1. Introduction
Olecranon, the proximal articular region of the ulna, accounts for about 5% of all elbow fractures in children [
1] and approximately 20% are complicated by other ipsilateral elbow injuries [
2]. Primarily (68%) male patients are affected by these traumas. Mean ages ranged from 7.3 to 13.5 years, and the youngest documented patient was 2 months old according to a recent systematic review [
3]. High-energy direct blows or falling to either an outstretched hand or a flexed elbow during sports activities are common mechanisms of injury [
4].
Clinically they may present as sharp, intense elbow pain with swelling, tenderness, bruising, ecchymosis, restricted motions, crepitus, or even visible deformities, bleeding, and exposed bones [
5]. During the neurological examination, sensations over the little finger should be carefully checked, ensuring that the small muscles of the hand are functioning normally because the ulnar nerve is particularly at risk of injury along with an olecranon fracture.
Pediatric olecranon fractures have been classified using various systems, yet no single approach has gained universal acceptance or proven superior in guiding treatment decisions. Caterini et al. proposed a five-type categorization based on the anatomical site of the fracture line, the degree of displacement, and the presence of associated injuries [
2]. Horne and Tanzer introduced a three-type system that categorizes fractures based on their location within the olecranon [
6], while the Mayo classification, originally designed for adult fractures, considers the extent of displacement and the stability of the elbow joint [
7]. For children, most recently, the Arbeitsgemeinschaft für Osteosynthesefragen (AO) Foundation developed the Pediatric Comprehensive Classification of Fractures (PCCF) protocol, which focuses on the morphological characteristics of the fracture [
8],
Elbow X-ray is the primary initial imaging modality for pediatric olecranon fracture diagnostics from anteroposterior (AP) and lateral views [
9]. On lateral radiographs, specific markers such as the anterior humeral and radial head-capitellar lines, along with the Baumann angle, help assess proper alignment [
10]. A positive posterior fat pad sign in the lateral projection or a longitudinal crack may indicate an occult fracture [
11]. In case of uncertainty, they can be followed by computer tomography (CT) – for more precise, three-dimensional (3D) bone visualization, or magnetic resonance imaging (MRI) for assessing the surrounding soft tissues and to avoid ionizing radiation. Regrettably, MRI has inferior bone imaging capabilities, compared to CT. Ultrasound (US) may be also able to detect fractures in the hands of an experienced user.
Six secondary ossification centers of the elbow ossify predictably according to the age and sex child, generally two years earlier in girls [
12]. Familiarity with their morphology and pattern is essential for accurate radiologic differential diagnoses of normal bone development phases from fractures. They can be remembered using the CRITOE mnemonic (C: capitellum, R: radial head, I: Internal (medial) epicondyle, T: trochlea, O: olecranon E: external (lateral) epicondyle) [
10]. Contralateral imaging for comparison is contraindicated in children, due to the high frequency of unilateral anatomical variations in the ossification centers [
13]. However, bilateral injuries may also occur, therefore, imaging both limbs are advised if clinical symptoms or injury mechanisms suggest it.
Generally, stable, non-displaced fractures can be treated by a conservative method employing cast immobilization. Displaced intra-articular olecranon fractures are most commonly treated with open reduction and internal fixation (ORIF), utilizing various fixation methods such as plate osteosynthesis (POS), compression screws, tension band wires (TBW), or -sutures (TBS) [
4]. Tension band fixation remains the standard treatment for displaced transverse intra-articular olecranon fractures, though concerns of increased fixation revision risk have arisen in older (>14 years) and heavier (>50 kilograms (kgs)) patients when using TBS compared to TBW [
1,
14].
Originally, the TBW technique was developed by Weber and Vasey in 1963, and it is recommended by the AO Foundation [
15]. Traditionally it involves reducing the fracture, followed by the placement of two parallel Kirschner (K-) wires (i.e.
, pins) through the olecranon and across the fracture [
16]. Afterward, a transverse hole is drilled in the ulna distal to the fracture site, through which a steel wire is passed, forming a figure-of-eight tension band around the K-wires. To strengthen the attachmen
t’s rigidity, Weber and Vasey suggested twisting both figure-of-eight wire limbs [
16]. Rowland and Burkhart emphasized the mathematical need to place the transverse hole for the figure-of-eight tension band wire anterior to the intramedullary pin [
17]. However, a biomechanical cadaver study by Paremain et al. did not confirm this hypothesis, as their results showed no significant differences in yield loads or stiffness values between the Rowland-Murkhart and AO TBW techniques [
18]. While tension band fixation has been shown to provide articular compression, it can also be associated with painful hardware, leading to implant removal in up to 88% of patients. In active children with a thin subcutaneous layer, tension band wires can be particularly prominent and painful, often requiring a return to the operating theatre for hardware removal [
19].
Because K-wire and the cerclage ends were causing irritation in many cases, alongside K-wire fixation, a special absorbable suture (ultrahigh molecular weight braided polyester suture; FiberWire) was used to create the figure-of-eight TBS, which was found to be more advantageous in this regard [
20]. A previous adult study proved a new enhancement to the long-established AO TBW technique by incorporating bioabsorbable magnesium compression screws along with a polyethylene mesh tape [
21]. The latter approach provides the biomechanical advantages of TBW fixation while eliminating the concerns associated with hardware. It has proven successful in a small group of olecranon fractures, with no hardware-related or other significant complications observed.
In recent decades, biodegradable polyesters such as poly-glycolic acid (PGA) and poly-lactic acid (PLA) have been developed for medical use. An important benefit is their bending modulus, which is similar to that of bone, preventing complications associated with stress shielding, unlike when using metal hardware. Poly-L-lactic-co-glycolic acid (PLGA) implants retain their mechanical strength and properties for at least eight weeks before undergoing full absorption within approximately two years [
22,
23]. This biodegradable polymer is commonly used in medical devices due to its excellent biocompatibility. An optimal balance between strength and degradation rate is provided by the specific 85L:15G composition (85% lactic acid and 15% glycolic acid). The controlled absorption provided by this specific composition allows for continuous bone remodeling and recanalization of the pin-formed place. Implants made from this material have been shown to cause less inflammation and irritation in the surrounding tissues. In contrast, the previous generation of implants made from PGA faced challenges due to their rapid degradation, which produced acidic byproducts. These byproducts activated pro-inflammatory cytokines, leading to significant inflammation and poor clinical outcomes [
4].
Our previous cohort study showed that pediatric medial humeral epicondyle fractures could be effectively managed by PLGA pins and absorbable sutures [
24]. However, according to our literature search, currently, no study evaluated the clinical and radiological outcomes of resorbable PLGA pins and polydioxanone (PDS) loops in pediatric olecranon fractures. Therefore, this case series aims to evaluate these aforementioned bioresorbable alternatives to conventional metallic fixation.
2. Patients and Methods
2.1. Study Design and Patient Selection
Between Jan 2022 and January 2023, the Division of Surgery, Traumatology, Urology, and Otorhinolaryngology, Department of Pediatrics at the University of Pécs, Clinical Complex was involved in the consecutive treatment of three pediatric patients with olecranon fractures utilizing PLGA pin implants (Activa PIN™, Bioretec Ltd., Tampere, Finland) and PDS loops (Ethicon, Johnson & Johnson). Our single-center, prospective case series aims to present adolescent olecranon fracture treatment with resorbable implants and evaluate the one-year follow-ups of the result of this method.
This case series involves three patients, which were included due to meeting the following criteria: (1) all under 18 years of age at the time of injury, with (2) open physes (growth plates) who (3) sustained displaced intraarticular olecranon fractures (4) requiring surgical intervention, (5) utilizing resorbable pin fixation and a PDS compression loop, and later (6) attended the one-year follow-up. During the investigation period, all patients were included who met the inclusion criteria.
2.2. Operative Algorithm
The surgical technique was almost identical to the traditional method, with one additional step. In a supine position under general anesthesia, an open approach was made, and after accurate reduction, the fracture was temporarily stabilized with K-wires. These wires were then replaced with bioabsorbable pins. Compression was ensured by a PDS loop placed in a drilled canal distal to the fracture.
Post-surgical care involved placing the arm in a dorsal above-elbow cast with the elbow flexed at 90 degrees (°) for approximately three weeks. After the removal of the right angle cast, active physiotherapeutic rehabilitation ensued.
3. Results
3.1. Case 1
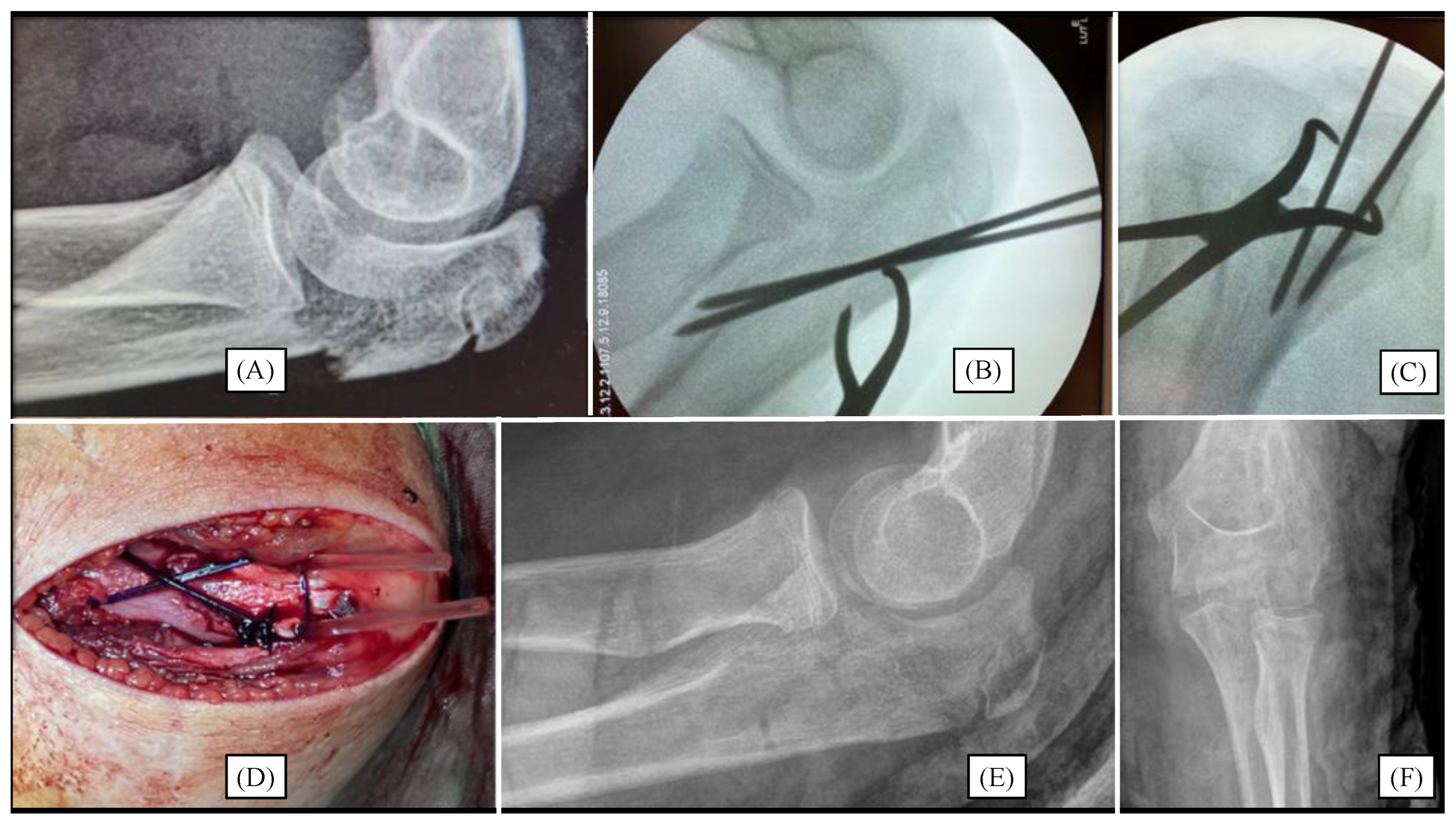
While cycling, a 12-year-old boy injured his left elbow. Initial X-rays confirmed a Mayo type II/A olecranon fracture (
Figure 1A). Due to the formation of joint steps, surgical intervention was necessary. Throughout the open approach, the fracture was reduced to an anatomical position and temporarily fixed with two K-wires (
Figure 1B). After the removal of the K-wires, the absorbable PLGA pins were placed into the cavity previously created by the wires. Subsequently, compression was achieved by PDS loops placed in a drilled canal distal to the fracture to ensure proper stability (
Figure 1D). A right-angle dorsal cast was employed to immobilize the left upper limb for three weeks, followed by active physiotherapy treatment.
During follow-up, the child’s range of motion (ROM) in the elbow gradually improved with regular physiotherapy. Three months after the surgery, the elbow ROM was fully restored. At the one-year follow-up, the motion of the left elbow was identical to that of the unaffected side. No sensitivity or irritation was reported around the surgical site. Follow-up X-rays showed complete healing of the fracture site with full joint congruence (
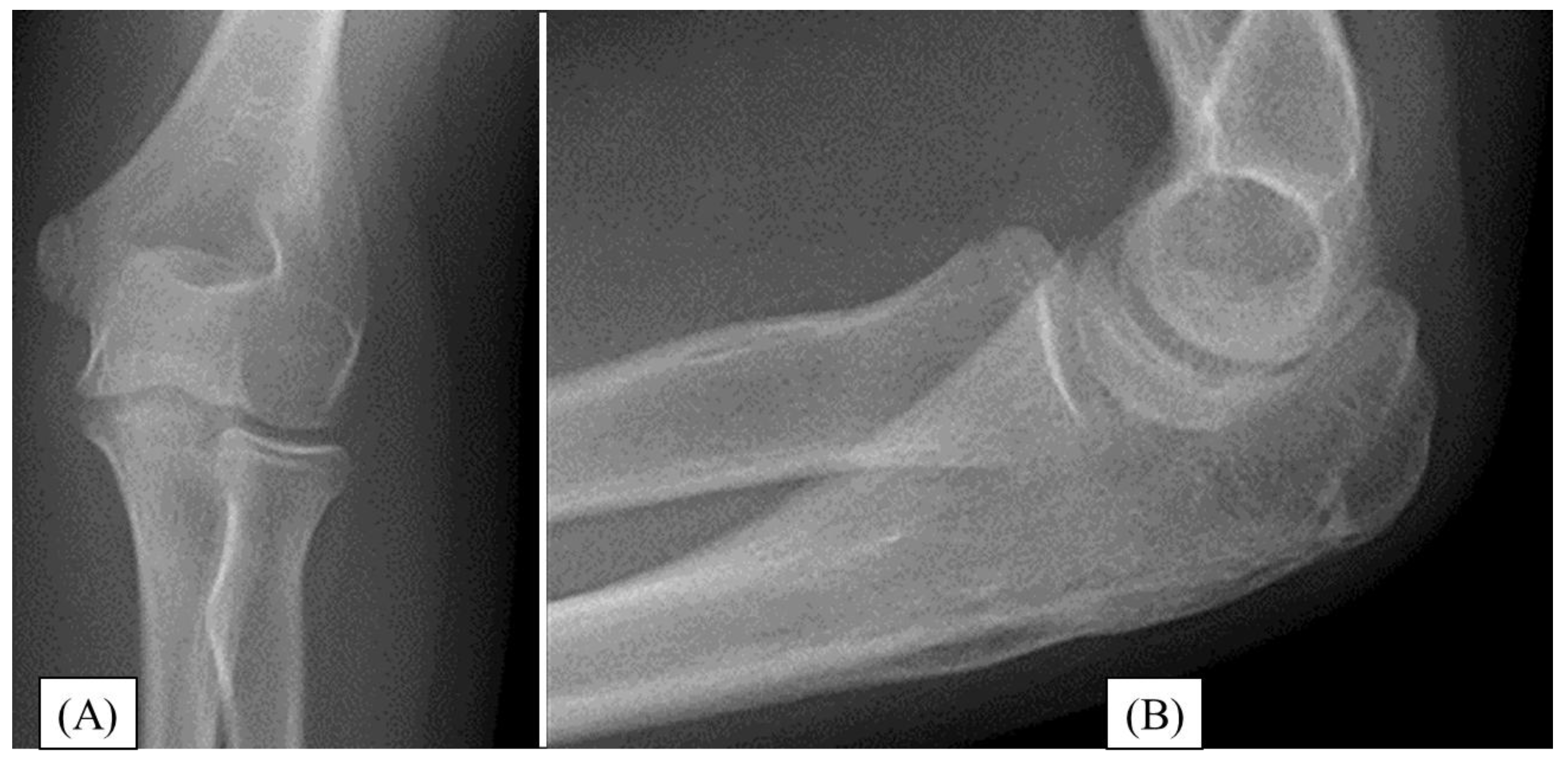
Figure 2). One year after the operation, the child was symptom-free and has returned to everyday sports activities.
3.2. Case 2
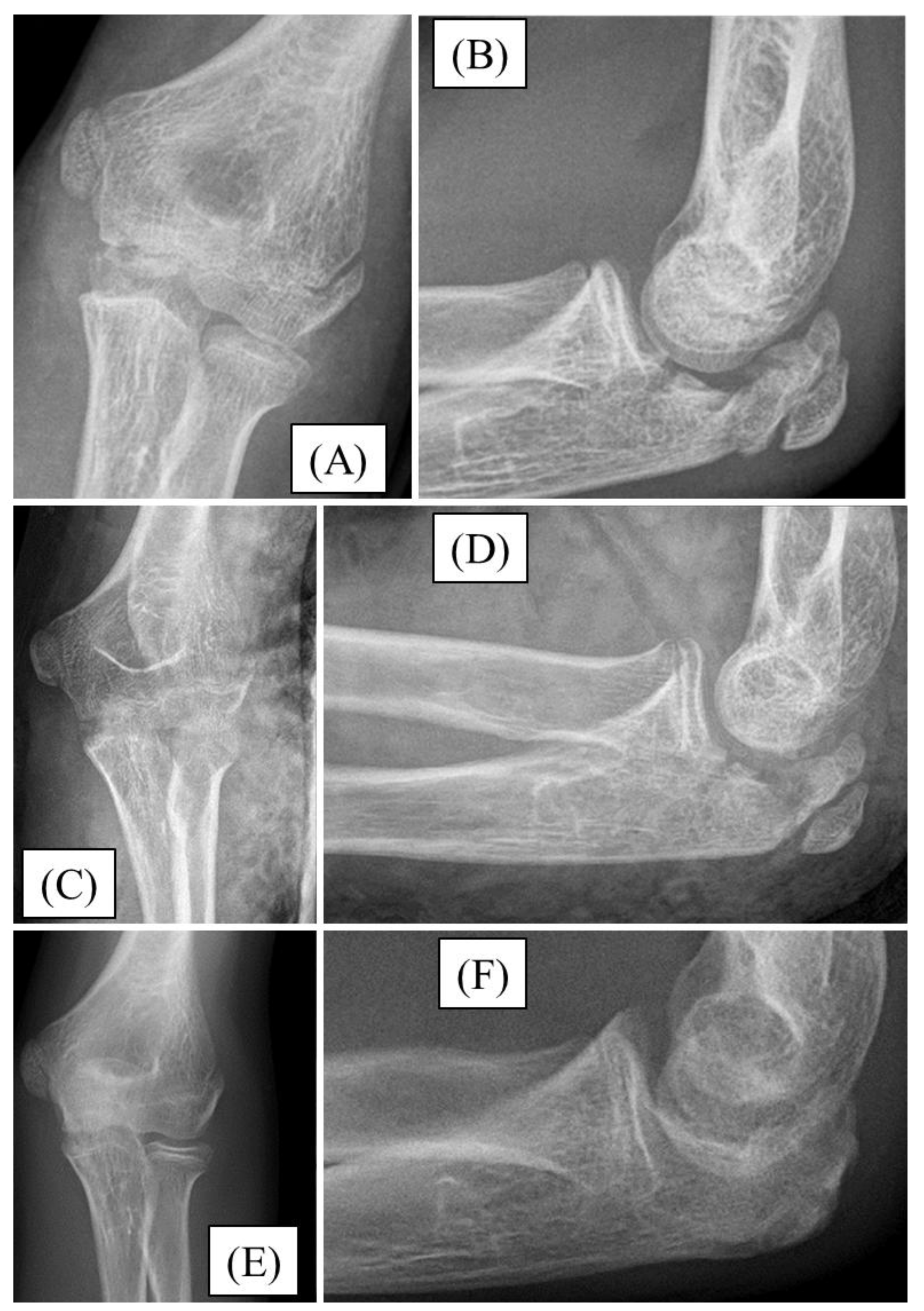
After falling down the stairs, a 12-year-old boy sustained an injury. Significant swelling and restricted joint movement developed above his left elbow. A Mayo type II/B olecranon fracture with joint step formation was confirmed by X-rays (
Figure 3A,B). After preparation, the fracture was reduced and stabilized with absorbable PLGA pins and a PDS loop. The follow-up X-ray showed the fracture in good alignment (
Figure 3C,D). The postoperative period was uneventful. For three weeks, the left upper limb was restrained in a long arm cast. Following the restriction, the child received active physiotherapy. All through the follow-up, we observed the gradual mending of the fracture. One-year follow-up radiographs confirmed finished fracture healing, with full elbow joint function (
Figure 3E,F).
3.3. Case 3
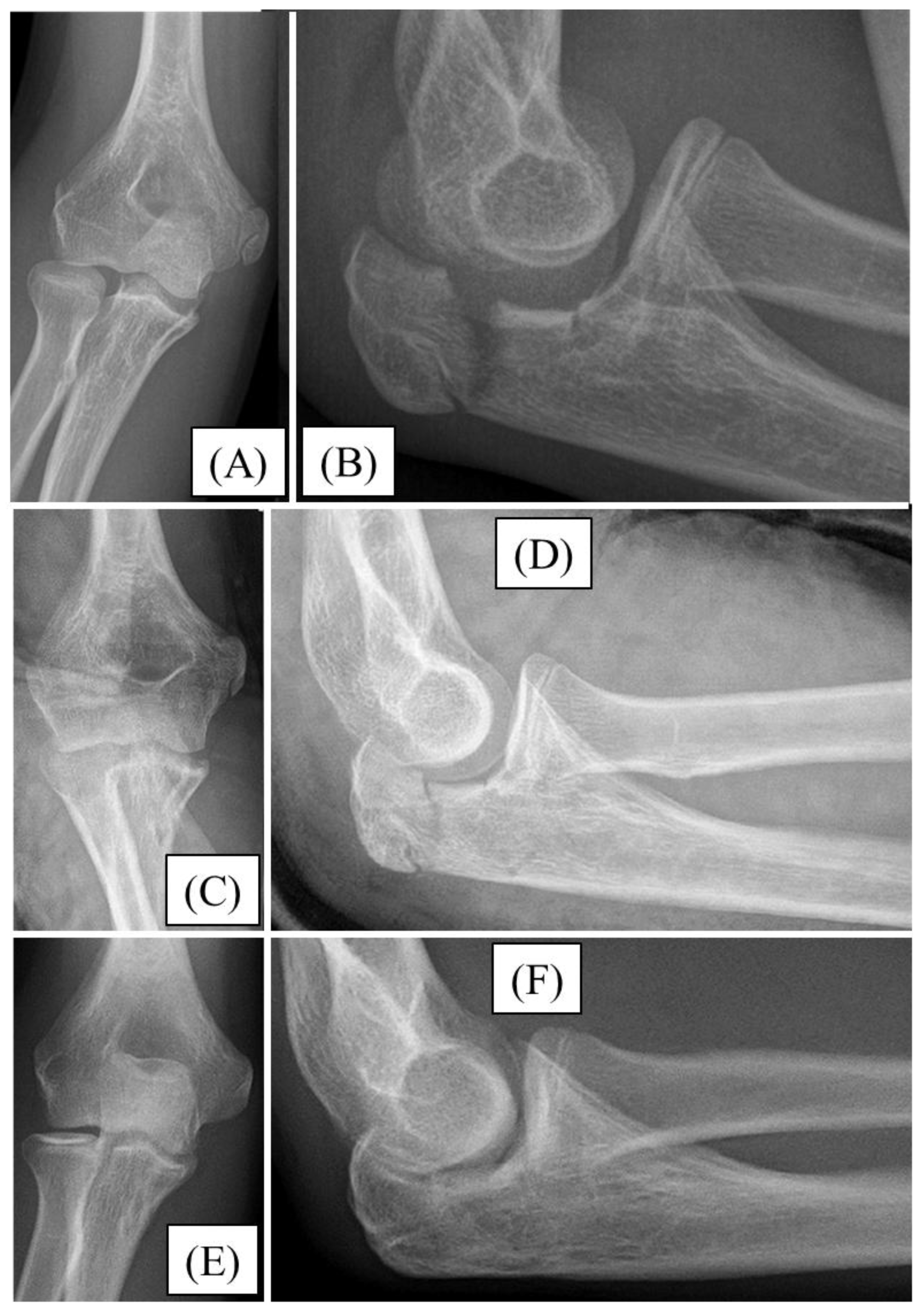
A 13-year-old boy injured his right elbow while cycling. He presented with significant swelling and restricted ROM. X-rays confirmed a comminuted Mayo type II/A olecranon fracture with joint involvement (
Figure 4A,B). During open surgery, after achieving the most accurate reduction, the fracture was stabilized with absorbable implants (PLGA pins and a PDS loop) (
Figure 4C,D). The postoperative period proceeded without complications. After three weeks of casting, the child underwent active physiotherapy. During follow-up, healing of the fracture was observed. One-year follow-up showed complete healing of the fracture on X-ray (
Figure 4E,F), with full elbow joint function.
4. Discussion
Pediatric olecranon fracture management must be approached with consideration for the growing skeletal system, as improper treatment can affect both function and future growth. Despite many advancements, the continued use of multiple classification systems underscores the lack of consensus on a standardized framework for assessing fracture severity and guiding optimal management in pediatric patients [
4]. Treatment options for these injuries generally depend on the age of the child and the nature of the fracture [
10,
11].
In cases of non-displaced fractures, where the fracture is stable, conservative treatment with immobilization in a cast or splint may be sufficient. Due to the higher potential for natural healing and remodeling, this approach is often favored in younger children.
Displaced or comminuted fractures, however, often require surgical intervention. Here, the goal is to restore the anatomical alignment of the olecranon and allow for optimal functional recovery. Surgical techniques typically include fixation with screws, wires, tension band wiring, or plates. However, in children, special care must be taken to avoid damaging the growth plate, as this could lead to long-term functional deficits or growth disturbances [
1,
4,
15,
19,
27,
28].
Pinning and tension band wiring is a common procedure used in pediatric olecranon fracture management. The method involves the usage of K-wires or other pinning techniques combined with a tension band to stabilize the fracture. While effective, it requires careful consideration regarding the possibility of hardware removal later, as the K-wires may cause irritation [
4,
29].
Among surgical treatments, compression screw utilization has also gained attention, but in many cases, the screw tip above the olecranon causes discomfort for the patients [
27]. However, Herbert screws also showed minor postoperative complications (implant loosening, bursitis) and better clinical outcomes (QuickDASH (Disabilities of the Arm, Shoulder, and Hand) score, intraoperative blood loss, surgery duration) compared to TBW in adolescents by a recent study [
30].
Comminuted olecranon fracture treatment may present a significant challenge in both adolescent and adult patients. Following reduction, plate fixation can be an appropriate solution, provided that significant growth is no longer expected in the child [
28].
Due to complications observed with metal implants, such as soft tissue irritation caused by wire ends and skin perforation, an increasing number of studies have presented their results achieved with resorbable implants [
1,
4,
19].
This study discussed the treatment of three children with displaced, intraarticular olecranon fractures using a new resorbable technique. Our surgical procedure, similar to interventions with metal implants, involved accurate repositioning and ensuring articular surface congruence. Fractures were then stabilized using resorbable PLGA pins, and then a PDS loop was applied to achieve adequate compression. After surgery, the operated limb was restrained in a cast for three weeks, followed by active physiotherapy to facilitate the swiftest recovery of function.
No complications were observed during the follow-up examinations. There was no sign of irritation, in any of the children, which is often observed with metal implants. At the one-year follow-up, all three children showed complete functional and radiological healing of the fractures, with good joint congruence and minimal scarring.
Several limitations restrict the general applicability of this trial. Statistical tests could not be run, due to not meeting the participant limit criteria. Nevertheless, due to the obsoleteness of the second, metal removal surgeries, it can be stipulated, that the benefits of resorbable implants when employed in other regions are similarly applicable to coronoid fractures. Clinically, advantages such as reduction in surgery-related complications (e.g., bleeding, infection, scarring, and nerve damage), average narcosis, ionizing-radiation exposure, and hospitalization duration, stress levels, along with the related total costs of the procedures were observed during the investigation period, but could not be statistically proven, due to the lack of a control group and low number of participants. As the trial was conducted in a single regional center, with only Caucasian and male participants, socio-economic, racial, and gender bias may be present. Therefore, greater population, at least single-blinded, randomized controlled trials (RCTs) are needed to further substantiate the qualities and constraints of resorbable implants for pediatric olecranon fractures.
Granting no far-reaching conclusions can be drawn from the results of these three instances, the presented cases focus on the potential of using a new method for treating pediatric and adolescent olecranon fractures in a more comfortable manner.
5. Conclusion
Management of pediatric olecranon fractures requires careful consideration of both immediate fracture stabilization and long-term outcomes. Bioresorbable PLGA implants and PDS loops represent a promising approach, offering the benefit of eliminating the need for removal surgery, which is a significant advantage in a growing child by reducing anesthetic and imaging radiation dosages, discomfort, hospitalization length, and financial burden related to an additional operation. However, their use must be weighed against concerns related to, strength, resorption rates, high initial costs, and surgical expertise required due to visualization difficulties. Ultimately, a personalized treatment plan that considers the individual needs of the child, the nature of the fracture, and the available resources will ensure the best outcomes for these patients.
Author Contributions
Conceptualization, A.L., G.J., M.V., T.K. and Z.T.; methodology, A.G.L., E.A., and Z.T.; validation, A.G.L., E.A., H.N., G.J., T.M. and Z.T.; formal analysis, A.L., A.G.L. and Z.T. ; investigation, A.G.L., E.A., G.J., T.M. and Z.T.; resources, G.J. and Z.T.; data curation, A.G.L., E.A., H.N.; writing—original draft preparation, A.L., G.J. and Z.T.; writing—review and editing, A.L., A.G.L., E.A., H.N., G.J., M.V., T.K., T.M., and Z.T; visualization, A.L., A.G.L., H.N., M.V. and T.K; supervision, G.J., M.V., T.K. and Z.T.; project administration, A.L., G.J., M.V. and T.K.; funding acquisition, G.J., M.V., and T.K. All authors have read and agreed to the published version of the manuscript. The authors are in agreement to be accountable for all aspects of the work in ensuring that questions related to the accuracy or integrity of any part of the work are appropriately investigated and resolved.
Institutional Review Board Statement
The study was conducted according to the guidelines of the Declaration of Helsinki and approved by the Regional Research Ethics Committee, Clinical Complex, University of Pécs (Pécsi Tudományegyetem, Klinikai Komplex, Regionális és Intézményi Kutatás-Etikai Bizottság) on 23 April 2021 (8737-PTE2021).
Informed Consent Statement
Informed consent was obtained from all subjects involved in the study. Written informed consent has been obtained from the patient’s guardians to publish this paper.
Data Availability Statement
Data is contained within the article.
Acknowledgements
We would like the thank the healthcare personnel of every Pediatric Hospital for their rigorous and conscientious efforts.
Conflicts of Interest
The authors declare no conflict of interest.
References
- Perkins, C.A.; Busch, M.T.; Christino, M.A.; Axelrod, J.; Devito, D.P.; Fabregas, J.A.; Flanagan, J.C.; Murphy, J.; Olszewski, D.; Schmitz, M.L.; et al. Olecranon Fractures in Children and Adolescents: Outcomes Based on Fracture Fixation. J. Child. Orthop. 2018, 12, 497–501. [Google Scholar] [CrossRef] [PubMed]
- Caterini, R.; Farsetti, P.; D’Arrigo, C.; Ippolito, E. Fractures of the Olecranon in Children. Long-Term Follow-up of 39 Cases. J. Pediatr. Orthop. Part B 2002, 11, 320–328. [Google Scholar] [CrossRef]
- Holme, T.J.; Karbowiak, M.; Arnander, M.; Gelfer, Y. Paediatric Olecranon Fractures: A Systematic Review. EFORT Open Rev. 2020, 5, 280–288. [Google Scholar] [CrossRef]
- De Maio, F.; Gorgolini, G.; Caterini, A.; Luciano, C.; Covino, D.; Farsetti, P. Treatment of Olecranon Fractures in Childhood: A Systematic Review. Front. Pediatr. 2022, 10, 1046243. [Google Scholar] [CrossRef] [PubMed]
- Sullivan, C.W.; Herron, T.; Hayat, Z. Olecranon Fracture. In StatPearls; StatPearls Publishing: Treasure Island, FL, USA, 2025. [Google Scholar]
- Horne, J.G.; Tanzer, T.L. Olecranon Fractures: A Review of 100 Cases. J. Trauma 1981, 21, 469–472. [Google Scholar]
- Morrey, B.F. Current Concepts in the Treatment of Fractures of the Radial Head, the Olecranon, and the Coronoid. JBJS 1995, 77, 316. [Google Scholar] [CrossRef]
- Joeris, A.; Lutz, N.; Blumenthal, A.; Slongo, T.; Audigé, L. The AO Pediatric Comprehensive Classification of Long Bone Fractures (PCCF). Acta Orthop. 2017, 88, 129–132. [Google Scholar] [CrossRef]
- Iyer, R.S.; Thapa, M.M.; Khanna, P.C.; Chew, F.S. Pediatric Bone Imaging: Imaging Elbow Trauma in Children???A Review of Acute and Chronic Injuries. Am. J. Roentgenol. 2012, 198, 1053–1068. [Google Scholar] [CrossRef]
- DeFroda, S.F.; Hansen, H.; Gil, J.A.; Hawari, A.H.; Cruz, A.I. Radiographic Evaluation of Common Pediatric Elbow Injuries. Orthop. Rev. 2017, 9, 7030. [Google Scholar] [CrossRef]
- Fujihara, Y.; Tatebe, M.; Fujihara, N.; Tanaka, H.; Hirata, H. Useful Plain Radiographic Findings in Diagnosis of Pediatric Olecranon Fracture Complicated With Proximal Radial Fracture. Pediatr. Emerg. Care 2017, 33, e105. [Google Scholar] [CrossRef]
- Cheng, J.C.; Wing-Man, K.; Shen, W.Y.; Yurianto, H.; Xia, G.; Lau, J.T.; Cheung, A.Y. A New Look at the Sequential Development of Elbow-Ossification Centers in Children. J. Pediatr. Orthop. 1998, 18, 161–167. [Google Scholar] [CrossRef] [PubMed]
- Khong, P.-L.; Ringertz, H.; Donoghue, V.; Frush, D.; Rehani, M.; Appelgate, K.; Sanchez, R.; ICRP. ICRP Publication 121: Radiological Protection in Paediatric Diagnostic and Interventional Radiology. Ann. ICRP 2013, 42, 1–63. [Google Scholar] [CrossRef]
- Chalidis, B.E.; Sachinis, N.C.; Samoladas, E.P.; Dimitriou, C.G.; Pournaras, J.D. Is Tension Band Wiring Technique the “Gold Standard” for the Treatment of Olecranon Fractures? A Long Term Functional Outcome Study. J. Orthop. Surg. 2008, 3, 9. [Google Scholar] [CrossRef] [PubMed]
- Müller, M.E.; Allgöwer, M.; Schneider, R.; Willenegger, H. Manual der OSTEOSYNTHESE: AO-Technik; Springer-Verlag, 2013. ISBN 978-3-642-87407-9.
- Weber, B.G.; Vasey, H. [OSTEOSYNTHESIS IN OLECRANON FRACTURES]. Z. Unfallmedizin Berufskrankh. Rev. Med. Accid. Mal. Prof. 1963, 56, 90–96. [Google Scholar]
- Rowland, S.A.; Burkhart, S.S. Tension Band Wiring of Olecranon Fractures. A Modification of the AO Technique. Clin. Orthop. 1992, 238–242. [Google Scholar]
- Paremain, G.P.; Novak, V.P.; Jinnah, R.H.; Belkoff, S.M. Biomechanical Evaluation of Tension Band Placement for the Repair of Olecranon Fractures. Clin. Orthop. 1997, 325–330. [Google Scholar] [CrossRef]
- Javier Martínez Romero; André Miran; Claus Hjorth Jensen Complications and Re-Operation Rate after Tension-Band Wiring of Olecranon Fractures. J. Orthop. Sci. 2000, 318–320. [CrossRef]
- Gortzak, Y.; Mercado, E.; Atar, D.; Weisel, Y. Pediatric Olecranon Fractures: Open Reduction and Internal Fixation with Removable Kirschner Wires and Absorbable Sutures. J. Pediatr. Orthop. 2006, 26, 39–42. [Google Scholar] [CrossRef]
- Crozier-Shaw, G.; Mahon, J.; Bayer, T.C. The Use of Bioabsorbable Compression Screws & Polyethylene Tension Band for Fixation of Displaced Olecranon Fractures. J. Orthop. 2020, 22, 525–529. [Google Scholar] [CrossRef]
- Eppley, B.L.; Reilly, M. Degradation Characteristics of PLLA-PGA Bone Fixation Devices. J. Craniofac. Surg. 1997, 8, 116. [Google Scholar] [CrossRef]
- Perhomaa, M.; Pokka, T.; Korhonen, L.; Kyrö, A.; Niinimäki, J.; Serlo, W.; Sinikumpu, J.-J. Randomized Controlled Trial of the Clinical Recovery and Biodegradation of Polylactide-Co-Glycolide Implants Used in the Intramedullary Nailing of Children’s Forearm Shaft Fractures with at Least Four Years of Follow-Up. J. Clin. Med. 2021, 10, 995. [Google Scholar] [CrossRef] [PubMed]
- Kassai, T.; Varga, M.; Józsa, G. Pediatric Medial Humeral Epicondyle Fracture in Children: Are Biodegradable Pins with Tension Band Absorbable Sutures Efficient? Medicine (Baltimore) 2022, 101, e29817. [Google Scholar] [CrossRef]
- Matthews, J.G. Fractures of the Olecranon in Children. Injury 1980, 12, 207–212. [Google Scholar] [CrossRef]
- Newell, R.L. Olecranon Fractures in Children. Injury 1975, 7, 33–36. [Google Scholar] [CrossRef] [PubMed]
- Mun, F.; Suresh, K.V.; Hayashi, B.; Margalit, A.; Sponseller, P.D.; Lee, R.J. Compression Screw Fixation for Pediatric Olecranon Fractures. J. Pediatr. Orthop. 2023, 43, e151. [Google Scholar] [CrossRef] [PubMed]
- INUI, A.; KURODA, T.; KUROSAWA, T.; KOKUBU, T.; MIFUNE, Y.; NISHIMOTO, H.; KURODA, R. Case Series of Comminuted Olecranon Fracture Treated by Plate Fixation; Do We Have to Remove the Plate? Kobe, J. Med. Sci. 2018, 64, E115–E118. [Google Scholar]
- Gaddy, B.C.; Strecker, W.B.; Schoenecker, P.L. Surgical Treatment of Displaced Olecranon Fractures in Children. J. Pediatr. Orthop. 1997, 17, 321–324. [Google Scholar] [CrossRef]
- Yang, W.; Zhang, X.; Sun, D.; Jin, S.; Chen, J.; Li, Y. Outcomes of Olecranon Fractures in Adolescents: Comparison of Tension Band Wiring and Herbert Screw Fixations. Front. Pediatr. 2024, 11. [Google Scholar] [CrossRef]
|
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2025 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (http://creativecommons.org/licenses/by/4.0/).