1. Introduction
Malignancy [
1] and vascular disease [
2] are 2 of the largest disease groups in today’s age. They share many similar risk factors such as smoking, and obesity [
3]. Furthermore, malignancy results in general hypercoagulable state and treatment e.g. chemotherapy resulting in low flow stat may increase risks of thrombo-embolic events [
4].
Thus, it is increasingly common to encounter patients who suffer from both [
5]. Nevertheless, with advances in medicine today and the ability to tailor care, neither disease have become a clear straight- out life- sentence and a reasonable quality of life can be achieved.
Treatment for malignancy, even less advanced ones, often cannot commence in the presence of septic focus such as gangrene foot but with proper tailored therapy, meaningful limb salvage can be achieved before an upfront limb amputation.
The aim of this paper is to present 2 patients who despite suffering from advanced or near terminal GI malignancy, underwent successful limb revascularization and salvage for wet gangrene and intractable rest pain thus having better quality end of life. In addition, the authors would like to share factors that might lean a clinician to be more favorable for limb salvage as opposed to upfront major amputation in these patients.
2. Case Presentation
Case A
The first patient is a 60-year-old male, driver, smoker with poorly controlled diabetes, Chronic Kidney Disease (CKD), Ischemic Heart Disease (IHD) and newly diagnosed locally advanced borderline resectable head of pancreas malignancy with superior mesenteric vessel involvement.
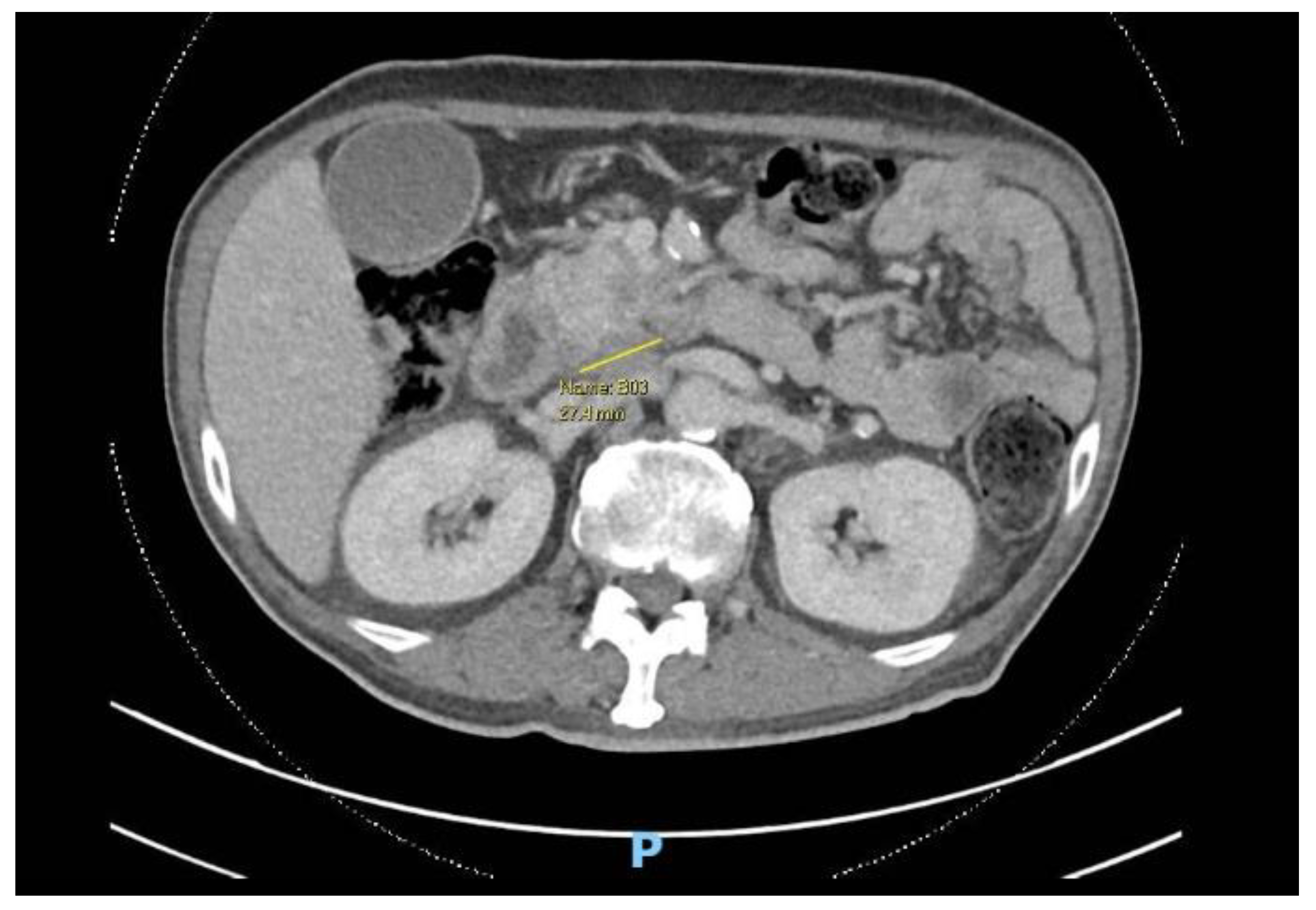
Figure 1.
Computed Tomography (CT) scan showing axial cut of pancreatic malignancy.
Figure 1.
Computed Tomography (CT) scan showing axial cut of pancreatic malignancy.
He was initiated on neoadjuvant chemotherapy with a view for definitive Whipple’s procedure but referred to the vascular unit for bilateral 5th toe gangrene that had begun as ulcers from poor fitted shoes.
Figure 2.
(A) Right foot lateral view (B) Left foot dorsum view.
Figure 2.
(A) Right foot lateral view (B) Left foot dorsum view.
Bilateral duplex us of his lower limb arterial system was performed and this placed him with a Wound, Ischemia, foot Infection (WIfI) score of Wound 3, Ischemia 2, Infection 2.
He complained of increasing rest pain in the leg with purulent discharge from the left side as well as fever, chills and rigors. His white cell count was 20 × 109/L and chemotherapy was held off with implications of delay in Whipple procedure.
After a multidisciplinary discussion, oncologist had placed the prognosis of his advanced untreated malignancy at less than 12 months with the cessation of treatment and likelihood of progression.
Options were discussed with the patient. Firstly, upfront bilateral below knee amputation which can allow the best chance of healing and wound closure so that chemotherapy can be restarted at the soonest. Secondly, limb salvage with pedal angioplasty and bilateral 5th toe amputation, understanding potential need for multiple debridement and failure to heal despite above measures given immunocompromised state, resulting in further delay to cancer treatment. Furthermore, surgery may be high risk in view of his comorbidities. Finally, an option of palliation with pain control, antibiotics and wound dressing. Patient had difficulties accepting a bilateral below knee amputation and was in low mood from diagnosis.
After much discussion, patient and vascular team decided to attempt limb salvage with bilateral lower limb angioplasties and fifth toe ray amputations at the same setting. Angioplasty to anterior tibial artery, posterior tibial artery, dorsalis pedis, common plantar artery was performed on the right lower limb with successful outcome. On the left lower limb, angioplasty to the anterior and posterior tibial artery was performed. Patient’s wound recovered with combination of culture directed antibiotics, vacuum dressing and motivation from a supportive family.
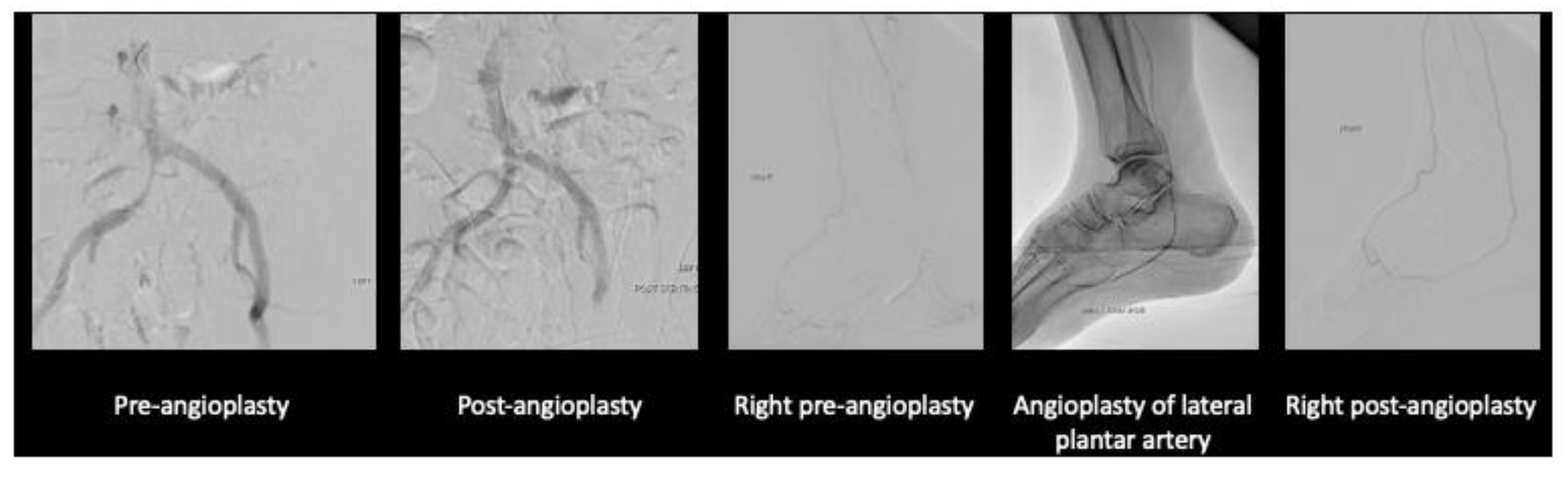
Figure 3.
Angioplasty images of the left lower limb.
Figure 3.
Angioplasty images of the left lower limb.
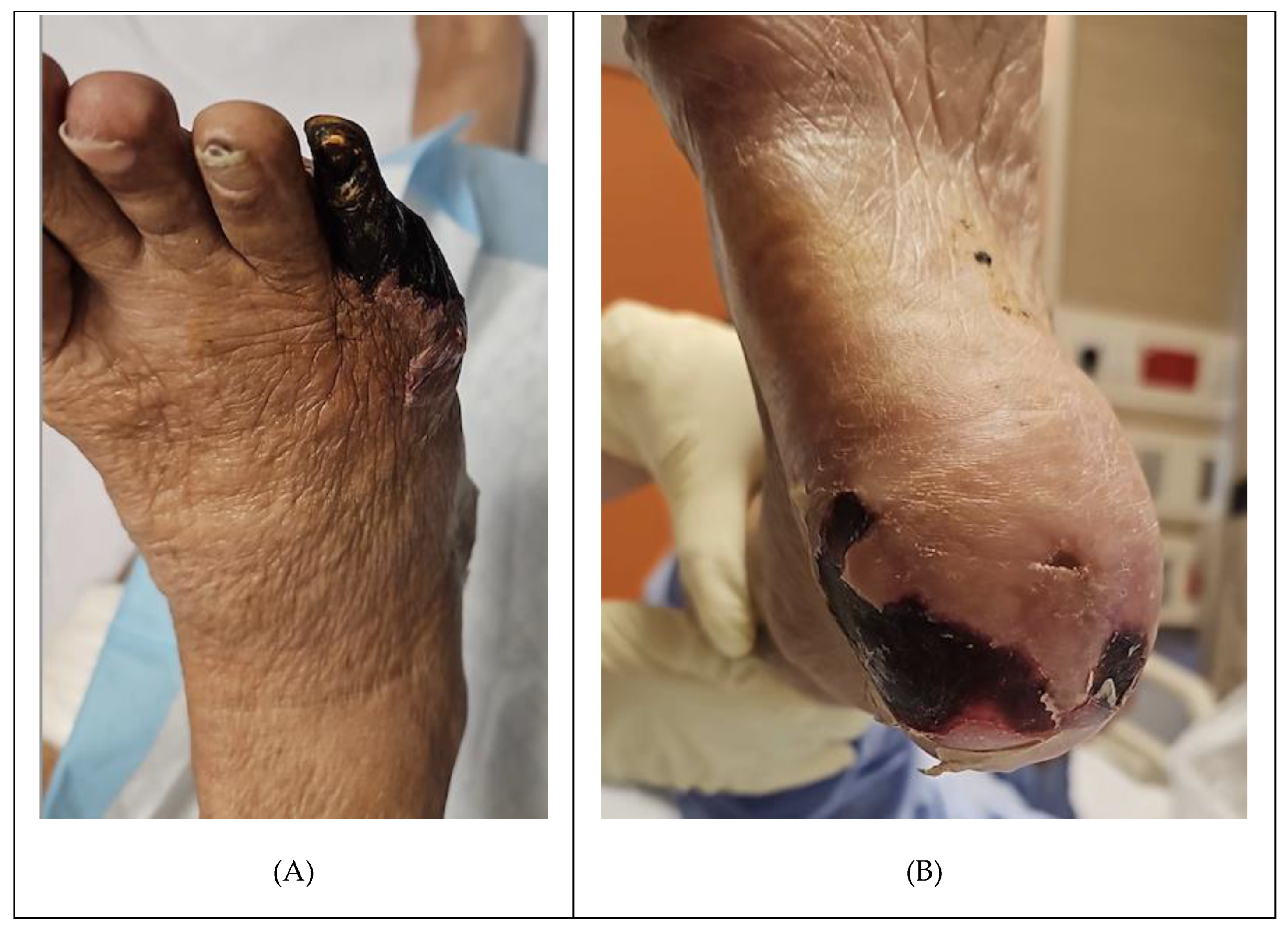
Figure 4.
Angioplasty images of the right lower limb.
Figure 4.
Angioplasty images of the right lower limb.
Figure 5.
(A) Right foot wound (B) Left foot wound.
Figure 5.
(A) Right foot wound (B) Left foot wound.
When the wounds showed that they had begun to granulate well and antibiotics were stopped with normalized inflammatory marker, the oncologists resumed his chemotherapy, and he eventually underwent the Whipple procedure 3 months after the bilateral lower limb revascularisation. Patient remains well at last review a year from diagnosis.
Case B
The second patient is a 73-year-old male smoker of 40 pack years, IHD with newly diagnosed gastric cancer with liver oligometastases and peritoneal thickening with ascites seen on imaging. He presented with transient gastric outlet obstruction which resolved with laparoscopic palliative gastrojejunal bypass and was planned for palliative chemotherapy.
He had incidental right common iliac artery occlusion seen on staging scans for which he has complained of buttock and thigh claudication with occasional rest pain for more than 6 months. He now presents with right 5th toe and heel dry gangrene associated with increased rest pain and inability to sleep at night despite multiple analgesia and opioids. His white cell count was 13 x 109/L C-Reactive protein 38.8mg/L.
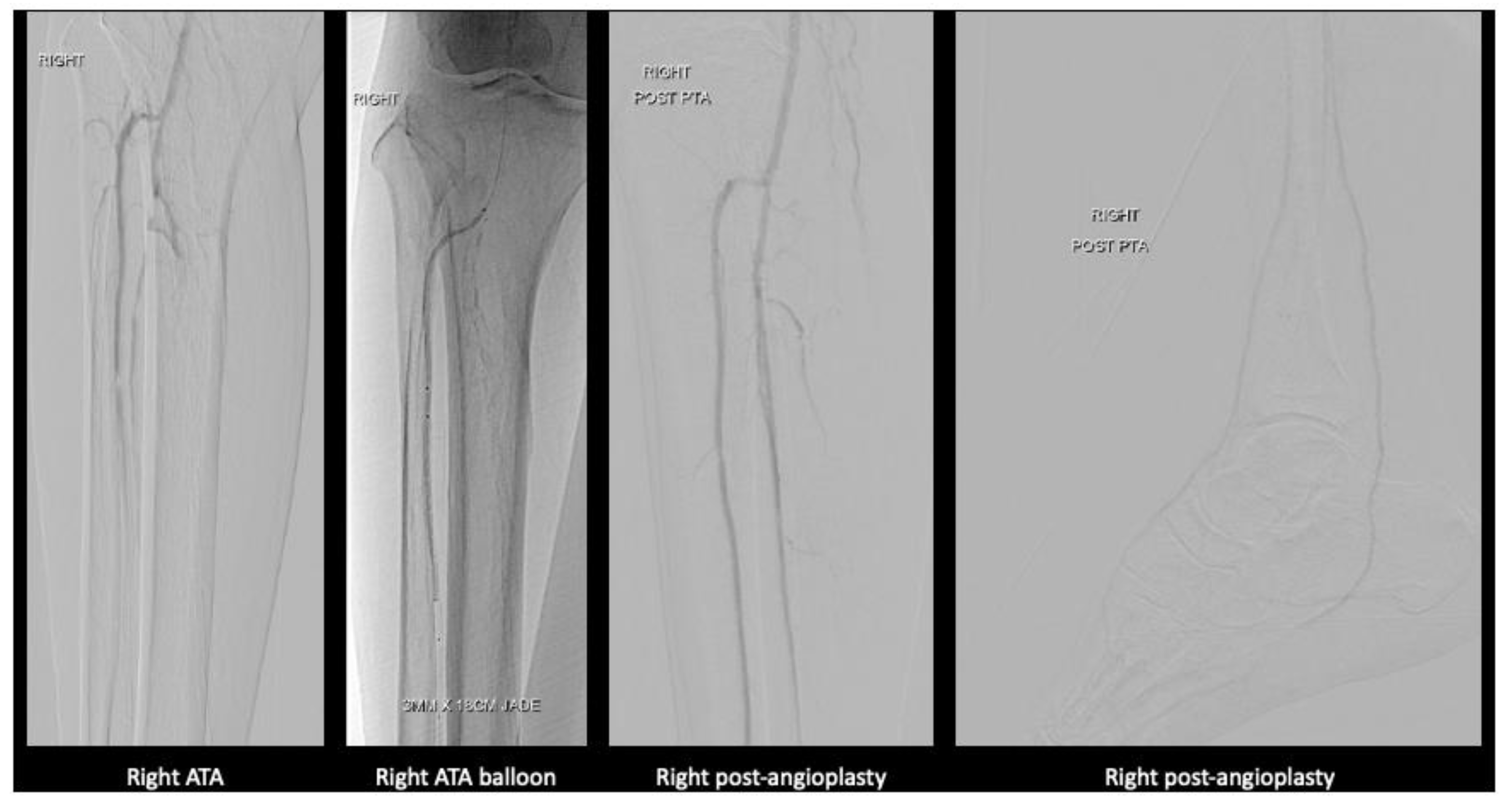
Figure 6.
(A) Right foot dorsum view (B) Right foot plantar view.
Figure 6.
(A) Right foot dorsum view (B) Right foot plantar view.
Discussion was held with family. While they noted that his life expectancy due to his malignancy was limited, their utmost concern was him having to deal with both cancer and leg pain along with the dry gangrene. His pain could not be fully palliated with the rest pain and wound in his leg. At the same time an upfront above knee amputation wound may not heal given the level of arterial disease. After thorough discussion, patient and family opted for angioplasty with stenting of his right iliac artery and angioplasty of his posterior tibial artery.
Figure 7.
(A) Right iliac artery and lower limb angioplasty.
Figure 7.
(A) Right iliac artery and lower limb angioplasty.
Fortunately, the angioplasty was successful, and his 5th toe gangrene was amputated with good granulation seen.
He agreed to quit smoking and was kept on low dose aspirin without any bleeding complications form the gastric malignancy. Unfortunately, a year later he passed on from progression of his cancer however patient was relieved of his lower limb rest pain and even ability to walk without claudication after the angioplasty.
3. Discussion
In peripheral arterial disease, there is a range of presentation, from asymptomatic, claudication, acute limb ischemia and chronic limb threatening ischemia (CLTI). While there is evidence to show that revascularization for acute limb ischemia in patients with cancer have acceptable short- and medium-term outcomes [
6,
7], there is a lack of consensus for treatment of CLTI.
CLTI has poor long-term prognosis [
8] with mortality of 17.5% at 1 year and for those with malignancy, the prognosis is likely worse. In a cohort study by El Sakka et al. [
9], CLTI patients with malignancy have higher 6-month mortality rate of 50% compared to 20.6% in patients without malignancy. From the resource allocation point of view, patients with advanced malignancy and CLTI may be offered upfront major limb amputation in the form of below or above knee amputation over revascularization and limb salvage due to limited lifespan. Some may also argue that it is more humane to take a palliative route and allow patients to demise from sepsis as opposed to subjecting patient to invasive procedures, chronic wound pain and potential future complications of underlying cancer and treatment costs. However, with advancement in medical science, vascular surgeons have an armamentarium for treatment of CLTI, with improvement of limb salvage [
10] thus preserving function in this group of patients. Furthermore, there is an increasing shift in mentality towards viewing malignancy as a chronic disease rather than a death sentence. Survival with cancer has also improved over the years [
11]. The goal is for patients to be able to at least maintain an acceptable quality of life even with diagnosis of CLTI and this could be achieved with limb salvage as opposed to non-surgical treatment or primary amputation which is more morbid and may be psychologically debilitating. The question of how then do we better select for patients who will benefit from revascularisation arises.
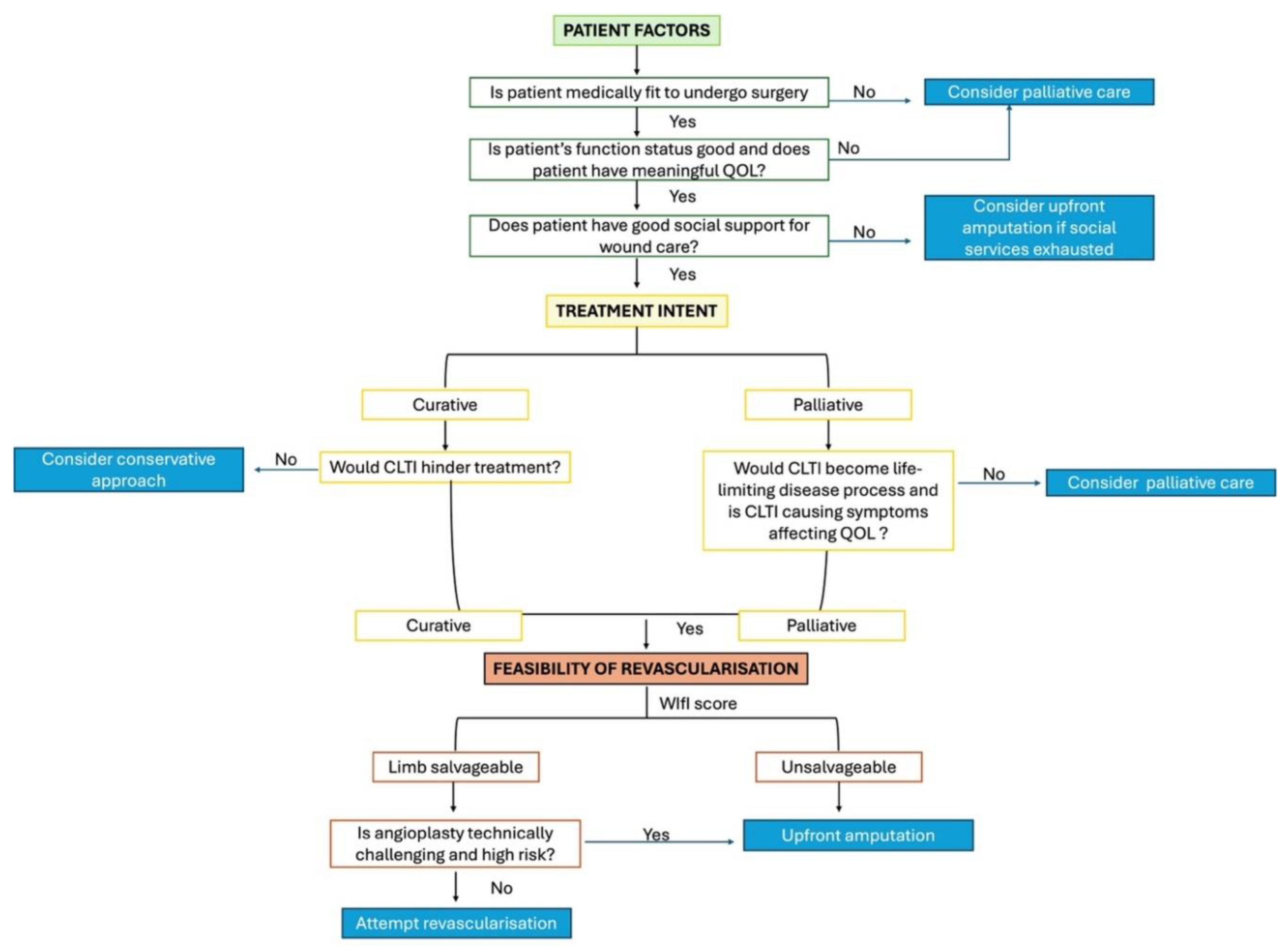
In these two cases, we demonstrated that there is still a role for lower limb revascularisation and limb salvage. We propose a holistic view and identify key factors to consider and how to tailor treatment to the individual.
Firstly, the treatment intent of malignancy has to be clear, be it curative or palliative. If treatment is curative in intent, would CLTI hinder the treatment? For cases where treatment is palliative in intent, we have to consider patient’s quality of life, pre-existing functional status and social support. Often, CLTI can affect quality of life more than malignancy itself.
Secondly, we have to consider the feasibility of the revascularisation. We can use the WIfI score to determine if limb salvage is reasonable or whether we should offer upfront amputation. If deemed salvageable, we have to consider if the angioplasty wound be technically challenging and patient’s fitness for surgery.
Figure 8.
Flowsheet depicting factors to consider .
Figure 8.
Flowsheet depicting factors to consider .
In Case A, CLTI has hindered patient’s cancer treatment. While amputation upfront may be the “best” solution to solve CLTI and allow patient to continue chemotherapy, patient was in low mood as a result of diagnosis and this could affect patient’s motivation to continue his journey. However, while we would like to motivate and offer the patient a glimpse of hope with revascularisation, we still had to inform patient that limb salvage may not be successful and amputation may still be required. Delay to treatment during wound healing may also result in tumour progression and unresectability.
In Case B, life expectancy of patient is limited. We have to consider quality of life in his remaining days. To alleviate rest pain and regain mobility was important to patient. Furthermore, if revascularisation is difficult and complications are expected then we should not proceed as the risks may outweigh the benefits. In this case, patient had meaning quality of life in his remaining days as compared to if he had major amputation.
4. Conclusions
Choosing revascularization and limb salvage over major amputation in patients with advanced malignancy can provide a better quality of life despite reduced life expectancy in a selected group of patients with good patient motivation, adequate social support, effective communication regarding risks and benefits and supportive multi-disciplinary team including oncology, anesthesia, palliative care and allied health teams. We hope that for those who suffer from both diseases, clinicians do not write them off and instead, have an open conversation and strive to achieve a good quality of life for them.
References
- ReFaey, K.; Tripathi, S.; Grewal, S.S.; Bhargav, A.G.; Quinones, D.J.; Chaichana, K.L.; Antwi, S.O.; Cooper, L.T.; Meyer, F.B.; Dronca, R.S.; et al. Cancer Mortality Rates Increasing vs Cardiovascular Disease Mortality Decreasing in the World: Future Implications. Mayo Clinic proceedings. Innovations, quality & outcomes 2021, 5, 645–653. [Google Scholar] [CrossRef]
- Kim, M.S.; Hwang, J.; Yon, D.K.; Lee, S.W.; Jung, S.Y.; Park, S.; Johnson, C.O.; A Stark, B.; Razo, C.; Abbasian, M.; et al. Global burden of peripheral artery disease and its risk factors, 1990–2019: a systematic analysis for the Global Burden of Disease Study 2019. Lancet Glob. Heal. 2023, 11, e1553–e1565. [Google Scholar] [CrossRef] [PubMed]
- van Kruijsdijk, R.C.; van der Graaf, Y.; Peeters, P.H.; Visseren, F.L. ; on behalf of the Second Manifestations of ARTerial disease (SMART) study group Cancer Risk in Patients with Manifest Vascular Disease: Effects of Smoking, Obesity, and Metabolic Syndrome. Cancer Epidemiology Biomarkers Prev. 2013, 22, 1267–1277. [Google Scholar] [CrossRef] [PubMed]
- Sanon, S.; Lenihan, D.J.; Mouhayar, E. Peripheral arterial ischemic events in cancer patients. Vasc. Med. 2010, 16, 119–130. [Google Scholar] [CrossRef] [PubMed]
- Kaschwich, M.; Peters, F.; Hischke, S.; Rieß, H.C.; Gansel, M.; Marschall, U.; L’hoest, H.; Heidemann, F.; Debus, E.S.; Acar, L.; et al. Long-term incidence of cancer after index treatment for symptomatic peripheral arterial disease – a health insurance claims data analysis. Vasa 2020, 49, 493–499. [Google Scholar] [CrossRef]
- Kelly, A.; Toale, C.; Moloney, M.A.; Kavanagh, E.G. Outcomes of Acute Limb Ischaemia in Patients with Underlying Malignancy: A Systematic Review. EJVES Vasc. Forum 2021, 54, 13–20. [Google Scholar] [CrossRef] [PubMed]
- Nicolajsen, C.W.; Dickenson, M.H.; Budtz-Lilly, J.; Eldrup, N. Frequency of cancer in patients operated on for acute peripheral arterial thrombosis and the impact on prognosis. J. Vasc. Surg. 2015, 62, 1598–1606. [Google Scholar] [CrossRef] [PubMed]
- E Rollins, K.; Jackson, D.; A Coughlin, P. Meta-analysis of contemporary short- and long-term mortality rates in patients diagnosed with critical leg ischaemia. Br. J. Surg. 2013, 100, 1002–1008. [Google Scholar] [CrossRef] [PubMed]
- El Sakka, K.; Gambhir, R.P.S.; Halawa, M.; Chong, P.; Rashid, H. Association of malignant disease with critical leg ischaemia. Br. J. Surg. 2005, 92, 1498–1501. [Google Scholar] [CrossRef] [PubMed]
- Teraa, M.; Conte, M.S.; Moll, F.L.; Verhaar, M.C. Critical Limb Ischemia: Current Trends and Future Directions. J. Am. Hear. Assoc. 2016, 5, e002938. [Google Scholar] [CrossRef] [PubMed]
- Henley, S.J.; Ward, E.M.; Scott, S.; Ma, J.; Anderson, R.N.; Firth, A.U.; Thomas, C.C.; Islami, F.; Weir, H.K.; Lewis, D.R.; et al. Annual Report to the Nation on the Status of Cancer, Part I: National Cancer Statistics. Cancer 2020, 126, 2225–2249. [Google Scholar] [CrossRef] [PubMed]
|
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2025 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (http://creativecommons.org/licenses/by/4.0/).