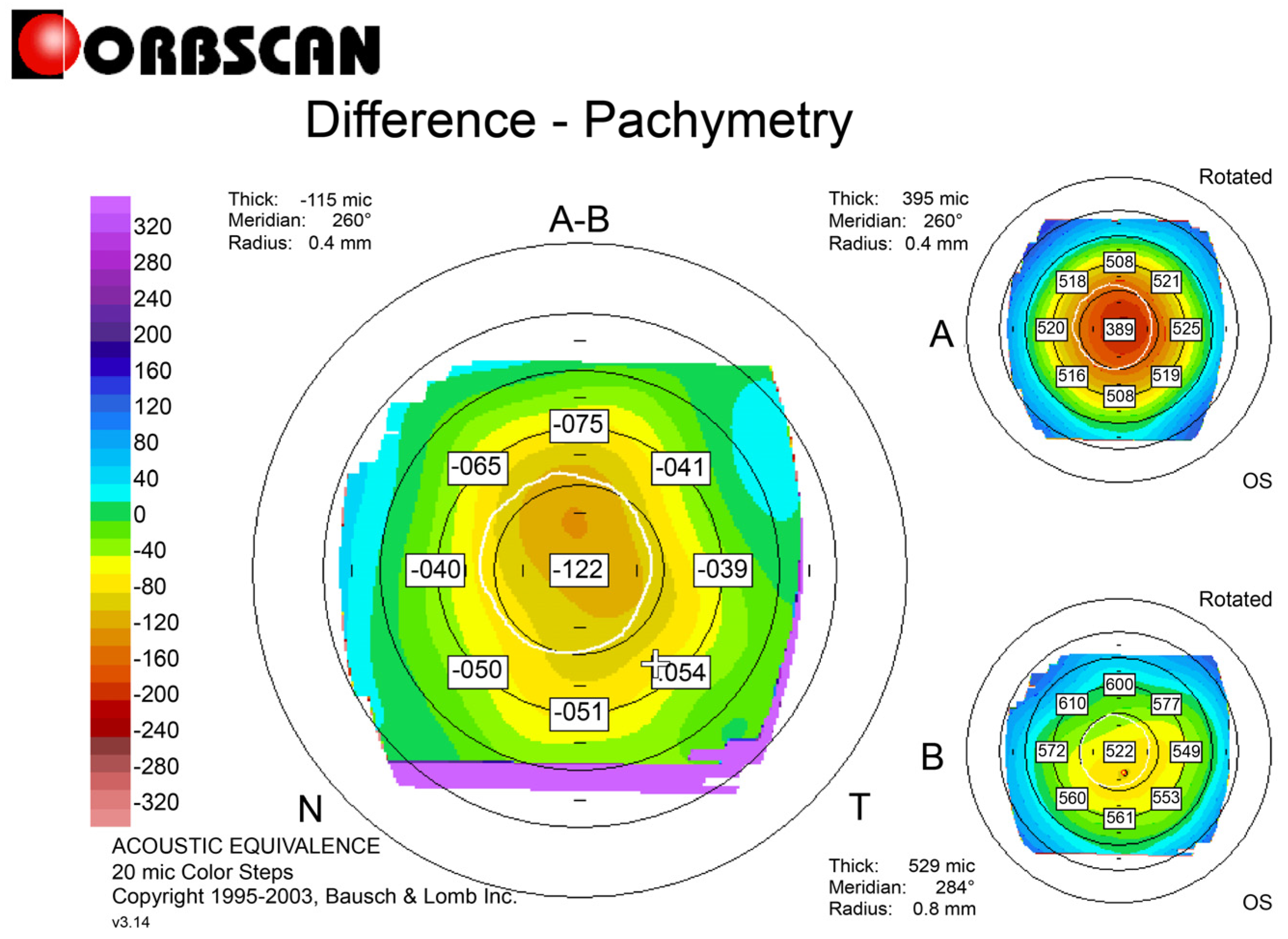
Figure 2A) and crescentic customized ablation (
Figure 2B) for both the thicker peripheral cornea and the central cornea to correct induced myopia due to LAK simultaneously with the same laser machine Therefore, we can correct both refractive errors and corneal morphology to be symmetric cornea (total ablation) (
Figure 2C,
Figure 3 and
Figure 4) [
13,
14,
15,
16,
17,
18].
The following variables were analyzed the pre- and the postoperative 1 year: UDVA measuring at a distance of 6 m, CDVA, spherical equivalent (SE), sphere, cylinder, keratometry (Kmean, Kmax), intraocular pressure (IOP), central pachymetry (CP), pupil size, SUM (µm), DISTANCE (mm), kappa angle, TBUT (second), tear osmolarity (mOsmol/L). The refraction with an auto refractometer/keratometer was calculated as the SE. UDVA was converted to the logarithm of the minimum angle of resolution (LogMAR). IOPs were measured by applanation tonometer. CP, pupil size, angle kappa were measured on Orbscan. II. At pre- and postoperative corneal symmetry were evaluated by SUM and DISTANCE on Orbscan maps (
Figure 1,
Figure 3 and
Figure 4) [
13,
14,
15,
16,
17,
18,
32,
33]. TBUT, tear osmolarity were measured with Keratograph 4 (Oculus, Germany).
For statistical analyses, the paired t test was used in case of variables following normal distribution and Wilcoxan signed rank test is used in case of variables not following normal distribution. P value of less than 0.05 was considered to be statistically significant. The data analysis was done using IBM SPSS software version 25. Refractive outcomes were used standard graphs and terms for refractive surgery results, and data analysis was done using Microsoft Excel and R software version 4.2.3.
3. Results
The age was 41.0±13.5 years of twenty patients (7 males and 13 females). 14 patients received operation of both eye, 6 ones of one eye, and follow up periods (months) were 24.1±2.3 (
Table 1). For laser ablation, optic zone (mm) in L- LAK was 6.35±0.09, ablation depths (µm) of central cornea was 64.53±24.41 for L-LAK, induced myopic (diopters) due to LAK was -1.92±0.48, residual stromal depth (µm) was 444.26±36.20 at L-LAK (
Table 2).
From preoperative to postoperative 1 year findings, SE (diopters) were from -2.57±1.64 to -0.40±0.43 (p=0.001). Sphere (diopters) were from -2.12±4.31 to -0.21±0.43 (P=0.001). Cylinder (diop ters) were from -1.02±2.27 to -0.45±0.42 (P=0.003). There were no cylindrical axial changes. The IOPs and pupil size of the patients were similar between preoperative and postoperative (Ps>0.05) (
Table 3). Kmean (diopters) and focal steep keratometric curvature (Kmax) had decreased from +45.23±0.93 to +42.67±1.84, and +48.21±0.89 to +44.47±1.38, respectively (Ps =0.001), and the CP (µm) had decreased from 568.32±32.33 to 521.68±49.98 (P=0.001) (
Table 4). Further, for corneal symmetry SUM, DISTANCE had decreased postoperatively (from 141.88±48.24 to 66.21±15.22 µm, from 1.11±1.14 to 0.46±0.40 mm, respectively) (Ps=0.001), kappa angle (degree) had decreased postoperatively (from 4.58±1.19 to 2.42±1.75) (P=0.02) (
Table 4,
Figure 1 and
Figure 3). TBUT (second) had markedly increased from 8.51±2.97 to 19.39±3.69 (P=0.001), but tear osmolarity (Osm/L) had decreased from 0.55±0.15 to 0.23±0.12 (P=0.001) (
Table 4).
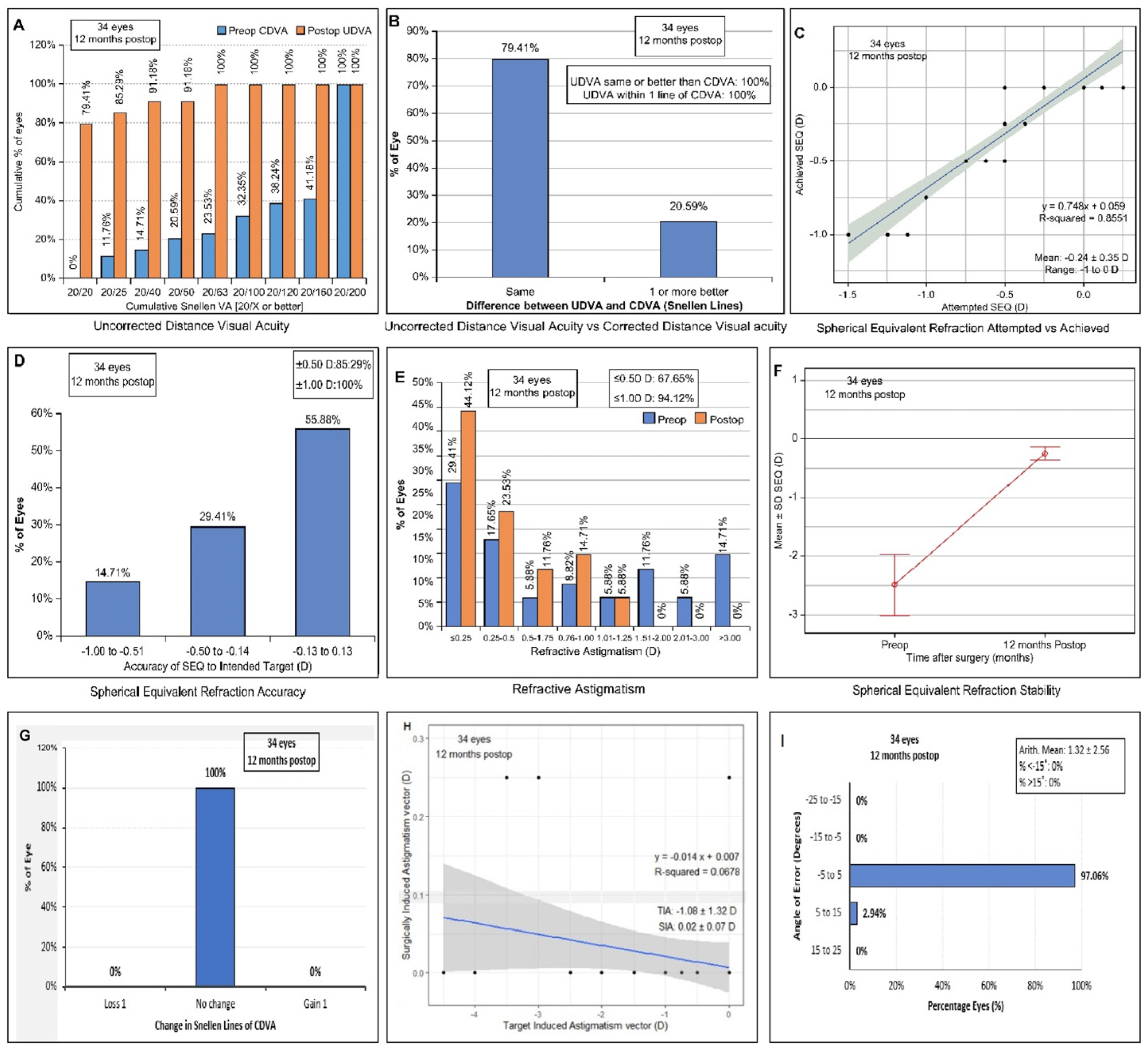
Standard graphs summarizing refractive outcomes are shown in
Figure 5. As can be seen, 79.4% (27/34) of eyes included eyes had an UCVA of 20/20 or better (
Figure 5A). 100% percent of eyes had no changes of CDVA. 79.4% were the same of both UDVA and CDVA,20.6% were better in CDVA than UDVA (
Figure 5B). 55.9% of all eyes had a plano refraction. 29.4% of eyes had a SE within 0.50D of intended (
Figure 5C,D). At 1 year postoperative, 44.1% (12/34) had ≤0.25 D of residual astigmatism, 23.5% had ≤0.50 D of residual astigmatism (
Figure 5E), 97.1 % of all eyes had refractive astigmatism angle of error within 5 degree (
Figure 5I). SE had stability of -0.40±0.43 D (
Figure 5F), no changes in Snellen line of CDVA were showed (
Figure 5G), surgically induced astigmatism vector decreased (
Figure 5H). No postoperative corneal ectasia was showed.
4. Discussion
This study showed all patients with KCS showed steep keratometric curvature greater than 47D, and thinnest pachymetry were 568.32±32.33μm in the patients, much higher than the 500-μm one of criteria of keratoconus suspect. But the important finding was SUM and DISTANCE, The more amounts of the SUM and DISTANCE, the more the postoperative thinner cornea could be moved forward due to corneal biomechanical interaction of corneal thickness, corneal stiffness and IOP, resulting in optical aberrations. In the patients SUM showed 141.88±48.24μm, preoperatively that showed higher than that of the symmetric cornea (SUM <80 μm), but postoperatively decreased to 66.21±15.22 µm that mean symmetric cornea, and also DISTANCE had decreased from 1.11±1.14 mm preoperatively to 0.46±0.40 mm postoperatively. We employed the Orbscan maps for corneal topography visualization rather than the current Sheimpflug techniques. DISTANCE and SUM can be calculated only on an Orbscan map because these maps feature a central visual axis and, thus, they are very useful for measuring symmetry
True KCS is an absolute contraindication to LASIK or photorefractive keratectomy (PRK) due to postoperative ectasia [
19,
20,
21,
22,
23,
24,
25,
26,
27,
28,
29]. But in this study L-LAK showed good postoperative 1 year outcomes without corneal ectasia and focal corneal steepening, because L-LAK could correct refractive errors (original ablation) and also make the cornea to be symmetric with ablating thicker peripheral cornea selectively (crescentic customized ablation). And also postoperative corneal symmetry evaluated with the SUM and DISTANCE on Orbscan map increased markedly, and focal steep keratometric curvature markedly decreased postoperatively, and also SE and UDVA showed good outcomes without postoperative corneal ectasia and focal corneal steepening.
When the SUM is >80 µm, that is, asymmetric cornea, biomechanical interaction of corneal thickness, corneal stiffness, IOP causes steepening of thinner regions easily at postoperative, leading inducing to corneal ectasia [
13,
14,
15,
16,
17,
18,
22,
23,
24,
25,
26,
27,
28,
29]. Postoperative corneal symmetry was one of the key findings to maintain good outcomes without postoperative corneal ectasia [
13,
14,
15,
16,
17,
18].
So, in this study we compared mainly focal steepen keratometric curvature (Kmax) and peripheral corneal thickness asymmetry (SUM and DISTANCE) between preoperative and postoperative 1 year. Keratometric curvature (Kmax) had decreased from +48.21±0.89 preoperatively to +44.47±1.38 postoperatively. The SUM and DISTANCE were markedly decreased postoperatively and are the important parameter to evaluate the outcomes [
13,
14,
15,
16,
17,
18]. In this study an Orbscan map can calculate SUM and DISTANCE. This corneal topography was quite useful for measuring the symmetry of the cornea centered on the visual axis [
13,
14,
15,
16,
17,
18]. But for detecting the earlier stage of KC, corneal aberrometry findings such as the posterior coma to 90° with Scheimpflug topography and focal epithelial thinning and epithelial thickness in the thinnest corneal zone with anterior corneal OCT are currently used as an indicator [
10,
11,
12]. But until now definition of KCS is not defined.
Vision-Up software (Well C, Republic of Korea) was newly developed and approved in Republic of Korea, FDA and calculated corneal customized ablation plan (amounts of thicker cornea, the direction of laser ablation, and induced myopia due to LAK), so could be possible to be symmetric cornea and also correct the original refractive errors simultaneously [
13,
14,
15,
16,
17,
18,
32,
33]. L-LAK could correct refractive errors (original ablation) and also improve corneal symmetry with reducing SUM and DISTANCE (crescentic customized ablation), and also could avoid post-LASIK adverse effects including corneal ectasia in myopic patients with asymmetric corneal thickness (SUM Orbscan maps >80 µm) [
14,
15,
18,
32,
33]. LAK could be new corneal remodeling method to make symmetric cornea on KCS with peripheral asymmetry of corneal thickness [
32,
33].
It is difficult to compare visual outcomes from this study with the other study because inclusion/exclusion criteria and testing methodologies are different. Additionally, in this study all cases are asymmetric cornea and the earlier stage of KC, so main goal of treatment was to make corneal morphology be corrected to be symmetric, another aspect was the patients’s aged the middle aged over 40-year-old, so need residual myopia for near vision planned.
In this study, the postoperative Kmax was flatten and also TBUTs (seconds) were markedly increased over 15 seconds. Most patients did not complain from dry eye and blurring postoperatively. It could be expected that uneven corneal curvature due to focal steepening cornea at pre-L-LAK make the tear break easily due to tear flowing down, but even corneal curvature by flattening of the steepening cornea postoperatively keep the tear layer intact and well maintained stabilization [
32,
33,
34,
35,
36]. So uneven corneal curvature due to peripheral asymmetric corneal thickness maybe have correlation with dry eye, further researches will be needed.
Corneal remodeling with LAK increases corneal symmetry by decreasing SUM to avoid postoperative corneal changes [
13,
14,
15]. L-LAK can customizedly ablate thicker areas of the cornea and correct the refractive errors simultaneously compared to conventional laser refractive surgery only, which symmetrically ablate the cornea to correct the refractive errors centrally, so it will be safe in correct myopic patients with KCS, especially with focal steep keratometry curvature greater than 47D, without postoperative corneal ectasia. Additionally, a corneal remodeling with LAK could be indicated to: 1) avoid laser refractive surgery adverse effects in patients with SUM ≥80 µm [
1][
15,
18], 2) a novel enhancement in patients with myopic regression after laser refractive surgery [
16,
17], 3) manage postoperative corneal adverse of cataract or glaucoma operations [
17,
37]. In the future, in cataract surgery with poor corneal shape, simultaneously performing Femto-LAK (LAK performed by Femtosecond laser) will be necessary to improve optical aberrations by corneal remodeling, and 4) new treatment in early KC or KCS with peripheral asymmetry of the corneal thickness [
28,
29,
32,
33]. Further research on LAK as customization method will be needed.
This study has several limitations that should be considered when interpreting the results: First, it was a single center retrospective study; therefore, there may have been some selection bias. Second, the sample size was relatively small, and relatively short follow up, 1 year. Third, it was not comparative study between L-LAK and conventional laser refractive surgery in KCS. Fourth, there is no information on HOA, biomechanical datas Finally, only Korean patients were included; thus the findings may not be generalizable to other ethnic group
In conclusion, L-LAK resulted in a decreased SUM and DISTANCE, increased corneal symmetry, no postoperative corneal ectasia, and increased TBUT with good visual outcomes in myopic patients with keratoconus suspect manifesting peripheral corneal asymmetry (SUM) ≥80 µm) and focal steep keratometric curvature greater than 47D..
Author Contributions
Conceptualization, H.J.C., B.M.M.; Data curation: B.M.M.; Formal analysis: H.J.C.; Investigation, H.J.C., B.M.M.; Methodology, H.J.C., B.M.M.; Project administration, H.J.C.; Resources, H.J.C., B.M.M.; Software, H.J.C., B.M.M.; Supervision, H.J.C., B.M.M.; Validation, H.J.C.; Visualization, H.J.C., B.M.M.; Writing – original draft, H.J.C., B.M.M.; Review & editing, H.J.C., B.M.M. All authors have read and agreed to the published version of the manuscript.
Funding
The research received no funding.
Institutional Review Board Statement
This study was conducted in accordance with the Helsinki Declaration of 1975, as revised in 1983, and approved by the Korean National Institute for Bioethics Policy (approval No P01-202209-01-024, the date of approval is September 16,2022) as retrospective study.
Informed Consent Statement
Written informed consent was obtained from all subjects involved in the study for publication of the details of their medical case and any accompanying images.
Data Availability Statement
The datasets generated and/or analyzed during the current study are not publicly available due to privacy and ethical reasons but are available from the corresponding author on reasonable request.
Acknowledgments
We would like to thank Editage (
www.editage.co.kr) for statistical analysis and English language editing, and Hye Won Jung, Rag Seon Han, Eun Mi Jang, Ji Yeon Choi, Mi Kyung Kim, Ji Suk Kwon, and Sun Hee Lee at the Woori Eye Clinic for assisting with the ocular examinations.
Conflicts of Interest
The authors declare that they have no competing interests.
Abbreviations
The following abbreviations are used in this manuscript:
| BFS |
best-fit-sphere |
| CP |
central pachymetry |
| FDA |
Food and Drug Administration |
| FFKC |
forme fruste keratoconus |
| IOP |
intraocular pressure |
| KC |
keratoconus |
| KCS |
keratoconus suspect |
| LASEK |
laser epithelial keratomileusis |
| L-LAK |
laser asymmetric keratectomy |
| PRK |
photorefractive keratectomy |
| SE |
spherical equivalent |
References
- Klyce, S.D. Chasing the suspect: keratoconus. Br J Ophthalmol 2009, 93, 845–847. [CrossRef]
- De Sanctis, U.; Aragno, V.; Dalmasso, P.; Brusasco, L.; Grignolo, F. Diagnosis of subclinical keratoconus using posterior elevation measured with 2 different methods. Cornea 2013, 32, 911–915. [CrossRef]
- Waring, G.O. Nomenclature for keratoconus suspects. J Refract Surg 1993, 9, 219–222. [CrossRef]
- Saad, A.; Gatinel, D. Evaluation of total and corneal wavefront high order aberrations for the detection of forme fruste keratoconus. Invest Ophthalmol Vis Sci 2012, 53, 2978–2992. [CrossRef]
- Shi, Y. Strategies for improving the early diagnosis of keratoconus. Clin Optom (Auckl) 2016, 8, 13–21. [CrossRef]
- Vazirani, J.; Basu, S. Keratoconus: current perspectives. Clin Ophthalmol 2013, 7, 2019–2030. [CrossRef]
- Li, X.; Yang, H.; Rabinowitz, Y.S. Keratoconus: classification scheme based on videokeratography and clinical signs. J Cataract Refract Surg 2009, 35, 1597–1603. [CrossRef]
- Schlegel, Z.; Hoang-Xuan, T.; Gatinel, D. Comparison of and correlation between anterior and posterior corneal elevation maps in normal eyes and keratoconus-suspect eyes. J Cataract Refract Surg 2008, 34, 789–795. [CrossRef]
- Rao, S.N.; Raviv, T.; Majmudar, P.A.; Epstein, R.J. Role of Orbscan II in screening keratoconus suspects before refractive corneal surgery. Ophthalmology 2002, 109, 1642–1646. [CrossRef]
- Castro-Luna, G.; Pérez-Rueda, A. A predictive model for early diagnosis of keratoconus. BMC Ophthalmol 2020, 20, 263. [CrossRef]
- Feng, K.; Zhang, Y.; Chen, Y.G. The possible causes for tomography suspect keratoconus in a Chinese cohort. BMC Ophthalmol 2021, 21, 47. [CrossRef]
- Levy, A.; Georgeon, C.; Knoeri, J.; Tourabaly, M.; Leveziel, L.; Bouheraoua, N.; Borderie, V.M. Corneal epithelial thickness mapping in the diagnosis of ocular surface disorders involving the corneal epithelium: A comparative study. Cornea 2022, 41, 1353–1361. [CrossRef]
- Agudo, J.A.R.; Park, J.; Park, J.; Lee, S.; Park, K. Laser asymmetric ablation method to improve corneal shape. Lasers Med Sci 2019, 34, 1763–1779. [CrossRef]
- Min, J.S.; Min, B.M. Comparison of outcomes of laser refractive surgery (LRS) alone and LRS with laser asymmetric keratectomy in patients with myopia: A retrospective study. Med 2021, 100, e25366. [CrossRef]
- Min, J.S.; Min, B.M. Comparison between surgical outcomes of LASIK with and without laser asymmetric keratectomy to avoid conventional laser refractive surgery adverse effects. Sci Rep 2020, 10, 10446. [CrossRef]
- Min, J.S.; Min, B.M. A novel approach to enhancement linked laser asymmetric keratectomy using semi-cylindrical ablation pattern in patients with myopic regression after laser refractive surgery. Clin Ophthalmol 2021, 15, 1751–1758. [CrossRef]
- Min, J.S.; Min, B.M. Clinical outcomes of laser asymmetric keratectomy to manage postoperative adverse effects-A retrospective clinical trial. TOOPHTJ 2021, 15, 171–177. [CrossRef]
- Min, J.S.; Min, B.M.; Lee, D.C. Laser asymmetric keratectomy using a semi-cylindrical ablation pattern to avoid adverse effects of laser refractive surgery. Austin J Clin Ophthalmol 2021, 8, 1120. [CrossRef]
- Krueger, R.R.; Kanellopoulos, A.J. Stability of simultaneous Topography-guided photorefractive keratectomy and riboflavin/UVA cross-linking for progressive keratoconus: case reports. J Refract Surg 2010, 26, S827–S832. [CrossRef]
- Guedj, M.; Saad, A.; Audureau, E.; Gatinel, D. Photorefractive keratectomy in patients with suspected keratoconus: five-year follow-up. J Cataract Refract Surg 2013, 39, 66–73. [CrossRef]
- Abdolahian, M.; Moalem, M.A.; Jahady Hoseiny, M.J.; Noorizadeh, F.; Zareei, A. Keratorefractive surgery outcomes in keratoconus suspect patients. J Ophthalmol 2020, 2020, 1–11. [CrossRef]
- Roberts, C. Biomechanical customization: the next generation of laser refractive surgery. J Cataract Refract Surg 2005, 31, 2–5. [CrossRef]
- Roberts, C.J.; Dupps, W.J. Jr. Biomechanics of corneal ectasia and biomechanical treatments. J Cataract Refract Surg 2014, 40, 991–998. [CrossRef]
- Ambrósio, R. Jr.; Nogueira, L.P.; Caldas, D.L.; Fontes, B.M.; Luz, A.; Cazal, J.O.; Alves, M.R.; Belin, M.W. Evaluation of corneal shape and biomechanics before LASIK. Int Ophthalmol Clin 2011, 51, 11–38. [CrossRef]
- Lee, H.; Roberts, C.J.; Kim, T.I.; Ambrósio, R. Jr.; Elsheikh, A.; Yong Kang, D.S. Changes in biomechanically corrected intraocular pressure and dynamic corneal response parameters before and after transepithelial photorefractive keratectomy and femtosecond laser-assisted laser in situ keratomileusis. J Cataract Refract Surg 2017, 43, 1495–1503. [CrossRef]
- Liu, J.; Roberts, C.J. Influence of corneal biomechanical properties on intraocular pressure measurement: quantitative analysis. J Cataract Refract Surg 2005, 31, 146–155. [CrossRef]
- Moshirfar, M.; Edmonds, J.N.; Behunin, N.L.; Christiansen, S.M. Corneal biomechanics in iatrogenic ectasia and keratoconus: a review of the literature. Oman J Ophthalmol 2013, 6, 12–17. [CrossRef]
- Wolffsohn, J.S.; Safeen, S.; Shah, S.; Laiquzzaman, M. Changes of corneal biomechanics with keratoconus. Cornea 2012, 31, 849–854. [CrossRef]
- Kerautret, J.; Colin, J.; Touboul, D.; Roberts, C. Biomechanical characteristics of the ectatic cornea. J Cataract Refract Surg 2008, 34, 510–513. [CrossRef]
- Carriazo, C.; Cosentino, M.J. A novel corneal remodeling technique for the management of keratoconus. J Refract Surg 2017, 33, 854–856. [CrossRef]
- Carriazo, C.; Cosentino, M.J. Long-term outcomes of a new surgical technique for corneal remodeling in corneal ectasia. J Refract Surg 2019, 35, 261–267. [CrossRef]
- Min, B.M. Corneal remodeling of laser asymmetric keratectomy combined with collagen cross linking in a patients with keratoconus suspect. J Ophthalmol Open Access 2023, 1, 1–10.
- Min, J.S.; Lee, D.C.; Lee, S.S.; Min, P.M. A novel approach for corneal remodeling of laser asymmetric keratectomy with collagen cross linking in patients with keratoconus suspect. TOOPHTJ 2024, 18, e18743641282093. [CrossRef]
- Liu, Z.; Pflugfelder, S.C. Corneal surface regularity and the effect of Artificial Tears in aqueous tear deficiency. Ophthalmology 1999, 106, 939–943. [CrossRef]
- Huang, F.C.; Tseng, S.H.; Shih, M.H.; Chen, F.K. Effect of Artificial Tears on corneal surface regularity, contrast sensitivity, and glare disability in dry eyes. Ophthalmology 2002, 109, 1934–1940. [CrossRef]
- Siyahkamari, M.; Asharlous, A.; Mirzajani, A.; Koohian, H.; Jafarzadepour, E.; Ostadimoghaddam, H.,Babaei N,Yekta A,Khabazkhoob M.,; et al. Effect of dry eye disease on central corneal thickness and corneal topometric indices measured by Scheimflug tomography. Acta Med Iran 2023, 60, 777–781.
- Hirasawa, K.; Nakakura, S.; Nakao, Y.; Fujino, Y.; Matsuura, M.; Murata, H.; Kiuchi, Y.; Asaoka, R. Changes in corneal biomechanics and intraocular pressure following cataract surgery. Am J Ophthalmol 2018, 195, 26–35. [CrossRef]
|
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2025 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (http://creativecommons.org/licenses/by/4.0/).