Submitted:
17 February 2025
Posted:
17 February 2025
You are already at the latest version
Abstract
Keywords:
1. Introduction
2. G Protein-Coupled Receptor (GPCR) Family
- -
- the classical A‒F system, in which GPCRs are grouped into six classes based on sequence homology and functional similarity
- -
- a newer alternative classification proposed for vertebrates, known by its acronym GRAFS, which stands for glutamate, rhodopsin, adhesion, Frizzled/Taste2, Secretin. The GRAFS system corresponds to classical classes C, A, B2 (Secretin receptor family, long N-terminal), F and B1+3 (other secretins) [44,45,46].
2.1. G protein Coupled Receptor-120 (GPR120)
3. Inflammatory Background of Metabolic Diseases
3.1. Inflammatory Response in Obesity
3.2. Anti-Inflammatory and Metabolic Effects of GPR120 Signaling in the Context of Overweight and Obesity
3.2.1. GPR120 in Adipose Tissue
3.2.2. GPR120 and Gastrointestinal Hormones
3.2.3. GPR120 and the Endocrine Function of the Pancreas
4. Targeting GPR120 Signaling as a Promising Therapeutic Approach in Obesity: The Need for New Ligands
4.1. Non-LCFA GPR120 Agonists Derived from Compounds of Natural Origin
4.2. GPR120 Synthetic Agonists
5. Concluding Remarks
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Conflicts of Interest
Abbreviations
| 7TM receptors | seven transmembrane domain receptors, also known as G protein-coupled receptors (GPCRs) |
| 9-PAHSA | palmitic-acid-9-hydroxy-stearic-acid |
| Ω-3 FAs | omega-3-fatty acids |
| AD | Alzheimer’s disease |
| ALA | alpha-linolenic acid |
| ANGPTL2 | angiopoietin-like 2 protein |
| APCs | antigen presenting cells |
| ARRβ2 | beta-arrestin2 |
| AT | adipose tissue |
| ATP | adenosine triphosphate |
| BAT | brown adipose tissue |
| BMI | body mass index |
| cAMP | cyclic adenosine 3,5-monophosphate |
| CCK | cholecystokinin |
| CICR | calcium-induced calcium release |
| CNS | central nervous system |
| cpdA | compound A |
| CRF2 | corticotropin-releasing factor type-2 |
| CRF2R | corticotropin-releasing factor type-2 receptor |
| CTL | cytotoxic T lymphocytes |
| DAG | diacyl glycerol |
| DHA | docosahexaenoic acid |
| DIO | diet-induced obesity |
| DPP-IV | dipeptidyl peptidase-IV |
| EC50 | half maximal effective concentration |
| ECL1–ECL3 | three extracellular loops (from 1 to 3) forming the GPCR |
| eNAMPT | extracellular nicotinamide phosphoribosyl transferase |
| EPA | eicosapentaenoic acid |
| ERK1/2 | extracellular regulated protein kinases 1/2 |
| ERKs | extracellular signal-regulated kinases |
| FDA | U.S. Food and Drug Administration |
| FFAR1 | free fatty acid receptor 1, also known as GPR40 |
| FFAR4 | free fatty acid receptor 4, also known as GPR120 |
| FFAs | free fatty acids |
| FGF-21 | fibroblast growth factor-21 |
| GDP | guanosine diphosphate |
| GEF | guanine nucleotide exchange factor |
| GHIH | growth hormone-inhibiting hormone, also known as somatotropin release inhibiting factor (SRIF) |
| GIP | gastric inhibitory polypeptide, also known as glucose-dependent insulinotropic polypeptide |
| GLP-1 | glucagon-like peptide-1 |
| GLUT4 | glucose transporter type 4 |
| GPCRs | G protein-coupled receptors, also known as seven transmembrane domain (7TM) receptors |
| GPR40 | G-protein-coupled receptor 40, also known as FFAR1 |
| GPR120 | G protein-coupled receptor 120, also known as FFAR4 |
| GPR120L | a long form of GPR120, |
| GPR120S | a short form of GPR120 |
| GRAFS | acronym defining classification of GPCRs that stands for Glutamate, Rhodopsin, Adhesion, Frizzled/Taste2 and Secretin |
| GSIS | glucose-stimulated insulin secretion |
| GSSS | glucose-stimulated somatostatin secretion |
| GTP | guanosine triphosphate |
| HbA1c | hemoglobin A1C |
| HDL | high-density lipoprotein |
| HEC | human embryonic kidney |
| HFD | high-fat diet |
| HIF-1 | hypoxia-induced factor 1 |
| ICL1–ICL3 | three intracellular loops (from 1 to 3) forming the GPCR |
| IFN-γ | interferon gamma |
| IKKβ | nuclear factor kappa-B kinase |
| IL1R | interleukin 1 receptor |
| IL-1RA | interleukin 1 receptor antagonist |
| ILs | interleukins, including IL-1β, IL-6, IL-8), |
| iNAMPT | intracellular nicotinamide phosphoribosyl transferase |
| INSR | insulin receptor |
| IP3 | inositol 1,4,5-trisphosphate |
| IR | insulin resistance |
| IRSs | insulin receptor substrates |
| IVGTT | intravenous glucose tolerance test |
| JNK | c-Jun N-terminal kinase |
| KATP | ATP-sensitive potassium channels |
| LA | linolenic acid |
| LCFAs | long-chain fatty acids |
| LPS | lipopolysaccharide |
| MAP3K7 | TGF-β activated kinase 1 |
| M1, M2 macrophages | classically activated and alternatively activated macrophages, respectively |
| MARTs | mono ADP-ribosyl transferases |
| MCFAs | medium-chain fatty acids |
| MCP-1 | monocyte chemoattractant protein-1, also known as CCL2 |
| MMPs | matrix metalloproteinases |
| MiMP | mitochondrial membrane potential |
| NAc | nucleus accumbens |
| N.A.D. | denotes no data or ambiguous data |
| NAFLD | nonalcoholic fatty liver disease |
| NAMPT | nicotinamide phosphoribosyl transferase |
| NCG | N-Carbamoyl-Beta-D-Glucopyranosylamine |
| NEMO | nuclear factor kappa-light-chain-enhancer of activated B cells (NF-кB) essential modulator |
| NF-κB | nuclear factor kappa-light-chain-enhancer of activated B cells |
| NLRP3 inflammasome | nucleotide-binding oligomerization domain (NOD), leucine-rich repeat (LRR)-containing protein (NLR) family member 3 inflammasome |
| PARPs | poly ADP-ribose polymerases |
| PC1/3 | proprotein convertase 1/3 |
| PDX1 | pancreatic duodenal homeobox-1 |
| pERK1/2 | phosphorylated extracellular regulated protein kinases 1/2 |
| PI3K | phosphoinositide 3-kinase |
| PIP2 | phosphatidylinositol 4,5-bisphosphate |
| PKC | protein kinase C |
| PLC-β | phospholipase C-beta |
| PPARγ | peroxisome proliferator-activated receptor gamma |
| PUFAs | polyunsaturated fatty acids |
| RAW 264.7 | monocyte/macrophage-like cell line |
| ROS | reactive oxygen species |
| RXRα | retinoid X receptor alpha |
| SAAs | sulfur amino acids |
| S1P | sphingosine-1-phosphate |
| S1P1 | sphingosine-1-phosphate receptor-1 |
| SCFAs | short-chain fatty acids |
| SNP | single nucleotide polymorphism |
| SPM | specialized pro-resolving mediators |
| SRIF | somatotropin release inhibiting factor, also known as growth hormone-inhibiting hormone (GHIH) |
| STC-1 | secretin tumor cell line 1 |
| S-V cells | stromal-vascular cells |
| T2D | type 2 diabetes mellitus |
| TAB1 | TAK1 binding protein 1 |
| TAK1 | TGFβ-activated kinase 1 |
| TGFβ | transforming growth factor-beta |
| Th1, Th2, Th17 | types of lymphocyte subpopulations |
| TLR4 | toll-like receptor 4 |
| TM1–TM7 | seven transmembrane heptahelical structures (from 1 to 7) forming GPCR |
| TNFR | tumor necrosis factor receptor |
| UCN3 | urocortin 3 |
| UCP1 | uncoupling protein 1 |
| VEGF | vascular endothelial growth factor |
| WAT | white adipose tissue |
| ZDF | Zucker Diabetic Fatty (rats) |
References
- Heindel, J.J.; Blumberg, B.; Cave, M.; Machtinger, R.; Mantovani, A.; Mendez, M.A.; Nadal, A.; Palanza, P.; Panzica, G.; Sargis, R.; Vandenberg, L.N.; Vom Saal, F. Metabolism disrupting chemicals and metabolic disorders. Reprod Toxicol. 2017, 68, 3–33. [Google Scholar] [CrossRef] [PubMed]
- Tummolo, A.; Carella, R.; De Giovanni, D.; Paterno, G.; Simonetti, S.; Tolomeo, M.; Leone, P.; Barile, M. Micronutrient Deficiency in Inherited Metabolic Disorders Requiring Diet Regimen: A Brief Critical Review. Int J Mol Sci. 2023, 24, 17024. [Google Scholar] [CrossRef] [PubMed]
- Nemer, M.; Osman, F.; Said, A. Dietary macro and micronutrients associated with MASLD: Analysis of a national US cohort database. Ann Hepatol. 2024, 29, 101491. [Google Scholar] [CrossRef]
- Ahola, A.J.; Harjutsalo, V.; Thorn, L.M.; Freese, R.; Forsblom, C.; Mäkimattila, S.; Groop, P.H. The association between macronutrient intake and the metabolic syndrome and its components in type 1 diabetes. Br J Nutr. 2017, 117, 450–456. [Google Scholar] [CrossRef]
- Saklayen, M.G. The Global Epidemic of the Metabolic Syndrome. Curr Hypertens Rep. 2018, 20, 12. [Google Scholar] [CrossRef]
- Safaei, M.; Sundararajan, E.A.; Driss, M.; Boulila, W.; Shapi'i, A. A systematic literature review on obesity: Understanding the causes & consequences of obesity and reviewing various machine learning approaches used to predict obesity. Comput Biol Med. 2021, 136, 104754. [Google Scholar] [CrossRef]
- Hruby, A.; Hu, F.B. The Epidemiology of Obesity: A Big Picture. Pharmacoeconomics. 2015, 33, 673–89. [Google Scholar] [CrossRef] [PubMed]
- Boutari, C.; Mantzoros, C.S. A 2022 update on the epidemiology of obesity and a call to action: as its twin COVID-19 pandemic appears to be receding, the obesity and dysmetabolism pandemic continues to rage on. Metabolism. 2022, 133, 155217. [Google Scholar] [CrossRef]
- World Obesity Federation. World Obesity Atlas 2024. London: World Obesity Federation, 2024. Available online: https://data.worldobesity.org/publications/?cat=22.
- Zhang, X.; Liu, J.; Ni, Y.; Yi, C.; Fang, Y.; Ning, Q.; Shen, B.; Zhang, K.; Liu, Y.; Yang, L.; Li, K.; Liu, Y.; Huang, R.; Li, Z. Global Prevalence of Overweight and Obesity in Children and Adolescents: A Systematic Review and Meta-Analysis. JAMA Pediatr. 2024, 178, 800–813. [Google Scholar] [CrossRef]
- Nuttall, F.Q. Body Mass Index: Obesity, BMI, and Health: A Critical Review. Nutr Today. 2015, 50, 117–128. [Google Scholar] [CrossRef]
- Tirthani, E.; Said, M.S.; Rehman, A. Genetics and Obesity. [Updated 2023 Jul 31]. In: StatPearls [Internet]. Treasure Island (FL): StatPearls Publishing; 2024 Jan-. Available online: https://www.ncbi.nlm.nih.gov/books/NBK573068/.
- Smith, E.N.L.; Chandanathil, M.; Millis, R.M. Epigenetic Mechanisms in Obesity: Broadening Our Understanding of the Disease. Cureus. 2023, 15, e47875. [Google Scholar] [CrossRef] [PubMed]
- Keller, M.; Svensson, S.I.A.; Rohde-Zimmermann, K.; Kovacs, P.; Böttcher, Y. Genetics and Epigenetics in Obesity: What Do We Know so Far? Curr Obes Rep. 2023, 12, 482–501. [Google Scholar] [CrossRef]
- Lee, A.; Cardel, M.; Donahoo, W.T. Social and Environmental Factors Influencing Obesity. [Updated 2019 Oct 12]. In: Feingold KR, Anawalt B, Blackman MR, et al., editors. Endotext [Internet]. South Dartmouth (MA): MDText.com, Inc.; 2000-. Available online: https://www.ncbi.nlm.nih.gov/books/NBK278977/.
- Yang, M.; Liu, S.; Zhang, C. The Related Metabolic Diseases and Treatments of Obesity. Healthcare (Basel). 2022, 10, 1616. [Google Scholar] [CrossRef] [PubMed]
- Ansari, S.; Haboubi, H.; Haboubi, N. Adult obesity complications: challenges and clinical impact. Ther Adv Endocrinol Metab. 2020, 11, 2042018820934955. [Google Scholar] [CrossRef]
- Jin, X.; Qiu, T.; Li, L.; Yu, R.; Chen, X.; Li, C.; Proud, C.G.; Jiang, T. Pathophysiology of obesity and its associated diseases. Acta Pharm Sin B. 2023, 13, 2403–2424. [Google Scholar] [CrossRef]
- Pinto, K.R.D.; Feckinghaus, C.M.; Hirakata, V.N. Obesity as a predictive factor for chronic kidney disease in adults: systematic review and meta-analysis. Braz J Med Biol Res. 2021, 54, e10022. [Google Scholar] [CrossRef] [PubMed]
- Rajesh, Y.; Sarkar, D. Association of Adipose Tissue and Adipokines with Development of Obesity-Induced Liver Cancer. Int J Mol Sci. 2021, 22, 2163. [Google Scholar] [CrossRef]
- Tzenios, N.; Tazanios, M.E.; Chahine, M. The impact of BMI on breast cancer - an updated systematic review and meta-analysis. Medicine (Baltimore). 2024, 103, e36831. [Google Scholar] [CrossRef]
- Tzenios, N.; Tazanios, M.E.; Chahine, M. The impact of body mass index on prostate cancer: An updated systematic review and meta-analysis. Medicine (Baltimore). 2022, 101, e30191. [Google Scholar] [CrossRef]
- Opio, J.; Wynne, K.; Attia, J.; Oldmeadow, C.; Hancock, S.; Kelly, B.; Inder, K.; McEvoy, M. Metabolic Health, Overweight or Obesity, and Depressive Symptoms among Older Australian Adults. Nutrients. 2024, 16, 928. [Google Scholar] [CrossRef]
- Maurizi, G.; Della Guardia, L.; Maurizi, A.; Poloni, A. Adipocytes properties and crosstalk with immune system in obesity-related inflammation. J Cell Physiol. 2018, 233, 88–97. [Google Scholar] [CrossRef]
- Savulescu-Fiedler, I.; Mihalcea, R.; Dragosloveanu, S.; Scheau, C.; Baz, R.O.; Caruntu, A.; Scheau, A.E.; Caruntu, C.; Benea, S.N. The Interplay between Obesity and Inflammation. Life (Basel). 2024, 14, 856. [Google Scholar] [CrossRef] [PubMed]
- Guria, S.; Hoory, A.; Das, S.; Chattopadhyay, D.; Mukherjee, S. Adipose tissue macrophages and their role in obesity-associated insulin resistance: an overview of the complex dynamics at play. Biosci Rep. 2023, 43, BSR20220200. [Google Scholar] [CrossRef] [PubMed]
- Zatterale, F.; Longo, M.; Naderi, J.; Raciti, G.A.; Desiderio, A.; Miele, C.; Beguinot, F. Chronic Adipose Tissue Inflammation Linking Obesity to Insulin Resistance and Type 2 Diabetes. Front Physiol. 2020, 10, 1607. [Google Scholar] [CrossRef]
- Szukiewicz, D. Molecular Mechanisms for the Vicious Cycle between Insulin Resistance and the Inflammatory Response in Obesity. Int J Mol Sci. 2023, 24, 9818. [Google Scholar] [CrossRef]
- Zhang, M.; Chen, T.; Lu, X.; Lan, X.; Chen, Z.; Lu, S. G protein-coupled receptors (GPCRs): advances in structures, mechanisms, and drug discovery. Signal Transduct Target Ther. 2024, 9, 88. [Google Scholar] [CrossRef] [PubMed]
- Liu, S.; Anderson, P.J.; Rajagopal, S.; Lefkowitz, R.J.; Rockman, H.A. G Protein-Coupled Receptors: A Century of Research and Discovery. Circ Res. 2024, 135, 174–197. [Google Scholar] [CrossRef]
- Liu HD, Wang WB, Xu ZG, Liu CH, He DF, Du LP, Li MY, Yu X, Sun JP. FFA4 receptor (GPR120): A hot target for the development of anti-diabetic therapies. Eur J Pharmacol. 2015; 763(Pt B):160-8. [CrossRef]
- Al Mahri, S.; Malik, S.S.; Al Ibrahim, M.; Haji, E.; Dairi, G.; Mohammad, S. Free Fatty Acid Receptors (FFARs) in Adipose: Physiological Role and Therapeutic Outlook. Cells. 2022, 11, 750. [Google Scholar] [CrossRef]
- Royal Swedish Academy of Sciences (10 October 2012) "The Nobel Prize in Chemistry 2012 Robert, J. Lefkowitz, Brian K. Kobilka". Retrieved 10 October 2012.
- Vithani, N.; Todd, T.D.; Singh, S.; Trent, T.; Blumer, K.J.; Bowman, G.R. G Protein Activation Occurs via a Largely Universal Mechanism. J Phys Chem B. 2024, 128, 3554–3562. [Google Scholar] [CrossRef]
- Afzal, M.S. G proteins: binary switches in health and disease. Cent Eur J Immunol. 2020, 45, 364–367. [Google Scholar] [CrossRef]
- Calvert PD, Krasnoperova NV, Lyubarsky AL, Isayama T, Nicoló M, Kosaras B, Wong G, Gannon KS, Margolskee RF, Sidman RL, Pugh EN Jr, Makino CL, Lem J. Phototransduction in transgenic mice after targeted deletion of the rod transducin alpha -subunit. Proc Natl Acad Sci U S A. 2000, 97, 13913-8. [CrossRef]
- Syrovatkina, V.; Alegre, K.O.; Dey, R.; Huang, X.Y. Regulation, Signaling, and Physiological Functions of G-Proteins. J Mol Biol. 2016, 428, 3850–68. [Google Scholar] [CrossRef] [PubMed]
- Liu, Y.; Wang, X.; Dong, D.; Guo, L.; Dong, X.; Leng, J.; Zhao, B.; Guo, Y.D.; Zhang, N. Research Advances in Heterotrimeric G-Protein α Subunits and Uncanonical G-Protein Coupled Receptors in Plants. Int J Mol Sci. 2021, 22, 8678. [Google Scholar] [CrossRef]
- Rehman, S.; Rahimi, N.; Dimri, M. Biochemistry, G Protein Coupled Receptors. [Updated 2023 Jul 30]. In: StatPearls [Internet]. Treasure Island (FL): StatPearls Publishing; 2024 Jan-. Available online: https://www.ncbi.nlm.nih.gov/books/NBK518966/.
- Odoemelam CS, Percival B, Wallis H, Chang MW, Ahmad Z, Scholey D, Burton E, Williams IH, Kamerlin CL, Wilson PB. G-Protein coupled receptors: structure and function in drug discovery. RSC Adv. 2020, 10, 36337–36348. [CrossRef]
- Yang, D.; Zhou, Q.; Labroska, V.; Qin, S.; Darbalaei, S.; Wu, Y.; Yuliantie, E.; Xie, L.; Tao, H.; Cheng, J.; Liu, Q.; Zhao, S.; Shui, W.; Jiang, Y.; Wang, M.W. G protein-coupled receptors: structure- and function-based drug discovery. Signal Transduct Target Ther. 2021, 6, 7. [Google Scholar] [CrossRef]
- Fredriksson, R.; Lagerström, M.C.; Lundin, L.G.; Schiöth, H.B. The G-protein-coupled receptors in the human genome form five main families. Phylogenetic analysis, paralogon groups, and fingerprints. Mol Pharmacol. 2003, 63, 1256–72. [Google Scholar] [CrossRef]
- Wess, J. Designer GPCRs as Novel Tools to Identify Metabolically Important Signaling Pathways. Front Endocrinol (Lausanne). 2021, 12, 706957. [Google Scholar] [CrossRef]
- Scholz, N.; Langenhan, T.; Schöneberg, T. Revisiting the classification of adhesion GPCRs. Ann N Y Acad Sci. 2019, 1456, 80–95. [Google Scholar] [CrossRef]
- Krishnan, A.; Nijmeijer, S.; de Graaf, C.; Schiöth, H.B. Classification, Nomenclature, and Structural Aspects of Adhesion GPCRs. Handb Exp Pharmacol. 2016, 234, 15–41. [Google Scholar] [CrossRef]
- Wittlake, A.; Prömel, S.; Schöneberg, T. The Evolutionary History of Vertebrate Adhesion GPCRs and Its Implication on Their Classification. Int J Mol Sci. 2021, 22, 11803. [Google Scholar] [CrossRef]
- Zhou, Q.; Yang, D.; Wu, M.; Guo, Y.; Guo, W.; Zhong, L.; Cai, X.; Dai, A.; Jang, W.; Shakhnovich, E.I.; Liu, Z.J.; Stevens, R.C.; Lambert, N.A.; Babu, M.M.; Wang, M.W.; Zhao, S. Common activation mechanism of class A GPCRs. Elife. 2019, 8, e50279. [Google Scholar] [CrossRef] [PubMed]
- Stuttgen GM, Sahoo D. FFAR4: A New Player in Cardiometabolic Disease? Endocrinology 2021, 162, bqab111. [CrossRef] [PubMed]
- Rosenbaum, D.M.; Rasmussen, S.G.; Kobilka, B.K. The structure and function of G-protein-coupled receptors. Nature. 2009, 459, 356–63. [Google Scholar] [CrossRef]
- Venkatakrishnan, A.J.; Deupi, X.; Lebon, G.; Tate, C.G.; Schertler, G.F.; Babu, M.M. Molecular signatures of G-protein-coupled receptors. Nature. 2013, 494, 185–94. [Google Scholar] [CrossRef]
- Edward Zhou, X.; Melcher, K.; Eric Xu, H. Structural biology of G protein-coupled receptor signaling complexes. Protein Sci. 2019, 28, 487–501. [Google Scholar] [CrossRef]
- Cheng, L.; Xia, F.; Li, Z.; Shen, C.; Yang, Z.; Hou, H.; Sun, S.; Feng, Y.; Yong, X.; Tian, X.; Qin, H.; Yan, W.; Shao, Z. Structure, function and drug discovery of GPCR signaling. Mol Biomed. 2023, 4, 46. [Google Scholar] [CrossRef]
- Laschet, C.; Dupuis, N.; Hanson, J. The G protein-coupled receptors deorphanization landscape. Biochem Pharmacol. 2018, 153, 62–74. [Google Scholar] [CrossRef] [PubMed]
- Alexander SPH, Christopoulos A, Davenport AP, Kelly E, Mathie A, Peters JA, Veale EL, Armstrong JF, Faccenda E, Harding SD, Pawson AJ, Sharman JL, Southan C, Davies JA; CGTP Collaborators. THE CONCISE GUIDE TO PHARMACOLOGY 2019/20: G protein-coupled receptors. Br J Pharmacol. 2019;176 Suppl 1(Suppl 1):S21-S141. [CrossRef]
- Santhanam, B.; Sluter, M.; Babu, M.M. Exploring GPCR signaling pathway networks as cancer therapeutic targets. Cell Genom. 2024, 4, 100560. [Google Scholar] [CrossRef]
- Arora, C.; Matic, M.; Bisceglia, L.; Di Chiaro, P.; De Oliveira Rosa, N.; Carli, F.; Clubb, L.; Nemati Fard, L.A.; Kargas, G.; Diaferia, G.R.; Vukotic, R.; Licata, L.; Wu, G.; Natoli, G.; Gutkind, J.S.; Raimondi, F. The landscape of cancer-rewired GPCR signaling axes. Cell Genom. 2024, 4, 100557. [Google Scholar] [CrossRef]
- Wang J, Gareri C, Rockman HA. G-Protein-Coupled Receptors in Heart Disease. Circ Res. 2018, 123, 716–735. [CrossRef]
- Zhao, J.; Deng, Y.; Jiang, Z.; Qing, H. G Protein-Coupled Receptors (GPCRs) in Alzheimer's Disease: A Focus on BACE1 Related GPCRs. Front Aging Neurosci. 2016, 8, 58. [Google Scholar] [CrossRef] [PubMed]
- Wong, T.S.; Li, G.; Li, S.; Gao, W.; Chen, G.; Gan, S.; Zhang, M.; Li, H.; Wu, S.; Du, Y. G protein-coupled receptors in neurodegenerative diseases and psychiatric disorders. Signal Transduct Target Ther. 2023, 8, 177. [Google Scholar] [CrossRef] [PubMed]
- Schöneberg, T.; Liebscher, I. Mutations in G Protein-Coupled Receptors: Mechanisms, Pathophysiology and Potential Therapeutic Approaches. Pharmacol Rev. 2021, 73, 89–119. [Google Scholar] [CrossRef]
- Thompson, M.D.; Percy, M.E.; Cole, D.E.C.; Bichet, D.G.; Hauser, A.S.; Gorvin, C.M. G protein-coupled receptor (GPCR) gene variants and human genetic disease. Crit Rev Clin Lab Sci. 2024, 61, 317–346. [Google Scholar] [CrossRef]
- Shimada I, Ueda T, Kofuku Y, Eddy MT, Wüthrich K. GPCR drug discovery: integrating solution NMR data with crystal and cryo-EM structures. Nat Rev Drug Discov 2019, 18, 59–82. [CrossRef]
- Saikia, S.; Bordoloi, M.; Sarmah, R. Established and In-trial GPCR Families in Clinical Trials: A Review for Target Selection. Curr Drug Targets. 2019, 20, 522–539. [Google Scholar] [CrossRef] [PubMed]
- Hauser, A.S.; Chavali, S.; Masuho, I.; Jahn, L.J.; Martemyanov, K.A.; Gloriam, D.E.; Babu, M.M. Pharmacogenomics of GPCR Drug Targets. Cell. 2018;172(1-2):41-54.e19. [CrossRef]
- Sriram, K.; Insel, P.A. G Protein-Coupled Receptors as Targets for Approved Drugs: How Many Targets and How Many Drugs? Mol Pharmacol. 2018, 93, 251–258. [Google Scholar] [CrossRef]
- Wang, A.; Gu, Z.; Heid, B.; Akers, R.M.; Jiang, H. Identification and characterization of the bovine G protein-coupled receptor GPR41 and GPR43 genes. J Dairy Sci. 2009, 92, 2696–705. [Google Scholar] [CrossRef]
- Ang, Z.; Ding, J.L. GPR41 and GPR43 in Obesity and Inflammation - Protective or Causative? Front Immunol. 2016, 7, 28. [Google Scholar] [CrossRef]
- Luscombe, V.B.; Lucy, D.; Bataille, C.J.R.; Russell, A.J.; Greaves, D.R. 20 Years an Orphan: Is GPR84 a Plausible Medium-Chain Fatty Acid-Sensing Receptor? DNA Cell Biol. 2020;39 (11):1926-1937. [CrossRef]
- Milligan, G.; Alvarez-Curto, E.; Watterson, K.R.; Ulven, T.; Hudson, B.D. Characterizing pharmacological ligands to study the long-chain fatty acid receptors GPR40/FFA1 and GPR120/FFA4. Br J Pharmacol. 2015, 172, 3254–65. [Google Scholar] [CrossRef]
- Son, S.E.; Kim, N.J.; Im, D.S. Development of Free Fatty Acid Receptor 4 (FFA4/GPR120) Agonists in Health Science. Biomol Ther (Seoul). 2021, 29, 22–30. [Google Scholar] [CrossRef] [PubMed]
- Galindo, M.M.; Voigt, N.; Stein, J.; van Lengerich, J.; Raguse, J.D.; Hofmann, T.; Meyerhof, W.; Behrens, M. G protein-coupled receptors in human fat taste perception. Chem Senses. 2012, 37, 123–39. [Google Scholar] [CrossRef]
- Carullo, G.; Mazzotta, S.; Vega-Holm, M.; Iglesias-Guerra, F.; Vega-Pérez, J.M.; Aiello, F.; Brizzi, A. GPR120/FFAR4 Pharmacology: Focus on Agonists in Type 2 Diabetes Mellitus Drug Discovery. J Med Chem. 2021, 64, 4312–4332. [Google Scholar] [CrossRef] [PubMed]
- Moore, K.; Zhang, Q.; Murgolo, N.; Hosted, T.; Duffy, R. Cloning, expression, and pharmacological characterization of the GPR120 free fatty acid receptor from cynomolgus monkey: comparison with human GPR120 splice variants. Comp Biochem Physiol B Biochem Mol Biol. 2009, 154, 419–26. [Google Scholar] [CrossRef]
- Watson, S.J.; Brown, A.J.; Holliday, N.D. Differential signaling by splice variants of the human free fatty acid receptor GPR120. Mol Pharmacol. 2012, 81, 631–42. [Google Scholar] [CrossRef]
- Zhang, X.; Guseinov, A.A.; Jenkins, L.; Li, K.; Tikhonova, I.G.; Milligan, G.; Zhang, C. Structural basis for the ligand recognition and signaling of free fatty acid receptors. Sci Adv. 2024, 10, eadj2384. [Google Scholar] [CrossRef]
- Sadler, F.; Ma, N.; Ritt, M.; Sharma, Y.; Vaidehi, N.; Sivaramakrishnan, S. Autoregulation of GPCR signalling through the third intracellular loop. Nature. 2023, 615, 734–741. [Google Scholar] [CrossRef] [PubMed]
- Burns, R.N.; Moniri, N.H. Agonism with the omega-3 fatty acids alpha-linolenic acid and docosahexaenoic acid mediates phosphorylation of both the short and long isoforms of the human GPR120 receptor. Biochem Biophys Res Commun. 2010, 396, 1030–5. [Google Scholar] [CrossRef]
- Kimura, I.; Ichimura, A.; Ohue-Kitano, R.; Igarashi, M. Free Fatty Acid Receptors in Health and Disease. Physiol Rev. 2020, 100, 171–210. [Google Scholar] [CrossRef]
- Vestmar, M.A.; Andersson, E.A.; Christensen, C.R.; Hauge, M.; Glümer, C.; Linneberg, A.; Witte, D.R.; Jørgensen, M.E.; Christensen, C.; Brandslund, I.; Lauritzen, T.; Pedersen, O.; Holst, B.; Grarup, N.; Schwartz, T.W.; Hansen, T. Functional and genetic epidemiological characterisation of the FFAR4 (GPR120) p. R270H variant in the Danish population. J Med Genet. 2016, 53, 616–23. [Google Scholar] [CrossRef]
- Oh, D.Y.; Walenta, E. Omega-3 Fatty Acids and FFAR4. Front Endocrinol (Lausanne). 2014; 5:115. [CrossRef]
- Cheshmehkani, A.; Senatorov, I.S.; Kandi, P.; Singh, M.; Britt, A.; Hayslett, R.; Moniri, N.H. Fish oil and flax seed oil supplemented diets increase FFAR4 expression in the rat colon. Inflamm Res. 2015, 64, 809–815. [Google Scholar] [CrossRef] [PubMed]
- Yin, J.; Li, H.; Meng, C.; Chen, D.; Chen, Z.; Wang, Y.; Wang, Z.; Chen, G. Inhibitory effects of omega-3 fatty acids on early brain injury after subarachnoid hemorrhage in rats: Possible involvement of G protein-coupled receptor 120/β-arrestin2/TGF-β activated kinase-1 binding protein-1 signaling pathway. Int J Biochem Cell Biol. 2016, 75, 11–22. [Google Scholar] [CrossRef] [PubMed]
- Cornall, L.M.; Mathai, M.L.; Hryciw, D.H.; McAinch, A.J. Diet-induced obesity up-regulates the abundance of GPR43 and GPR120 in a tissue specific manner. Cell Physiol Biochem. 2011, 28, 949–58. [Google Scholar] [CrossRef]
- Karakuła-Juchnowicz, H.; Róg, J.; Juchnowicz, D.; Morylowska-Topolska, J. GPR120: Mechanism of action, role and potential for medical applications. Postepy Hig Med Dosw (Online). 2017, 71, 942–953. [Google Scholar] [CrossRef]
- Gotoh, C.; Hong, Y.H.; Iga, T.; Hishikawa, D.; Suzuki, Y.; Song, S.H.; Choi, K.C.; Adachi, T.; Hirasawa, A.; Tsujimoto, G.; Sasaki, S.; Roh, S.G. The regulation of adipogenesis through GPR120. Biochem Biophys Res Commun. 2007, 354, 591–7. [Google Scholar] [CrossRef] [PubMed]
- Moriyama, R.; Deura, C.; Imoto, S.; Nose, K.; Fukushima, N. Expression of the long-chain fatty acid receptor GPR120 in the gonadotropes of the mouse anterior pituitary gland. Histochem Cell Biol. 2015, 143, 21–7. [Google Scholar] [CrossRef]
- Nakamura, S.; Noda, K.; Miwa, M.; Minabe, S.; Hagiwara, T.; Hirasawa, A.; Matsuyama, S.; Moriyama, R. Colocalization of GPR120 and anterior pituitary hormone-producing cells in female Japanese Black cattle. J Reprod Dev. 2020, 66, 135–141. [Google Scholar] [CrossRef]
- Deura, C.; Kimura, Y.; Nonoyama, T.; Moriyama, R. Gpr120 mRNA expression in gonadotropes in the mouse pituitary gland is regulated by free fatty acids. J Reprod Dev. 2020; 66:249-254. [CrossRef]
- Duah, M.; Zhang, K.; Liang, Y.; Ayarick, V.A.; Xu, K.; Pan, B. Immune regulation of poly unsaturated fatty acids and free fatty acid receptor 4. J Nutr Biochem. 2023, 112, 109222. [Google Scholar] [CrossRef]
- Kim, J.M.; Lee, K.P.; Park, S.J.; Kang, S.; Huang, J.; Lee, J.M.; Sato, K.; Chung, H.Y.; Okajima, F.; Im, D.S. Omega-3 fatty acids induce Ca(2+) mobilization responses in human colon epithelial cell lines endogenously expressing FFA4. Acta Pharmacol Sin. 2015, 36, 813–20. [Google Scholar] [CrossRef]
- Oh DY, Talukdar S, Bae EJ, Imamura T, Morinaga H, Fan W, Li P, Lu WJ, Watkins SM, Olefsky JM. GPR120 is an omega-3 fatty acid receptor mediating potent anti-inflammatory and insulin-sensitizing effects. Cell 2010, 142, 687–98. [CrossRef]
- Kasonga, A.E.; Kruger, M.C.; Coetzee, M. Free fatty acid receptor 4-β-arrestin 2 pathway mediates the effects of different classes of unsaturated fatty acids in osteoclasts and osteoblasts. Biochim Biophys Acta Mol Cell Biol Lipids. 2019, 1864, 281–289. [Google Scholar] [CrossRef] [PubMed]
- Alharbi, A.G.; Tobin, A.B.; Milligan, G. How Arrestins and GRKs Regulate the Function of Long Chain Fatty Acid Receptors. Int J Mol Sci. 2022, 23, 12237. [Google Scholar] [CrossRef]
- Schulte, G.; Fredholm, B.B. Signalling from adenosine receptors to mitogen-activated protein kinases. Cell Signal. 2003, 15, 813–27. [Google Scholar] [CrossRef]
- Anbazhagan, A.N.; Priyamvada, S.; Gujral, T.; Bhattacharyya, S.; Alrefai, W.A.; Dudeja, P.K.; Borthakur, A. A novel anti-inflammatory role of GPR120 in intestinal epithelial cells. Am J Physiol Cell Physiol. 2016, 310, C612–C621. [Google Scholar] [CrossRef] [PubMed]
- Aydin, Y.; Coin, I. Biochemical insights into structure and function of arrestins. FEBS J. 2021, 288, 2529–2549. [Google Scholar] [CrossRef]
- Zhao, Y.F. Free fatty acid receptors in the endocrine regulation of glucose metabolism: Insight from gastrointestinal-pancreatic-adipose interactions. Front Endocrinol (Lausanne). 2022, 13, 956277. [Google Scholar] [CrossRef] [PubMed]
- Sidhu, S.S.; Thompson, D.G.; Warhurst, G.; Case, R.M.; Benson, R.S. Fatty acid-induced cholecystokinin secretion and changes in intracellular Ca2+ in two enteroendocrine cell lines, STC-1 and GLUTag. J Physiol. 2000;528 Pt 1(Pt 1):165-76. [CrossRef]
- Rhee, S.G. Regulation of phosphoinositide-specific phospholipase C. Annu Rev Biochem. 2001, 70, 281–312. [Google Scholar] [CrossRef]
- Danciu, T.E.; Adam, R.M.; Naruse, K.; Freeman, M.R.; Hauschka, P.V. Calcium regulates the PI3K-Akt pathway in stretched osteoblasts. FEBS Lett. 2003;536(1-3):193-7. [CrossRef]
- Liang, Y.; Yin, W.; Yin, Y.; Zhang, W. Ghrelin Based Therapy of Metabolic Diseases. Curr Med Chem. 2021, 28, 2565–2576. [Google Scholar] [CrossRef]
- Bang, A.S.; Soule, S.G.; Yandle, T.G.; Richards, A.M.; Pemberton, C.J. Characterisation of proghrelin peptides in mammalian tissue and plasma. J Endocrinol. 2007, 192, 313–23. [Google Scholar] [CrossRef]
- Simonds, W.F. G protein regulation of adenylate cyclase. Trends Pharmacol Sci. 1999; 20:66-73. [CrossRef]
- Fredriksson, R.; Höglund, P.J.; Gloriam, D.E.; Lagerström, M.C.; Schiöth, H.B. Seven evolutionarily conserved human rhodopsin G protein-coupled receptors lacking close relatives. FEBS Lett. 2003, 554, 381–8. [Google Scholar] [CrossRef]
- da Silva Batista, E.; Nakandakari, S.C.B.R.; Ramos da Silva, A.S.; Pauli, J.R.; Pereira de Moura, L.; Ropelle, E.R.; Camargo, E.A.; Cintra, D.E. Omega-3 pleiad: The multipoint anti-inflammatory strategy. Crit Rev Food Sci Nutr. 2024, 64, 4817–4832. [Google Scholar] [CrossRef] [PubMed]
- Yang, L.; Lei, X.T.; Huang, Q.; Wang, T.; Sun, H.B.; Wang, H.Y. A novel GPR120-selective agonist promotes insulin secretion and improves chronic inflammation. Life Sci. 2021, 269, 119029. [Google Scholar] [CrossRef] [PubMed]
- Suckow, A.T.; Polidori, D.; Yan, W.; Chon, S.; Ma, J.Y.; Leonard, J.; Briscoe, C.P. Alteration of the glucagon axis in GPR120 (FFAR4) knockout mice: a role for GPR120 in glucagon secretion. J Biol Chem. 2014, 289, 15751–63. [Google Scholar] [CrossRef]
- Wang, Y.; Liu, H.; Zhang, Z. Recent Advance in Regulatory Effect of GRP120 on Bone Metabolism. Aging Dis. 2023, 14, 1714–1727. [Google Scholar] [CrossRef]
- Zhang, X.; Macielag, M.J. GPR120 agonists for the treatment of diabetes: a patent review (2014 present). Expert Opin Ther Pat. 2020, 30, 729–742. [Google Scholar] [CrossRef]
- Satapati, S.; Qian, Y.; Wu, M.S.; Petrov, A.; Dai, G.; Wang, S.P.; Zhu, Y.; Shen, X.; Muise, E.S.; Chen, Y.; Zycband, E.; Weinglass, A.; Di Salvo, J.; Debenham, J.S.; Cox, J.M.; Lan, P.; Shah, V.; Previs, S.F.; Erion, M.; Kelley, D.E.; Wang, L.; Howard, A.D.; Shang, J. GPR120 suppresses adipose tissue lipolysis and synergizes with GPR40 in antidiabetic efficacy. J Lipid Res. 2017, 58, 1561–1578. [Google Scholar] [CrossRef]
- Sun, Q.; Li, J.; Gao, F. New insights into insulin: The anti-inflammatory effect and its clinical relevance. World J Diabetes. 2014, 5, 89–96. [Google Scholar] [CrossRef]
- Chang, Y.W.; Hung, L.C.; Chen, Y.C.; Wang, W.H.; Lin, C.Y.; Tzeng, H.H.; Suen, J.L.; Chen, Y.H. Insulin Reduces Inflammation by Regulating the Activation of the NLRP3 Inflammasome. Front Immunol. 2021, 11, 587229. [Google Scholar] [CrossRef] [PubMed]
- Chen, Q.; Yu, W.; Shi, J.; Shen, J.; Gao, T.; Zhang, J.; Xi, F.; Li, J.; Li, N. Insulin alleviates the inflammatory response and oxidative stress injury in cerebral tissues in septic rats. J Inflamm (Lond). 2014, 11, 18. [Google Scholar] [CrossRef]
- Huang, C.T.; Lue, J.H.; Cheng, T.H.; Tsai, Y.J. Glycemic control with insulin attenuates sepsis-associated encephalopathy by inhibiting glial activation via the suppression of the nuclear factor kappa B and mitogen-activated protein kinase signaling pathways in septic rats. Brain Res. 2020, 1738, 146822. [Google Scholar] [CrossRef]
- Khanna, D.; Khanna, S.; Khanna, P.; Kahar, P.; Patel, B.M. Obesity: A Chronic Low-Grade Inflammation and Its Markers. Cureus. 2022, 14, e22711. [Google Scholar] [CrossRef] [PubMed]
- Matuschik, L.; Riabov, V.; Schmuttermaier, C.; Sevastyanova, T.; Weiss, C.; Klüter, H.; Kzhyshkowska, J. Hyperglycemia Induces Inflammatory Response of Human Macrophages to CD163-Mediated Scavenging of Hemoglobin-Haptoglobin Complexes. Int J Mol Sci. 2022; 23:1385. [CrossRef]
- Moganti, K.; Li, F.; Schmuttermaier, C.; Riemann, S.; Klüter, H.; Gratchev, A.; Harmsen, M.C.; Kzhyshkowska, J. Hyperglycemia induces mixed M1/M2 cytokine profile in primary human monocyte-derived macrophages. Immunobiology. 2017, 222, 952–959. [Google Scholar] [CrossRef] [PubMed]
- Wang, R.; Lan, C.; Benlagha, K.; Camara, N.O.S.; Miller, H.; Kubo, M.; Heegaard, S.; Lee, P.; Yang, L.; Forsman, H.; Li, X.; Zhai, Z.; Liu, C. The interaction of innate immune and adaptive immune system. MedComm (2020). 2024, 5, e714. [Google Scholar] [CrossRef] [PubMed]
- Engin, A.B. Adipocyte-Macrophage Cross-Talk in Obesity. Adv Exp Med Biol. 2017, 960, 327–343. [Google Scholar] [CrossRef] [PubMed]
- Hu, T.; Liu, C.H.; Lei, M.; Zeng, Q.; Li, L.; Tang, H.; Zhang, N. Metabolic regulation of the immune system in health and diseases: mechanisms and interventions. Signal Transduct Target Ther. 2024, 9, 268. [Google Scholar] [CrossRef]
- Ignacio, R.M.; Kim, C.S.; Kim, S.K. Immunological Profiling of Obesity. J Lifestyle Med. 2014, 4, 1–7. [Google Scholar] [CrossRef]
- Li, X.; Ren, Y.; Chang, K.; Wu, W.; Griffiths, H.R.; Lu, S.; Gao, D. Adipose tissue macrophages as potential targets for obesity and metabolic diseases. Front Immunol. 2023, 14, 1153915. [Google Scholar] [CrossRef]
- Rowan, C.R.; McManus, J.; Boland, K.; O'Toole, A. Visceral adiposity and inflammatory bowel disease. Int J Colorectal Dis. 2021, 36, 2305–2319. [Google Scholar] [CrossRef]
- Santillana, N.; Astudillo-Guerrero, C.; D'Espessailles, A.; Cruz, G. White Adipose Tissue Dysfunction: Pathophysiology and Emergent Measurements. Nutrients. 2023, 15, 1722. [Google Scholar] [CrossRef]
- Lee, Y.H.; Park, J.; Min, S.; Kang, O.; Kwon, H.; Oh, S.W. Impact of Visceral Obesity on the Risk of Incident Metabolic Syndrome in Metabolically Healthy Normal Weight and Overweight Groups: A Longitudinal Cohort Study in Korea. Korean J Fam Med. 2020, 41, 229–236. [Google Scholar] [CrossRef]
- Mongraw-Chaffin, M.; Hairston, K.G.; Hanley, A.J.G.; Tooze, J.A.; Norris, J.M.; Palmer, N.D.; Bowden, D.W.; Lorenzo, C.; Chen, Y.I.; Wagenknecht, L.E. Association of Visceral Adipose Tissue and Insulin Resistance with Incident Metabolic Syndrome Independent of Obesity Status: The IRAS Family Study. Obesity (Silver Spring). 2021, 29, 1195–1202. [Google Scholar] [CrossRef] [PubMed]
- Navaneeth, G.C.; Hiremath, R.; Poojary, S.R.; Kini, D.V.; Chittaragi, K.B. Computed tomographic abdominal fat volume estimation - a handy tool to predict the risk of metabolic syndrome. Pol J Radiol. 2023, 88, e379–e388. [Google Scholar] [CrossRef]
- Daryabor, G.; Kabelitz, D.; Kalantar, K. An update on immune dysregulation in obesity-related insulin resistance. Scand J Immunol. 2019, 89, e12747. [Google Scholar] [CrossRef] [PubMed]
- Shang, C.; Yuan, M.; Wang, Y.; Wang, Y.; Bao, W.; Zeng, S.; Zhang, D.; Liu, P.; Sun, L. Association Between Visceral Obesity and Glycemic Control in Patients with Type 2 Diabetes Mellitus: A Retrospective Study. Diabetes Metab Syndr Obes. 2024, 17, 2869–2880. [Google Scholar] [CrossRef]
- Doyle, S.L.; Donohoe, C.L.; Lysaght, J.; Reynolds, J.V. Visceral obesity, metabolic syndrome, insulin resistance and cancer. Proc Nutr Soc. 2012, 71, 181–9. [Google Scholar] [CrossRef] [PubMed]
- Zheng, X.; Wang, Y.; Chen, Y.; Liu, T.; Liu, C.; Lin, S.; Xie, H.; Ma, X.; Wang, Z.; Shi, J.; Zhang, H.; Yang, M.; Liu, X.; Deng, L.; Zhang, Q.; Shi, H. Metabolic obesity phenotypes and the risk of cancer: a prospective study of the Kailuan cohort. Front Endocrinol (Lausanne). 2024, 15, 1333488. [Google Scholar] [CrossRef]
- Rumyantsev, K.A.; Polyakova, V.V.; Sorokina, I.V.; Feoktistova, P.S.; Khatkov, I.E.; Bodunova, N.A.; Zhukova, L.G. The Gut Microbiota Impacts Gastrointestinal Cancers through Obesity, Diabetes, and Chronic Inflammation. Life (Basel). 2024, 14, 1219. [Google Scholar] [CrossRef]
- Kolb, H. Obese visceral fat tissue inflammation: from protective to detrimental? BMC Med. 2022, 20, 494. [Google Scholar] [CrossRef]
- Yu, J.Y.; Choi, W.J.; Lee, H.S.; Lee, J.W. Relationship between inflammatory markers and visceral obesity in obese and overweight Korean adults: An observational study. Medicine (Baltimore). 2019, 98, e14740. [Google Scholar] [CrossRef]
- Ellulu, M.S.; Patimah, I.; Khaza'ai, H.; Rahmat, A.; Abed, Y. Obesity and inflammation: the linking mechanism and the complications. Arch Med Sci. 2017, 13, 851–863. [Google Scholar] [CrossRef]
- Li, H.; Meng, Y.; He, S.; Tan, X.; Zhang, Y.; Zhang, X.; Wang, L.; Zheng, W. Macrophages, Chronic Inflammation, and Insulin Resistance. Cells. 2022, 11, 3001. [Google Scholar] [CrossRef]
- Graßmann, S.; Wirsching, J.; Eichelmann, F.; Aleksandrova, K. Association Between Peripheral Adipokines and Inflammation Markers: A Systematic Review and Meta-Analysis. Obesity (Silver Spring). 2017, 25, 1776–1785. [Google Scholar] [CrossRef] [PubMed]
- Wnuk, A.; Stangret, A.; Wątroba, M.; Płatek, A.E.; Skoda, M.; Cendrowski, K.; Sawicki, W.; Szukiewicz, D. Can adipokine visfatin be a novel marker of pregnancy-related disorders in women with obesity? Obes Rev. 2020, 21, e13022. [Google Scholar] [CrossRef] [PubMed]
- Kirichenko, T.V.; Markina, Y.V.; Bogatyreva, A.I.; Tolstik, T.V.; Varaeva, Y.R.; Starodubova, A.V. The Role of Adipokines in Inflammatory Mechanisms of Obesity. Int J Mol Sci. 2022, 23, 14982. [Google Scholar] [CrossRef] [PubMed]
- Saddi-Rosa, P.; Oliveira, C.S.; Giuffrida, F.M.; Reis, A.F. Visfatin, glucose metabolism and vascular disease: a review of evidence. Diabetol Metab Syndr. 2010, 2, 21. [Google Scholar] [CrossRef]
- Dakroub, A.; ANasser, S.; Younis, N.; Bhagani, H.; Al-Dhaheri, Y.; Pintus, G.; Eid, A.A.; El-Yazbi, A.F.; Eid, A.H. Visfatin: A Possible Role in Cardiovasculo-Metabolic Disorders. Cells. 2020; 9:2444. [CrossRef]
- Abdalla, M.M.I. Role of visfatin in obesity-induced insulin resistance. World J Clin Cases. 2022, 10, 10840–10851. [Google Scholar] [CrossRef]
- McLaughlin, T.; Ackerman, S.E.; Shen, L.; Engleman, E. Role of innate and adaptive immunity in obesity-associated metabolic disease. J Clin Invest. 2017, 127, 5–13. [Google Scholar] [CrossRef]
- Wellen, K.E.; Hotamisligil, G.S. Obesity-induced inflammatory changes in adipose tissue. J Clin Invest. 2003, 112, 1785–8. [Google Scholar] [CrossRef]
- Pitharouli, M.C.; Hagenaars, S.P.; Glanville, K.P.; Coleman, J.R.I.; Hotopf, M.; Lewis, C.M.; Pariante, C.M. Elevated C-Reactive Protein in Patients With Depression, Independent of Genetic, Health, and Psychosocial Factors: Results From the UK Biobank. Am J Psychiatry. 2021, 178, 522–529. [Google Scholar] [CrossRef] [PubMed]
- Parkitny, L.; McAuley, J.H.; Di Pietro, F.; Stanton, T.R.; O'Connell, N.E.; Marinus, J.; van Hilten, J.J.; Moseley, G.L. Inflammation in complex regional pain syndrome: a systematic review and meta-analysis. Neurology. 2013, 80, 106–17. [Google Scholar] [CrossRef]
- Gutierrez-Rodelo, C.; Arellano-Plancarte, A.; Hernandez-Aranda, J.; Landa-Galvan, H.V.; Parra-Mercado, G.K.; Moreno-Licona, N.J.; Hernandez-Gonzalez, K.D.; Catt, K.J.; Villalobos-Molina, R.; Olivares-Reyes, J.A. Angiotensin II Inhibits Insulin Receptor Signaling in Adipose Cells. Int J Mol Sci. 2022, 23, 6048. [Google Scholar] [CrossRef]
- Kim, J.; Lee, S.K.; Jang, Y.J.; Park, H.S.; Kim, J.H.; Hong, J.P.; Lee, Y.J.; Heo, Y.S. Enhanced ANGPTL2 expression in adipose tissues and its association with insulin resistance in obese women. Sci Rep. 2018, 8, 13976. [Google Scholar] [CrossRef] [PubMed]
- Corbin, J.A.; Bhaskar, V.; Goldfine, I.D.; Issafras, H.; Bedinger, D.H.; Lau, A.; Michelson, K.; Gross, L.M.; Maddux, B.A.; Kuan, H.F.; Tran, C.; Lao, L.; Handa, M.; Watson, S.R.; Narasimha, A.J.; Zhu, S.; Levy, R.; Webster, L.; Wijesuriya, S.D.; Liu, N.; Wu, X.; Chemla-Vogel, D.; Lee, S.R.; Wong, S.; Wilcock, D.; Rubin, P.; White, M.L. Inhibition of insulin receptor function by a human, allosteric monoclonal antibody: a potential new approach for the treatment of hyperinsulinemic hypoglycemia. MAbs. 2014, 6, 262–72. [Google Scholar] [CrossRef] [PubMed]
- Willard, D.L.; Stevenson, M.; Steenkamp, D. Type B insulin resistance syndrome. Curr Opin Endocrinol Diabetes Obes. 2016, 23, 318–23. [Google Scholar] [CrossRef] [PubMed]
- Boucher, J.; Kleinridders, A.; Kahn, C.R. Insulin receptor signaling in normal and insulin-resistant states. Cold Spring Harb Perspect Biol. 2014, 6, a009191. [Google Scholar] [CrossRef]
- Pei, J.; Wang, B.; Wang, D. Current Studies on Molecular Mechanisms of Insulin Resistance. J Diabetes Res. 2022, 2022, 1863429. [Google Scholar] [CrossRef]
- Lorenzo, M.; Fernández-Veledo, S.; Vila-Bedmar, R.; Garcia-Guerra, L.; De Alvaro, C.; Nieto-Vazquez, I. Insulin resistance induced by tumor necrosis factor-alpha in myocytes and brown adipocytes. J Anim Sci. 2008;86(14 Suppl):E94-104. [CrossRef]
- Singh, A.; Kukreti, R.; Saso, L.; Kukreti, S. Mechanistic Insight into Oxidative Stress-Triggered Signaling Pathways and Type 2 Diabetes. Molecules. 2022, 27, 950. [Google Scholar] [CrossRef]
- Freeman, A.M.; Pennings, N. StatPearls [Internet] StatPearls Publishing; Treasure Island, FL, USA: 2023. Insulin Resistance.
- Petersen, M.C.; Shulman, G.I. Mechanisms of Insulin Action and Insulin Resistance. Physiol Rev. 2018, 98, 2133–2223. [Google Scholar] [CrossRef]
- Zhao, X.; An, X.; Yang, C.; Sun, W.; Ji, H.; Lian, F. The crucial role and mechanism of insulin resistance in metabolic disease. Front Endocrinol (Lausanne). 2023, 14, 1149239. [Google Scholar] [CrossRef]
- Auguet, T.; Guiu-Jurado, E.; Berlanga, A.; Terra, X.; Martinez, S.; Porras, J.A.; Ceausu, A.; Sabench, F.; Hernandez, M.; Aguilar, C.; Sirvent, J.J.; Del Castillo, D.; Richart, C. Downregulation of lipogenesis and fatty acid oxidation in the subcutaneous adipose tissue of morbidly obese women. Obesity (Silver Spring). 2014, 22, 2032–8. [Google Scholar] [CrossRef]
- Zhou, W.; Ramachandran, D.; Mansouri, A.; Dailey, M.J. Glucose stimulates intestinal epithelial crypt proliferation by modulating cellular energy metabolism. J Cell Physiol. 2018, 233, 3465–3475. [Google Scholar] [CrossRef] [PubMed]
- Saltiel, A.R.; Olefsky, J.M. Inflammatory mechanisms linking obesity and metabolic disease. J Clin Invest. 2017, 127, 1–4. [Google Scholar] [CrossRef] [PubMed]
- Duca, F.A.; Swartz, T.D.; Sakar, Y.; Covasa, M. Decreased intestinal nutrient response in diet-induced obese rats: role of gut peptides and nutrient receptors. Int J Obes (Lond). 2013, 37, 375–81. [Google Scholar] [CrossRef]
- Wang, Y.; Xie, T.; Zhang, D.; Leung, P.S. GPR120 protects lipotoxicity-induced pancreatic β-cell dysfunction through regulation of PDX1 expression and inhibition of islet inflammation. Clin Sci (Lond). 2019, 133, 101–116. [Google Scholar] [CrossRef]
- Miyabe, M.; Gin, A.; Onozawa, E.; Daimon, M.; Yamada, H.; Oda, H.; Mori, A.; Momota, Y.; Azakami, D.; Yamamoto, I.; Mochizuki, M.; Sako, T.; Tamura, K.; Ishioka, K. Genetic variants of the unsaturated fatty acid receptor GPR120 relating to obesity in dogs. J Vet Med Sci. 2015; 77:1201-6. [CrossRef]
- Luo, L.; Liu, M. Adipose tissue in control of metabolism. J Endocrinol. 2016, 231, R77–R99. [Google Scholar] [CrossRef] [PubMed]
- Scheja, L.; Heeren, J. The endocrine function of adipose tissues in health and cardiometabolic disease. Nat Rev Endocrinol. 2019, 15, 507–524. [Google Scholar] [CrossRef]
- An, S.M.; Cho, S.H.; Yoon, J.C. Adipose Tissue and Metabolic Health. Diabetes Metab J. 2023, 47, 595–611. [Google Scholar] [CrossRef]
- Teixeira, L.; Whitmire, J.K.; Bourgeois, C. Editorial: The role of adipose tissue and resident immune cells in infections. Front Immunol. 2024, 15, 1360262. [Google Scholar] [CrossRef]
- Rosenwald, M.; Wolfrum, C. The origin and definition of brite versus white and classical brown adipocytes. Adipocyte. 2014, 3, 4–9. [Google Scholar] [CrossRef]
- Chen, Y.; Pan, R.; Pfeifer, A. Fat tissues, the brite and the dark sides. Pflugers Arch. 2016; 468(11-12):1803-1807. [CrossRef]
- Ikeda, K.; Yamada, T. UCP1 Dependent and Independent Thermogenesis in Brown and Beige Adipocytes. Front Endocrinol (Lausanne). 2020, 11, 498. [Google Scholar] [CrossRef]
- Kazak, L.; Chouchani, E.T.; Jedrychowski, M.P.; Erickson, B.K.; Shinoda, K.; Cohen, P.; Vetrivelan, R.; Lu, G.Z.; Laznik-Bogoslavski, D.; Hasenfuss, S.C.; Kajimura, S.; Gygi, S.P.; Spiegelman, B.M. A creatine-driven substrate cycle enhances energy expenditure and thermogenesis in beige fat. Cell. 2015, 163, 643–55. [Google Scholar] [CrossRef]
- Bertholet, A.M.; Kazak, L.; Chouchani, E.T.; Bogaczyńska, M.G.; Paranjpe, I.; Wainwright, G.L.; Bétourné, A.; Kajimura, S.; Spiegelman, B.M.; Kirichok, Y. Mitochondrial Patch Clamp of Beige Adipocytes Reveals UCP1-Positive and UCP1-Negative Cells Both Exhibiting Futile Creatine Cycling. Cell Metab. 2017, 25, 811–822.e4. [Google Scholar] [CrossRef] [PubMed]
- van Marken Lichtenbelt, W.D.; Vanhommerig, J.W.; Smulders, N.M.; Drossaerts, J.M.; Kemerink, G.J.; Bouvy, N.D.; Schrauwen, P.; Teule, G.J. Cold-activated brown adipose tissue in healthy men. N Engl J Med. 2009, 360, 1500–8. [Google Scholar] [CrossRef] [PubMed]
- Zhang, Z.; Yang, D.; Xiang, J.; Zhou, J.; Cao, H.; Che, Q.; Bai, Y.; Guo, J.; Su, Z. Non-shivering Thermogenesis Signalling Regulation and Potential Therapeutic Applications of Brown Adipose Tissue. Int J Biol Sci. 2021, 17, 2853–2870. [Google Scholar] [CrossRef] [PubMed]
- Sanchez-Delgado, G.; Martinez-Tellez, B.; Acosta, F.M.; Virtue, S.; Vidal-Puig, A.; Gil, A.; Llamas-Elvira, J.M.; Ruiz, J.R. Brown Adipose Tissue Volume and Fat Content Are Positively Associated With Whole-Body Adiposity in Young Men-Not in Women. Diabetes. 2021, 70, 1473–1485. [Google Scholar] [CrossRef]
- Chiadak, J.D.; Arsenijevic, T.; Verstrepen, K.; Gregoire, F.; Bolaky, N.; Delforge, V.; Flamand, V.; Perret, J.; Delporte, C. Forskolin Inhibits Lipopolysaccharide-Induced Modulation of MCP-1 and GPR120 in 3T3-L1 Adipocytes through an Inhibition of NFκB. Mediators Inflamm. 2016; 2016:1431789. [CrossRef]
- Song, T.; Yang, Y.; Zhou, Y.; Wei, H.; Peng, J. GPR120: a critical role in adipogenesis, inflammation, and energy metabolism in adipose tissue. Cell Mol Life Sci. 2017, 74, 2723–2733. [Google Scholar] [CrossRef]
- Otto, T.C.; Lane, M.D. Adipose development: from stem cell to adipocyte. Crit Rev Biochem Mol Biol. 2005, 40, 229–42. [Google Scholar] [CrossRef]
- Ichimura, A.; Hirasawa, A.; Poulain-Godefroy, O.; Bonnefond, A.; Hara, T.; Yengo, L.; Kimura, I.; Leloire, A.; Liu, N.; Iida, K.; Choquet, H.; Besnard, P.; Lecoeur, C.; Vivequin, S.; Ayukawa, K.; Takeuchi, M.; Ozawa, K.; Tauber, M.; Maffeis, C.; Morandi, A.; Buzzetti, R.; Elliott, P.; Pouta, A.; Jarvelin, M.R.; Körner, A.; Kiess, W.; Pigeyre, M.; Caiazzo, R.; Van Hul, W.; Van Gaal, L.; Horber, F.; Balkau, B.; Lévy-Marchal, C.; Rouskas, K.; Kouvatsi, A.; Hebebrand, J.; Hinney, A.; Scherag, A.; Pattou, F.; Meyre, D.; Koshimizu, T.A.; Wolowczuk, I.; Tsujimoto, G.; Froguel, P. Dysfunction of lipid sensor GPR120 leads to obesity in both mouse and human. Nature. 2012, 483, 350–4. [Google Scholar] [CrossRef]
- Ichimura, A.; Hara, T.; Hirasawa, A. Regulation of Energy Homeostasis via GPR120. Front Endocrinol (Lausanne). 2014, 5, 111. [Google Scholar] [CrossRef]
- Song, T.; Zhou, Y.; Peng, J.; Tao, Y.X.; Yang, Y.; Xu, T.; Peng, J.; Ren, J.; Xiang, Q.; Wei, H. GPR120 promotes adipogenesis through intracellular calcium and extracellular signal-regulated kinase 1/2 signal pathway. Mol Cell Endocrinol. 2016, 434, 1–13. [Google Scholar] [CrossRef]
- Christian, M. Elucidation of the roles of brown and brite fat genes: GPR120 is a modulator of brown adipose tissue function. Exp Physiol. 2020, 105, 1201–1205. [Google Scholar] [CrossRef]
- Quesada-López, T.; Cereijo, R.; Turatsinze, J.V.; Planavila, A.; Cairó, M.; Gavaldà-Navarro, A.; Peyrou, M.; Moure, R.; Iglesias, R.; Giralt, M.; Eizirik, D.L.; Villarroya, F. The lipid sensor GPR120 promotes brown fat activation and FGF21 release from adipocytes. Nat Commun. 2016, 7, 13479. [Google Scholar] [CrossRef] [PubMed]
- Yamada, H.; Umemoto, T.; Kakei, M.; Momomura, S.I.; Kawakami, M.; Ishikawa, S.E.; Hara, K. Eicosapentaenoic acid shows anti-inflammatory effect via GPR120 in 3T3-L1 adipocytes and attenuates adipose tissue inflammation in diet-induced obese mice. Nutr Metab (Lond). 2017; 14:33. [CrossRef]
- Murano, I.; Severi, I.; Venema, W.; Cecchini, M.P.; Kershaw, E.E.; Barbatelli, G.; Haemmerle, G.; Zechner, R.; Cinti, S. Brown adipose tissue whitening leads to brown adipocyte death and adipose tissue inflammation. J Lipid Res. 2018, 59, 784–794. [Google Scholar] [CrossRef]
- Pærregaard, S.I.; Agerholm, M.; Serup, A.K.; Ma, T.; Kiens, B.; Madsen, L.; Kristiansen, K.; Jensen, B.A. FFAR4 (GPR120) Signaling Is Not Required for Anti-Inflammatory and Insulin-Sensitizing Effects of Omega-3 Fatty Acids. Mediators Inflamm. 2016, 2016, 1536047. [Google Scholar] [CrossRef]
- Sveiven, S.N.; Anesko, K.; Morgan, J.; Nair, M.G.; Nordgren, T.M. Lipid-Sensing Receptor FFAR4 Modulates Pulmonary Epithelial Homeostasis following Immunogenic Exposures Independently of the FFAR4 Ligand Docosahexaenoic Acid (DHA). Int J Mol Sci. 2023, 24 7072. [CrossRef]
- Hirasawa, A.; Tsumaya, K.; Awaji, T.; Katsuma, S.; Adachi, T.; Yamada, M.; Sugimoto, Y.; Miyazaki, S.; Tsujimoto, G. Free fatty acids regulate gut incretin glucagon-like peptide-1 secretion through GPR120. Nat Med. 2005, 11, 90–4. [Google Scholar] [CrossRef] [PubMed]
- Katsuma, S.; Hatae, N.; Yano, T.; Ruike, Y.; Kimura, M.; Hirasawa, A.; Tsujimoto, G. Free fatty acids inhibit serum deprivation-induced apoptosis through GPR120 in a murine enteroendocrine cell line STC-1. J Biol Chem. 2005, 280, 19507–15. [Google Scholar] [CrossRef]
- Cawthon, C.R.; de La Serre, C.B. The critical role of CCK in the regulation of food intake and diet-induced obesity. Peptides. 2021, 138, 170492. [Google Scholar] [CrossRef]
- Tanaka, T.; Katsuma, S.; Adachi, T.; Koshimizu, T.A.; Hirasawa, A.; Tsujimoto, G. Free fatty acids induce cholecystokinin secretion through GPR120. Naunyn Schmiedebergs Arch Pharmacol. 2008;377(4-6):523-7. [CrossRef]
- Popoviciu, M.S.; Păduraru, L.; Yahya, G.; Metwally, K.; Cavalu, S. Emerging Role of GLP-1 Agonists in Obesity: A Comprehensive Review of Randomised Controlled Trials. Int J Mol Sci. 2023, 24, 10449. [Google Scholar] [CrossRef]
- McKillop, A.M.; Miskelly, M.G.; Moran, B.M.; Flatt, P.R. Incretins play an important role in FFA4/GPR120 regulation of glucose metabolism by GW-9508. Life Sci. 2023, 318, 121475. [Google Scholar] [CrossRef]
- Loona, D.P.S.; Das, B.; Kaur, R.; Kumar, R.; Yadav, A.K. Free Fatty Acid Receptors (FFARs): Emerging Therapeutic Targets for the Management of Diabetes Mellitus. Curr Med Chem. 2023, 30, 3404–3440. [Google Scholar] [CrossRef]
- Patil, M.; Casari, I.; Warne, L.N.; Falasca, M. G protein-coupled receptors driven intestinal glucagon-like peptide-1 reprogramming for obesity: Hope or hype? Biomed Pharmacother. 2024, 172, 116245. [Google Scholar] [CrossRef]
- Sankoda, A.; Harada, N.; Iwasaki, K.; Yamane, S.; Murata, Y.; Shibue, K.; Thewjitcharoen, Y.; Suzuki, K.; Harada, T.; Kanemaru, Y.; Shimazu-Kuwahara, S.; Hirasawa, A.; Inagaki, N. Long-Chain Free Fatty Acid Receptor GPR120 Mediates Oil-Induced GIP Secretion Through CCK in Male Mice. Endocrinology. 2017, 158, 1172–1180. [Google Scholar] [CrossRef] [PubMed]
- Sankoda, A.; Harada, N.; Kato, T.; Ikeguchi, E.; Iwasaki, K.; Yamane, S.; Murata, Y.; Hirasawa, A.; Inagaki, N. Free fatty acid receptors, G protein-coupled receptor 120 and G protein-coupled receptor 40, are essential for oil-induced gastric inhibitory polypeptide secretion. J Diabetes Investig. 2019, 10, 1430–1437. [Google Scholar] [CrossRef]
- Iwasaki, K.; Harada, N.; Sasaki, K.; Yamane, S.; Iida, K.; Suzuki, K.; Hamasaki, A.; Nasteska, D.; Shibue, K.; Joo, E.; Harada, T.; Hashimoto, T.; Asakawa, Y.; Hirasawa, A.; Inagaki, N. Free fatty acid receptor GPR120 is highly expressed in enteroendocrine K cells of the upper small intestine and has a critical role in GIP secretion after fat ingestion. Endocrinology. 2015, 156, 837–46. [Google Scholar] [CrossRef] [PubMed]
- Yamane, S.; Harada, N.; Inagaki, N. Mechanisms of fat-induced gastric inhibitory polypeptide/glucose-dependent insulinotropic polypeptide secretion from K cells. J Diabetes Investig. 2016;7 Suppl 1(Suppl 1):20-6. [CrossRef]
- Yasuda, T.; Harada, N.; Hatoko, T.; Ichimura, A.; Ikeguchi-Ogura, E.; Murata, Y.; Wada, N.; Kiyobayashi, S.; Yamane, S.; Hirasawa, A.; Inagaki, N. Inhibition of GPR120 signaling in intestine ameliorates insulin resistance and fatty liver under high-fat diet feeding. Am J Physiol Endocrinol Metab. 2023, 324, E449–E460. [Google Scholar] [CrossRef] [PubMed]
- Nauck, M.A.; Meier, J.J. Incretin hormones: Their role in health and disease. Diabetes Obes Metab. 2018;20 Suppl 1:5-21. [CrossRef]
- Codoñer-Alejos, A.; Carrasco-Luna, J.; Carrasco-García, Á.; Codoñer-Franch, P. Reduced Free Fatty Acid Receptor 4 Gene Expression is Associated With Extreme Obesity and Insulin Resistance in Children. J Pediatr Gastroenterol Nutr. 2022, 74, 535–540. [Google Scholar] [CrossRef]
- Stone, V.M.; Dhayal, S.; Brocklehurst, K.J.; Lenaghan, C.; Sörhede Winzell, M.; Hammar, M.; Xu, X.; Smith, D.M.; Morgan, N.G. GPR120 (FFAR4) is preferentially expressed in pancreatic delta cells and regulates somatostatin secretion from murine islets of Langerhans. Diabetologia. 2014, 57, 1182–91. [Google Scholar] [CrossRef]
- Croze, M.L.; Flisher, M.F.; Guillaume, A.; Tremblay, C.; Noguchi, G.M.; Granziera, S.; Vivot, K.; Castillo, V.C.; Campbell, S.A.; Ghislain, J.; Huising, M.O.; Poitout, V. Free fatty acid receptor 4 inhibitory signaling in delta cells regulates islet hormone secretion in mice. Mol Metab. 2021; 45:101166. [CrossRef]
- Rorsman, P.; Huising, M.O. The somatostatin-secreting pancreatic δ-cell in health and disease. Nat Rev Endocrinol. 2018, 14, 404–414. [Google Scholar] [CrossRef]
- Moran, B.M.; Abdel-Wahab, Y.H.; Flatt, P.R.; McKillop, A.M. Evaluation of the insulin-releasing and glucose-lowering effects of GPR120 activation in pancreatic β-cells. Diabetes Obes Metab. 2014, 16, 1128–39. [Google Scholar] [CrossRef]
- Vergari, E.; Denwood, G.; Salehi, A.; Zhang, Q.; Adam, J.; Alrifaiy, A.; Wernstedt Asterholm, I.; Benrick, A.; Chibalina, M.V.; Eliasson, L.; Guida, C.; Hill, T.G.; Hamilton, A.; Ramracheya, R.; Reimann, F.; Rorsman, N.J.G.; Spilliotis, I.; Tarasov, A.I.; Walker, J.N.; Rorsman, P.; Briant, L.J.B. Somatostatin secretion by Na+-dependent Ca2+-induced Ca2+ release in pancreatic delta-cells. Nat Metab. 2020, 2, 32–40. [Google Scholar] [CrossRef]
- Denwood, G.; Tarasov, A.; Salehi, A.; Vergari, E.; Ramracheya, R.; Takahashi, H.; Nikolaev, V.O.; Seino, S.; Gribble, F.; Reimann, F.; Rorsman, P.; Zhang, Q. Glucose stimulates somatostatin secretion in pancreatic δ-cells by cAMP-dependent intracellular Ca2+ release. J Gen Physiol. 2019, 151, 1094–1115. [Google Scholar] [CrossRef] [PubMed]
- Greenhill, C. Urocortin 3 function in glucose metabolism. Nat Rev Endocrinol. 2022; 18:333. [CrossRef]
- Wang, K.Y.; Gao, M.X.; Qi, H.B.; An, W.T.; Lin, J.Y.; Ning, S.L.; Yang, F.; Xiao, P.; Cheng, J.; Pan, W.; Cheng, Q.X.; Wang, J.; Fang, L.; Sun, J.P.; Yu, X. Differential contributions of G protein- or arrestin subtype-mediated signalling underlie urocortin 3-induced somatostatin secretion in pancreatic δ cells. Br J Pharmacol. 2024, 181, 2600–2621. [Google Scholar] [CrossRef]
- Du, Y.Q.; Sha, X.Y.; Cheng, J.; Wang, J.; Lin, J.Y.; An, W.T.; Pan, W.; Zhang, L.J.; Tao, X.N.; Xu, Y.F.; Jia, Y.L.; Yang, Z.; Xiao, P.; Liu, M.; Sun, J.P.; Yu, X. Endogenous Lipid-GPR120 Signaling Modulates Pancreatic Islet Homeostasis to Different Extents. Diabetes. 2022, 71, 1454–1471. [Google Scholar] [CrossRef] [PubMed]
- Hong, S.W.; Lee, J.; Moon, S.J.; Kwon, H.; Park, S.E.; Rhee, E.J.; Lee, W.Y. Docosahexanoic Acid Attenuates Palmitate-Induced Apoptosis by Autophagy Upregulation via GPR120/mTOR Axis in Insulin-Secreting Cells. Endocrinol Metab (Seoul). 2024, 39, 353–363. [Google Scholar] [CrossRef]
- Zhang, D.; So, W.Y.; Wang, Y.; Wu, S.Y.; Cheng, Q.; Leung, P.S. Insulinotropic effects of GPR120 agonists are altered in obese diabetic and obese non-diabetic states. Clin Sci (Lond). 2017, 131, 247–260. [Google Scholar] [CrossRef]
- Owolabi, A.I.; Corbett, R.C.; Flatt, P.R.; McKillop, A.M. Positive interplay between FFAR4/GPR120, DPP-IV inhibition and GLP-1 in beta cell proliferation and glucose homeostasis in obese high fat fed mice. Peptides. 2024, 177, 171218. [Google Scholar] [CrossRef]
- Ichimura, A.; Hasegawa, S.; Kasubuchi, M.; Kimura, I. Free fatty acid receptors as therapeutic targets for the treatment of diabetes. Front Pharmacol. 2014, 5, 236. [Google Scholar] [CrossRef]
- Pedroni, L.; Perugino, F.; Magnaghi, F.; Dall'Asta, C.; Galaverna, G.; Dellafiora, L. Free fatty acid receptors beyond fatty acids: A computational journey to explore peptides as possible binders of GPR120. Curr Res Food Sci. 2024, 8, 100710. [Google Scholar] [CrossRef] [PubMed]
- Suzuki, T.; Igari, S.; Hirasawa, A.; Hata, M.; Ishiguro, M.; Fujieda, H.; Itoh, Y.; Hirano, T.; Nakagawa, H.; Ogura, M.; Makishima, M.; Tsujimoto, G.; Miyata, N. Identification of G protein-coupled receptor 120-selective agonists derived from PPARgamma agonists. J Med Chem. 2008, 51, 7640–4. [Google Scholar] [CrossRef]
- Yan, Y.; Jiang, W.; Spinetti, T.; Tardivel, A.; Castillo, R.; Bourquin, C.; Guarda, G.; Tian, Z.; Tschopp, J.; Zhou, R. Omega-3 fatty acids prevent inflammation and metabolic disorder through inhibition of NLRP3 inflammasome activation. Immunity. 2013, 38, 1154–63. [Google Scholar] [CrossRef]
- Li, X.; Yu, Y.; Funk, C.D. Cyclooxygenase-2 induction in macrophages is modulated by docosahexaenoic acid via interactions with free fatty acid receptor 4 (FFA4). FASEB J. 2013; 27:4987-97. [CrossRef]
- Zhang, D.; Leung, P.S. Potential roles of GPR120 and its agonists in the management of diabetes. Drug Des Devel Ther. 2014, 8, 1013–27. [Google Scholar] [CrossRef]
- Pal, A.; Curtin, J.F.; Kinsella, G.K. In silico and in vitro screening for potential anticancer candidates targeting GPR120. Bioorg Med Chem Lett. 2021, 31, 127672. [Google Scholar] [CrossRef] [PubMed]
- Rubbino, F.; Garlatti, V.; Garzarelli, V.; Massimino, L.; Spanò, S.; Iadarola, P.; Cagnone, M.; Giera, M.; Heijink, M.; Guglielmetti, S.; Arena, V.; Malesci, A.; Laghi, L.; Danese, S.; Vetrano, S. GPR120 prevents colorectal adenocarcinoma progression by sustaining the mucosal barrier integrity. Sci Rep. 2022, 12, 381. [Google Scholar] [CrossRef]
- He, Q.; Zhu, S.; Lin, M.; Yang, Q.; Wei, L.; Zhang, J.; Jiang, X.; Zhu, D.; Lu, X.; Chen, Y.Q. Increased GPR120 level is associated with gestational diabetes mellitus. Biochem Biophys Res Commun. 2019, 512, 196–201. [Google Scholar] [CrossRef] [PubMed]
- Pompili, S.; Cappariello, A.; Vetuschi, A.; Sferra, R. G-Protein-Coupled Receptor 120 Agonist Mitigates Steatotic and Fibrotic Features Triggered in Obese Mice by the Administration of a High-Fat and High-Carbohydrate Diet. ACS Omega. 2024, 9, 31899–31909. [Google Scholar] [CrossRef]
- Milligan, G.; Alvarez-Curto, E.; Hudson, B.D.; Prihandoko, R.; Tobin, A.B. FFA4/GPR120: Pharmacology and Therapeutic Opportunities. Trends Pharmacol Sci. 2017, 38, 809–821. [Google Scholar] [CrossRef] [PubMed]
- Abedi, E.; Sahari, M.A. Long-chain polyunsaturated fatty acid sources and evaluation of their nutritional and functional properties. Food Sci Nutr. 2014, 2, 443–63. [Google Scholar] [CrossRef]
- Murff, H.J.; Edwards, T.L. Endogenous Production of Long-Chain Polyunsaturated Fatty Acids and Metabolic Disease Risk. Curr Cardiovasc Risk Rep. 2014, 8, 418. [Google Scholar] [CrossRef]
- Rodriguez-Pacheco, F.; Garcia-Serrano, S.; Garcia-Escobar, E.; Gutierrez-Repiso, C.; Garcia-Arnes, J.; Valdes, S.; Gonzalo, M.; Soriguer, F.; Moreno-Ruiz, F.J.; Rodriguez-Cañete, A.; Gallego-Perales, J.L.; Martinez-Ferriz, A.; Rojo-Martínez, G.; Garcia-Fuentes, E. Effects of obesity/fatty acids on the expression of GPR120. Mol Nutr Food Res. 2014, 58, 1852–60. [Google Scholar] [CrossRef]
- Holliday, N.D.; Watson, S.J.; Brown, A.J. Drug discovery opportunities and challenges at g protein coupled receptors for long chain free Fatty acids. Front Endocrinol (Lausanne). 2012, 2, 112. [Google Scholar] [CrossRef]
- Hansen, S.V.; Ulven, T. Pharmacological Tool Compounds for the Free Fatty Acid Receptor 4 (FFA4/GPR120). Handb Exp Pharmacol. 2017, 236, 33–56. [Google Scholar] [CrossRef]
- Serhan, C.N.; Chiang, N.; Dalli, J. New pro-resolving n-3 mediators bridge resolution of infectious inflammation to tissue regeneration. Mol Aspects Med. 2018, 64, 1–17. [Google Scholar] [CrossRef] [PubMed]
- Yore, M.M.; Syed, I.; Moraes-Vieira, P.M.; Zhang, T.; Herman, M.A.; Homan, E.A.; Patel, R.T.; Lee, J.; Chen, S.; Peroni, O.D.; Dhaneshwar, A.S.; Hammarstedt, A.; Smith, U.; McGraw, T.E.; Saghatelian, A.; Kahn, B.B. Discovery of a class of endogenous mammalian lipids with anti-diabetic and anti-inflammatory effects. Cell. 2014, 159, 318–32. [Google Scholar] [CrossRef] [PubMed]
- Wang, Y.M.; Liu, H.X.; Fang, N.Y. 9-PAHSA promotes browning of white fat via activating G-protein-coupled receptor 120 and inhibiting lipopolysaccharide / NF-kappa B pathway. Biochem Biophys Res Commun. 2018, 506, 153–160. [Google Scholar] [CrossRef]
- Hara, T.; Hirasawa, A.; Sun, Q.; Sadakane, K.; Itsubo, C.; Iga, T.; Adachi, T.; Koshimizu, T.A.; Hashimoto, T.; Asakawa, Y.; Tsujimoto, G. Novel selective ligands for free fatty acid receptors GPR120 and GPR40. Naunyn Schmiedebergs Arch Pharmacol. 2009, 380, 247–55. [Google Scholar] [CrossRef] [PubMed]
- Sun, Q.; Hirasawa, A.; Hara, T.; Kimura, I.; Adachi, T.; Awaji, T.; Ishiguro, M.; Suzuki, T.; Miyata, N.; Tsujimoto, G. Structure-activity relationships of GPR120 agonists based on a docking simulation. Mol Pharmacol. 2010, 78, 804–10. [Google Scholar] [CrossRef]
- Hirasawa, A.; Hara, T.; Katsuma, S.; Adachi, T.; Tsujimoto, G. Free fatty acid receptors and drug discovery. Biol Pharm Bull. 2008, 31, 1847–51. [Google Scholar] [CrossRef]
- Zhao, Y.; Zhang, H.; Yan, A.; Zhu, J.; Liu, K.; Chen, D.; Xie, R.; Xu, X.; Su, X. Grifolic acid induces mitochondrial membrane potential loss and cell death of RAW264. 7 macrophages. Mol Med Rep. 2018, 17, 3281–3287. [Google Scholar] [CrossRef]
- Bouyahya, A.; El Allam, A.; Zeouk, I.; Taha, D.; Zengin, G.; Goh, B.H.; Catauro, M.; Montesano, D.; El Omari, N. Pharmacological Effects of Grifolin: Focusing on Anticancer Mechanisms. Molecules. 2022, 27, 284. [Google Scholar] [CrossRef]
- Wilson, C.H.; Kumar, S. Caspases in metabolic disease and their therapeutic potential. Cell Death Differ. 2018, 25, 1010–1024. [Google Scholar] [CrossRef]
- Bock, F.J.; Riley, J.S. When cell death goes wrong: inflammatory outcomes of failed apoptosis and mitotic cell death. Cell Death Differ. 2023, 30, 293–303. [Google Scholar] [CrossRef]
- Konda, V.R.; Desai, A.; Darland, G.; Grayson, N.; Bland, J.S. KDT501, a derivative from hops, normalizes glucose metabolism and body weight in rodent models of diabetes. PLoS One. 2014, 9, e87848. [Google Scholar] [CrossRef] [PubMed]
- Kern, P.A.; Finlin, B.S.; Ross, D.; Boyechko, T.; Zhu, B.; Grayson, N.; Sims, R.; Bland, J.S. Effects of KDT501 on Metabolic Parameters in Insulin-Resistant Prediabetic Humans. J Endocr Soc. 2017, 1, 650–659. [Google Scholar] [CrossRef]
- Finlin, B.S.; Zhu, B.; Kok, B.P.; Godio, C.; Westgate, P.M.; Grayson, N.; Sims, R.; Bland, J.S.; Saez, E.; Kern, P.A. The Influence of a KDT501, a Novel Isohumulone, on Adipocyte Function in Humans. Front Endocrinol (Lausanne). 2017, 8, 255. [Google Scholar] [CrossRef]
- Nagasawa, T.; Ishimaru, K.; Higashiyama, S.; Hama, Y.; Mitsutake, S. Teadenol A in microbial fermented tea acts as a novel ligand on GPR120 to increase GLP-1 secretion. Food Funct. 2020, 11, 10534–10541. [Google Scholar] [CrossRef] [PubMed]
- Wilches, I.; Jiménez-Castillo, P.; Cuzco, N.; Clos, M.V.; Jiménez-Altayó, F.; Peñaherrera, E.; Jerves-Andrade, L.; Tobar, V.; Vander Heyden, Y.; Leon-Tamariz, F.; Vila, E. Anti-inflammatory and sedative activities of Peperomia galioides: in vivo studies in mice. Nat Prod Res. 2021, 35, 1657–1661. [Google Scholar] [CrossRef] [PubMed]
- Ye, C.; Jin, M.; Li, R.; Sun, J.; Wang, R.; Wang, J.; Li, S.; Zhou, W.; Li, G. Phytochemical and chemotaxonomic study on the leaves of Rhododendron Dauricum, L. Biochem. Syst. Ecol. 2020, 90, 104038. [Google Scholar] [CrossRef]
- Wang, Y.; Alkhalidy, H.; Liu, D. The Emerging Role of Polyphenols in the Management of Type 2 Diabetes. Molecules. 2021, 26, 703. [Google Scholar] [CrossRef]
- Nukata, M.; Hashimoto, T.; Yamamoto, I.; Iwasaki, N.; Tanaka, M.; Asakawa, Y. Neogrifolin derivatives possessing anti-oxidative activity from the mushroom Albatrellus ovinus. Phytochemistry. 2002, 59, 731–7. [Google Scholar] [CrossRef]
- Grabovyi, G.A.; Mohr, J.T. Total Synthesis of Grifolin, Grifolic Acid, LL-Z1272α, LL-Z1272β, and Ilicicolinic Acid A. Org Lett. 2016, 18, 5010–5013. [Google Scholar] [CrossRef]
- Elsayed, E.A.; El Enshasy, H.; Wadaan, M.A.; Aziz, R. Mushrooms: a potential natural source of anti-inflammatory compounds for medical applications. Mediators Inflamm. 2014, 2014, 805841. [Google Scholar] [CrossRef] [PubMed]
- Muszyńska, B.; Grzywacz-Kisielewska, A.; Kała, K.; Gdula-Argasińska, J. Anti-inflammatory properties of edible mushrooms: A review. Food Chem. 2018, 243, 373–381. [Google Scholar] [CrossRef] [PubMed]
- Janssen, S.; Laermans, J.; Iwakura, H.; Tack, J.; Depoortere, I. Sensing of fatty acids for octanoylation of ghrelin involves a gustatory G-protein. PLoS One. 2012, 7, e40168. [Google Scholar] [CrossRef] [PubMed]
- 270. Bukhari SNA. An insight into the multifunctional role of ghrelin and structure activity relationship studies of ghrelin receptor ligands with clinical trials. Eur J Med Chem. 2022; 235:114308. [CrossRef]
- Usui, A.; Nakamura, A.; Era, M.; Matsuo, Y.; Tanaka, T.; Ishimaru, K. A New Flavonoid from Camellia sinensis Fermented Tea. Nat Prod Commun. 2016, 11, 1281–1282. [Google Scholar] [CrossRef]
- Wulandari, R.A.; Amano, M.; Yanagita, T.; Tanaka, T.; Kouno, I.; Kawamura, D.; Ishimaru, K. New phenolic compounds from Camellia sinensis L. leaves fermented with Aspergillus sp. J Nat Med. 2011;65(3-4):594-7. [CrossRef]
- Katanasaka, Y.; Sunagawa, Y.; Miyazaki, Y.; Funamoto, M.; Shimizu, S.; Shimizu, K.; Yamakage, H.; Satoh-Asahara, N.; Toyama, K.; Sabashi, T.; Suzuki, M.; Hamabe, T.; Komiyama, M.; Wada, H.; Mori, K.; Hasegawa, K.; Morimoto, T. Ameliorating prediabetic subject status via fermented tea supplementation: A randomized, double-blind, parallel-group comparison study. J Funct Foods. 2022, 97, 105257. [Google Scholar] [CrossRef]
- Achari, A.E.; Jain, S.K. Adiponectin, a Therapeutic Target for Obesity, Diabetes, and Endothelial Dysfunction. Int J Mol Sci. 2017, 18, 1321. [Google Scholar] [CrossRef] [PubMed]
- Klobučar, I.; Habisch, H.; Klobučar, L.; Trbušić, M.; Pregartner, G.; Berghold, A.; Kostner, G.M.; Scharnagl, H.; Madl, T.; Frank, S.; Degoricija, V. Serum Levels of Adiponectin Are Strongly Associated with Lipoprotein Subclasses in Healthy Volunteers but Not in Patients with Metabolic Syndrome. Int J Mol Sci. 2024, 25, 5050. [Google Scholar] [CrossRef]
- Ma, S.; Li, Z.; Yang, Y.; Zhang, L.; Li, M.; Du, L. Fluorescent Ligand-Based Discovery of Small-Molecule Sulfonamide Agonists for GPR120. Front Chem. 2022, 10, 816014. [Google Scholar] [CrossRef]
- Shimpukade, B.; Hudson, B.D.; Hovgaard, C.K.; Milligan, G.; Ulven, T. Discovery of a potent and selective GPR120 agonist. J Med Chem. 2012, 55, 4511–5. [Google Scholar] [CrossRef]
- Briscoe, C.P.; Peat, A.J.; McKeown, S.C.; Corbett, D.F.; Goetz, A.S.; Littleton, T.R.; McCoy, D.C.; Kenakin, T.P.; Andrews, J.L.; Ammala, C.; Fornwald, J.A.; Ignar, D.M.; Jenkinson, S. Pharmacological regulation of insulin secretion in MIN6 cells through the fatty acid receptor GPR40: identification of agonist and antagonist small molecules. Br J Pharmacol. 2006, 148, 619–28. [Google Scholar] [CrossRef]
- Li, Y.; Yu, H.; Lopes-Virella, M.F.; Huang, Y. GPR40/GPR120 Agonist GW9508 Improves Metabolic Syndrome-Exacerbated Periodontitis in Mice. Int J Mol Sci. 2024, 25, 9622. [Google Scholar] [CrossRef]
- Milligan, G.; Shimpukade, B.; Ulven, T.; Hudson, B.D. Complex Pharmacology of Free Fatty Acid Receptors. Chem Rev. 2017, 117, 67–110. [Google Scholar] [CrossRef] [PubMed]
- Hudson, B.D.; Shimpukade, B.; Mackenzie, A.E.; Butcher, A.J.; Pediani, J.D.; Christiansen, E.; Heathcote, H.; Tobin, A.B.; Ulven, T.; Milligan, G. The pharmacology of TUG-891, a potent and selective agonist of the free fatty acid receptor 4 (FFA4/GPR120), demonstrates both potential opportunity and possible challenges to therapeutic agonism. Mol Pharmacol. 2013, 84, 710–25. [Google Scholar] [CrossRef] [PubMed]
- Ji, G.; Guo, Q.; Xue, Q.; Kong, R.; Wang, S.; Lei, K.; Liu, R.; Wang, X. Novel GPR120 Agonists with Improved Pharmacokinetic Profiles for the Treatment of Type 2 Diabetes. Molecules. 2021, 26, 6907. [Google Scholar] [CrossRef]
- Wang, X.; Li, X.; Wei, S.; Wang, M.; Xu, Y.; Hu, W.; Gao, Z.; Liu, R.; Wang, S.; Ji, G. Discovery of Novel and Selective G-Protein Coupled Receptor 120 (GPR120) Agonists for the Treatment of Type 2 Diabetes Mellitus. Molecules. 2022, 27, 9018. [Google Scholar] [CrossRef] [PubMed]
- Adams, G.L.; Velazquez, F.; Jayne, C.; Shah, U.; Miao, S.; Ashley, E.R.; Madeira, M.; Akiyama, T.E.; Di Salvo, J.; Suzuki, T.; Wang, N.; Truong, Q.; Gilbert, E.; Zhou, D.; Verras, A.; Kirkland, M.; Pachanski, M.; Powles, M.; Yin, W.; Ujjainwalla, F.; Venkatraman, S.; Edmondson, S.D. Discovery of Chromane Propionic Acid Analogues as Selective Agonists of GPR120 with in Vivo Activity in Rodents. ACS Med Chem Lett. 2016, 8, 96–101. [Google Scholar] [CrossRef]
- Sparks, S.M.; Aquino, C.; Banker, P.; Collins, J.L.; Cowan, D.; Diaz, C.; Dock, S.T.; Hertzog, D.L.; Liang, X.; Swiger, E.D.; Yuen, J.; Chen, G.; Jayawickreme, C.; Moncol, D.; Nystrom, C.; Rash, V.; Rimele, T.; Roller, S.; Ross, S. Exploration of phenylpropanoic acids as agonists of the free fatty acid receptor 4 (FFA4): Identification of an orally efficacious FFA4 agonist. Bioorg Med Chem Lett. 2017, 27, 1278–1283. [Google Scholar] [CrossRef]
- Oh, D.Y.; Walenta, E.; Akiyama, T.E.; Lagakos, W.S.; Lackey, D.; Pessentheiner, A.R.; Sasik, R.; Hah, N.; Chi, T.J.; Cox, J.M.; Powels, M.A.; Di Salvo, J.; Sinz, C.; Watkins, S.M.; Armando, A.M.; Chung, H.; Evans, R.M.; Quehenberger, O.; McNelis, J.; Bogner-Strauss, J.G.; Olefsky, J.M. A Gpr120-selective agonist improves insulin resistance and chronic inflammation in obese mice. Nat Med. 2014 ;20:942-7. [CrossRef]
- Son, S.E.; Park, S.J.; Koh, J.M.; Im, D.S. Free fatty acid receptor 4 (FFA4) activation ameliorates 2,4-dinitrochlorobenzene-induced atopic dermatitis by increasing regulatory T cells in mice. Acta Pharmacol Sin. 2020, 41, 1337–1347. [Google Scholar] [CrossRef]
- Sundström, L.; Myhre, S.; Sundqvist, M.; Ahnmark, A.; McCoull, W.; Raubo, P.; Groombridge, S.D.; Polla, M.; Nyström, A.C.; Kristensson, L.; Någård, M.; Winzell, M.S. The acute glucose lowering effect of specific GPR120 activation in mice is mainly driven by glucagon-like peptide 1. PLoS One. 2017, 12, e0189060. [Google Scholar] [CrossRef]
- McCloskey, A.G.; Miskelly, M.G.; Flatt, P.R.; McKillop, A.M. Pharmacological potential of novel agonists for FFAR4 on islet and enteroendocrine cell function and glucose homeostasis. Eur J Pharm Sci. 2020, 142, 105104. [Google Scholar] [CrossRef]
- Cox, J.M.; Chu, H.D.; Chelliah, M.V.; Debenham, J.S.; Eagen, K.; Lan, P.; Lombardo, M.; London, C.; Plotkin, M.A.; Shah, U.; Sun, Z.; Vaccaro, H.M.; Venkatraman, S.; Suzuki, T.; Wang, N.; Ashley, E.R.; Crespo, A.; Madeira, M.; Leung, D.H.; Alleyne, C.; Ogawa, A.M.; Souza, S.; Thomas-Fowlkes, B.; Di Salvo, J.; Weinglass, A.; Kirkland, M.; Pachanski, M.; Powles, M.A.; Tozzo, E.; Akiyama, T.E.; Ujjainwalla, F.; Tata, J.R.; Sinz, C.J. Design, Synthesis, and Evaluation of Novel and Selective G-protein Coupled Receptor 120 (GPR120) Spirocyclic Agonists. ACS Med Chem Lett. 2016, 8, 49–54. [Google Scholar] [CrossRef] [PubMed]
- Chen, X.; Liu, C.; Ruan, L. G-Protein-Coupled Receptors 120 Agonist III Improves Hepatic Inflammation and ER Stress in Steatohepatitis. Dig Dis Sci. 2021, 66, 1090–1096. [Google Scholar] [CrossRef]
- Watterson, K.R.; Hansen, S.V.F.; Hudson, B.D.; Alvarez-Curto, E.; Raihan, S.Z.; Azevedo, C.M.G.; Martin, G.; Dunlop, J.; Yarwood, S.J.; Ulven, T.; Milligan, G. Probe-Dependent Negative Allosteric Modulators of the Long-Chain Free Fatty Acid Receptor FFA4. Mol Pharmacol. 2017, 91, 630–641. [Google Scholar] [CrossRef] [PubMed]
- Azevedo, C.M.; Watterson, K.R.; Wargent, E.T.; Hansen, S.V.; Hudson, B.D.; Kępczyńska, M.A.; Dunlop, J.; Shimpukade, B.; Christiansen, E.; Milligan, G.; Stocker, C.J.; Ulven, T. Non-Acidic Free Fatty Acid Receptor 4 Agonists with Antidiabetic Activity. J Med Chem. 2016, 59, 8868–8878. [Google Scholar] [CrossRef]
- Dragano, N.R.V.; Solon, C.; Ramalho, A.F.; de Moura, R.F.; Razolli, D.S.; Christiansen, E.; Azevedo, C.; Ulven, T.; Velloso, L.A. Polyunsaturated fatty acid receptors, GPR40 and GPR120, are expressed in the hypothalamus and control energy homeostasis and inflammation. J Neuroinflammation. 2017, 14, 91. [Google Scholar] [CrossRef] [PubMed]
- Tian, M.; Wu, Z.; Heng, J.; Chen, F.; Guan, W.; Zhang, S. Novel advances in understanding fatty acid-binding G protein-coupled receptors and their roles in controlling energy balance. Nutr Rev. 2022, 80, 187–199. [Google Scholar] [CrossRef]
- Gong, Z.; Yoshimura, M.; Aizawa, S.; Kurotani, R.; Zigman, J.M.; Sakai, T.; Sakata, I. G protein-coupled receptor 120 signaling regulates ghrelin secretion in vivo and in vitro. Am J Physiol Endocrinol Metab. 2014, 306, E28–E35. [Google Scholar] [CrossRef]
- Graciano, M.F.; Valle, M.M.; Curi, R.; Carpinelli, A.R. Evidence for the involvement of GPR40 and NADPH oxidase in palmitic acid-induced superoxide production and insulin secretion. Islets. 2013, 5, 139–48. [Google Scholar] [CrossRef]
- Raptis, D.A.; Limani, P.; Jang, J.H.; Ungethüm, U.; Tschuor, C.; Graf, R.; Humar, B.; Clavien, P.A. GPR120 on Kupffer cells mediates hepatoprotective effects of ω3-fatty acids. J Hepatol. 2014, 60, 625–32. [Google Scholar] [CrossRef]
- Chen, Y.L.; Lin, Y.P.; Sun, C.K.; Huang, T.H.; Yip, H.K.; Chen, Y.T. Extracorporeal shockwave against inflammation mediated by GPR120 receptor in cyclophosphamide-induced rat cystitis model. Mol Med. 2018, 24, 60. [Google Scholar] [CrossRef]
- Olmo, I.; Teuber, S.; Larrazabal, C.; Alarcon, P.; Raipane, F.; Burgos, R.A.; Hidalgo, M.A. Docosahexaenoic acid and TUG-891 activate free fatty acid-4 receptor in bovine neutrophils. Vet Immunol Immunopathol. 2019, 209, 53–60. [Google Scholar] [CrossRef] [PubMed]
- Gozal, D.; Qiao, Z.; Almendros, I.; Zheng, J.; Khalyfa, A.; Shimpukade, B.; Ulven, T. Treatment with TUG891, a free fatty acid receptor 4 agonist, restores adipose tissue metabolic dysfunction following chronic sleep fragmentation in mice. Int J Obes (Lond). 2016, 40, 1143–9. [Google Scholar] [CrossRef] [PubMed]
- Schilperoort, M.; van Dam, A.D.; Hoeke, G.; Shabalina, I.G.; Okolo, A.; Hanyaloglu, A.C.; Dib, L.H.; Mol, I.M.; Caengprasath, N.; Chan, Y.W.; Damak, S.; Miller, A.R.; Coskun, T.; Shimpukade, B.; Ulven, T.; Kooijman, S.; Rensen, P.C.; Christian, M. The GPR120 agonist TUG-891 promotes metabolic health by stimulating mitochondrial respiration in brown fat. EMBO Mol Med. 2018, 10:e8047. [CrossRef]
- Murtaza, B.; Hichami, A.; Khan, A.S.; Shimpukade, B.; Ulven, T.; Ozdener, M.H.; Khan, N.A. Novel GPR120 agonist TUG891 modulates fat taste perception and preference and activates tongue-brain-gut axis in mice. J Lipid Res. 2020, 61, 133–142. [Google Scholar] [CrossRef]
- Zhang, X.; Cai, C.; Sui, Z.; Macielag, M.; Wang, Y.; Yan, W.; Suckow, A.; Hua, H.; Bell, A.; Haug, P.; Clapper, W.; Jenkinson, C.; Gunnet, J.; Leonard, J.; Murray, W.V. Discovery of an Isothiazole-Based Phenylpropanoic Acid GPR120 Agonist as a Development Candidate for Type 2 Diabetes. ACS Med Chem Lett. 2017, 8, 947–952. [Google Scholar] [CrossRef] [PubMed]
- Ma, J.; Novack, A.; Nashashibi, I.; Pham, P.; Rabbat, C.J.; Song, J.; Shi, D.F.; Zhao, Z.; Choi, Y.J.; Chen, X. (2010). Aryl GPR120 receptor agonists and uses thereof. International Patent WO 2010/048207.
- Wang, C.; Liu, Y.; Pan, Y.; Jin, H. Effect of GSK-137647A, the first non-carboxylic FFA4 agonist, on the osteogenic and adipogenic differentiation of bone mesenchymal stem cells in db/db mice. J Pharm Pharmacol. 2020, 72, 461–469. [Google Scholar] [CrossRef]
- Salaga, M.; Bartoszek, A.; Binienda, A.; Krajewska, J.B.; Fabisiak, A.; Mosińska, P.; Dziedziczak, K.; Niewinna, K.; Talar, M.; Tarasiuk, A.; Kordek, R.; Fichna, J. Activation of Free Fatty Acid Receptor 4 Affects Intestinal Inflammation and Improves Colon Permeability in Mice. Nutrients. 2021, 13, 2716. [Google Scholar] [CrossRef]
- Hasan, A.U.; Ohmori, K.; Hashimoto, T.; Kamitori, K.; Yamaguchi, F.; Noma, T.; Igarashi, J.; Tsuboi, K.; Tokuda, M.; Nishiyama, A.; Kohno, M. GPR120 in adipocytes has differential roles in the production of pro-inflammatory adipocytokines. Biochem Biophys Res Commun. 2017, 486, 76–82. [Google Scholar] [CrossRef]
- Grundmann, M.; Bender, E.; Schamberger, J.; Eitner, F. Pharmacology of Free Fatty Acid Receptors and Their Allosteric Modulators. Int J Mol Sci. 2021, 22, 1763. [Google Scholar] [CrossRef]
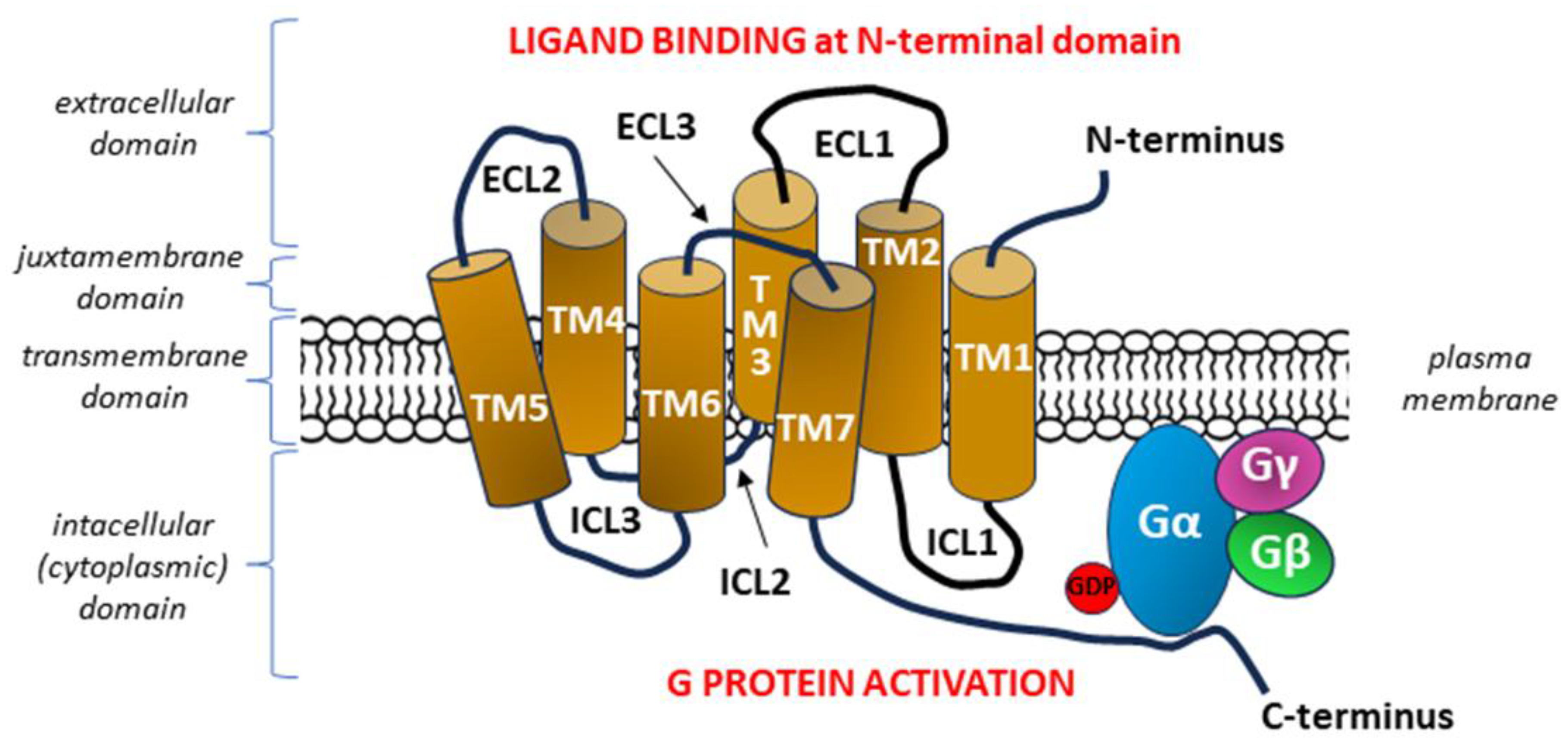
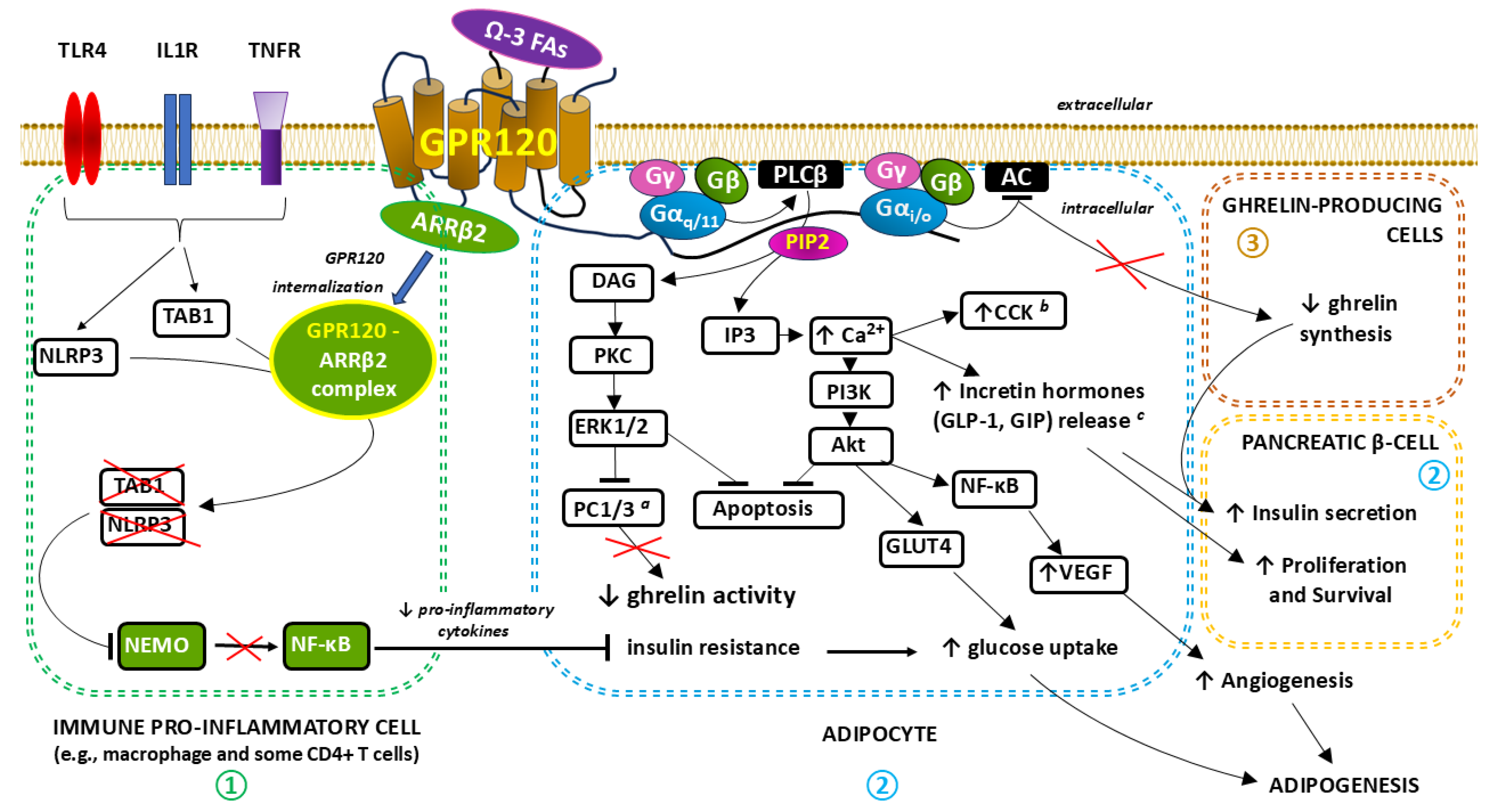
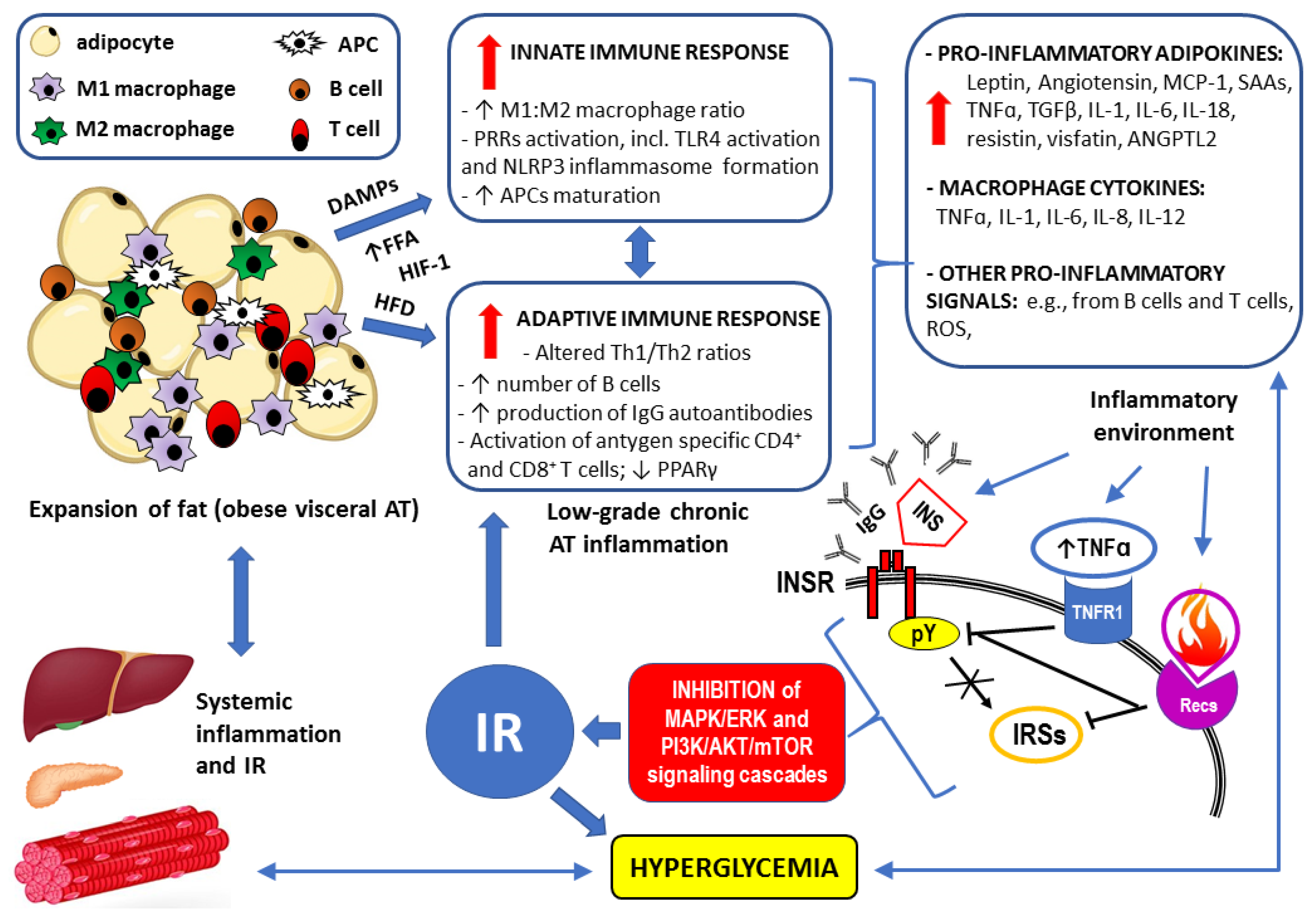
| GPR120/FFAR4 non-LCAF agonist from natural sources | The structure of the molecule and chemical nomenclature | Source | Agonist’s potency (EC50)* | Selectivity | Documented metabolic effects in obesity-related disorders |
|---|---|---|---|---|---|
|
Grifolin derivatives: - grifolic acid and - grifolic acid methyl ether |
 2,4-dihydroxy-6-methyl-3-[(2E,6E)-3,7,11-trimethyldodeca-2,6,10-trienyl] benzoic acid 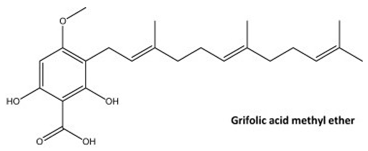 2-hydroxy-4-methoxy-6-methyl-3-[(2E,6E)-3,7,11-trimethyldodeca-2,6,10-trienyl] benzoic acid |
First extracted from the mushroom Albatrellus confluens, its content was also confirmed in Albatrellus dispansus, Albatrellus ovinus, Peperomia galioides, a species of plant in the family Piperaceae, and other organisms with data available (i.e., Rhododendron dauricum), including tomato (Solanum lycopersicum L.) [238,245,246] |
> 30 µM [234,235,247] > 30 µM [234,235,247] |
Selective partial agonist Selective partial agonist |
- Antioxidative activity properties more potent than both α-tocopherol and butylated hydroxyanisole (BHA) [248,249]. - As partial agonists with high selectivity, grifolin derivatives mediate the anti-inflammatory effects of n-3 polyunsaturated fatty acids (PUFA), however, are less efficacious in activating GPR120 compared to ALA. Additionally, although acting in a GPR120-independent manner, grifolic acid may reduce inflammation by stimulating apoptosis (a non-inflammatory event) of cells involved in the inflammatory reaction, including macrophages [234,237,240,245,250,251]. - By acting on GPR120 expressed on neuroendocrine intestinal L- and K-cells, grifolin derivatives stimulate GLP-1/GIP secretory pathways involved in mediating enhanced insulin secretion and improved glucose tolerance [193,197,198]. - Contrary to in vitro conditions, grifolin derivatives after oral administration in WT mice increase ghrelin secretion and its concentration in plasma. Next, ghrelin secreted from GPR120 (+) cells can sense LCFAs and MCFAs directly. Thus, GPR120-related the lipid sensing cascade of the ghrelin cell, despite of reduction in inflammation, may be responsible for the increases in adipogenesis, gluconeogenesis, triglyceride and FAs synthesis as well as increased appetite and food intake [252,253]. |
| KDT501 (isohumulone) |
 potassium;(1R,5S)-2-hydroxy-3-(3-methylbutanoyl)-5-(3-methylbutyl)-1-(4-methylpentanoyl)-4-oxocyclopent-2-en-1-olate |
Substituted 1,3-cyclopentadione chemically derived from hops (Humulus lupulus L.) extracts [241] | 30.3 µM (mice) [241] | Non-selective, also partial PPARγ agonist [241] | - Oral administration of KDT501 in diet-induced obese (DIO) mouse and in a standard model for metabolic syndrome and T2D, the Zucker Diabetic Fatty (ZDF) rats, improved glucose metabolism and reduced plasma hemoglobin A1C (HbA1c) content [70,241]. - Dose-dependent reduction of weight gain and total cholesterol was demonstrated in ZDF rats receiving KDT501 [241]. - When high doses of KDT501 were used in rodent models of diabetes, weight loss was observed that was equivalent to significant reduction in fat mass [241]. - No effect of KDT501 on lipogenesis was observed during DHA administration [70,241]. - In a small study (n = 9) of patients with obesity and prediabetes, treatment with KDT501 to a maximum dose of 1000 mg every 12 hours for a total of 28 days demonstrated a reduction in systemic inflammatory markers and improvement in postmeal plasma triglyceride levels [242]. - KDT501 induced post-transcriptionally secretion of adiponectin and increased gene expression of thermogenic and lipolytic genes in response to cold stimulation [243]. - The assessment of the effects should take into account the lack of selectivity towards GPR120 and stimulation of PPAR-γ [241]. |
| Teadenol A |
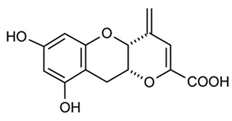 (4aR,10aR)-7,9-dihydroxy-4-methylidene-10,10a-dihydro-4aH-pyrano[3,2-b]chromene-2-carboxylic acid |
Polyphenol isolated from both Japanese and Chinese post-fermented teas (Camellia sinensis L.) [244] |
N.A.D.# | Selective agonist [244] | - The beneficial effects of teadenol A observed in metabolic syndrome were completely dependent on GPR120 expression on target cells [244,254]. - Under the influence of teadenol A, the secretion of GLP-1 from intestinal endorine STC-1 cells increases - consequently, GLP-1 suppresses appetite and increases insulin secretion, exhibiting anti-diabetic effects [244,255]. - Teadenol A-containing teas are expected to improve fasting blood glucose levels and IR because teadenol A promotes the secretion of adiponectin from adipocytes [244,256]. - Microbial fermented containing teadenol A improves triglyceride levels in prediabetic subjects, which is most likely due to the promotion of adiponectin secretion, a well-known adipokine that lowers triglycerides and LDL cholesterol levels [256,257,258]. |
| Synthetic GPR120/FFAR4 agonist | The structure of the molecule and chemical nomenclature |
Agonist’s potency (EC50)* | Selectivity |
Documented metabolic effects in obesity-related disorders |
|---|---|---|---|---|
| GW9508 |
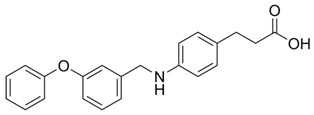 4-{[(3-phenoxyphenyl)methyl]amino} benzenepropanoic acid |
2.2 µM [89] |
Non-selective: ~100-fold selectivity for GPR40 over GPR120 | - Decrease in ghrelin secretion [279]. - Increase in the thermogenic activity of BAT and WAT [183] - Increase in glucose-induced insulin secretion with subsequent reduction of plasma glucose [206,280]. - Increased insulin sensitivity [262]. - Induction of the release of fibroblast growth factor 21 (FGF-21) by brown and beige adipocytes to maintain glucose homeostasis with subsequent increase in blood FGF-21 levels to improve metabolic adaptation to fasting [183]. - Inhibition of inflammatory responses in obesity, including improvement of metabolic syndrome-exacerbated periodontitis in mice [262,281,282] |
| NCG21 |
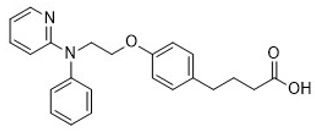 4-{4-[2-(phenyl-pyridin-2-yl-amino)-ethoxy]-phenyl}-butyric acid |
N.A.D. [217,225,235,263] |
PPAR-γ agonist derivative; high (albeit incomplete) selectivity for GPR120 over GPR40 | - Increase in GLP-1 secretion [235] - Intracolonic administration of NCG21 in mice was positively correlated with increased plasma GLP-1 levels [235,263]. |
| TUG-891 |
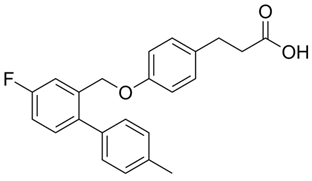 ortho-biphenyl ligand 4-{[4-fluoro-4′-methyl(1,1′-biphenyl)-2-yl]methoxy}-benzenepropanoic acid |
73.74 μM, (bovine neutrophils) [283] | GPR40 non-selective agonist GW9508 derivative; a potent and selective agonist of the GPR120 with 1000-fold selectivity over human GPR40 | - Amelioration of meta-inflammation and IR by increased visceral WAT p-Akt/Akt responses to insulin [284]. - Prevention of increased food intake and weight gain in mice undergoing chronic sleep fragmentation [284]. -Increase of fat oxidation and reduction of fat mass by stimulation of mitochondrial respiration in BAT [182,285]. - Increase in GLP-1 secretion and decrease in circulating LDL [286]. - Promoting the differentiation of 3T3-L1 adipocytes, i.e. adipogenesis from preadipocytes to mature adipocytes [181]. - Protective effect against lipotoxicity-induced pancreatic β-cell dysfunction, via the mediation of the pancreatic and duodenal homeobox 1 (PDX1) expression and inhibition of islet inflammation [162]. - Activation of thermogenesis by activation of UCP1, which constitutes one of the primary mechanisms by which BAT increases energy expenditure [182,285]. |
|
Compound 29 (phenylpropanoic acid) |
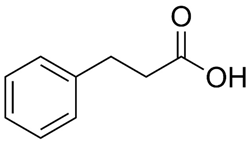 3-Phenylpropanoic acid |
42 nM [287] | Highly selective, medium potency | - Increased insulin sensitivity [267,268]. |
| Compound 18 (chromane propionic acid derivative) |
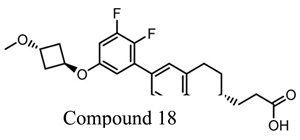 |
35 nM (mice) [267] | Highly selective and potent | - Increased insulin sensitivity [267]. |
| Compound A (Merck) |
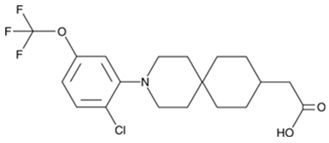 3-[2-chloro-5-(trifluoromethoxy)phenyl]-3-azaspiro[5.5]undecane-9-acetic acid |
~ 0.35 µM (mice) [269] |
Highly selective, reversible superagonist |
- Anti-inflammatory effects in macrophages in vitro [269]. - Improvement in glucose tolerance and decrease in hyperinsulinemia [269] - When administered orally in obese mice on a high-fat diet, concentration-dependent anti-inflammatory and insulin-sensitizing effects of comparable potency to ω3-FA administration [80]. - Reduction of fatty liver disease [269] |
|
Metabolex 36 |
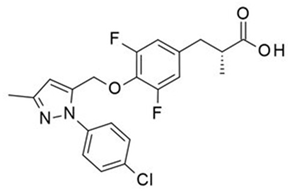 3-(3,5-difluoro-4-((3-methyl-1-phenyl-1H-pyrazol-5-yl)methoxy)phenyl)-2-methylpropanoic acid |
570 nM [203] | Selective and potent | - Improved oral glucose tolerance and increased insulin secretion in lean mice during the intravenous glucose tolerance test (IVGTT) [203,288]. - Suppression of glucose-induced somatostatin secretion from pancreatic δ cells [203]. - Inhibition of cAMP production in mouse islet cells and increased production and secretion of GLP-1 from an intestinal neuroendocrine STC-1 cells [271,288]. |
|
AZ13581837 |
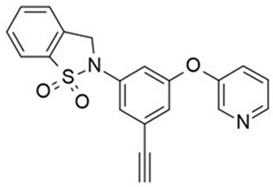 2-(3-Ethynyl-5-(3-pyridyloxy)phenyl)-3H-1,2-benzothiazole 1,1-dioxide |
120 nM [271] |
Selective and potent |
- Inhibition of cAMP production in mouse islet cells and increased production and secretion of GLP-1 from an intestinal neuroendocrine STC-1 cells [204,271]. pancreatic δ cells [203]. - Improved oral glucose tolerance and increased insulin secretion in IVGTT in lean mice [204,272]. |
| GPR120 agonist III |
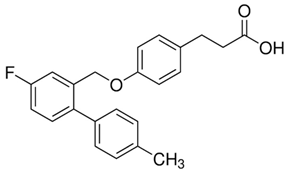 3-(4-((4-Fluoro-4ʹ-methyl-(1,1ʹ-biphenyl)-2-yl)methoxy)-phenyl)propanoic acid |
44 nM [260] | Fully selective for GPR120 and potent | - Improvement in insulin sensitivity overcoming IR [269]. - Stimulating the ability of insulin to inhibit gluconeogenesis in the liver [269,274]. - Significant anti-inflammatory activity manifested by the inhibition of LPS-induced phosphorylation of TAK1, IKKβ, and JNK, and blocked IκB degradation [273]. - Beneficial effect on hepatic lipid metabolism by lowering the level of hepatic triglycerides and DAGs, reducing the content of saturated FFAs and reducing liver steatosis [274]. |
| GSK137647A |
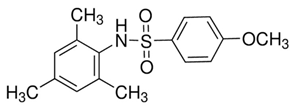 4-Methoxy-N-(2,4,6-trimethylphenyl)-benzenesulfonamide, N-Mesityl-4-methoxybenzenesulfonamide |
501 nM (mice) [289] | Selective and potent | - Participation in glycemic homeostasis by inducing insulin secretion and inhibiting epithelial ion transport [290]. - Protection of pancreatic β cell dysfunction by inhibiting islet inflammation [162]. - Anti-inflammatory response accompanied by a reduction in NO production by macrophages [290]. - Suppression of adipogenic differentiation of mesenchymal stem cells [289]. - Anti-inflammatory effect in adipose tissue related to the inhibition of the NF-κB pathway and, consequently, limiting the production of pro-inflammatory adipocytokines [291]. |
| TUG-1197 (compound 34) |
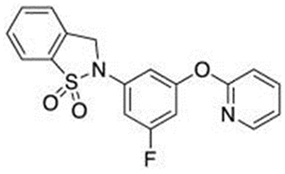 2-(3-fluoro-5-pyridin-2-yloxyphenyl)-3H-1,2-benzothiazole 1,1-dioxide |
24 nM [292] | Fully selective for GPR120 and very potent |
- Improved glucose tolerance after oral dosing in an oral glucose tolerance test performed both in normal and diet-induced obese (DIO) mice [70,276] - Chronic dosing of TUG-1197 in DIO mice increased insulin sensitivity in an GPR120-dependent manner [276]. - Improvement in glucose homeostasis correlated with moderate but significant reduction in bodyweight in DIO mice [276]. |
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2025 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (http://creativecommons.org/licenses/by/4.0/).




