Submitted:
06 September 2024
Posted:
09 September 2024
You are already at the latest version
Abstract
Keywords:
1. Introduction
1.1. Background
2. Materials and Methods
2.1. Design
2.2. Study Setting and Participants (Inclusion and Exclusion Criteria):
2.3. Data Collection
2.4. Data Analysis
2.5. Rigour and Reflexivity
3. Results
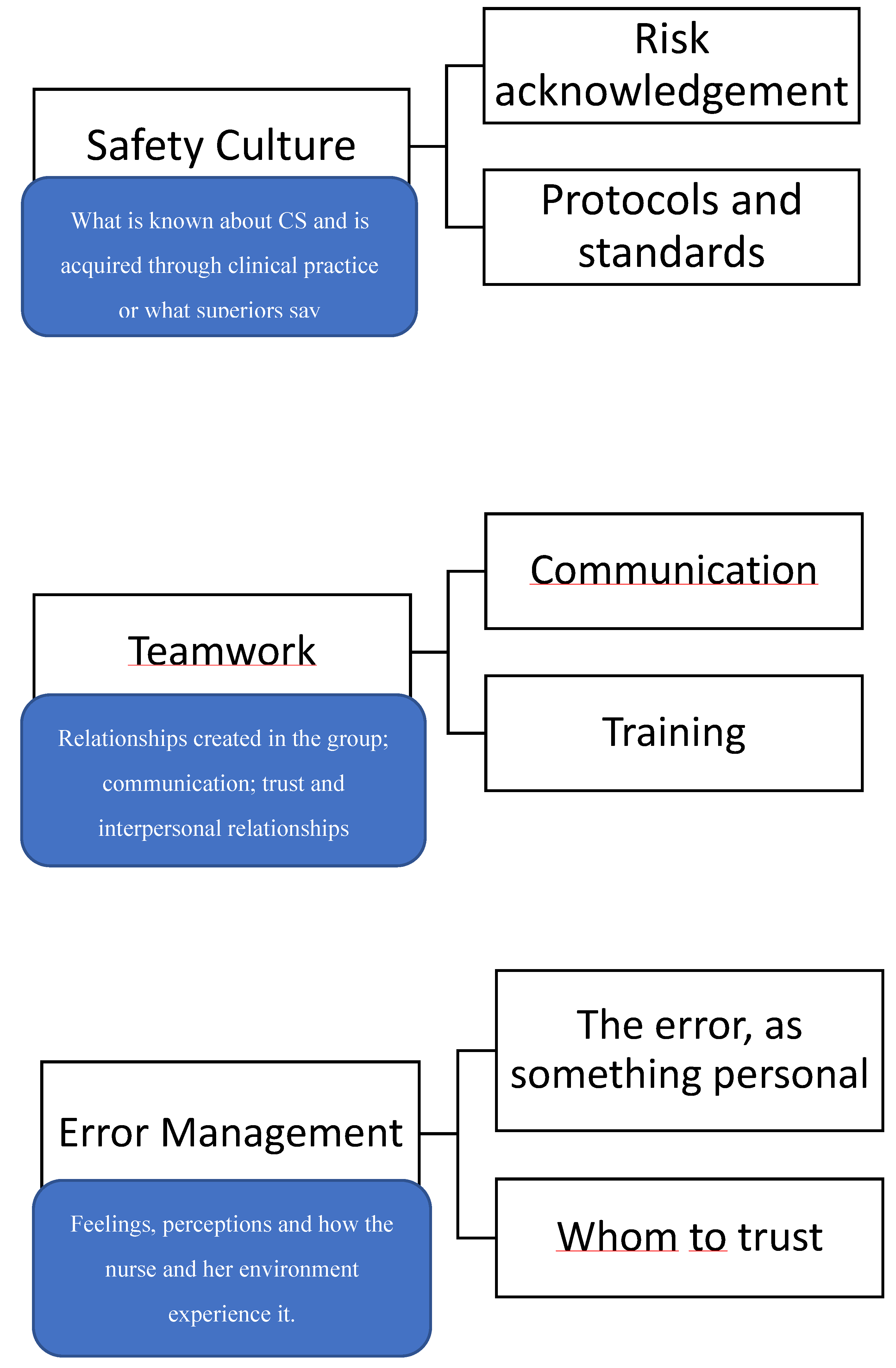
3.1. Safety Culture
3.1.1. Risk Acknowledgement
3.1.1. Protocols and Standars
3.2. Team Work:
3.2.1. Communication:
3.2.2. Training:
3.3. Error Management:
3.3.1. The Error, as Something Personal:
3.3.2. Whom to Trust:
4. Discussion
4.1. Strengths and Limitations:
4.2. Recommendations for Further Research
5. Conclusions
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Public
Guidelines and Standards Statement
Use of Artificial Intelligence
Conflicts of Interest
Appendix A
References
- World Health Organization Global Patient Safety action Plan 2021-2030: Towards eliminating avoidable harm in health care. 2021.
- Patient Safety. Available online: https://www.who.int/es/news-room/fact-sheets/detail/patient-safety (accessed on 30 May 2024).
- Gonzales, K. Medication administration errors and the pediatric population: A systematic search of the literature. J Pediatr Nurs 2010, 25, 555–565. [Google Scholar] [CrossRef] [PubMed]
- Sutherland, A.; Phipps, D.L.; Tomlin, S.; Ashcroft, D.M. Mapping the prevalence and nature of drug related problems among hospitalised children in the United Kingdom: A systematic review. BMC Pediatr 2019, 19, 486. [Google Scholar] [CrossRef] [PubMed]
- Mittiga, M.R., MD; Geis, G.L., MD; Kerrey, Benjamin T., MD, MS; Rinderknecht, A.S., MD The Spectrum and Frequency of Critical Procedures Performed in a Pediatric Emergency Department: Implications of a Provider-Level View. Annals of emergency medicine, 2012; 61, 263–270. [CrossRef]
- Gates, P.J.; Baysari, M.T.; Gazarian, M.; Raban, M.Z.; Meyerson, S.; Westbrook, J.I. Prevalence of Medication Errors Among Paediatric Inpatients: Systematic Review and Meta-Analysis. Drug Saf 2019, 42, 1329–1342. [Google Scholar] [CrossRef]
- Woo, M.W.J.; Avery, M.J. Nurses' experiences in voluntary error reporting: An integrative literature review. Int J Nurs Sci 2021, 8, 453–469. [Google Scholar] [CrossRef]
- Garfinkel, H. Estudios en Etnometodología, Anthropos: Barcelona, 2006.
- Taylor, S.J.; Bogdan, R. Introducción a métodos cualitativos de investigación, Paidós: Barcelona, 2002.
- Lincoln, Y.S.; Guba, E.G. Naturalistic inquiry, Sage Publications: Beverly Hills, 1985.
- Denzin, N.K.; Lincoln, Y.S. The Sage Handbook of Qualitative Research, Gedisa: Barcelona, 2015.
- Tong, A.; Sainsbury, P.; Craig, J. Consolidated criteria for reporting qualitative research (COREQ): A 32-item checklist for interviews and focus groups. International journal for quality in health care 2007, 19, 349–357. [Google Scholar] [CrossRef]
- Wu, A.W. Medical error: The second victim. BMJ 2000, 320, 726–727. [Google Scholar] [CrossRef]
- Delacroix, R. Exploring the experience of nurse practitioners who have committed medical errors: A phenomenological approach. J Am Assoc Nurse Pract 2017, 29, 403–409. [Google Scholar] [CrossRef]
- Vanhaecht, K.; Seys, D.; Russotto, S.; Strametz, R.; Mira, J.; Sigurgeirsdóttir, S.; Wu, A.W.; Põlluste, K.; Popovici, D.G.; Sfetcu, R.; Kurt, S.; Panella, M. An Evidence and Consensus-Based Definition of Second Victim: A Strategic Topic in Healthcare Quality, Patient Safety, Person-Centeredness and Human Resource Management. Int J Environ Res Public Health 2022, 19, 16869. [Google Scholar] [CrossRef] [PubMed]
- Dirik, H.F.; Samur, M.; Seren Intepeler, S.; Hewison, A. Nurses' identification and reporting of medication errors. J Clin Nurs 2019, 28, 931–938. [Google Scholar] [CrossRef]
- Mahat, S.; Rafferty, A.M.; Vehviläinen-Julkunen, K.; Härkänen, M. Negative emotions experienced by healthcare staff following medication administration errors: A descriptive study using text-mining and content analysis of incident data. BMC health services research 2022, 22, 1474. [Google Scholar] [CrossRef]
- Alomari, A.; Wilson, V.; Solman, A.; Bajorek, B.; Tinsley, P. Pediatric Nurses' Perceptions of Medication Safety and Medication Error: A Mixed Methods Study. Compr Child Adolesc Nurs 2018, 41, 94–110. [Google Scholar] [CrossRef] [PubMed]
- Lee, J. Understanding nurses' experiences with near-miss error reporting omissions in large hospitals. Nurs Open 2021, 8, 2696–2704. [Google Scholar] [CrossRef]
- Granel, N.; Manresa-Domínguez, J.M.; Watson, C.E.; Gómez-Ibáñez, R.; Bernabeu-Tamayo, M.D. Nurses' perceptions of patient safety culture: A mixed-methods study. BMC health services research 2020, 20, 584. [Google Scholar] [CrossRef]
- Yousef, A.; Abu Farha, R.; Da'meh, K. Medication administration errors: Causes and reporting behaviours from nurses perspectives. Int J Clin Pract 2021, 75, e14541. [Google Scholar] [CrossRef]
- Ferrús, L.; Silvestre, C.; Olivera, G.; Mira, J.J. Qualitative Study About the Experiences of Colleagues of Health Professionals Involved in an Adverse Event. J Patient Saf 2021, 17, 36–43. [Google Scholar] [CrossRef]
- Guerra-Paiva, S.; Lobão, M.J.; Simões, D.G.; Fernandes, J.; Donato, H.; Carrillo, I.; Mira, J.J.; Sousa, P. Key factors for effective implementation of healthcare workers support interventions after patient safety incidents in health organisations: A scoping review. BMJ Open 2023, 13, e078118. [Google Scholar] [CrossRef] [PubMed]
- The Role of Undergraduate Nursing Education in Patient Safety. Available online: https://psnet.ahrq.gov/perspective/role-undergraduate-nursing-education-patient-safety (accessed on 13 May 2024).
- Pardo Hernández, A.; Claveria Fontán, A.; García Urbaneja, M.; López Barba, J. Las unidades funcionales para la gestión de riesgos sanitarios (seguridad del paciente). Medicina Clínica 2008, 131, 64–71. [Google Scholar] [CrossRef] [PubMed]
- Alteren, J.; Hermstad, M.; Nerdal, L.; Jordan, S. Working in a minefield; Nurses’ strategies for handling medicine administration interruptions in hospitals, -a qualtiative interview study. BMC health services research 2021, 21, 1–1094. [Google Scholar] [CrossRef]
- Martyn, J.; Paliadelis, P. Safe medication administration: Perspectives from an appreciative inquiry of the practice of registered nurses in regional Australia. Nurs Educ Pract 2019, 34, 111–116. [Google Scholar] [CrossRef]
- Baraki, Z.; Abay, M.; Tsegay, L.; Gerensea, H.; Kebede, A.; Teklay, H. Medication administration error and contributing factors among pediatric inpatient in public hospitals of Tigray, northern Ethiopia. BMC Pediatr 2018, 18, 321. [Google Scholar] [CrossRef]
- Martyn, J.; Paliadelis, P.; Perry, C. The safe administration of medication: Nursing behaviours beyond the five-rights. Nurse Education in Practice 2019, 37, 109–114. [Google Scholar] [CrossRef] [PubMed]
- Rohde, E.; Domm, E. Nurses’ clinical reasoning practices that support safe medication administration: An integrative review of the literature. J Clin Nurs 2018, 27, e402–e411. [Google Scholar] [CrossRef] [PubMed]
- Vaismoradi, M.; Tella, S.; A Logan, P.; Khakurel, J.; Vizcaya-Moreno, F. Nurses' Adherence to Patient Safety Principles: A Systematic Review. Int J Environ Res Public Health 2020, 17. [Google Scholar] [CrossRef] [PubMed]
- Niemann, D.; Bertsche, A.; Meyrath, D.; Koepf, E.D.; Traiser, C.; Seebald, K.; Schmitt, C.P.; Hoffmann, G.F.; Haefeli, W.E.; Bertsche, T. A prospective three-step intervention study to prevent medication errors in drug handling in paediatric care. J Clin Nurs 2015, 24, 101–114. [Google Scholar] [CrossRef]
- Stang, A.; Thomson, D.; Hartling, L.; Shulhan, J.; Nuspl, M.; Ali, S. Safe Care for Pediatric Patients: A Scoping Review Across Multiple Health Care Settings. Clin Pediatr 2018, 57, 62–75. [Google Scholar] [CrossRef]
| Topics | Questions |
|---|---|
| Safety barriers * | Which patient safety policies are implemented? Who makes those policies? |
| What is your opinion about those safety policies? | |
| Do you feel any difficulties putting them in place? What is the team's opinion? In your opinion, what is the most relevant aspect of safe clinical practice? | |
| Making an error process | Why do you think ME happen? When is the most critical moment for treatment administration? |
| Who are the most vulnerable patients? About an ME, could you tell me in your opinion what happened? If you were back in time, is there anything you could have done differently? Did you talk to your colleagues? How do you manage the situation with the patients? Is it always the same protocol? In case of a ME, do you inform the relatives? Who does it? Do you think relevant they know about it? What is your perception of other colleagues' experiences? How is it felt among the team when a ME happens? What is your opinion about ME notification? Do you consider it useful to prevent errors? What is your guess about your colleagues' ME perception? In your opinion, which factors contribute to a ME? | |
| Support perception | What happens in the department when an ME occurs? |
| In case an ME happens while you are on shift, how is an ME managed? Are they always managed in the same way? What it depends on? | |
| Do you do some training with the team after a serious ME happened? Do you think there is any factor that helps to minimize the consequences on the team? | |
| What is the response from the management team and the institution? | |
| Personal repercussion of making a mistake | Did this incident have any repercussions on the rest of the shift? On the following days? Has an ME, either yours or by a colleague, changed the way you interact with the team, relatives, or patients? What did you feel when you realize you made a mistake? |
| How would you feel if they implemented a new policy after you or a colleague made a mistake? Has any of these ME changed the way you work? | |
| Solutions | What is your perception about safety measures taken in place, for example, a double check of medication? Do you think the current reporting system is useful and practical? Do you think there is a way to avoid ME or to get almost all ME to get reported? In your opinion, what is the most relevant aspect of the topic? If you could decide, would you make any changes? How do you feel when a new clinical safety measure is implemented? |
| Code | Age | Safety Lead | Years in paediatric emergency |
|---|---|---|---|
| E1 | 35 | No | 7 years |
| E2 | 23 | No | 20 months |
| E3 | 36 | No | 16 years |
| E4 | 55 | No | 17 months |
| E5 | 35 | No | 18 months |
| E6 | 39 | Yes | 16 years |
| E7 | 39 | Yes | 5 years |
| E8 | 35 | Yes | 6 years |
| E9 | 50 | Yes | 7 years |
| E10* | 27 | No | 3 years |
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2024 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (http://creativecommons.org/licenses/by/4.0/).





