1. Introduction
The International Continence Society defines normal pelvic floor muscle contraction as the ability to contract and relax the pelvic floor muscles in a controlled manner [
1,
2]. Studies indicate that women, even if they have received detailed education about the pelvic floor, have difficulty distinguishing pelvic floor muscle contractions from other muscle contractions. Therefore, it is emphasized that women are often unsure whether they are contracting these muscles correctly [2-4]. Studies in the literature highlight that both asymptomatic women and those with Pelvic Floor Dysfunction (PFD) have low success rates in voluntary muscle contractions. It is also mentioned that being able to contract the pelvic floor muscles correctly is as important as the muscle strength itself [
4]. Thompson et all [
5] have stated that 23% of women perform pelvic floor muscle exercises incorrectly and that pelvic floor muscle contraction should be individually assessed by a healthcare professional experienced in this area. During pelvic floor muscle contraction, some common mistakes can be observed. These mistakes include contracting the abdominal muscles, hip adductor muscles, or gluteal muscles, stop breathing, enhanced inhaling, pelvic tilt and straining [
2,
6].
A study in the literature has coined the term COMMOV for "C"ontractions of "O"ther "M"uscles (m. rectus abdominus, the gluteal muscles, and the adductors), and other "MOV"ements (pelvic tilt, breath holding, and straining) [
6].
Although pelvic floor muscle training is recommended as a first-line treatment [
7], studies on pelvic floor muscle contraction training techniques are limited. This situation leads to difficulties for physiotherapists in choosing the therapeutic methods they would prefer. In the literature, individuals are provided with muscle contraction training through various assessment methods to help them acquire motor skills [8-10].
Motor learning, which involves the long-term acquisition of motor skills, can occur in various ways. In the execution of a motor skill, focusing on the body movements of the individual is defined as internal focus, while focusing on the effect of the movement with the help of any device or tool is defined as external focus. External focus facilitates the automation of the movement by shortening the initial stages of learning. Thus, it is assumed that the learning process is shortened (constrained action hypothesis). As a result, less fatigue and better endurance against stress are achieved. Studies have shown that external focus leads to better learning and improved performance, while the effects of internal focus are found to be less significant [
11,
12]. A large-scale meta-analysis has also reported that external focus is superior to internal focus[
13]. In designing our study, we aimed to investigate pelvic floor muscle contraction training with verbal instructions as internal focus, while examining pelvic floor muscle contraction training using digital vaginal palpation and a perineometer device as external focus. Additionally, we intended to explore the effects of different types of focus on motor learning.
To the best of our knowledge, there are no studies in the literature that thoroughly investigate the effects of different teaching methods used in pelvic floor muscle contraction training (PFMCT) on common errors. The aim of this study was to compare the effects of verbal instruction-based PFMCT, DVP-based PFMCT, and perineometer-based PFMCT, and to examine their impact on common errors that occur during pelvic floor muscle contraction.
2. Materials and Methods
2.1. Design and Participants
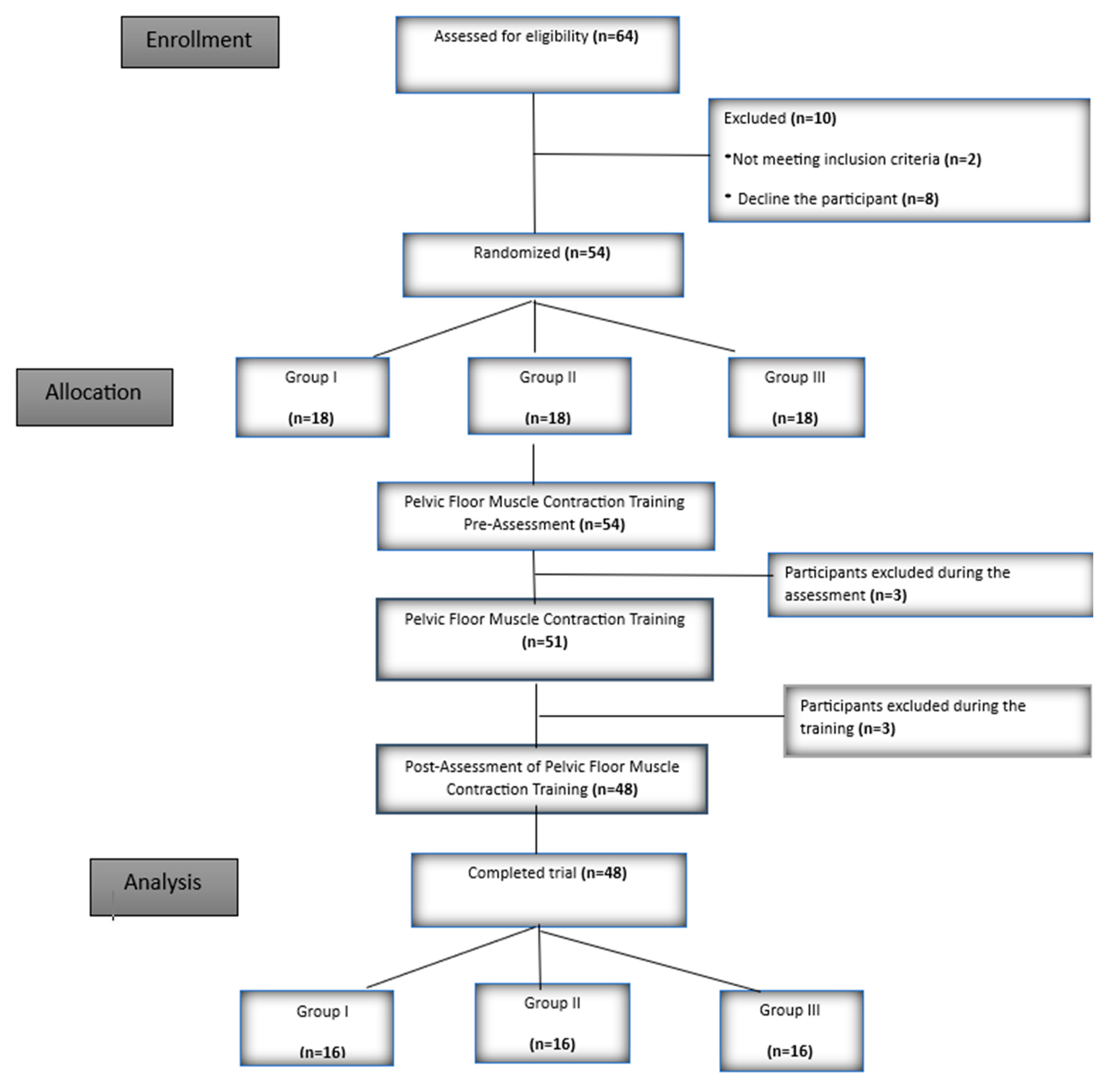
This study is a randomized controlled, single-center study. Participants were selected from women attending routine check-ups at a gynecology clinic affiliated with the university. Out of 64 women who visited the clinic, 48 women who volunteered and met the inclusion criteria were included in the study. The study protocol was approved by the Ethics Committee (no: 2023/437) and registered on ClinicalTrials.gov (ID: NCT06306703). Participants were informed about the study in accordance with the principles outlined in the Helsinki Declaration, and each participant was asked to read and sign an informed consent form. Additionally, this study was financially supported by TÜBİTAK (The Scientific and Technological Research Council of Turkey) 1002A Rapid Support Program (no: 224S541). This study was produced as part of a doctoral thesis.
The inclusion criteria were as follows: being a woman between the ages of 20 and 50, volunteering to participate in the study, scoring 25 or higher on the Mini Mental Test, having the ability to perform pelvic floor muscle contractions (>2 points according to MOS), and not having previously received pelvic floor muscle contraction training. Women who were pregnant, had stage ≥3 symptomatic pelvic organ prolapse, had communication problems, could not cooperate, had a urinary tract infection, epilepsy, or associated neurological disorders were excluded from the study.
2.2. Randomization
Participants were equally assigned to each group using a computer-based block randomization procedure prepared by an independent researcher who was not involved in the study.
2.3. Assessments
To assess the participants' cognitive adequacy, the Mini Mental Test [
14,
15] was first administered, and those who scored 25 or higher were included in the study. Demographic, physical, and obstetric information of the participants was then collected. Following this, participants were assessed prior to pelvic floor muscle contraction training (PFMCT). To ensure complete relaxation of the pelvic floor muscles, reduce the effects of gravity, and eliminate accessory muscles such as the hip adductors, participants were positioned supine with their knees approximately 140° flexed, thighs and feet about 30 cm apart, and the soles of their feet in contact with the bed.
2.3.1. Assessment of Pelvic Floor Muscle Strength with DVP Before PFMCT
Pelvic floor muscle strength with digital vaginal palpation (DVP) was assessed using the Modified Oxford Scale (MOS) [
16]. The physiotherapist inserted their index and middle fingers into the participant's vagina approximately 3 to 5 centimeters (cm). During the procedure, the participant was instructed, "Tighten strongly around the fingers that I have placed in your vagina." The participants were instructed to squeeze three times, and the highest value obtained was recorded [17-19].
2.3.2. Assessment of Pelvic Floor EMG Muscle Activation Before PFMCT
The EMG activity of the participants' pelvic floor muscles was assessed using an intravaginal EMG probe (Everyway Medical Instruments Co.) connected to the NeuroTrac® Myo Plus Pro device (Verity Medical, Hampshire, UK). The NeuroTrac Software 5.1.1 was used to link the device to the computer. The EMG reference cable was placed with a surface electrode on the participant’s right thigh. Participants were instructed to "contract and relax the muscles you use to hold urine." The peak values of maximum voluntary contractions were recorded in microvolts (μV). Measurements were repeated three times, with 5 seconds of contraction followed by 5 seconds of relaxation [
7,
20,
21].
2.3.3. Assessment of Errors During PFMCT and Before PFMCT
Six potential errors during pelvic floor muscle contraction (PFMC) were evaluated. These errors were examined using the error and observation methods described by Bø et al.[
2]. To specifically assess the co-contraction of abdominal muscles during PFMC, an EMG-BF device was used instead of visual observation. All error recordings were made while participants were performing PFMC.
For tracking the contraction of abdominal muscles, the electrical activity in the obliquus internus abdominis and transversus abdominis muscles was recorded by placing surface electrodes on the medial aspect of the anterior superior iliac spines. During the measurement, the passive electrode was placed on the participant's right thigh. The EMG NeuroTrac® Myo Plus Pro device (Verity Medical, Hampshire, UK) was used for evaluation [
22]. The co-contraction of the abdominal muscles during PFMC was recorded as peak values in microvolts (μV).
Contractions of the hip adductor muscles were monitored by the physiotherapist placing her hand on the adductor muscles. The test was considered positive if a contraction was felt in the inner thigh muscles or if the legs moved closer together. Gluteal muscle contraction was determined by observing the participant’s movement of squeezing and lifting their hips off the bed. Enhanced inhaling was identified when the participant took a deep breath during PFMC, causing the chest to rise excessively during inspiration. Stop breathing was determined by observing the participant closing their mouth and holding their breath. Straining was recorded when the therapist's fingers or the perineometer probe were pushed during the procedure [
2].
2.4. Training
After the assessments, participants were provided with similar training regardless of the group they were assigned to. The training included detailed presentations on pelvic floor anatomy and function, pelvic floor dysfunction (PFD), risk factors, the relationship between posture and pelvic floor function, importance of diaphragmatic breathing, and pelvic floor muscle training. Additionally, visual materials and videos were used during the training. Pelvic floor contraction and relaxation techniques were explained according to the group to which the participants were assigned.
In Group I, participants received verbal instruction only, without any tactile or visual biofeedback.
In Group II, participants were trained using Digital Vaginal Palpation (DVP), where the physiotherapist placed her index and middle fingers into the participant's vagina.
In Group III, an intravaginal probe of a perineometer device (Peritron 9300 perineometer-Laborie, Mississauga, ON, Canada) was placed in the participants' vaginas. The display section of the device was handed to the participant [
23]. This allowed for visual biofeedback through numerical values generated by the contraction and relaxation of the pelvic floor muscles.
2.5. Post-PFMCT Assessments
After the pelvic floor muscle contraction training (PFMCT), the assessments were repeated. These included the evaluation of muscle strength using Digital Vaginal Palpation (DVP) (MOS), the assessment of pelvic floor muscle activation (EMG-BF), and the evaluation of errors during pelvic floor muscle contraction (PFMC).
2.6. Sample Size Estimation
The sample size was calculated using the G-Power 3.1.9.4 program, taking into account the significance level of the hypothesis and the effect size. The effect size of 0.47, obtained from the reference study [
24] was used. To detect a significant difference in the study, with α=0.05 and 1-β=0.80, the sample size for each group was calculated to be a minimum of 16 participants (total of 48 women) with 80% power.
2.7. Statistical Analysis
The data were analyzed using SPSS 25.0 (IBM SPSS Statistics 25 software, Armonk, NY: IBM Corp.). Continuous variables were presented as mean ± standard deviation, median (range), and categorical variables as frequency and percentage. The normality of the data was assessed using the Shapiro-Wilk test. When the assumptions of parametric tests were met, independent group differences were compared using one-way analysis of variance (post hoc: Tukey test). When the assumptions of parametric tests were not met, independent group differences were compared using the Kruskal-Wallis variance analysis (post hoc: Bonferroni-corrected Mann-Whitney U test). Differences between categorical variables were examined using the Chi-square test. For pre- and post-training comparisons of categorical variables, the McNemar test was used. For continuous variables, when parametric test assumptions were met, dependent group differences were assessed using the paired t-test, and when parametric assumptions were not met, the Wilcoxon signed-rank test was used. A p-value of <0.05 was considered statistically significant in all analyses.
3. Results
The study took place between March 1, 2024 and June 15, 2024. 48 participants completed the trial, with Group I (n=16), Group II (n=16), and Group III (n=16) (
Figure 1).
3.1. Baseline Characteristics
The demographic, physical, and obstetric characteristics, educational status, and type of delivery of the participants in the study were similar (p> 0.05) (
Table 1).
3.2. Pelvic Floor Muscle Strength and Activation Values
The change in MOS values after training significantly increased in the second and third groups (p<0.05), while the increase in MOS values in the group trained with verbal instructions was not statistically significant (p>0.05). According to the results of muscle activation data assessed with vaginal BF-EMG; only in the second group, the muscle contraction value significantly increased after training (p<0.05), while no significant difference was found in the other groups (p>0.05) (
Table 2).
3.3. The Amount of Errors and Abdominal Muscle Activation Values
When looking at the amount of errors after training, a decrease was observed in all three groups (p<0.05), but there was no significant difference between the groups (p>0.05). According to the BF-EMG data of abdominal muscle contraction during PFMC, a decrease in abdominal muscle contraction values was found in the second group after training (p<0.05), while an increase was observed in the other groups, but no statistically significant difference was found (p>0.05) (
Table 3).
3.4. Between-group Comparison of Errors
There was no significant difference between the groups in the comparison of incorrect movements were made during PFMC (p>0.05).
Table 4.
Between-group Comparison of Errors Made During PFMC.
Table 4.
Between-group Comparison of Errors Made During PFMC.
| |
|
Group I |
Group II |
Group III |
Between-group (p) |
| Addcont Pre-T |
Yes |
10 (%62,5) |
10 (%62,5) |
7 (%43,8) |
0,467 (χ²=1,524) |
| No |
6 (%37,5) |
6 (%37,5) |
9 (%56,3) |
| Addcont Post-T |
Yes |
1 (%6,3) |
2 (%12,5) |
3 (%18,8) |
0,552 (χ²=1,189) |
| No |
15 (%93,8) |
14 (%87,5) |
13 (%81,3) |
| Glcont Pre-T |
Yes |
11 (%68,8) |
9 (%56,3) |
11 (%68,8) |
0,695 (χ²=0,729) |
| No |
5 (%31,3) |
7 (%43,8) |
5 (%31,3) |
| Glcont Post-T |
Yes |
2 (%12,5) |
3 (%18,8) |
3 (%18,8) |
0,855 (χ²=0,312) |
| No |
14 (%87,5) |
13 (%81,3) |
13 (%81,3) |
| SB Pre-T |
Yes |
4 (%25) |
4 (%25) |
5 (%31,3) |
0,901 (χ²=0,208) |
| No |
12 (%75) |
12 (%75) |
11 (%68,8) |
| SB Post-T |
Yes |
0 (%0) |
2 (%12,5) |
2 (%12,5) |
0,181 (χ²=3,423) |
| No |
16 (%100) |
14 (%87,5) |
14 (%87,5) |
| EI Pre-T |
Yes |
1 (%6,3) |
2 (%12,5) |
3 (%18,8) |
0,552 (χ²=1,189) |
| No |
15 (%93,8) |
14 (%87,5) |
13 (%81,3) |
| EI Post-T |
Yes |
0 (%0) |
1 (%6,3) |
0 (%0) |
0,326 (χ²=2,24) |
| No |
16 (%100) |
15 (%93,8) |
16 (%100) |
| St Pre-T |
Yes |
4 (%25) |
2 (%12,5) |
2 (%12,5) |
0,564 (χ²=1,146) |
| No |
12 (%75) |
14 (%87,5) |
14 (%87,5) |
| St Post-T |
Yes |
1 (%6,3) |
1 (%6,3) |
3 (%18,8) |
0,433 (χ²=1,673) |
| No |
15 (%93,8) |
15 (%93,8) |
13 (%81,3) |
3.5. Within-Group Comparison of Errors
The error in adductor muscle contraction decreased in the first and second groups (p<0.05), while gluteal muscle contraction decreased in all three groups (p<0.05). In the first group, no "yes" responses were observed for breath holding, so statistical tests could not be performed. In the second and third groups, no significant difference was found (p>0.05). In the first and third groups, hyperventilation did not occur in the participants, so statistical tests could not be performed. In the second group, no significant difference was found (p>0.05). In terms of straining, no within-group differences were found in any group (p>0.05) (
Table 5).
3.6. Statistical Power Analysis
Our study was conducted with 48 women (16 women per group). When examining the power analysis based on the error rates obtained after the training, a medium effect size (F=0.458) was found between the groups. For this effect size, it was determined that our study achieved 81% power at a 95% confidence level. Additionally, when examining the power levels for the pre-training and post-training error rates in the groups, strong effect sizes were observed in all groups (Group 1: dz=1.121; Group 2: dz=0.895; Group 3: dz=1.139).When the power of these changes was examined, it was found that the first group achieved 98.6% power, the second group achieved 91.7%, and the third group achieved 98.9% power.
4. Discussion
In our study, it was found that both perineometer and DVP (assessed with MOS) were equally effective in teaching PFMC, while all three techniques were effective in reducing incorrect movements. Additionally, in the EMG-BF measurements, it was found that only the DVP technique reduced abdominal contraction and significantly increased pelvic floor muscle activation values. As far as we know, this study is the first randomized controlled trial comparing methods for teaching PFMC and evaluating which technique is more effective in reducing errors made by women during these trainings.
Studies have reported that pelvic health and women's health physiotherapists experience uncertainty about which method to use in clinical practice and research. Many PFMCT protocols have been used in the literature, but there is no consensus on a standard method. Furthermore, the errors (during PFMCT) have not been adequately assessed from both objective and subjective perspectives [
4].
In one study, women were given only verbal instructions during the first week postpartum, and their PFMCs were assessed observationally. While 29% of the participants were unable to perform any PFMCs, 24% exhibited insufficient contractions. However, after the verbal instructions were given, the correct PFMC performance rate increased to 73.6% [
25]. In our study, although comprehensive training was provided beforehand, no significant increase was observed in terms of MOS values and muscle activation data measured with BF-EMG in Group I. The difference between our study and the literature may be due to the fact that we used different and more objective evaluation methods.In a systematic review examining different physiotherapy methods for facilitating PFMC, vaginal palpation is recommended for correct PFMC due to the simultaneous feedback provided by the therapist and the stimulation through tactile stimulation [
4]. Thus, it has been reported that an interactive approach can encourage individuals' participation and learning [
10]. In our study, the increase in the MOS values observed in PFMC in Group II may be a result of the training method applied with this stimulation technique, supporting the literature.
The evaluation of pelvic floor muscles using surface electrodes placed on the perineum may be influenced by the activity of other muscles, such as the gluteal muscles, obturator muscles, or anal sphincter, making it not an ideal assessment method. To assess pelvic floor muscle activation more accurately and objectively, an intravaginal probe is used due to its proximity to the vagina [
26]. In our study, we assessed the participants' pelvic floor muscle activation using EMG-BF with an intravaginal probe. According to the results we obtained, a significant increase in muscle activation values was observed in Group II (which received training only with DVP). This result supports the view that sensory stimulation provided through vaginal palpation may lead to more effective outcomes in training.
During internal focus, individuals tend to disrupt automatic control processes while trying to consciously control their movements. When the focus is on the effect of the movement, automatic reflex-type control can occur. This allows for the control of unconscious, involuntary movements while promoting more effective and efficient movements. Studies have indicated that external focus enhances learning, while internal focus does not negatively affect learning [
11]. In our study, we obtained more effective results with the training provided using external focus. While with internal focus, we only observed a reduction in 5 incorrect movements. This suggests that, although training can have positive effects in both cases, the impact generated through external focus is greater.
In our study, we addressed a total of 6 incorrect movements. Five of these incorrect movements were assessed through inspection or palpation. To objectively determine the coactivation of abdominal muscles during PFMC, we preferred to use EMG-BF. For other muscles, since we did not have a multi-channel device to assess them simultaneously, we controlled them using palpation and inspection techniques. The core region is a three-dimensional cylindrical structure composed of the abdominal muscles in the front, paraspinal muscles in the back, oblique muscles on the sides, the diaphragm at the top, and the pelvic floor muscles at the bottom. These muscles respond to postural changes and external loads to maintain the body's mechanical stability. EMG studies in the literature have shown that the pelvic floor muscles contribute to stabilization by contracting simultaneously with the transversus abdominis and diaphragm muscles [
27]. While it is emphasized in the literature that abdominal muscles should relax during PFMC, performing the correct PFMC that activates the deep abdominal muscles without causing an increase in intra-abdominal pressure can be challenging. Additionally, it has been found that completely eliminating abdominal muscle activity reduces voluntary contraction of the pelvic floor muscles by 25%. Therefore, controlling and minimizing abdominal muscle activity during PFMC is important. Neumann and Gill found that it is not possible for women to fully contract their PFM without also contracting their transversus abdominis and internal oblique muscles[
28]. They found that maximum PFM contraction could not be achieved without an increase in EMG activity in the lower part of the rectus abdominis [
29]. Based on these findings, we observed a reduction in abdominal muscle contraction with training provided using only the DVP technique. This result suggests that, in terms of error rates, DVP is more effective than the other techniques.
Pinheiro et al. emphasized that correct muscle contraction is as important as muscle strength itself and reported that 90% of the participants initially used accessory muscles. However, after the training, 90% of these women stopped using these muscles [
6,
10] found that 216 out of 386 women (57%) contracted at least one other muscle group simultaneously during PFMC. Among these women, the most common muscle contractions were abdominal muscle contraction (n = 131; 35%), breath-holding (n = 123; 33%), and gluteal muscle contraction (n = 84; 22%). In our study, before the training, we found the adductor error to be 62.5% in Group I, 62.5% in Group II, and 43.8% in Group III; gluteal error to be 68.8% in Group I, 56.3% in Group II, and 68.8% in Group III; and breath-holding to be 25% in Group I, 25% in Group II, and 31.3% in Group III. Based on these data, among the five categories, gluteal muscle co-contraction, adductor muscle co-contraction, and breath-holding were the most commonly observed errors. These results suggest that greater attention should be given to these areas during PFMT, as post-training, the values for these errors decreased significantly.
Our study had some limitations. One of the first limitations was that the physiotherapist administering the assessment and training could not be blinded to the treatment groups. To minimize the impact of this on the evaluation results, objective measurements were utilized in this study. Another limiting factor could be the use of a single-channel EMG-BF device, which only allowed for the evaluation of abdominal muscles. In future studies, we recommend evaluating other muscles with EMG-BF as well. Despite these limitations, the randomized controlled design, and the use of both objective and subjective measurements are strengths of our study. This study, which highlights the importance of treatment planning in healthcare and the necessity of error-free pelvic floor muscle training, is the first to compare three different PFMCTs. Teaching and maintaining movement through feedback methods and providing proprioceptive input is crucial. Proprioceptive information can facilitate both the learning process of movement and the continuation of learned motor behaviors. The feedback methods we used in our study were also one of our strengths.
5. Conclusions
In our study, we observed that digital vaginal palpation (DVP), which does not require additional costs, special equipment, and is practical to apply, contributed to a reduction in incorrect movements and the formation of stronger pelvic floor muscle contractions during PFMCT. This is the first study supporting the use of DVP in training, which can easily be implemented in clinical settings. These results also emphasize the importance of evaluating incorrect movements during PFMCT. Future research will help develop more comprehensive strategies to improve pelvic floor health through these training methods. Planning follow-up studies with a duration of at least 3 months to assess the long-term effects of the training will provide valuable insights into the literature on this topic.
Author Contributions
Conceptualization and design of the study: D.S.-Ö., T.-A.; data curation, D.S.-Ö., T.-A., F.-K.H.; formal analysis, D.S.-Ö., T.-A; investigation: all; methodology: D.S.-Ö., T.-A, F.-K.H.; supervision: T.-A., H.-D., writing—original draft: D.S.-Ö., T.-A., H.-D.; writing—review and editing: all. All authors have read and agreed to the published version of the manuscript.
Funding
This research has received funding financially supported by TÜBİTAK (The Scientific and Technological Research Council of Turkey) 1002A Rapid Support Program (224S541).
Institutional Review Board Statement
The research protocol was approved by the local Ethics Committee The study protocol was approved by the Ethics Committee (no: 2023/437) (Necmettin Erbakan University, Health Sciences Scientific Research Ethics Committee, Konya). The research was conducted according to the Declaration of Helsinki and its later amendments. It has been registered on ClinicalTrials.gov under the ID: NCT06306703.
Informed Consent Statement
All the participants signed a written informed consent form.
Data Availability Statement
The datasets used and/or analyzed during the current study are available from the corresponding author upon reasonable request, due to ethical committee restrictions.
Acknowledgments
The authors thank all the participants in this study.
Conflicts of Interest
The authors declare that they have no conflicts of interests.
References
- Talasz, H.; Kofler, M.; Kalchschmid, E.; Pretterklieber, M.; Lechleitner, M. Breathing with the pelvic floor? Correlation of pelvic floor muscle function and expiratory flows in healthy young nulliparous women. Int Urogynecol J 2010, 21, 475–481. [Google Scholar] [CrossRef] [PubMed]
- Bø, K.; Berghmans, B. Evidence-Based Physical Therapy for the Pelvic Floor bridging science and clinical practice (Second Edition); Elsevier Churchill Livingstone, 2015. [Google Scholar] [CrossRef]
- Fitz, F.F.; Paladini, L.M.; Ferreira, L.d.A.; Gimenez, M.M.; Bortolini, M.A.T.; Castro, R.A. Ability to contract the pelvic floor muscles and association with muscle function in incontinent women. International urogynecology journal 2020, 31, 2337–2344. [Google Scholar] [CrossRef]
- Mateus-Vasconcelos, E.C.L.; Ribeiro, A.M.; Antonio, F.I.; Brito, L.G.d.O.; Ferreira, C.H.J. Physiotherapy methods to facilitate pelvic floor muscle contraction: A systematic review. Physiotherapy theory and practice 2018, 34, 420–432. [Google Scholar] [CrossRef]
- Thompson, J.A.; O'Sullivan, P.B.; Briffa, N.K.; Neumann, P. Assessment of voluntary pelvic floor muscle contraction in continent and incontinent women using transperineal ultrasound, manual muscle testing and vaginal squeeze pressure measurements. Int Urogynecol J Pelvic Floor Dysfunct 2006, 17, 624–630. [Google Scholar] [CrossRef] [PubMed]
- Neels, H.; De Wachter, S.; Wyndaele, J.-J.; Van Aggelpoel, T.; Vermandel, A. Common errors made in attempt to contract the pelvic floor muscles in women early after delivery: A prospective observational study. European Journal of Obstetrics & Gynecology and Reproductive Biology 2018, 220, 113–117. [Google Scholar]
- Brækken, I.H.; Villumstad, T.K.; Evensen, N.M. Randomised controlled pilot trial to assess effect of electrical stimulation of weak pelvic floor muscles. Archives of Gynecology and Obstetrics 2024, 309, 2921–2929. [Google Scholar] [CrossRef]
- Dietz, H.; Wilson, P.; Clarke, B. The use of perineal ultrasound to quantify levator activity and teach pelvic floor muscle exercises. International urogynecology journal 2001, 12, 166–169. [Google Scholar] [CrossRef]
- Fine, P.; Burgio, K.; Borello-France, D.; Richter, H.; Whitehead, W.; Weber, A.; Brown, M.; Network, P.F.D. Teaching and practicing of pelvic floor muscle exercises in primiparous women during pregnancy and the postpartum period. American journal of obstetrics and gynecology 2007, 197, 107–e101. [Google Scholar] [CrossRef] [PubMed]
- Pinheiro, B.d.F.; Franco, G.R.; Feitosa, S.M.; Yuaso, D.R.; Castro, R.d.A.; Girão, M.J.B.C. Physiotherapy for perineal consciousness: A comparison between pelvic floor muscle training alone and with biofeedback. Fisioterapia em Movimento 2012, 25, 639–648. [Google Scholar] [CrossRef]
- Zachry, T.; Wulf, G.; Mercer, J.; Bezodis, N. Increased movement accuracy and reduced EMG activity as the result of adopting an external focus of attention. Brain research bulletin 2005, 67, 304–309. [Google Scholar] [CrossRef]
- Benjaminse, A.; Gokeler, A.; Dowling, A.V.; Faigenbaum, A.; Ford, K.R.; Hewett, T.E.; Onate, J.A.; Otten, B.; Myer, G.D. Optimization of the anterior cruciate ligament injury prevention paradigm: Novel feedback techniques to enhance motor learning and reduce injury risk. journal of orthopaedic & sports physical therapy 2015, 45, 170–182. [Google Scholar]
- Chua, L.K.; Jimenez-Diaz, J.; Lewthwaite, R.; Kim, T.; Wulf, G. Superiority of external attentional focus for motor performance and learning: Systematic reviews and meta-analyses. Psychol Bull 2021, 147, 618–645. [Google Scholar] [CrossRef] [PubMed]
- Folstein, M.F.; Folstein, S.E.; McHugh, P.R. “Mini-mental state”: A practical method for grading the cognitive state of patients for the clinician. Journal of psychiatric research 1975, 12, 189–198. [Google Scholar] [CrossRef] [PubMed]
- Güngen, C.; Ertan, T.; Eker, E.; Yaşar, R.; Engin, F. Standardize mini mental test’in Türk toplumunda hafif demans tan› s› nda geçerlik ve güvenilirliği. Türk Psikiyatri Dergisi 2002, 13, 273–281. [Google Scholar]
- Akbayrak, T.K.S. Kadın Sağlığında Fizyoterapi ve Rehabilitasyon; Hipokrat Kitabevi&Pelikan Kitabevi, 2016. [Google Scholar]
- Arranz-Martín, B.; García-Gallego, P.; Romay-Barrero, H.; Navarro-Brazález, B.; Martínez-Torres, C.; Torres-Lacomba, M. Bladder Base Displacement during Abdominal Muscles Contraction and Functional Activities in Primiparous Women Assessed by Transabdominal Ultrasound: A Descriptive Study. J Clin Med 2021, 11. [Google Scholar] [CrossRef]
- Iaocharoen, P.; Lekskulchai, O.; Chiengthong, K.; Bunyavejchevin, S.; Tanprasertkul, C.; Somprasit, C. The Correlations between Three Methods of Pelvic Floor Muscle Strength Assessment in Nulliparous Women: 2D Transperineal Ultrasound, Modified Oxford Scale, and PFX2® Perineometer. Asian Medical Journal and Alternative Medicine 2023, 23, 72–80. [Google Scholar]
- Porrón-Irigaray, A.; Rodríguez-López, E.S.; Acevedo-Gómez, M.B.; Ojedo-Martín, C.; Benito-de-Pedro, M. Coactivation of the Pelvic Floor and Gluteus Medius Muscles While Walking and Running in Female Runners. Sensors (Basel) 2024, 24, 1356. [Google Scholar] [CrossRef]
- Chmielewska, D.; Stania, M.; Sobota, G.; Kwaśna, K.; Błaszczak, E.; Taradaj, J.; Juras, G. Impact of different body positions on bioelectrical activity of the pelvic floor muscles in nulliparous continent women. BioMed research international 2015, 2015, 905897. [Google Scholar] [CrossRef]
- Kurtoglu, A.; Ciftci, R.; Car, B.; Konar, N. Investigation of Deltoid Muscle Activation From Different Angles in Body Building Athletes. The Medical Bulletin of Sisli Etfal Hospital 2023, 57, 410. [Google Scholar] [CrossRef]
- Navarro Brazález, B.; Sánchez Sánchez, B.; Prieto Gómez, V.; De La Villa Polo, P.; McLean, L.; Torres Lacomba, M. Pelvic floor and abdominal muscle responses during hypopressive exercises in women with pelvic floor dysfunction. Neurourology and urodynamics 2020, 39, 793–803. [Google Scholar] [CrossRef]
- Abe-Takahashi, Y.; Kitta, T.; Ouchi, M.; Okayauchi, M.; Chiba, H.; Higuchi, M.; Togo, M.; Shinohara, N. Reliability and validity of pelvic floor muscle strength assessment using the MizCure perineometer. BMC Women's Health 2020, 20, 1–7. [Google Scholar] [CrossRef] [PubMed]
- Şahin, Ü.K. Stres İnkontinansı Olan Kadınlarda Pelvik Taban Kas Eğitimine Ek Olarak Uygulanan Eksternal Elektrik Stimülasyonunun Etkileri. 2020.
- Vermandel, A.; De Wachter, S.; Beyltjens, T.; D’Hondt, D.; Jacquemyn, Y.; Wyndaele, J.J. Pelvic floor awareness and the positive effect of verbal instructions in 958 women early postdelivery. International urogynecology journal 2015, 26, 223–228. [Google Scholar] [CrossRef] [PubMed]
- Keshwani, N.; McLean, L. State of the art review: Intravaginal probes for recording electromyography from the pelvic floor muscles. Neurourol Urodyn 2015, 34, 104–112. [Google Scholar] [CrossRef] [PubMed]
- Kaçar, R. Effect of core muscle endurance on pain, posture and upper extremity function in upper strings players. Master's Thesis, Gazi Üniversitesi, 2024. [Google Scholar]
- Neumann, P.; Gill, V. Pelvic floor and abdominal muscle interaction: EMG activity and intra-abdominal pressure. Int Urogynecol J Pelvic Floor Dysfunct 2002, 13, 125–132. [Google Scholar] [CrossRef]
- Bø, K.; Kvarstein, B.; Hagen, R.R.; Larsen, S. Pelvic floor muscle exercise for the treatment of female stress urinary incontinence: II. Validity of vaginal pressure measurements of pelvic floor muscle strength and the necessity of supplementary methods for control of correct contraction. Neurourology and urodynamics 1990, 9, 479–487. [Google Scholar] [CrossRef]
|
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2025 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (http://creativecommons.org/licenses/by/4.0/).