Submitted:
17 January 2025
Posted:
20 January 2025
You are already at the latest version
Abstract
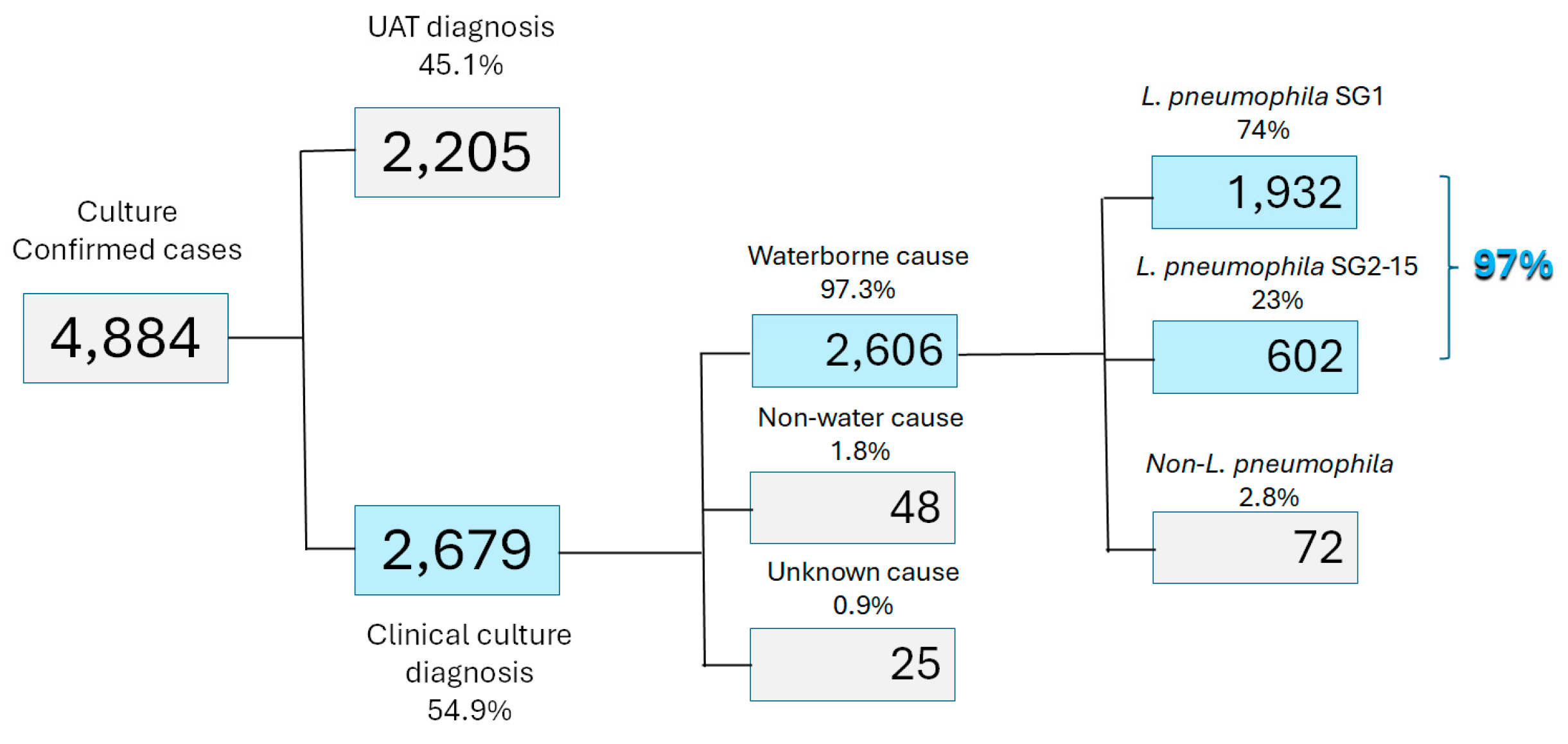
As cases of Legionnaires’ disease increase worldwide, there is uncertainty on whether water management plans should focus on the measurement of Legionella species or specifically on L. pneumophila. This paper makes the case that, for public water systems and buildings, the target organism should be L. pneumophila as it is the overwhelming cause of illness, has simple methods for analysis, and remediation procedures avoid unnecessary costs that produce little public health benefit.
Keywords:
1. Introduction
2. Legionella Overview
3. Methods for Legionella Detection
4. Guidelines for Legionella Management
5. Conclusions
- For both community-acquired and healthcare associated Legionnaires’ disease, L. pneumophila is the overwhelming cause of illness. Waterborne Illnesses due to non-pneumophila species of Legionella are rare, particularly outside clinical environments.
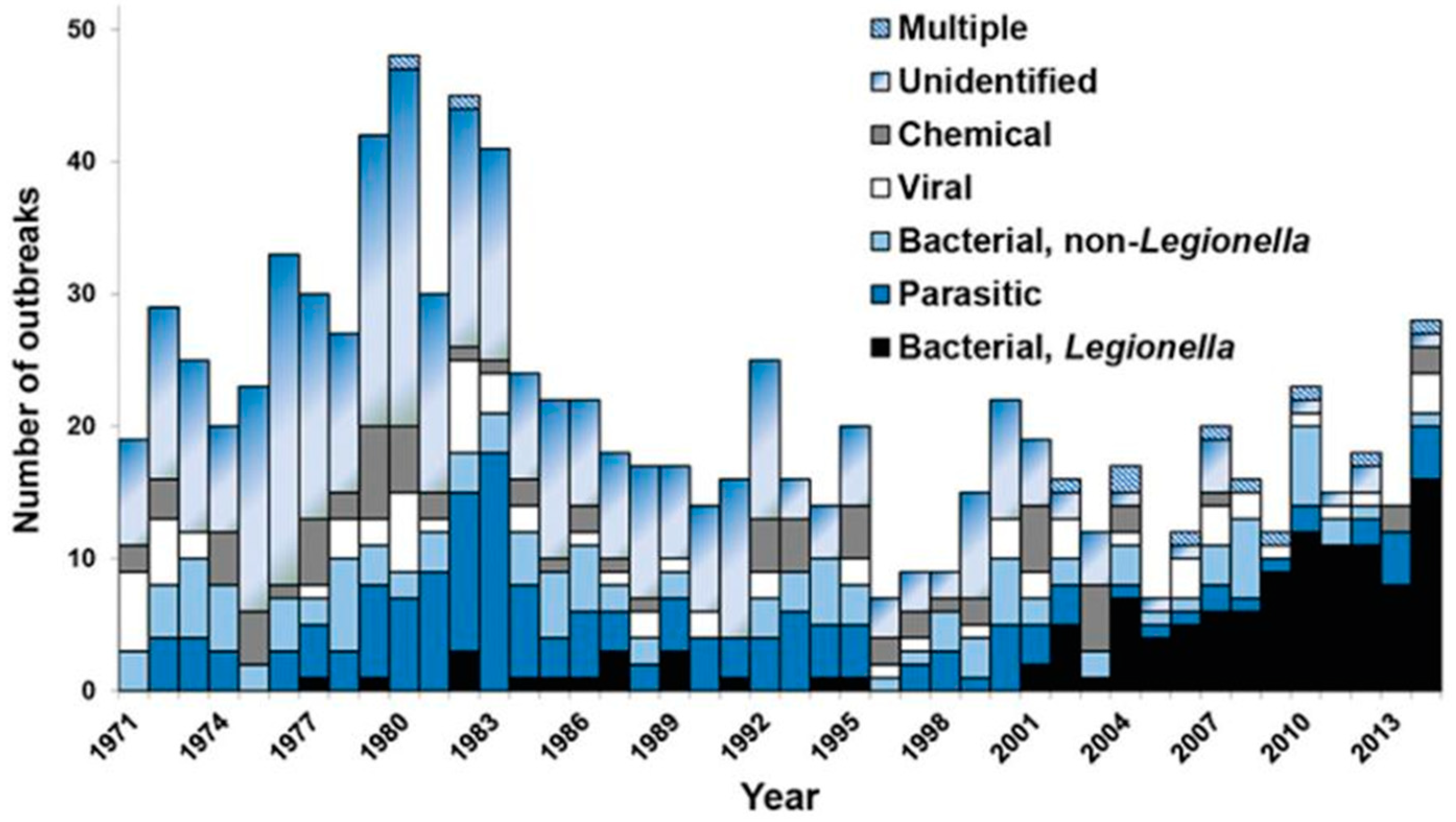
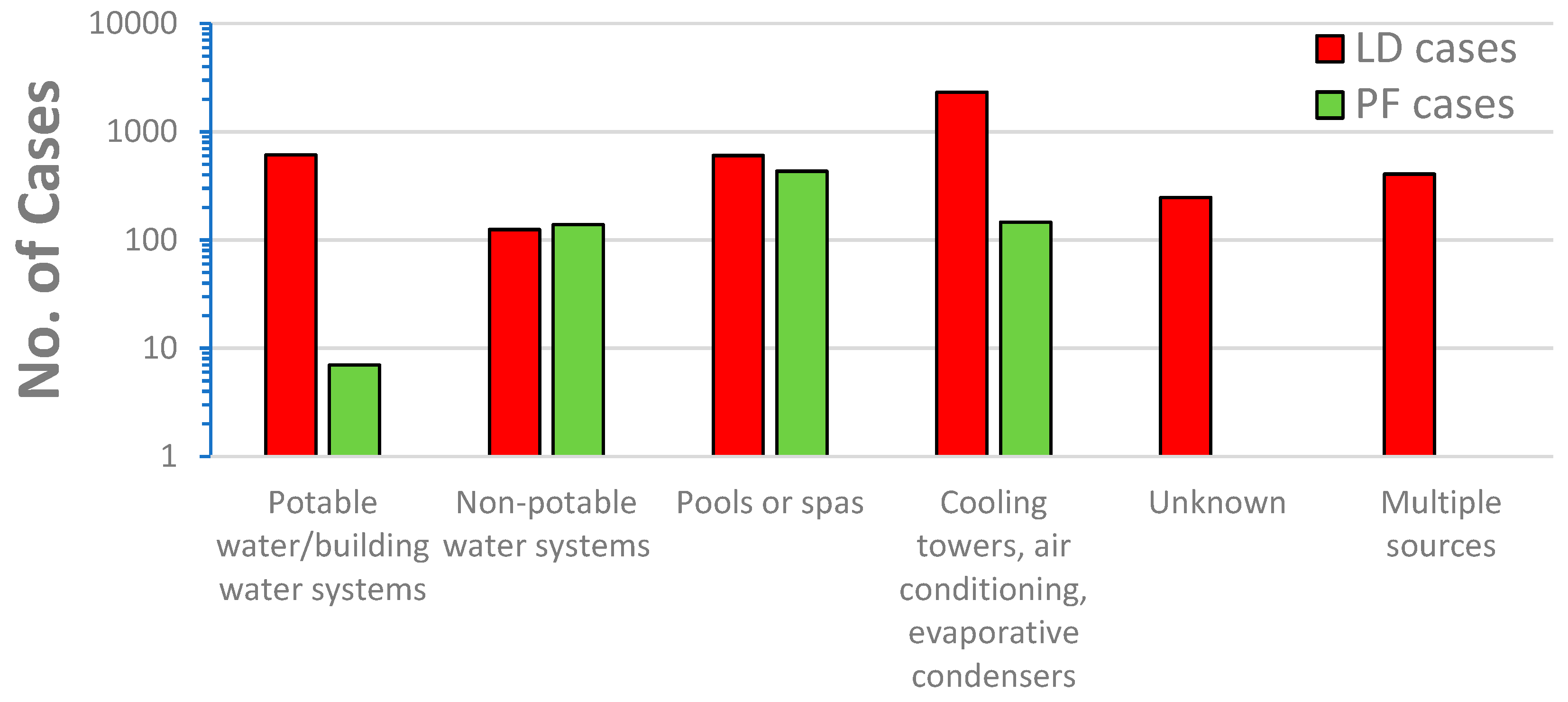
- Although less well studied, cases of Pontiac Fever have not followed the same 20-year trend in increases in cases of Legionnaires’ disease. Most cases of Pontiac Fever are associated with non-potable sources of water.
- The concentration or occurrence of Legionella species has not been shown to be a reliable predictor of L. pneumophila and the health impacts of Legionella species is low relative to L. pneumophila. Treating counts of L. pneumophila and non-pneumophila species equally is without any scientific basis and results in unnecessary cost with little public health benefit.
- Careful consideration must be taken when selecting an appropriate method for monitoring Legionella in water systems. There are many alternatives to the ISO 11731:2017 that are easier to use and provide more accurate analyses. Although molecular methods hold the promise of more rapid analyses, the commercial kits require additional validation and viability analyses need more research. The Legiolert test has proven to be simple, accurate, and feasible for use by water utilities.
- Although a challenge, it would be useful to develop quantitative risk assessments for L. pneumophila and non-pneumophila species in water.
- Countries continue to determine how to focus their guidelines and whether they should promote routine monitoring and control of Legionella species and/or L. pneumophila. One option would be to consider water in clinically significant settings differently from distribution systems or non-health care buildings. It is prudent to hold health care facilities to a higher water quality standard than for potable water systems or public buildings when severely immunocompromised patients may be present.
Author Contributions
Funding
Author
Acknowledgments
Conflicts of Interest
References
- NASEM (National Academies of Sciences, Engineering, and Medicine). 2019. Management of Legionella in Water Systems. Washington, DC: The National Academies Press. [CrossRef]
- Khodr, A., E. Kay, L. Gomez-Valero, C. Ginevra, P. Doublet, C. Buchrieser, and S. Jarraud. 2016. Molecular epidemiology, phylogeny, and evolution of Legionella. Infect Genet Evol. 43:108-122.
- Vaccaro, L., F. Izquierdo, A. Magnet, C. Hurtado, M. A. Salinas, T. Santos Gomes, S. Angulo, S. Salso, J. Pelaez, M. I. Tejeda, A. Alhambra, C. Gómez, A. Enríquez, E. Estirado, S. Fenoy, and C. del Aguila. 2016. First case of Legionnaire’s disease caused by Legionella anisa in Spain and the limitations on the diagnosis of Legionella non-pneumophila infections. PLoS ONE 11(9):e016293.
- Fields, B.S., R.F. Benson, R.E. Besser. 2002. Legionella and Legionnaires’ Disease: 25 Years of Investigation. Clinical Microbiology Reviews, 15(3): 506–526. . [CrossRef]
- Beauté, J., D, Plachouras, S. Sandin, J. Giesecke, P. Sparén. 2020. Healthcare-Associated Legionnaires' Disease, Europe, 2008-2017. Emerging Infectious Diseases, 26(10): 2309-2318. [CrossRef]
- Cross, K. E., J. W. Mercante, A. J. Benitez, E. W. Brown, M. H. Diaz, and J. M. Winchell. 2016. Simultaneous detection of Legionella species and L. anisa, L. bozemanii, L. longbeachae, and L. micdadei using conserved primers and multiple probes in a multiplex real-time PCR assay. Diagnostic Microbiology and Infectious Diseases 85(3):295-301.
- Dooling, K. L., K.-A. Toews, L. A. Hicks, L. E. Garrison, B. Bachaus, S. Zansky, L. R. Carpenter, B. Schaffner, E. Parker, S. Petit, A. Thomas, S. Thomas, R. Mansmann, C. Morin, B. White, and G. E. Langley. 2013. Active bacterial core surveillance for Legionellosis—United States, 2011–2013. Morb. Mortal. Wkly. Rep. 64(42):1190-1193.
- von Baum, H., S. Ewig, R. Marre, N. Suttorp, S. Gonschior, T. Welte, and C. Lück. 2008. Community-acquired Legionella pneumonia: New insights from the German competence network for community acquired pneumonia. Clin. Infect. Dis. 46(9):1356-64.
- Yu, V. L., J. F. Plouffe, M. C. Pastoris, J. E. Stout, M. Schousboe, A. Widmer, J. Summersgill, T. File, C. M. Heath, D. L. Paterson, and A. Chereshsky. 2002. Distribution of Legionella species and serogroups isolated by culture in patients with sporadic community-acquired legionellosis: an international collaborative survey. J. Infect. Dis. 186:127-128.
- Collier, S. A., Deng, L., Adam, E. A., Benedict, K. M., Beshearse, E. M., Blackstock, A. J....Beach, M. J. 2021. Estimate of Burden and Direct Healthcare Cost of Infectious Waterborne Disease in the United States. Emerging Infectious Diseases, 27(1), 140-149. [CrossRef]
- ECDC. 2023. European Centre for Disease Prevention and Control. Legionnaires’ disease. https://www.ecdc.europa.eu/en/legionnaires-disease.
- Whiley, H., and R. Bentham. 2011. Legionella longbeachae and legionellosis. Emerging Infectious Diseases 17(4):579-583.
- Chambers, S.T., Slow, S., Scott-Thomas, A. and Murdoch, D.R., 2021. Legionellosis caused by non-Legionella pneumophila species, with a focus on Legionella longbeachae. Microorganisms, 9(2), p.291. [CrossRef]
- Miyashita, N., Higa, F., Aoki, Y., Kikuchi, T., Seki, M., Tateda, K., Maki, N., Uchino, K., Ogasawara, K., Kiyota, H. and Watanabe, A., 2020. Distribution of Legionella species and serogroups in patients with culture-confirmed Legionella pneumonia. Journal of Infection and Chemotherapy, 26(5), pp.411-417. [CrossRef]
- Romano Spica, V., P. Borella, A. Bruno, C. Carboni, M. Exner, P. Hartemann, G. Gianfranceschi, P. Laganà, A. Mansi, M.T. Montagna, and O. De Giglio. 2024. Legionnaires’ Disease Surveillance and Public Health Policies in Italy: A Mathematical Model for Assessing Prevention Strategies. Water, 16(15), p.2167. [CrossRef]
- Centers for Disease Control and Prevention (CDC). 2025. BEAM (Bacteria, Enterics, Amoeba, and Mycotics) Dashboard. Atlanta, Georgia: U.S. Department of Health and Human Services. www.cdc.gov/ncezid/dfwed/BEAM-dashboard.html. Accessed January 2025. https://data.cdc.gov/Foodborne-Waterborne-and-Related-Diseases/NORS/5xkq-dg7x/data_preview. .
- Kunz JM, Lawinger H, Miko S, et al. Surveillance of Waterborne Disease Outbreaks Associated with Drinking Water — United States, 2015–2020. MMWR Surveill Summ 2024;73(No. SS-1):1–23. http://dx.doi.org/10.15585/mmwr.ss7301a1.
- Hammes, F. 2024. https://media.licdn.com/dms/image/v2/D4D22AQFh4Ro1Ifwp7g/feedshare-shrink_800/feedshare-shrink_800/0/1724099223915?e=1738800000&v=beta&t=kd0-cPi70ARvJf5p-l_8JSJTqAX0ozrmEuEw-nVFOuc (accessed 12/24).
- Holsinger, H., Tucker, N., Regli, S., Studer, K., Roberts, V.A., Collier, S., Hannapel, E., Edens, C., Yoder, J.S. and Rotert, K., 2022. Characterization of reported legionellosis outbreaks associated with buildings served by public drinking water systems: United States, 2001–2017. Journal of Water and Health, 20(4), pp.702-711. [CrossRef]
- Benedict, K. M.; Reses, H.; Vigar, M.; Roth, D. M.; Roberts, V. A.; Mattioli, M.; Colley, L.A. et al. 2017. Surveillance for waterborne disease outbreaks associated with drinking water—United States, 2013–2014. Morbidity and Mortality Weekly Report, 66:44:1216. [CrossRef]
- Hamilton, K.A., A.J. Prussin, W. Ahmed & C.N. Haas. 2018. Outbreaks of Legionnaires’ Disease and Pontiac Fever 2006–2017. Current Environmental Health Reports. 5:263–271. [CrossRef]
- Fields BS, Barbaree JM, Sanden GN, Morrill WE. 1990. Virulence of a Legionella anisa strain associated with Pontiac fever: an evaluation using protozoan, cell culture, and guinea pig models. Infect Immun. 58(9):3139-42. PMID: 2117580.
- Garrison LE, Kunz JM, Cooley LA, et al. 2016. Vital Signs: Deficiencies in Environmental Control Identified in Outbreaks of Legionnaires’ Disease — North America, 2000–2014. MMWR Morb Mortal Wkly Rep 65:576 – 584. [CrossRef]
- Muder, R. R., and L. Y. Victor. 2002. Infection due to Legionella species other than L. pneumophila. Clin. Infect. Dis. 35(8):990-998. [CrossRef]
- Gonçalves, I.G., Fernandes, H.S., Melo, A., Sousa, S.F., Simoes, L.C. and Simoes, M., 2021. LegionellaDB–a database on legionella outbreaks. Trends in Microbiology, 29(10), pp.863-866. [CrossRef]
- LegionellaDB. 2024. LegionellaDB, A database on Legionella outbreaks. https://legionelladb.biosim.pt/ (accessed 12/24).
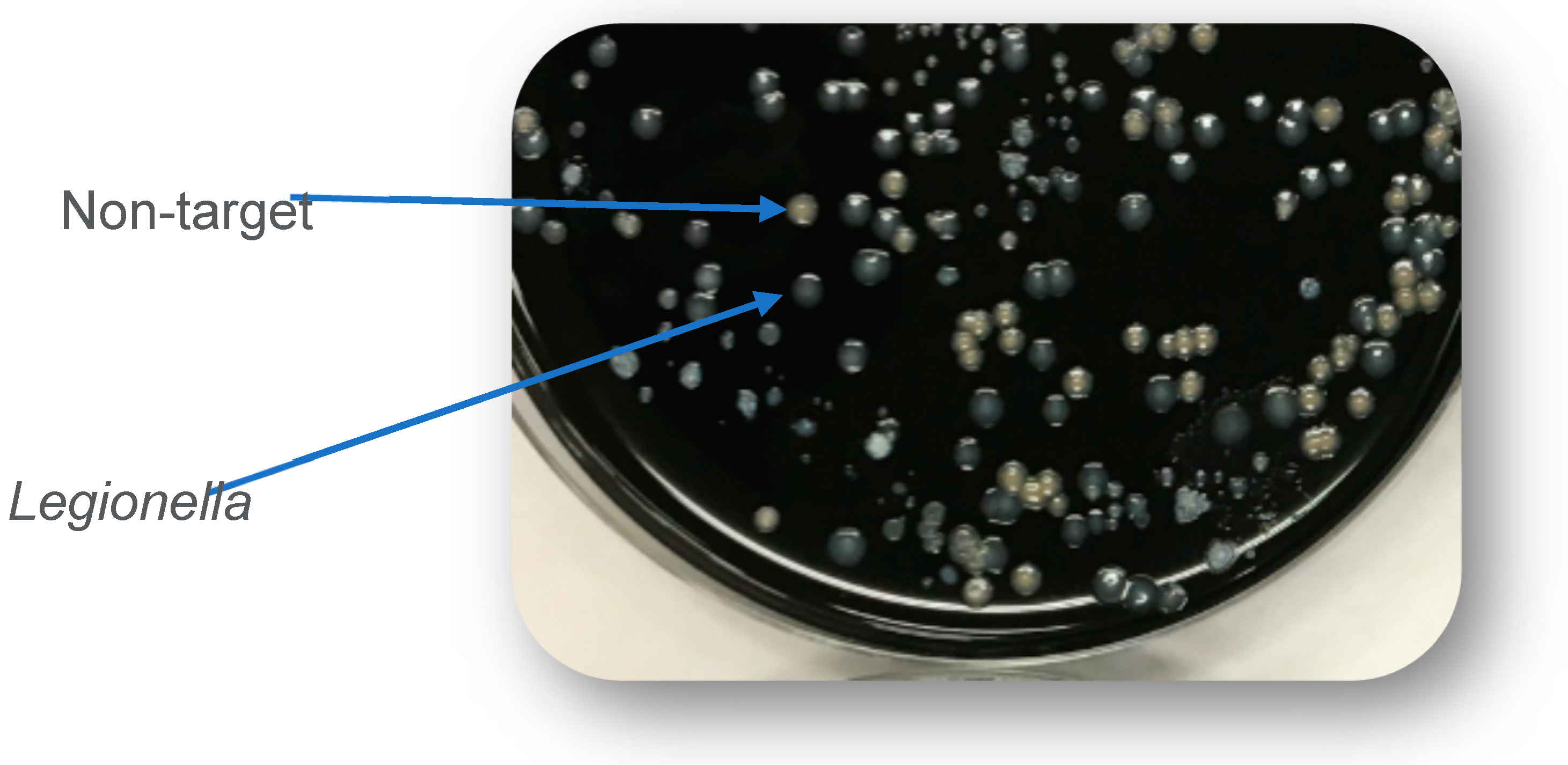
- ISO, 2017. Water Quality – Enumeration of Legionella. ISO 11731:2017. International Organization for Standardization, Geneva, Switzerland. https://www.iso.org/standard/61782.html.
- Lee, T.C., R.M. Vickers, V.L. Yu, M.M. Wagener. 1993. Growth of 28 Legionella Species on Selective Culture Media: a Comparative Study. J. Clin. Microbiol., 31(10): 2764-2768.
- Luck, P.C., Igel, L., Helbig, J.H., Kuhlisch, E., Jatzwauk, L., 2004. Comparison of commercially available media for the recovery of Legionella species. Int. J. Hyg. Environ. Health 207, 589–593.
- Sartory, D.P., Spies, K., Lange, B., Schneider, S., Langer, B., 2017. Evaluation of a most probable number method for the enumeration of Legionella pneumophila from potable and related water samples. Letters in Applied Microbiology 64, 271–275.
- Spies, K., Pleischl, S., Lange, B., Langer, B., Hübner, I., Jurzik, L., Luden, K., Exner, M., 2018. Comparison of the LegiolertTM/Quanti-Tray® MPN test for the enumeration of Legionella pneumophila from potable water samples with the German regulatory requirements methods ISO 11731-2 and ISO 11731. International journal of hygiene and environmental health 221, 1047–1053.
- Petrisek, R., Hall, J., 2017. Evaluation of a most probable number method for the enumeration of Legionella pneumophila from North American potable and nonpotable water samples. Journal of Water and Health 16, 25–33.
- CDC. 2024. Laboratory Testing for Legionella. https://www.cdc.gov/legionella/php/laboratories/index.html (Accessed 12/2024.
- Rech, M.M., Swalla, B.M., Dobranic, J.K., 2018. Evaluation of Legiolert for Quantification of Legionella pneumophila from Non-potable Water. Current Microbiology 75, 1282–1289.
- Barrette, I., 2019. Comparison of Legiolert and a Conventional Culture Method for Detection of Legionella pneumophila from Cooling Towers in Québec. Journal of AOAC International 102, 1235–1240.
- Scaturro, M., Buffoni, M., Girolamo, A., Cristino, S., Girolamini, L., Mazzotta, M., Bucci Sabattini, M.A., Zaccaro, C.M., Chetti, L., Laboratory, M.A.N., 2020. Performance of Legiolert test vs. ISO 11731 to confirm Legionella pneumophila contamination in potable water samples. Pathogens 9, 690.
- Boczek, L.A., Tang, M., Formal, C., Lytle, D., Ryu, H., 2021. Comparison of two culture methods for the enumeration of Legionella pneumophila from potable water samples. Journal of Water and Health 19, 468–477.
- Checa, J., Carbonell, I., Manero, N., Martí, I., 2021. Comparative study of Legiolert with ISO 11731-1998 standard method-conclusions from a Public Health Laboratory. Journal of Microbiological Methods 186, 106242.
- Dowdell, K.S., Greenwald, H.D., Joshi, S., Grimard-Conea, M., Pitell, S., Song, Y., Ley, C., Kennedy, L.C., Vosloo, S., Huo, L., 2022. Legionella pneumophila Occurrence in Reduced-Occupancy Buildings in 11 Cities during the COVID-19 Pandemic. medRxiv. [CrossRef]
- Hirsh, M., Baron, J.L., Mietzner, S., Rihs, J.D., Stout, J.E., 2021. Cross-reactivity of the IDEXX Legiolert Method with other Gram-negative Bacteria and Waterborne Pathogens Leads to False-Positive Assay Results. Letters in Applied Microbiology 72, 750–756. [CrossRef]
- Inoue, H., Baba, M., Tayama, S., 2020. Evaluation of Legiolert for quantification of Legionella pneumophila from bath water samples. Biocontrol Science 25, 179–182.
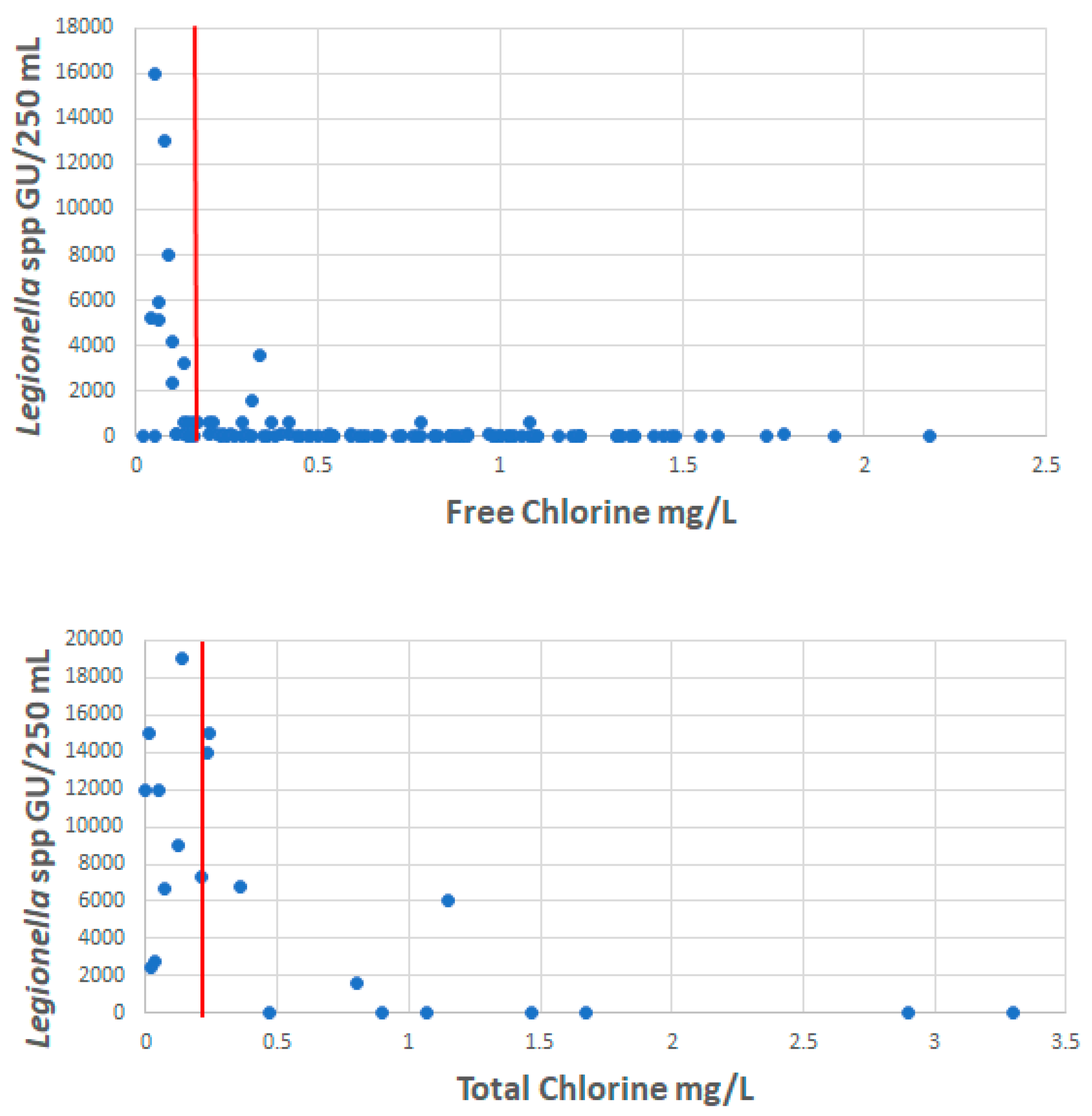
- LeChevallier, M.W. 2019a. Monitoring distribution systems for Legionella pneumophila using Legiolert. AWWA Water Science. 2019:e1122. [CrossRef]
- LeChevallier, M.W. 2019b. Occurrence of culturable Legionella pneumophila in drinking water distribution systems. AWWA Wat Sci. 2019;e1139. . [CrossRef]
- Li, Y., Yang, K., Fu, L., Gong, L., Liu, L., Gao, J., 2021. Comparison of the Legiolert enzyme-substrate method and the conventional cultivation for the detection of Legionella pneumophila in water samples from public places. Journal of Public Health and Preventive Medicine 51–54.
- Mapili, K., Pieper, K.J., Dai, D., Pruden, A., Edwards, M.A., Tang, M., Rhoads, W.J., 2020. Legionella pneumophila Occurrence in Drinking Water Supplied by Private Wells. Letters in Applied Microbiology. [CrossRef]
- Maqbool, A., 2019. Potential for Human Exposure to Legionella near Newtown Creek in Brooklyn, New York. Senior Projects Spring 2019. 176. https://digitalcommons.bard.edu/senproj_s2019/176.
- McCuin, R.M., Bartrand, T.A., Clancy, J.L., 2021. Legionella pneumophila recovery using Legiolert and a traditional culture method. AWWA Water Science 3, e1228.
- Niu, C., Zhang, Yajie, Zhang, Yong, 2022. Evaluation of a Most Probable Number Method for Detection and Quantification of Legionella pneumophila. Pathogens 11, 789. [CrossRef]
- Omoregie, E., Szczerba, A., Novak, J., Rubinstein, I., Chuang, Y., Wu, J., Wang, J., Kretz, C., Hughes, S., Capetanakis, A., 2022. Legionella monitoring in the New York City water distribution system 2017 to 2019. AWWA Water Science 4, e1272.
- Dietersdorfer, E., A. Kirschner, B. Schrammel, A. Ohradanova-Repic, H. Stockinger, R. Sommer, J. Walochnik, and S. Cervero-Arago. 2018. Starved viable but non-culturable (VBNC) Legionella strains can infect and replicate in amoebae and human macrophages. Water Research 141:428-438. [CrossRef]
- Cervero-Aragó, S., B. Schrammel, E. Dietersdorfer, R. Sommer, C. Lück, J. Walochnik, and A. Kirschner. 2019. Viability and infectivity of viable but nonculturable Legionella pneumophila strains induced at high temperatures. Water research 158: 268-279. [CrossRef]
- Steinert, M., L. Emödy, R. Amann, and J. Hacker.1997. Resuscitation of viable but nonculturable Legionella pneumophila Philadelphia JR32 by Acanthamoeba castellanii. Applied and environmental microbiology 63, no. 5 (1997): 2047-2053. [CrossRef]
- Bartrand, T.A., M. LeChevallier, J.L. Clancy, G. Burlingame, R. McCuin. 2024. Occurrence of Legionella pneumophila in Drinking Water Distribution Systems. The Water Research Foundation, Denver, CO. https://www.waterrf.org/research/projects/occurrence-legionella-pneumophila-drinking-water-distribution-systems.
- Wang, H., Edwards, M., Falkinham, J.O., Pruden, A., 2012. Molecular Survey of the Occurrence of Legionella spp., Mycobacterium spp., Pseudomonas aeruginosa, and Amoeba Hosts in Two Chloraminated Drinking Water Distribution Systems. Applied and Environmental Microbiology. 78, 6285–6294. [CrossRef]
- van der Lugt, W., S.M. Euser, J.P. Bruin, J.W. den Boer, and E.P. Yzerman. 2019. Wide-scale study of 206 buildings in the Netherlands from 2011 to 2015 to determine the effect of drinking water management plans on the presence of Legionella spp. Water research, 161, pp.581-589. [CrossRef]
- Wéry, N., V. Bru-Adan, C. Minervini, J.P. Delgénes, L. Garrelly and J.J. Godon. 2008. Dynamics of Legionella spp. and bacterial populations during the proliferation of L. pneumophila in a cooling tower facility. Applied and environmental microbiology, 74(10), pp.3030-3037. [CrossRef]
- AIHA. 2015. Recognition, Evaluation, and Control of Legionella in Building Water Systems. American Industrial Hygiene Association. Falls Church, VA.
- KWR, Berenschot, 2021. Towards a More Effective Legislation for Legionella Control in Drinking Water Systems. Sent to the Dutch House of Representatives by the Minister of Infrastructure and Water Management by letter on November 16 2021. https://open.overheid.nl/documenten/ronl-d2695abf-d88e-4e42-ad99-31d38403cdb9/pdf.
- CDC, 2021. Toolkit for Controlling Legionella in Common Sources of Exposure (Legionella Control Toolkit) [WWW Document]. https://www.cdc.gov/control-legionella/media/pdfs/Control-Toolkit-All-Modules.pdf (Accessed 12/2024).
- ASHRAE (American Society of Heating, Refrigerating and Air-Conditioning Engineers). 2018. Standard 188 legionellosis: Risk management for building water systems. Atlanta, GA: ASHRAE.
- ASHRAE. 2020. ASHRAE Guideline 12-2020. Minimizing the risk of legionellosis associated with building water systems. Atlanta, GA: ASHRAE.
- European Drinking Water Directive. 2020. Directive (EU) 2020/2184 of the European Parliament and of the Council of 16 December 2020 on the quality of water intended for human consumption. https://eur-lex.europa.eu/legal-content/EN/TXT/PDF/?uri=CELEX:32020L2184.
- Doleans, A., H. Aurell, M. Reyrolle, G. Lina, J. Freney, F. Vandenesch, J. Etienne, and S. Jarraud. 2004. Clinical and environmental distributions of Legionella strains in France are different. Journal of Clinical Microbiology, 42(1), pp.458-460. [CrossRef]
- Zacharias, N., F. Waßer, L. Freier, K. Spies, C. Koch, S. Pleischl, N.T. Mutters, and T. Kistemann. 2023. Legionella in drinking water: the detection method matters. Journal of Water and Health, 21(7), pp.884-894. [CrossRef]
- Rucinski, S. L., M. P. Murphy, K. D. Kies, S. A. Cunnignham, A. N. Schuetz, and R. Patel. 2018. Eight years of clinical Legionella PCR testing illustrate seasonal patterns. Clin. Infect. Dis. [CrossRef]
- Cunha, B. A., A. Burillo, and E. Bouza. 2016. Légionnaires’ disease. Lancet. 387(10016):376-385. [CrossRef]
- Hamilton, K.A. and C.N. Haas. 2016. Critical review of mathematical approaches for quantitative microbial risk assessment (QMRA) of Legionella in engineered water systems: research gaps and a new framework. Environmental Science: Water Research & Technology, 2(4), pp.599-613. [CrossRef]
- Bentham, R. and H. Whiley. 2018. Quantitative microbial risk assessment and opportunist waterborne infections–are there too many gaps to fill?. International journal of environmental research and public health, 15(6), p.1150. [CrossRef]
- Kenagy, E., P.C. Priest, C.M. Cameron, D. Smith, P. Scott, V. Cho, P. Mitchell and D.R. Murdoch. 2017. Risk factors for Legionella longbeachae legionnaires’ disease, New Zealand. Emerging infectious diseases, 23(7), p.1148.
| Species | Number in 2020 | Percent of Cases |
| L. pneumphila | 843 | 95.2 |
| L. anisa | 1 | 0.1 |
| L. bozemanii | 6 | 0.7 |
| L. longbeachae | 17 | 1.9 |
| L. micdadei | 7 | 0.8 |
| L. other species | 11 | 1.2 |
| L. species unknown | 15 | 1.7 |
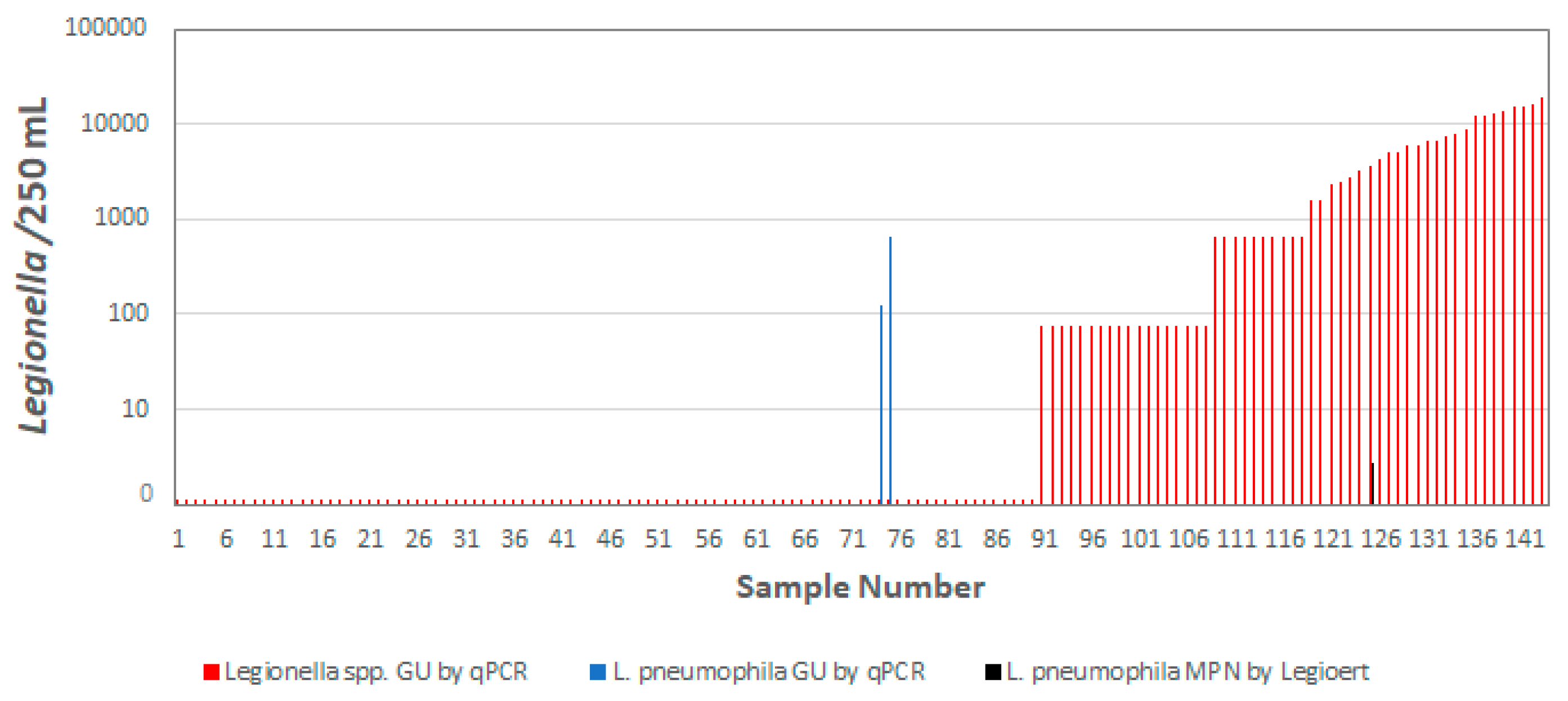
| Drinking Water Distribution System Samples (n=143) | # L. pneumophila positive (Percent) |
|---|---|
| Samples positive by the ISO 11731 method | 0 |
| Samples positive by Legiolert | 1 (0.7%) |
| Samples positive by viability qPCR | 2 (1.4%) |
| Bartrand et al. [53] |
Omoregie et al. [49] |
Wang et al. [54] |
|
|---|---|---|---|
| Samples analyzed | 143 | 544 or 528 1 | 56 |
| Legiolert (L. pneumophila) positive samples (%) | 0.7% | 2.2% | ND |
| ISO method (L. pneumophila) positive samples (%) | 0% | 1.1% | 1.8% |
| viability qPCR/qPCR (L. pneumophila) positive samples (%) | 1.4% | 0.95% | 5.6% |
| Legionella spp. positive samples by v-qPCR2 or qPCR3 (%) | 37% 2 | 84.8% 3 | 86.3% 3 |
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2025 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (http://creativecommons.org/licenses/by/4.0/).





