1. Introduction
The Coronal Plane Alignment of the Knee (CPAK) classification reported by MacDessi et al. in 2021 provides a simple and pragmatic distribution of nine phenotypes for coronal knee alignment [
1]. The CPAK classification is based on constitutional limb alignment and joint line obliquity and can be used in healthy and arthritic knees [
1]. The CPAK classification is not the only classification proposed for the coronal plane of the knee [
2,
3,
4,
5,
6,
7,
8]. Furthermore, not all authors agree that the CPAK classification helps stratify the different phenotypes in the coronal plane [
9,
10,
11,
12]. In addition to the limitation of being reduced to a phenotypic description of the knee in a single plane (coronal), various arguments have been published against the CPAK classification adequacy, for instance: (1) The three-dimensional orientation of the articular surface relative to the floor does not correlate with the two-dimensional orientation of the coronal joint line, and the CPAK classification types do not correctly represent it [
11]. (2) The CPAK matrix groups do not show a direct correlation with a specific pattern of extra-articular deformity [
10]. (3) The CPAK joint line obliquity measurement technique can be misleading in defining the position of the apex of the knee joint line obliquity and that the agreement between them is less than 50% [
9]. In addition, in a recent publication from our group [
13], we observed something that has been reported in several published studies analysing the CPAK classification of different populations: the low percentage representation of CPAK groups VII and, essentially, VIII and IX, with percentages of less than 1% in most studies [
1,
14,
15,
16,
17,
18,
19,
20,
21]. Despite criticism, knee surgeons use the CPAK classification most widely to define the coronal plane’s different morphotypes, providing a common language among healthcare professionals.
The relationship of the different morphological or angular variables between the three planes is an area for improvement in any attempt to phenotypically classify the knee joint. Regardless of the alignment strategy chosen for total knee arthroplasty (TKA) surgery, including mechanical, adjusted mechanical, anatomical, unrestricted or restricted kinematic, inverse kinematic or functional alignment, it is a mistake to focus solely on the coronal plane and ignore the various variables in the sagittal and axial planes that can potentially affect the outcomes of the operation.
Several authors have previously investigated the relationship between the coronal plane and variables in the other two planes [
22,
23,
24,
25,
26]. We also observed a linear relationship between the coronal alignment, the rotational geometry of the distal femur, and the tibial torsion [
27]. More recently, other authors have investigated the relationship between phenotypes based on the CPAK classification and sagittal and axial plane geometry [
28,
29,
30]. Contrary to Corbett et al., who claimed that the CPAK phenotype has little correlation with 3-dimensional alignment characteristics and that these results do not support the need to extend the CPAK classification beyond coronal plane alignment [
28], Ziegenhorn et al. postulated that there is a correlation between the coronal alignment of the lower limb and femoral torsion and that therefore this may provide a basis for extending the CPAK classification beyond the coronal plane [
29]. Jagota et al. [
30] also found no clear relationship between variables in the sagittal and axial planes and the coronal description according to the CPAK classification criteria.
In TKA surgery, some morphological variables in the axial and sagittal planes are particularly interesting. For example, distal femoral rotation can condition the rotational alignment of the femoral component. Inadequate rotational alignment can cause patellofemoral complications, pain, stiffness, and component failure in TKA [
31,
32,
33].
The important clinical implications of achieving an adequate distal femoral rotation after TKA surgery motivated the present study. It aimed to evaluate whether there is an association between coronal alignment according to the CPAK classification and the distal femoral rotation in a population sample with osteoarthritis (OA).
2. Materials and Methods
The study was retrospective, cross-sectional and observational. Data from 622 cases in 535 OA patients who underwent primary TKA have been retrospectively analysed. In all cases, these were patients undergoing TKA surgery and, therefore, Kellgren-Lawrence grade 3 or 4 knees. Our study group, with an average age of 70.3 years (range 45 to 84) and an average body mass index of 29.08 Kg/m
2 (range 22.8 to 41.8), comprised 364 (58.5%) female and 258 (41.5%) male cases. Out of an initial series of 709 knees, we excluded cases that, due to previous interventions (e.g., femoral or tibial osteotomies) or fractures, presented a possible alteration of the native constitutional axes (23 cases), patients with a flexion contracture of 15 degrees or more (because the study protocol for computed tomography (CT) scanning states that measurement accuracy may be lost in knees with a severe flexion contracture; 17 cases) and patients with ipsilateral hip replacements (as the implantation of the hip prosthesis may alter the constitutionality of the knee alignment [
34,
35]; 47 cases).
Following the same methodology as in other papers published by our group [
36,
37], we used the Somatom Scope scanner (Siemens Healthcare GmbH, Erlangen, Germany) for the image acquisition. For the CT scan, images were acquired with the patient positioned supine in the isocenter of the gantry with the leg of interest in full extension. The acquisition comprised three brief spiral axial scans encompassing the hip, knee, and ankle regions. Each acquisition was accurately centred and zoomed to ensure that the field of view (FoV) circumscribed the region of interest to the greatest possible extent. The scans were acquired in slices of at least 512 x 512 pixels. The thickness of a single slice was 2 mm for the hip and ankle and 0.6 mm for the knee, with a maximum field of view (FoV) of 200 mm. The peak voltage was set to 130 kV, and the X-ray tube current to 60 mA. The average effective radiation dose per CT scan was 0.4 mSv. The images were archived on the Picture Archiving and Communication System (PACS, Siemens Healthcare GmbH, Erlangen, Germany) server in the international standard DICOM (Digital Imaging and Communications in Medicine) format. Measurements on CT scans were performed using MyPlanner
® software (Medacta International, Castel San Pietro, Switzerland) to create virtual 3D models by the MyKnee engineering staff.
The alignment was measured, and the value obtained was rounded to 0.5 degrees. The non-weight-bearing mechanical hip-knee-ankle angle (mHKA angle) was obtained from the intersection of the femoral and tibial mechanical axes. The mechanical lateral distal femoral angle (LDFA) was defined as the lateral angle between the femoral mechanical axis and the distal femoral joint line (tangent between the most distal points of the femoral condyles). The medial mechanical proximal tibial angle (MPTA) was defined as the medial angle between the mechanical axis of the tibia and the proximal tibial joint line (the line between the deepest points of the medial and lateral tibial condyles).
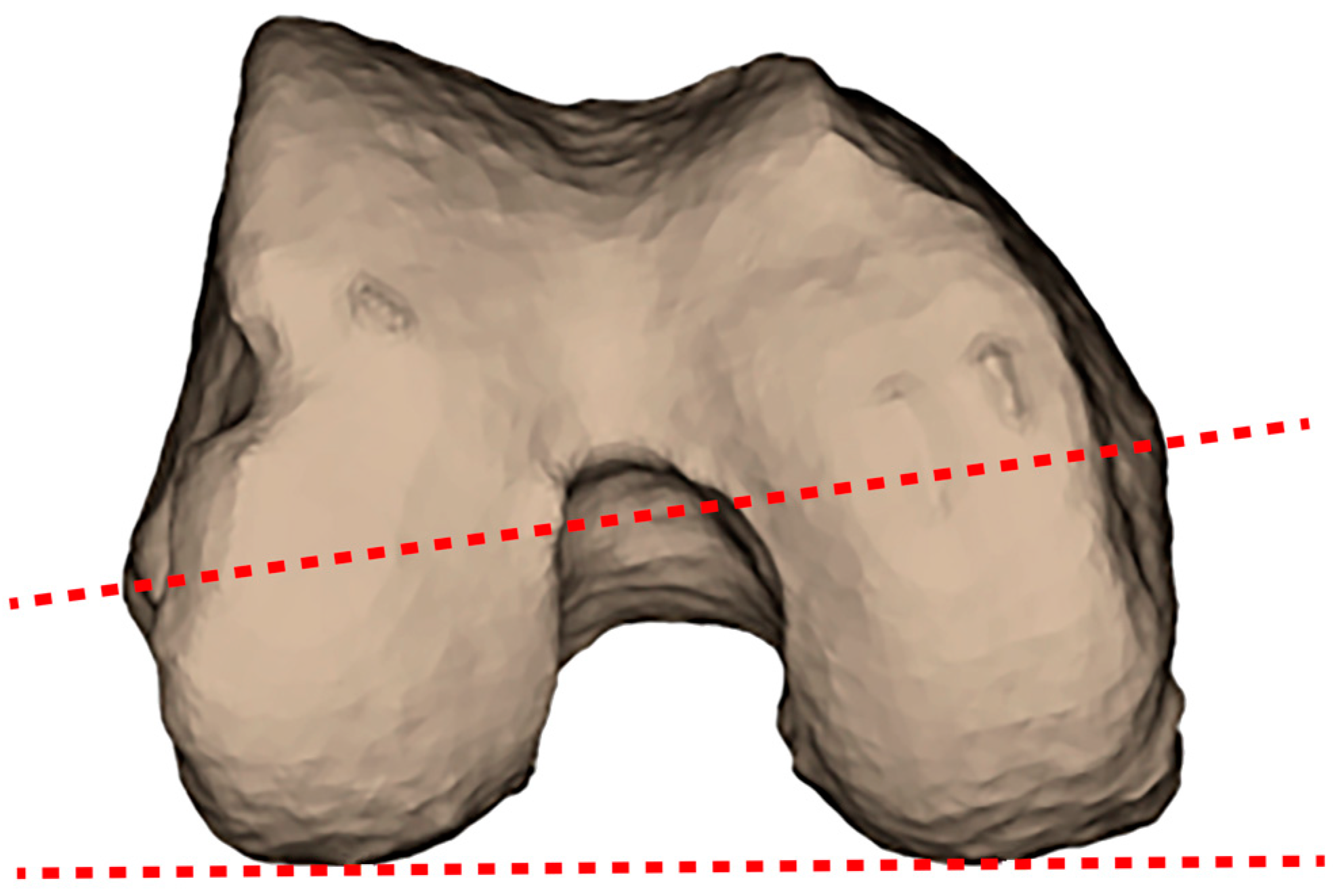
Distal femoral rotation was measured using the condylar twist angle (CTA), first described by Yoshioka et al. [
38]. The CTA (
Figure 1) is defined as the angle between the posterior condylar line (PCL) (the line connecting the most posterior margins of the lateral and medial posterior condyles) and the clinical or anatomical trans-epicondylar axis (cTEA) (a line connecting the tip of the medial and lateral epicondylar prominences of the femur).
The CPAK classification evaluates two criteria: constitutional limb alignment (or arithmetic hip-knee-ankle angle (aHKA angle)) and joint line obliquity (JLO) [
1]. These criteria can be calculated according to the LDFA and the MPTA. Constitutional limb alignment is described as varus, neutral, or valgus. The aHKA is calculated by subtracting the LDFA value from the MPTA value. The JLO is described as apex distal, neutral, or proximal and calculated by adding the value of MPTA to the value of LDFA. The three subgroups of aHKA are crossed with the three subgroups of JLO to yield the nine CPAK types [
1].
Statistical analysis was performed using the Statistical Package for the Social Sciences (SPSS), version 25 for Windows (SPSS, Inc., Chicago, IL, USA) and Minitab Statistical Software, version 22 for Windows (Minitab LLC, Pennsylvania, USA). Our study followed the ethical standards of the World Medical Association Declaration of Helsinki, as revised in 2024. The institutional review board of the author’s institution approved the study protocol (CEIC-HMM-16/19). Given the research’s retrospective nature and medical imaging’s anonymisation (employing a user-defined anonymisation function on the identifiers (the medical record number of each patient) in the Microsoft Excel workbook (Microsoft 365)), the institutional review board considered the study exempt from requiring patients’ informed consent.
3. Results
The values below Q1− (1.5 interquartile range (IQR)) and above Q3+ (1.5 IQR) for the three variables (not the individual outliers of each variable, as each pair of aHKA and JLO values must correspond to a CTA value) have been identified. The values mentioned above, which we have classified as outliers, have been removed from each distribution. This step is of paramount importance, as it prevents the inclusion of patients whose bone morphology is more attributable to significant arthritic bone loss than to the phenotypic characteristics. The IQT method with a scale of 1.5 is the most widely used, and there is a certain consensus in the statistical literature that it should be adopted as the standardisation method, taking as outlier’s data that are at least 2.7 standard deviations away from the arithmetical mean.
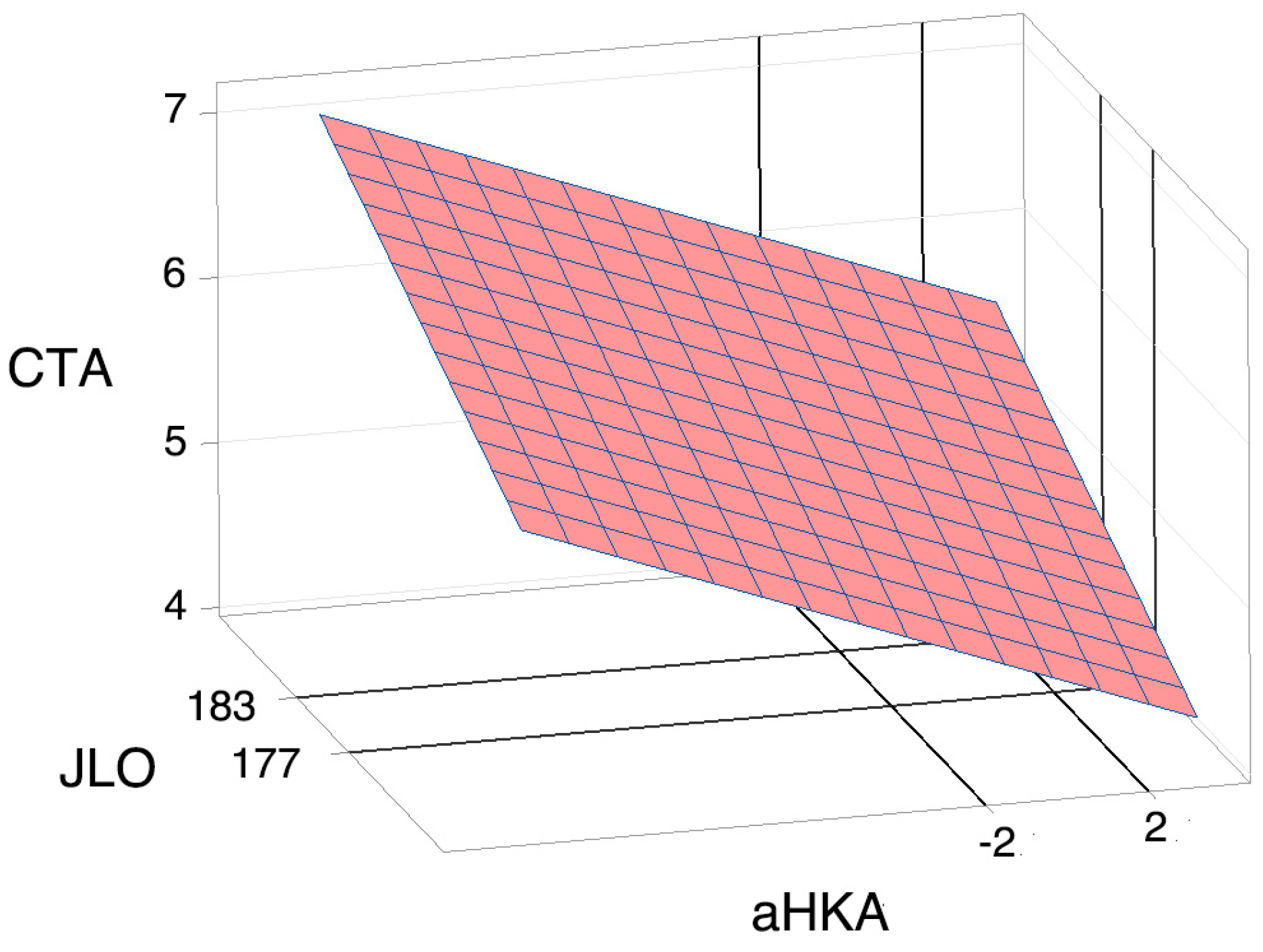
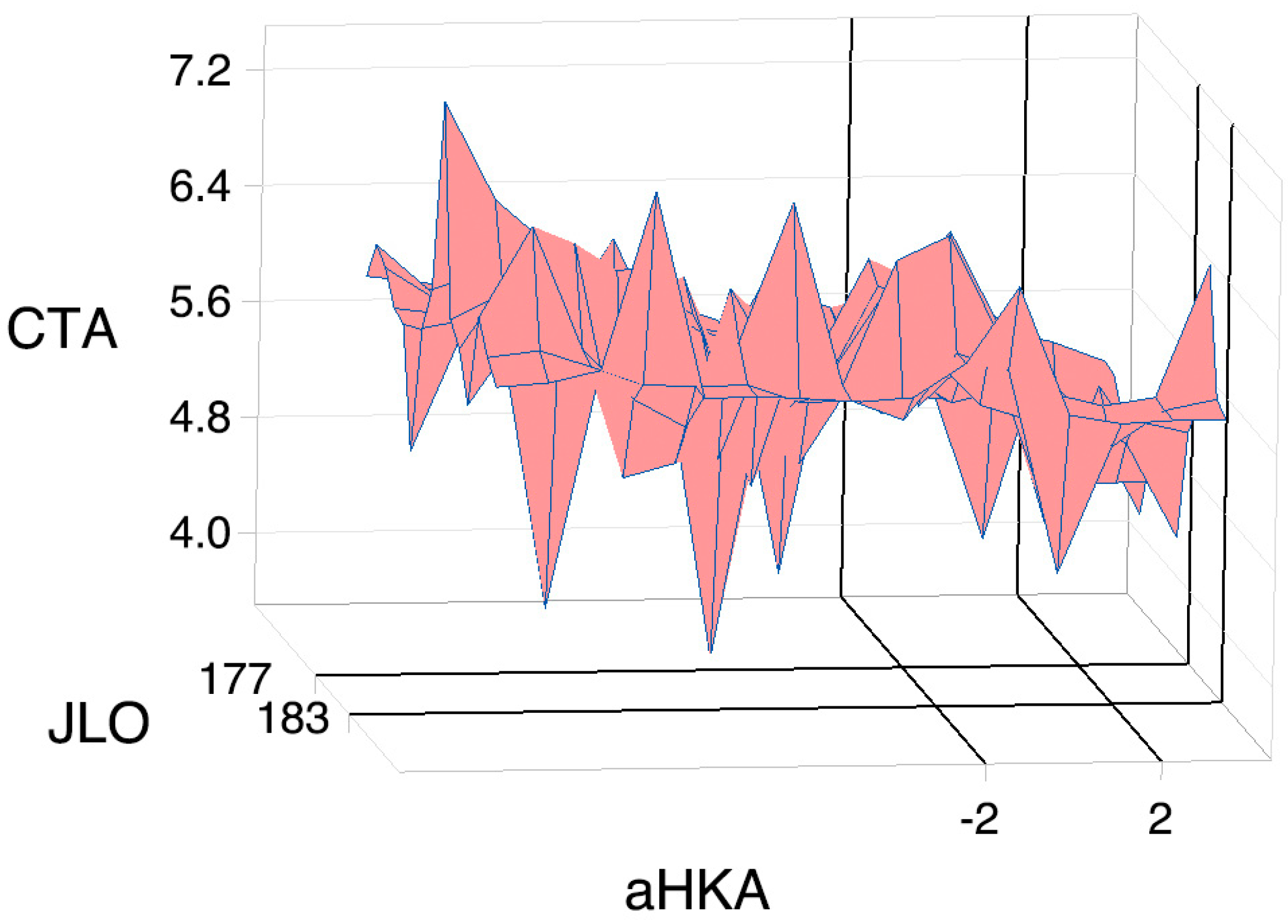
We have calculated the plane that best fits each distribution, as shown in
Figure 2.
The variables are perfectly uncorrelated according to the regression equation: CTA = −4.45 − 0.0897 aHKA + 0.0540 JLO (r2 = 0.0608). Given the absence of correlation, we have obtained a graphical representation that can provide information on the characteristics of the distributions.
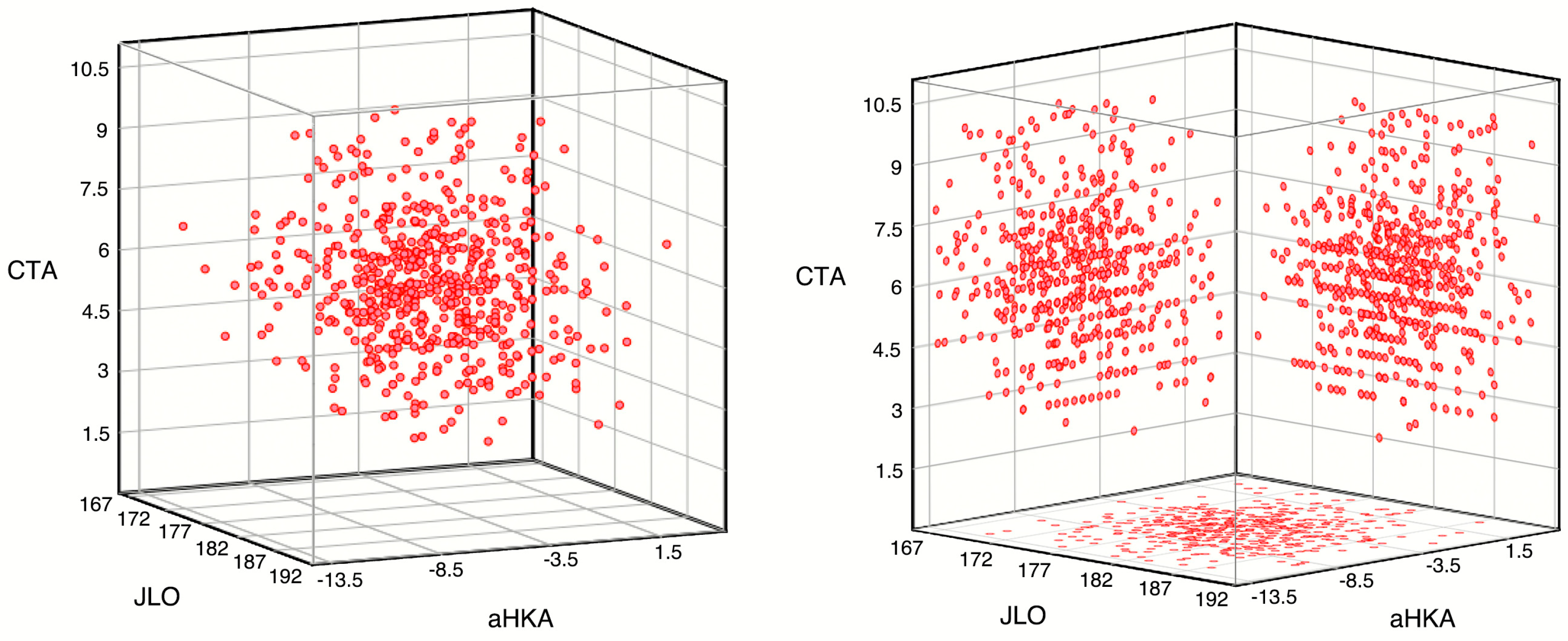
The distribution of the response variables has been evaluated (see
Figure 3). None of the plans exhibited a discernible distribution pattern.
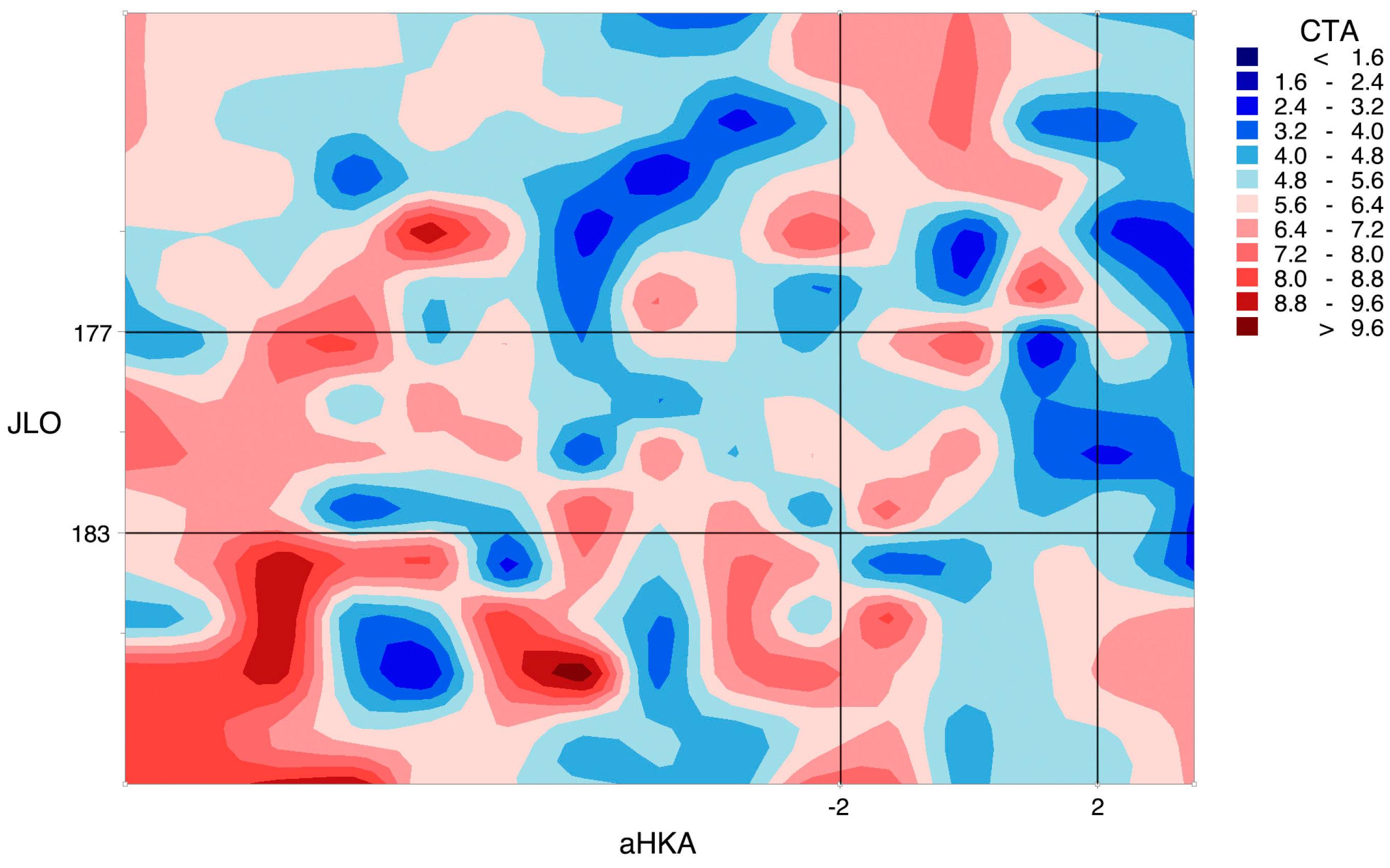
Upon visualising the CTA function using a contour map (a way to depict functions with a two-dimensional input and a one-dimensional output) formed by contour lines on the aHKA, JLO plane (see
Figure 4) or using surface curves with low interpolation (see
Figure 5), it becomes evident that the data do not follow any discernible pattern.
The distribution of the aHKA, JLO and CTA, has been divided into the nine CPAK classification groups, with single outliers discarded for each variable.
Table 1 shows the values of the variables aHKA, JLO and CTA according to the CPAK classification groups. Upon examination of the variables using normality tests (Kolmogorov-Smirnov and Shapiro-Wilk, depending on the sample size), it was determined that all distributions exhibited the requisite normality characteristics except for the CTA variable for the CPAK IV group. This is not a cause for concern, as this variable follows a unimodal distribution and has a sufficiently large n (central limit theorem).
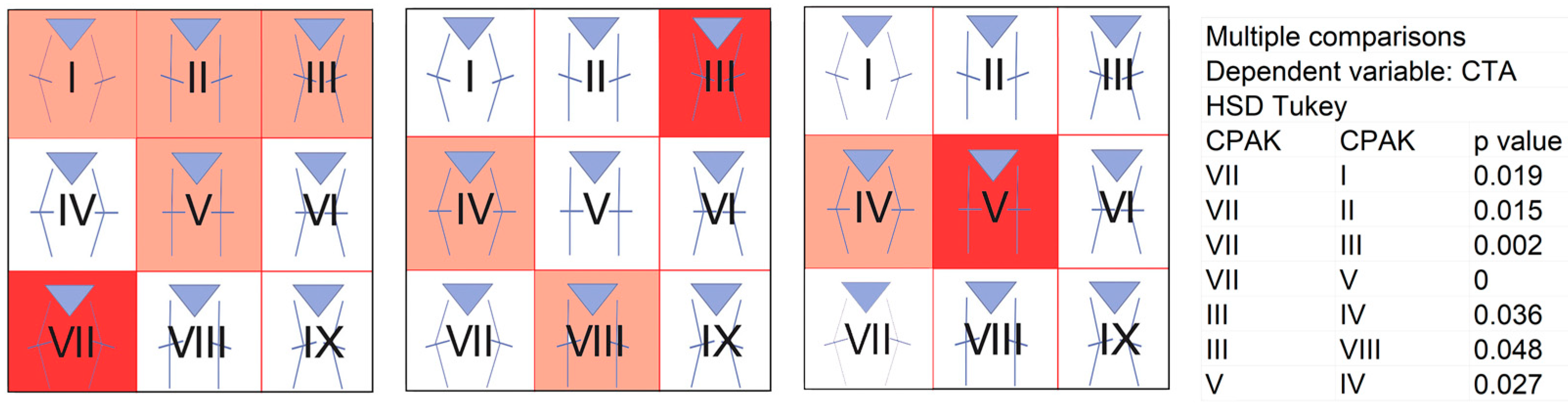
Using ANOVA, we found that there were statistically significant differences between the distributions of the CPAK groups for CTA (F = 5.81; p < 0.001). We calculated Tukey’s comparisons to see which distributions differed statistically, as shown in
Figure 6.
4. Discussion
Our study aimed to search for relationships between phenotypes based on CPAK classification and the distal femoral rotation. In 2021, MacDessi et al. [
1] published a simple and pragmatic classification system for coronal knee alignment based on constitutional limb alignment and joint line obliquity. This system, known as CPAK classification, can be used to categorise nine phenotypes for coronal knee alignment in healthy and arthritic knees. The CPAK classification is one of several proposed for the coronal plane of the knee [
2,
3,
4,
5,
6,
7,
8]. Its limitations have been criticised [
9,
10,
11,
12,
19]. Possibly, the decision to set the boundaries for neutral aHKA at -2º and 2° and for neutral JLO at 177° and 183°, and thus to set mean typical values of 0° for aHKA and 180° for JLO (which mathematically assumes a mean value of 90° of normality for LDFA and MPTA), is probably the origin of some of the limitations of the CPAK classification. Several publications, including the classic paper by Bellemans et al. [
39] describing the “constitutional varus concept”, already showed that the mean values of LDFA and MPTA differ from 90°. For example, in the present study of 622 knees (remembering that these are OA knees), the mean values (with standard deviation) for LDFA are 91.75° (3.08°) and for MPTA 87.28° (2.91°). However, the CPAK classification is, nowadays, the most widely used categorisation to describe a grouped distribution of the different variants of coronal plane alignment [
1,
13,
14,
15,
16,
17,
18,
19,
20,
21,
40,
41,
42]. For some authors, the current focus on static constitutional alignment of the lower limb according to one of the many phenotype classifications may overlook dynamic alignment measures during gait. They advocate the concept of dynamic HKA, which ultimately measures the coronal alignment of the knee throughout the gait cycle [
43].
Corbett et al. [
28] recently measured coronal, sagittal and rotational alignment on CT images of 509 OA knees. Their study aimed to determine if sagittal and rotational knee alignments vary among CPAK types. The authors found few clinically important differences in sagittal and rotational alignment between CPAK types, suggesting that the CPAK phenotype has little correlation with three-dimensional (3D) alignment characteristics. In the opposite direction, Ziegenhorn et al. [
29] found a correlation between coronal alignment of the lower limb and femoral torsion after measuring digital 3D reconstructions of 1,000 EOS images of the legs of patients with knee pain. The authors found no correlation for tibial torsion. Jagota et al. [
30] recently performed a retrospective analysis of a CT database (7,450 knees). They observed weak linear correlations between the axial and sagittal measurements assessed and the aHKA and JLO. In the present study, our observations indicate an absence of a relationship between the values utilised for the stratification of the different groups of the CPAK classification (aHKA and JLO) and the axial plane value analysed (CTA). Consequently, our perspective aligns with that of Corbett et al. [
28], while we disagree with Ziegenhorn et al. [
29]. We do not consider extending the CPAK classification with variables from planes other than the coronal as necessary or feasible. Instead, we propose re-examining the boundaries delineating each group within the CPAK classification as a potentially fruitful avenue of research.
In a prospective study, our group analysed CTA, proximal femoral version, and tibial torsion in 3D reconstructions from CT images of 385 osteoarthritic knees [
27]. We found that as coronal alignment changed from varus to valgus, femoral external rotation increased (r = 0.217, p < 0.001), and external tibial torsion increased (r = 0.248, p < 0.001). No correlation was found between the global coronal alignment and the femoral version.
Aglietti et al. [
44] first reported a linear relationship between the coronal alignment and the distal femoral external rotation measured through the posterior condylar angle (PCA). PCA is the angle between the PCL and the surgical trans-epicondylar axis (a line connecting the lateral epicondyle’s most prominent point with the medial sulcus’s deepest point). Luyckx et al. [
22] published a clear linear relationship between the overall coronal alignment and the rotational geometry of the distal femur consistent with Aglietti’s prior postulate. In the three studies mentioned above [
22,
27,
44], the mechanical tibiofemoral angle (angle between the femoral and tibial mechanical axes) (or, in other words, the mHKA) was used as the reference for coronal alignment. However, we have used both the aHKA and the JLO for our current comparison and have not observed any relationship in line with Corbett et al. [
28]. We analysed possible correlations with both parametric (based on the normality indicated by graphical methods) and non-parametric (based on the results of the Kolmogorov-Smirnov test for variables < 0.05) tests in our series using the non-weight-bearing mHKA value and observed a significant relationship (Pearson: r=0.249, p<0.001; Spearman: r=0.236, p<0.001) between the mHKA and distal femoral rotation as measured by CTA. Consistent with previous studies [
22,
27,
44], distal femoral external rotation increases with increasing the valgus alignment. These results force us to interpret that the presence or absence of a relationship between coronal plane alignment and distal femoral rotation depends on the mathematical terms used. The result is different when using non-weight-bearing mHKA or aHKA, so we can infer that non-weight-bearing mHKA (and perhaps the weight-bearing mHKA, although we cannot say for sure) and aHKA do not measure exactly the same thing.
The existing difference between the distributions of the CPAK groups for CTA (F = 5.81; p < 0.001) does not imply a correlation (i.e., a dependency relationship between the CTA distribution data and the variables that define each CPAK classification group, in consideration of the regression equations obtained). Both concepts are not mutually exclusive.
There were several potential limitations in this study. First, we have only classified the cases according to the CPAK classification. We have not contrasted the cases with the functional knee phenotype concept [
2,
3,
4,
45] or the classifications proposed by Lin et al. [
5], Mullaji et al. [
7,
8] or Marchand et al. [
6]. Second, this was a retrospective cohort study based on the database of a single centre of patients originating from a determined region of our country, which limits the generalisability of the results to a larger or broader population. Third, this study only included data from patients with knee OA (Kellgren-Lawrence grade 3 or 4) and did not examine healthy patients. However, some studies argue that the CPAK classification does not change with OA progression [
17,
46] and most morphological analyses are based on CT scans performed in the context of preoperative planning for TKA surgery (and, therefore, late-stage OA). Fourth, we have not analysed the values regarding the femoral version, femoral bowing, tibial torsion, and rotation at the knee. Fifth, we removed values outside the interquartile range, as we considered these values to be outliers in the data set and not reflect the natural variability of the data. However, this would likely have a limited effect on the results, given the large numbers in this cohort. Eliminating outliers is imperative in any study because they impact the normality of the sample and influence the sample mean and standard deviation. Sixth, we have evaluated the angular values (mHKA angle, LDFA, MPTA, and CTA) and thus aHKA and JLO under non-weight-bearing conditions obtained from CT scan studies. Notwithstanding, recent observations [
47] posit that CT scan-based measurements are more accurate than full-length anteroposterior lower limb radiographs. Seventh, although our study analysed 622 knees to minimise type I statistical error, the numbers of cases grouped into CPAK types VII to IX were small. We do not consider this a significant limitation, as these patients are rare in the general population based on the CPAK classification. Finally, we lack a specific determination of intra- and inter-observer variability. However, based on the findings of earlier studies [
24], these variabilities can be assumed to be negligible.
5. Conclusions
We did not observe any correlation between the coronal plane alignment according to the CPAK classification groups with distal femoral rotation (CTA). On the other hand, when we used the mHKA, and not the aHKA, for the analysis, there was a correlation: the more significant the valgus, the greater the distal femoral external rotation. Perhaps the stratification of the CPAK groups (i.e., a purely arithmetical aspect) hides possible relationships between the coronal and axial planes. When using the CPAK classification in total knee arthroplasty surgery planning, we must pay close attention to the morphological and angular characteristics in the coronal plane and, independently, to these characteristics in the axial plane.
Author Contributions
Conceptualization, Vicente J. León-Muñoz, Mirian López-López and Joaquín Moya-Angeler; Data curation, Vicente J. León-Muñoz, José Hurtado-Avilés and Mirian López-López; Formal analysis, Vicente J. León-Muñoz and José Hurtado-Avilés; Methodology, Vicente J. León-Muñoz and José Hurtado-Avilés; Supervision, Vicente J. León-Muñoz, Fernando Santonja-Medina and Joaquín Moya-Angeler; Validation, Vicente J. León-Muñoz, Fernando Santonja-Medina, Francisco Lajara-Marco and Joaquín Moya-Angeler; Visualization, José Hurtado-Avilés; Writing – original draft, Vicente J. León-Muñoz; Writing – review & editing, Vicente J. León-Muñoz, José Hurtado-Avilés, Fernando Santonja-Medina, Francisco Lajara-Marco, Mirian López-López and Joaquín Moya-Angeler.
Funding
This research received no external funding.
Institutional Review Board Statement
The study was conducted in accordance with the Declaration of Helsinki and approved by the Institutional Review Board of Hospital Morales Meseguer (CEIC-HMM-16/19).
Informed Consent Statement
Patient consent was waived due to the research’s retrospective nature and medical imaging’s anonymisation.
Data Availability Statement
The raw data supporting the conclusions of this article will be made available by the authors on request.
Conflicts of Interest
The authors declare no conflicts of interest.
Abbreviations.ethic
The following abbreviations are used in this manuscript:
| CPAK |
Coronal Plane Alignment of the Knee |
| TKA |
Total Knee Arthroplasty |
| OA |
Osteoarthritis |
| CT |
Computed Tomography |
| mHKA |
mechanical hip-knee-ankle |
| LDFA |
mechanical lateral distal femoral angle |
| MPTA |
medial mechanical proximal tibial angle |
| CTA |
condylar twist angle |
| aHKA |
arithmetic hip-knee-ankle |
| JLO |
joint line obliquity |
References
- MacDessi SJ, Griffiths-Jones W, Harris IA, Bellemans J, Chen DB (2021) Coronal Plane Alignment of the Knee (CPAK) classification. Bone Joint J 103-B:329–337. [CrossRef]
- Hirschmann MT, Hess S, Behrend H, Amsler F, Leclercq V, Moser LB (2019) Phenotyping of hip-knee-ankle angle in young non-osteoarthritic knees provides better understanding of native alignment variability. Knee Surg Sports Traumatol Arthrosc 27:1378–1384. [CrossRef]
- Hirschmann MT, Moser LB, Amsler F, Behrend H, Leclercq V, Hess S (2019) Phenotyping the knee in young non-osteoarthritic knees shows a wide distribution of femoral and tibial coronal alignment. Knee Surg Sports Traumatol Arthrosc 27:1385–1393. [CrossRef]
- Hirschmann MT, Moser LB, Amsler F, Behrend H, Leclerq V, Hess S (2019) Functional knee phenotypes: a novel classification for phenotyping the coronal lower limb alignment based on the native alignment in young non-osteoarthritic patients. Knee Surg Sports Traumatol Arthrosc 27:1394–1402. [CrossRef]
- Lin Y-H, Chang F-S, Chen K-H, Huang K-C, Su K-C (2018) Mismatch between femur and tibia coronal alignment in the knee joint: classification of five lower limb types according to femoral and tibial mechanical alignment. BMC Musculoskelet Disord 19:411. [CrossRef]
- Marchand R, Shul C, Hameed D, Dubin J, Roche M, Bowes M, Scholl L, Gutowski T, Mont MA (2024) Three-dimensional-based native alignment phenotype classification system: Description for use in planning for deformities during total knee arthroplasty. J Orthop 54:163–167. [CrossRef]
- Mullaji A, Bhoskar R, Singh A, Haidermota M (2022) Valgus arthritic knees can be classified into nine phenotypes. Knee Surg Sports Traumatol Arthrosc 30:2895–2904. [CrossRef]
- Mullaji A, Shah R, Bhoskar R, Singh A, Haidermota M, Thakur H (2022) Seven phenotypes of varus osteoarthritic knees can be identified in the coronal plane. Knee Surg Sports Traumatol Arthrosc 30:2793–2805. [CrossRef]
- Şahbat Y, Chou T-FA, An J-S, Gülağacı F, Ollivier M (2024) CPAK classification detect the real knee joint apex position in less than half of the knees. Knee Surg Sports Traumatol Arthrosc 32:1548–1556. [CrossRef]
- Loddo G, An J-S, Claes S, Jacquet C, Kley K, Argenson J-N, Sharma A, Ollivier M (2024) CPAK classification cannot be used to determine segmental coronal extra-articular knee deformity. Knee Surg Sports Traumatol Arthrosc 32:1557–1570. [CrossRef]
- Sasaki R, Niki Y, Kaneda K, Yamada Y, Nagura T, Nakamura M, Jinzaki M (2023) Three-dimensional joint surface orientation does not correlate with two-dimensional coronal joint line orientation in knee osteoarthritis: Three-dimensional analysis of upright computed tomography. Knee 43:10–17. [CrossRef]
- Hirschmann MT, von Eisenhart-Rothe R, Graichen H (2023) Any technology assisting total knee arthroplasty (TKA) will fail without the correct 3D alignment and balancing target. Knee Surg. Sports Traumatol. Arthrosc. 31:733–735.
- León-Muñoz VJ, Hurtado-Avilés J, López-López M, Santonja-Medina F, Moya-Angeler J (2024) The Distribution of Coronal Plane Alignment of the Knee Classification in a Sample of Spanish Southeast Osteoarthritic Population: A Retrospective Cross-Sectional Observational Study. Medicina (B Aires) 60:1612. [CrossRef]
- Sappey-Marinier E, Batailler C, Swan J, Schmidt A, Cheze L, MacDessi SJ, Servien E, Lustig S (2022) Mechanical alignment for primary TKA may change both knee phenotype and joint line obliquity without influencing clinical outcomes: a study comparing restored and unrestored joint line obliquity. Knee Surg Sports Traumatol Arthrosc 30:2806–2814. [CrossRef]
- Mulpur P, Desai KB, Mahajan A, Masilamani ABS, Hippalgaonkar K, Reddy AVG (2022) Radiological Evaluation of the Phenotype of Indian Osteoarthritic Knees based on the Coronal Plane Alignment of the Knee Classification (CPAK). Indian J Orthop 56:2066–2076. [CrossRef]
- Toyooka S, Osaki Y, Masuda H, Arai N, Miyamoto W, Ando S, Kawano H, Nakagawa T (2023) Distribution of Coronal Plane Alignment of the Knee Classification in Patients with Knee Osteoarthritis in Japan. J Knee Surg 36:738–743. [CrossRef]
- Nomoto K, Hanada M, Hotta K, Matsuyama Y (2023) Distribution of coronal plane alignment of the knee classification does not change as knee osteoarthritis progresses: a longitudinal study from the Toei study. Knee Surg Sports Traumatol Arthrosc 31:5507–5513. [CrossRef]
- Şenel A, Eren M, Sert S, Gürpınar T, Çarkçı E, Polat B (2024) Phenotyping of the Turkish population according to Coronal Plane Alignment of the Knee classification: A retrospective cross-sectional study. Jt Dis Relat Surg 35:194–201. [CrossRef]
- Liu L, Lei K, Du D, Lin Y, Pan Z, Guo L (2024) Functional knee phenotypes appear to be more suitable for the Chinese OA population compared with CPAK classification: A study based on 3D CT reconstruction models. Knee Surg Sports Traumatol Arthrosc 32:1264–1274. [CrossRef]
- Palanisamy Y, Natarajan S, Prasad AR, Rajan D V (2024) Coronal Plane Alignment Classification of Arthritic Knees in a South Indian Population and Functional Outcome Comparison Post-mechanical Alignment Total Knee Arthroplasty. Indian J Orthop 58:740–746. [CrossRef]
- Coetzee K, Charilaou J, Burger M, Jordaan J (2024) Increased prevalence of valgus constitutional alignment subtypes in a South African arthritic population group using the coronal plane alignment of the knee (CPAK) classification. Knee 49:158–166. [CrossRef]
- Luyckx T, Zambianchi F, Catani F, Bellemans J, Victor J (2013) Coronal alignment is a predictor of the rotational geometry of the distal femur in the osteo-arthritic knee. Knee Surg Sports Traumatol Arthrosc 21:2331–2337. [CrossRef]
- Cohen DA, Gursel AC, Low AK (2019) How coronal alignment affects distal femoral anatomy: an MRI-based comparison of varus and valgus knees. J Orthop Surg Res 14:92. [CrossRef]
- Thienpont E, Schwab P-E, Paternostre F, Koch P (2014) Rotational alignment of the distal femur: anthropometric measurements with CT-based patient-specific instruments planning show high variability of the posterior condylar angle. Knee Surgery, Sport Traumatol Arthrosc 22:2995–3002. [CrossRef]
- Murgier J, Chantalat É, Li K, Chiron P, Telmon N, Huang W, Berard E, Cavaignac E (2018) Distal femoral torsion: Differences between caucasians and asians. A multicentre computed tomography study of 515 distal femurs. Orthop Traumatol Surg Res 104:997–1001. [CrossRef]
- Chang MJ, Jeong HJ, Kang S-B, Chang CB, Yoon C, Shin JY (2018) Relationship Between Coronal Alignment and Rotational Profile of Lower Extremity in Patients With Knee Osteoarthritis. J Arthroplasty 33:3773–3777. [CrossRef]
- León-Muñoz VJ, Manca S, López-López M, Martínez-Martínez F, Santonja-Medina F (2021) Coronal and axial alignment relationship in Caucasian patients with osteoarthritis of the knee. Sci Rep 11:7836. [CrossRef]
- Corbett J, Sinha P, Esposito CI, Wood JA, Chen DB, MacDessi SJ (2024) Multi-Planar Expansion of the Coronal Plane Alignment of the Knee Classification? A Computed Tomographic Study Indicates No Significant Correlation With Alignment Parameters in Other Planes. J Arthroplasty 39:336–342. [CrossRef]
- Ziegenhorn J, Kirschberg J, Heinecke M, von Eisenhart-Rothe R, Matziolis G (2024) Significant difference in femoral torsion between coronal plane alignment of the knee type 1 and 4. Knee Surg Sports Traumatol Arthrosc 32:1199–1206. [CrossRef]
- Jagota I, Twiggs J, Miles B, Baré J V (2024) Variability of three-dimensional knee morphology cannot be effectively assessed using a coronal plane knee alignment classification in total knee arthroplasty patients. J Exp Orthop 11:e70039. [CrossRef]
- Berger RA, Crossett LS, Jacobs JJ, Rubash HE (1998) Malrotation causing patellofemoral complications after total knee arthroplasty. Clin Orthop Relat Res 144–153. [CrossRef]
- Barrack RL, Schrader T, Bertot AJ, Wolfe MW, Myers L (2001) Component rotation and anterior knee pain after total knee arthroplasty. Clin Orthop Relat Res 46–55. [CrossRef]
- Romero J, Stähelin T, Wyss T, Hofmann S (2003) [Significance of axial rotation alignment of components of knee prostheses]. Orthopade 32:461–468. [CrossRef]
- Ollivier M, Parratte S, Lecoz L, Flecher X, Argenson J-N (2013) Relation between lower extremity alignment and proximal femur anatomy. Parameters during total hip arthroplasty. Orthop Traumatol Surg Res 99:493–500. [CrossRef]
- Choi YS, Park J-W, Kim TW, Kang KS, Lee Y-K, Koo K-H, Chang CB (2023) Effect of Total Hip Arthroplasty on Ipsilateral Lower Limb Alignment and Knee Joint Space Width: Minimum 5-Year Follow-up. J Korean Med Sci 38:e148. [CrossRef]
- León-Muñoz VJ, López-López M, Martínez-Martínez F, Santonja-Medina F (2020) Comparison of weight-bearing full-length radiographs and computed-tomography-scan-based three-dimensional models in the assessment of knee joint coronal alignment. Knee 27:543–551. [CrossRef]
- León-Muñoz VJ, López-López M, Lisón-Almagro AJ, Martínez-Martínez F, Santonja-Medina F (2022) Computed Tomography-Based Patient-Specific Instrumentation Loses Accuracy with Significant Varus Preoperative Misalignment. J Knee Surg 35:574–582. [CrossRef]
- Yoshioka Y, Siu D, Cooke TD (1987) The anatomy and functional axes of the femur. J Bone Jt Surg Am 69:873–880.
- Bellemans J, Colyn W, Vandenneucker H, Victor J (2012) The Chitranjan Ranawat award: is neutral mechanical alignment normal for all patients? The concept of constitutional varus. Clin Orthop Relat Res 470:45–53. [CrossRef]
- Tarassoli P, Wood JA, Chen DB, Griffiths-Jones W, Bellemans J, MacDessi SJ (2022) Arithmetic hip-knee-ankle angle and stressed hip-knee-ankle angle: equivalent methods for estimating constitutional lower limb alignment in kinematically aligned total knee arthroplasty. Knee Surg Sports Traumatol Arthrosc 30:2980–2990. [CrossRef]
- Yang HY, Yoon TW, Kim JY, Seon JK (2024) Radiologic Assessment of Knee Phenotypes Based on the Coronal Plane Alignment of the Knee Classification in a Korean Population. Clin Orthop Surg 16:422–429. [CrossRef]
- Gao Y-H, Qi Y-M, Huang P-H, Zhao X-Y, Qi X (2024) Distribution of coronal plane alignment of the knee classification in Chinese osteoarthritic and healthy population: a retrospective cross-sectional observational study. Int J Surg 110:2583–2592. [CrossRef]
- Indelli PF (2024) The epidemic of alignment classifications in total knee arthroplasty forgives the kinematic of the human knee. J. Exp. Orthop. 11:e70052.
- Aglietti P, Sensi L, Cuomo P, Ciardullo A (2008) Rotational position of femoral and tibial components in TKA using the femoral transepicondylar axis. Clin Orthop Relat Res 466:2751–2755. [CrossRef]
- Jenny J-Y, Baldairon F (2023) The coronal plane alignment of the knee classification does not correlate with the functional knee phenotype classification. Knee Surg Sports Traumatol Arthrosc. [CrossRef]
- Hess S, Moser LB, Robertson EL, Behrend H, Amsler F, Iordache E, Leclercq V, Hirschmann MT (2022) Osteoarthritic and non-osteoarthritic patients show comparable coronal knee joint line orientations in a cross-sectional study based on 3D reconstructed CT images. Knee Surg Sports Traumatol Arthrosc 30:407–418. [CrossRef]
- Wong WK, Zulkhairi SZ, Chua H Sen (2025) CT-Based Software-Generated Measurements Permit More Objective Assessments of Arithmetic Hip-Knee-Ankle Axis and Joint Line Obliquity. Life 15:188. [CrossRef]
|
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2025 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (http://creativecommons.org/licenses/by/4.0/).