Submitted:
19 February 2025
Posted:
20 February 2025
You are already at the latest version
Abstract
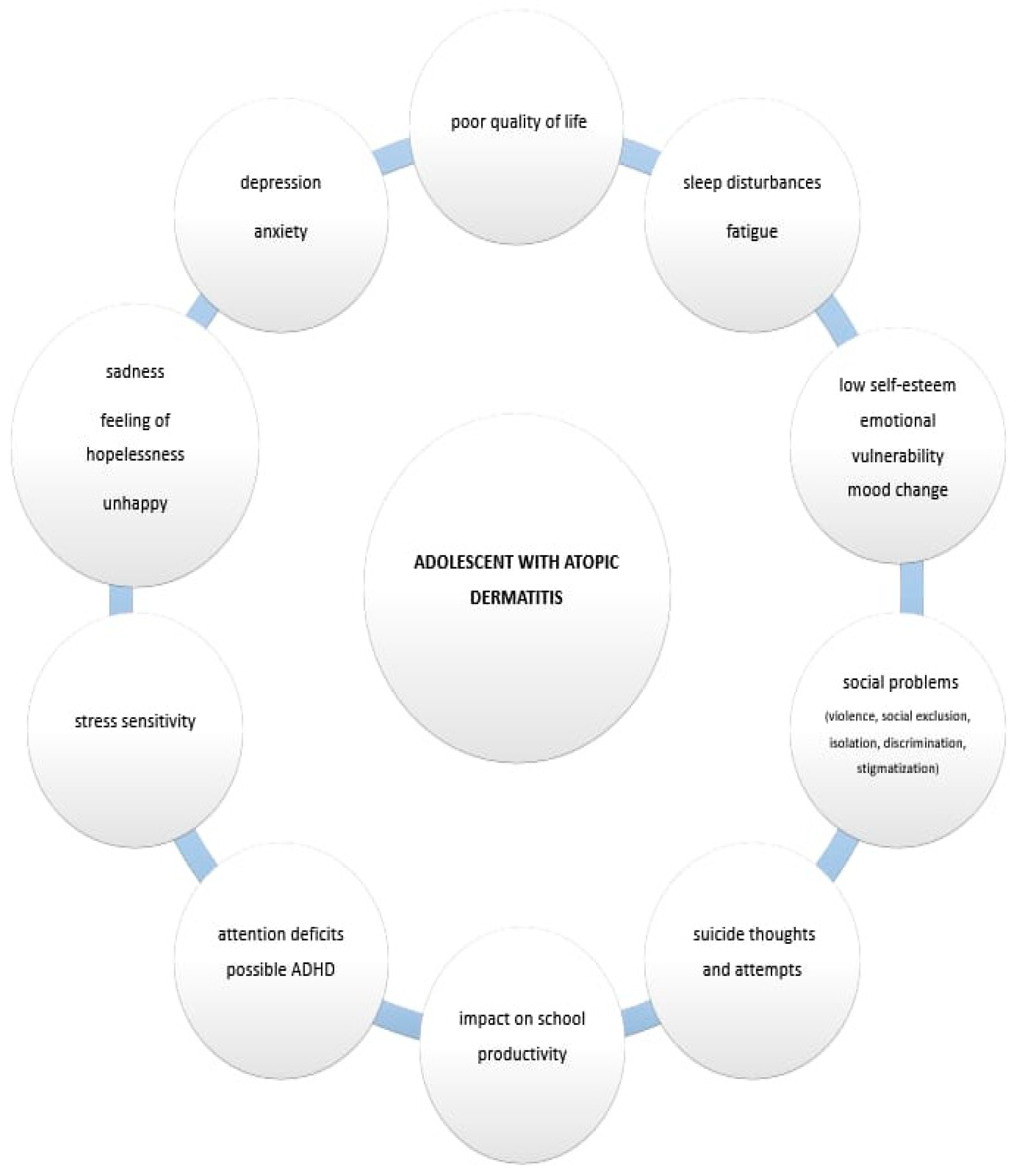
Background/Objectives:Adolescence is a particularly sensitive period of development, marked by numerous changes, and the adolescent` quality of life (QoL) could be significantly affected by the disease like atopic dermatitis (AD). The chronic nature of AD is particularly significant: due to recurring (relapsing) skin lesions, adolescents are likely exposed to greater stress and depressive symptoms than those experiencing transient or one-time symptoms. Aesthetic and functional AD skin lesions during adolescence lead to reduced happiness, high stress and depression. Methods: In this review we wanted to present the current knowledge on mental health, psychological features and psychiatric comorbidity of adolescents with AD, based on the previous studies/research on this topic presented in Pubmed basis. Results: Previous studies have confirmed that sleep disturbances, behavioural disorders, internalizing profiles, depression and anxiety, stress symptoms and suicidality represent the most prevalent psychiatric comorbidities and psychological features in adolescents with AD. According to research data, adolescents with AD also reported a tendency toward feelings of sadness and hopelessness and even suicidal thoughts and attempts. The interplay between sleep disturbances, depression and anxiety, behavioural disorders as well as suicidality (as the most frequent psychiatric comorbidity in adolescents with AD) seems to be rather complex. Conclusions: So, adequate social competence is essential for healthy mental development, as its impairment may be associated with psychological disorders in childhood and adolescence and potentially persist into adulthood. These findings highlight the need for a psychological approach and the introduction of intervention programs from an early age, such as mental health assessments and professional supervision following diagnosis.
Keywords:
1. Introduction
2. Materials and Methods
3. Results
| AUTHOR, YEAR, STUDY TYPE | OBJECTIVES/ ANALYSED FACTORS |
METHODS AND EXAMINEES/PATIENTS |
RESULTS | CONCLUSIONS |
| Yaghmaie P, et al., 2013 (cross-sectional study) [16] |
To quantify mental health comorbidity in noninstitutionalized children with AD |
92,642 children (0-17 years); lifetime prevalence of various mental health conditions, calculated for those with and without a history of AD; data analyzed from the 2007 National Survey of Children's Health |
Odds of having ADHD significantly greater for children with AD. The adjusted odds ratios for depression, anxiety, conduct disorder, and autism were 1.81, 1.77, 1.87 and 3.04, respectively |
A striking association between mental health disorders and AD in the US pediatric population; a clear dose-dependent relationship between the prevalence of a mental health disorder and reported AD severity |
| Noh HM, et al., 2016 (web-based survey) [17] |
The relationship between suicidal behaviors and AD in Korean adolescents |
Prevalence of adolescent health risk behaviors among Korean students from grades 7 to 12; data from the 2012 Eighth Korea Youth Risk Behavior Web-Based Survey (KYRBWS-VIII) (suicidal ideation, planning and suicide attempts, AD, mental health status, etc.) |
Significant associations between AD and suicidal behaviors for girls but not for boys. The overestimation of weight perception might have an additive impact on suicidal risk among girls. |
AD increased the risk of suicidal behaviors in girls in the 7th–12th grades, even after adjustments for multiple confounding factors. |
| Becker-Haimes EM, et al., 2017 (clinical study) [18] |
Atopic disease and anxiety as a comorbidity |
189 youth who presented for treatment services at a specialty clinic for child/adolescent anxiety and depressive disorders; youth and their parents completed a diagnostic interview and a large number of questionnaires |
High rates of atopy in the clinical sample (51.3 % reporting history of ≥1 atopic diseases); anxious youth with atopy exhibited more overall and generalized anxiety symptoms relative to non-atopic youth (ps < .05). |
Comparable or elevated rates of atopy in this clinical sample relative to estimates of community prevalence rates. Youth with anxiety and atopy presented with higher anxiety severity than those without comorbid atopy. |
| Lee S, et al., 2017 (web-based survey) [19] |
Association of AD with depressive symptoms and suicidal behaviors among Korean adolescents (2013 Korean Youth Risk Behavior Survey) | 72,435 middle and high school adolescents in Korea; self-reporting on AD and yes-or-no answers to questions about depressive symptoms and suicide ideation, suicide planning, and suicide attempts |
6.8% of adolescents had AD. The proportion reporting depressive feelings was 31.0%, suicide ideation was 16.3%, suicide planning was 5.8%, and suicide attempts was 4.2%. |
Adolescents with AD have a higher prevalence of depression symptoms and suicidal behaviors and are significantly more prone to experience depressive feelings, suicide ideation, suicide planning and suicide attempts than those without AD. |
| Kuniyoshi Y, et al., 2018 (cross-sectional study) [20] |
The association between eczema and mental health problems in Japanese school children | 9954 participants (2nd to 8th grade) from the 2014 and 2015 ToMMo Child Health Study; ISAAC Eczema Symptom Questionnaire; Clinical ranges of Strengths and Difficulties Questionnaire (SDQ): total difficulties scores and four SDQ subcategories of emotional symptoms, conduct problems, hyperactivity/inattention, and peer problems were defined as scores ≥16, ≥5, ≥5, ≥7, and ≥5, respectively | As eczema status worsened, the mean SDQ total difficulties score significantly increased (OR of scores in the clinical range for SDQ total difficulties were 1.51 for mild/moderate eczema and 2.63 for severe eczema, adjusted for sex, school grade, current wheeze, and disaster-related factors, using normal eczema as a reference). The association between eczema severity and the four SDQ subcategories showed a similar trend. | A significant association between eczema severity and mental health problems exists. The presence of eczema was associated with four the SDQ subcategories. |
| Kim SY, et al., 2019 (web-based survey) [21] |
Exploring psychological distress in Korean adolescents having allergic disease comorbid with obesity |
703,869 adolescents completed the Korean Youth Risk Behavior survey between 2007 and 2016; 4 groups (healthy control, allergic disease only, obesity only, and comorbidity of allergic disease and obesity); comparison of mental health between groups |
Adolescents with both AD and obesity had significantly greater odds of experiencing unhappiness (OR, 1.17), stress (OR, 1.32), and suicidal ideation (OR, 1.25). The comorbidity groups also showed significantly greater odds of stress and suicidal ideation than the allergic disease-only and obesity-only groups. |
Allergic disease and obesity negatively and additively influence mental health in adolescents. |
| Hsu DY, et al., 2019 (clinical study) [22] |
Association between AD and hospitalization for mental health (MH) disorders in the United States |
835 AD (1.36%) and 2,434,703 non-AD (0.75%) patients with primary admission for an MH disorder; data analysis from the Nationwide Inpatient Sample from 2002 to 2012 (containing a representative 20% sample of US hospitalizations) |
AD patients admitted for MH disorders are younger, Asian, Black, in a higher income quartile and have an increasing number of chronic conditions. AD was associated with a primary admission for MH disorders in adults, including mood disorders, schizophrenia, and developmental disorders. This association was not present in children. | AD was associated with higher odds of hospitalization for all MH disorders and substantial excess costs of inpatient care. |
| Wan J, et al., 2020 (cross-sectional study) [23] |
Association between pediatric AD and mental health impairment |
Children with and without AD were assessed for mental disorder with impairment (MDI) using a validated behavioral screening questionnaire; mental health services utilization was also reported; United States National Health Interview Survey data (2013-2017) |
MDI prevalence was 26.7% among children with AD and 17.7% for those without AD, severe MDI being present in 10.9% and 6.2%, respectively). AD was associated with higher odds of MDI, including impairments in conduct, emotions, peer relationships, and attention. |
AD is associated with clinically significant mental health symptoms, but many affected children may not seek or receive care. |
| Kyung Y, et al., 2020 (cross-sectional study) [24] |
Association of AD with suicide risk |
788,411 adolescents, Korean Youth Risk Behavior Web-based Survey; survey data obtained from a stratified, multistage, clustered sample; students self-reported AD if they had received a diagnosis of AD by a physician; influencing factors for suicidal behaviors tested by logistic regression models. |
Reported suicide ideation: 19.0%; suicide attempts: 4.5%. AD patients were more likely to skip breakfast less frequently, to exercise less frequently, to drink less alcohol, and to not be current smokers and were significantly more likely to have negative mental health states. |
Adolescents with AD had a meaningful prevalence of suicidal behaviors. |
| Kyung Y, et al., 2020 (cross-sectional study) [25] |
Identification of the influencing factors for mental health in adolescents with AD | 62,276 participants; 13th Korean Youth Risk Behavior Web-based Survey (KYRBS) conducted in 2017—data obtained from a stratified, multistage, clustered sample. Participants responded to the question “have you ever been diagnosed with AD by a doctor?” and several yes/no questions about stress, depressive symptoms and suicidal ideation. |
Adolescents with AD were significantly more prone to stress (59.1%), depressive symptoms (27.8% ) and suicidal ideation ( 13.9%). Subjective unhappiness was most strongly associated with stress; depression and suicidal ideation were reciprocally key risk factors. |
AD in adolescents is associated with a higher prevalence of stress, depressive symptoms and suicidal ideation. |
| Hou A, et al., 2021 (cross-sectional study) [26] |
Predictors, and age-dependent pattern, of psychologic problems in childhood AD |
Data on 228,898 children (2-17 years old) from the 1997-2018 National Health Interview Survey.
|
Children with AD more commonly experienced depression/sadness, had ADD/ADHD, emotional/behavioral difficulties feelings of frequent worry, and autism. Also, psychologic comorbidity was associated with atopic comorbidities, multimorbidity and being white, households with a lower income and educational background, and no insurance coverage. |
AD is associated with multiple psychologic disorders, particularly among those who are white, have atopic comorbidities and a low household income. Psychologic comorbidities increased in an age-dependent pattern, though in a way like children without AD. |
| Keller W, et al., 2021 (clinical study) [27] |
Associations between atopic diseases and behavioural difficulties | 2701 participants (3-18 years old), data on behavioural difficulties (Strengths and Difficulties Questionnaire - SDQ) and on atopic diseases (participant's medical history). Two groups: Group I (3- to 10-year-olds), parent-reported SDQ (n = 1764); Group II (11- to 18-year-olds), parent-reported SDQ (n = 937) and self-reported SDQ (n = 915) |
In younger children, AD was strongly associated with higher total difficulties scores, more emotional/conduct problems and more symptoms of hyperactivity/inattention. |
In younger children, AD is associated with internalizing and externalizing problems. Parents of adolescents are more likely to perceive associations between atopic diseases and behavioural difficulties than the adolescents themselves. |
| Fishbein AB, et al., 2021 (cross-sectional study) [28] |
Prevalence and severity of sleep disturbance in school-aged children with AD |
180 parent-child dyads with AD; stratified sampling based on AD severity (POEM: mild [n = 30], moderate [n = 75], severe [n = 75]), age, and race; symptoms of sleep and psychologic health assessed using the Patient-Reported Outcome Measurement Information System. |
In children ages 5 to 17 with AD, sleep disturbance is common (66.9%). Children who reported sleep disturbance had increased odds of sleep-related impairment, depression, fatigue, and anxiety. Predictors of parent proxy-reported sleep disturbance were itch intensity and low income |
Sleep disturbance is a common AD symptom that affects about 3 million US children and is associated with neuropsychiatric impairment, including depression, anxiety, and inattention. |
| Kern C, et al., 2021 (longitudinal cohort study) [29] |
Association between AD and internalizing behaviors and symptoms of depression at multiple points across childhood and adolescence |
11,181 participants; annual period prevalence of AD assessed at 11 points from 6 months to 18 years of age; symptoms of depression (measured using the Short Moods and Feelings Questionnaire at 5 points from 10 to 18 years of age) and internalizing behaviors (measured by maternal report of the Emotional Symptoms subscale of the Strength and Difficulties Questionnaire at 7 points from 4 to 16 years of age |
The period prevalence of symptoms of depression ranged from 6.0% to 21.6%; for internalizing behaviors, from 10.4% to 16.0%. Mild to moderate AD was associated with internalizing behaviors as early as 4 years of age. Severe AD was associated with symptoms of depression and internalizing symptoms. |
Severe AD is associated with symptoms of depression and internalizing behaviors throughout childhood/adolescence. Increased risk of internalizing symptoms even for children with mild AD beginning early in childhood. |
| Cheng BT, et al., 2021 (cross-sectional study) [30] |
The prevalence and predictors of social and behavioral symptoms and functional impairment among US children with AD |
2,553 US children with AD; behavioral and functional issues examined using Columbia Impairment Scale (CIS) scores |
Childhood AD was associated with behavioral/functional problems, particularly nervousness, home behavior, staying out of trouble, and relationships with other kids or siblings. Higher CIS scores in children with AD (vs. without AD and with psoriasis)—higher scores notably associated with male sex, older age, lower household income, public insurance, and comorbid depression and anxiety. |
AD is associated with behavioral and functional impairment, similar to psoriasis and other common chronic conditions. |
| Moraes MM, et al., 2024 (cross-sectional study) [31] |
Prevalence and pattern of behavioral problems in children and adolescents with AD | 100 AD patients (ages 6-17); assessment of competencies and syndrome scale scores of behavioral problems using the Child Behavior Checklist 6-18 (CBCL 6-18) and AD severity using the EASI score |
Borderline/abnormal values for the following: total social competence (75% of patients); internalization (57%); externalization (27%); and aggressive behavior (18%). More common aggressive behavior and sleep disorders in patients with moderate/severe AD than in those with mild AD. Children with current/previous use of immunosuppressants/biological tests had a lower frequency of normal social competence. |
Common behavioral problems among children/adolescents with AD, with a predominance of internalizing profiles, mainly anxiety and depression. In children with moderate/severe AD, higher prevalence of aggressive behaviors and sleep disorders. |
| Sockler PG, et al., 2024 (cohort study) [32] |
The effect of AD on cognitive function and psychiatric comorbidities across early childhood and adolescence |
14,975 individuals followed since birth in 1991-92; AD was assessed 11 times (6-166 months); general cognition (IQ) was measured at 18, 49, 103 and 186 months of age using 4 scales (GMDS, WPPSI, WISC, WASI); secondary analyses were stratified by the presence or absence of psychiatric or learning disorder |
No significant associations were observed between AD status and full-scale IQ scores on the GMDS, WPPSI, WISC and WASI. However, at age 8, among children with active/moderate-severe AD, WISC Performance IQ and verbal IQ were significantly higher than among those with inactive AD. | No clinically meaningful associations between AD activity and severity and general cognitive function during early childhood and adolescence. |
| Cai XC, et al., 2024 (analysis of seven electronic databases) [33] |
Epidemiology of mental health comorbidity in AD patients |
Analysis of 7 electronic databases from creation to October 2022; the Agency for Healthcare Research and Quality (AHRQ) and Newcastle–Ottawa Scale (NOS) tools were used to assess the quality of observational studies |
1998-October 2022 global prevalence rates in AD patients: ADHD (7%), depression (17%), anxiety (21%) and suicidal ideation (13%). Among children aged < 18, North American children with AD had highest prevalence rates of ADHD (10%), depression (13%) and anxiety (20%). Among adults (aged ≥ 18), adults in Africa with AD had highest prevalence rates of depression (36%) and anxiety (44%); Asian adults with AD had highest prevalence rates of ADHD (7%) and suicidal ideation (20%). |
Results show high prevalence and comorbidity rates of mental illnesses with AD. |
| Paller AS, et al., 2024 (cross-sectional study) [34] |
Stigmatization and mental health impact of chronic pediatric skin disorders |
1671 children (ages 8-17) with chronic dermatoses and 1 parent. The extent of stigma with child-, caregiver-, and physician-assessed disease visibility (primary outcome) was compared to (a) severity, using the PROMIS Stigma-Skin, (b) reduced QOL (assessed by Skindex-Teen), (c) depression, (d) anxiety, and (e) poor peer relationships (PROMIS child and proxy tools) (secondary outcomes) |
56.4% participants had self-reported high disease visibility and 50.5% had moderate disease severity. Stigma scores significantly differed by level of physician-assessed and child/proxy-assessed disease visibility and severity. Among children with chronic dermatoses (acne, AD, etc.), only 27.0% had minimal or no stigma and 43.8% had at least moderate stigma. Stigma scores correlated strongly with reduced QOL, depression, anxiety, and poor peer relationships. |
Physician assessment of disease severity and visibility is insufficient to evaluate disease impact on the patient/caregiver. |
| Paller AS, et al., 2024 (cross-sectional study) [35] |
Attentiveness and mental health in adolescents with moderate-to-severe AD without ADHD | 44 AD patients (ages 12–17) (moderate-to-severe AD) without clinician-diagnosed ADHD; Attention was evaluated using: the Conners CPT-3 and the Stroop Color and Word Test; lesional severity measures included EASI and BSA involvement; subjects completed self-report rating scales for sensory responsiveness patterns (AASP), itch (PP-NRS), skin pain, QOL, sleep, anxiety, and depressive symptoms |
Substantial AD impact on sleep, QOL, and comorbid anxiety and depressive symptoms. According to subject-level data review by two psychologists, only 2 subjects demonstrated an overall response pattern that clearly indicated attenti on deficit. |
Adolescents with moderate-to-severe AD without an existing ADHD diagnosis did not demonstrate greater attention problems on performance-based measures than would be expected in age/gender-matched peers. |
| Blanco Sequeiros A, et al., 2024 (clinical study) [36] |
Psychiatric comorbidities of childhood-onset AD in relation to eczema severity |
Children diagnosed with AD before the age of 12; patient health record data obtained from the Finnish Health Register for Health Care (CRHC); diagnosis codes for psychiatric comorbidities following AD diagnosis were searched for in CRHC for individuals aged < 18 and ≤ 30 years. |
Increased risk of several psychiatric disorders associated with increased severity in childhood-onset AD (not for other examined factors, i.e., depression, anxiety disorders, panic disorder, and bipolar disorder) | Childhood-onset AD is associated with different psychiatric comorbidities depending on AD severity. |
4. Discussion
Sleep Disturbances, Internalizing Profiles, Depression and Anxiety, Stress and Suicidality as the Most Prominent Psychological Characteristics and Psychiatric Comorbidities of Adolescents with AD
4.2. Functioning and Quality of Life, Behavioural Disorders, Attention Disturbances/ADHD and Suicidal Ideations of Adolescents with Atopic Dermatitis
4.3. Coping with Atopic Dermatitis, Positive Measures/Activities, and Related Treatment Possibilities
5. Conclusions
Author Contributions
Funding
Data Availability Statement
Conflicts of Interest
Abbreviations
References
- Laughter, M.; Maymone, M.; Mashayekhi, S.; Arents, B.; Karimkhani, C.; Langan, S.; Dellavalle, R.; Flohr, C. The global burden of atopic dermatitis: lessons from the Global Burden of Disease Study 1990–2017*. Br. J. Dermatol. 2020, 184, 304–309. [CrossRef]
- Silverberg JI, Howe W. Atopic dermatitis (eczema): Pathogenesis, clinical manifestations, and diagnosis https://www.uptodate.com/contents/atopic-dermatitis-eczema-pathogenesis-clinical-manifestations-and-diagnosis/print.
- Fasseeh, A.N.; Elezbawy, B.; Korra, N.; Tannira, M.; Dalle, H.; Aderian, S.; Abaza, S.; Kaló, Z. Burden of Atopic Dermatitis in Adults and Adolescents: a Systematic Literature Review. Dermatol. Ther. 2022, 12, 2653–2668. [CrossRef]
- Kim, J.P.; Chao, L.X.; Simpson, E.L.; Silverberg, J.I. Persistence of atopic dermatitis (AD): A systematic review and meta-analysis. J. Am. Acad. Dermatol. 2016, 75, 681–687.e11. [CrossRef]
- Russo, F.; Santi, F.; Cioppa, V.; Orsini, C.; Lazzeri, L.; Cartocci, A.; Rubegni, P. Meeting the Needs of Patients With Atopic Dermatitis: A Multidisciplinary Approach. Dermatitis® 2022, 33, S141–S143. [CrossRef]
- El Hachem, M.; Di Mauro, G.; Rotunno, R.; Giancristoforo, S.; De Ranieri, C.; Carlevaris, C.M.; Verga, M.C.; Iacono, I.D. Pruritus in pediatric patients with atopic dermatitis: a multidisciplinary approach - summary document from an Italian expert group. Ital. J. Pediatr. 2020, 46, 1–9. [CrossRef]
- Park, J.-H.; Prochnow, T.; Chang, J.; Kim, S.J. Health-Related Behaviors and Psychological Status of Adolescent Patients with Atopic Dermatitis: The 2019 Korea Youth Risk Behavior Web-Based Survey. Patient Preference Adherence 2023, ume 17, 739–747. [CrossRef]
- Bieber, T.; Paller, A.; Kabashima, K.; Feely, M.; Rueda, M.; Terres, J.R.; Wollenberg, A. Atopic dermatitis: pathomechanisms and lessons learned from novel systemic therapeutic options. J. Eur. Acad. Dermatol. Venereol. 2022, 36, 1432–1449. [CrossRef]
- Patel, J.S.; Oh, Y.; Rand, K.L.; Wu, W.; Cyders, M.A.; Kroenke, K.; Stewart, J.C. Measurement invariance of the patient health questionnaire-9 (PHQ-9) depression screener in U.S. adults across sex, race/ethnicity, and education level: NHANES 2005-2016. Depress Anxiety. 2019;36(9):813-823. [CrossRef]
- Rønnstad, A.T.M.; Halling-Overgaard, A.-S.; Hamann, C.R.; Skov, L.; Egeberg, A.; Thyssen, J.P. Association of atopic dermatitis with depression, anxiety, and suicidal ideation in children and adults: A systematic review and meta-analysis. J. Am. Acad. Dermatol. 2018, 79, 448–456.e30. [CrossRef]
- Slattery, M.J.; Essex, M.J.; Paletz, E.M.; Vanness, E.R.; Infante, M.; Rogers, G.M.; Gern, J.E. Depression, anxiety, and dermatologic quality of life in adolescents with atopic dermatitis. J. Allergy Clin. Immunol. 2011, 128, 668–671.e3. [CrossRef]
- Mann, C.; Dreher, M.; Weeß, H.; Staubach, P. Sleep Disturbance in Patients with Urticaria and Atopic Dermatitis: An Underestimated Burden. Acta Dermato-Venereologica 2020, 100, adv00073–6. [CrossRef]
- Pedersen, C.J.; Uddin, M.J.; Saha, S.K.; Darmstadt, G.L. Prevalence and psychosocial impact of atopic dermatitis in Bangladeshi children and families. PLOS ONE 2021, 16, e0249824. [CrossRef]
- Marron, S.E.; Cebrian-Rodriguez, J.; Alcalde-Herrero, V.M.; Garcia-Latasa de Aranibar, F.J.; Tomas-Aragones, L. Psychosocial impact of atopic dermatitis in adults: a qualitative study. Actas Dermosifiliogr. (Engl. Ed.). 2020, 111, 513-517. [CrossRef]
- Yaghmaie, P.; Koudelka, C.W.; Simpson, E.L. Mental health comorbidity in patients with atopic dermatitis. J. Allergy Clin. Immunol. 2012, 131, 428–433. [CrossRef]
- Noh, H.-M.; Cho, J.J.; Park, Y.S.; Kim, J.-H. The relationship between suicidal behaviors and atopic dermatitis in Korean adolescents. J. Heal. Psychol. 2016, 21, 2183–2194. [CrossRef]
- Becker-Haimes, E.M.; Diaz, K.I.; Haimes, B.A.; Ehrenreich-May, J. Anxiety and Atopic Disease: Comorbidity in a Youth Mental Health Setting. Child Psychiatry Hum. Dev. 2016, 48, 528–536. [CrossRef]
- Lee, S.; Shin, A. Association of atopic dermatitis with depressive symptoms and suicidal behaviors among adolescents in Korea: the 2013 Korean Youth Risk Behavior Survey. BMC Psychiatry 2017, 17, 1–11. [CrossRef]
- Kuniyoshi, Y.; Kikuya, M.; Miyashita, M.; Yamanaka, C.; Ishikuro, M.; Obara, T.; Metoki, H.; Nakaya, N.; Nagami, F.; Tomita, H.; et al. Severity of eczema and mental health problems in Japanese schoolchildren: The ToMMo Child Health Study. Allergol. Int. 2018, 67, 481–486. [CrossRef]
- Kim, S.Y.; Choi, S.H.; Kim, J.D.; Sol, I.S.; Kim, M.J.; Kim, Y.H.; Jung, Y.-C.; Sohn, M.H.; Kim, K.W. Korean Youth with Comorbid Allergic Disease and Obesity Show Heightened Psychological Distress. J. Pediatr. 2019, 206, 99–+. [CrossRef]
- Hsu, D.Y.; Smith, B.; Silverberg, J.I. Atopic Dermatitis and Hospitalization for Mental Health Disorders in the United States. Dermatitis® 2019, 30, 54–61. [CrossRef]
- Wan, J.; Takeshita, J.; Shin, D.B.; Gelfand, J.M. Mental health impairment among children with atopic dermatitis: A United States population-based cross-sectional study of the 2013-2017 National Health Interview Survey. J. Am. Acad. Dermatol. 2020, 82, 1368–1375. [CrossRef]
- Kyung, Y.; Choi, M.H.; Jeon, Y.J.; Lee, J.S.; Lee, J.H.; Jo, S.H.; Kim, S.H. Association of atopic dermatitis with suicide risk among 788,411 adolescents. Ann. Allergy, Asthma Immunol. 2020, 125, 55–64. [CrossRef]
- Kyung, Y.; Lee, J.S.; Lee, J.H.; Jo, S.H.; Kim, S.H. Health-related behaviors and mental health states of South Korean adolescents with atopic dermatitis: A Korean cross-sectional study. J. Dermatol. 2020, 47, 699–706. [CrossRef]
- Hou, A.; Silverberg, J.I. Predictors and age-dependent pattern of psychologic problems in childhood atopic dermatitis. Pediatr. Dermatol. 2021, 38, 606–612. [CrossRef]
- Keller, W.; Vogel, M.; Prenzel, F.; Genuneit, J.; Jurkutat, A.; Hilbert, C.; Hiemisch, A.; Kiess, W.; Poulain, T. Atopic diseases in children and adolescents are associated with behavioural difficulties. BMC Pediatr. 2021, 21, 1–10. [CrossRef]
- Fishbein, A.B.; Cheng, B.T.; Tilley, C.C.; Begolka, W.S.; Carle, A.C.; Forrest, C.B.; Zee, P.C.; Paller, A.S.; Griffith, J.W. Sleep Disturbance in School-Aged Children with Atopic Dermatitis: Prevalence and Severity in a Cross-Sectional Sample. J. Allergy Clin. Immunol. Pr. 2021, 9, 3120–3129.e3. [CrossRef]
- Kern, C.; Wan, J.; LeWinn, K.Z.; Ramirez, F.D.; Lee, Y.; McCulloch, C.E.; Langan, S.M.; Abuabara, K. Association of atopic dermatitis and mental health outcomes across childhood: a longitudinal cohort study. JAMA Dermatol. 2021, 157, 1200-1208. [CrossRef]
- Cheng, B.T.; Fishbein, A.B.; Silverberg, J.I. Mental Health Symptoms and Functional Impairment in Children With Atopic Dermatitis. Dermatitis® 2020, 32, 353–361. [CrossRef]
- Moraes, M.M.; Vaz, F.P.C.; Roque, R.M.S.d.A.; Mallozi, M.d.C.; Solé, D.; Wandalsen, G.F. Behavioral disorders in children and adolescents with atopic dermatitis. J. de Pediatr. 2023, 100, 93–99. [CrossRef]
- Sockler, P.G.; Hooper, S.R.; Abuabara, K.; Ma, E.Z.; Radtke, S.; Bao, A.; Kim, E.; Musci, R.J.; Kartawira, K.; Wan, J. Atopic dermatitis, cognitive function and psychiatric comorbidities across early childhood and adolescence in a population-based UK birth cohort. Br. J. Dermatol. 2023, 190, 501–509. [CrossRef]
- Cai, X.; Wang, S.; Wang, C.; Liu, L.; Wang, J.; Shen, Y.; Li, X. Epidemiology of mental health comorbidity in patients with atopic dermatitis: An analysis of global trends from 1998 to 2022. J. Eur. Acad. Dermatol. Venereol. 2023, 38, 496–512. [CrossRef]
- Paller, A.S.; Rangel, S.M.; Chamlin, S.L.; Hajek, A.; Phan, S.; Hogeling, M.; Castelo-Soccio, L.; Lara-Corrales, I.; Arkin, L.; Lawley, L.P.; et al. Pediatric dermatology research alliance. Stigmatization and Mental Health Impact of Chronic Pediatric Skin Disorders. JAMA Dermatol. 2024, 160, 621–686. [CrossRef]
- Paller, A.S.; Gonzalez, M.E.; Barnum, S.; Jaeger, J.; Shao, L.; Ozturk, Z.E.; Korotzer, A. Attentiveness and mental health in adolescents with moderate-to-severe atopic dermatitis without ADHD. Arch. Dermatol. Res. 2024, 316, 1–9. [CrossRef]
- Sequeiros, A.B.; Sinikumpu, S.-P.; Jokelainen, J.; Huilaja, L. Psychiatric Comorbidities of Childhood-onset Atopic Dermatitis in Relation to Eczema Severity: A Register-based Study among 28,000 Subjects in Finland. Acta Dermato-Venereologica 2024, 104, adv40790–adv40790. [CrossRef]
- Malekzad, F.; Arbabi, M.; Mohtasham, N.; Toosi, P.; Jaberian, M.; Mohajer, M.; Mohammadi M.R.; Roodsari, M.R.; Nasiri, S. Efficacy of oral naltrexone on pruritus in atopic eczema: a double-blind, placebo-controlled study. J. Eur. Acad. Dermatol. Venereol. 2009, 23, 948-950. [CrossRef]
- Choi, C. The factors affecting the life satisfaction of adolescents with atopic dermatitis. Stud Korean Youth. 2015;26:111–144.
- Schut, C.; Weik, U.; Tews, N.; Gieler, U.; Deinzer, R.; Kupfer, J. Psychophysiological Effects of Stress Management in Patients with Atopic Dermatitis: A Randomized Controlled Trial. Acta Dermato-Venereologica 2013, 93, 57–61. [CrossRef]
- Ramirez, F.D.; Chen, S.; Langan, S.M.; Prather, A.A.; McCulloch, C.E.; Kidd, S.A.; Cabana, M.D.; Chren, M.-M.; Abuabara, K. Association of Atopic Dermatitis With Sleep Quality in Children. JAMA Pediatr. 2019, 173, e190025–e190025. [CrossRef]
- Silverberg, J.I.; Garg, N.K.; Paller, A.S.; Fishbein, A.B.; Zee, P.C. Sleep Disturbances in Adults with Eczema Are Associated with Impaired Overall Health: A US Population-Based Study. J. Investig. Dermatol. 2015, 135, 56–66. [CrossRef]
- Bešlić, I.; Lugović-Mihić, L.; Vrtarić, A.; Bešlić, A.; Škrinjar, I.; Hanžek, M.; Crnković, D.; Artuković, M. Melatonin in Dermatologic Allergic Diseases and Other Skin Conditions: Current Trends and Reports. Int. J. Mol. Sci. 2023, 24, 4039. [CrossRef]
- Ma, E.Z.; Chang, H.R.; Radtke, S.; Wan, J. Symptoms of Cognitive Impairment Among Children With Atopic Dermatitis. JAMA Dermatol. 2024, 160, 447–452. [CrossRef]
- Muzzolon, M.; Canato, M.; Muzzolon, S.B.; Lima, M.N.; Carvalho, V.O. Dermatite atopica e transtornos mentais: associacao em relacao a gravidade da doenca. Rev. Bras. Neurol. Psiquiatr. 2021, 25, 52-62.
- Teixeira, C.; Garcia, M.J.; Freitas, A.; Silva, H. Impact of atopic dermatitis on the mental health of adolescents—literature review. Med. Sci. Forum. 2022, 6, 8. [CrossRef]
- Schonmann, Y.; Mansfield, K.E.; Hayes, J.F.; Abuabara, K.; Roberts, A.; Smeeth, L.; Langan, S.M. Atopic Eczema in Adulthood and Risk of Depression and Anxiety: A Population-Based Cohort Study. 2019, 8, 248–257.e16. [CrossRef]
- Kage, P.; Simon, J.; Treudler, R. Atopic dermatitis and psychosocial comorbidities. JDDG: J. der Dtsch. Dermatol. Ges. 2020, 18, 93–102. [CrossRef]
- Mina, S.; Jabeen, M.; Singh, S.; Verma, R. Gender differences in depression and anxiety among atopic dermatitis patients. Indian J. Dermatol. 2015, 60, 211. [CrossRef]
- Kwon, J.A.; Park, E.C.; Lee, M.; Yoo, K.B.; Park, S. Does stress increase the risk of atopic dermatitis in adolescents? results of the Korea Youth Risk Behavior Web-based Survey (KYRBWS-VI). PLoS One. 2013, 8, e67890. [CrossRef]
- Lee, K.S.; Rha, Y.H.; Oh, I.H.; Choi, Y.S.; Choi, S.H. Socioeconomic and sociodemographic factors related to allergic diseases in Korean adolescents based on the Seventh Korea Youth Risk Behavior Web-based Survey: a cross-sectional study. BMC Pediatr. 2016, 16, 1–9. [CrossRef]
- Mercer, M.J.; Joubert, G.; Ehrlich, R.I.; Nelson, H.; Poyser, M.A.; Puterman, A.; Weinberg, E.G. Socioeconomic status and prevalence of allergic rhinitis and atopic eczema symptoms in young adolescents. Pediatr. Allergy Immunol. 2004, 15, 234–241. [CrossRef]
- Kern, C.; Wan, J.; LeWinn, K.Z.; Ramirez, F.D.; Lee, Y.; McCulloch, C.E.; Langan, S.M.; Abuabara, K. Association of atopic dermatitis and mental health outcomes across childhood: a longitudinal cohort study. JAMA Dermatol. 2021, 157, 1200-1208. [CrossRef]
- Burt, K.B.; Obradović, J.; Long, J.D.; Masten, A.S. The Interplay of Social Competence and Psychopathology Over 20 Years: Testing Transactional and Cascade Models. Child Dev. 2008, 79, 359–374. [CrossRef]
- Reed, B.; Blaiss, M.S. The burden of atopic dermatitis. Allergy Asthma Proc. 2018, 39, 406-410.
- Zuberbier, T.; Orlow, S.J.; Paller, A.S.; Taïeb, A.; Allen, R.; Hernanz-Hermosa, J.M.; Ocampo-Candiani, J.; Cox, M.; Langeraar, J.; Simon, J.C. Patient perspectives on the management of atopic dermatitis. J. Allergy Clin. Immunol. 2006, 118, 226–232. [CrossRef]
- Keller, W.; Vogel, M.; Prenzel, F.; Genuneit, J.; Jurkutat, A.; Hilbert, C.; Hiemisch, A.; Kiess, W.; Poulain, T. Atopic diseases in children and adolescents are associated with behavioural difficulties. BMC Pediatr. 2021, 21, 1–10. [CrossRef]
- Fontes Neto, P.T.; Weber, M.B.; Fortes, S.D.; Cestari, T.F.; Escobar, G.F.; Mazotti, N.; Barzenski, B.; da Silva, L.T.; Soirefmann, Mariana.; Pratti, Clarissa. Evaluation of emotional and behavioral symptoms in children and adolescents with atopic dermatitis. Rev. Psiquiatr. Rio Gd. Sul. 2005, 27, 279-291. [CrossRef]
- Paller, A.S.; Gonzalez, M.E.; Barnum, S.; Jaeger, J.; Shao, L.; Ozturk, Z.E.; Korotzer, A. Attentiveness and mental health in adolescents with moderate-to-severe atopic dermatitis without ADHD. Arch. Dermatol. Res. 2024, 316, 497. [CrossRef]
- Kruse, L.L.; Cices, A.; Fishbein, A.B.; Paller, A.S. Neurocognitive function in moderate–severe pediatric atopic dermatitis: A case–control study. Pediatr. Dermatol. 2018, 36, 110–114. [CrossRef]
- Feng, L.-J.; Chen, A.-W.; Luo, X.-Y.; Wang, H. Increased attention deficit/hyperactivity and oppositional defiance symptoms of 6–12 years old Chinese children with atopic dermatitis. Medicine 2020, 99, e20801. [CrossRef]
- Zhou, N.Y.; Nili, A.; Blackwell, C.K.; Ogbuefi, N.; Cummings, P.; Lai, J.; Griffith, J.W.; Paller, A.S.; Wakschlag, L.S.; Fishbein, A.B. Parent report of sleep health and attention regulation in a cross-sectional study of infants and preschool-aged children with atopic dermatitis. Pediatr. Dermatol. 2021, 39, 61–68. [CrossRef]
- Sandhu, J.K.; Wu, K.K.; Bui, T.L.; Armstrong, A.W. Association between atopic dermatitis and suicidality: a systematic review and meta-analysis. JAMA Dermatol. 2019, 155, 178-187. [CrossRef]
- Kishimoto, S.; Watanabe, N.; Yamamoto, Y.; Imai, T.; Aida, R.; Germer, C.; Tamagawa-Mineoka, R., Shimizu, R.; Hickman S.; Nakayama Y.; et. Efficacy of integrated online mindfulness and self-compassion training for adults with atopic dermatitis: a randomized clinical trial. JAMA Dermatol. 2023;159(6):628-636. [CrossRef]
- Oska, C.; Nakamura, M. Alternative Psychotherapeutic Approaches to the Treatment of Eczema. Clin. Cosmet. Investig. Dermatol. 2022, 15, 2721–2735. [CrossRef]
- Spielman, S.C.; LeBovidge, J.S.; Timmons, K.G.; Schneider, L.C. A Review of Multidisciplinary Interventions in Atopic Dermatitis. J. Clin. Med. 2015, 4, 1156–1170. [CrossRef]
- Lugović-Mihić, L.; Barac, E.; Tomašević, R.; Parać, E.; Zanze, L.; Ljevar, A.; Dolački, L.; Štrajtenberger, M. Atopic Dermatitis-Related Problems in Daily Life, Goals of Therapy and Deciding Factors for Systemic Therapy: A Review. Pharmaceuticals 2024, 17, 1455. [CrossRef]
- Lugović-Mihić, L.; Meštrović-Štefekov, J.; Potočnjak, I.; Cindrić, T.; Ilić, I.; Lovrić, I.; Skalicki, L.; Bešlić, I.; Pondeljak, N. Atopic Dermatitis: Disease Features, Therapeutic Options, and a Multidisciplinary Approach. Life 2023, 13, 1419. [CrossRef]
- Kong, S.; Koo, J.; Kil Lim, S. Associations between Stress and Physical Activity in Korean Adolescents with Atopic Dermatitis Based on the 2018–2019 Korea Youth Risk Behavior Web-Based Survey. Int. J. Environ. Res. Public Heal. 2020, 17, 8175. [CrossRef]
- O'Dougherty, M.; Hearst, M.O.; Syed, M.; Kurzer, M.S.; Schmitz, K.H. Life events, perceived stress and depressive symptoms in a physical activity intervention with young adult women. Ment. Heal. Phys. Act. 2012, 5, 148–154. [CrossRef]
- Murota, H.; Yamaga, K.; Ono, E.; Murayama, N.; Yokozeki, H.; Katayama, I. Why does sweat lead to the development of itch in atopic dermatitis? Exp. Dermatol. 2019, 28, 1416-1421. [CrossRef]
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2025 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (http://creativecommons.org/licenses/by/4.0/).




