Introduction
Modern medical education is presently undergoing a dynamic and unique pattern alteration [
1,
2,
3], categorized by a firm commitment to active and experiential learning methods that encompass a vast spectrum of intricate clinical procedures. Within this expansive array of essential competencies, the mastery of in-vitro male catheterization undeniably emerges as an unequivocal cornerstone skill for healthcare practitioners [
4,
5,
6,
7]. This indispensable procedure not only assumes a pivotal role in effectively managing urinary retention but also serves as an invaluable diagnostic tool and plays a continuous monitoring role in assessing urinary output, thus firmly anchoring its profound significance within the healthcare domain.
Amidst this ongoing transformation of the educational landscape, healthcare simulation has emerged as a revolutionary and indispensable pedagogical tool, heralding a momentous departure from conventional, didactic teaching approaches [
8,
9,
10,
11,
12]. This powerful instrument offers a multifaceted approach to skill acquisition, rapidly gaining recognition for its capacity to engender a controlled, risk-free learning environment that faithfully replicates real-world clinical scenarios with unparalleled precision. At the heart of this educational metamorphosis lies the profound recognition that practical proficiency is most effectively cultivated through a trifecta of deliberate practice, extensive skill repetition, and the unique capacity to confidently navigate both the commonplace and the rare, intricate clinical scenarios that healthcare practitioners encounter [
13,
14,
15,
16,
17].
The purpose of this research attempt is to embark on a comprehensive, in-depth exploration of the profound and incontrovertible influence that healthcare simulation wields within the realm of medical education. In this endeavor, we cast our focused gaze upon the highly specialized domain of in-vitro male catheterization procedures, meticulously dissecting its multifaceted impact on the proficiency, competence, and confidence of medical students [
18,
19,
20]. Through this concerted effort, we aspire to illuminate the transformative potential inherent in healthcare simulation, transcending the constraints of conventional pedagogical paradigms and paving the way for an exciting new era of experiential learning within the illustrious domain of medical education.
Materials and Methods
The research methodology employed in this investigation is characterized by its multi-faceted and severe nature, attached in a systematic approach that builds upon a solid foundation. The methodology unfolds in a sequence that begins with an exhaustive and comprehensive literature review, laying the groundwork upon which the entire study is constructed.
Subsequently, we executed a meticulously designed study, characterized by a pre-post design framework that was methodically tailored to scrutinize the profound effects of simulation-based training on the development of medical students’ prowess in the intricate domain of in-vitro male catheterization on Simulator (
Image-2 and Image-3) [
21].
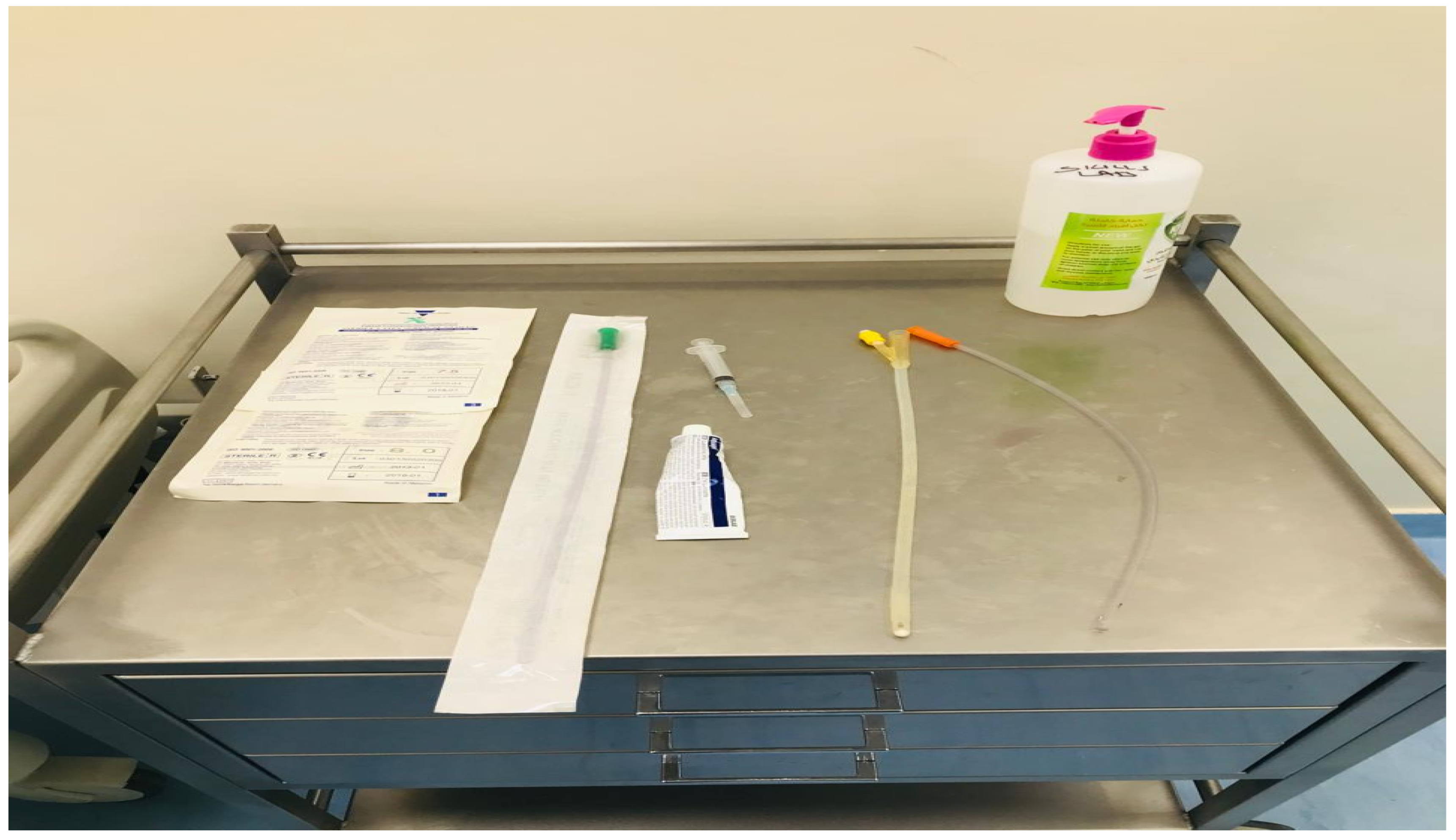
Image 1.
Surgical Table with basic required item for characterization.
Image 1.
Surgical Table with basic required item for characterization.
Image 2.
Male Characterization Simulation Manikin.
Image 2.
Male Characterization Simulation Manikin.
The study group, a diverse group of medical students, was judiciously divided into two distinct and well-defined groups. The first group underwent conventional didactic instruction in the nuanced art of in-vitro male catheterization. In stark contrast, the second group was enveloped in an immersive and transformative simulation-based training curriculum, a distinction that serves as the fulcrum of this research’s exploration.
List of Required Materials
Simulation-based training sessions within the latter group were conducted using cutting-edge simulators (Image-2), meticulously designed to replicate the complexities of anatomical structures and physiological responses with an unparalleled level of fidelity. Each training session within this immersive curriculum was meticulously structured, consisting of a series of deliberate practice scenarios that were thoughtfully overseen by seasoned instructors with a wealth of experience in the field.
To holistically assess the impact of simulation-based training on the students’ skill acquisition and confidence levels, the study embraced a multifaceted evaluation approach. This comprehensive evaluation included both pre-training and post-training assessments, objectively measuring the acquisition of skills and knowledge. Furthermore, it encompassed objective structured clinical examinations (OSCEs), which provided a robust platform to gauge the students’ ability to apply their newfound expertise in real-world clinical scenarios [
12,
13,
14,
15,
16]. Complementing these objective measures, surveys were thoughtfully employed to solicit students’ self-assessed confidence levels, thereby capturing a nuanced understanding of their evolving perceptions and confidence in performing in-vitro male catheterization procedures [
17].
In sum, our research methodology represents a well-orchestrated symphony of meticulous planning, systematic execution, and comprehensive evaluation, serving as the bedrock upon which the transformative influence of simulation-based training on medical students is meticulously unveiled [
18,
19,
20].
Image 3.
Passing the catheter into the male meatus [
21].
Image 3.
Passing the catheter into the male meatus [
21].
Results/Explanation
The findings originating from our comprehensive research endeavor undeniably reveal a multitude of noteworthy outcomes, showcasing pronounced enhancements in both the technical competencies and the self-assessed confidence levels of medical students who enthusiastically engaged in simulation-based training, which was meticulously centered on the intricacies of in-vitro male catheterization procedures. These pivotal findings, which have surfaced as a result of our methodical exploration, illuminate the transformative potential of simulation-based education in the medical realm:
Skill Proficiency: The students who were fortunate to participate in the simulation-based training sessions exhibited a significantly elevated level of skill proficiency in the domain of in-vitro male catheterization. They consistently demonstrated an exceptional ability to adroitly catheterize the simulated anatomical model, execute meticulous sterile preparation procedures, and effectively navigate and manage potential complications that can arise during this intricate procedure.
Confidence Levels: It is noteworthy that the students who were exposed to the immersive world of simulation-based training reported significantly heightened levels of self-assuredness and confidence in their aptitude to proficiently execute in-vitro male catheterization procedures. This striking contrast was particularly evident when comparing them with their counterparts who received traditional didactic instruction, underscoring the profound impact of simulation-based learning on bolstering students’ belief in their competencies.
Retention of Knowledge: Beyond the realm of skill acquisition, our research elucidates that simulation-based training offers a unique advantage—superior knowledge retention. Students who partook in this immersive educational experience not only mastered the procedural intricacies but also demonstrated a deep-seated understanding of the underlying principles and best practices governing in-vitro male catheterization. This heightened retention augments their ability to apply theoretical knowledge to real-world clinical scenarios, thereby enhancing their efficacy as future healthcare professionals.
Patient Safety: Significantly, our research extends beyond the realm of procedural mastery. It delves into the broader implications of simulation training, with an unwavering focus on patient safety considerations, including infection control practices. The results are indicative of an overall heightened awareness among simulation-trained students regarding the critical importance of safeguarding patient well-being. This profound emphasis on patient safety further underscores the transformative potential of simulation-based education in cultivating the overarching ethos of patient-centered care, which is a cornerstone of the healthcare profession.
In essence, the findings emerging from our research represent an unmistakable testament to the multifaceted benefits of simulation-based training in the realm of medical education. These results transcend the boundaries of traditional teaching methodologies, ushering in an era of enhanced competency, confidence, knowledge retention, and unwavering dedication to patient safety among the next generation of healthcare practitioners.
Discussion
The visions collected from our thorough of research endeavor firmly position healthcare simulation as a transformative paradigm within the expansive realm of medical education. This study provides compelling evidence substantiating its efficacy in profoundly enhancing the practical aptitude of medical students, with a specific focus on the intricate intricacies of in-vitro male catheterization. While the immediate benefits of simulation-based training are palpable, manifested in heightened skill proficiency and bolstered self-confidence among learners, it is imperative to acknowledge the long-term implications that extend far beyond the confines of skill acquisition.
One of the paramount facets that necessitates further exploration is the enduring impact of simulation training on patient safety and the mitigation of medical errors. As the healthcare landscape evolves at an unprecedented pace, the imperative to ensure patient safety and minimize the occurrence of errors becomes increasingly pivotal. Therefore, it is incumbent upon the medical education community to delve deeper into the nexus between simulation-based training and patient safety, investigating how this pedagogical approach can serve as a potent instrument in equipping future healthcare practitioners with the knowledge, skills, and attitudes necessary to safeguard patient well-being.
Conclusions
In the dynamic ambiance of modern medical education, healthcare simulation emerges not merely as an adjunct to traditional pedagogical approaches but as an indispensable cornerstone. Our meticulously conducted study reverberates with a resounding message, underscoring the pivotal role that simulation training assumes in elevating the proficiency of medical students, particularly in the intricate domain of in-vitro male catheterization procedures.
As we navigate the uncharted waters of a healthcare landscape that continues to rapidly evolve, the significance of simulation training becomes irrefutable. It is not only a conduit for enhancing clinical competencies but a transformative force that ensures future healthcare practitioners are well-equipped to navigate the complex and dynamic clinical scenarios they will invariably encounter. Moreover, our research serves as a clarion call, heralding the imperative need to explore the long-term implications of simulation training, particularly in the context of patient safety and error reduction—a journey that promises to redefine the future of medical education and, by extension, the delivery of high-quality patient care.
Acknowledgements
The authors are grateful to the Deanship of Scientific Research, Prince Sattam bin Abdulaziz University, Al-Kharj, Saudi Arabia for the support and encouragement in conducting the research and publishing this article.
Conflicts of Interest
The authors declare no conflicts of interest relevant to this article.
References
- Al-Elq, AH. Medicine and Clinical Skills Laboratories. J Fam Community Med. 2007; 14:59–63.
- Al-Elq, AH. Simulation-based medical teaching and learning. J Family Community Med. 2010;17(1):35-40.
- Bates DW, Spell N, Cullen DJ, Burdick E, Laird N, Petersen LA, et al. Cost of adverse drug events in hospitalized patients.Adverse drug events prevention study group. JAMA. 1997; 277:307–11.
- Brennan TA, Leape LL, Laird NM, Hebert L, Localio AR, Lawthers AG, et al. Incidence of adverse events and negligence in hospitalized patients: Results of the Harvard Medical practice Study 1. N Engl J Med. 1991; 324:360–76.
- Cannon-Bowers, JA. Recent advances in Scenario-based training for medical education. Curr Opin Anaethesiol. 2008; 21:784–9.
- Cheng A, Duff J, Grant E, Kissoon N, Grant VJ. Simualtion in paediatrics: An educational revolution. Paediatr Child Health. 2007; 12:465–8.
- Cherry RA, Ali J. Current concepts in simulation-based trauma education. J Trauma. 2008;65: 1186–93.
- Costanza ME, Luckmann R, Quirk ME, Clemow L, White MJ, Stoddard AM. The Effectiveness of Using Standardized Patients to Improve Community Physician Skills in Mammography Counseling and Clinical Breast Exam. Prev Med. 1999; 29:241–8.
- Dent, JA. Current trends and future implications in the developing role of clinical skills centres. Med Teach. 2001; 23:483–9.
- Flangan B, Nestel D, Joseph M. Making patient safety the focus: Crisis resorce management in the undergraduate curriculum. Med Edu. 2004; 38:56–66.
- Gordon JA, Oriol NE, Cooper JB. Bringing good teaching cases “to life”: A simulation-based medical education service. Acad Med. 2004; 79:23–7.
- Gordon JA, Wilkerson WM, Shaffer DW, Armstrong EG. Practicing medicine without risk: Students’ and educators’ response to high-fidelity patient simulation. Acad Med. 2001; 76:469–72.
- Issenberg SB, Gordon MS, Gordon Dl, Safford RE, hart IR. Simulation and new learning technologies. Med Teach. 2001; 16:16–23.
- Issenberg SB, McGaghie WC, Gordon DL, Symes S, Petrusa ER, Hart IR, et al. Effectiveness of a Cardiology Review Course for Internal Medicine Using Simulation Technology and Deliberate Practice. Teach Learn Med. 2002; 14:223–8.
- Issenberg SB, McGaghie WC, Petrusa ER, Lee Gordon D, Scalese RJ. Feature and uses of high-fidelity medical simulations that lead to effective learning: A BEME systematic review. Med Teach. 2005; 27:10–28.
- Jeffries, PR. A framework for Designing, Implementing and Evaluating Simulation Used as Teaching Strategies in Nursing. Nurs Educ Perspect. 2005; 26:96–103.
- Jones A, McArdle PF, O’Neill PA. Howe well prepared are graduates for the role of pre-registration house officer? A comparison of the perceptions of new graduates and educational supervisors. Med Edu. 2001; 35:578–84.
- Kohn LT, Corrigan JM, Donaldson MS. To err is human: Building a safer health system. Washington DC: National Academy Press; 1999.
- Langdale LA, Schaad D, Wipf J, Marshall S, Vontver L, Scott CS. Preparing Graduates for the First Year of Residency: Are Medical Schools Meeting the Need? Acad Med. 2003; 78:39–44.
- Ledingham McA, Harden RM. Twelve tips for setting up a clinical skills training facility. Med Teach. 1998; 20:503–7.
- Massey-Pawadyira, J. (2023). Indwelling urinary catheter insertion 2: procedure for adults. Nursing Times, 2.
|
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2025 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).