Submitted:
20 January 2025
Posted:
21 January 2025
You are already at the latest version
Abstract
Keywords:
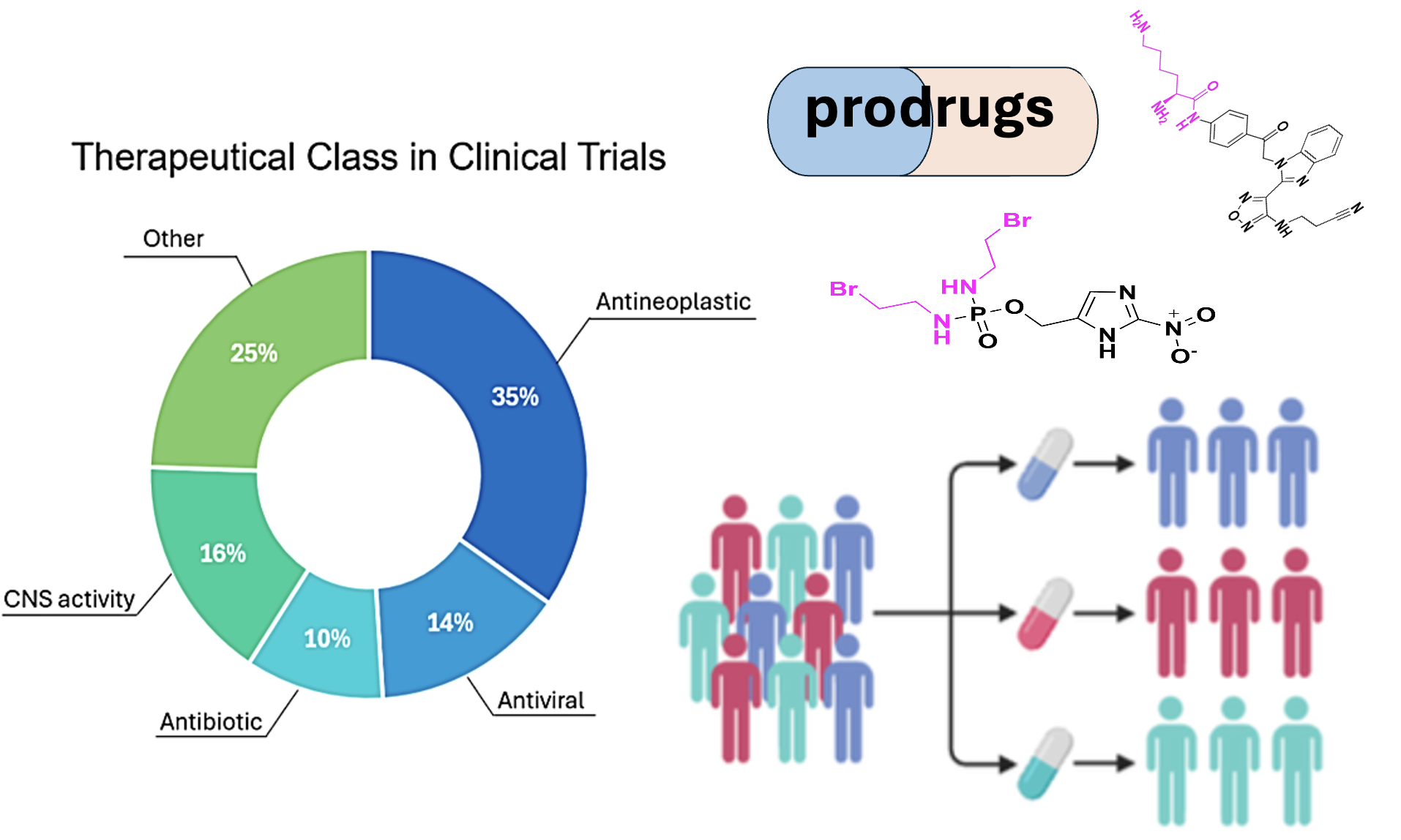
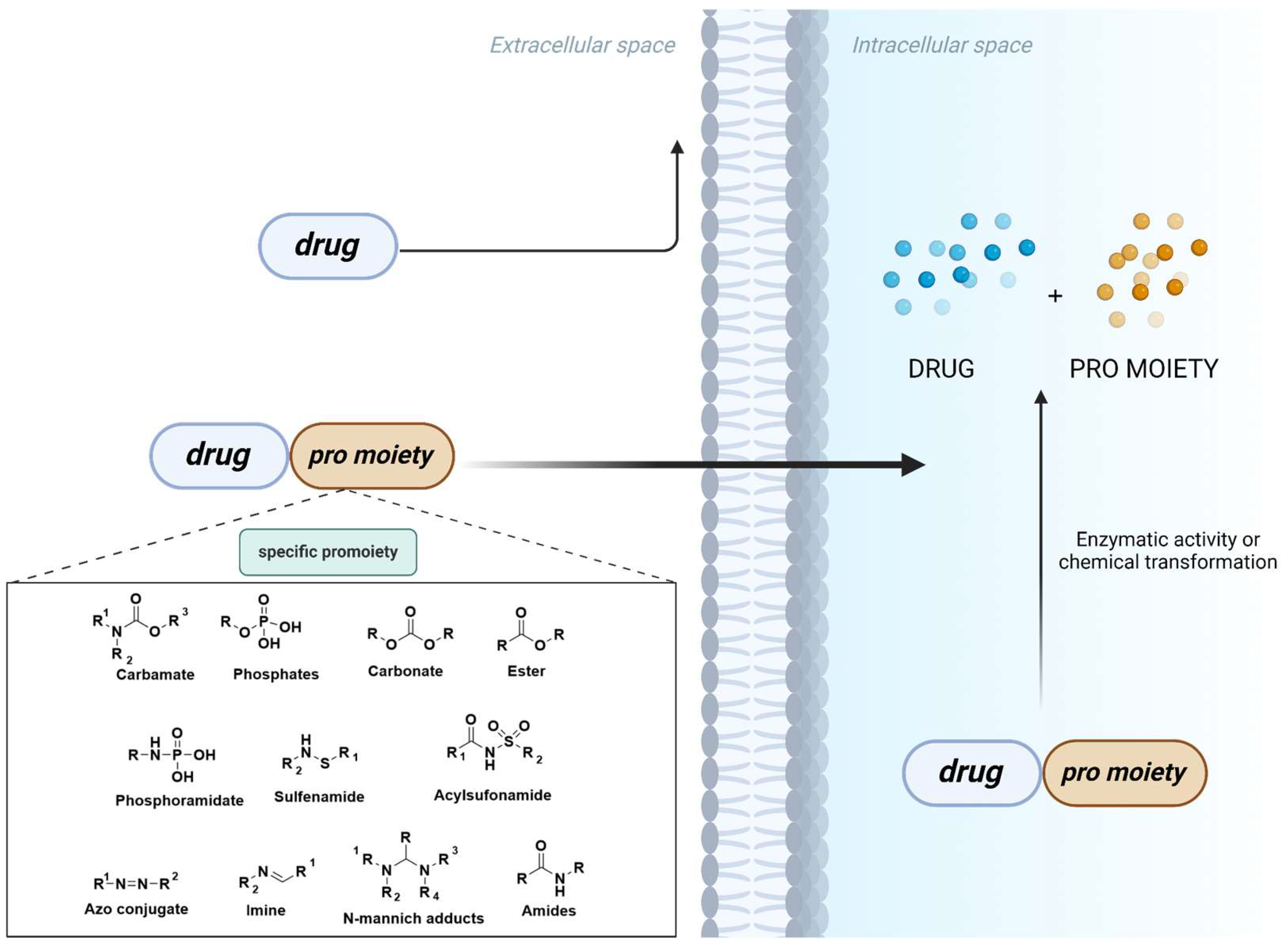
1. Introduction
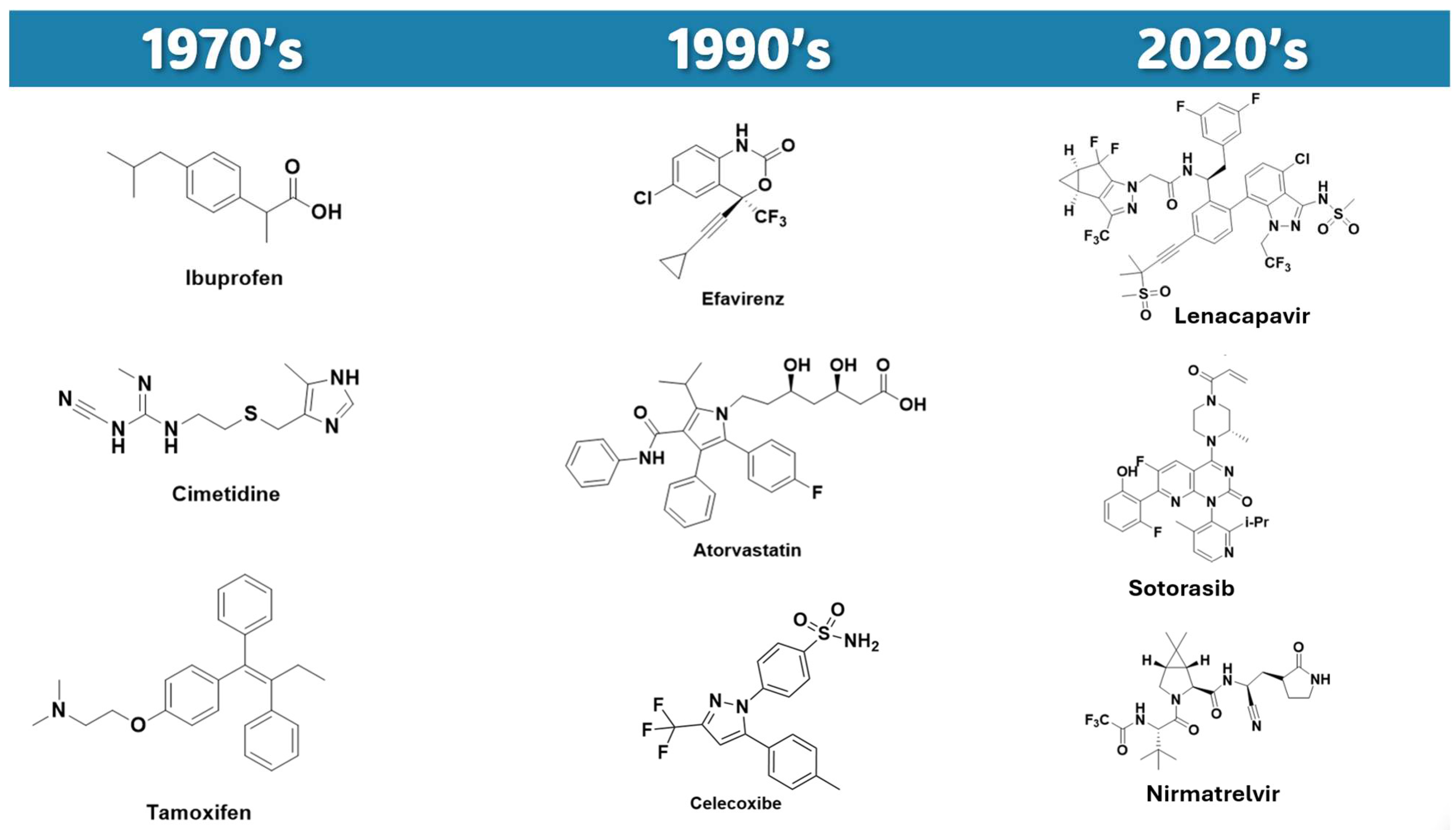
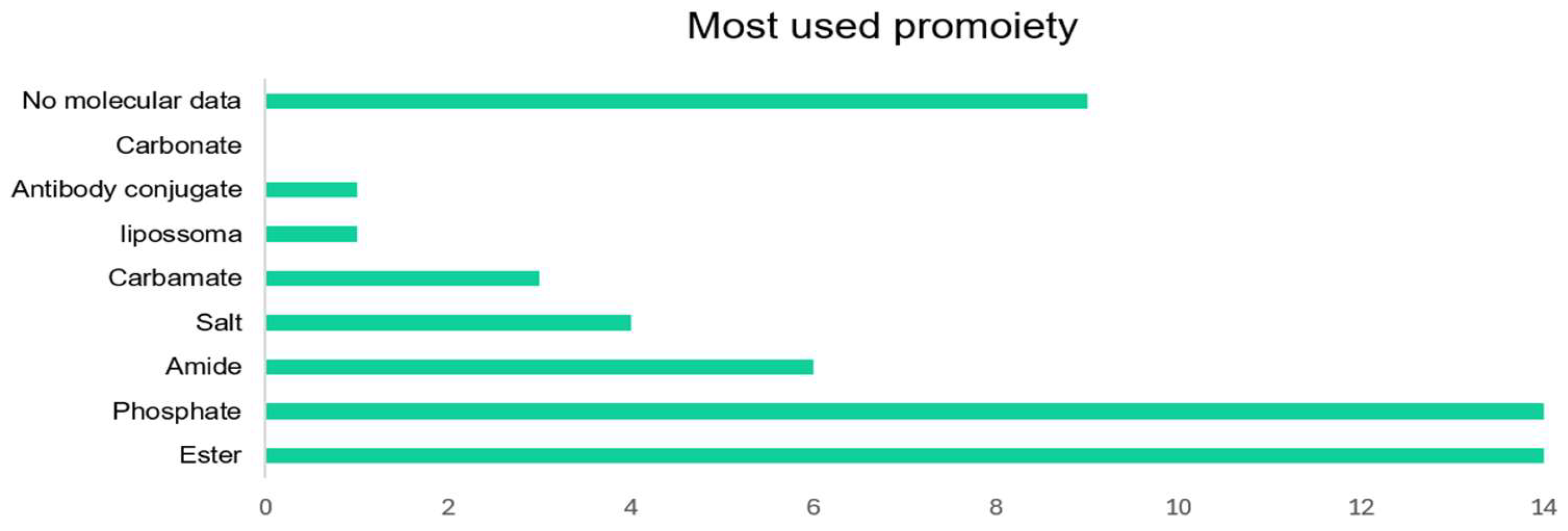
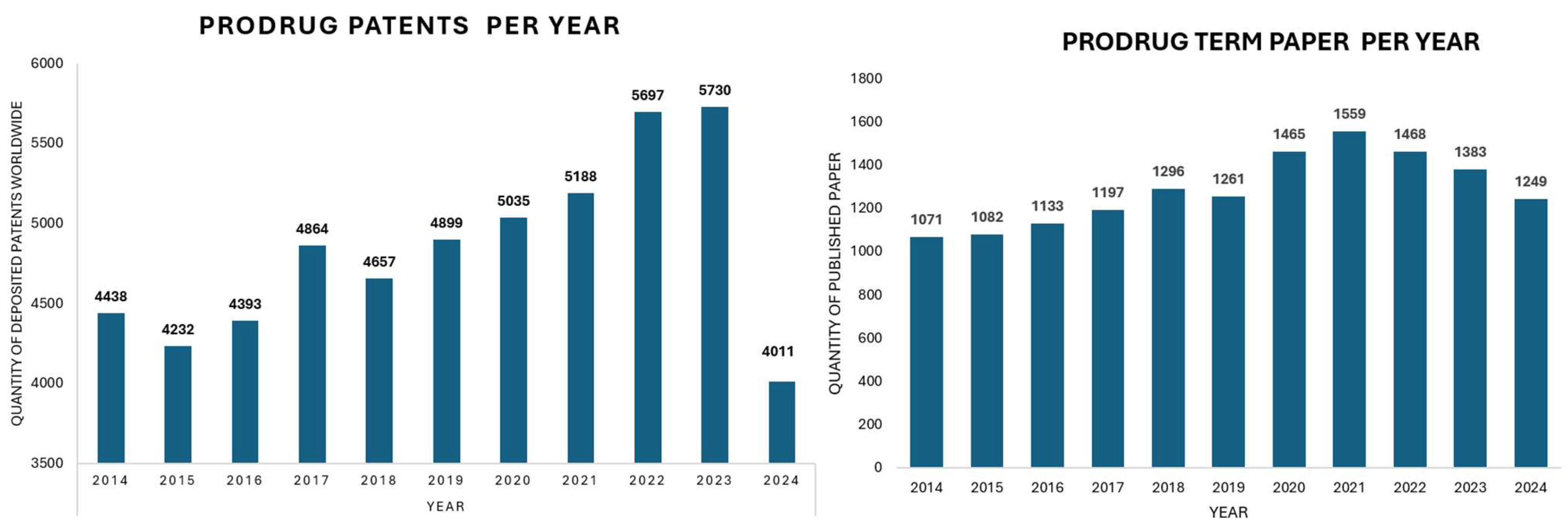
2. Evolving landscape of prodrug design
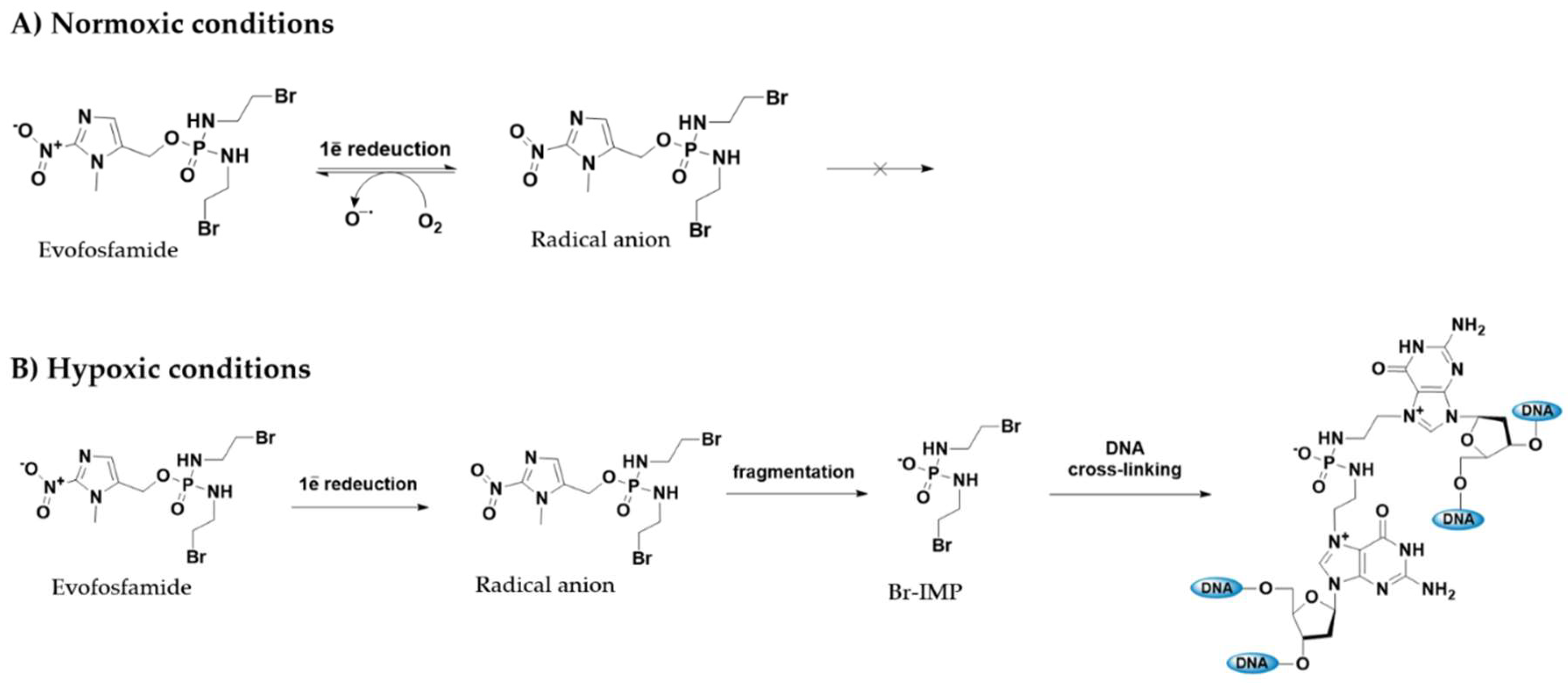
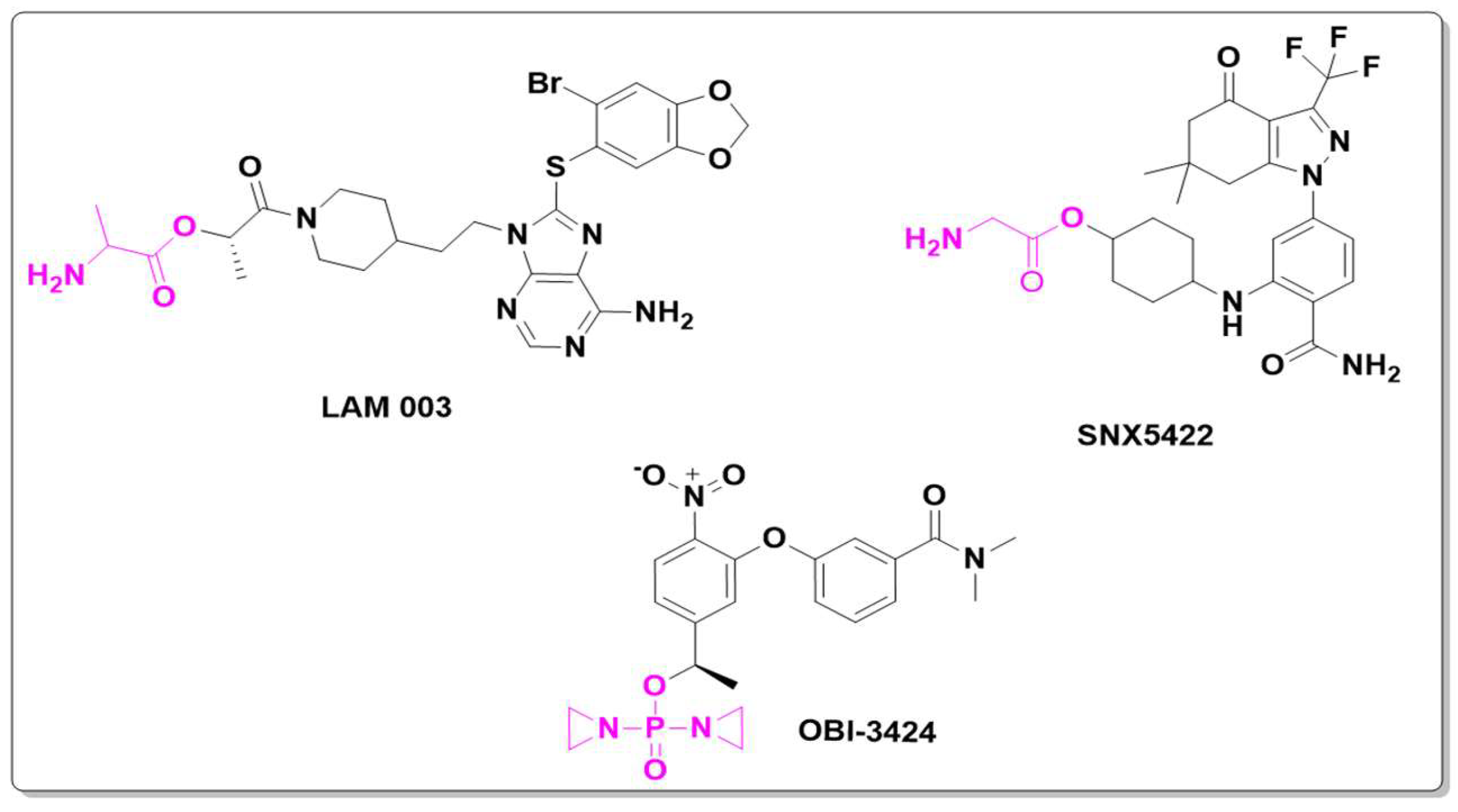
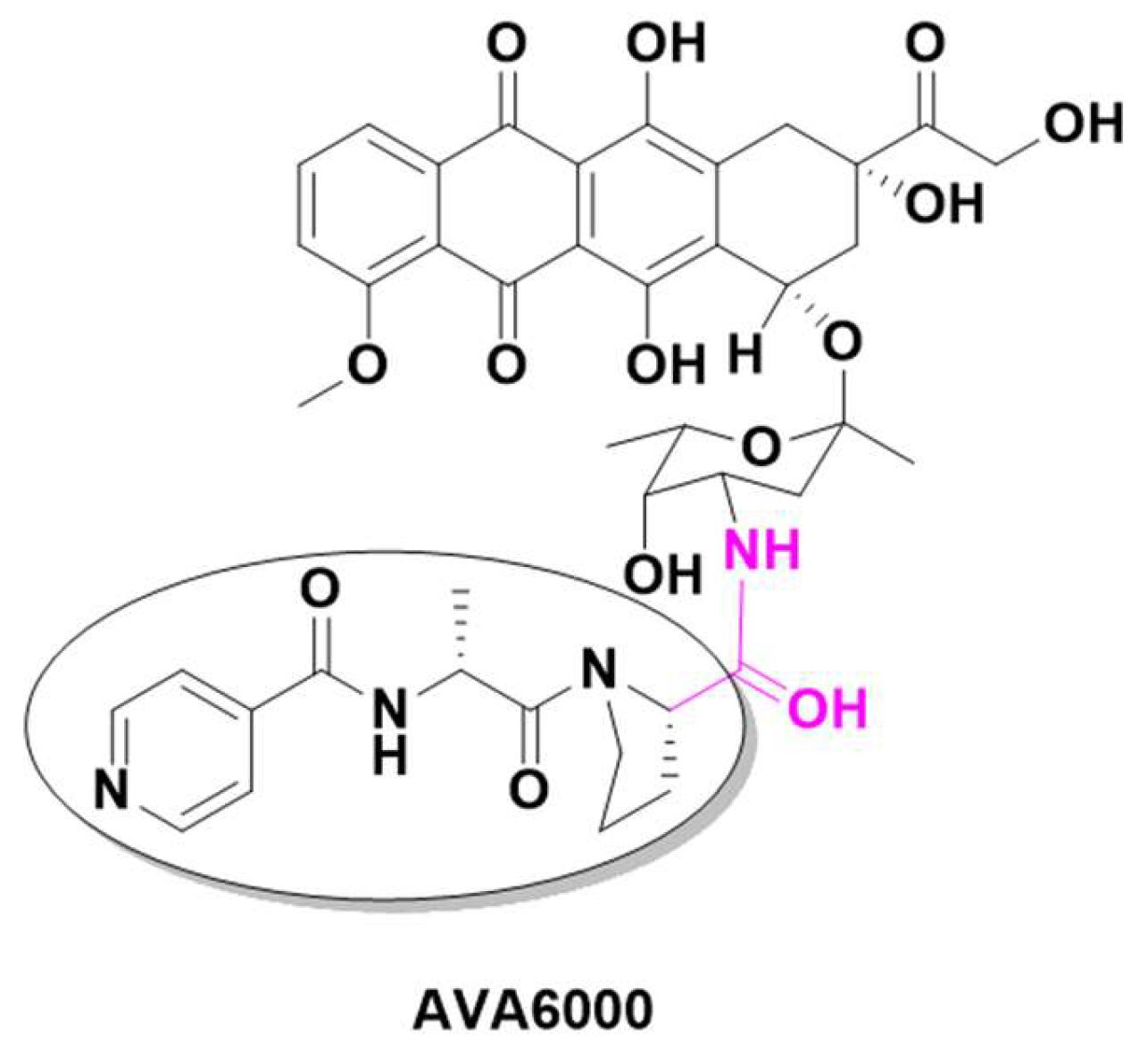
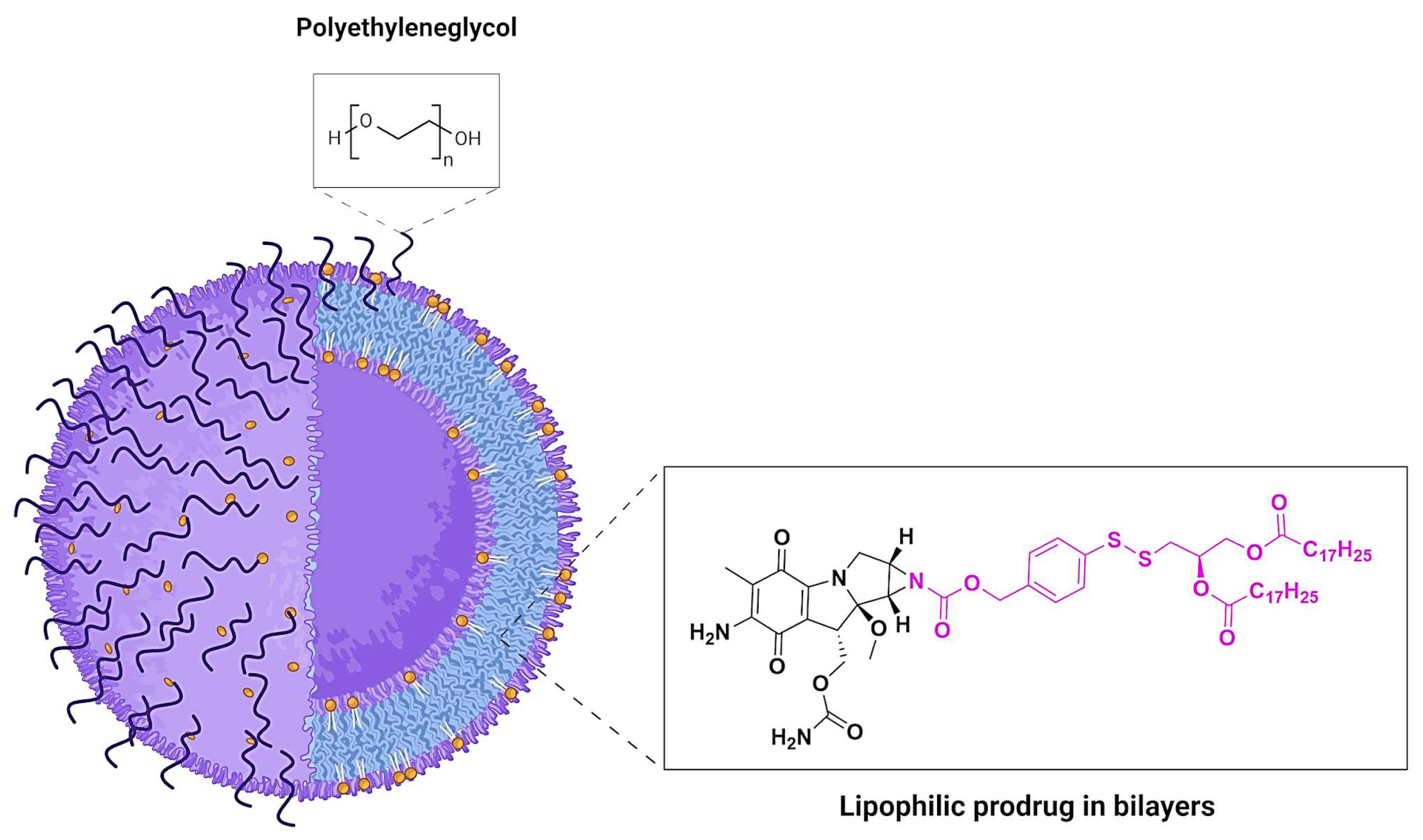
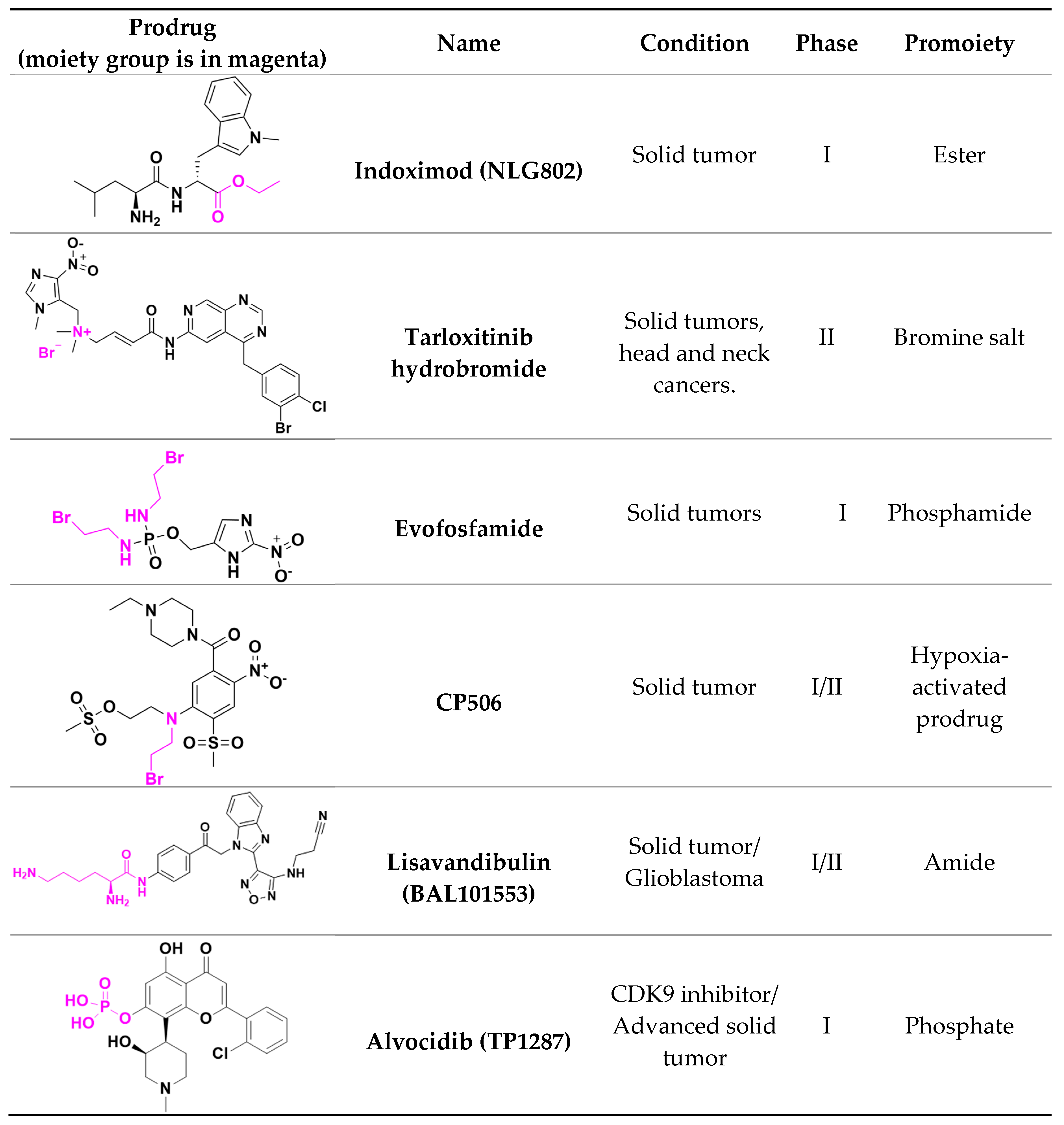
2.1. Antineoplastic Prodrugs

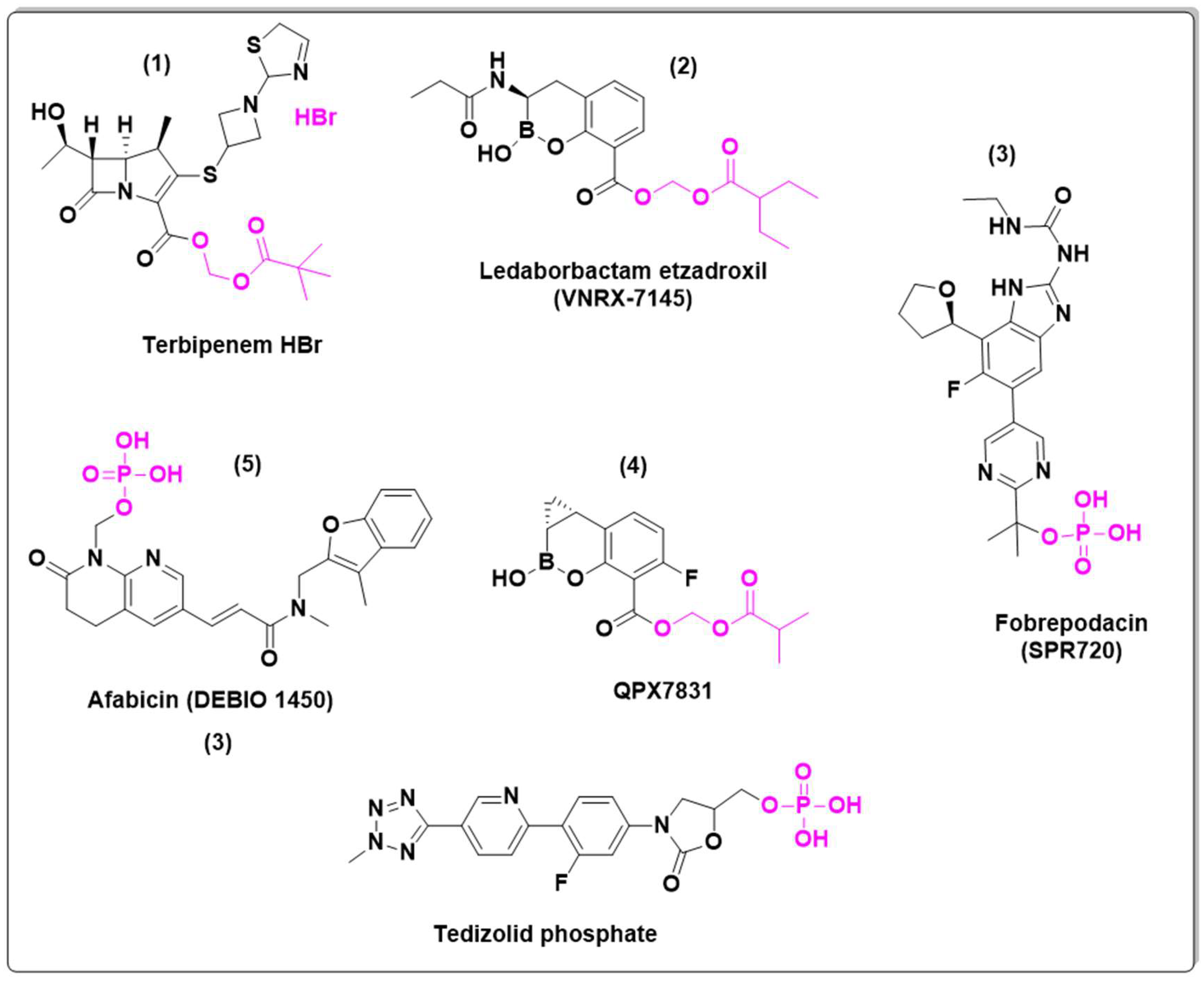
2.2. Antibiotic Prodrugs
2.3. Antiviral Prodrugs
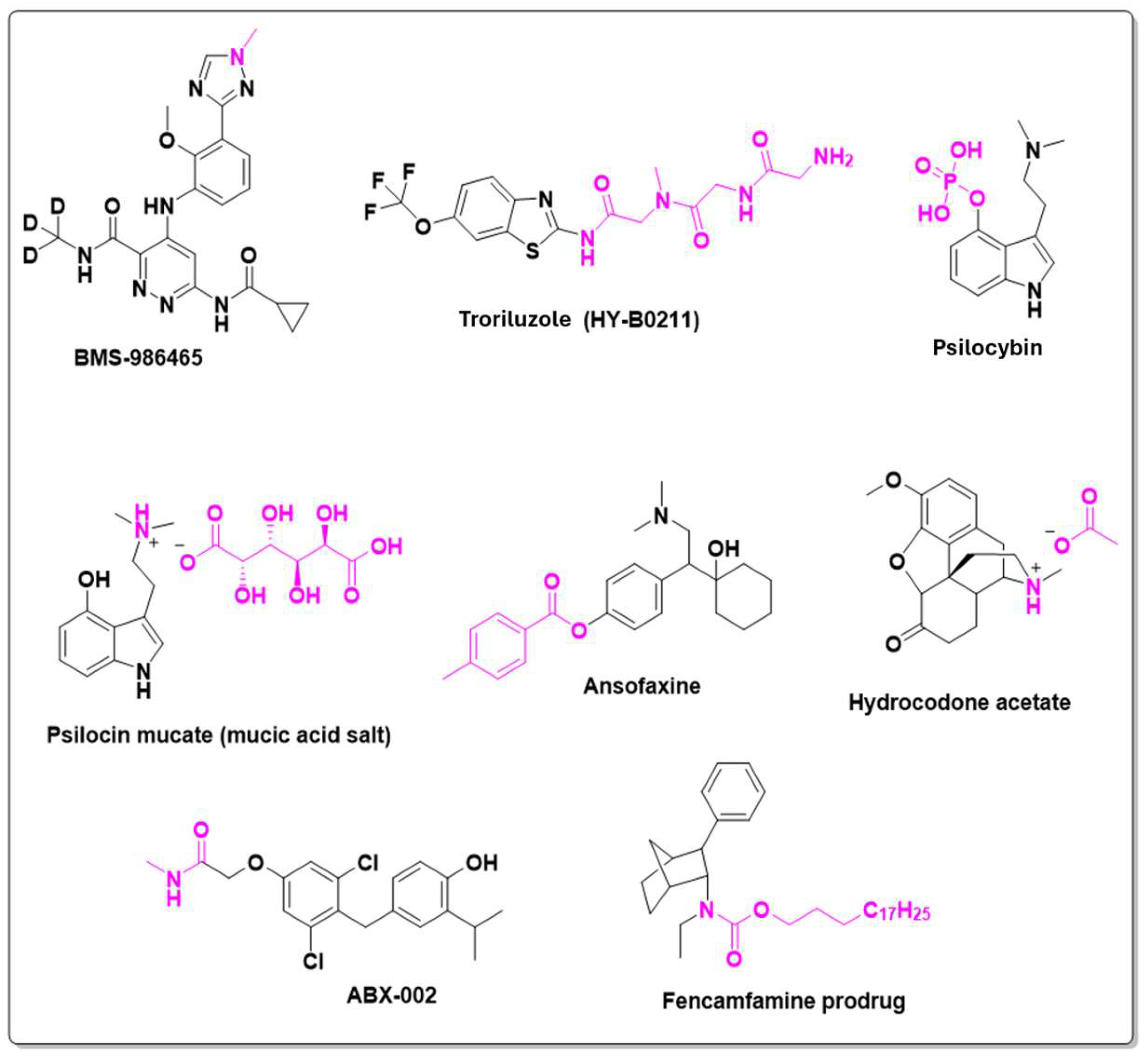
2.4. Central Nervous System Active Prodrugs
2.5. Other prodrugs
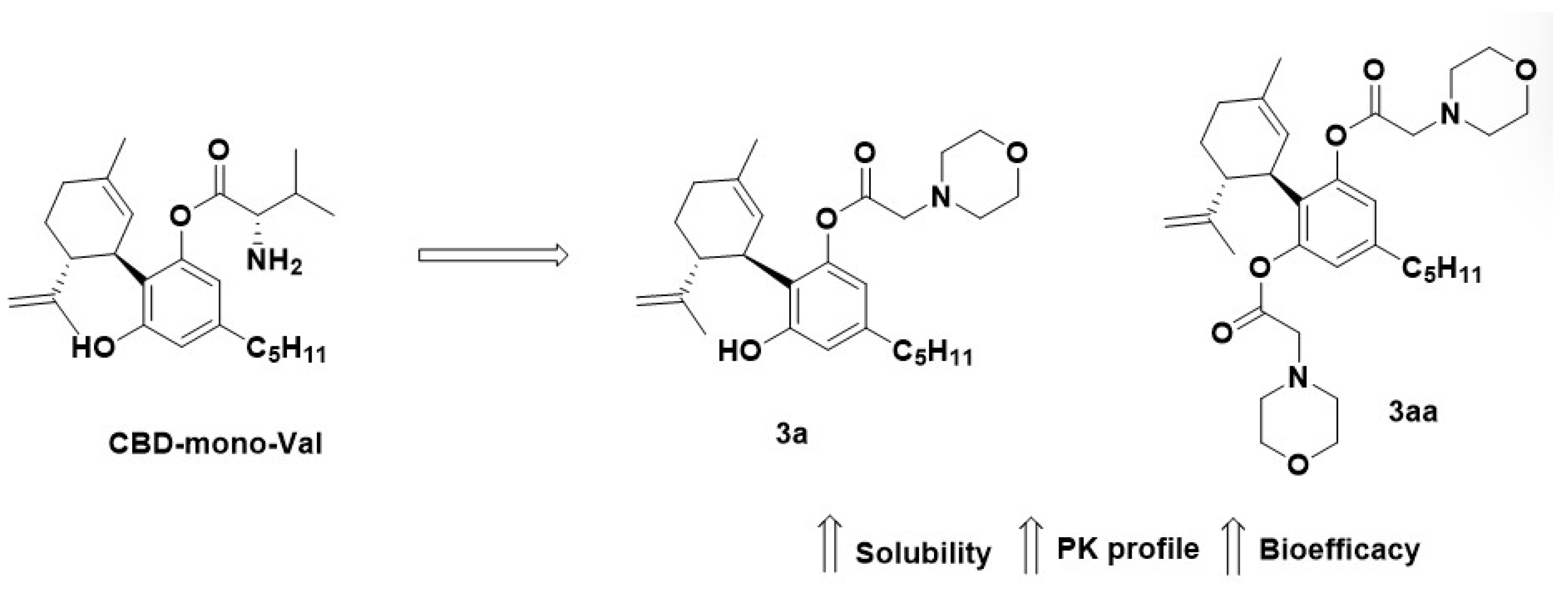
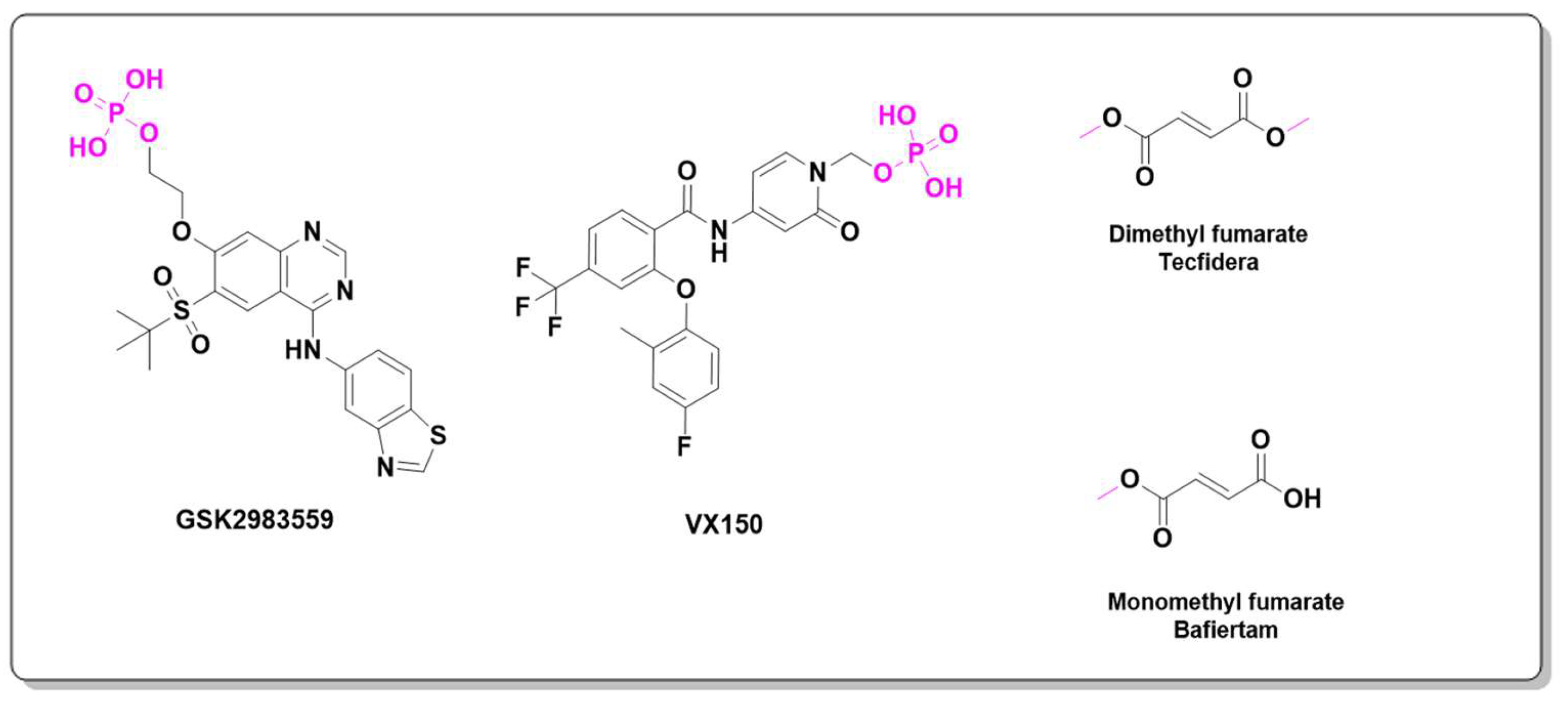
2.5.1. Anti-inflammatory
2.5.2. Immunomodulator
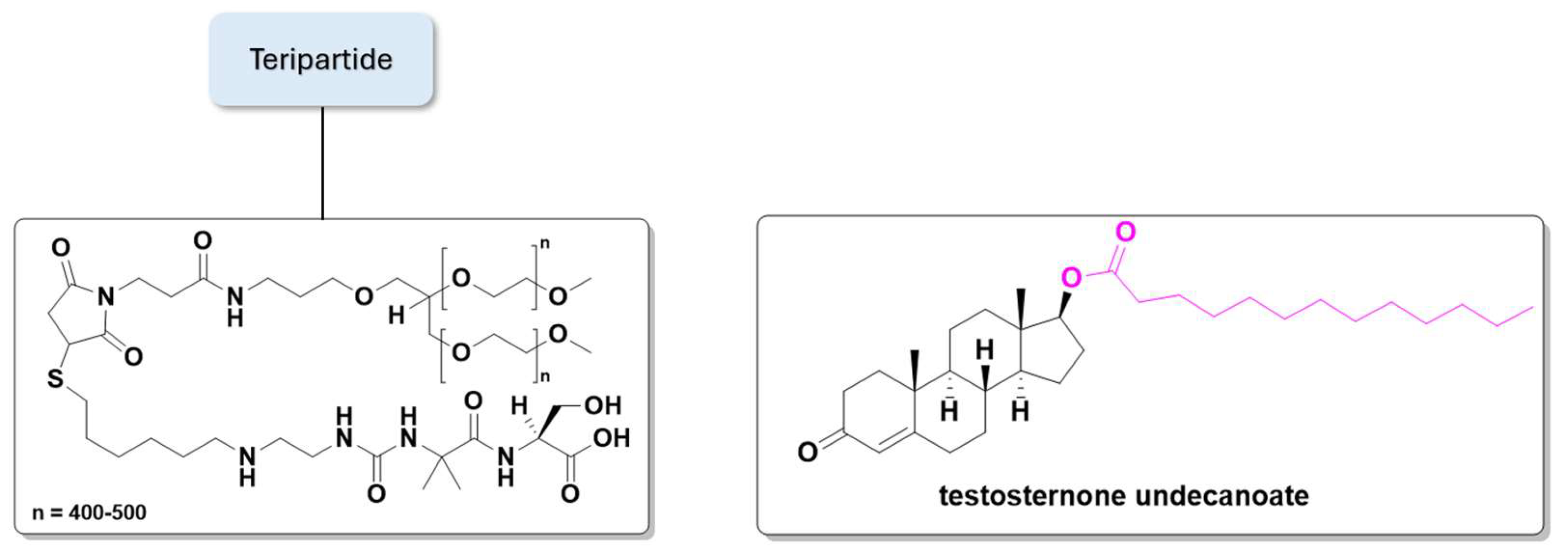
2.5.3. Hormones
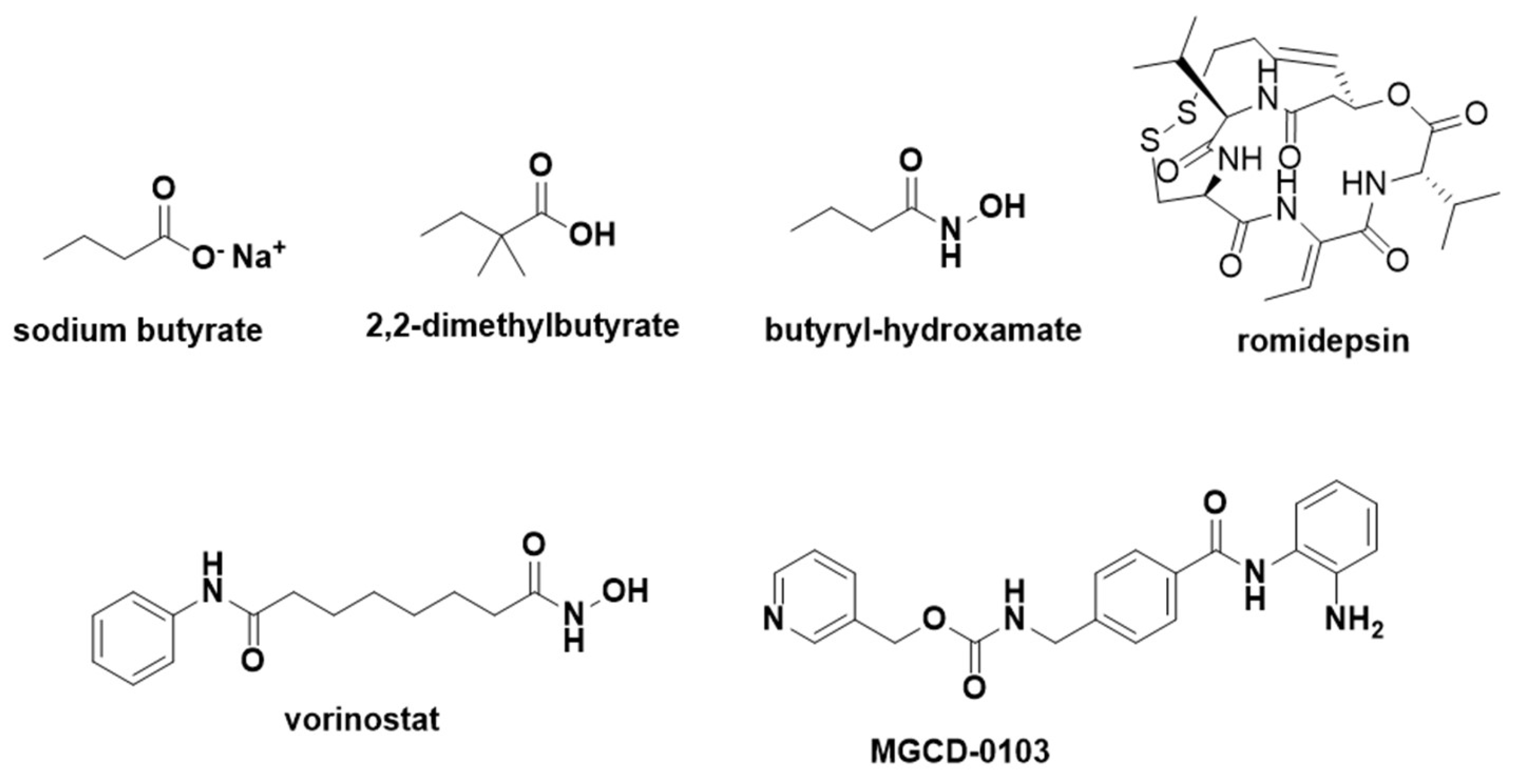
2.5.4. Sickle Cell Disease
2.5.5. Antifungal
2.5.6. Diabetic Macular Edema
2.5.7. Hypertension
2.5.8. Toxicity Reduction
3. Conclusion and Future Directions
Author Contributions
Funding
Institutional Review Board Statement
Data Availability Statement
Acknowledgments
Conflicts of Interest
References
- Baró, E.L.; Catti, F.; Estarellas, C.; Ghashghaei, O.; Lavilla, R. Drugs from Drugs: New Chemical Insights into a Mature Concept. Drug Discovery Today 2024, 29, 104212. [CrossRef]
- Jornada, D.H.; dos Santos Fernandes, G.F.; Chiba, D.E.; de Melo, T.R.F.; dos Santos, J.L.; Chung, M.C. The Prodrug Approach: A Successful Tool for Improving Drug Solubility. Molecules 2015, 21, 42. [CrossRef]
- Fernandes, L.D.R.; Lopes, J.R.; Bonjorno, A.F.; Prates, J.L.B.; Scarim, C.B.; Dos Santos, J.L. The Application of Prodrugs as a Tool to Enhance the Properties of Nucleoside Reverse Transcriptase Inhibitors. Viruses 2023, 15, 2234. [CrossRef]
- Ghosh, A.K.; Brindisi, M. Organic Carbamates in Drug Design and Medicinal Chemistry. J. Med. Chem. 2015, 58, 2895–2940. [CrossRef]
- Husain, A.; Monga, J.; Narwal, S.; Singh, G.; Rashid, M.; Afzal, O.; Alatawi, A.; Almadani, N.M. Prodrug Rewards in Medicinal Chemistry: An Advance and Challenges Approach for Drug Designing. Chem Biodivers 2023, 20, e202301169. [CrossRef]
- He, Z.; Yang, W.; Yang, F.; Zhang, J.; Ma, L. Innovative Medicinal Chemistry Strategies for Enhancing Drug Solubility. European Journal of Medicinal Chemistry 2024, 279, 116842. [CrossRef]
- Rautio, J.; Kumpulainen, H.; Heimbach, T.; Oliyai, R.; Oh, D.; Järvinen, T.; Savolainen, J. Prodrugs: Design and Clinical Applications. Nat Rev Drug Discov 2008, 7, 255–270. [CrossRef]
- Cheng, A.V.; Wuest, W.M. Signed, Sealed, Delivered: Conjugate and Prodrug Strategies as Targeted Delivery Vectors for Antibiotics. ACS Infect. Dis. 2019, 5, 816–828. [CrossRef]
- Dean, T.T.; Jelú-Reyes, J.; Allen, A.C.; Moore, T.W. Peptide–Drug Conjugates: An Emerging Direction for the Next Generation of Peptide Therapeutics. J. Med. Chem. 2024, 67, 1641–1661. [CrossRef]
- Deng, S.; Wen, X.; Wang, J. Recent Advances in the Linkers of Drug Conjugates. CMC 2024, 31. [CrossRef]
- Hobson, A.D. The Medicinal Chemistry Evolution of Antibody–Drug Conjugates. RSC Med. Chem. 2024, 15, 809–831. [CrossRef]
- Klein, C.; Brinkmann, U.; Reichert, J.M.; Kontermann, R.E. The Present and Future of Bispecific Antibodies for Cancer Therapy. Nat Rev Drug Discov 2024, 23, 301–319. [CrossRef]
- Millar, S.A.; Stone, N.L.; Yates, A.S.; O’Sullivan, S.E. A Systematic Review on the Pharmacokinetics of Cannabidiol in Humans. Front. Pharmacol. 2018, 9, 1365. [CrossRef]
- Millar, S.A.; Maguire, R.F.; Yates, A.S.; O’Sullivan, S.E. Towards Better Delivery of Cannabidiol (CBD). Pharmaceuticals 2020, 13, 219. [CrossRef]
- Singh Cham, P.; Kotwal, P.; Sharma, K.; Dhiman, S.; Singh, L.; Pratap Singh, V.; Kumar, A.; Nandi, U.; Pal Singh, P. Cannabidiol-Based Prodrugs: Synthesis and Bioevaluation. ACS Med. Chem. Lett. 2024, 15, 221–229. [CrossRef]
- Banerjee, A.; Hayward, J.J.; Trant, J.F. “Breaking Bud”: The Effect of Direct Chemical Modifications of Phytocannabinoids on Their Bioavailability, Physiological Effects, and Therapeutic Potential. Org. Biomol. Chem. 2023, 21, 3715–3732. [CrossRef]
- Cao, T.; Zhang, W.; Wang, Q.; Wang, C.; Ma, W.; Zhang, C.; Ge, M.; Tian, M.; Yu, J.; Jiao, A.; et al. Cancer SLC6A6-Mediated Taurine Uptake Transactivates Immune Checkpoint Genes and Induces Exhaustion in CD8+ T Cells. Cell 2024, 187, 2288-2304.e27. [CrossRef]
- Causes and Prevalence of Visual Impairment Among Adults in the UnitedStates. Arch Ophthalmol 2004, 122, 477. [CrossRef]
- Pieken, W.A.; Olsen, D.B.; Benseler, F.; Aurup, H.; Eckstein, F. Kinetic Characterization of Ribonuclease-Resistant 2′-Modified Hammerhead Ribozymes. Science 1991, 253, 314–317. [CrossRef]
- Drolet, D.W.; Green, L.S.; Gold, L.; Janjic, N. Fit for the Eye: Aptamers in Ocular Disorders. Nucleic Acid Ther 2016, 26, 127–146. [CrossRef]
- Gragoudas, E.S.; Adamis, A.P.; Cunningham, E.T.; Feinsod, M.; Guyer, D.R. Pegaptanib for Neovascular Age-Related Macular Degeneration. N Engl J Med 2004, 351, 2805–2816. [CrossRef]
- Swanton, C.; Bernard, E.; Abbosh, C.; André, F.; Auwerx, J.; Balmain, A.; Bar-Sagi, D.; Bernards, R.; Bullman, S.; DeGregori, J.; et al. Embracing Cancer Complexity: Hallmarks of Systemic Disease. Cell 2024, 187, 1589–1616. [CrossRef]
- Takahashi, M.; Wakabayashi, K. Gene Mutations and Altered Gene Expression in Azoxymethane-Induced Colon Carcinogenesis in Rodents. Cancer Sci 2004, 95, 475–480. [CrossRef]
- Armaghany, T.; Wilson, J.D.; Chu, Q.; Mills, G. Genetic Alterations in Colorectal Cancer. Gastrointest Cancer Res 2012, 5, 19–27.
- Cree, I.A.; Charlton, P. Molecular Chess? Hallmarks of Anti-Cancer Drug Resistance. BMC Cancer 2017, 17, 10. [CrossRef]
- Cooper, G.M. The Development and Causes of Cancer. In The Cell: A Molecular Approach. 2nd edition; Sinauer Associates, 2000.
- Ajt, A.J.; Me, R.M.; Rg, R.; Am, G.; Lh, D.O.; So, B.; Neto J, S.; Oh, K.; Ja, R.J.; Ja, R.N. Malignant Small Bowel Tumor - Case Series and Literature Review. Colorec Cancer 2018, 04. [CrossRef]
- Lesniewska-Kowiel, M.A.; Muszalska, I. Strategies in the Designing of Prodrugs, Taking into Account the Antiviral and Anticancer Compounds. Eur J Med Chem 2017, 129, 53–71. [CrossRef]
- Beeharry, N.; Landrette, S.; Gayle, S.; Hernandez, M.; Grotzke, J.E.; Young, P.R.; Beckett, P.; Zhang, X.; Carter, B.Z.; Andreeff, M.; et al. LAM-003, a New Drug for Treatment of Tyrosine Kinase Inhibitor-Resistant FLT3-ITD-Positive AML. Blood Adv 2019, 3, 3661–3673. [CrossRef]
- Evans, K.; Duan, J.; Pritchard, T.; Jones, C.D.; McDermott, L.; Gu, Z.; Toscan, C.E.; El-Zein, N.; Mayoh, C.; Erickson, S.W.; et al. OBI-3424, a Novel AKR1C3-Activated Prodrug, Exhibits Potent Efficacy against Preclinical Models of T-ALL. Clinical Cancer Research 2019, 25, 4493–4503. [CrossRef]
- Torabifard, H.; Fattahi, A. Mechanisms and Kinetics of Thiotepa and Tepa Hydrolysis: DFT Study. J Mol Model 2012, 18, 3563–3576. [CrossRef]
- Birbo, B.; Madu, E.E.; Madu, C.O.; Jain, A.; Lu, Y. Role of HSP90 in Cancer. IJMS 2021, 22, 10317. [CrossRef]
- Gutierrez, M.; Guo, R.; Giaccone, G.; Liu, S.V.; Hao, Z.; Hilton, C.; Hinson, J.M.; Kris, M.G.; Orlemans, E.O.; Drilon, A. Phase 1 Multicenter Study of the HSP90 Inhibitor SNX-5422 plus Carboplatin and Paclitaxel in Patients with Lung Cancers. Lung Cancer 2021, 162, 23–28. [CrossRef]
- Puyo, S.; Montaudon, D.; Pourquier, P. From Old Alkylating Agents to New Minor Groove Binders. Crit Rev Oncol Hematol 2014, 89, 43–61. [CrossRef]
- Bagshawe, K.D. ADEPT and Related Concepts. Cell Biophysics 1994, 24–25, 83–91. [CrossRef]
- Sharma, S.K.; Bagshawe, K.D. Antibody Directed Enzyme Prodrug Therapy (ADEPT): Trials and Tribulations. Advanced Drug Delivery Reviews 2017, 118, 2–7. [CrossRef]
- Yang, S.; Li, N.; Wang, J.; Ma, L.; Zhao, Y.; Chen, H.; Wu, H.; Jiang, W. Abstract 4068: In Vitro Masked Effect, in Vivo Anti-Tumor Activity and Toxicology Study of KGX101, an Interleukin-12 Prodrug, in Monotherapy or in Combination with Anti-PD-L1 Antibody. Cancer Research 2024, 84, 4068. [CrossRef]
- Definition of Anti-CD137 Agonistic Monoclonal Antibody ADG206 - NCI Drug Dictionary - NCI Available online: https://www.cancer.gov/publications/dictionaries/cancer-drug/def/anti-cd137-agonistic-monoclonal-antibody-adg206 (accessed on 21 November 2024).
- Otano, I.; Azpilikueta, A.; Glez-Vaz, J.; Alvarez, M.; Medina-Echeverz, J.; Cortés-Domínguez, I.; Ortiz-de-Solorzano, C.; Ellmark, P.; Fritzell, S.; Hernandez-Hoyos, G.; et al. CD137 (4-1BB) Costimulation of CD8+ T Cells Is More Potent When Provided in Cis than in Trans with Respect to CD3-TCR Stimulation. Nat Commun 2021, 12, 7296. [CrossRef]
- Huang, S.; Fang, R.; Xu, J.; Qiu, S.; Zhang, H.; Du, J.; Cai, S. Evaluation of the Tumor Targeting of a FAPα-Based Doxorubicin Prodrug. J Drug Target 2011, 19, 487–496. [CrossRef]
- Gabizon, A.; Shmeeda, H.; Tahover, E.; Kornev, G.; Patil, Y.; Amitay, Y.; Ohana, P.; Sapir, E.; Zalipsky, S. Development of Promitil®, a Lipidic Prodrug of Mitomycin c in PEGylated Liposomes: From Bench to Bedside. Advanced Drug Delivery Reviews 2020, 154–155, 13–26. [CrossRef]
- Hutchings, M.I.; Truman, A.W.; Wilkinson, B. Antibiotics: Past, Present and Future. Current Opinion in Microbiology 2019, 51, 72–80. [CrossRef]
- Tooke, C.L.; Hinchliffe, P.; Bragginton, E.C.; Colenso, C.K.; Hirvonen, V.H.A.; Takebayashi, Y.; Spencer, J. β-Lactamases and β-Lactamase Inhibitors in the 21st Century. J Mol Biol 2019, 431, 3472–3500. [CrossRef]
- Lewis, K. The Science of Antibiotic Discovery. Cell 2020, 181, 29–45. [CrossRef]
- Erah, P.O.; Goddard, A.F.; Barrett, D.A.; Shaw, P.N.; Spiller, R.C. The Stability of Amoxycillin, Clarithromycin and Metronidazole in Gastric Juice: Relevance to the Treatment of Helicobacter Pylori Infection. Journal of Antimicrobial Chemotherapy 1997, 39, 5–12. [CrossRef]
- Reddy, K.R.; Parkinson, J.; Sabet, M.; Tarazi, Z.; Boyer, S.H.; Lomovskaya, O.; Griffith, D.C.; Hecker, S.J.; Dudley, M.N. Selection of QPX7831, an Orally Bioavailable Prodrug of Boronic Acid β-Lactamase Inhibitor QPX7728. J. Med. Chem. 2021, 64, 17523–17529. [CrossRef]
- Lavis, L.D. Ester Bonds in Prodrugs. ACS Chem. Biol. 2008, 3, 203–206. [CrossRef]
- Cotroneo, N.; Stokes, S.S.; Pucci, M.J.; Rubio, A.; Hamed, K.A.; Critchley, I.A. Efficacy of SPR720 in Murine Models of Non-Tuberculous Mycobacterial Pulmonary Infection. Journal of Antimicrobial Chemotherapy 2024, 79, 875–882. [CrossRef]
- Flamm, R.K.; Rhomberg, P.R.; Kaplan, N.; Jones, R.N.; Farrell, D.J. Activity of Debio1452, a FabI Inhibitor with Potent Activity against Staphylococcus Aureus and Coagulase-Negative Staphylococcus Spp., Including Multidrug-Resistant Strains. Antimicrob Agents Chemother 2015, 59, 2583–2587. [CrossRef]
- Hafkin, B.; Berg, J.K.; Kaplan, N.; Métral, V.N.; Ménétrey, A.; Alcorn, H.; Wittke, F. Single-Dose Escalation Study to Evaluate the Safety, Tolerability, and Pharmacokinetics of a FabI Inhibitor, the Prodrug Debio 1450 and Its Active Moiety Debio 1452, Administered Intravenously in Healthy Subjects. Open Forum Infectious Diseases 2015, 2, 797. [CrossRef]
- Trout, R.E.; Zulli, A.; Mesaros, E.; Jackson, R.W.; Boyd, S.; Liu, B.; Hamrick, J.; Daigle, D.; Chatwin, C.L.; John, K.; et al. Discovery of VNRX-7145 (VNRX-5236 Etzadroxil): An Orally Bioavailable β-Lactamase Inhibitor for Enterobacterales Expressing Ambler Class A, C, and D Enzymes. J Med Chem 2021, 64, 10155–10166. [CrossRef]
- Iqbal, K.; Milioudi, A.; Wicha, S.G. Pharmacokinetics and Pharmacodynamics of Tedizolid. Clin Pharmacokinet 2022, 61, 489–503. [CrossRef]
- Kilmarx, P.H. Global Epidemiology of HIV: Current Opinion in HIV and AIDS 2009, 4, 240–246. [CrossRef]
- Greene, W.C. A History of AIDS: Looking Back to See Ahead. Eur. J. Immunol. 2007, 37, S94–S102. [CrossRef]
- Agarwal-Jans, S. Timeline: HIV. Cell 2020, 183, 550. [CrossRef]
- Nowicka-Sans, B.; Gong, Y.-F.; McAuliffe, B.; Dicker, I.; Ho, H.-T.; Zhou, N.; Eggers, B.; Lin, P.-F.; Ray, N.; Wind-Rotolo, M.; et al. In Vitro Antiviral Characteristics of HIV-1 Attachment Inhibitor BMS-626529, the Active Component of the Prodrug BMS-663068. Antimicrob Agents Chemother 2012, 56, 3498–3507. [CrossRef]
- Zhou, N.; Nowicka-Sans, B.; McAuliffe, B.; Ray, N.; Eggers, B.; Fang, H.; Fan, L.; Healy, M.; Langley, D.R.; Hwang, C.; et al. Genotypic Correlates of Susceptibility to HIV-1 Attachment Inhibitor BMS-626529, the Active Agent of the Prodrug BMS-663068. J Antimicrob Chemother 2014, 69, 573–581. [CrossRef]
- Hoffman, R.L.; Kania, R.S.; Brothers, M.A.; Davies, J.F.; Ferre, R.A.; Gajiwala, K.S.; He, M.; Hogan, R.J.; Kozminski, K.; Li, L.Y.; et al. Discovery of Ketone-Based Covalent Inhibitors of Coronavirus 3CL Proteases for the Potential Therapeutic Treatment of COVID-19. J Med Chem 2020, 63, 12725–12747. [CrossRef]
- Yuen, M.-F.; Balabanska, R.; Cottreel, E.; Chen, E.; Duan, D.; Jiang, Q.; Patil, A.; Triyatni, M.; Upmanyu, R.; Zhu, Y.; et al. TLR7 Agonist RO7020531 versus Placebo in Healthy Volunteers and Patients with Chronic Hepatitis B Virus Infection: A Randomised, Observer-Blind, Placebo-Controlled, Phase 1 Trial. The Lancet Infectious Diseases 2023, 23, 496–507. [CrossRef]
- Palmer, A.M.; Stephenson, F.A. CNS Drug Discovery: Challenges and Solutions. Drug News Perspect 2005, 18, 51–57.
- Central Nervous System Drugs Global Market Report 2022 Available online: https://finance.yahoo.com/news/central-nervous-system-drugs-global-075400795.html (accessed on 26 September 2024).
- Ruiz-López, E.; Schuhmacher, A.J. Transportation of Single-Domain Antibodies through the Blood–Brain Barrier. Biomolecules 2021, 11, 1131. [CrossRef]
- Rankovic, Z. CNS Drug Design: Balancing Physicochemical Properties for Optimal Brain Exposure. J. Med. Chem. 2015, 58, 2584–2608. [CrossRef]
- Abbott, N.J.; Patabendige, A.A.K.; Dolman, D.E.M.; Yusof, S.R.; Begley, D.J. Structure and Function of the Blood-Brain Barrier. Neurobiol Dis 2010, 37, 13–25. [CrossRef]
- Okamoto, M.; Gray, J.D.; Larson, C.S.; Kazim, S.F.; Soya, H.; McEwen, B.S.; Pereira, A.C. Riluzole Reduces Amyloid Beta Pathology, Improves Memory, and Restores Gene Expression Changes in a Transgenic Mouse Model of Early-Onset Alzheimer’s Disease. Transl Psychiatry 2018, 8, 1–13. [CrossRef]
- Silk, A.W.; Saraiya, B.; Groisberg, R.; Chan, N.; Spencer, K.; Girda, E.; Shih, W.; Palmeri, M.; Saunders, T.; Berman, R.M.; et al. A Phase Ib Dose-Escalation Study of Troriluzole (BHV-4157), an Oral Glutamatergic Signaling Modulator, in Combination with Nivolumab in Patients with Advanced Solid Tumors. Eur J Med Res 2022, 27, 107. [CrossRef]
- Grassi, G.; Cecchelli, C.; Vignozzi, L.; Pacini, S. Investigational and Experimental Drugs to Treat Obsessive-Compulsive Disorder. J Exp Pharmacol 2020, 12, 695–706. [CrossRef]
- Meglio, marco Biohaven Submits New Drug Application for Troriluzole as Spinocerebellar Ataxia Type 3 Therapy Available online: https://www.neurologylive.com/view/biohaven-submits-new-drug-application-for-troriluzole-spinocerebellar-ataxia-type-3-therapy (accessed on 21 November 2024).
- Passie, T.; Seifert, J.; Schneider, U.; Emrich, H.M. The Pharmacology of Psilocybin. Addict Biol 2002, 7, 357–364. [CrossRef]
- Nichols, D.E. Psilocybin: From Ancient Magic to Modern Medicine. J Antibiot (Tokyo) 2020, 73, 679–686. [CrossRef]
- Sharp, T.; Collins, H. Mechanisms of SSRI Therapy and Discontinuation. Curr Top Behav Neurosci 2024, 66, 21–47. [CrossRef]
- Mi, W.; Yang, F.; Li, H.; Xu, X.; Li, L.; Tan, Q.; Wang, G.; Zhang, K.; Tian, F.; Luo, J.; et al. Efficacy, Safety, and Tolerability of Ansofaxine (LY03005) Extended-Release Tablet for Major Depressive Disorder: A Randomized, Double-Blind, Placebo-Controlled, Dose-Finding, Phase 2 Clinical Trial. Int J Neuropsychopharmacol 2021, 25, 252–260. [CrossRef]
- A Phase 3, Multicenter, Double-Blind, Randomized, Placebo-Controlled Clinical Trial to Verify the Efficacy and Safety of Ansofaxine (LY03005) for Major Depressive Disorder | Translational Psychiatry Available online: https://www.nature.com/articles/s41398-023-02435-0 (accessed on 23 September 2024).
- DeLucia, R.; Planeta, C.S. Fencamfamine. Gen Pharmacol 1990, 21, 161–163. [CrossRef]
- Gorenstein, C.; DeLucia, R.; Gentil, V. Psychostimulant Effects of Fencamfamine in Healthy Volunteers. Braz J Med Biol Res 1988, 21, 475–477.
- Leon Duque, M.A.; Vallavoju, N.; Woo, C.M. Chemical Tools for the Opioids. Mol Cell Neurosci 2023, 125, 103845. [CrossRef]
- Baldo, B.A.; Rose, M.A. Mechanisms of Opioid-Induced Respiratory Depression. Arch Toxicol 2022, 96, 2247–2260. [CrossRef]
- Montinari, M.R.; Minelli, S.; De Caterina, R. The First 3500 years of Aspirin History from Its Roots - A Concise Summary. Vascul Pharmacol 2019, 113, 1–8. [CrossRef]
- Vane, J.R.; Botting, R.M. Anti-Inflammatory Drugs and Their Mechanism of Action. Inflamm Res 1998, 47 Suppl 2, S78-87. [CrossRef]
- Jensen, S.; Seidelin, J.B.; LaCasse, E.C.; Nielsen, O.H. SMAC Mimetics and RIPK Inhibitors as Therapeutics for Chronic Inflammatory Diseases. Sci Signal 2020, 13, eaax8295. [CrossRef]
- Tian, E.; Zhou, C.; Quan, S.; Su, C.; Zhang, G.; Yu, Q.; Li, J.; Zhang, J. RIPK2 Inhibitors for Disease Therapy: Current Status and Perspectives. European Journal of Medicinal Chemistry 2023, 259, 115683. [CrossRef]
- Alles, S.R.A.; Smith, P.A. Peripheral Voltage-Gated Cation Channels in Neuropathic Pain and Their Potential as Therapeutic Targets. Front Pain Res (Lausanne) 2021, 2, 750583. [CrossRef]
- Hijma, H.J.; Siebenga, P.S.; de Kam, M.L.; Groeneveld, G.J. A Phase 1, Randomized, Double-Blind, Placebo-Controlled, Crossover Study to Evaluate the Pharmacodynamic Effects of VX-150, a Highly Selective NaV1.8 Inhibitor, in Healthy Male Adults. Pain Med 2021, 22, 1814–1826. [CrossRef]
- Wang, Y.; Hu, S.; Chen, Y.; Chen, M.; Zhang, D.; Liu, W.; Chen, C.; Gan, Y.; Luo, M.; Ke, B. Discovery of a Novel Series of Pyridone Amides as NaV1.8 Inhibitors. Bioorganic & Medicinal Chemistry Letters 2024, 101, 129655. [CrossRef]
- Kornberg, M.D.; Bhargava, P.; Kim, P.M.; Putluri, V.; Snowman, A.M.; Putluri, N.; Calabresi, P.A.; Snyder, S.H. Dimethyl Fumarate Targets GAPDH and Aerobic Glycolysis to Modulate Immunity. Science 2018, 360, 449–453. [CrossRef]
- Okuda, D.T.; Kantarci, O.; Lebrun-Frénay, C.; Sormani, M.P.; Azevedo, C.J.; Bovis, F.; Hua, L.H.; Amezcua, L.; Mowry, E.M.; Hotermans, C.; et al. Dimethyl Fumarate Delays Multiple Sclerosis in Radiologically Isolated Syndrome. Ann Neurol 2023, 93, 604–614. [CrossRef]
- Morand, E.F.; Fernandez-Ruiz, R.; Blazer, A.; Niewold, T.B. Advances in the Management of Systemic Lupus Erythematosus. BMJ 2023, 383, e073980. [CrossRef]
- Stefanski, A.-L.; Tomiak, C.; Pleyer, U.; Dietrich, T.; Burmester, G.R.; Dörner, T. The Diagnosis and Treatment of Sjögren’s Syndrome. Dtsch Arztebl Int 2017, 114, 354–361. [CrossRef]
- Mauro, D.; Thomas, R.; Guggino, G.; Lories, R.; Brown, M.A.; Ciccia, F. Ankylosing Spondylitis: An Autoimmune or Autoinflammatory Disease? Nat Rev Rheumatol 2021, 17, 387–404. [CrossRef]
- Camellino, D.; Giusti, A.; Girasole, G.; Bianchi, G.; Dejaco, C. Pathogenesis, Diagnosis and Management of Polymyalgia Rheumatica. Drugs Aging 2019, 36, 1015–1026. [CrossRef]
- Simakou, T.; Butcher, J.P.; Reid, S.; Henriquez, F.L. Alopecia Areata: A Multifactorial Autoimmune Condition. J Autoimmun 2019, 98, 74–85. [CrossRef]
- Petagna, L.; Antonelli, A.; Ganini, C.; Bellato, V.; Campanelli, M.; Divizia, A.; Efrati, C.; Franceschilli, M.; Guida, A.M.; Ingallinella, S.; et al. Pathophysiology of Crohn’s Disease Inflammation and Recurrence. Biol Direct 2020, 15, 23. [CrossRef]
- Liang, Y.; Sarkar, M.K.; Tsoi, L.C.; Gudjonsson, J.E. Psoriasis: A Mixed Autoimmune and Autoinflammatory Disease. Curr Opin Immunol 2017, 49, 1–8. [CrossRef]
- Swiecicki, P.L.; Hegerova, L.T.; Gertz, M.A. Cold Agglutinin Disease. Blood 2013, 122, 1114–1121. [CrossRef]
- Lahita, R.G. Sex Hormones as Immunomodulators of Disease. Ann N Y Acad Sci 1993, 685, 278–287. [CrossRef]
- Güçlü-Ustündağ, O.; Mazza, G. Saponins: Properties, Applications and Processing. Crit Rev Food Sci Nutr 2007, 47, 231–258. [CrossRef]
- Khan, A.A.; Rejnmark, L.; Rubin, M.; Schwarz, P.; Vokes, T.; Clarke, B.; Ahmed, I.; Hofbauer, L.; Marcocci, C.; Pagotto, U.; et al. PaTH Forward: A Randomized, Double-Blind, Placebo-Controlled Phase 2 Trial of TransCon PTH in Adult Hypoparathyroidism. J Clin Endocrinol Metab 2022, 107, e372–e385. [CrossRef]
- Holten-Andersen, L.; Pihl, S.; Rasmussen, C.E.; Zettler, J.; Maitro, G.; Baron, J.; Heinig, S.; Hoffmann, E.; Wegge, T.; Krusch, M.; et al. Design and Preclinical Development of TransCon PTH, an Investigational Sustained-Release PTH Replacement Therapy for Hypoparathyroidism. J Bone Miner Res 2019, 34, 2075–2086. [CrossRef]
- Pavan, A.R.; Dos Santos, J.L. Advances in Sickle Cell Disease Treatments. Curr Med Chem 2021, 28, 2008–2032. [CrossRef]
- Ferreira De Melo, T.R.; Chin, C.M.; Dos Santos, J.L. What Are the Most Promising Emerging Therapies for Sickle Cell Disease? Future Med. Chem. 2014, 6, 979–982. [CrossRef]
- Kato, G.J.; Piel, F.B.; Reid, C.D.; Gaston, M.H.; Ohene-Frempong, K.; Krishnamurti, L.; Smith, W.R.; Panepinto, J.A.; Weatherall, D.J.; Costa, F.F.; et al. Sickle Cell Disease. Nat Rev Dis Primers 2018, 4, 18010. [CrossRef]
- Riley, C.; Kraft, W.K.; Miller, R. Hydroxyurea in the Sickle Cell Disease Modern Era. Expert Review of Clinical Pharmacology 2024, 17, 777–791. [CrossRef]
- Weaver, S.B.; Singh, D.; Wilson, K.M. Gene Therapies for Sickle Cell Disease. Journal of Pharmacy Technology 2024, 40, 236–247. [CrossRef]
- Pavan, A.R.; Lopes, J.R.; Dos Santos, J.L. The State of the Art of Fetal Hemoglobin-Inducing Agents. Expert Opinion on Drug Discovery 2022, 17, 1279–1293. [CrossRef]
- Perrine, S.P.; Ginder, G.D.; Faller, D.V.; Dover, G.H.; Ikuta, T.; Witkowska, H.E.; Cai, S.P.; Vichinsky, E.P.; Olivieri, N.F. A Short-Term Trial of Butyrate to Stimulate Fetal-Globin-Gene Expression in the Beta-Globin Disorders. N Engl J Med 1993, 328, 81–86. [CrossRef]
- Atweh, G.F.; Sutton, M.; Nassif, I.; Boosalis, V.; Dover, G.J.; Wallenstein, S.; Wright, E.; McMahon, L.; Stamatoyannopoulos, G.; Faller, D.V.; et al. Sustained Induction of Fetal Hemoglobin by Pulse Butyrate Therapy in Sickle Cell Disease. Blood 1999, 93, 1790–1797.
- Kutlar, A.; Reid, M.; Taher, A.T.; Inati, A.; Abboud, M.R.; El-Beshlawy, A.; Buchanan, G.R.; Smith, H.; Ataga, K.I.; Koshy, N.; et al. A Randomized, Open-Label, Multicenter, Dose Escalation Study of HQK-1001 (2,2-Dimethylbutyrate, Sodium Salt) in Sickle Cell Disease. Blood 2012, 120, 998. [CrossRef]
- Kutlar, A.; Ataga, K.; Reid, M.; Vichinsky, E.P.; Neumayr, L.; Blair-Britt, L.; Labotka, R.; Glass, J.; Keefer, J.R.; Wargin, W.A.; et al. A Phase 1/2 Trial of HQK-1001, an Oral Fetal Globin Inducer, in Sickle Cell Disease. American J Hematol 2012, 87, 1017–1021. [CrossRef]
- Kutlar, A.; Reid, M.E.; Inati, A.; Taher, A.T.; Abboud, M.R.; El-Beshlawy, A.; Buchanan, G.R.; Smith, H.; Ataga, K.I.; Perrine, S.P.; et al. A Dose-Escalation Phase IIa Study of 2,2-Dimethylbutyrate (HQK-1001), an Oral Fetal Globin Inducer, in Sickle Cell Disease. Am J Hematol 2013, 88, E255-260. [CrossRef]
- Skarpidi, E.; Cao, H.; Heltweg, B.; White, B.F.; Marhenke, R.L.; Jung, M.; Stamatoyannopoulos, G. Hydroxamide Derivatives of Short-Chain Fatty Acids Are Potent Inducers of Human Fetal Globin Gene Expression. Exp Hematol 2003, 31, 197–203. [CrossRef]
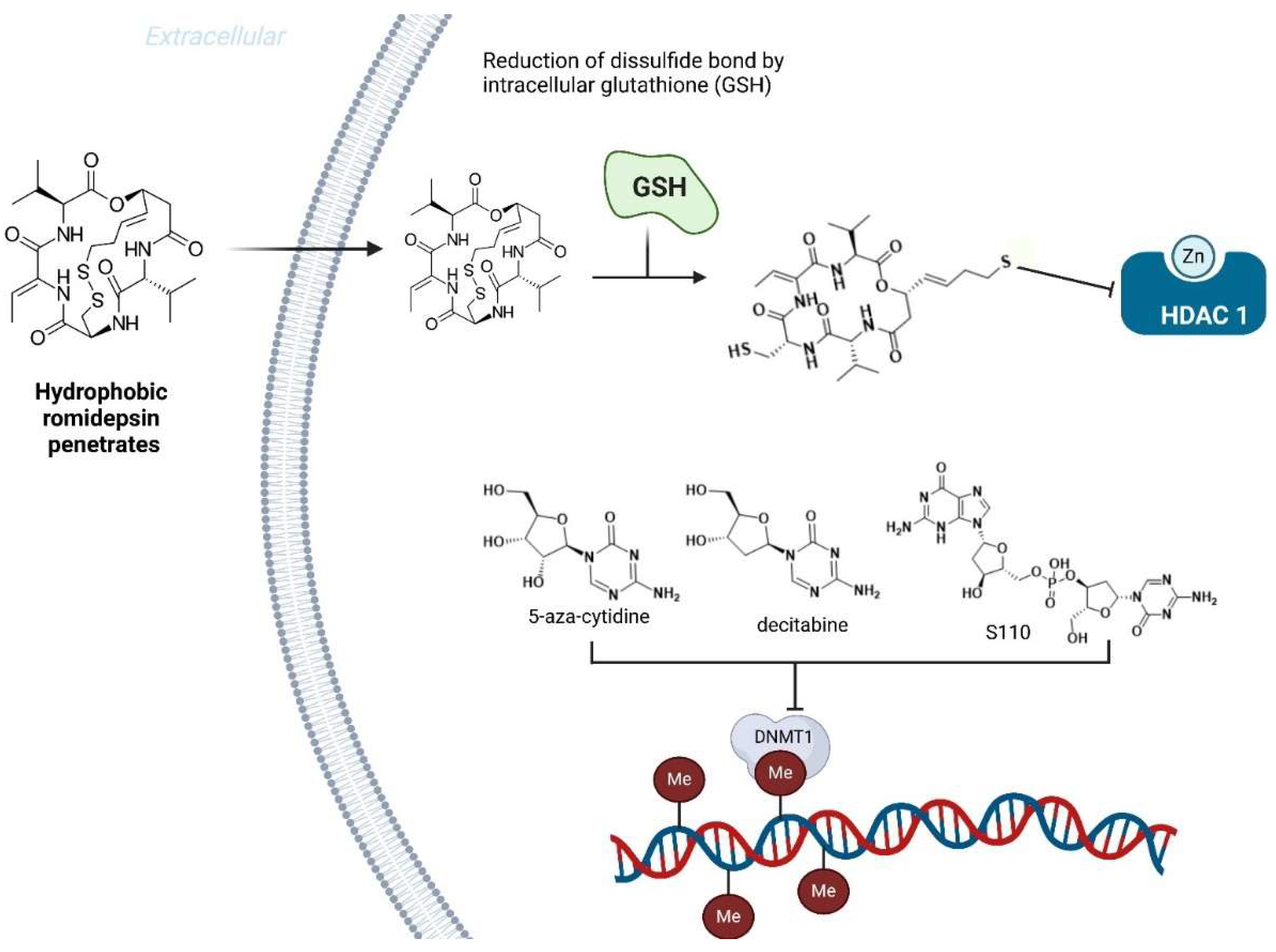
- Cao, H.; Stamatoyannopoulos, G. Histone Deacetylase Inhibitor FK228 Is a Potent Inducer of Human Fetal Hemoglobin. Am J Hematol 2006, 81, 981–983. [CrossRef]
- Okam, M.M.; Esrick, E.B.; Mandell, E.; Campigotto, F.; Neuberg, D.S.; Ebert, B.L. Phase 1/2 Trial of Vorinostat in Patients with Sickle Cell Disease Who Have Not Benefitted from Hydroxyurea. Blood 2015, 125, 3668–3669. [CrossRef]
- Bradner, J.E.; Mak, R.; Tanguturi, S.K.; Mazitschek, R.; Haggarty, S.J.; Ross, K.; Chang, C.Y.; Bosco, J.; West, N.; Morse, E.; et al. Chemical Genetic Strategy Identifies Histone Deacetylase 1 (HDAC1) and HDAC2 as Therapeutic Targets in Sickle Cell Disease. Proc Natl Acad Sci U S A 2010, 107, 12617–12622. [CrossRef]
- Shearstone, J.R.; Golonzhka, O.; Chonkar, A.; Tamang, D.; van Duzer, J.H.; Jones, S.S.; Jarpe, M.B. Chemical Inhibition of Histone Deacetylases 1 and 2 Induces Fetal Hemoglobin through Activation of GATA2. PLoS One 2016, 11, e0153767. [CrossRef]
- Chonkar, A.; Jarpe, M.; Bhol, K.; Jones, S.S.; Shearstone, J.R. The Histone Deacetylase 1 and 2 (HDAC1/2) Inhibitor ACY-957: Impact of Dosing Schedule on Pharmacokinetics (PK), Pharmacodynamics (PD), Hematopoietic Toxicity, and Gamma Globin (HBG, ɣ) Expression in Monkey. Blood 2016, 128, 323–323. [CrossRef]
- Ley, T.; DeSimone, J.; Noguchi, C.; Turner, P.; Schechter, A.; Heller, P.; Nienhuis, A. 5-Azacytidine Increases Gamma-Globin Synthesis and Reduces the Proportion of Dense Cells in Patients with Sickle Cell Anemia. Blood 1983, 62, 370–380. [CrossRef]
- DeSimone, J.; Koshy, M.; Dorn, L.; Lavelle, D.; Bressler, L.; Molokie, R.; Talischy, N. Maintenance of Elevated Fetal Hemoglobin Levels by Decitabine during Dose Interval Treatment of Sickle Cell Anemia. Blood 2002, 99, 3905–3908. [CrossRef]
- Molokie, R.; Lavelle, D.; Gowhari, M.; Pacini, M.; Krauz, L.; Hassan, J.; Ibanez, V.; Ruiz, M.A.; Ng, K.P.; Woost, P.; et al. Oral Tetrahydrouridine and Decitabine for Non-Cytotoxic Epigenetic Gene Regulation in Sickle Cell Disease: A Randomized Phase 1 Study. PLoS Med 2017, 14, e1002382. [CrossRef]
- Lavelle, D.; Saunthararajah, Y.; Vaitkus, K.; Singh, M.; Banzon, V.; Phiasivongsva, P.; Redkar, S.; Kanekal, S.; Bearss, D.; Shi, C.; et al. S110, a Novel Decitabine Dinucleotide, Increases Fetal Hemoglobin Levels in Baboons (P. Anubis). J Transl Med 2010, 8, 92. [CrossRef]
- Singh, V.; Sharma, P.; Capalash, N. DNA Methyltransferase-1 Inhibitors as Epigenetic Therapy for Cancer. CCDT 2013, 13, 379–399. [CrossRef]
- Terra, L.; Abreu, P.A.; Teixeira, V.L.; Paixão, I.C.P.; Pereira, R.; Leal, B.; Lourenço, A.L.; Rampelotto, P.H.; Castro, H.C. Mycoses and Antifungals: Reviewing the Basis of a Current Problem That Still Is a Biotechnological Target for Marine Products. Front. Mar. Sci. 2014, 1. [CrossRef]
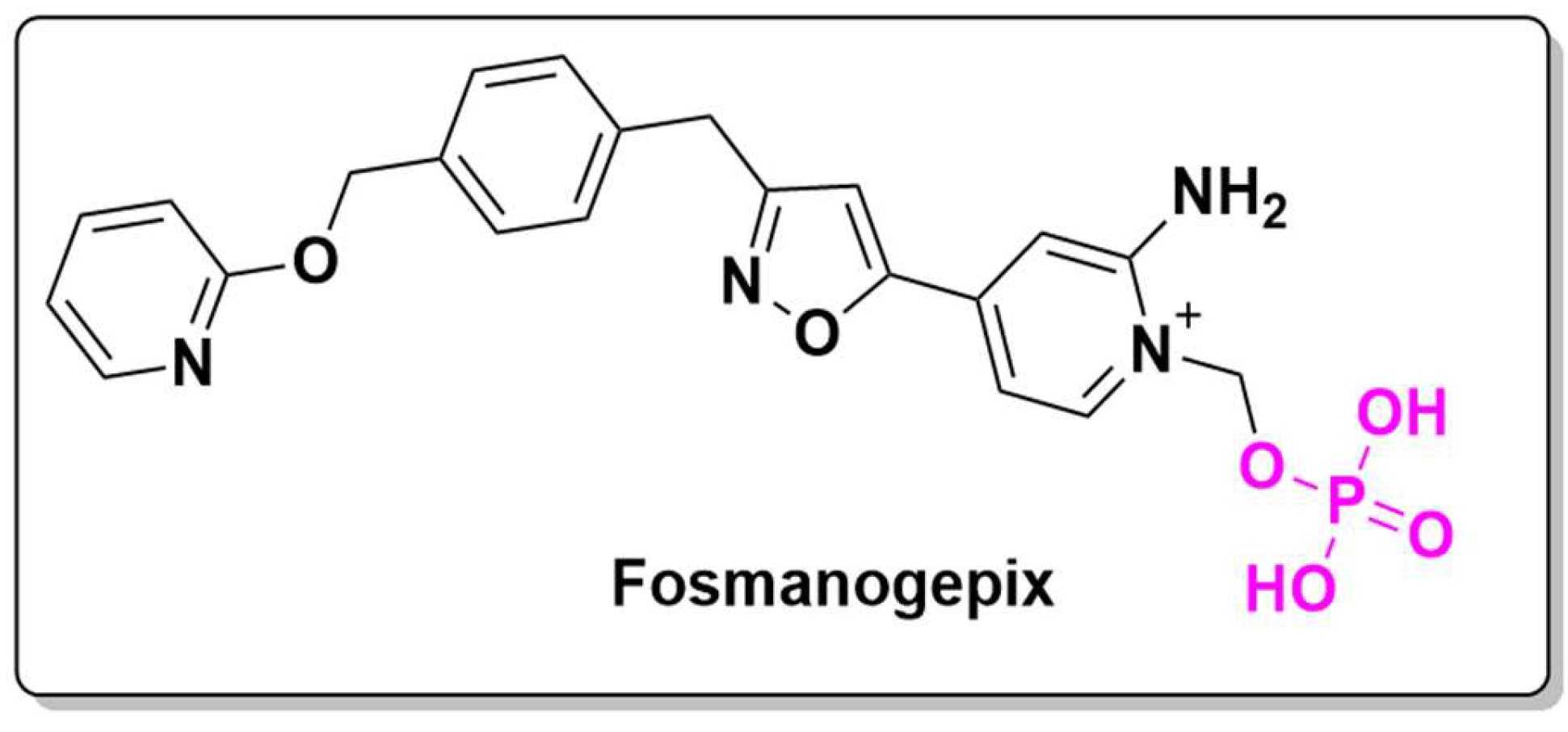
- Shaw, K.J.; Ibrahim, A.S. Fosmanogepix: A Review of the First-in-Class Broad Spectrum Agent for the Treatment of Invasive Fungal Infections. J Fungi (Basel) 2020, 6, 239. [CrossRef]
- Badali, H.; Patterson, H.P.; Sanders, C.J.; Mermella, B.; Gibas, C.F.C.; Ibrahim, A.S.; Shaw, K.J.; Wiederhold, N.P. Manogepix, the Active Moiety of the Investigational Agent Fosmanogepix, Demonstrates In Vitro Activity against Members of the Fusarium Oxysporum and Fusarium Solani Species Complexes. Antimicrob Agents Chemother 2021, 65, e02343-20. [CrossRef]
- Musat, O.; Cernat, C.; Labib, M.; Gheorghe, A.; Toma, O.; Zamfir, M.; Boureanu, A.M. DIABETIC MACULAR EDEMA. Rom J Ophthalmol 2015, 59, 133–136.
- Tatsumi, T. Current Treatments for Diabetic Macular Edema. Int J Mol Sci 2023, 24, 9591. [CrossRef]
- Bhisitkul, R.; Klier, S.; Tsuruda, P.; Xie, B.; Masaki, L.; Bautista, J.; Khan, A.; Dananberg, J. UBX1325, A Novel Senolytic Treatment for Patients with Advanced DME or Wet AMD: 24-Week Results of a Phase 1 Study. Investigative Ophthalmology & Visual Science 2022, 63, 4287.
- Hypertension Available online: https://www.who.int/news-room/fact-sheets/detail/hypertension (accessed on 21 November 2024).
- Dhaneshwar, S.S.; Vadnerkar, G. Rational Design and Development of Colon-Specific Prodrugs. Curr Top Med Chem 2011, 11, 2318–2345. [CrossRef]
- Aiello, R.J.; Bourassa, P.-A.; Zhang, Q.; Dubins, J.; Goldberg, D.R.; De Lombaert, S.; Humbert, M.; Guignabert, C.; Cavasin, M.A.; McKinsey, T.A.; et al. Tryptophan Hydroxylase 1 Inhibition Impacts Pulmonary Vascular Remodeling in Two Rat Models of Pulmonary Hypertension. J Pharmacol Exp Ther 2017, 360, 267–279. [CrossRef]
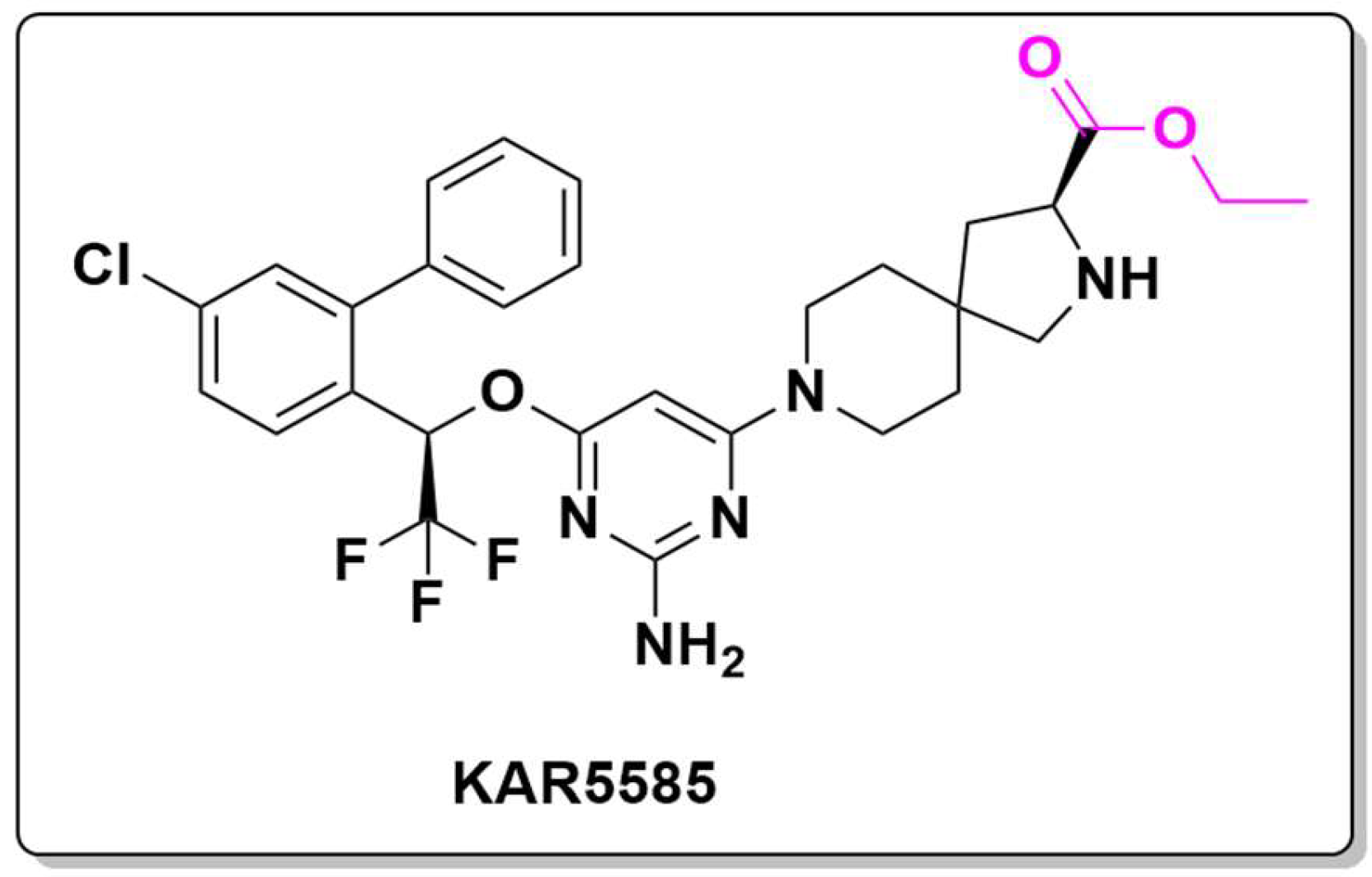
- Paralkar, V.; Pearson, P.; Mason, J.W.; Li, S.-X.; Curry, S.; Aiello, R.; Feig, P.U. KAR5585, a First-in-Class Oral Tryptophan Hydroxylase 1 (TPH1) Inhibitor as a Novel Candidate for the Treatment of Pulmonary Arterial Hypertension. In B71. PULMONARY HYPERTENSION LIFE: ANIMAL MODELS AND EX VIVO STUDIES IN PULMONARY HYPERTENSION; American Thoracic Society International Conference Abstracts; American Thoracic Society, 2017; pp. A4193–A4193.
- Kato, Y.; Fuchi, N.; Saburi, H.; Nishimura, Y.; Watanabe, A.; Yagi, M.; Nakadera, Y.; Higashi, E.; Yamada, M.; Aoki, T. Discovery of 2,8-Diazaspiro[4.5]Decane-Based Trisubstituted Urea Derivatives as Highly Potent Soluble Epoxide Hydrolase Inhibitors and Orally Active Drug Candidates for Treating Hypertension. Bioorganic & Medicinal Chemistry Letters 2013, 23, 5975–5979. [CrossRef]
- Gorman, G.S.; Chinnery, P.F.; DiMauro, S.; Hirano, M.; Koga, Y.; McFarland, R.; Suomalainen, A.; Thorburn, D.R.; Zeviani, M.; Turnbull, D.M. Mitochondrial Diseases. Nat Rev Dis Primers 2016, 2, 16080. [CrossRef]
- Gerards, M.; Sallevelt, S.C.E.H.; Smeets, H.J.M. Leigh Syndrome: Resolving the Clinical and Genetic Heterogeneity Paves the Way for Treatment Options. Mol Genet Metab 2016, 117, 300–312. [CrossRef]
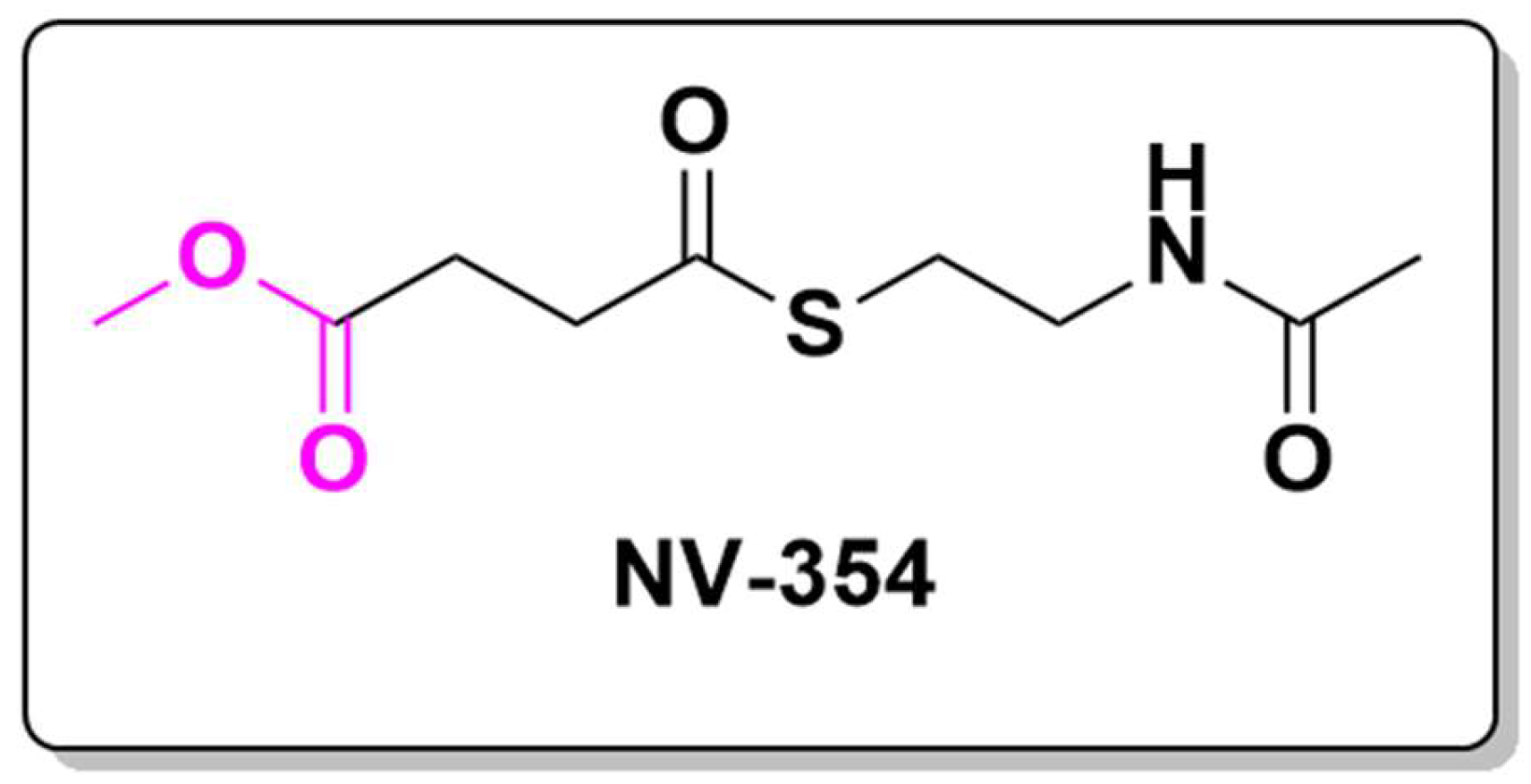
- Ehinger, J.K.; Piel, S.; Ford, R.; Karlsson, M.; Sjövall, F.; Frostner, E.Å.; Morota, S.; Taylor, R.W.; Turnbull, D.M.; Cornell, C.; et al. Cell-Permeable Succinate Prodrugs Bypass Mitochondrial Complex I Deficiency. Nat Commun 2016, 7, 12317. [CrossRef]
- Piel, S.; Janowska, J.I.; Ward, J.L.; McManus, M.J.; Jose, J.S.; Starr, J.; Sheldon, M.; Clayman, C.L.; Elmér, E.; Hansson, M.J.; et al. Succinate Prodrugs in Combination with Atropine and Pralidoxime Protect Cerebral Mitochondrial Function in a Rodent Model of Acute Organophosphate Poisoning. Sci Rep 2022, 12, 20329. [CrossRef]




| NCT ID | ADC ID | Target | Status | Phase | Sponsor |
|
NCT06561607 |
TQB2102 |
Breast cancer with low HER2 expression in the recurrent Metastatic stage | Not yet recruiting | 1 | Chia Tai Tianqing Pharmaceutical Group Co., Ltd. |
|
NCT06496490 |
TQB2102 | Locally advanced or metastatic non-small cell lung cancer with HER2 gene abnormality | Recruiting | 2 | Chia Tai Tianqing Pharmaceutical Group Nanjing Shunxin Pharmaceutical Co., Ltd. |
| NCT06431490 | TQB2102 |
HER2-positive Biliary Tract Cancer |
Recruiting | 1/2 | Chia Tai Tianqing Pharmaceutical Group Nanjing Shunxin Pharmaceutical Co., Ltd. |
| NCT06555744 | ZW191 | Folate Receptor Alpha for Advanced Solid Tumors | Recruiting | 1 | Zymeworks BC Inc. |
| NCT06555263 | Luveltamab Tazevibulin - STRO-002 |
Advanced or metastatic non-small cell lung cancer expressing FOLR1 (FolRα) |
Recruiting | 2 | Sutro Biopharma, Inc. |
| NCT06549816 | Sigvotatug vedotin SGN-B6A |
Advanced solid tumors | Recruiting | 1 | Seagen Inc. |
| NCT06545617 | BAT8006 | Folate receptor α (FRα). Subjects with solid tumors. | Not yet recruiting | 1 | Bio-Thera Solutions |
| NCT06533826 | Datopotamab deruxtecan and Trastuzumab deruxtecan |
HER2-low locally advanced unresectable or metastatic breast cancer (MBC) | Not yet recruiting | 2 | Ana C Garrido-Castro, MD |
| NCT06519370 | FDA018-ADC |
Locally recurrent inoperable or metastatic Triple-negative Breast cancer (TNBC) who are resistant to or recurring during or after taxane therapy. | Recruiting | 3 | Shanghai Fudan-Zhangjiang Bio-Pharmaceutical Co., Ltd. |
|
NCT06509997 |
MRG003 combined with Dalpicicilip posterior line | Recurrent/metastatic CDKN2A gene variant head and neck squamous cell carcinoma (HNSCC) | Not yet recruiting | 2 | Lei Liu, West China Hospital |
|
NCT06465069 |
LY4052031 (enfortumab vedotin-ejfv) |
Anti-nectin-4 advanced or metastatic solid tumors including urothelial cancer. |
Recruiting | 1 | Eli Lilly and Company |
| NCT06457997 | PHN-010 | Advanced solid tumors. | Recruiting | 1b | Pheon Therapeutics |
| NCT06453044 | Polatuzumab vedotin |
Relapsed or Refractory grade 1-3a Follicular Lymphoma | Recruiting | 2 | City of Hope Medical Center |
| NCT06440005 | AGX101 |
Advanced Solid Tumors | Recruiting | 1 | Angiex, Inc. |
| NCT06384807 | PBI-410 |
Advanced Solid Tumors |
Recruiting | 1/2 | Biohaven Therapeutics Ltd. |
| NCT06362252 | Ifinatamab deruxtecan (I-DXd), the ADC in combination with immune checkpoint inhibitor (ICI) atezolizumab with or without carboplatin | Extensive stage-small cell lung cancer (ES-SCLC) in the first line (1L) setting. | Recruiting | 1/2 | Daiichi Sankyo |
| NCT06341400 | RC48 Combined with Toripalimab |
Platinum-intolerant bladder cancer patients. tumor cells |
Recruiting | 1/2 | Zhujiang Hospital |
|
NCT06265727 |
CRB-701 |
Solid tumors that express nectin-4. | Recruiting | 1/2 | Corbus Pharmaceuticals Inc. |
|
NCT06238479 |
LY4101174 |
Humanized immunoglobulin G1 (IgG1) Fcg-silent monoclonal antibody directed against the cell surface adhesion molecule and tumor-associated antigen (TAA) nectin-4 (PVRL4) conjugated, via maleimide-beta-glucuronide poly-sarcosine linkers, to the camptothecin analog and topoisomerase 1 inhibitor exatecan, with potential antineoplastic activity. | Recruiting | 1 | Eli Lilly and Company |
|
NCT06234423 |
CUSP06-1001 |
Platinum-Refractory/Resistant Ovarian Cancer and Other Advanced Solid Tumors |
Recruiting | 1 | OnCusp Therapeutics, Inc. |
|
NCT06210490 |
Disitamab Vedotin |
Adjuvant Treatment of HER2 Overexpressing UTUC Patients with high risk factors for recurrence after radical surgery | Not yet recruiting | 2 | Peking University First Hospital |
|
NCT06210815 |
HLX42 |
EGFR-targeting ADC, for cetuximab or TKI resistant cancer |
Recruiting | Shanghai Henlius Biotech | |
| NCT06144723 | HS-20105 | Targeting Trop-2 advanced solid tumors |
Not yet recruiting | 1/2 | |
|
NCT06132958 |
Sacituzumab Tirumotecan (MK-2870) |
Endometrial cancer (EC) that have previously received treatment with platinum-based therapy. | Recruiting | 3 | Merck Sharp & Dohme LLC |
|
NCT06112704 |
HS-20093 |
Advanced esophageal carcinoma and other solid tumor | Recruiting | 2 | Hansoh BioMedical R&D Company |
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2025 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (http://creativecommons.org/licenses/by/4.0/).





