Introduction
Medicine, despite its notable advances and its noble purpose of healing and preserving life, is not an infallible science. In their daily practice, healthcare professionals face a number of challenges and complexities that can sometimes lead to errors. These errors, known as medical errors, can have significant consequences for both patients and the healthcare system as a whole.
Definition and Scope of the Problem
A medical error can be defined as any act or omission committed by a healthcare professional during patient care that causes or has the potential to cause harm to the patient. These errors can occur at any stage of the care process, from diagnosis to treatment and follow-up. The extent of the problem is alarming, with recent studies suggesting that medical errors are a leading cause of death and disability worldwide. The World Health Organization estimates that millions of patients suffer preventable harm each year due to medical errors, resulting in considerable economic cost to healthcare systems and a considerable burden on patients and their families.
Medical errors can manifest themselves in a variety of ways, the most common types include:
Diagnostic errors: They include erroneous, delayed or missed diagnoses, as well as overdiagnosis, which can lead to unnecessary and potentially harmful treatments.
Treatment errors: They cover errors in prescribing, administering and monitoring medications, as well as errors in surgical procedures and other medical treatments.
Prevention errors: They refer to the failure to implement preventive measures, such as vaccination or disease screening, which can increase the risk of complications and diseases.
Communication errors: They include failures in communication between health professionals, as well as between professionals and patients, which can lead to misunderstandings and incorrect clinical decisions.
It is important to note that medical errors are not always the result of negligence or incompetence of healthcare professionals; they are often the result of a complex interaction of factors, including healthcare system limitations, lack of resources, patient fatigue, personnel, care pressure and cognitive biases.
Impact of Medical Errors on Public Health and the Economy
The impact of medical errors on public health is significant. In addition to the deaths and disabilities directly attributable to these errors, they can also lead to long-term complications, increase the length of hospital stays, require additional treatments, and decrease patient confidence in the healthcare system. From an economic point of view, medical errors represent a considerable burden on health systems. Direct costs include expenses associated with the treatment of complications and adverse events, as well as compensation for medical negligence. Indirect costs, such as lost productivity and social costs, are also relevant. Medical errors are a complex and multifactorial problem that affects patients, healthcare professionals and healthcare systems around the world. Its impact on public health and the economy is considerable, underscoring the urgent need to address this problem effectively. Despite advances in patient safety in recent decades, much remains to be done to ensure that all patients receive safe, quality health care.
Historical Perspective of Patient Safety
Patient safety has been a growing concern in recent decades. Although medical errors have existed since the beginning of medicine, it was not until the end of the 20th century that the problem began to be systematically addressed. In 1999, the United States Institute of Medicine published the report “To Err is Human: Building a Safer Health System”, which highlighted the magnitude of the problem and called for action to improve patient safety, since then, various initiatives have been implemented to reduce medical errors, including the creation of error reporting and learning systems, the promotion of safety culture, patient safety training for healthcare professionals and the development of tools and technologies to improve safety in healthcare. Despite these advances, medical errors remain a persistent problem. Health system complexity, human variability, and resource limitations continue to pose significant challenges to patient safety. It is essential to continue investigating the causes of medical errors and develop effective strategies to prevent them and mitigate their consequences.
The Silent Impact: An Analysis of the Types of Medical Errors
Medicine, despite its notable advances, is not an infallible science. Medical errors, although undesirable, are a reality that can affect any patient, regardless of their condition or the prestige of the medical institution. These errors, which can manifest in various forms, from misdiagnosis to poor communication, have a profound impact on the lives of patients and their families, generating consequences ranging from deterioration of health to loss of life. In this article, we will explore the different types of medical errors, classifying them according to their severity and consequences, and examine real cases that illustrate their impact. Medical errors are a worrying reality in the health field, with consequences that can be devastating for patients. It is essential to recognize the existence of these errors and work to prevent them through improving care processes, effective communication and continuous training of health professionals. Only in this way can we move towards a safer and more reliable health system, where patients receive the care they deserve without putting their well-being at risk.
Classification of Medical Errors According to Their Seriousness and Consequences
Medical errors can have varying consequences, from minor and temporary to serious and permanent. Below is a classification of medical errors according to their severity:
Mild adverse events: These are errors that cause minimal or temporary harm to the patient, such as a mild allergic reaction to a medication or a small infection at the site of an injection.
Moderate adverse events: They are errors that cause significant but reversible harm to the patient, such as a bone fracture during a fall in the hospital or an adverse reaction to a medication that requires hospitalization.
Serious adverse events: These are errors that cause permanent or life-threatening harm to the patient, such as a brain injury during surgery or a severe allergic reaction that causes anaphylactic shock.
Fatal adverse events: These are errors that result in the death of the patient, such as a fatal medication error or a serious nosocomial infection.
Examples of Medical Error Cases
Misdiagnosis: A patient with severe abdominal pain is diagnosed with indigestion and sent home, but in reality suffers from acute appendicitis that ruptures, causing peritonitis and putting his life at risk.
Medication error: A patient receives an excessive dose of an anticoagulant medication, causing severe internal bleeding and requiring an emergency blood transfusion.
Surgical error: During knee surgery, the surgeon accidentally injures a nerve, causing permanent loss of sensation in the patient's leg.
Communication error: A patient with a history of allergy to penicillin receives this antibiotic, despite having reported his allergy to the doctor. The patient suffers a severe anaphylactic reaction and requires urgent medical attention.
Contributing Factors to Medical Errors: A Multidimensional Analysis
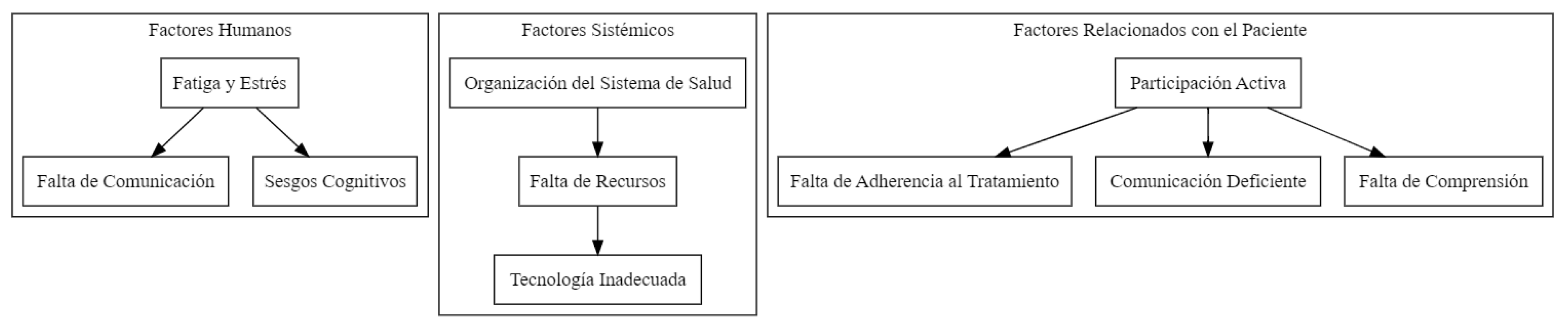
Medical errors, defined as preventable incidents that occur during the healthcare process, place a considerable burden on patients, their loved ones, and the healthcare system as a whole. These failures can manifest themselves in various ways, ranging from imprecise diagnoses to counterproductive therapies, and their repercussions can range from temporary discomfort to permanent consequences, even leading to the death of the patient. To develop effective prevention and mitigation strategies, it is crucial to understand the factors that lead to medical errors. Research in the fields of medicine and law has identified a wide range of elements that can increase the likelihood of these errors occurring. These factors can be grouped into three main categories: human, systemic and patient-related. Each of these categories encompasses a series of specific components that interact in an intricate way, generating an environment susceptible to the appearance of errors.
Chart 1.
Factors that contribute to medical error.
Chart 1.
Factors that contribute to medical error.
Human Factors: Lack of Healthcare Professionals
Health professionals, despite their training and experience, are human beings susceptible to errors. Fatigue, stress, lack of effective communication, and cognitive biases are some of the human factors that can compromise patient safety.
Fatigue and Stress: Excessive workload, long shifts, and lack of adequate rest can negatively affect the cognitive and physical performance of healthcare professionals, increasing the risk of errors. Fatigue can decrease attention, concentration, memory, and decision-making ability, while chronic stress can lead to emotional exhaustion and depersonalization, which can affect empathy and the quality of care provided.
Lack of Communication: Effective communication between members of the healthcare team is essential to ensure patient safety. Lack of clarity in the transmission of information, ambiguous verbal orders, lack of coordination between different professionals involved in patient care, and linguistic or cultural barriers can lead to misunderstandings and errors.
Cognitive Biases: Cognitive biases are systematic thinking patterns that can lead to erroneous judgments and decisions. In the medical context, these biases can influence the way professionals collect, interpret and process clinical information, which can lead to diagnostic and treatment errors. Some common cognitive biases in medical practice include confirmation bias (the tendency to seek information that confirms pre-existing beliefs), anchoring bias (the tendency to rely too much on the first information received), and availability bias (the tendency to overestimate the probability of events that are easily remembered).
Systemic Factors: The Context of Health Care
The health system in which medical care is provided can also contribute to errors. System organization, lack of resources, inadequate technology, and organizational culture are some of the systemic factors that can affect patient safety.
Organization of the Health System: The way the healthcare system is organized and managed can influence patient safety. Lack of clear protocols, fragmentation of care, lack of continuity of care, and lack of adequate supervision can increase the risk of errors. Additionally, pressure to reduce costs and increase efficiency can lead to work overload and staff reduction, which can compromise the quality of care.
Lack of Resources: Lack of human, material and financial resources can limit the ability of healthcare professionals to provide safe, quality care. Staff shortages can lead to work overload and burnout, while a lack of adequate medical equipment and supplies can make diagnosis and treatment difficult.
Inadequate Technology: Medical technology, while it can improve the efficiency and accuracy of care, can also be a source of errors if not used appropriately. Lack of training in the use of new technologies, lack of interoperability between different information systems and technical failures can contribute to medical errors.
Diagnostic Error: Definition and Types
Diagnostic error (DI) is a complex and multifaceted problem that affects medical practice at all levels of care. Although medicine has advanced significantly in recent decades, the possibility of misdiagnosis, delayed or missed diagnosis remains a worrying reality. The Institute of Medicine (IOM), now known as the National Academy of Medicine (NAM), defines ED as “the failure to establish an accurate and timely explanation of the patient's health problem or problems, or to communicate that explanation to the patient” . This patient-centered definition emphasizes the importance of not only reaching a correct diagnosis, but also conveying that information in a clear and understandable manner to the patient.
The Society for Improving Diagnosis in Medicine (SIDM) proposes a classification of EDs into three main categories:
Missed or missing diagnosis: When no explanation is found for the patient's symptoms, despite the diagnostic tests performed.
Wrong diagnosis: When the initial diagnosis turns out to be incorrect and the true cause of the symptoms is discovered later.
Delayed diagnosis: When the correct diagnosis is established, but with a significant delay that may have negatively affected the patient's prognosis or treatment.
It is important to note that these categories are not mutually exclusive and that, in many cases, a diagnostic error may involve a combination of them.
Factors of Diagnostic Error in Medicine
Medical diagnosis is a complex and crucial process in healthcare, which involves the identification of the disease or condition that affects a patient. However, despite advances in medicine, diagnostic errors remain a persistent and worrying problem. These errors in diagnosis can have serious consequences for the health and well-being of patients, including delays in treatment, inappropriate treatments and even death. The causes of diagnostic errors are multifactorial and can be attributed to a combination of cognitive, systemic, and patient-related factors.
I. Cognitive Factors
Cognitive factors refer to the mental processes that clinicians use to collect, interpret, and evaluate clinical information. Despite their training and experience, physicians are susceptible to a number of biases and cognitive limitations that can influence their judgment and lead to diagnostic errors.
-
Limitations of Human Reasoning
In addition to biases and heuristics, human reasoning has inherent limitations that can contribute to diagnostic errors. These limitations include:
- ∘
Limited information processing capacity: Clinicians must process large amounts of clinical information in a short period of time, which can lead to errors due to cognitive overload.
- ∘
Fatigue and stress: Fatigue and stress can affect attention span, memory, and judgment, increasing the likelihood of errors.
- ∘
Lack of knowledge or experience: Doctors can make diagnostic errors if they do not have the knowledge or experience necessary to recognize a particular disease.
II. Systemic Factors
Systemic factors refer to characteristics of the work environment and the organization of the health system that may contribute to diagnostic errors.
Lack of Time: Healthcare pressure and lack of time in medical consultations are important factors that can lead to diagnostic errors. Physicians often have to care for a large number of patients in a limited time, which can make it difficult to take a complete history and physical examination, as well as consider all possible diagnostic hypotheses.
Assistance Pressure: The pressure of care, especially in emergency departments or during times of high demand, can increase the stress and fatigue of doctors, which can affect their diagnostic ability. Furthermore, the need to make quick decisions in emergency situations can lead to errors due to lack of reflection and analysis.
Poor Communication: Poor communication between different health professionals caring for the same patient can be an important cause of diagnostic errors. Failure to share relevant information, misinterpretation of test results, or lack of coordination in patient follow-up can lead to delays in diagnosis or misdiagnoses.
Addressing Contributing Factors: Toward Safer Health Care
Preventing medical errors requires a multidimensional approach that addresses human, systemic, and patient-related factors. Some key strategies include:
Communication Improvement: Encourage open and effective communication between members of the healthcare team and between professionals and patients. This involves using clear and understandable language, actively listening, checking understanding, and encouraging patient participation in decision-making.
Training and Training: Provide ongoing training to healthcare professionals on patient safety, effective communication, teamwork and error management. Training in clinical reasoning and decision-making skills can also help reduce cognitive biases and improve diagnostic accuracy.
Optimization of Health Systems: Improve the organization and management of the health system, guaranteeing the availability of adequate resources, the implementation of clear protocols and continuity of care. Foster a culture of safety in which mistakes are seen as opportunities for learning and improvement, rather than cause for blame or punishment.
Technology Implementation: Use technology effectively to improve patient safety, such as implementing electronic clinical information systems, early warning systems, and decision support tools.
Patient Empowerment: Encourage the active participation of the patient in their care, providing clear and understandable information about their disease and its treatment, and promoting adherence to treatment.
The prevention of medical errors is an ongoing challenge that requires the commitment and collaboration of all actors in the health system. By addressing human, systemic and patient-related factors, we can create a safer healthcare environment and improve quality of life for patients. Patient safety is not a destination, but rather a continuous journey toward excellence in healthcare.
Overdiagnosis and Its Implications
Overdiagnosis is an increasingly recognized phenomenon in modern medicine and refers to the diagnosis of a medical condition that, if undetected, would never have caused symptoms or affected the patient's health. Overdiagnosis can occur due to a number of factors, including overuse of screening tests, lowering thresholds for defining diseases, and pressure to find explanations for the patient's symptoms.
The implications of overdiagnosis are significant. Firstly, it can lead to unnecessary treatment, which can be expensive, cause side effects and cause anxiety in the patient. Second, overdiagnosis can divert health system resources that could be used to treat patients with real and potentially serious illnesses. Finally, overdiagnosis can create a false sense of security in the patient, leading them to ignore important symptoms of other diseases.
Diagnostic and Therapeutic Cascades
Diagnostic and therapeutic cascades are a series of events triggered by an incidental finding in a diagnostic test or by a side effect of a treatment. These cascades can lead to unnecessary additional testing, potentially harmful treatments, and increased anxiety and stress in the patient. An example of a diagnostic cascade would be the finding of a lung nodule on a chest x-ray performed for another reason. This finding may lead to a CT scan, biopsy, and in some cases even surgery, even though most lung nodules are benign.
Diagnostic Error in Primary Care
Primary care is the first point of contact for most patients with the health system. Family physicians face a wide variety of patients, with a wide range of complexity, in a limited time and with limited diagnostic resources. This situation makes primary care professionals especially vulnerable to diagnostic errors.
Diagnostic errors in primary care can have serious consequences for patients, as they can delay the diagnosis and treatment of serious diseases, such as cancer or cardiovascular diseases. Furthermore, diagnostic errors can lead to unnecessary or even harmful treatments being prescribed, which can increase the risk of side effects and complications. Diagnostic error is a complex and multifaceted problem that affects all levels of healthcare, but especially primary care. It is essential to recognize the existence of these errors and their different types, including misdiagnosis, delayed diagnosis, missed diagnosis, and overdiagnosis. Furthermore, it is crucial to understand the underlying causes of these errors, which can be both cognitive and systemic.
Preventing diagnostic errors requires a multidisciplinary approach that includes improving doctor-patient communication, training and training in clinical reasoning, the use of diagnostic support tools, and the implementation of error reporting and learning systems. . Only through a joint effort by all actors in the health system can we reduce the incidence of diagnostic errors and improve patient safety.
The Impact of Diagnostic Error on Health
Medical diagnosis is the cornerstone of health care. An accurate and timely diagnosis allows the implementation of effective treatments, the prevention of complications and the improvement of the patient's quality of life. However, diagnostic errors, whether misdiagnoses, delayed or missed diagnoses, can have a devastating impact on the health and well-being of patients and their families. This article will explore the profound consequences of diagnostic errors, from deteriorating physical health to emotional suffering and financial burdens.
Consequences for the Patient's Health
The most direct and obvious impact of a diagnostic error is manifested on the patient's health. A misdiagnosis can lead to inappropriate or even harmful treatments, while a delayed diagnosis can allow a disease to progress to more advanced and difficult-to-treat stages. These situations can result in:
Increased morbidity: Morbidity refers to the presence of a disease or medical condition. Diagnostic errors can increase morbidity by delaying the initiation of appropriate treatment, which can lead to long-term complications and sequelae. For example, a late diagnosis of cancer can reduce the chances of survival and increase the risk of metastasis.
Increased mortality: In severe cases, diagnostic errors can have fatal consequences. A study published in the British Medical Journal estimated that medical errors, including diagnostic errors, are the third leading cause of death in the United States.
Decreased quality of life: Even when not fatal, diagnostic errors can significantly affect a patient's quality of life. Chronic pain, disability, anxiety and depression are just some of the possible long-term consequences of a misdiagnosis or delayed diagnosis.
Emotional and Psychological Consequences
The impact of a diagnostic error goes beyond the physical. Patients and their families may also experience a number of emotional and psychological consequences, including:
Anxiety and stress: Uncertainty and the lack of a clear diagnosis can generate high levels of anxiety and stress. Prolonged waiting for a diagnosis or receiving a misdiagnosis can be emotionally draining experiences.
Depression: The diagnosis of a serious illness or the lack of effective treatment can lead to depression. Additionally, the feeling of having been ignored or mistreated by the healthcare system can contribute to feelings of hopelessness and sadness.
Loss of confidence in the health system: A diagnostic error can erode patient trust in health professionals and the system in general. This can make it difficult to seek medical care in the future and affect the doctor-patient relationship.
Impact on family relationships: An erroneous or late diagnosis can generate tensions and conflicts within the family. Family members may experience feelings of guilt, frustration, and helplessness as they watch their loved one suffer without a clear diagnosis or effective treatment.
Economic Impact
Diagnostic errors also have a significant economic impact, both for patients and the healthcare system as a whole. These costs may include:
Additional medical expenses: Misdiagnosis or late diagnosis can lead to unnecessary tests and treatments, increasing medical expenses for the patient and the healthcare system.
Loss of productivity: Undiagnosed or misdiagnosed illnesses can lead to decreased work productivity, resulting in loss of income for the patient and their family.
Litigation costs: In some cases, diagnostic errors can lead to medical negligence claims, resulting in legal and compensation costs for healthcare professionals and healthcare institutions.
Burden on the health system: Diagnostic errors can increase the demand for health services, which can overload the system and affect the care of other patients.
Diagnostic errors have a multifaceted and profound impact on the health and well-being of patients and their families. From deteriorating physical health to emotional suffering and financial burdens, the consequences of a misdiagnosis or delayed diagnosis can be devastating. It is essential that health professionals, health institutions and policy makers work together to improve the accuracy and timeliness of medical diagnosis. Implementing prevention strategies, such as improving doctor-patient communication, training in clinical reasoning, and the use of diagnostic support tools, can help reduce the incidence of errors and ensure safer and more effective medical care for all. Preventing diagnostic errors is not only a matter of improving the quality of medical care, but also of protecting the health and well-being of patients and their families. By addressing this issue holistically, we can build a safer, fairer, and more patient-centered healthcare system.
Consequences of a medical error.
| Consequence |
Description |
| Patient harm |
It can manifest as physical harm, such as injuries or health complications, or as psychological harm, such as anxiety, depression, or loss of trust in the health system. |
| Delay or avoidance of appropriate treatment |
A wrong or late diagnosis can lead to the patient not receiving the necessary treatment in time, which can aggravate their condition and decrease their chances of recovery. |
| Unnecessary or dangerous treatment |
An incorrect diagnosis can result in the administration of treatments that the patient does not need, which may be ineffective or even harmful to their health. |
| Psychological repercussions |
A diagnostic error, especially a serious one, can have a significant emotional impact on the patient and their families, including anxiety, depression, post-traumatic stress, and loss of trust in health professionals. |
| Financial implications |
Medical errors can result in additional expenses for the patient and their family, such as additional treatment costs, loss of income due to inability to work, and legal expenses in the event of malpractice lawsuits. |
| Malpractice Lawsuits |
Patients affected by medical errors can file legal claims against the healthcare professionals or institutions involved, seeking compensation for damages suffered. |
| Impact on the reputation of the professional and the institution |
Medical errors, especially if made public, can damage the reputation of the healthcare professional and the institution where the error occurred, which can affect the trust of patients and the community at large. |
Strategies for Preventing Diagnostic Errors
Diagnostic errors represent a significant challenge in healthcare, negatively impacting patients' health and generating considerable costs for healthcare systems. Preventing these errors is an ethical and public health imperative that requires a multifaceted approach. In this article, we will explore various strategies aimed at minimizing the occurrence of diagnostic errors, focusing on improving doctor-patient communication, training and training in clinical reasoning and decision making, the use of diagnostic support tools, the implementation of error notification and learning systems, and the active participation of the patient in the diagnostic process.
Improved Doctor-Patient Communication
Effective communication between doctors and patients is essential for an accurate and timely diagnosis. The doctor-patient relationship should be based on trust, empathy and mutual respect. The physician must take sufficient time to listen carefully to the patient, understand his or her concerns, and obtain a complete and detailed medical history. Clear and understandable communication is essential to explain the diagnosis, prognosis and treatment options to the patient, ensuring that they understand the information and can actively participate in making decisions about their health.
Implementing strategies to improve doctor-patient communication may include:
Active listening: The doctor must pay full attention to the patient, avoiding interruptions and demonstrating genuine interest in their history and concerns.
Open-ended questions: The use of open-ended questions allows the patient to express their symptoms and concerns in their own words, providing valuable information for diagnosis.
Clear and simple language: Avoid the use of medical jargon and explain medical concepts in terms understandable to the patient.
Empathy and validation: Recognize and validate the patient's emotions, demonstrating understanding and support.
Shared decision making: Involve the patient in the decision-making process, explaining the different treatment options and their risks and benefits, and respecting their preferences and values.
Optimal interprofessional communication, as well as with patients, is essential for patient care. Therefore, communication errors often lead to adverse events. Reasons for poor communication include disruptive patient behavior, environmental distractions (e.g., cell phones and pagers), cultural differences, hierarchy issues, personality differences, language barriers, and socioeconomic variables such as education and literacy.
A courteous and respectful workplace where the interprofessional team collaborates promotes a safe work environment for all members of the healthcare team, families and patients. Risk management committees and interprofessional working groups should work collaboratively on risk assessment and reduction. Co-education programs help providers and support staff learn roles and develop relationships to improve safety.
Additionally, healthcare personnel should avoid common errors in written communication, such as using non-standard abbreviations, illegible handwriting, failing to question inappropriately written orders, and failing to complete correct specimen labeling. Therefore, staff should be encouraged to ask questions when they are unsure and trained to double-check that the patient's name is spelled correctly and that the patient's correct date of birth is listed.
Clinicians must also follow well-communicated protocols that guide care and communication with patients. Providers should listen to patients' questions about how care is provided. Concerns should be respected and accepted if care plans contradict established evidence-based medicine. Implementation of standardized physician-family communication at the patient's bedside with family involvement and two-way communication also reduced the frequency of harmful medical errors and positively influenced the family experience. Communication errors during patient transfer can occur when incorrect information is passed to the receiving physician or pertinent information is omitted. Several techniques developed to minimize errors during patient transfer include the use of electronic records and mnemonics (e.g., situation, background, assessment, and recommendation [SBAR]) to address all pertinent information. The SBAR tool is considered a best practice communication technique for delivering information in an organized and logical manner during handover and critical patient care situations. [43]
The U.S. National Academies of Sciences, Engineering, and Medicine also recommends that these handoffs occur in real time and allow the opportunity to ask and answer questions about relevant facts about patient care. This principle should also be used when discharging patients from the hospital. Clinicians should remember to perform a final bedside assessment and review discharge instructions before sending any patient home, including giving the patient a complete written follow-up plan, advice on new medications, and instructions for returning to the hospital or to the office if new or worsening symptoms appear.
Education and Training in Clinical Reasoning and Decision Making
Clinical reasoning and decision making are essential skills for healthcare professionals. Education and continuous training in these areas are essential to improve diagnostic accuracy and reduce errors. Training programs should include teaching clinical reasoning strategies, such as generating diagnostic hypotheses, searching for and evaluating evidence, and making decisions based on the best available evidence. Additionally, it is important to address cognitive biases that may influence the diagnostic process. Health professionals must be aware of these biases and learn to recognize and mitigate them. Training in metacognition, that is, the ability to reflect on one's own thinking, can help doctors identify and correct errors in their clinical reasoning.
Clinical Importance
Medical errors are a common cause of injury or death in the United States. Healthcare professionals work hard to save countless lives; however, the incidence of concomitant errors is high. All health professions should focus on the effort to “do no harm” and work to reduce human and system errors. Most medical errors do not occur solely as a result of one doctor or group of doctors; most are due to system or process failures that lead to errors, such as holding dangerous and routine medications together without a pharmacist's supervision or cost control measures that increase workload and the rate of medical errors.
Errors can be prevented by modifying processes to make it more difficult to perform incorrect actions, such as using electronic systems for various aspects of patient care. However, changes cannot be made to systems and processes unless problems are identified. Through reporting protocols, medical error pattern recognition, root cause analysis, and outcome monitoring can be performed to address institutional deficiencies. [1] However, healthcare professionals may be reluctant to report errors for fear of sanctions or legal consequences. While people must be held accountable for their individual errors, the system and culture must be reviewed so that error reporting leads to system improvement, not individual punishment. [45]
The greatest good for the greatest number of patients is achieved when processes consistently focus on quality improvement and avoiding repetition of the same mistake. While they want greater safety for patients, healthcare professionals and other staff may fear that reporting an incident could lead to disciplinary action, including losing their jobs. While failure to report medical errors contributes to the likelihood of serious harm to patients, many healthcare institutions have rigid policies that create a contentious environment. This can cause staff to hesitate to report errors, minimize problems, or fail to document problems, contributing to an evolving cycle of medical errors and ultimately tarnishing a healthcare institution's reputation. [8]
Therefore, an essential first step in reducing medical errors is to encourage reporting by removing any barriers that may exist so that adverse events and near misses can be identified. The most common barrier to reporting medical errors is fear of consequences. [46] Implementing confidential notification options is critical to the success of a notification system to overcome any concerns a person may have. [1] Additionally, changing workplace culture, in addition to developing protocols to address medical errors, can encourage the reporting of medical errors. Adopting a culture of patient safety, in which doctors are empowered and rewarded for identifying medical errors that could lead to patient harm, has been shown to overcome fear of consequences. Consequently, patient safety improves with institutional cultures that incorporate both training and improvement efforts aimed at system redesign and an environment where people feel safe from retaliation. Everyone on the healthcare team must play a role in making healthcare safer for patients and healthcare workers.
Implementation of Error Notification and Learning Systems
Implementing error reporting systems is essential to learn from errors and improve patient safety. These systems must be confidential and non-punitive, promoting safety culture and organizational learning. Errors must be analyzed systematically to identify root causes and develop effective prevention strategies.
Patient safety training should be an integral part of the education and training of health professionals. Students and residents must learn to identify, report and analyze errors, and to actively participate in improving patient safety.
Patient Participation in the Diagnostic Process
Active patient participation in the diagnostic process is crucial to improve diagnostic accuracy and reduce errors. Patients should be encouraged to share relevant information about their medical history, symptoms, and concerns. They should also be informed about the diagnostic tests and proposed treatments, and given the opportunity to ask questions and express their preferences. Access to the electronic medical record can be a powerful tool to empower patients and encourage their participation in the diagnostic process. Patients can review their medical records, ask questions, and share additional information with their doctors. Preventing diagnostic errors requires a comprehensive approach that addresses both human and systemic factors. The improvement of doctor-patient communication, training and training in clinical reasoning and decision making, the use of diagnostic support tools, the implementation of error notification and learning systems, and the active participation of the patient in the diagnostic process are key strategies to achieve this objective. It is essential to foster a culture of safety in which errors are seen as opportunities for learning and improvement, rather than as grounds for blame or punishment. Collaboration between healthcare professionals, patients and healthcare organizations is essential to create a safer healthcare environment and improve the quality of healthcare.
Ethical Considerations in the Prevention and Management of Medical Errors
Medical practice, despite its noble purpose of preserving and improving health, is not exempt from the possibility of error. Medical errors, whether diagnostic, treatment or any other type, can have significant consequences for patients, their families and the health professionals involved. In this context, ethics plays a fundamental role in the prevention and management of these errors, guiding actions and decisions towards the protection of patients and the promotion of safe and quality medical care.
The Importance of Transparency and Open Communication with the Patient
Transparency and open communication are fundamental pillars of a doctor-patient relationship based on trust and mutual respect. When a medical error occurs, honesty and timely communication are essential to maintaining this trust and allowing the patient to make informed decisions about their health.
The duty to inform. The doctor's duty to inform the patient about a medical error that has affected him or her is supported by fundamental ethical principles, such as respect for the patient's autonomy and the principle of beneficence. The patient has the right to know the truth about his or her health and to actively participate in decisions that affect it. Concealing a medical error not only violates these rights, but can also have negative consequences for the patient's health, as it may prevent them from receiving appropriate treatment or taking steps to prevent future complications.
Benefits of open communication. Open communication about medical errors can have several benefits for both the patient and the healthcare professional. For the patient, open communication can:
Reduce anxiety and uncertainty: Knowing what happened and why can help the patient better understand their situation and feel more in control.
Facilitate informed decision making: Knowing the consequences of the error and the available treatment options allows the patient to make informed decisions about their care.
Strengthen the doctor-patient relationship: Honesty and transparency can foster trust and mutual respect, which is essential for an effective therapeutic relationship.
For the health professional, open communication can:
Relieve emotional burden: Admitting a mistake and apologizing can help a doctor deal with guilt and prevent burnout.
Encourage learning and improvement: Recognizing errors and analyzing their causes can help doctors learn from them and take steps to prevent future errors.
Improve reputation: Honesty and transparency can strengthen patients' trust in the doctor and the health institution.
Barriers to open communication. Despite the benefits of open communication, there are barriers that can make it difficult. Doctors can fear the legal or professional repercussions of admitting a mistake, or they may feel ashamed or guilty. Patients, for their part, may feel intimidated or distrust the health system. Overcoming these barriers requires a cultural change in which mistakes are seen as opportunities for learning and improvement, rather than personal failures.
The Physician's Duty to Report Errors and Their Consequences
The physician's duty to inform the patient of a medical error is not limited to simply admitting that an error occurred. The doctor must also explain the consequences of the error, both those that have already occurred and potential future complications. In addition, you must offer the patient treatment and follow-up options, and answer their questions in a clear and understandable manner. The information provided to the patient must be complete, accurate and adapted to their level of understanding. The doctor should avoid the use of medical jargon and explain complex concepts simply and clearly. You should also ensure that the patient has understood the information provided and give them the opportunity to ask questions.. Informing a patient of a medical error can be an emotionally difficult experience for both the patient and the doctor. The doctor must show empathy and understanding, and offer the patient emotional support and resources to help him deal with the consequences of the error. The doctor must ensure that the patient receives the necessary follow-up and medical care after a medical error. This may include referring you to specialists, scheduling additional tests, or adjusting treatment. The doctor should also maintain open communication with the patient and respond to their questions or concerns as they arise.
Nursing, Allied Health, and Interprofessional Team Interventions
To effectively reduce medical error rates and keep their patients safe, healthcare organizations must restructure nursing work environments, particularly hospitals and long-term care facilities. Inappropriate work environments, excessive work hours, and high workloads can lead to missed nursing care and increased risk of adverse events. [49] According to the Institute of Medicine (IOM), fatigue during shift work increases error rates and should be addressed to improve patient safety. [50] They propose the following recommendations to combat nursing fatigue during shift work:
Avoid scheduling long periods of wakefulness. Long shifts with more than 17 hours of wakefulness can negatively affect task performance, which is equivalent to the legal limit for alcohol intoxication.
Avoid scheduling more than 4 consecutive 12-hour shifts.
Avoid short rest periods. Rest periods of less than 8 hours can cause excessive fatigue during the next shift.
Avoid extending work hours beyond what was previously scheduled for the day.
According to the IOM report, these interventions are intended to guide scheduling and are not absolute for work hours. Additionally, the IOM stated that the overall error rate for nurses was approximately 0.00336 errors per hour worked, which did not increase significantly with overtime work, working longer than scheduled on a given day, or working of additional shifts unless the length of the shift exceeded 12 consecutive hours. [50] When shift lengths exceeded 12 hours, a substantial increase in the error rate was observed even if the shift was voluntarily scheduled. The IOM subsequently asked legislative and regulatory bodies to prohibit nursing staff from providing patient care for more than 12 hours in a given 24-hour period under any circumstances. The IOM also recommended limiting direct nursing patient care to 60 hours every 7 days. Other interventions recommended by the IOM focus on establishing a work environment that allows easy follow-up of patients, limits interruptions, and minimizes administrative tasks. Special education and training should be provided for error-prone tasks such as medication administration, patient transfer, and supervision of trainees. [50] The latter is essential to promote a continued culture of patient safety and error-free medication administration. A recent study that surveyed nursing students about their perception of medical errors made during direct patient care reported that "less knowledge" about the task or procedure and "lack of supervision" were the main causes of medical errors they made during training. An overall commitment to patient safety at the organizational level greatly influences a nurse's adherence to and compliance with patient safety principles. Creating an organizational patient safety climate, managing workload, reducing time pressure, and providing education to improve knowledge and skills improve your adherence to patient safety principles. Implementation of patient safety interventions should be followed by close monitoring of medical errors, near misses, and nurse fatigue, as non-punitive, focused, and effective feedback can improve patient safety adherence and clinical results. Additionally, emphasis should be given to people who require personal motivation, resist change, or are reluctant to innovate. These individuals need empowerment and a nonjudgmental approach in their training on patient safety practices. Improving knowledge of patient care tasks and the extent of medical errors that can be prevented by adherence to patient safety principles has been shown to improve your commitment to patient safety.
Improve Healthcare Team Outcomes
Medical errors are a major concern for patient safety in the healthcare sector. Healthcare professionals and policy makers can reduce medical errors by focusing on clinical education and the implementation of healthcare protocols that avoid the most common errors. [48] Unintentional medical errors are always likely to occur. However, the risk of medical errors can be significantly reduced by encouraging error reporting, standardized communication systems, electronic data and order entry, medication reconciliation, and clinical care protocols for error prevention. Physicians, healthcare professionals, nurses, pharmacists, surgical and pharmaceutical technicians, and other members of the healthcare team must work together to identify deficiencies that lead to medical errors and implement preventative strategies. Interventions such as surgical checklists, medication reconciliation, and confirmation of verbal orders are only effective when these individual team members contribute to improving patient safety. Additionally, each healthcare professional is responsible for monitoring the patient and creating an environment that encourages effective communication to help minimize clinical errors. Additionally, accreditation agencies and training programs should continually focus on improving patient safety and teaching ways to reduce common medical errors. A collaborative interprofessional team of these agencies, clinicians, and administrators can identify inherent system and process deficiencies and develop corrective measures to reduce the incidence of medical errors in the healthcare industry.
The Role of Ethics Committees in the Management of Medical Errors
Ethics committees play a crucial role in the management of medical errors, providing guidance and support to both patients and healthcare professionals. These committees are composed of experts in ethics, medicine, law, and other relevant disciplines, and their primary function is to promote ethical, quality healthcare. Analysis and resolution of ethical conflicts. Ethics committees can help analyze and resolve ethical conflicts that arise in connection with medical errors. These conflicts may involve difficult decisions about treatment, disclosure of information, or allocation of resources. The ethics committee can provide an unbiased and objective perspective and help the parties involved reach a fair and ethical solution. Development of policies and procedures. Ethics committees can also contribute to the development of policies and procedures to prevent and manage medical errors. These policies may include protocols for reporting errors, communicating with patients, and implementing corrective measures. The ethics committee can help ensure that these policies are ethical and respectful of patients' rights. Ethics committees play a crucial role in the management of medical errors, acting as safeguards that promote integrity and accountability in healthcare. Below are relevant examples from the literature that highlight its importance.
Functions of the Ethics Committees
Protection of Human Rights: Ethics committees are essential to protect the rights of patients and ensure that medical practices are carried out ethically. Its creation is justified by the need to legislate on the use of human organs and critical end-of-life decisions, which highlights its role in preventing abuses and errors in medical care.
Evaluation of Research Projects: Health research ethics committees are responsible for evaluating projects to ensure the protection of participants and scientific integrity. This includes reviewing research protocols that could be related to medical errors, ensuring that ethical practices are followed and that risks to patients are minimized[5,8].
Confidence Building: These committees not only address ethics in research, but also foster trust between healthcare professionals and patients. By establishing a framework for ethical discussion, committees help resolve conflicts and make consistent decisions, which is essential for the management of medical errors.
Independence and Autonomy: The independence of ethics committees is crucial to their effectiveness. They must operate without outside influences to fairly evaluate cases of medical errors and ensure that decisions are made based on sound ethical principles.
Ethics committees are essential in the management of medical errors, as they protect the rights of patients, evaluate ethics in research, and foster trust in the health system. Your independence and ability to address ethical dilemmas are critical to improving the quality of healthcare and preventing future errors.
Preventing and managing medical errors is a complex challenge that requires a multifaceted approach. Ethics plays a crucial role in this process, guiding actions and decisions toward protecting patients and promoting safe, quality healthcare. Transparency, open communication, the duty to inform and the role of ethics committees are key elements to address medical errors in an ethical and responsible manner, promoting a culture of safety and learning in the field of health.
Legal Liability for Diagnostic Errors: A Legal Analysis
Medicine, despite its advances, is not an exact science. The medical act, particularly diagnosis, is subject to the uncertainty inherent to human knowledge and the variability of biological responses. This reality opens the door to the possibility of errors, which, in certain circumstances, can generate legal liability for the healthcare professional. The doctor-patient relationship is configured as a service leasing contract, in which the doctor undertakes to provide his or her professional services with due diligence. Jurisprudence has established that this obligation is one of means, not results. That is, the doctor does not guarantee the patient's cure, but rather undertakes to put at his disposal all the means at his disposal to achieve that end. In the event of failure to comply with this obligation, whether by action or omission, the doctor may incur civil liability. Diagnostic error, as we will see below, can be one of the manifestations of this non-compliance. In cases of medical liability due to diagnostic error, the burden of proof falls on the patient or their family members. That is, they are the ones who must demonstrate that the doctor acted negligently or recklessly, that damage occurred and that there is a causal relationship between the medical action and the damage suffered. Proving medical negligence or recklessness can be complex, since it requires proving that the doctor deviated from the "lex artis ad hoc", that is, the body of knowledge and practices accepted by the medical community at the time of the action. To do this, medical experts are usually used to evaluate the professional's performance in light of the standards of the profession.
Furthermore, the existence of real and certain damage must be proven, as well as the causal link between the medical action and the damage. This involves demonstrating that the diagnostic error was the direct and determining cause of the harm suffered by the patient.
Concepts of Guilt, Negligence and Recklessness
Fault, in the field of medical civil liability, refers to the lack of diligence or care in professional performance. It manifests itself in two forms:
Negligence: Omission of due diligence. That is, the doctor does not do what he should do according to the standards of the profession. For example, not performing the necessary diagnostic tests for the patient's symptoms.
Imprudence: Hasty or reckless action, without taking due precautions. For example, performing a medical procedure without having the necessary training or experience.
For civil liability to exist, the fault must be serious. A simple diagnostic error, without negligence or recklessness, is not sufficient to generate liability. Jurisprudence has recognized the difficulty inherent in medical diagnosis and has established that error, by itself, does not constitute liability.
Legal liability for diagnostic errors is a complex and delicate issue. The doctor has the obligation to act with due diligence, in accordance with the "lex artis ad hoc", but a guaranteed result cannot be required. The burden of proof falls on the patient, who must demonstrate medical negligence or recklessness, the damage suffered and the causal relationship between the two. It is important to note that not every diagnostic error generates civil liability. The fault must be serious and there must be real and certain damage caused by the medical action. Jurisprudence has evolved towards a more objectivist conception of fault, but continues to recognize the difficulty inherent in the medical act and the need to assess each case individually. Preventing diagnostic errors is a constant challenge for the health system. The continuous training of professionals, the improvement of doctor-patient communication and the implementation of diagnostic support tools are some of the key strategies to reduce the incidence of these errors and guarantee safer and quality health care.
References
- **Instituto de Medicina.** (1999). *To Err is Human: Building a Safer Health System*. Washington, DC: National Academy Press.
- **Organización Mundial de la Salud.** (s.f.). *Estimaciones sobre errores médicos*.
- **Sociedad para Mejorar el Diagnóstico en Medicina (SIDM).** (s.f.). *Clasificación de los errores de diagnóstico*.
- **British Medical Journal.** (s.f.). *Estudio sobre errores médicos en Estados Unidos*.
- **Instituto de Medicina (IOM).** (s.f.). *Informe sobre la fatiga durante el trabajo por turnos*.
- **Academias Nacionales de Ciencias, Ingeniería y Medicina de los Estados Unidos.** (s.f.). *Recomendaciones para la transferencia de pacientes*.
- **Instituto de Medicina (IOM).** (s.f.). *Recomendaciones para la programación de turnos de enfermería*.
- **Instituto de Medicina.** (2001). *Crossing the Quality Chasm: A New Health System for the 21st Century*. Washington, DC: National Academy Press.
- **World Health Organization.** (2019). *Global Patient Safety Action Plan 2021–2030*. Geneva: WHO.
- **Agency for Healthcare Research and Quality.** (2020). *Patient Safety: Achievements and Challenges*. Rockville, MD: AHRQ.
- **National Institute for Health and Care Excellence.** (2021). *Patient Safety and Quality Improvement*. London: NICE.
- **American Medical Association.** (2022). *Addressing Medical Errors: A Guide for Physicians*. Chicago, IL: AMA.
- **Institute for Healthcare Improvement.** (2023). *Reducing Medical Errors: Strategies for Improvement*. Cambridge, MA: IHI.
- **European Commission.** (2023). *Patient Safety in Europe: Current Challenges and Future Directions*. Brussels: EC.
- **Canadian Patient Safety Institute.** (2023). *Safer Healthcare Now!: A National Patient Safety Initiative*. Edmonton, AB: CPSI.
|
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2025 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (http://creativecommons.org/licenses/by/4.0/).